Risk Factors and Prognosis of Stroke in Gynecologic Cancer Patients
Abstract
:Simple Summary
Abstract
1. Introduction
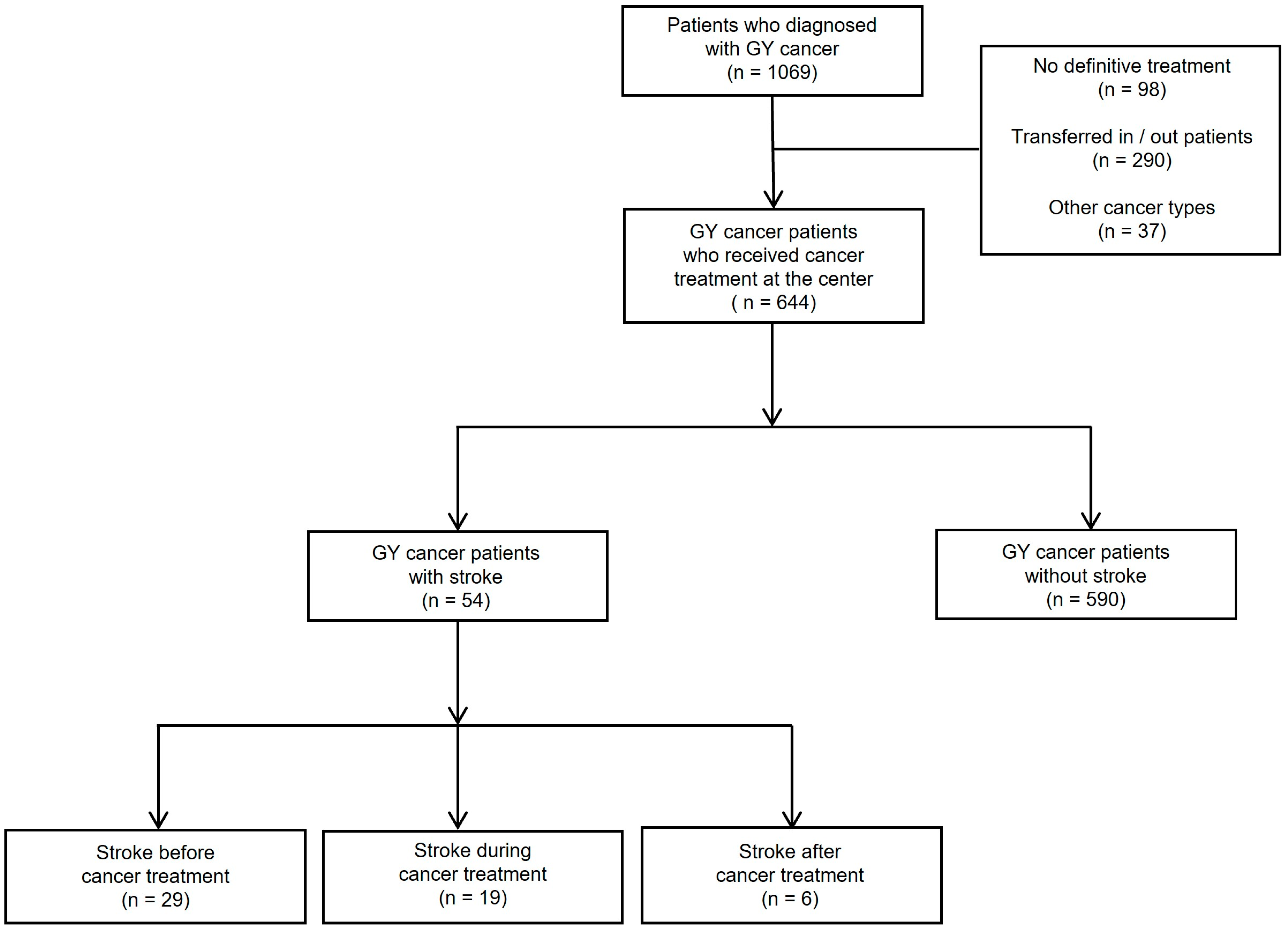
2. Materials and Methods
3. Results
3.1. Baseline Characteristics
3.2. Risk Factors of Stroke in Patients with Cancers
3.3. Prognosis of Patients with Cancer and Stroke
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Statistics Korea. Korean Statistical Information Service; Statistics Korea: Daejeon, Republic of Korea, 2022. Available online: http://kosis.kr (accessed on 30 April 2023).
