Developing and Validating a Lung Cancer Risk Prediction Model: A Nationwide Population-Based Study
Abstract
Simple Summary
Abstract
1. Introduction
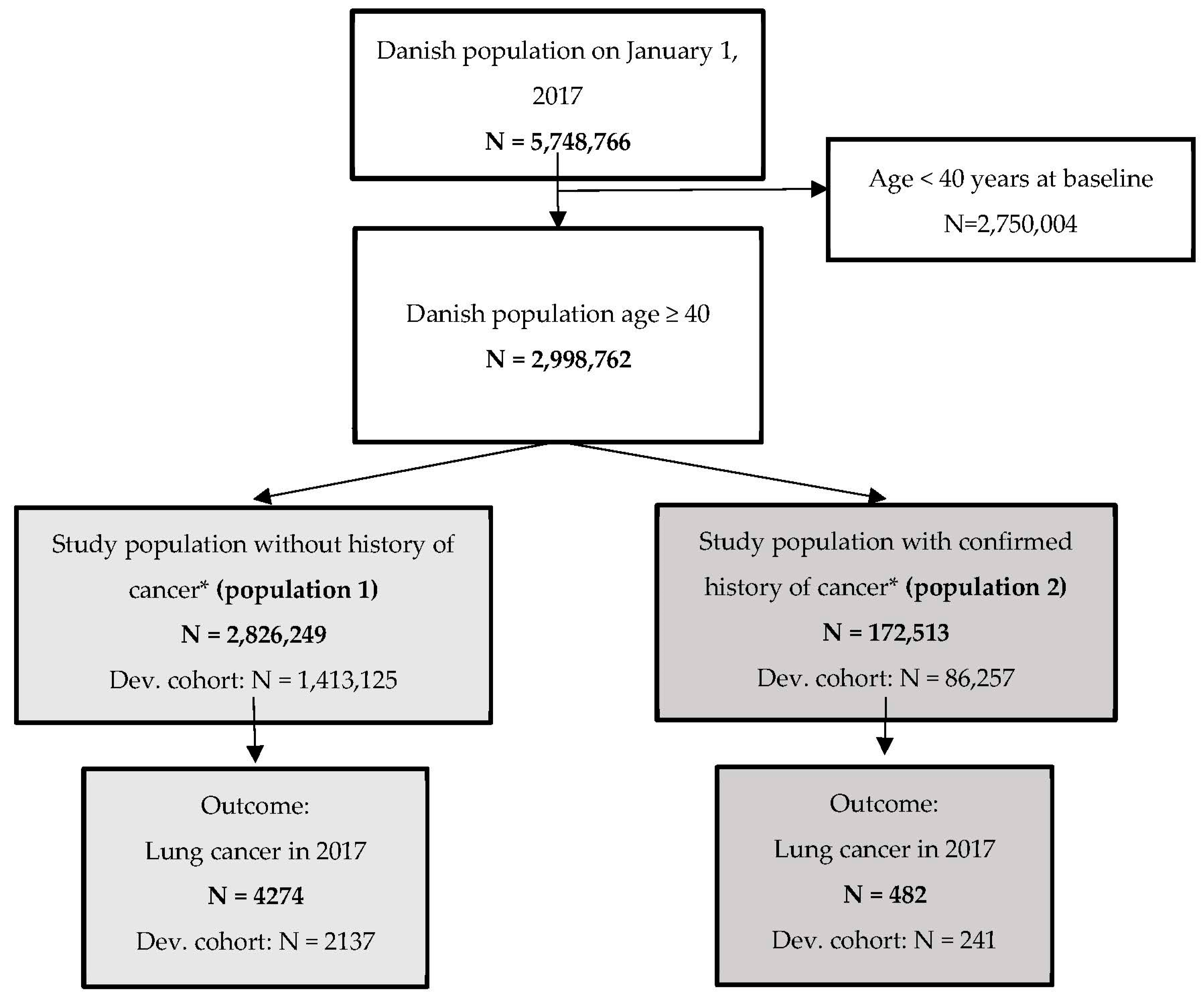
2. Subjects and Methods
2.1. Study Design
2.2. Data Sources
2.2.1. Sociodemographic Data
2.2.2. Cancer Specific Data
2.2.3. Other Health Data
2.3. Outcome (Cancer)
2.4. Statistical Analyses
- Model A contained ICD-10 codes, ATC codes, and GP and specialist contacts, as well as age and sex
- Model B contained ICD-10 codes, ATC codes, GP and specialist contacts, and SES (including marital status and ethnicity), as well as age and sex
- Model C contained age and sex
- Model D contained SES (including marital status and ethnicity)
3. Results
3.1. Predictive Risk Factors for Population 1 (Individuals without a History of Cancer Diagnosis from 2007 to 2016)
3.2. Predictive Risk Factors for Population 2 (Individuals with a History of Cancer Diagnosis from 2007 to 2016)
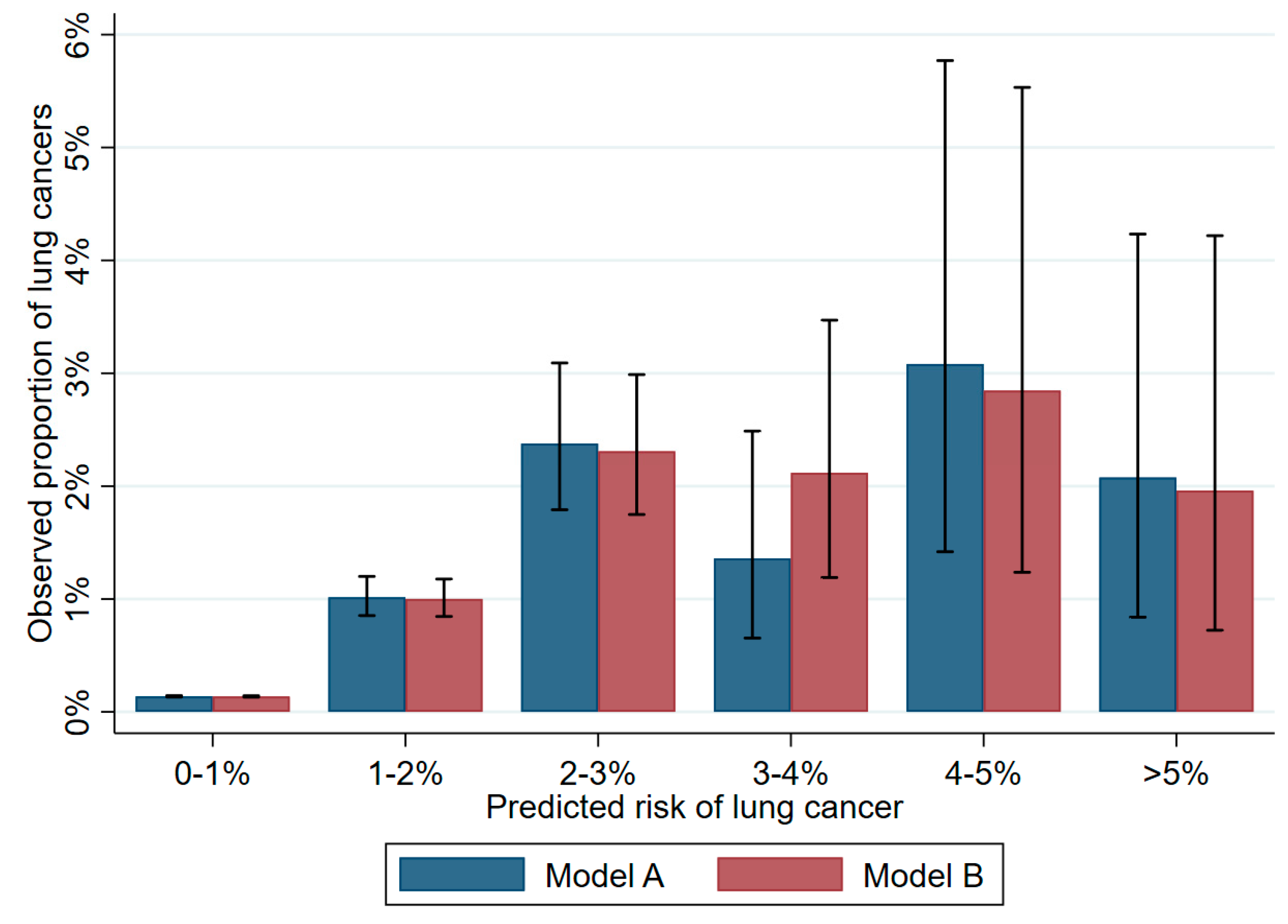
3.3. Validation of the Different Models, Population 1 (Individuals without a History of cancer Diagnosis within 2007 to 2016)
3.4. Validation of the Different Models, Poulation 2 (Individuals wih a History of Cancer Diagnosis within 2007 to 2016)
3.5. Predictive Performance
4. Discussion
4.1. Strengths and Limitations
4.2. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fitzmaurice, C.; Dicker, D.; Pain, A.; Hamavid, H.; Moradi-Lakeh, M.; MacIntyre, M.F.; Allen, C.; Hansen, G.; Woodbrook, R.; Wolfe, C.; et al. The Global Burden of Cancer 2013. JAMA Oncol. 2015, 1, 505–527. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Autier, P.; Boniol, M.; Heanue, M.; Colombet, M.; Boyle, P. Estimates of the cancer incidence and mortality in Europe in 2006. Ann. Oncol. 2007, 18, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Bradley, S.H.; Kennedy, M.P.T.; Neal, R.D. Recognising Lung Cancer in Primary Care. Adv. Ther. 2019, 36, 19–30. [Google Scholar] [CrossRef]
- Shim, J.; Brindle, L.; Simon, M.; George, S. A systematic review of symptomatic diagnosis of lung cancer. Fam. Pract. 2014, 31, 137–148. [Google Scholar] [CrossRef]
