Depth of Invasion: Influence of the Latest TNM Classification on the Prognosis of Clinical Early Stages of Oral Tongue Squamous Cell Carcinoma and Its Association with Other Histological Risk Factors
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
- -
- Patients had initial clinical stages of oral tongue SCC (cT1, cT2, cN0, stages I, II) according to the eighth edition of the AJCC.
- -
- Patients had undergone surgery at the Oral and Maxillofacial Surgery Department of the Gregorio Marañón University Hospital.
- -
- Patients’ surgical procedures consisted of extensive tumour removal and elective neck dissection.
- -
- The tumour margins of the surgical resection were negative.
- -
- Patients were over the age of 18.
- -
- Disease that extended beyond the anterior two thirds of the tongue, therefore affecting the oropharynx.
- -
- Patients, in whose medical records, variables of interest were not identified.
- -
- Patients who were previously treated for carcinoma of the oral cavity (surgery, radiotherapy, or chemotherapy).
3. Results
3.1. Total Sample Descriptive Analysis
3.2. Descriptive Analysis of the Sample Divided into Subgroups Depending on T Pathological According to DOI
- -
- Subgroup pT1 according to DOI (n = 17): DOI ≤ 5 mm.
- -
- Subgroup pT2 according to DOI (n = 24): DOI between 5 and 10 mm.
- -
- Subgroup pT3 according to DOI (n = 20): DOI > 10 mm.
3.3. Analysis of Primary and Secondary Objectives
3.3.1. Main Aim (DFS, OS)
3.3.2. Secondary Objectives
Clinical and Pathological Discrepancy of the T Category According to DOI
How DOI Impacts the Staging System—Comparison of the 7th and 8th Editions of the AJCC
Correlation of DOI with the Presence of Positive Neck Nodes
Correlation of DOI with Perineural Invasion
Correlation of DOI with Lymphovascular Invasion
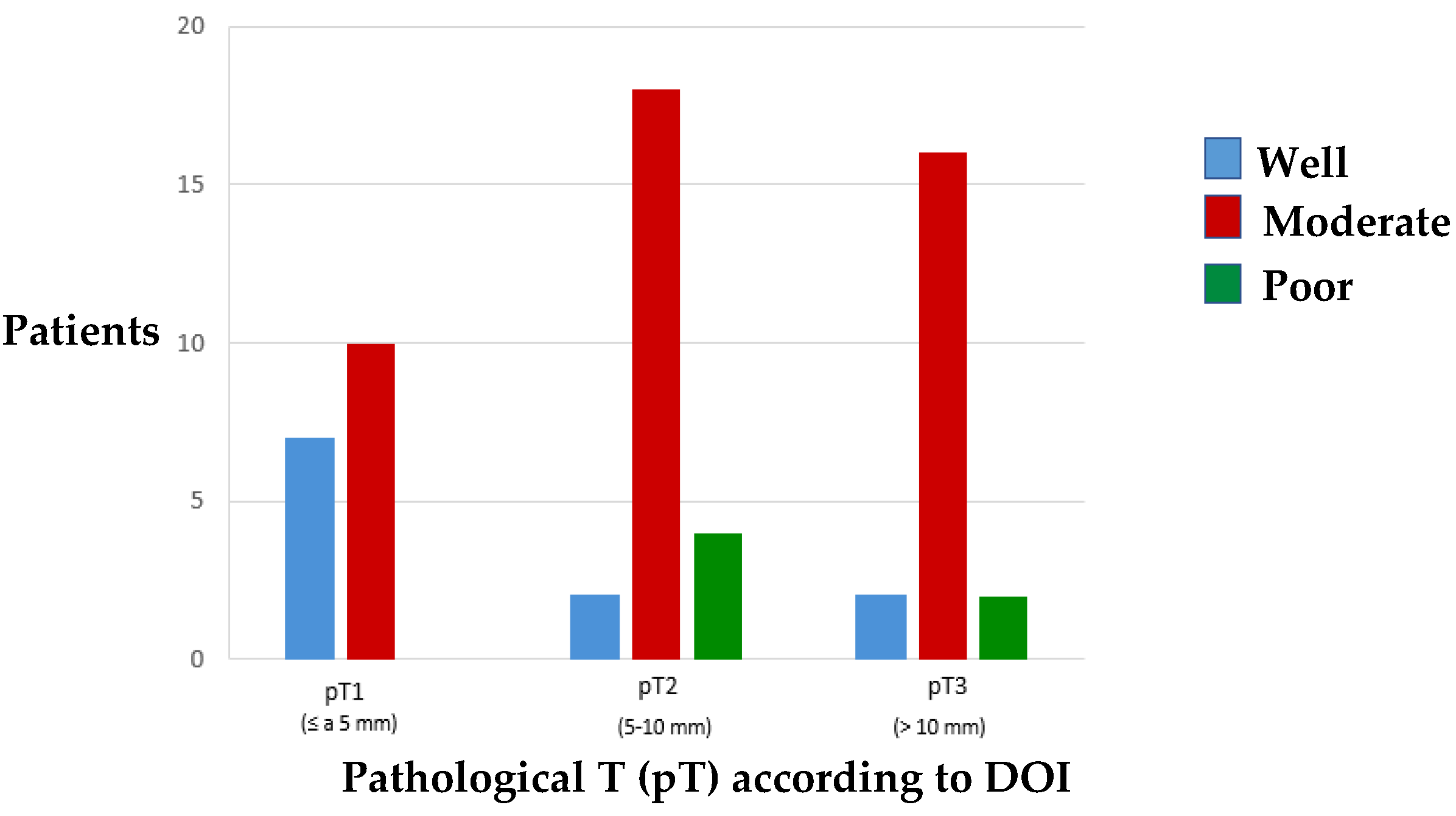
Correlation of DOI with Tumour Differentiation Grade
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Rivera, C. Essentials of oral cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 11884–11894. [Google Scholar] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Chatterjee, A.; Laskar, S.G.; Chaukar, D. Management of early oral cavity squamous cancers. Oral Oncol. 2020, 104, 104627. [Google Scholar] [CrossRef]
- Flach, G.B.; Tenhagen, M.; de Bree, R.; Brakenhoff, R.H.; van der Waal, I.; Bloemena, E.; Kuik, D.J.; Castelijns, J.A.; Leemans, C.R. Outcome of patients with early stage oral cancer managed by an observation strategy towards the N0 neck using ultrasound guided fine needle aspiration cytology: No survival difference as compared to elective neck dissection. Oral Oncol. 2013, 49, 157–164. [Google Scholar] [CrossRef]
- D’Cruz, A.K.; Vaish, R.; Kapre, N.; Dandekar, M.; Gupta, S.; Hawaldar, R.; Agarwal, J.P.; Pantvaidya, G.; Chaukar, D.; Deshmukh, A.; et al. Elective versus Therapeutic Neck Dissection in Node-Negative Oral Cancer. N. Engl. J. Med. 2015, 373, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, I.L.; Ridout, F.; Cheung, S.M.Y.; Shah, N.; Hardee, P.; Surwald, C.; Thiruchelvam, J.; Cheng, L.; Mellor, T.K.; Brennan, P.A.; et al. Nationwide randomised trial evaluating elective neck dissection for early stage oral cancer (SEND study) with meta-analysis and concurrent real-world cohort. Br. J. Cancer 2019, 121, 827–836. [Google Scholar] [CrossRef] [PubMed]
- Schilling, C.; Stoeckli, S.J.; Haerle, S.K.; Broglie, M.A.; Huber, G.F.; Sorensen, J.A.; Bakholdt, V.; Krogdahl, A.; von Buchwald, C.; Bilde, A.; et al. Sentinel European Node Trial (SENT): 3-year results of sentinel node biopsy in oral cancer. Eur. J. Cancer 2015, 51, 2777–2784. [Google Scholar] [CrossRef]
- Boysen, M.; Lövdal, O.; Söberg, R.; Jacobsen, A.B.; Tausjö, J.; Evensen, J.F. Elective radiotherapy of the neck in patients with squamous cell carcinoma of the head and neck. ORL J. Otorhinolaryngol. Relat. Spec. 1992, 54, 103–107. [Google Scholar] [CrossRef]