- Noh, H.; Seo, J.; Lee, S.; Yi, N.; Park, S.; Choi, Y.; Huh, S. Cause-of-Death Statistics in 2020 in the Republic of Korea. J. Korean Med. Assoc. 2023, 66, 132–142. [Google Scholar]
- National Cancer Center. National Cancer Information Center; National Cancer Center: Goyang, Republic of Korea, 2022. Available online: http://www.cancer.go.kr (accessed on 30 April 2023).
- Hong, K.S.; Bang, O.Y.; Kang, D.W.; Yu, K.H.; Bae, H.J.; Lee, J.S.; Heo, J.H.; Kwon, S.U.; Oh, C.W.; Lee, B.C.; et al. Stroke Statistics in Korea: Part I. Epidemiology and Risk Factors: A Report from the Korean Stroke Society and Clinical Research Center for Stroke. J. Stroke 2013, 15, 2–20. [Google Scholar] [CrossRef] [PubMed]
- Dearborn, J.L.; Urrutia, V.C.; Zeiler, S.R. Stroke and Cancer—A Complicated Relationship. J. Neurol. Transl. Neurosci. 2014, 2, 1039. [Google Scholar] [PubMed]
- Salazar-Camelo, R.A.; Moreno-Vargas, E.A.; Cardona, A.F.; Bayona-Ortiz, H.F. Ischemic Stroke: A Paradoxical Manifestation of Cancer. Crit. Rev. Oncol. Hematol. 2021, 157, 103181. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.W.; Won, Y.J.; Hong, S.; Kong, H.J.; Lee, E.S. Prediction of Cancer Incidence and Mortality in Korea, 2020. Cancer Res. Treat. 2020, 52, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Suh, D.H.; Ha, H.I.; Lee, Y.J.; Lim, J.; Won, Y.J.; Lim, M.C. Incidence and Treatment Outcomes of Uterine Cervical Cancer in Korea 1999–2018 from the National Cancer Registry. J. Gynecol. Oncol. 2023, 34, e39. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.W.; Won, Y.J.; Hong, S.; Kong, H.J.; Im, J.S.; Seo, H.G. Prediction of Cancer Incidence and Mortality in Korea, 2021. Cancer Res. Treat. 2021, 53, 316–322. [Google Scholar] [CrossRef]
- Jung, K.W.; Won, Y.J.; Kang, M.J.; Kong, H.J.; Im, J.S.; Seo, H.G. Prediction of Cancer Incidence and Mortality in Korea, 2022. Cancer Res. Treat. 2022, 54, 345–351. [Google Scholar] [CrossRef]
- Seol, H.J.; Ki, K.D.; Lee, J.M. Epidemiologic Characteristics of Cervical Cancer in Korean Women. J. Gynecol. Oncol. 2014, 25, 70–74. [Google Scholar] [CrossRef]
- Shin, H.Y.; Lee, Y.Y.; Song, S.Y.; Park, B.; Suh, M.; Choi, K.S.; Jun, J.K. Trends in Cervical Cancer Screening Rates Among Korean Women: Results of the Korean National Cancer Screening Survey, 2005–2020. J. Gynecol. Oncol. 2022, 33, e39. [Google Scholar] [CrossRef]
- Lim, M.C.; Won, Y.J.; Ko, M.J.; Kim, M.; Shim, S.H.; Suh, D.H.; Kim, J.W. Incidence of Cervical, Endometrial, and Ovarian Cancer in Korea During 1999–2015. J. Gynecol. Oncol. 2019, 30, e38. [Google Scholar] [CrossRef]