- Haastrup, P.F.; Jarbøl, D.E.; Balasubramaniam, K.; Sætre, L.M.S.; Søndergaard, J.; Rasmussen, S. Predictive values of lung cancer alarm symptoms in the general population: A nationwide cohort study. NPJ Prim. Care Respir. Med. 2020, 30, 15. [Google Scholar] [CrossRef]
- Crispo, A.; Brennan, P.; Jöckel, K.H.; Schaffrath-Rosario, A.; Wichmann, H.E.; Nyberg, F.; Simonato, L.; Merletti, F.; Forastiere, F.; Boffetta, P.; et al. The cumulative risk of lung cancer among current, ex- and never-smokers in European men. Br. J. Cancer 2004, 91, 1280–1286. [Google Scholar] [CrossRef]
- Cassidy, A.; Duffy, S.W.; Myles, J.P.; Liloglou, T.; Field, J.K. Lung cancer risk prediction: A tool for early detection. Int. J. Cancer 2007, 120, 1–6. [Google Scholar] [CrossRef]
- Wu, G.X.; Nelson, R.A.; Kim, J.Y.; Raz, D.J. Non–Small Cell Lung Cancer as a Second Primary Among Patients With Previous Malignancy: Who Is at Risk? Clin. Lung Cancer 2017, 18, 543–550.e3. [Google Scholar] [CrossRef]
- Cassidy, A.; Myles, J.P.; van Tongeren, M.; Page, R.D.; Liloglou, T.; Duffy, S.W.; Field, J.K. The LLP risk model: An individual risk prediction model for lung cancer. Br. J. Cancer 2008, 98, 270–276. [Google Scholar] [CrossRef]
- Spitz, M.R.; Hong, W.K.; Amos, C.I.; Wu, X.; Schabath, M.B.; Dong, Q.; Shete, S.; Etzel, C.J. A Risk Model for Prediction of Lung Cancer. JNCI J. Natl. Cancer Inst. 2007, 99, 715–726. [Google Scholar] [CrossRef]
- Hippisley-Cox, J.; Coupland, C. Identifying patients with suspected lung cancer in primary care: Derivation and validation of an algorithm. Br. J. Gen. Pract. 2011, 61, e715–e723. [Google Scholar] [CrossRef]
- Clegg, L.X.; Reichman, M.E.; Miller, B.A.; Hankey, B.F.; Singh, G.K.; Lin, Y.D.; Goodman, M.T.; Lynch, C.F.; Schwartz, S.M.; Chen, V.W.; et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: Selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 2009, 20, 417–435. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.; Cheung, M.C.; Byrne, M.M.; Huang, Y.; Nguyen, D.; Lally, B.E.; Koniaris, L.G. Do racial or socioeconomic disparities exist in lung cancer treatment? Cancer 2010, 116, 2437–2447. [Google Scholar] [CrossRef]