- Melchers, L.J.; Schuuring, E.; van Dijk, B.A.; de Bock, G.H.; Witjes, M.J.; van der Laan, B.F.; van der Wal, J.E.; Roodenburg, J.L. Tumour infiltration depth ≥ 4 mm is an indication for an elective neck dissection in pT1cN0 oral squamous cell carcinoma. Oral Oncol. 2012, 48, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.H.; Hwang, D.; Lockwood, G.; Goldstein, D.P.; O’Sullivan, B. Predictive value of tumor thickness for cervical lymph-node involvement in squamous cell carcinoma of the oral cavity: A meta-analysis of reported studies. Cancer 2009, 115, 1489–1497. [Google Scholar] [CrossRef] [PubMed]
- Faisal, M.; Abu Bakar, M.; Sarwar, A.; Adeel, M.; Batool, F.; Malik, K.I.; Jamshed, A.; Hussain, R. Depth of invasion (DOI) as a predictor of cervical nodal metastasis and local recurrence in early stage squamous cell carcinoma of oral tongue (ESSCOT). PLoS ONE 2018, 13, e0202632. [Google Scholar] [CrossRef] [PubMed]
- Tarsitano, A.; Del Corso, G.; Tardio, M.L.; Marchetti, C. Tumor Infiltration Depth as Predictor of Nodal Metastasis in Early Tongue Squamous Cell Carcinoma. J. Oral Maxillofac. Surg. 2016, 74, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Pentenero, M.; Gandolfo, S.; Carrozzo, M. Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: A review of the literature. Head Neck 2005, 27, 1080–1091. [Google Scholar] [CrossRef]
- Kowalski, L.P.; Medina, J.E. Nodal metastases: Predictive factors. Otolaryngol. Clin. North Am. 1998, 31, 621–637. [Google Scholar] [CrossRef]
- Nathanson, A.; Agren, K.; Biörklund, A.; Lind, M.G.; Andréason, L.; Anniko, M.; Freijd, A.; Lejdeborn, L.; Kinman, S.; Kumlien, A.; et al. Evaluation of some prognostic factors in small squamous cell carcinoma of the mobile tongue: A multicenter study in Sweden. Head Neck 1989, 11, 387–392. [Google Scholar] [CrossRef]
- Loganathan, P.; Sayan, A.; Hsu, D.W.K.; Paraneetharan, S.; Ilankovan, V. Squamous cell carcinoma of the anterior tongue: Is tumour thickness an indicator for cervical metastasis? Int. J. Oral Maxillofac. Surg. 2017, 46, 407–412. [Google Scholar] [CrossRef] [PubMed]
- charoenrat, P.; Pillai, G.; Patel, S.; Fisher, C.; Archer, D.; Eccles, S.; Rhys-Evans, P. Tumour thickness predicts cervical nodal metastases and survival in early oral tongue cancer. Oral Oncol. 2003, 39, 386–390. [Google Scholar] [CrossRef]
- Lydiatt, W.M.; Patel, S.G.; O’Sullivan, B.; Brandwein, M.S.; Ridge, J.A.; Migliacci, J.C.; Loomis, A.M.; Shah, J.P. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 122–137. [Google Scholar] [CrossRef]
- Lydiatt, W.M.; Patel, S.G.; Rigde, J.A.; O’Sullivan, B.; Shah, J.P. Staging Head and Neck Cancers. In AJCC Cancer Staging Manual, 8th ed.; Amit, M.B., Ed.; Springer Nature: Basel, Switzerland, 2017; Volume 1, pp. 55–65. [Google Scholar]
- Benjamin, M.; Aliano, K.; Davenport, T.; Frank, D. Functional Outcomes Regarding Facial Artery Musculomucosal Flap for Reconstruction of Partial Glossectomy Defects. Ann. Plast. Surg. 2020, 85, S76–S79. [Google Scholar] [CrossRef]
- Engel, H.; Huang, J.J.; Lin, C.Y.; Lam, W.; Kao, H.K.; Gazyakan, E.; Cheng, M.H. A strategic approach for tongue reconstruction to achieve predictable and improved functional and aesthetic outcomes. Plast. Reconstr. Surg. 2010, 126, 1967–1977. [Google Scholar] [CrossRef]
- Braasch, D.C.; Lam, D.; Oh, E.S. Maxillofacial reconstruction with nasolabial and facial artery musculomucosal flaps. Oral Maxillofac. Surg. Clin. North Am. 2014, 26, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Navarro, C.I.; González, T.; Ruiz, J.A.; Navarro Vila, C. Reconstruction of soft tissue defects using microsurgical flaps. In Reconstructive Oral and Maxillofacial Surgery; Navarro Vila, C., Ed.; Springer: Berlin/Heidelberg, Germany, 2015; pp. 103–128. [Google Scholar]
