Planning Strategy to Optimize the Dose-Averaged LET Distribution in Large Pelvic Sarcomas/Chordomas Treated with Carbon-Ion Radiotherapy
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Characteristics
2.2. Treatment Simulation and Planning: Clinical
2.3. DRBE and LETd Evaluation
2.4. LETd Optimization: Distal Patching
2.5. Statistical Analysis
3. Results
3.1. DRBE|LEM-I, DRBE|mMKM Evaluation in Small vs. Large Pelvic Sarcomas/Chordomas
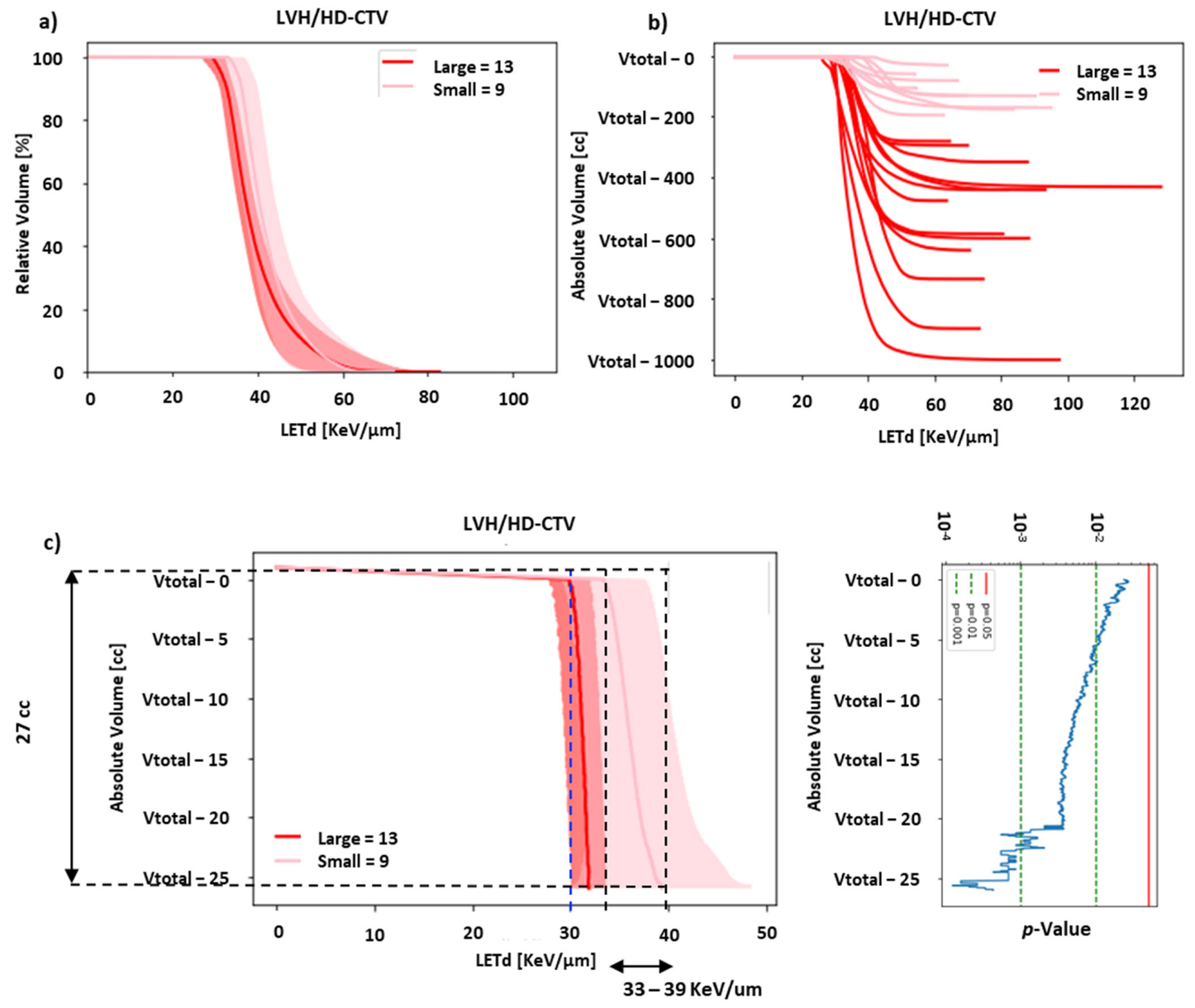
3.2. LETd Evaluation in Small and Large Pelvic Sarcomas/Chordomas
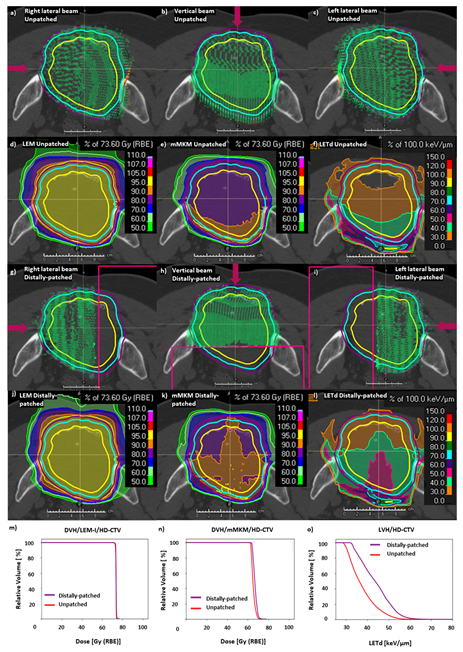
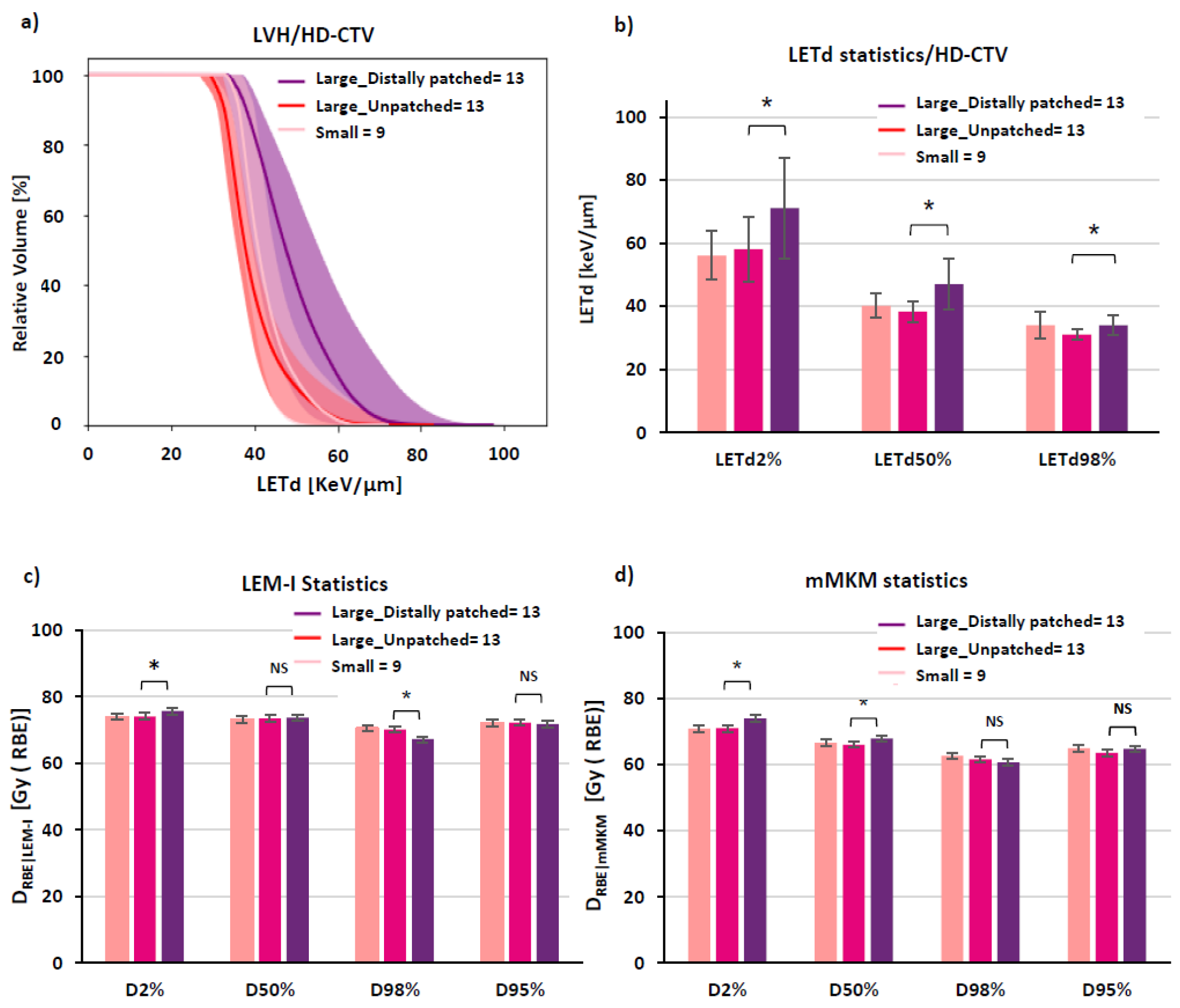
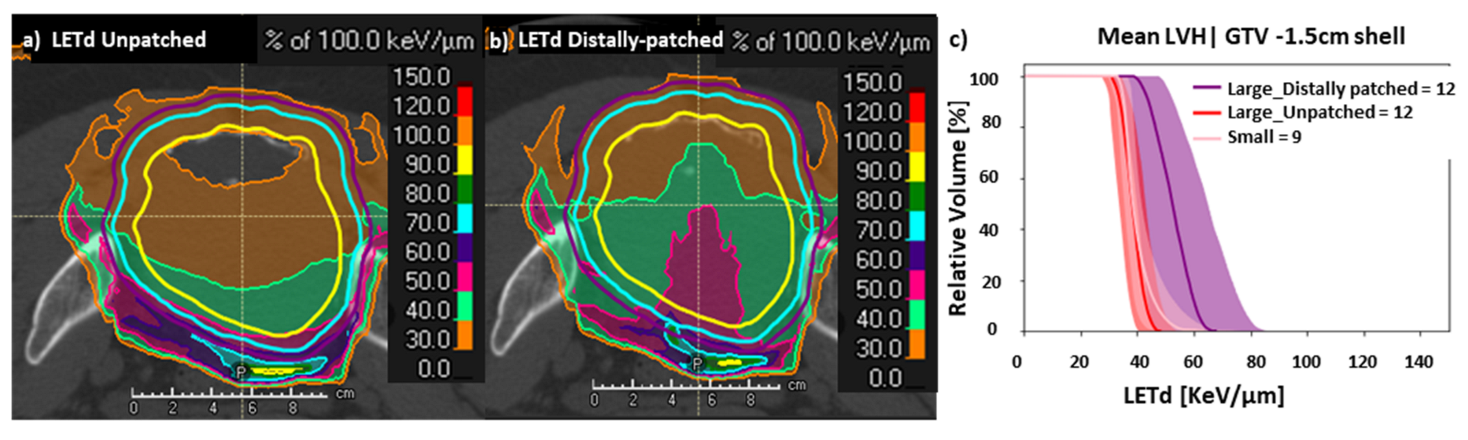
3.3. LETd Optimization in Large Pelvic Sarcomas/Chordomas with ‘Distal Patching’
3.4. Evaluation of DRBE|LEM-I, DRBE|mMKM and LETd Distributions for OARs in LETd Optimization by ‘Distal Patching’
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Matsunobu, A.; Imai, R.; Kamada, T.; Imaizumi, T.; Tsuji, H.; Tsujii, H.; Shioyama, Y.; Honda, H.; Tatezaki, S.; Working Group for Bone and Soft Tissue Sarcomas. Impact of carbon ion radiotherapy for unresectable osteosarcoma of the trunk. Cancer 2012, 118, 4555–4563. [Google Scholar] [CrossRef] [PubMed]
- Imai, R.; Kamada, T.; Araki, N. Clinical efficacy of carbon ion radiotherapy for unresectable chondrosarcomas. Anticancer Res. 2017, 37, 6959–6964. [Google Scholar] [PubMed]
- Demizu, Y.; Imai, R.; Kiyohara, H.; Matsunobu, A.; Okamoto, M.; Okimoto, T.; Tsuji, H.; Ohno, T.; Shioyama, Y.; Nemoto, K.; et al. Carbon ion radiotherapy for sacral chordoma: A retrospective nationwide multicentre study in Japan. Radiother. Oncol. 2021, 154, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Demizu, Y.; Jin, D.; Sulaiman, N.S.; Nagano, F.; Terashima, K.; Tokumaru, S.; Akagi, T.; Fujii, O.; Daimon, T.; Sasaki, R.; et al. Particle therapy using protons or carbon ions for unresectable or incompletely resected bone and soft tissue sarcomas of the pelvis. Int. J. Radiat. Oncol. Biol. Phys. 2017, 98, 367–374. [Google Scholar] [CrossRef]
- Mohamad, O.; Imai, R.; Kamada, T.; Nitta, Y.; Araki, N. Carbon ion radiotherapy for inoperable pediatric osteosarcoma. Oncotarget 2018, 9, 22976. [Google Scholar] [CrossRef]
- Shiba, S.; Okamoto, M.; Kiyohara, H.; Okazaki, S.; Kaminuma, T.; Shibuya, K.; Kohama, I.; Saito, K.; Yanagawa, T.; Chikuda, H.; et al. Impact of carbon ion radiotherapy on inoperable bone sarcoma. Cancers 2021, 13, 1099. [Google Scholar] [CrossRef]
