Overview, Diagnosis, and Perioperative Systemic Therapy of Upper Tract Urothelial Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
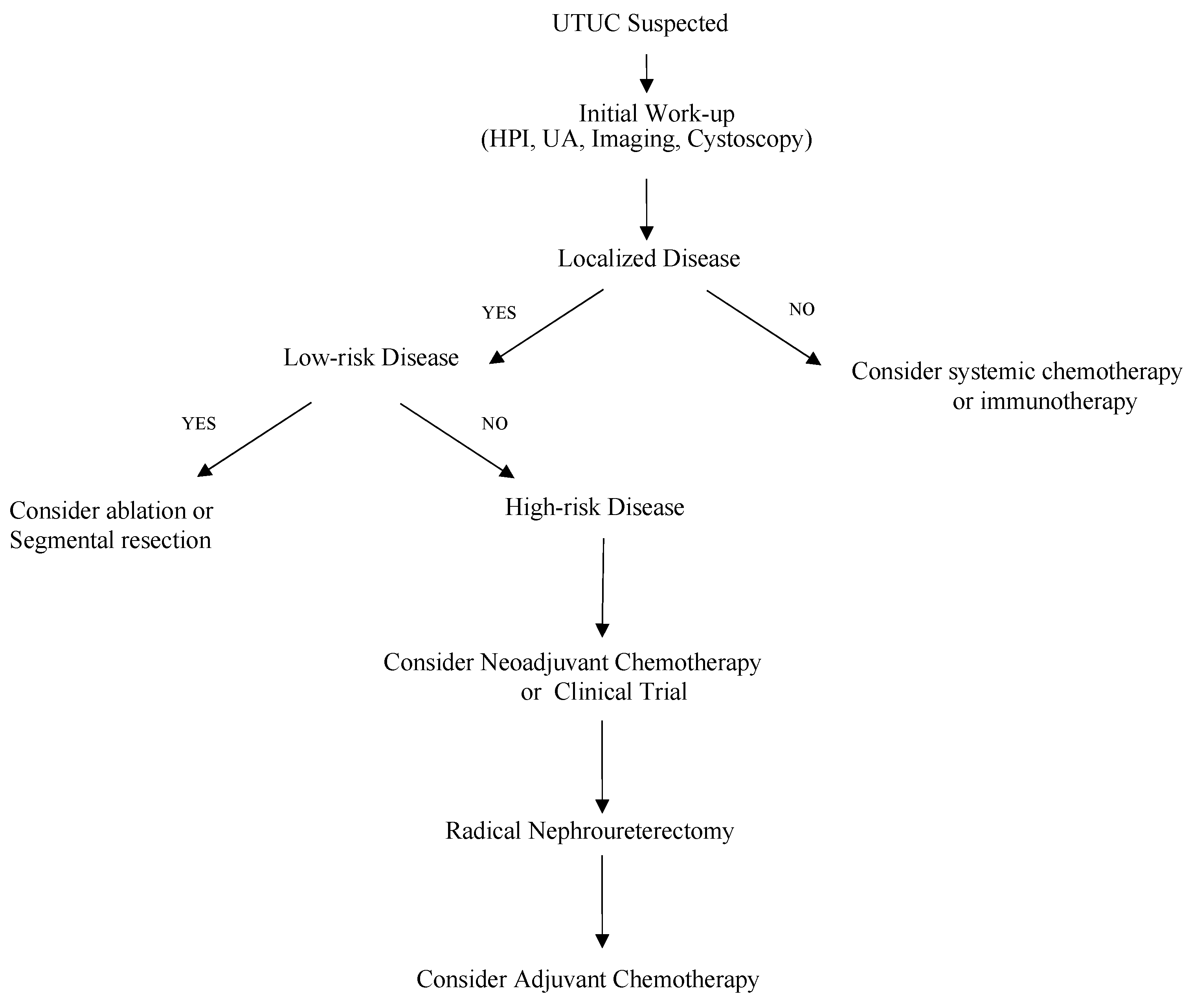
2. Diagnosis
3. Treatment:
3.1. Perioperative Chemotherapy
3.2. Perioperative Immunotherapy
4. Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Name of Trial or Study Drug | NCT Identifier | Trial Setting | Clinical Setting | Number of Study Subjects/UTUC Patients | Primary Measure | Treatment Efficacy | Treatment |
|---|---|---|---|---|---|---|---|
| POUT | NCT01993979 | Phase 3 | Adjuvant | 261 total/261 UTUC patients | Disease-free Survival | 3-year DFS: 77% vs. 46% (Treatment vs. Surveillance) | Chemotherapy (Cisplatin or Carboplatin) vs. Surveillance |
| PURE-02 | NCT02736266 | Phase 2 | Neoadjuvant | 10 total/10 UTUC | Pathological Response | Not Reported | Pembrolizumab |
| Checkmate 274 | NCT02632409 | Phase 3 | Adjuvant | 709 total/149 UTUC patients | Disease-free Survival | DFS: 21.2 months vs. 20.8 months (Nivolumab vs. Placebo) | Nivolumab vs. Placebo |
| Imvigor-210 | NCT02108652 | Phase 2 | Advanced | 119 total/33 UTUC patients | Objective Response Rate | Not Reported | Atezolizumab |
| AMBASSADOR | NCT03244384 | Phase 3 | Adjuvant | 739 total | Overall Survival, Disease-free Survival | DFS: 16.9 months vs. 8.3 months (Pembrolizumab vs. Surveillance) | Pembrolizumab vs. Surveillance |
| Infigratanib (Lyou et al. [47]) | NCT01004224 | Phase 1b | Advanced | 67 total/8 UTUC patients | Objective Response Rate | ORR: 31% | Infigratanib |
| Erdafitinib (Loriot et al. [46]) | NCT02365597 | Phase 2 | Advanced | 99 total/99 UTUC patients | Objective Response Rate | ORR: 40% | Erdafitinib |
| Gemcitabine and Cisplatin (Coleman et al. [33]) | NCT01261728 | Phase 2 | Neoadjuvant | 57 total/57 UTUC patients | Pathological Response Rate | PRR: 63% | Gemcitabine and Cisplatin |
| aMVAC vs. GCa (Margulis et al. [29]) | NCT02412670 | Phase 2 | Neoadjuvant | 30 total/30 UTUC patients | Pathologic Complete Response | PCR: 14% (aMVAC arm) | Accelerated Methotrexate, Vinblastine, Doxorubicin, Cisplatin vs. Gemcitabine and Carboplatin |