- Jarbøl, D.E.; Hyldig, N.; Möller, S.; Wehberg, S.; Rasmussen, S.; Balasubramaniam, K.; Haastrup, P.F.; Søndergaard, J.; Rubin, K.H. Can National Registries Contribute to Predict the Risk of Cancer? The Cancer Risk Assessment Model (CRAM). Cancers 2022, 14, 3823. [Google Scholar] [CrossRef] [PubMed]
- McCloud, R.F.; Jung, M.; Gray, S.W.; Viswanath, K. Class, race and ethnicity and information avoidance among cancer survivors. Br. J. Cancer 2013, 108, 1949–1956. [Google Scholar] [CrossRef] [PubMed]
- Galarce, E.M.; Ramanadhan, S.; Weeks, J.; Schneider, E.C.; Gray, S.W.; Viswanath, K. Class, race, ethnicity and information needs in post-treatment cancer patients. Patient Educ. Couns. 2011, 85, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.A.; Jensen, H.; Virgilsen, L.F.; Falborg, A.Z.; Møller, H.; Vedsted, P. Time from incident primary cancer until recurrence or second primary cancer: Risk factors and impact in general practice. Eur. J. Cancer Care 2019, 28, e13123. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Schmidt, S.A.J.; Adelborg, K.; Sundboll, J.; Laugesen, K.; Ehrenstein, V.; Sorensen, H.T. The Danish health care system and epidemiological research: From health care contacts to database records. Clin. Epidemiol. 2019, 11, 563–591. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Pedersen, L.; Sorensen, H.T. The Danish Civil Registration System as a tool in epidemiology. Eur. J. Epidemiol. 2014, 29, 541–549. [Google Scholar] [CrossRef]
- Baadsgaard, M.; Quitzau, J. Danish registers on personal income and transfer payments. Scand. J. Public Health 2011, 39, 103–105. [Google Scholar] [CrossRef]
- Jensen, V.M.; Rasmussen, A.W. Danish Education Registers. Scand. J. Public Health 2011, 39, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Gjerstorff, M.L. The Danish Cancer Registry. Scand. J. Public Health 2011, 39, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Schmidt, S.A.; Sandegaard, J.L.; Ehrenstein, V.; Pedersen, L.; Sorensen, H.T. The Danish National Patient Registry: A review of content, data quality, and research potential. Clin. Epidemiol. 