- Sowder, J.C.; Cannon, R.B.; Buchmann, L.O.; Hunt, J.P.; Hitchcock, Y.; Lloyd, S.; Grossmann, K.F.; Monroe, M.M. Treatment-related determinants of survival in early-stage (T1-2N0M0) oral cavity cancer: A population-based study. Head Neck 2017, 39, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Aksu, G.; Karadeniz, A.; Saynak, M.; Fayda, M.; Kadehci, Z.; Kocaelli, H. Treatment results and prognostic factors in oral tongue cancer: Analysis of 80 patients. Int. J. Oral Maxillofac. Surg. 2006, 35, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Yuen, A.P.; Ho, C.M.; Chow, T.L.; Tang, L.C.; Cheung, W.Y.; Ng, R.W.; Wei, W.I.; Kong, C.K.; Book, K.S.; Yuen, W.C.; et al. Prospective randomized study of selective neck dissection versus observation for N0 neck of early tongue carcinoma. Head Neck 2009, 31, 765–772. [Google Scholar] [CrossRef]
- Schilling, C.; Stoeckli, S.J.; Vigili, M.G.; de Bree, R.; Lai, S.Y.; Alvarez, J.; Christensen, A.; Cognetti, D.M.; D’Cruz, A.K.; Frerich, B.; et al. Surgical consensus guidelines on sentinel node biopsy (SNB) in patients with oral cancer. Head Neck 2019, 41, 2655–2664. [Google Scholar] [CrossRef]
- Yang, Y.; Zhou, J.; Wu, H. Diagnostic value of sentinel lymph node biopsy for cT1/T2N0 tongue squamous cell carcinoma: A meta-analysis. Eur. Arch. Otorhinolaryngol. 2017, 274, 3843–3852. [Google Scholar] [CrossRef]
- Moore, C.; Kuhns, J.G.; Greenberg, R.A. Thickness as prognostic aid in upper aerodigestive tract cancer. Arch. Surg. 1986, 121, 1410–1414. [Google Scholar] [CrossRef]
- Ambrosch, P.; Kron, M.; Fischer, G.; Brinck, U. Micrometastases in carcinoma of the upper aerodigestive tract: Detection, risk of metastasizing, and prognostic value of depth of invasion. Head Neck 1995, 17, 473–479. [Google Scholar] [CrossRef]
- Breuninger, H.; Black, B.; Rassner, G. Microstaging of squamous cell carcinomas. Am. J. Clin. Pathol. 1990, 94, 624–627. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.H. Cervical lymph node metastases of oral carcinoma related to the depth of invasion of the primary lesion. J. Surg. Oncol. 1986, 31, 120–122. [Google Scholar] [CrossRef]
- Breslow, A. Thickness, cross-sectional areas and depth of invasion in the prognosis of cutaneous melanoma. Ann. Surg. 1970, 172, 902–908. [Google Scholar] [CrossRef]
- Woolgar, J.A. T2 carcinoma of the tongue: The histopathologist’s perspective. Br. J. Oral Maxillofac. Surg. 1999, 37, 187–193. [Google Scholar] [CrossRef]
- Karas, D.E.; Baredes, S.; Chen, T.S.; Karas, S.F. Relationship of biopsy and final specimens in evaluation of tumor thickness in floor of mouth carcinoma. Laryngoscope 1995, 105, 491–493. [Google Scholar] [CrossRef] [PubMed]
- Morton, R.P.; Ferguson, C.M.; Lambie, N.K.; Whitlock, R.M. Tumor thickness in early tongue cancer. Arch. Otolaryngol. Head Neck Surg. 1994, 120, 717–720. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.R.; Lodge-Rigal, R.D.; Reddick, R.L.; Tudor, G.E.; Shockley, W.W. Prognostic factors in the recurrence of stage I and II squamous cell cancer of the oral cavity. Arch. Otolaryngol. Head Neck Surg. 1992, 118, 483–485. [Google Scholar] [CrossRef] [PubMed]
- Tumuluri, V.; Thomas, G.A.; Fraser, I.S. The relationship of proliferating cell density at the invasive tumour front with prognostic and risk factors in human oral squamous cell carcinoma. J. Oral Pathol. Med. 2004, 33, 204–208. [Google Scholar] [CrossRef]
- Giacomarra, V.; Tirelli, G.; Papanikolla, L.; Bussani, R. Predictive factors of nodal metastases in oral cavity and oropharynx carcinomas. Laryngoscope 1999, 109, 795–799. [Google Scholar] [CrossRef]
- Gonzalez-Moles, M.A.; Esteban, F.; Rodriguez-Archilla, A.; Ruiz-Avila, I.; Gonzalez-Moles, S. Importance of tumour thickness measurement in prognosis of tongue cancer. Oral Oncol. 2002, 38, 394–397. [Google Scholar] [CrossRef]
- Ebrahimi, A.; Gil, Z.; Amit, M.; Yen, T.C.; Liao, C.T.; Chaturvedi, P.; Agarwal, J.P.; Kowalski, L.P.; Kreppel, M.; Cernea, C.R. Primary tumor staging for oral cancer and a proposed modification incorporating depth of invasion: An international multicenter retrospective study. JAMA Otolaryngol—Head Neck Surg. 2014, 140, 1138–1148. [Google Scholar] [CrossRef]