- Bostel, T.; Mattke, M.; Nicolay, N.H.; Welzel, T.; Wollschläger, D.; Akbaba, S.; Mayer, A.; Sprave, T.; Debus, J.; Uhl, M. High-dose carbon-ion based radiotherapy of primary and recurrent sacrococcygeal chordomas: Long-term clinical results of a single particle therapy center. Radiat. Oncol. 2020, 15, 206. [Google Scholar] [CrossRef]
- Nishida, Y.; Kamada, T.; Imai, R.; Tsukushi, S.; Yamada, Y.; Sugiura, H.; Shido, Y.; Wasa, J.; Ishiguro, N. Clinical outcome of sacral chordoma with carbon ion radiotherapy compared with surgery. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 110–116. [Google Scholar] [CrossRef]
- Mizoe, J.E.; Hasegawa, A.; Jingu, K.; Takagi, R.; Bessyo, H.; Morikawa, T.; Tonoki, M.; Tsuji, H.; Kamada, T.; Tsujii, H.; et al. Results of carbon ion radiotherapy for head and neck cancer. Radiother. Oncol. 2012, 103, 32–37. [Google Scholar] [CrossRef]
- Akbaba, S.; Ahmed, D.; Mock, A.; Held, T.; Bahadir, S.; Lang, K.; Syed, M.; Hoerner-Rieber, J.; Forster, T.; Federspil, P.; et al. Treatment outcome of 227 patients with sinonasal adenoid cystic carcinoma (ACC) after intensity modulated radiotherapy and active raster-scanning carbon ion boost: A 10-year single-center experience. Cancers 2019, 11, 1705. [Google Scholar] [CrossRef]
- Uhl, M.; Mattke, M.; Welzel, T.; Roeder, F.; Oelmann, J.; Habl, G.; Jensen, A.; Ellerbrock, M.; Jäkel, O.; Haberer, T.; et al. Highly effective treatment of skull base chordoma with carbon ion irradiation using a raster scan technique in 155 patients: First long-term results. Cancer 2014, 120, 3410–3417. [Google Scholar] [CrossRef] [PubMed]
- Saitoh, J.I.; Shirai, K.; Mizukami, T.; Abe, T.; Ebara, T.; Ohno, T.; Minato, K.; Saito, R.; Yamada, M.; Nakano, T. Hypofractionated carbon-ion radiotherapy for stage I peripheral nonsmall cell lung cancer (GUNMA0701): Prospective phase II study. Cancer Med. 2019, 8, 6644–6650. [Google Scholar] [CrossRef] [PubMed]
- Yamada, S.; Takiyama, H.; Isozaki, Y.; Shinoto, M.; Makishima, H.; Yamamoto, N.; Tsuji, H. Carbon-ion Radiotherapy for Colorectal Cancer. J. Anus Rectum Colon 2021, 5, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Shinoto, M.; Yamada, S.; Terashima, K.; Yasuda, S.; Shioyama, Y.; Honda, H.; Kamada, T.; Tsujii, H.; Saisho, H.; Asano, T.; et al. Carbon ion radiation therapy with concurrent gemcitabine for patients with locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 2016, 95, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Tsuji, H.; Kamada, T.; Akakura, K.; Suzuki, H.; Shimazaki, J.; Tsujii, H.; Working Group for Genitourinary Tumors. Carbon-ion radiation therapy for prostate cancer. Int. J. Urol. 2012, 19, 296–305. [Google Scholar] [CrossRef]