2015, 7, 449–490. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Pottegard, A.; Schmidt, S.A.J.; Wallach-Kildemoes, H.; Sorensen, H.T.; Hallas, J.; Schmidt, M. Data Resource Profile: The Danish National Prescription Registry. Int. J. Epidemiol. 2017, 46, 798–798f. [Google Scholar] [CrossRef]
- Gould, M.K.; Huang, B.Z.; Tammemagi, M.C.; Kinar, Y.; Shiff, R. Machine Learning for Early Lung Cancer Identification Using Routine Clinical and Laboratory Data. Am. J. Respir. Crit. Care Med. 2021, 204, 445–453. [Google Scholar] [CrossRef]
- Tammemagi, M.C.; Lam, S. Screening for lung cancer using low dose computed tomography. BMJ Br. Med. J. 2014, 348, g2253. [Google Scholar] [CrossRef]
- Thygesen, L.C.; Ersbøll, A.K. When the entire population is the sample: Strengths and limitations in register-based epidemiology. Eur. J. Epidemiol. 2014, 29, 551–558. [Google Scholar] [CrossRef]
- Crosbie, P.A.J.; Gabe, R.; Simmonds, I.; Hancock, N.; Alexandris, P.; Kennedy, M.; Rogerson, S.; Baldwin, D.; Booton, R.; Bradley, C.; et al. Participation in community-based lung cancer screening: The Yorkshire Lung Screening Trial. Eur. Respir. J. 2022, 60, 2200483. [Google Scholar] [CrossRef]
- Shapley, M.; Mansell, G.; Jordan, J.L.; Jordan, K.P. Positive predictive values of ≥5% in primary care for cancer: Systematic review. Br. J. Gen. Pract. 2010, 60, e366–e377. [Google Scholar] [CrossRef]
- Koo, M.M.; Unger-Saldaña, K.; Mwaka, A.D.; Corbex, M.; Ginsburg, O.; Walter, F.M.; Calanzani, N.; Moodley, J.; Rubin, G.P.; Lyratzopoulos, G. Conceptual Framework to Guide Early Diagnosis Programs for Symptomatic Cancer as Part of Global Cancer Control. JCO Glob. Oncol. 2021, 7, 35–45. [Google Scholar] [CrossRef] [PubMed]
| No history of Cancer (Population 1) | History of Cancer (Population 2) | |||||||
|---|---|---|---|---|---|---|---|---|
| Cases (n = 4274) | Controls (n = 2,821,975) | Cases (n = 482) | Controls (n = 172,031) | |||||