| Nivolumab plus Ipilimumab (Teo M. et al. [37]) | NCT03520491 | Phase 2 | Neoadjuvant | 45 total | Pathologic Complete Response | Not Reported | Nivolumab vs. Nivolumab + Ipilimumab |
| ABACUS | NCT02662309 | Phase 2 | Neoadjuvant | 96 total | Pathologic Complete Response | PCR: 31% | Atezolizumab |
| DANUBE | NCT02516241 | Phase 3 | Advanced | 1032 total | Overall Survival | OS: 15.1 months vs. 12.1 months (Treatment vs. Standard of Care) | Durvalumab + Tremelimumab vs. SOC |
| iNDUCT | NCT04617756 | Phase 2 | Neoadjuvant | 50 total | Pathologic Complete Response | Not Reported | Durvalumab + Gemcitabine/(Cisplatin or Carboplatin) |
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Margulis, V.; Shariat, S.F.; Matin, S.F.; Kamat, A.M.; Zigeuner, R.; Kikuchi, E.; Lotan, Y.; Weizer, A.; Raman, J.D.; Wood, C.G.; et al. Outcomes of radical nephroureterectomy: A series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer 2009, 115, 1224–1233. [Google Scholar] [CrossRef] [PubMed]
- Comperat, E.; Larre, S.; Roupret, M.; Neuzillet, Y.; Pignot, G.; Quintens, H.; Houede, N.; Roy, C.; Durand, X.; Varinot, J.; et al. Clinicopathological characteristics of urothelial bladder cancer in patients less than 40 years old. Virchows Arch. 2015, 466, 589–594. [Google Scholar] [CrossRef]
- Oswald, D.; Pallauf, M.; Deininger, S.; Torzsok, P.; Sieberer, M.; Eiben, C. Neoadjuvant Chemotherapy before Nephroureterectomy in High-Risk Upper Tract Urothelial Cancer: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 4841. [Google Scholar] [CrossRef]
- Wu, J.; Chen, S.; Wu, X.; Mao, W.; Wang, Y.; Xu, B.; Zheng, D.; Chen, M. Trends of incidence and prognosis of upper tract urothelial carcinoma. Bosn. J. Basic. Med. Sci. 2021, 21, 607–619. [Google Scholar] [CrossRef]
- Ng, K.L. The Etiology of Renal Cell Carcinoma and Upper Tract Urothelial Carcinoma. In Urologic Cancers; Barber, N., Ali, A., Eds.; Exon Publications: Brisbane, Australia, 2022. [Google Scholar]
- Roupret, M.; Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Comperat, E.M.; Cowan, N.C.; Dominguez-Escrig, J.L.; Gontero, P.; Hugh Mostafid, A.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur. Urol. 2021, 79, 62–79. [Google Scholar]