- Kim, S.I.; Kim, J.H.; Lee, C.; Ha, J.; Jung, K.W.; Lim, M.C. Incidence and Survival Rates of Primary Uterine Carcinosarcoma in Korea: A National Cancer Registry Study. J. Gynecol. Oncol. 2023, 34, e9. [Google Scholar] [CrossRef] [PubMed]
- Bang, O.Y.; Chung, J.W.; Lee, M.J.; Seo, W.K.; Kim, G.M.; Ahn, M.J.; OASIS-Cancer Study Investigators. Cancer-Related Stroke: An Emerging Subtype of Ischemic Stroke with Unique Pathomechanisms. J. Stroke 2020, 22, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Navi, B.B.; Iadecola, C. Ischemic Stroke in Cancer Patients: A Review of an Underappreciated Pathology. Ann. Neurol. 2018, 83, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Lun, R.; Siegal, D.; Ramsay, T.; Dowlatshahi, D. Cancer and Stroke: What Do We Know and Where Do We Go? Thromb. Res. 2022, 219, 133–140. [Google Scholar] [CrossRef]
- Cestari, D.M.; Weine, D.M.; Panageas, K.S.; Segal, A.Z.; DeAngelis, L.M. Stroke in Patients with Cancer: Incidence and Etiology. Neurology 2004, 62, 2025–2030. [Google Scholar] [CrossRef]
- Zaorsky, N.G.; Zhang, Y.; Tchelebi, L.T.; Mackley, H.B.; Chinchilli, V.M.; Zacharia, B.E. Stroke Among Cancer Patients. Nat. Commun. 2019, 10, 5172. [Google Scholar] [CrossRef]
- Shim, S.H.; Lim, M.C.; Lee, D.; Won, Y.J.; Ha, H.I.; Chang, H.K.; Cho, H. Cause-Specific Mortality Rate of Ovarian Cancer in the Presence of Competing Risks of Death: A Nationwide Population-Based Cohort Study. J. Gynecol. Oncol. 2022, 33, e5. [Google Scholar] [CrossRef]
- Selvik, H.A.; Thomassen, L.; Logallo, N.; Næss, H. Prior Cancer in Patients with Ischemic Stroke: The Bergen NORSTROKE Study. J. Stroke Cerebrovasc. Dis. 2014, 23, 919–925. [Google Scholar] [CrossRef]
- Grazioli, S.; Paciaroni, M.; Agnelli, G.; Acciarresi, M.; Alberti, A.; D’Amore, C.; Caso, V.; Venti, M.; Guasti, L.; Ageno, W.; et al. Cancer-Associated Ischemic Stroke: A Retrospective Multicentre Cohort Study. Thromb. Res. 2018, 165, 33–37. [Google Scholar] [CrossRef]
- Navi, B.B.; Kasner, S.E.; Elkind, M.S.V.; Cushman, M.; Bang, O.Y.; DeAngelis, L.M. Cancer and Embolic Stroke of Undetermined Source. Stroke 2021, 52, 1121–1130. [Google Scholar] [CrossRef] [PubMed]
- Zuber, M. Stroke and Cancer. Rev. Neurol. 2023, 179, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Dardiotis, E.; Aloizou, A.M.; Markoula, S.; Siokas, V.; Tsarouhas, K.; Tzanakakis, G.; Libra, M.; Kyritsis, A.P.; Brotis, A.G.; Aschner, M.; et al. Cancer-Associated Stroke: Pathophysiology, Detection and Management (Review). Int. J. Oncol. 2019, 54, 779–796. [Google Scholar] [CrossRef] [PubMed]