- Pollaers, K.; Hinton-Bayre, A.; Friedland, P.L.; Farah, C.S. AJCC 8th Edition oral cavity squamous cell carcinoma staging—Is it an improvement on the AJCC 7th Edition? Oral Oncol. 2018, 82, 23–28. [Google Scholar] [CrossRef]
- Tirelli, G.; Gatto, A.; Boscolo Nata, F.; Bussani, R.; Piccinato, A.; Marcuzzo, A.V.; Tofanelli, M. Prognosis of oral cancer: A comparison of the staging systems given in the 7th and 8th editions of the American Joint Committee on Cancer Staging Manual. Br. J. Oral Maxillofac. Surg. 2018, 56, 8–13. [Google Scholar] [CrossRef]
- Matos, L.L.; Dedivitis, R.A.; Kulcsar, M.A.V.; de Mello, E.S.; Alves, V.A.F.; Cernea, C.R. External validation of the AJCC Cancer Staging Manual, 8th edition, in an independent cohort of oral cancer patients. Oral Oncol. 2017, 71, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Amit, M.; Tam, S.; Takahashi, H.; Choi, K.Y.; Zafereo, M.; Bell, D.; Weber, R.S. Prognostic performance of the American Joint Committee on Cancer 8th edition of the TNM staging system in patients with early oral tongue cancer. Head Neck 2019, 41, 1270–1276. [Google Scholar] [CrossRef] [PubMed]
- Vuity, D.; McMahon, J.; Takhiuddin, S.; Slinger, C.; McLellan, D.; Wales, C.; MacIver, C.; Thomson, E.; McCaul, J.; Hislop, S. Is the 8th edition of the Union for International Cancer Control staging of oral cancer good enough? Br. J. Oral Maxillofac. Surg. 2018, 56, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Caldeira, P.C.; Soto, A.M.L.; de Aguiar, M.C.F.; Martins, C.C. Tumor depth of invasion and prognosis of early-stage oral squamous cell carcinoma: A meta-analysis. Oral Dis. 2020, 26, 1357–1365. [Google Scholar] [CrossRef] [PubMed]
- Wunschel, M.; Neumeier, M.; Utpatel, K.; Reichert, T.E.; Ettl, T.; Spanier, G. Staging more important than grading? Evaluation of malignancy grading, depth of invasion, and resection margins in oral squamous cell carcinoma. Clin. Oral Investig. 2021, 25, 1169–1182. [Google Scholar] [CrossRef] [PubMed]
- Mattavelli, D.; Ferrari, M.; Taboni, S.; Morello, R.; Paderno, A.; Rampinelli, V.; Del Bon, F.; Lombardi, D.; Grammatica, A.; Bossi, P.; et al. The 8th TNM classification for oral squamous cell carcinoma: What is gained, what is lost, and what is missing. Oral Oncol. 2020, 111, 104937. [Google Scholar] [CrossRef]
- Dirven, R.; Ebrahimi, A.; Moeckelmann, N.; Palme, C.E.; Gupta, R.; Clark, J. Tumor thickness versus depth of invasion—Analysis of the 8th edition American Joint Committee on Cancer Staging for oral cancer. Oral Oncol. 2017, 74, 30–33. [Google Scholar] [CrossRef]
- Tai, S.K.; Li, W.Y.; Chu, P.Y.; Chang, S.Y.; Tsai, T.L.; Wang, Y.F.; Huang, J.L. Risks and clinical implications of perineural invasion in T1-2 oral tongue squamous cell carcinoma. Head Neck 2012, 34, 994–1001. [Google Scholar] [CrossRef]
- Tai, S.K.; Li, W.Y.; Yang, M.H.; Chang, S.Y.; Chu, P.Y.; Tsai, T.L.; Wang, Y.F.; Chang, P.M. Treatment for T1-2 oral squamous cell carcinoma with or without perineural invasion: Neck dissection and postoperative adjuvant therapy. Ann. Surg. Oncol. 2012, 19, 1995–2002. [Google Scholar] [CrossRef]
- Rahima, B.; Shingaki, S.; Nagata, M.; Saito, C. Prognostic significance of perineural invasion in oral and oropharyngeal carcinoma. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 423–431. [Google Scholar] [CrossRef]
- Tai, S.K.; Li, W.Y.; Yang, M.H.; Chu, P.Y.; Wang, Y.F.; Chang, P.M. Perineural invasion as a major determinant for the aggressiveness associated with increased tumor thickness in t1-2 oral tongue and buccal squamous cell carcinoma. Ann. Surg. Oncol. 2013, 20, 3568–3574. [Google Scholar] [CrossRef]