| Development (n = 2137) | Validation (n = 2137) | Development (n = 1,410,988) | Validation (n = 1,410,987) | Development (n = 241) | Validation (n = 241) | Development (n = 86,016) | Validation (n = 86,015) | |
| Age (Median (Q1–Q3)) | 70.9 (64.2–76.7) | 71.0 (63.8–76.9) | 58.3 (49.2–69.5) | 58.3 (49.2–69.6) | 71.7 (66.1–77.6) | 72.7 (67.4–77.8) | 70.2 (61.6–76.9) | 70.2 (61.6–76.9) |
| Age categories | ||||||||
| Age 40.0–59.9 | 302 (14.1%) | 300 (14.0%) | 763,284 (54.1%) | 761,932 (54.0%) | 19 (7.9%) | 13 (5.4%) | 18,773 (21.8%) | 18,831 (21.9%) |
| Age 60.0–79.9 | 1507 (70.5%) | 1521 (71.2%) | 537,684 (38.1%) | 538,598 (38.2%) | 178 (73.9%) | 188 (78.0%) | 52,995 (61.6%) | 52,816 (61.4%) |
| Age ≥ 80.0 | 328 (15.3%) | 316 (14.8%) | 110,020 (7.8%) | 110,457 (7.8%) | 44 (18.3%) | 40 (16.6%) | 14,248 (16.6%) | 14,368 (16.7%) |
| Sex | ||||||||
| Male | 1089 (51.0%) | 1043 (48.8%) | 685,720 (48.6%) | 685,644 (48.6%) | 125 (51.9%) | 138 (57.3%) | 41,027 (47.7%) | 41,128 (47.8%) |
| Female | 1048 (49.0%) | 1094 (51.2%) | 725,268 (51.4%) | 725,343 (51.4%) | 116 (48.1%) | 103 (42.7%) | 44,989 (52.3%) | 44,887 (52.2%) |
| Marital status | ||||||||
| Married | 1110 (51.9%) | 1139 (53.3%) | 830,201 (58.8%) | 831,395 (58.9%) | 134 (55.6%) | 127 (52.7%) | 51,856 (60.3%) | 51,992 (60.4%) |
| Widow or widower | 385 (18.0%) | 383 (17.9%) | 131,362 (9.3%) | 131,660 (9.3%) | 50 (20.7%) | 46 (19.1%) | 14,007 (16.3%) | 13,805 (16.0%) |
| Divorced | 431 (20.2%) | 418 (19.6%) | 226,502 (16.1%) | 225,893 (16.0%) | 41 (17.0%) | 49 (20.3%) | 12,345 (14.4%) | 12,513 (14.5%) |
| Unmarried | 211 (9.9%) | 197 (9.2%) | 222,923 (15.8%) | 222,039 (15.7%) | 16 (6.6%) | 19 (7.9%) | 7808 (9.1%) | 7705 (9.0%) |
| Ethnicity | ||||||||
| Danish | 2046 (95.7%) | 2032 (95.1%) | 1,283,538 (91.0%) | 1,283,637 (91.0%) | 227 (94.2%) | 236 (97.9%) | 81,822 (95.1%) | 81,854 (95.2%) |
| Immigrants/ Descendants | 91 (4.3%) | 105 (4.9%) | 127,450 (9.0%) | 127,350 (9.0%) | 14 (5.8%) | 5 (2.1%) | 4194 (4.9%) | 4161 (4.8%) |
| Income # | ||||||||
| High tertile | 877 (41.0%) | 874 (40.9%) | 469,621 (33.3%) | 470,706 (33.4%) | 94 (39.0%) | 92 (38.2%) | 28,703 (33.4%) | 28,620 (33.3%) |