- Grisold, W.; Oberndorfer, S.; Struhal, W. Stroke and Cancer: A Review. Acta Neurol. Scand. 2009, 119, 1–16. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kang, K.; Kang, J.; Koo, J.; Kim, D.H.; Kim, B.J.; Kim, W.J.; Kim, E.G.; Kim, J.G.; Kim, J.M.; et al. Executive Summary of Stroke Statistics in Korea 2018: A Report from the Epidemiology Research Council of the Korean Stroke Society. J. Stroke 2019, 21, 42–59. [Google Scholar] [CrossRef]
- Martinez-Majander, N.; Tatlisumak, T. Cancer-Associated Ischemic Stroke. Acta Neurol. Scand. 2020, 141, 202–203. [Google Scholar] [CrossRef]
- Stefan, O.; Vera, N.; Otto, B.; Heinz, L.; Wolfgang, G. Stroke in Cancer Patients: A Risk Factor Analysis. J. Neuro-Oncol. 2009, 94, 221–226, Erratum in J. Neuro-Oncol. 2009, 94, 227. [Google Scholar] [CrossRef]
- Yousufuddin, M.; Young, N. Aging and Ischemic Stroke. Aging 2019, 11, 2542–2544. [Google Scholar] [CrossRef]
- Messerli, F.H.; Bangalore, S. Blood Pressure and Stroke: Findings from Recent Trials. J. Am. Coll. Cardiol. 2011, 57, 114–115. [Google Scholar] [CrossRef]
- Weiss, J.; Freeman, M.; Low, A.; Fu, R.; Kerfoot, A.; Paynter, R.; Motu’apuaka, M.; Kondo, K.; Kansagara, D. Benefits and Harms of Intensive Blood Pressure Treatment in Adults Aged 60 Years or Older: A Systematic Review and Meta-analysis. Ann. Intern. Med. 2017, 166, 419–429. [Google Scholar] [CrossRef]
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. INTERSTROKE investigators. Risk Factors for Ischaemic and Intracerebral Haemorrhagic Stroke in 22 Countries (the INTERSTROKE Study): A Case-Control Study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef]
- Feigin, V.L.; Norrving, B.; Mensah, G.A. Global Burden of Stroke. Circ. Res. 2017, 120, 439–448. [Google Scholar] [CrossRef]
- Rost, N.S.; Wolf, P.A.; Kase, C.S.; Kelly-Hayes, M.; Silbershatz, H.; Massaro, J.M.; D’Agostino, R.B.; Franzblau, C.; Wilson, P.W. Plasma Concentration of C-Reactive Protein and Risk of Ischemic Stroke and Transient Ischemic Attack: The Framingham Study. Stroke 2001, 32, 2575–2579. [Google Scholar] [CrossRef] [PubMed]
- Kurth, T.; Gaziano, J.M.; Berger, K.; Kase, C.S.; Rexrode, K.M.; Cook, N.R.; Buring, J.E.; Manson, J.E. Body Mass Index and the Risk of Stroke in Men. Arch. Intern. Med. 2002, 162, 2557–2562. [Google Scholar] [CrossRef] [PubMed]
- Penn, A.; Snyder, C.A. 1,3 Butadiene, a Vapor Phase Component of Environmental Tobacco Smoke, Accelerates Arteriosclerotic Plaque Development. Circulation 1996, 93, 552–557. [Google Scholar] [CrossRef]
- Dennis, M.S.; Lo, K.M.; McDowall, M.; West, T. Fractures After Stroke: Frequency, Types, and Associations. Stroke 2002, 33, 728–734. [Google Scholar] [CrossRef]
- Pouwels, S.; Lalmohamed, A.; Leufkens, B.; de Boer, A.; Cooper, C.; van Staa, T.; de Vries, F. Risk of Hip/Femur Fracture After Stroke: A Population-Based Case-Control Study. Stroke 2009, 40, 3281–3285. [Google Scholar] [CrossRef]