- Jones, H.B.; Sykes, A.; Bayman, N.; Sloan, P.; Swindell, R.; Patel, M.; Musgrove, B. The impact of lymphovascular invasion on survival in oral carcinoma. Oral Oncol. 2009, 45, 10–15. [Google Scholar] [CrossRef]
- Chandu, A.; Adams, G.; Smith, A.C. Factors affecting survival in patients with oral cancer: An Australian perspective. Int. J. Oral Maxillofac. Surg. 2005, 34, 514–520. [Google Scholar] [CrossRef]
- Cassidy, R.J.; Switchenko, J.M.; Jegadeesh, N.; Sayan, M.; Ferris, M.J.; Eaton, B.R.; Higgins, K.A.; Wadsworth, J.T.; Magliocca, K.R.; Saba, N.F.; et al. Association of Lymphovascular Space Invasion With Locoregional Failure and Survival in Patients With Node-Negative Oral Tongue Cancers. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 382–388. [Google Scholar] [CrossRef]
- Broders, A. Squamous cell epithelioma of the lip. A study of five hundred and thirty-seven cases. JAMA 1920, 74, 656–664. [Google Scholar] [CrossRef]
- Weijers, M.; Snow, G.B.; Bezemer, P.D.; van der Waal, I. Malignancy grading is no better than conventional histopathological grading in small squamous cell carcinoma of tongue and floor of mouth: Retrospective study in 128 patients. J. Oral Pathol. Med. 2009, 38, 343–347. [Google Scholar] [CrossRef]
- Migueláñez-Medrán, B.C.; Pozo-Kreilinger, J.J.; Cebrián-Carretero, J.L.; Martínez-García, M.A.; López-Sánchez, A.F. Oral squamous cell carcinoma of tongue: Histological risk assessment. A pilot study. Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e603–e609. [Google Scholar] [CrossRef]
- Frierson, H.F., Jr.; Cooper, P.H. Prognostic factors in squamous cell carcinoma of the lower lip. Hum. Pathol. 1986, 17, 346–354. [Google Scholar] [CrossRef]
- Chuang, S.T.; Chen, C.C.; Yang, S.F.; Chan, L.P.; Kao, Y.H.; Huang, M.Y.; Tang, J.Y.; Huang, C.M.; Huang, C.J. Tumor histologic grade as a risk factor for neck recurrence in patients with T1-2N0 early tongue cancer. Oral Oncol. 2020, 106, 104706. [Google Scholar] [CrossRef] [PubMed]



| Variable | Category | Total Sample (n = 61) N (%) |
|---|---|---|
| * Age (years) | 59.72 ± 15.74 y.o. | |
| Age (years) | Under 40 | 5 (8.2%) |
| 40–60 | 25 (41.0%) | |
| Over 60 | 31 (50.8%) | |
| Gender | Male | 40 (65.6%) |
| Female | 21 (34.4%) | |
| Smoking | No | 35 (57.4%) |
| Yes | 26 (42.6%) | |
| Alcohol intake | No | 50 (82.0%) |
| Yes | 11 (18.0%) |
| Variable | Category | Total Sample (n = 61) N (%) |
|---|---|---|
| Clinical tumour size (cm) | T1 (under 2 cm) | 27 (44.3%) |
| T2 (between 2 and 4 cm) | 34 (55.7%) | |
| Tumour location | Lateral border | 50 (82%) |
| Dorsal tongue (submucosal) | 2 (3.3%) | |
| Ventral tongue | 9 (14.7%) | |
| CT scan | No | 1 (1.6%) |
| Yes | 60 (98.4%) | |
| MR imaging | No | 47 (77.0%) |
| Yes | 14 (23.0%) | |
| Radiological tumour size (cm) | Not appreciable | 24 (39.3%) |
| T1 (under 2 cm) | 23 (37.7%) | |
| T2 (between 2 and 4 cm) | 14 (23%) | |
| Reconstruction | Direct closure, granulation | 28 (45.9%) |
| Local flap | 15 (24.6%) | |
| Microsurgery | 18 (29.5%) | |
| Elective neck dissection | Unilateral | 33 (54.1%) |
| Bilateral | 28 (45.9%) | |
| Postoperative radiotherapy | No | 32 (52.5%) |
| Yes | 29 (47.5%) | |
| Postoperative chemotherapy | No | 59 (96.7%) |
| Yes | 2 (3.3%) |
| Variable | Category | Total Sample (n = 61) N (%) |
|---|---|---|
| * Depth of invasion (mm) | 9.03 ± 5.34 mm | |
| Tumour differentiation grade | Well | 11 (18.0%) |
| Moderate | 44 (72.2%) | |
| Poor | 6 (9.8%) | |
| Perineural invasion | No | 37 (60.7%) |
| Yes | 24 (39.3%) | |
| Lymphovascular invasion | No | 56 (91.8%) |
| Yes | 5 (8.2%) | |
| Pathological T according to DOI (mm) | pT1 (under 5 mm) | 17 (27.9%) |
| pT2 (between 5 and 10 mm) | 24 (39.43%) | |
| pT3 (over 10 mm) | 20 (32.8%) | |
| Pathological T according to size (cm) | pT1 (under 2 cm) | 30 (49.2%) |
| pT2 (between 2 and 4 cm) | 28 (45. 9%) | |
| pT3 (over 4 cm) | 3 (4.9%) | |
| Pathological T of the 7th edition of the AJCC | pT1 | 30 (49.2%) |
| pT2 | 28 (45.9%) | |