| Middle tertile | 798 (37.3%) | 774 (36.2%) | 470,625 (33.4%) | 469,875 (33.3%) | 92 (38.2%) | 91 (37.8%) | 28,775 (33.5%) | 28,546 (33.2%) |
| Low tertile/Unknown or missing | 462 (21.6%) | 489 (22.9%) | 470,721 (33.4%) | 470,390 (33.3%) | 55 (22.8%) | 58 (24.1%) | 28,538 (33.2%) | 28,848 (33.5%) |
| Occupational status | ||||||||
| Employed/Education | 364 (17.0%) | 384 (18.0%) | 754,453 (53.5%) | 752,975 (53.4%) | 32 (13.3%) | 30 (12.4%) | 23,172 (26.9%) | 23,256 (27.0%) |
| Unemployed or on welfare payment/Unknown or missing | 98 (4.6%) | 91 (4.3%) | 101,338 (7.2%) | 101,208 (7.2%) | 12 (5.0%) | 6 (2.5%) | 3407 (4.0%) | 3293 (3.8%) |
| Early retirement | 229 (10.7%) | 237 (11.1%) | 120,084 (8.5%) | 120,159 (8.5%) | 16 (6.6%) | 18 (7.5%) | 6722 (7.8%) | 6832 (7.9%) |
| Retirement pension | 1446 (67.7%) | 1425 (66.7%) | 435,113 (30.8%) | 436,645 (30.9%) | 181 (75.1%) | 187 (77.6%) | 52,715 (61.3%) | 52,634 (61.2%) |
| Education | ||||||||
| High education | 272 (12.7%) | 307 (14.4%) | 416,218 (29.5%) | 416,453 (29.5%) | 41 (17.0%) | 37 (15.4%) | 22,227 (25.8%) | 22,171 (25.8%) |
| Medium education | 887 (41.5%) | 850 (39.8%) | 591,310 (41.9%) | 591,770 (41.9%) | 83 (34.4%) | 99 (41.1%) | 35,436 (41.2%) | 35,669 (41.5%) |
| Low education/Unknown or missing | 978 (45.8%) | 980 (45.9%) | 403,460 (28.6%) | 402,764 (28.5%) | 117 (48.5%) | 105 (43.6%) | 28,353 (33.0%) | 28,175 (32.8%) |
| Dead in year 2017 | 701 (32.8%) | 738 (34.5%) | 18,881 (1.3%) | 19,047 (1.3%) | 54 (22.4%) | 56 (23.2%) | 6379 (7.4%) | 6323 (7.4%) |
| Incident lung cancer | ||||||||
| Age 40.0–59.9 | 302 (14.1%) | 300 (14.0%) | 19 (7.9%) | 13 (5.4%) | ||||
| Age 60.0–79.9 | 1507 (70.5%) | 1521 (71.2%) | 178 (73.9%) | 188 (78.0%) | ||||
| Age ≥ 80.0 | 328 (15.3%) | 316 (14.8%) | 44 (18.3%) | 40 (16.6%) | ||||
| Cohort without History of Cancer (Population 1) | Cohort with History of Cancer (Population 2) | |||
|---|---|---|---|---|
| Models | Development cohort | Validation cohort | Development cohort | Validation cohort |
| Model A * | 0.81 (0.81–0.82) | 0.80 (0.79–0.81) | 0.73 (0.70–0.764 | 0.65 (0.620–0.69) |