- Shibuya, K.; Ohno, T.; Terashima, K.; Toyama, S.; Yasuda, S.; Tsuji, H.; Okimoto, T.; Shioyama, Y.; Nemoto, K.; Kamada, T.; et al. Short-course carbon-ion radiotherapy for hepatocellular carcinoma: A multi-institutional retrospective study. Liver Int. 2018, 38, 2239–2247. [Google Scholar] [CrossRef]
- Kubo, N.; Saitoh, J.I.; Shimada, H.; Shirai, K.; Kawamura, H.; Ohno, T.; Nakano, T. Dosimetric comparison of carbon ion and X-ray radiotherapy for Stage IIIA non-small cell lung cancer. J. Radiat. Res. 2016, 57, 548–554. [Google Scholar] [CrossRef]
- Dong, M.; Liu, R.; Zhang, Q.; Luo, H.; Wang, D.; Wang, Y.; Chen, J.; Ou, Y.; Wang, X. Efficacy and safety of carbon ion radiotherapy for bone sarcomas: A systematic review and meta-analysis. Radiat. Oncol. 2022, 17, 172. [Google Scholar] [CrossRef]
- Tinganelli, W.; Durante, M. Carbon Ion Radiobiology. Cancers 2020, 12, 3022. [Google Scholar] [CrossRef]
- Ozaki, T.; Flege, S.; Kevric, M.; Lindner, N.; Maas, R.; Delling, G.; Schwarz, R.; Von Hochstetter, A.R.; Salzer-Kuntschik, M.; Berdel, W.E.; et al. Osteosarcoma of the Pelvis: Experience of the Cooperative Osteosarcoma Study Group. J. Clin. Oncol. 2003, 21, 334–341. [Google Scholar] [CrossRef]
- Pennicooke, B.; Laufer, I.; Sahgal, A.; Varga, P.P.; Gokaslan, Z.L.; Bilsky, M.H.; Yamada, Y.J. Safety and local control of radiation therapy for chordoma of the spine and sacrum: A systematic review. Spine 2016, 41, S186. [Google Scholar] [CrossRef] [PubMed]
- Ozaki, T.; Flege, S.; Liljenqvist, U.; Hillmann, A.; Delling, G.; Salzer-Kuntschik, M.; Jürgens, H.; Kotz, R.; Winkelmann, W.; Bielack, S.S. Osteosarcoma of the spine: Experience of the Cooperative Osteosarcoma Study Group. Cancer 2002, 94, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Tinkle, C.L.; Lu, J.; Han, Y.; Li, Y.; McCarville, B.M.; Neel, M.D.; Bishop, M.W.; Krasin, M.J. Curative-intent radiotherapy for pediatric osteosarcoma: The St. Jude experience. Pediatr. Blood Cancer 2019, 66, e27763. [Google Scholar] [CrossRef] [PubMed]
- Kanai, T.; Furusawa, Y.; Fukutsu, K.; Itsukaichi, H.; Eguchi-Kasai, K.; Ohara, H. Irradiation of mixed beam and design of spread-out Bragg peak for heavy-ion radiotherapy. Radiat. Res. 1997, 147, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Kanai, T.; Endo, M.; Minohara, S.; Miyahara, N.; Koyama-Ito, H.; Tomura, H.; Matsufuji, N.; Futami, Y.; Fukumura, A.; Hiraoka, T.; et al. Biophysical characteristics of HIMAC clinical irradiation system for heavy-ion radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 1999, 44, 201–210. [Google Scholar] [CrossRef]