| pT3 | 3 (4.9%) | |
| Pathological T of the 8th edition of the AJCC | pT1 | 15 (24.6%) |
| pT2 | 25 (41.0%) | |
| pT3 | 21 (34.4%) | |
| Histological positive neck | No | 40 (65.6%) |
| Yes | 21 (34.4%) | |
| Histological neck | pN0 | 40 (65.5%) |
| pN+ ipsilaterally | 17 (27.9%) | |
| pN+ bilaterally | 4 (6.6%) | |
| Extranodal extension | No | 59 (95.1%) |
| Yes | 3 (4.9%) | |
| Histological neck according to the 7th edition of the AJCC | pN0 | 40 (65.6%) |
| pN1 | 10 (16.4%) | |
| pN2b | 7 (11.5%) | |
| pN2c | 4 (6.5%) | |
| Histological neck according to the 8th edition of the AJCC | pN0 | 40 (65.6%) |
| pN1 | 9 (14.8%) | |
| pN2a | 1 (1.6%) | |
| pN2b | 6 (9.8%) | |
| pN2c | 3 (4.9%) | |
| pN3b | 2 (3.3%) | |
| Staging according to the 7th edition of the AJCC | Stage I | 24 (39.3%) |
| Stage II | 15 (24.7%) | |
| Stage III | 11 (18.0%) | |
| Stage IVa | 11 (18.0%) | |
| Staging according to the 8th edition of the AJCC | Stage I | 13 (21.3%) |
| Stage II | 19 (31.1%) | |
| Stage III | 17 (27.9%) | |
| Stage IVa | 10 (16.4%) | |
| Stage IVb | 2 (3.3%) |
| Variable | Category | Total Sample (n = 61) N (%) |
|---|---|---|
| Loco-regional recurrence | No | 47 (77.0%) |
| Yes | 14 (23.0%) | |
| Distant recurrence | No | 56 (91.8%) |
| Yes | 5 (8.2%) | |
| Total recurrence | No | 47 (77.0%) |
| Yes | 14 (23.0%) | |
| Deaths | No | 49 (80.3%) |
| Yes | 12 (19.7%) |
| Variable | Category | Subgroup pT1 % (CI 95) | Subgroup pT2 % (CI 95) | Subgroup T3 % (CI 95) | p Value |
|---|---|---|---|---|---|
| * Age (years old) | 63.47 ± 17.80 | 58.04 ± 15.32 | 58.55 ± 14.65 | 0.411 | |
| Age (years old) | Under 40 | 40.0% (9.4–79.1) | 60.0% (20.9–90.6) | 0.0% | 0.357 |
| 40–60 | 20.0% (8.1–38.4) | 36.0% (19.5–55.5) | 44.0% (26.1–63.2) | ||
| Over 60 | 32.3% (17.9–49.7) | 38.7% (23.2–56.2) | 29.0% (15.4–46.3) | ||
| Gender | Male | 35.0% (21.7–50.4) | 35.0% (21.7–50.4) | 30.0% (17.6–45.2) | 0.228 |
| Female | 14.3% (4.2–33.4) | 47.6% (27.7–68.1) | 38.1% (19.9–59.3) | ||
| Smoking | No | 22.9% (11.4–38.5) | 40.0% (25.1–56.5) | 37.1% (22.7–52.7) | 0.542 |
| Yes | 34.6% (18.7–53.7) | 38.5% (21.8–57.6) | 26.9% (12.9–45.7) | ||
| Alcohol intake | No | 28.0% (17.0–41.4) | 38.0% (25.5–51.8) | 34.0% (22.1–47.7) | 0.881 |
| Yes | 27.3% (8.3–56.5) | 45.4% (20.0–73.0) | 27.3% (8.3–56.5) |
| Variable | Category | Subgroup pT1 % (CI 95) | Subgroup pT2 % (CI 95) | Subgroup pT3 % (CI 95) | p Value |
|---|---|---|---|---|---|
| Clinical tumour size (cm) | T1 (under 2 cm) | 48.1% (30.3–66.4) | 37.1% (20.9–55.8) | 14.8% (5.2–31.5) | 0.002 |
| T2 (between 2 and 4 cm) | 11.8% (4.1–25.6) | 41.2% (25.9–57.9) | 47.0% (31.1–63.5) | ||
| Tumour location | Lateral border | 30.0% (18.7–43.6) | 36.0% (23.8–49.8) | 34.0% (22.1–47.7) | 0.726 |
| Dorsal tongue (submucosal) | 0.0% | 50.0% (6.1–93.9) | 50.0% (6.1–93.9) | ||
| Ventral tongue | 22.2% (4.9–54.4) | 55.6% (25.4–82.7) | 22.2% (4.9–54.4) | ||
| CT scan | No | 0.0% | 0.0% | 100.0% | 0.353 |
| Yes | 28.3% (18.1–40.6) | 40.0% (28.3–52.6) | 31.7% (21–44.1) | ||
| MR imaging | No | 27.7% (16.5–41.5) | 40.4% (27.3–54.7) | 31.9% (20.0–46.0) | 0.946 |
| Yes | 28.6% (10.5–54.5) | 35.7% (15.1–65.5) | 35.7% (15.1–65.5) | ||
| Radiological tumour size (cm) | Not appreciable | 33.3% (17.2–53.2) | 45.8% (27.3–65.3) | 20.9% (8.4–39.8) | 0.048 |
| T1 (under 2 cm) | 39.1% (21.4–59.4) | 30.4% (14.8–50.7) | 30.5% (14.8–50.7) | ||
| T2 (between 2 and 4 cm) | 0.0% | 42.9% (20.3–68.1) | 57.1% (31.9–79.7) | ||
| Reconstruction | Direct closure, granulation | 50.0% (32.2–67.8) | 50.0% (32.2–67.8) | 0.0% | <0.001 |
| Loco-regional flap | 6.6% (0.7–27.2) | 46.7% (23.9–70.6) | 46.7% (23.9–70.6) | ||
| Microsurgery | 11.1% (2.4–31.1) | 16.7% (4.9–38.1) | 72.2% (49.4–88.5) | ||
| Elective neck dissection | Unilateral | 39.4% (22.4–54.8) | 51.5% (36.2–69.5) | 9.1% (2.7–23) | <0.001 |
| Bilateral | 14.3% (5.0–30.5) | 25.0% (11.9–42.9) | 60.7% (42.3–77) | ||