- Wang, L.; Kang, S.; Zou, D.; Zhan, L.; Li, Z.; Zhu, W.; Su, H. Bone Fracture Pre-ischemic Stroke Exacerbates Ischemic Cerebral Injury in Mice. PLoS ONE 2016, 11, e0153835. [Google Scholar] [CrossRef]
- An, Q.; Chen, Z.; Huo, K.; Su, H.; Qu, Q.M. Risk Factors for Ischemic Stroke Post Bone Fracture. J. Clin. Neurosci. 2019, 59, 224–228. [Google Scholar] [CrossRef]
- Bae, H.S.; Hong, J.H.; Ki, K.D.; Song, J.Y.; Shin, J.W.; Lee, J.M.; Lee, J.K.; Lee, N.W.; Lee, C.; Lee, K.W.; et al. The Effect of Body Mass Index on Survival in Advanced Epithelial Ovarian Cancer. J. Korean Med. Sci. 2014, 29, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Jeong, N.H.; Lee, J.M.; Lee, J.K.; Kim, J.W.; Cho, C.H.; Kim, S.M.; Seo, S.S.; Park, C.Y.; Kim, K.T.; Lee, J. Role of Body Mass Index as a Risk and Prognostic Factor of Endometrioid Uterine Cancer in Korean Women. Gynecol. Oncol. 2010, 118, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Khasraw, M.; Posner, J.B. Neurological Complications of Systemic Cancer. Lancet Neurol. 2010, 9, 1214–1227. [Google Scholar] [CrossRef]
- Sun, M.Y.; Bhaskar, S.M.M. When Two Maladies Meet: Disease Burden and Pathophysiology of Stroke in Cancer. Int. J. Mol. Sci. 2022, 23, 15769. [Google Scholar] [CrossRef] [PubMed]
- Sener, U.; Keser, Z. Ischemic Stroke in Patients with Malignancy. Mayo Clin. Proc. 2022, 97, 2139–2144. [Google Scholar] [CrossRef]
- Jung, S.H. Stroke Rehabilitation Fact Sheet in Korea. Ann. Rehabil. Med. 2022, 46, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, H.; Moon, J.; Shin, J.; Jeong, H.; Kim, Y. Temporal Trend of First-Ever Ischaemic Stroke Incidence from 2010 to 2019 in South Korea: A Nationwide Retrospective Cohort Study. BMJ Open 2022, 12, e059956. [Google Scholar] [CrossRef]
- Kim, J.Y.; Lee, K.J.; Kang, J.; Kim, B.J.; Kim, S.E.; Oh, H.; Park, H.K.; Cho, Y.J.; Park, J.M.; Park, K.Y.; et al. Acute Stroke Care in Korea in 2013–2014: National Averages and Disparities. J. Korean Med. Sci. 2020, 35, e167. [Google Scholar] [CrossRef]
- Choi, H.Y.; Cha, M.J.; Nam, H.S.; Kim, Y.D.; Hong, K.S.; Heo, J.H.; Korean Stroke Unit Study Collaborators. Stroke Units and Stroke Care Services in Korea. Int. J. Stroke 2012, 7, 336–340. [Google Scholar] [CrossRef]

| Characteristics | With Stroke (n = 54) | Without Stroke (n = 590) | p-Value |
|---|---|---|---|
| Median age at diagnosis, years (range) | 65.50 (36–86) | 53 (20–89) | <0.001 |
| Median BMI at diagnosis, kg/m2 (range) | 25 (16–36) | 24 (13–40) | 0.219 |
| Comorbidities, n (%) | |||
| DM | 18 (33.3) | 72 (12.2) | <0.001 |