- Kase, Y.; Kanai, T.; Matsumoto, Y.; Furusawa, Y.; Okamoto, H.; Asaba, T.; Sakama, M.; Shinoda, H. Microdosimetric measurements and estimation of human cell survival for heavy-ion beams. Radiat. Res. 2006, 166, 629–638. [Google Scholar] [CrossRef]
- Inaniwa, T.; Kanematsu, N.; Matsufuji, N.; Kanai, T.; Shirai, T.; Noda, K.; Tsuji, H.; Kamada, T.; Tsujii, H. Reformulation of a clinical-dose system for carbon-ion radiotherapy treatment planning at the National Institute of Radiological Sciences, Japan. Phys. Med. Biol. 2015, 60, 3271–3286. [Google Scholar] [CrossRef]
- Inaniwa, T.; Furukawa, T.; Kase, Y.; Matsufuji, N.; Toshito, T.; Matsumoto, Y.; Furusawa, Y.; Noda, K. Treatment planning for a scanned carbon beam with a modified microdosimetric kinetic model. Phys. Med. Biol. 2010, 55, 6721–6737. [Google Scholar] [CrossRef]
- Scholz, M.; Kellerer, A.M.; Kraft-Weyrather, W.; Kraft, G. Computation of cell survival in heavy ion beams for therapy. Radiat. Environ. Biophys. 1997, 36, 59–66. [Google Scholar] [CrossRef]
- Matsumoto, S.; Lee, S.H.; Imai, R.; Inaniwa, T.; Matsufuji, N.; Fukahori, M.; Kohno, R.; Yonai, S.; Okonogi, N.; Yamada, S.; et al. Unresectable chondrosarcomas treated with carbon ion radiotherapy: Relationship between dose-averaged linear energy transfer and local recurrence. Anticancer Res. 2020, 40, 6429–6435. [Google Scholar] [CrossRef]
- Hagiwara, Y.; Bhattacharyya, T.; Matsufuji, N.; Isozaki, Y.; Takiyama, H.; Nemoto, K.; Tsuji, H.; Yamada, S. Influence of dose-averaged linear energy transfer on tumour control after carbon-ion radiation therapy for pancreatic cancer. Clin. Transl. Radiat. Oncol. 2020, 21, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Molinelli, S.; Magro, G.; Mairani, A.; Allajbej, A.; Mirandola, A.; Chalaszczyk, A.; Imparato, S.; Ciocca, M.; Fiore, M.R.; Orlandi, E. How LEM-based RBE and dose-averaged LET affected clinical outcomes of sacral chordoma patients treated with carbon ion radiotherapy. Radiother. Oncol. 2021, 163, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Inaniwa, T.; Kanematsu, N.; Noda, K.; Kamada, T. Treatment planning of intensity modulated composite particle therapy with dose and linear energy transfer optimization. Phys. Med. Biol. 2017, 62, 5180. [Google Scholar] [CrossRef] [PubMed]
- Kohno, R.; Koto, M.; Ikawa, H.; Lee, S.H.; Sato, K.; Hashimoto, M.; Inaniwa, T.; Shirai, T. High–Linear Energy Transfer Irradiation in Clinical Carbon-Ion Beam with the Linear Energy Transfer Painting Technique for Patients with Head and Neck Cancer. Adv. Radiat. Oncol. 2023, 101317. [Google Scholar] [CrossRef]