| Postoperative radiotherapy | No | 43.8% (27.7–60.9) | 50.0% (33.3–66.7) | 6.2% (1.3–18.6) | <0.001 |
| Yes | 10.3% (3.0–25.1) | 27.6% (14.0–45.4) | 62.1% (44–77.9) | ||
| Postoperative chemotherapy | No | 28.8% (18.5–41.2) | 39.0% (27.3–51.7) | 32.2% (21.4–44.8) | 0.663 |
| Yes | 0.0% | 50.0% (6.1–93.9) | 50.0% (6.1–93.9) |
| Variable | Category | Subgroup pT1 % (CI 95) | Subgroup pT2 % (CI 95) | Subgroup pT3 % (CI 95) | p Value |
|---|---|---|---|---|---|
| * DOI (mm) | 3.41 ± 1.32 | 7.88 ± 1.96 | 15.20 ± 3.73 | <0.001 | |
| Tumour differentiation grade | Well | 63.6% (34.8–86.3) | 18.2% (4.0–46.7) | 18.2% (4.0–46.7) | 0.034 |
| Moderate | 22.7% (12.3–36.6) | 40.9% (27.3–55.6) | 36.4% (23.4–51.1) | ||
| Poor | 0.0% | 66.7% (28.6–92.3) | 33.3% (7.7–71.4) | ||
| Perineural invasion | No | 40.5% (25.9–96.6) | 40.5% (25.9–96.6) | 19.0% (8.9–33.6) | 0.004 |
| Yes | 8.3% (1.8–24.1) | 37.5% (20.4–57.4) | 54.2% (34.7–72.7) | ||
| Lymphovascular invasion | No | 30.4% (19.5–43.2) | 37.5% (25.7–50.5) | 32.1% (21.0–45.0) | 0.334 |
| Yes | 0.0% | 60.0% (20.9–90.6) | 40.0% (9.4–79.1) | ||
| Pathological T according to size (cm) | pT1 (under 2 cm) | 50.0% (32.8–67.2) | 40.0% (24–57.8) | 10.0% (2.9–24.3) | 0.001 |
| pT2 (between 2 and 4 cm) | 7.1% (1.5–21.0) | 39.3% (23.0–57.7) | 53.6% (35.5–70.9) | ||
| pT3 (over 4 cm) | 0.0% | 33.3% (3.9–82.3) | 66.7% (17.7–96.1) | ||
| Pathological T of the 7th edition of the AJCC | pT1 | 50.0% (32.8–67.2) | 40.0% (24.0–57.8) | 10.0% (2.9–24.3) | 0.001 |
| pT2 | 7.1% (1.5–21.0) | 39.3% (23.0–57.7) | 53.6% (35.5–70.9) | ||
| pT3 | 0.0% | 33.3% (3.9–82.3) | 66.7% (17.7–96.1) | ||
| Pathological T of the 8th edition of the AJCC | pT1 | 100.0% | 0.0% | 0.0% | <0.001 |
| pT2 | 8.0% (1.7–23.0) | 92.0% (76.7–98.3) | 0.0% | ||
| pT3 | 0.0% | 4.8% (0.5–20.2) | 95.2% (79.8–99.5) | ||
| Histological positive neck | No | 35.0% (21.7–50.4) | 45.0% (30.4–60.3) | 20.0% (9.9–30.2) | 0.012 |
| Yes | 14.3% (4.2–33.4) | 28.6% (12.9–49.7) | 57.1% (36.2–76.3) | ||
| Histological neck | pN0 | 35.0% (21.7–50.4) | 45.0% (30.4–60.3) | 20.0% (9.9–34.2) | 0.045 |
| pN+ ipsilateral | 17.6% (5.2–40.0) | 29.4% (12.2–53.0) | 53.0% (30.3–74.6) | ||
| pN+ bilateral | 0.0% | 25.0% (2.8–71.6) | 75.0% (28.4–97.2) | ||
| Extranodal extension | No | 29.3% (18.8–41.8) | 37.9% (26.3–50.8) | 32.8% (21.7–45.4) | 0.478 |
| Yes | 0.0% | 66.7% (17.7–96.1) | 33.3% (3.9–82.3) | ||
| Histological neck according to the 7th edition of the AJCC | pN0 | 35.0% (21.7–50.4) | 45.0% (30.4–60.3) | 20.0% (9.9–34.2) | 0.099 |
| pN1 | 20.0% (4.4–50.3) | 20.0% (4.4–50.3) | 60.0% (30.4–84.7) | ||
| pN2b | 14.2% (1.6–50.1) | 42.9% (13.9–76.5) | 42.9% (13.9–76.5) | ||
| pN2c | 0.0% | 25.0% (2.8–71.6) | 75.0% (28.4–97.2) | ||
| Histological neck according to the 8th edition of the AJCC | pN0 | 35.0% (21.7–50.4) | 45.0% (30.4–60.3) | 20.0% (9.9–34.2) | 0.091 |
| pN1 | 22.2% (4.9–54.4) | 22.2% (4.9–54.4) | 55.6% (25.4–82.7) | ||
| pN2a | 0.0% | 0.0% | 100% | ||
| pN2b | 16.7% (1.9–55.8) | 33.3% (7.7–71.4) | 50.0% (16.7–83.3) | ||
| pN2c | 0.0% | 0.0% | 100.0% | ||
| pN3b | 0.0% | 100.0% | 0.0% | ||
| Staging according to the 7th edition of the AJCC | Stage I | 52.0% (33.1–70.5) | 36.0% (19.5–55.5) | 12.0% (3.5–28.7) | 0.001 |
| Stage II | 6.6% (0.7–27.2) | 66.7% (41.6–86.0) | 26.7% (9.7–51.7) | ||
| Stage III | 18.2% (4.0–46.7) | 18.2% (4.0–46.7) | 63.6% (34.8–86.3) | ||
| Stage Iva | 9.1% (1.1–38.1) | 36.3% (9.3–60.6) | 54.6% (30.4–84.7) | ||
| Staging according to the 8th edition of the AJCC | Stage I | 100.0% | 0.0% | 0.0% | <0.001 |
| Stage II | 5.3% (0.6–22.1) | 94.7% (77.9–99.4) | 0.0% | ||
| Stage III | 11.8% (2.5–32.7) | 11.8% (2.5–32.7) | 76.4% (53.3–91.5) | ||
| Stage Iva | 10.0% (1.2–41.4) | 20.0% (4.9–54.4) | 70.0% (34.8–89.6) | ||
| Stage Ivb | 0.0% | 100.0% | 0.0% |
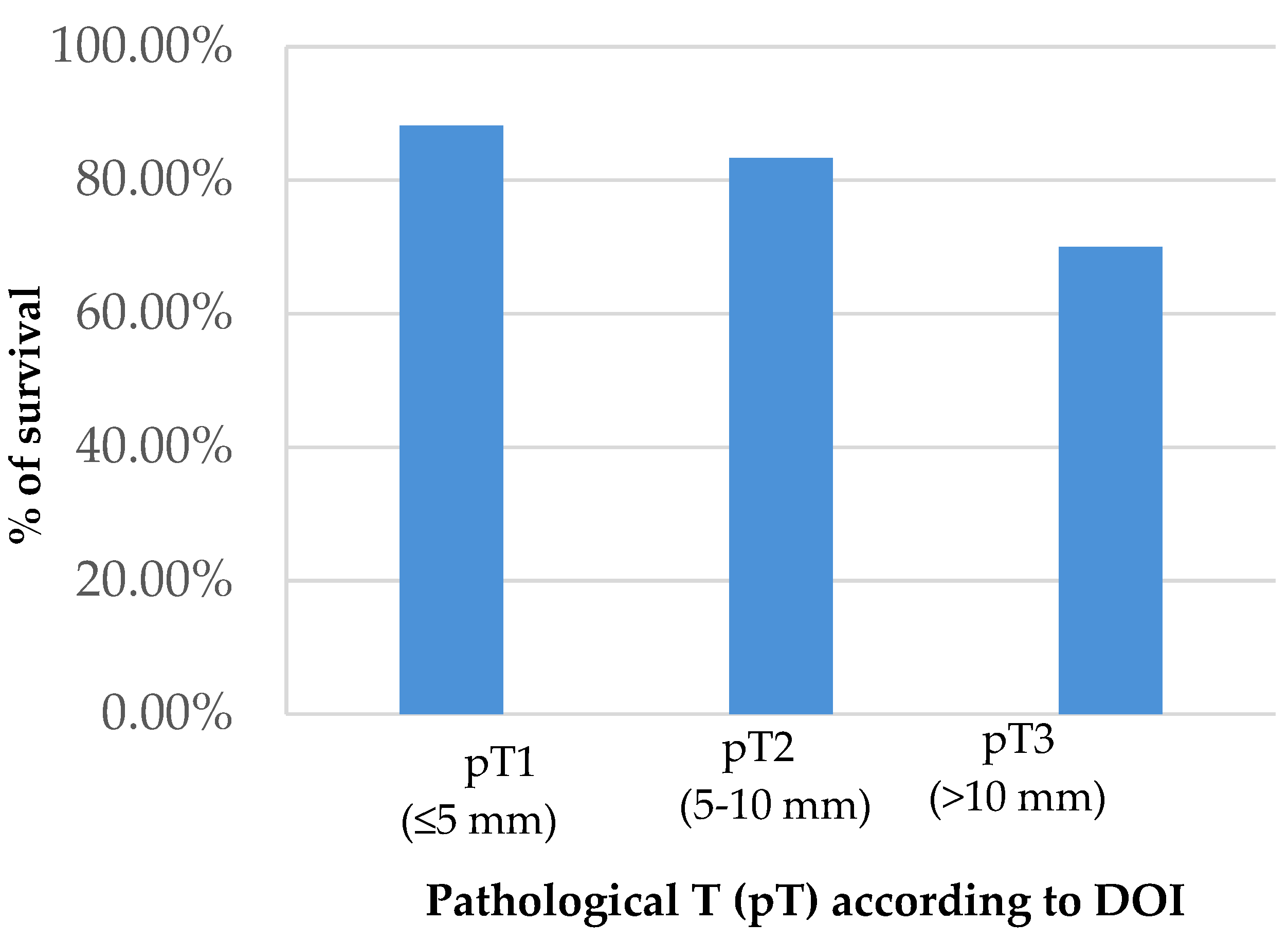
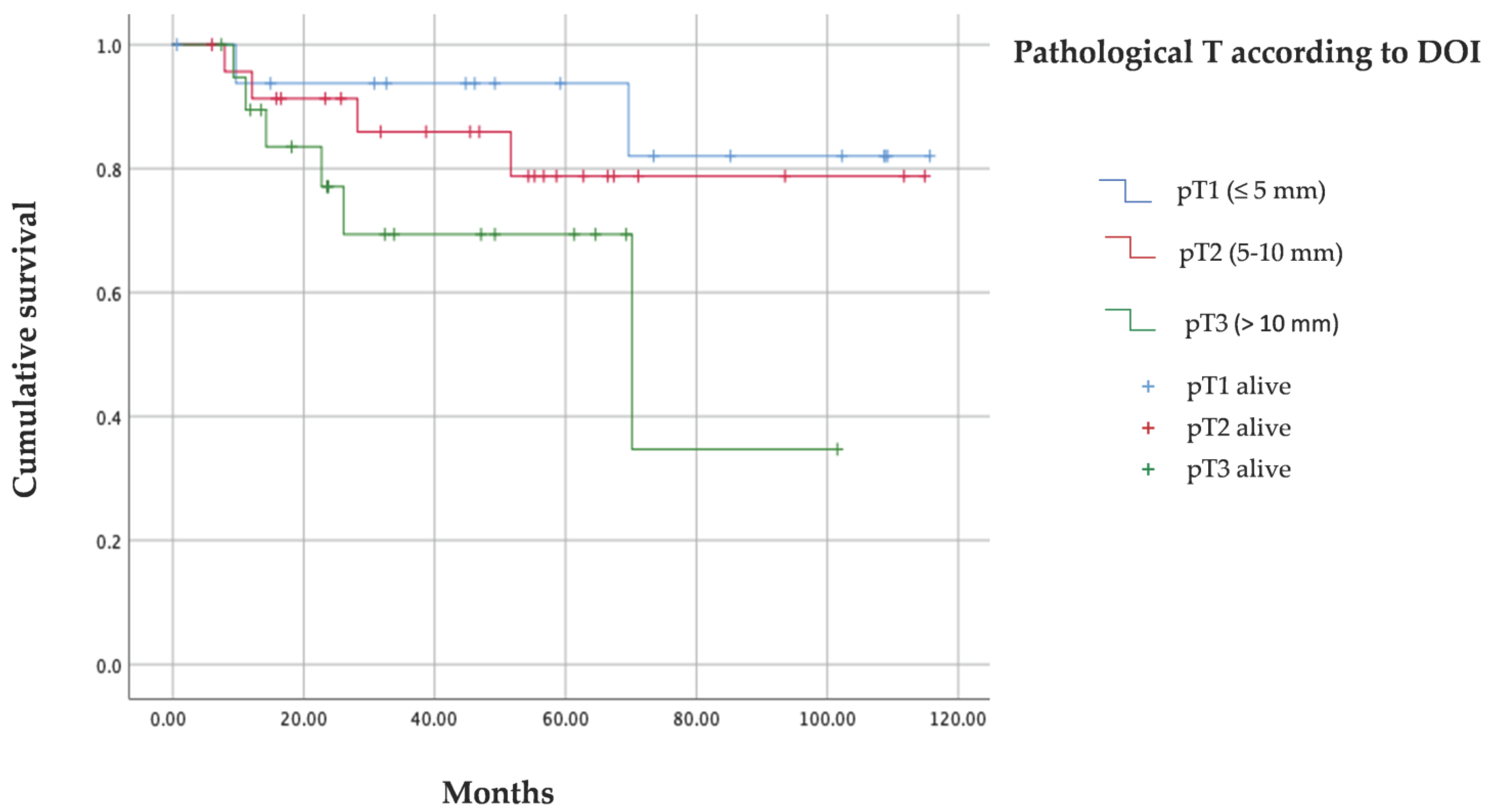
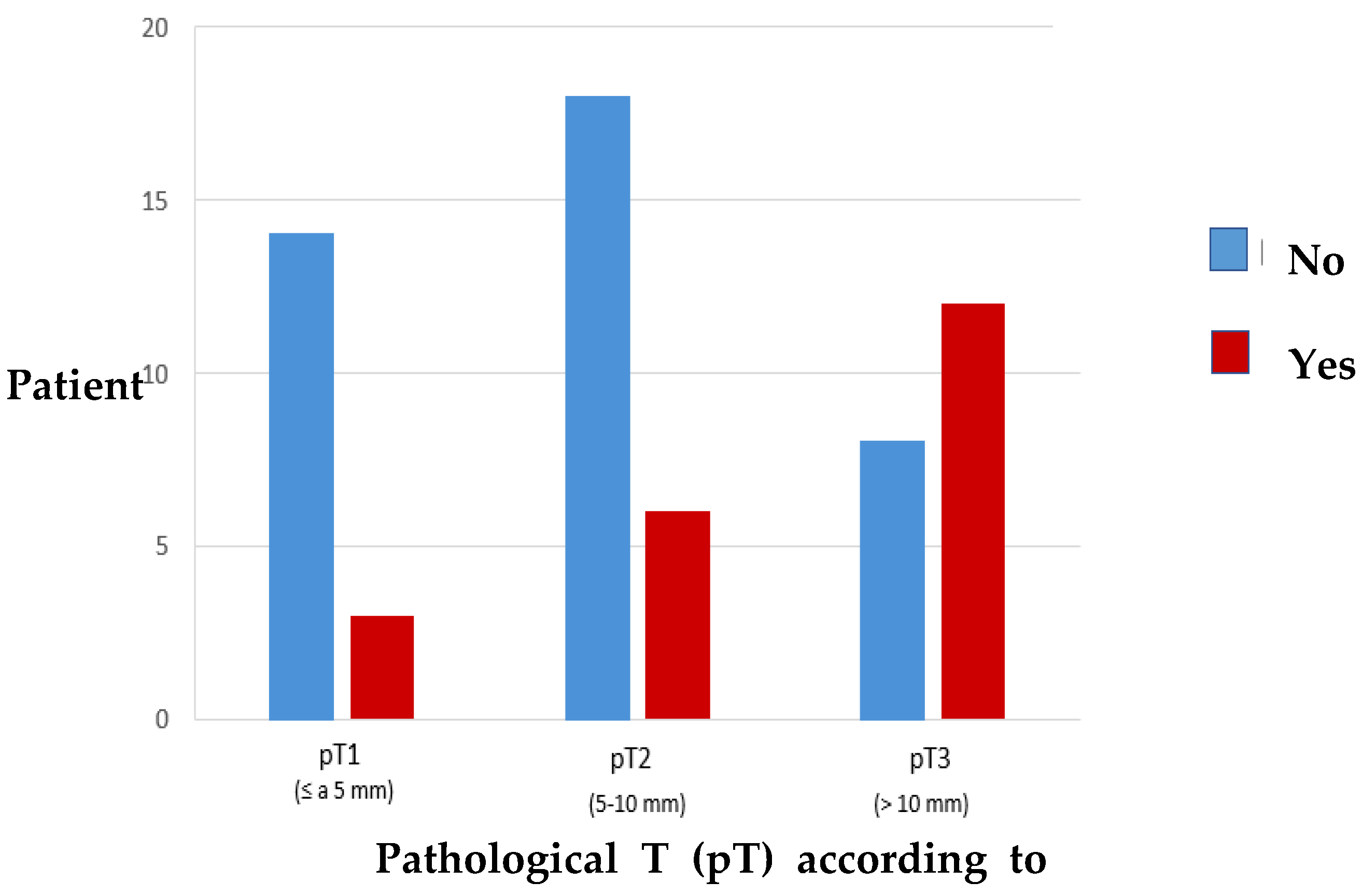