| HTN | 39 (72.2) | 153 (25.9) | <0.001 |
| PTE/DVT | 5 (9.3) | 25 (4.2) | 0.097 |
| Heart disease 1 | 22 (40.7) | 84 (14.2) | <0.001 |
| Fractures 2 | 4 (7.4) | 19 (3.2) | 0.118 |
| Smoking | 3 (5.6) | 36 (6.1) | >0.999 |
| Cancer type | 0.805 | ||
| Cervix | 21 (38.9) | 236 (40.0) | |
| Endometrium | 17 (31.5) | 162 (27.5) | |
| Ovary | 16 (29.6) | 192 (32.5) | |
| Histological subtype, n (%) | 0.289 | ||
| Usual type 3 | 39 (72.2) | 463 (78.5) | |
| Unusual type | 15 (27.8) | 127 (21.5) | |
| Histological grade, n (%) | 0.170 | ||
| Well/Moderate | 18 (58.1) | 274 (69.9) | |
| Poor | 13 (41.9) | 118 (30.1) | |
| FIGO stage, n (%) | 0.108 | ||
| I/II | 33 (61.1) | 422 (71.5) | |
| III/IV | 21 (38.9) | 168 (28.5) | |
| Type of treatment | |||
| Surgery, n (%) | 42 (77.8) | 528 (89.5) | 0.010 |
| Radiotherapy, n (%) | 15 (27.8) | 130 (22.0) | 0.333 |
| Chemotherapy, n (%) | 31 (57.4) | 304 (51.5) | 0.408 |
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Age (yr) | 1.074 (1.050–1.098) | <0.001 | 1.055 (1.027–1.084) | <0.001 |
| BMI (kg/m2) | 1.042 (0.977–1.112) | 0.210 | ||
| DM | <0.001 | 0.077 | ||
| No (n = 554) | 1.00 (Reference) | 1.00 (Reference) | ||
| Yes (n = 90) | 3.597 (1.941–6.668) | 1.852 (0.934–3.672) | ||
| HTN | <0.001 | <0.001 | ||
| No (n = 452) | 1.00 (Reference) | 1.00 (Reference) | ||
| Yes (n = 192) | 7.426 (3.982–13.850) | 3.579 (1.801–7.115) | ||
| PTE/DVT | 0.103 | |||
| No (n = 614) | 1.00 (Reference) | |||
| Yes (n = 30) | 2.306 (0.845–6.291) | |||
| Heart disease 1 | <0.001 | 0.144 | ||
| No (n = 538) | 1.00 (Reference) | 1.00 (Reference) | ||
| Yes (n = 106) | 4.141 (2.296–7.470) | 1.635 (0.845–3.164) | ||
| Fractures 2 | 0.124 | |||
| No (n = 621) | 1.00 (Reference) | |||
| Yes (n = 23) | 2.404 (0.787–7.341) | |||
| Smoking history | 0.872 | |||
| No (n = 605) | 1.00 (Reference) | |||
| Past/Current (n = 39) | 0.905 (0.269–3.042) | |||
| Cancer type | 0.661 | |||
| Cervix/Endometrium (n = 436) | 1.00 (Reference) | |||
| Ovary (n = 208) | 0.873 (0.475–1.605) | |||
| Histological subtype | 0.291 | |||
| Usual type 3 (n = 502) | 1.00 (Reference) | |||
| Unusual type (n = 142) | 1.402 (0.749–2.625) | |||
| Histological grade | 0.174 | |||
| Well/Moderate (n = 292) | 1.00 (Reference) | |||
| Poor (n = 131) | 1.677 (0.794–3.519) | |||
| Stage | 0.142 | |||
| I/II (n = 455) | 1.00 (Reference) | |||
| III/IV (n = 189) | 1.529 (0.796–3.534) | |||
| Surgery | 0.012 | 0.984 | ||
| No (n = 74) | 1.00 (Reference) | 1.00 (Reference) | ||
| Yes (n = 570) | 0.411 (0.205–0.822) | 0.991 (0.420–2.338) | ||
| Radiotherapy | 0.335 | |||
| No (n = 499) | 1.00 (Reference) | |||
| Yes (n = 145) | 1.361 (0.727–2.546) | |||