- Radaelli, S.; Fossati, P.; Stacchiotti, S.; Akiyama, T.; Asencio, J.M.; Bandiera, S.; Boglione, A.; Boland, P.; Bolle, S.; Bruland, Ø.; et al. The sacral chordoma margin. Eur. J. Surg. Oncol. 2020, 46, 1415–1422. [Google Scholar] [CrossRef]
- Salerno, K.E.; Alektiar, K.M.; Baldini, E.H.; Bedi, M.; Bishop, A.J.; Bradfield, L.; Chung, P.; DeLaney, T.F.; Folpe, A.; Kane, J.M.; et al. Radiation therapy for treatment of soft tissue sarcoma in adults: Executive summary of an ASTRO clinical practice guideline. Pract. Radiat. Oncol. 2021, 11, 339–351. [Google Scholar] [CrossRef]
- Stock, M.; Georg, D.; Ableitinger, A.; Zechner, A.; Utz, A.; Mumot, M.; Kragl, G.; Hopfgartner, J.; Gora, J.; Bohlen, T.; et al. The technological basis for adaptive ion beam therapy at MedAustron: Status and outlook. Med. Phys. 2018, 28, 196–210. [Google Scholar] [CrossRef]
- Carlino, A.; Boehlen, T.; Vatnitsky, S.; Grevillot, L.; Osorio, J.; Dreindl, R.; Palmans, H.; Stock, M.; Kragl, G. Commissioning of pencil beam and Monte Carlo dose engines for non-isocentric treatments in scanned proton beam therapy. Phys. Med. Biol. 2019, 28, 17NT01. [Google Scholar] [CrossRef]
- Fossati, P.; Molinelli, S.; Matsufuji, N.; Ciocca, M.; Mirandola, A.; Mairani, A.; Mizoe, J.; Hasegawa, A.; Imai, R.; Kamada, T.; et al. Dose prescription in carbon ion radiotherapy: A planning study to compare NIRS and LEM approaches with a clinically-oriented strategy. Phys. Med. Biol. 2012, 57, 7543. [Google Scholar] [CrossRef]
- Lomax, N.J.; Scheib, S.G. Quantifying the degree of conformity in radiosurgery treatment planning. Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 1409–1419. [Google Scholar] [CrossRef]
- Semenenko, V.A.; Reitz, B.; Day, E.; Qi, X.S.; Miften, M.; Li, X.A. Evaluation of a commercial biologically based IMRT treatment planning system. Med. Phys. 2008, 35, 5851–5860. [Google Scholar] [CrossRef] [PubMed]
- Hahn, C.; Heuchel, L.; Ödén, J.; Traneus, E.; Wulff, J.; Plaude, S.; Timmermann, B.; Bäumer, C.; Lühr, A. Comparing biological effectiveness guided plan optimization strategies for cranial proton therapy: Potential and challenges. Radiat. Oncol. 2022, 17, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Schafasand, M.; Resch, A.F.; Nachankar, A.; Gora, J.; Traneus, E.; Glimelius, L.; Georg, D.; Stock, M.; Carlino, A.; Fossati, P. Investigation on the high linear energy transfer dose distribution in small and large tumors in carbon ion therapy. Med. Phys. 2023. [Google Scholar] [CrossRef] [PubMed]