| Model B ¤ | 0.82 (0.81–0.83) | 0.81 (0.80–0.82) | 0.72 (0.68–0.75) | 0.65 (0.62–0.69) |
| Model C # | 0.75 (0.74–0.76) | 0.75 (0.74–0.76) | 0.58 (0.55–0.62) | 0.58 (0.55–0.61) |
| Model D ^ | 0.74 (0.73–0.75) | 0.73 (0.72–0.74) | 0.63 (0.60–0.67) | 0.61 (0.57–0.64) |
| Validation Cohort | Population 1 Model A | Population 2 Model A | |
|---|---|---|---|
| Individuals | 1,413,124 | 86,256 | |
| Total cancer cases | 2137 | 241 | |
| Risk cut-off | 1% | 5% | 1% |
| Number of subjects predicted above cutoff | 17,002 | 337 | 2324 |
| Cancer cases detected | 216 | 7 | 14 |
| Positive Predictive value | 1.3% | 2.1% | 0.6% |
| Sensitivity | 10.1% | 0.3% | 5.8% |
| Odds ratio (95% Confidence Interval) | 9.33 (8.08; 10.77) | 14.05 (5.60; 29.32) | 2.23 (1.20; 3.84) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rubin, K.H.; Haastrup, P.F.; Nicolaisen, A.; Möller, S.; Wehberg, S.; Rasmussen, S.; Balasubramaniam, K.; Søndergaard, J.; Jarbøl, D.E. Developing and Validating a Lung Cancer Risk Prediction Model: A Nationwide Population-Based Study. Cancers 2023, 15, 487. https://doi.org/10.3390/cancers15020487
Rubin KH, Haastrup PF, Nicolaisen A, Möller S, Wehberg S, Rasmussen S, Balasubramaniam K, Søndergaard J, Jarbøl DE. Developing and Validating a Lung Cancer Risk Prediction Model: A Nationwide Population-Based Study. Cancers. 2023; 15(2):487. https://doi.org/10.3390/cancers15020487
Chicago/Turabian StyleRubin, Katrine H., Peter F. Haastrup, Anne Nicolaisen, Sören Möller, Sonja Wehberg, Sanne Rasmussen, Kirubakaran Balasubramaniam, Jens Søndergaard, and Dorte E. Jarbøl. 2023. "Developing and Validating a Lung Cancer Risk Prediction Model: A Nationwide Population-Based Study" Cancers 15, no. 2: 487. https://doi.org/10.3390/cancers15020487
APA StyleRubin, K. H., Haastrup, P. F., Nicolaisen, A., Möller, S., Wehberg, S., Rasmussen, S., Balasubramaniam, K., Søndergaard, J., & Jarbøl, D. E. (2023). Developing and Validating a Lung Cancer Risk Prediction Model: A Nationwide Population-Based Study. Cancers, 15(2), 487. https://doi.org/10.3390/cancers15020487