| Chemotherapy | 0.408 | |||
| No (n = 309) | 1.00 (Reference) | |||
| Yes (n = 335) | 1.268 (0.722–2.227) | |||
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age (yr) | 1.044 (1.031–1.057) | <0.001 | 1.025 (1.006–1.045) | 0.008 |
| BMI (Kg/m2) | 0.919 (0.879–0.960) | < 0.001 | 0.952 (0.893–1.015) | 0.135 |
| DM | ||||
| No | 1.00 (Reference) | |||
| Yes | 1.287 (0.843–1.965) | 0.242 | ||
| HTN | ||||
| No | 1.00 (Reference) | 1.00 (Reference) | ||
| Yes | 1.433 (1.031–1.993) | 0.032 | 0.706 (0.406–1.227) | 0.217 |
| PTE/DVT | ||||
| No | 1.00 (Reference) | 1.00 (Reference) | ||
| Yes | 3.166 (1.853–5.410) | <0.001 | 2.932 (1.430–6.012) | 0.003 |
| Heart disease 1 | ||||
| No | 1.00 (Reference) | |||
| Yes | 1.196 (0.797–1.793) | 0.388 | ||
| Fracture 2 | ||||
| No | 1.00 (Reference) | |||
| Yes | 1.504 (0.766–2.954) | 0.236 | ||
| Stroke onset | ||||
| No stroke | 1.00 (Reference) | 1.00 (Reference) | ||
| Stroke before/after tx | 2.027 (1.165–3.528) | 0.012 | 2.030 (0.856–4.816) | 0.108 |
| Stroke during tx | 4.279 (2.501–7.321) | <0.001 | 2.182 (0.903–5.272) | 0.083 |
| Cancer type | ||||
| Cervix/Endometrium | 1.00 (Reference) | 1.00 (Reference) | ||
| Ovary | 3.145 (2.277–4.343) | <0.001 | 1.606 (0.958–2.693) | 0.072 |
| Histological subtype | ||||
| Usual 3 | 1.00 (Reference) | 1.00 (Reference) | ||
| Unusual | 2.010 (1.425–2.834) | <0.001 | 1.539 (0.921–2.571) | 0.100 |
| Histological grade | ||||
| Well/Moderate | 1.00 (Reference) | 1.00 (Reference) | ||
| Poor | 4.372(2.851–6.705) | <0.001 | 1.898 (1.142–3.155) | 0.013 |
| Stage | ||||
| I/II | 1.00 (Reference) | 1.00 (Reference) | ||
| III/IV | 8.333 (5.873–11.823) | <0.001 | 3.482 (2.006–6.043) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, J.Y.; Park, K.; Song, J.M.; Pyeon, S.Y.; Lee, S.H.; Chung, Y.S.; Lee, J.-M. Risk Factors and Prognosis of Stroke in Gynecologic Cancer Patients. Cancers 2023, 15, 4895. https://doi.org/10.3390/cancers15194895
Kwon JY, Park K, Song JM, Pyeon SY, Lee SH, Chung YS, Lee J-M. Risk Factors and Prognosis of Stroke in Gynecologic Cancer Patients. Cancers. 2023; 15(19):4895. https://doi.org/10.3390/cancers15194895
Chicago/Turabian StyleKwon, Ji Young, Kena Park, Jeong Min Song, Seung Yeon Pyeon, Seon Hwa Lee, Young Shin Chung, and Jong-Min Lee. 2023. "Risk Factors and Prognosis of Stroke in Gynecologic Cancer Patients" Cancers 15, no. 19: 4895. https://doi.org/10.3390/cancers15194895
APA StyleKwon, J. Y., Park, K., Song, J. M., Pyeon, S. Y., Lee, S. H., Chung, Y. S., & Lee, J.-M. (2023). Risk Factors and Prognosis of Stroke in Gynecologic Cancer Patients. Cancers, 15(19), 4895. https://doi.org/10.3390/cancers15194895