- Schafasand, M.; Resch, A.F.; Traneus, E.; Glimelius, L.; Fossati, P.; Stock, M.; Gora, J.; Georg, D.; Carlino, A. Technical note: In silico benchmarking of the linear energy transfer-based functionalities for carbon ion beams in a commercial treatment planning system. Med. Phys. 2023, 50, 1871–1878. [Google Scholar] [CrossRef] [PubMed]
- Mein, S.; Klein, C.; Kopp, B.; Magro, G.; Harrabi, S.; Karger, C.P.; Haberer, T.; Debus, J.; Abdollahi, A.; Dokic, I.; et al. Assessment of RBE-weighted dose models for carbon ion therapy toward modernization of clinical practice at HIT. In vitro, in vivo and in patients. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, 779–791. [Google Scholar] [CrossRef]
- Bassler, N.; Jäkel, O.; Søndergaard, C.S.; Petersen, J.B. Dose-and LET-painting with particle therapy. Acta Oncol. 2010, 49, 1170–1176. [Google Scholar] [CrossRef]
- Morelli, L.; Parrella, G.; Molinelli, S.; Magro, G.; Annunziata, S.; Mairani, A.; Chalaszczyk, A.; Fiore, M.R.; Ciocca, M.; Paganelli, C.; et al. A Dosiomics Analysis Based on Linear Energy Transfer and Biological Dose Maps to Predict Local Recurrence in Sacral Chordomas after Carbon-Ion Radiotherapy. Cancers 2023, 15, 33. [Google Scholar] [CrossRef]
- Furusawa, Y.; Fukutsu, K.; Aoki, M.; Itsukaichi, H.; Eguchi-Kasai, K.; Ohara, H.; Yatagai, F.; Kanai TAndo, K. Inactivation of aerobic and hypoxic cells from three different cell lines by accelerated (3)He-, (12)C-and (20)Ne-ion beams. Radiat. Res. 2000, 154, 485–496. [Google Scholar] [CrossRef]
- Tinganelli, W.; Durante, M.; Hirayama, R.; Krämer, M.; Maier, A.; Kraft-Weyrather, W.; Furusawa, Y.; Friedrich, T.; Scifoni, E. Kill-painting of hypoxic tumours in charged particle therapy. Sci. Rep. 2015, 5, 17016. [Google Scholar] [CrossRef]
- Bassler, N.; Toftegaard, J.; Lühr, A.; Sørensen, B.S.; Scifoni, E.; Krämer, M.; Jäkel, O.; Mortensen, L.S.; Overgaard, J.; Petersen, J.B. LET-painting increases tumour control probability in hypoxic tumours. Acta Oncol. 2014, 53, 25–32. [Google Scholar] [CrossRef]
- Ebner, D.K.; Frank, S.J.; Inaniwa, T.; Yamada, S.; Shirai, T. The emerging potential of multi-ion radiotherapy. Front. Oncol. 2021, 11, 624786. [Google Scholar] [CrossRef] [PubMed]
- Mairani, A.; Mein, S.; Blakely, E.; Debus, J.; Durante, M.; Ferrari, A.; Fuchs, H.; Georg, D.; Grosshans, D.R.; Guan, F.; et al. Roadmap: Helium ion therapy. Phys. Med. Biol. 2022, 67, 15TR02. [Google Scholar] [CrossRef] [PubMed]
- Kopp, B.; Mein, S.; Dokic, I.; Harrabi, S.; Böhlen, T.T.; Haberer, T.; Debus, J.; Abdollahi, A.; Mairani, A. Development and Validation of Single Field Multi-Ion Particle Therapy Treatments. Int. Radiat. Oncol. Biol. Phys. 2020, 106, 194–205. [Google Scholar] [CrossRef] [PubMed]