| Variable | Category | Subgroup pT1 % (CI 95) | Subgroup pT2 % (CI 95) | Subgroup pT3 % (CI 95) | p Value |
|---|---|---|---|---|---|
| Loco-regional recurrence | No | 34.8% (22.3–49.1%) | 39.1% (26.0–53.5%) | 26.1% (15.1–40.0%) | 0.056 |
| Yes | 6.7% (0.7–27.2%) | 40.0% (18.8–64.7%) | 53.3% (29.4–76.1%) | ||
| Distant recurrence | No | 28.6% (18.0–41.3%) | 39.3% (27.3–52.4%) | 32.1% (21.0–45.0%) | 0.901 |
| Yes | 20.0% (2.3–62.9%) | 40.0% (9.4–79.1%) | 40.0% (9.4–79.1%) | ||
| Total recurrence | No | 34.8% (22.3–49.1%) | 39.1% (26–53.5%) | 26.1% (15.1–40.0%) | 0.056 |
| Yes | 6.7% (0.7–27.2%) | 40% (18.8–64.7%) | 53.3% (29.4–76.1%) | ||
| Deaths | No | 30.6% (19.1–44.3%) | 40.8% (27.9–54.8%) | 28.6% (24.3–75.7%) | 0.340 |
| Yes | 16.7% (3.6–43.6%) | 33.3% (12.5–61.2%) | 50.0% (24.3–75.7%) |
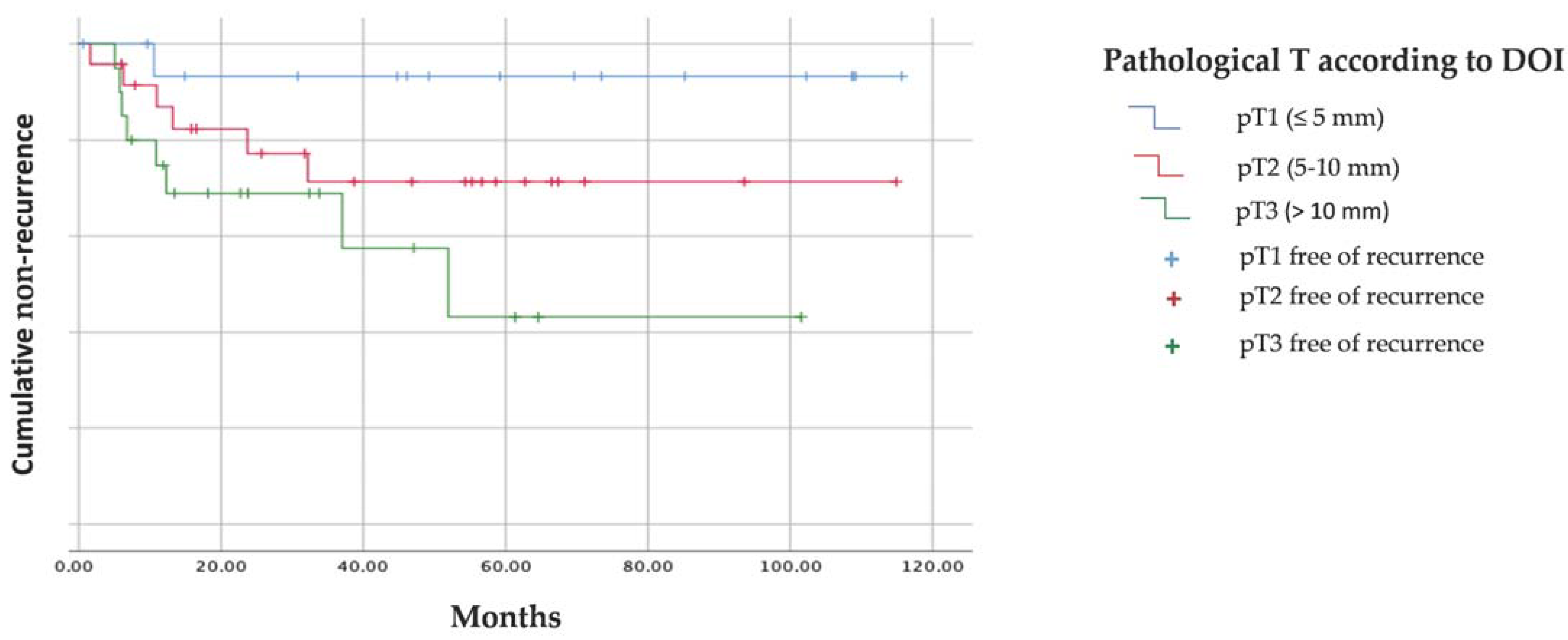
| Pathological T According to T | Media (Estimated ± Deviation) | Log-Rank (Mantel–Cox) (p Value) |
|---|---|---|
| pT1 (≤5 mm) | 108.67 ± 6.77 months | 0.043 |
| pT2 (5–10 mm) | 86.44 ± 9.92 months | |
| pT3 (>10 mm) | 57.93 ± 11.26 months |
| Pathological T According to DOI | Media (Estimated ± Deviation) | Log-Rank (Mantel–Cox) (p Value) |
|---|---|---|
| pT1 (≤5 mm) | 103.64 ± 7.89 months | 0.139 |
| pT2 (5–10 mm) | 96.59 ± 8.24 months | |
| pT3 (>10 mm) | 64.96 ± 11.03 months |
| Global T Category (Size and DOI) According to the 8th Edition of the AJCC | ||||
|---|---|---|---|---|
| Patients pt1 | Patients pt2 | Patients pt3 | Total | |
| Patients clinical T1 | 13 | 10 * | 4 * | 27 |
| Patients clinical T2 | 4 | 14 | 16 * | 34 |
| Total | 17 | 24 | 20 | 61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarro Cuéllar, I.; Espías Alonso, S.; Alijo Serrano, F.; Herrera Herrera, I.; Zamorano León, J.J.; Del Castillo Pardo de Vera, J.L.; López López, A.M.; Maza Muela, C.; Arenas de Frutos, G.; Ochandiano Caicoya, S.; et al. Depth of Invasion: Influence of the Latest TNM Classification on the Prognosis of Clinical Early Stages of Oral Tongue Squamous Cell Carcinoma and Its Association with Other Histological Risk Factors. Cancers 2023, 15, 4882. https://doi.org/10.3390/cancers15194882
Navarro Cuéllar I, Espías Alonso S, Alijo Serrano F, Herrera Herrera I, Zamorano León JJ, Del Castillo Pardo de Vera JL, López López AM, Maza Muela C, Arenas de Frutos G, Ochandiano Caicoya S, et al. Depth of Invasion: Influence of the Latest TNM Classification on the Prognosis of Clinical Early Stages of Oral Tongue Squamous Cell Carcinoma and Its Association with Other Histological Risk Factors. Cancers. 2023; 15(19):4882. https://doi.org/10.3390/cancers15194882
Chicago/Turabian StyleNavarro Cuéllar, Ignacio, Samuel Espías Alonso, Francisco Alijo Serrano, Isabel Herrera Herrera, José Javier Zamorano León, José Luis Del Castillo Pardo de Vera, Ana María López López, Cristina Maza Muela, Gema Arenas de Frutos, Santiago Ochandiano Caicoya, and et al. 2023. "Depth of Invasion: Influence of the Latest TNM Classification on the Prognosis of Clinical Early Stages of Oral Tongue Squamous Cell Carcinoma and Its Association with Other Histological Risk Factors" Cancers 15, no. 19: 4882. https://doi.org/10.3390/cancers15194882
APA StyleNavarro Cuéllar, I., Espías Alonso, S., Alijo Serrano, F., Herrera Herrera, I., Zamorano León, J. J., Del Castillo Pardo de Vera, J. L., López López, A. M., Maza Muela, C., Arenas de Frutos, G., Ochandiano Caicoya, S., Tousidonis Rial, M., García Sevilla, A., Antúnez-Conde, R., Cebrián Carretero, J. L., García-Hidalgo Alonso, M. I., Salmerón Escobar, J. I., Burgueño García, M., Navarro Vila, C., & Navarro Cuéllar, C. (2023). Depth of Invasion: Influence of the Latest TNM Classification on the Prognosis of Clinical Early Stages of Oral Tongue Squamous Cell Carcinoma and Its Association with Other Histological Risk Factors. Cancers, 15(19), 4882. https://doi.org/10.3390/cancers15194882