- Durante, M.; Brenner, D.J.; Formenti, S.C. Does heavy ion therapy work through the immune system? Int. Radiat. Oncol. Biol. Phys. 2016, 96, 934–936. [Google Scholar] [CrossRef]
- Kobayashi, D.; Oike, T.; Shibata, A.; Niimi, A.; Kubota, Y.; Sakai, M.; Amornwhichet, N.; Yoshimoto, Y.; Hagiwara, Y.; Kimura, Y.; et al. Mitotic catastrophe is a putative mechanism underlying the weak correlation between sensitivity to carbon ions and cisplatin. Sci. Rep. 2017, 7, 40588. [Google Scholar] [CrossRef] [PubMed]
- Nachankar, A.; Oike, T.; Hanaoka, H.; Kanai, A.; Sato, H.; Yoshida, Y.; Obinata, H.; Sakai, M.; Osu, N.; Hirota, Y.; et al. 64Cu-ATSM predicts efficacy of carbon ion radiotherapy associated with cellular antioxidant capacity. Cancers 2021, 13, 6159. [Google Scholar] [CrossRef]
- Tubin, S.; Yan, W.; Mourad, W.F.; Fossati, P.; Khan, M.K. The future of radiation-induced abscopal response: Beyond conventional radiotherapy approaches. Future Oncol. 2020, 16, 1137–1151. [Google Scholar] [CrossRef]

| Patient Characteristics | Small | Large | p-Value | |
|---|---|---|---|---|
| (n = 9) | (n = 13) | Small vs. Large | ||
| Age | Median [years] | 64 | 63 | NS * |
| Range [years] | 42–76 | 43–77 | ||
| Gender | Male | 7 | 12 | NS |
| Female | 2 | 1 | NS | |
| Follow-up | Median [months] | 15 | 14 | NS |
| Range [months] | 4–23 | 4–28 | ||
| Histology | Chordoma | 8 | 13 | NS |
| Sarcoma (Synovial) | 1 | 0 | NS | |
| Surgery | 1 | 1 | NS | |
| Chemotherapy | 0 | 1 | NS | |
| Tumor Characteristics | ||||
| GTV | Mean ± SD [cm3] | 55.9 ± 39.8 | 301 ± 243.5 | 0.004 |
| HD-CTV | Mean ± SD [cm3] | 116.3 ± 52.6 | 551.7 ± 211.3 | <0.001 |
| HD-PTV | Mean ± SD [cm3] | 195.1 ± 76.8 | 776.7 ± 257.7 | <0.001 |
| Maximum GTV diameter along the beam path | [cm] | 5.4 ± 2.1 | 9.1 ± 3.8 | 0.01 |
| CIRT dose [LEM-I] | Median [Gy (RBE)] | 73.6 | 73.6 | NS |
| Range [Gy (RBE)] | 70.4–73.6 | 70.4–73.6 | ||
| DRBE Statistics | ||||
| GTV | LEM-I | |||
| D2% Mean ± SD [Gy (RBE)] | 73.7 ± 1.6 | 74.5 ± 0.6 | NS | |
| D50% Mean ± SD [Gy (RBE)] | 73.1 ± 1.3 | 73.8 ± 0.2 | NS | |
| D98% Mean ± SD [Gy (RBE)] | 71.5 ± 1.1 | 72.0 ± 1.9 | NS | |
| mMKM | ||||
| D2% Mean ± SD [Gy (RBE)] | 69.0 ± 2.9 | 71.6 ± 3.8 | NS | |
| D50% Mean ± SD [Gy (RBE)] | 65.4 ± 2.1 | 66.6 ± 2.5 | NS | |
| D98% Mean ± SD [Gy (RBE)] | 63.1 ± 2.5 | 63.7 ± 1.3 | NS | |
| HD-CTV | LEM-I | |||
| D2% Mean ± SD [Gy (RBE)] | 74.1 ± 1.4 | 74.1 ± 1.0 | NS | |
| D50% Mean ± SD [Gy (RBE)] | 73.3 ± 1.0 | 73.5 ± 0.9 | NS | |
| D98% Mean ± SD [Gy (RBE)] | 70.5 ± 2.8 | 70.1 ± 2.8 | NS | |
| mMKM | ||||
| D2% Mean ± SD [Gy (RBE)] | 70.9 ± 1.8 | 71.0 ± 3.6 | NS | |
| D50% Mean ± SD [Gy (RBE)] | 66.6 ± 1.4 | 66.1 ± 2.7 | NS | |
| D98% Mean ± SD [Gy (RBE)] | 62.7 ± 3.8 | 61.6 ± 2.2 | NS | |
| HD-PTV | LEM-I | |||
| D2% Mean ± SD [Gy (RBE)] | 74.1 ± 1.3 | 74.1 ± 0.9 | NS | |
| D50% Mean ± SD [Gy (RBE)] | 73.2 ± 1.0 | 73.4 ± 0.9 | NS | |
| D98% Mean ± SD [Gy (RBE)] | 65.0 ± 10.2 | 66.5 ± 5.6 | NS | |
| mMKM | ||||
| D2% Mean ± SD [Gy (RBE)] | 72.6 ± 1.7 | 72.4 ± 3.2 | NS | |
| D50% Mean ± SD [Gy (RBE)] | 67.01 ± 1.6 | 66.3 ± 2.6 | NS | |
| D98% Mean ± SD [Gy (RBE)] | 56.9 ± 12.4 | 56.3 ± 7.0 | NS | |
| LETd Statistics | ||||
| GTV | LETd2% Mean ± SD [KeV/µm] | 51.1 ± 9.6 | 55.5 ± 9.8 | NS |
| LETd50% Mean ± SD [KeV/µm] | 37.6 ± 4.0 | 37.2 ± 2.2 | NS | |
| LETd98% Mean ± SD [KeV/µm] | 33.6 ± 3.9 | 31.2 ± 2.0 | NS | |
| HD-CTV | LETd2% Mean ± SD [KeV/µm] | 56.1 ± 7.7 | 58.1 ± 10.1 | NS |
| LETd50% Mean ± SD [KeV/µm] | 40.2 ± 3.8 | 38.3 ± 3.2 | NS | |
| LETd98% Mean ± SD [KeV/µm] | 34.0 ± 4.4 | 31.1 ± 1.7 | NS | |
| HD-PTV | LETd2% Mean ± SD [KeV/µm] | 67.4 ± 18.0 | 69.6 ± 12.5 | NS |
| LETd50% Mean ± SD [KeV/µm] | 45.0 ± 4.9 | 39.9 ± 3.2 | 0.02 | |
| LETd98% Mean ± SD [KeV/µm] | 40.3 ± 10.5 | 31.1 ± 2.0 | 0.04 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nachankar, A.; Schafasand, M.; Carlino, A.; Hug, E.; Stock, M.; Góra, J.; Fossati, P. Planning Strategy to Optimize the Dose-Averaged LET Distribution in Large Pelvic Sarcomas/Chordomas Treated with Carbon-Ion Radiotherapy. Cancers 2023, 15, 4903. https://doi.org/10.3390/cancers15194903
Nachankar A, Schafasand M, Carlino A, Hug E, Stock M, Góra J, Fossati P. Planning Strategy to Optimize the Dose-Averaged LET Distribution in Large Pelvic Sarcomas/Chordomas Treated with Carbon-Ion Radiotherapy. Cancers. 2023; 15(19):4903. https://doi.org/10.3390/cancers15194903
Chicago/Turabian StyleNachankar, Ankita, Mansure Schafasand, Antonio Carlino, Eugen Hug, Markus Stock, Joanna Góra, and Piero Fossati. 2023. "Planning Strategy to Optimize the Dose-Averaged LET Distribution in Large Pelvic Sarcomas/Chordomas Treated with Carbon-Ion Radiotherapy" Cancers 15, no. 19: 4903. https://doi.org/10.3390/cancers15194903
APA StyleNachankar, A., Schafasand, M., Carlino, A., Hug, E., Stock, M., Góra, J., & Fossati, P. (2023). Planning Strategy to Optimize the Dose-Averaged LET Distribution in Large Pelvic Sarcomas/Chordomas Treated with Carbon-Ion Radiotherapy. Cancers, 15(19), 4903. https://doi.org/10.3390/cancers15194903