- Cowan, N.C. CT urography for hematuria. Nat. Rev. Urol. 2012, 9, 218–226. [Google Scholar] [CrossRef]
- Fiuk, J.V.; Schwartz, B.F. Upper tract urothelial carcinoma: Paradigm shift towards nephron sparing management. World J. Nephrol. 2016, 5, 158–165. [Google Scholar] [CrossRef]
- Baard, J.; de Bruin, D.M.; Zondervan, P.J.; Kamphuis, G.; de la Rosette, J.; Laguna, M.P. Diagnostic dilemmas in patients with upper tract urothelial carcinoma. Nat. Rev. Urol. 2017, 14, 181–191. [Google Scholar] [CrossRef]
- Zhao, Y.; Deng, F.M.; Melamed, J.; Huang, W.C.; Huang, H.; Ren, Q. Diagnostic role of urine cytology and ureteroscopic biopsies in detection of high grade upper tract urothelial carcinoma. Am. J. Clin. Exp. Urol. 2021, 9, 221–228. [Google Scholar]
- Dogan, C.; Pelit, E.S.; Yildirim, A.; Zemheri, I.E.; Canakci, C.; Basok, E.K.; Caskurlu, T. The value of the NMP22 test for superficial bladder cancer diagnosis and follow-up. Turk. J. Urol. 2013, 39, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Freund, J.E.; Liem, E.; Savci-Heijink, C.D.; Baard, J.; Kamphuis, G.M.; de la Rosette, J.; de Bruin, D.M. Confocal laser endomicroscopy for upper tract urothelial carcinoma: Validation of the proposed criteria and proposal of a scoring system for real-time tumor grading. World J. Urol. 2019, 37, 2155–2164. [Google Scholar] [CrossRef] [PubMed]
- Cutress, M.L.; Stewart, G.D.; Zakikhani, P.; Phipps, S.; Thomas, B.G.; Tolley, D.A. Ureteroscopic and percutaneous management of upper tract urothelial carcinoma (UTUC): Systematic review. BJU Int. 2012, 110, 614–628. [Google Scholar] [CrossRef]
- Koll, F.J.; Meisenzahl, E.; Haller, B.; Maisch, P.; Kirchhoff, F.; Horn, T.; Gschwend, J.E.; Schmid, S.C. Evaluation of Pre-operative Biopsy, Surgical Procedures and Oncologic Outcomes in Upper Tract Urothelial Carcinoma (UTUC). Front. Surg. 2021, 8, 790738. [Google Scholar] [CrossRef] [PubMed]
- Raman, J.D.; Scherr, D.S. Management of patients with upper urinary tract transitional cell carcinoma. Nat. Clin. Pract. Urol. 2007, 4, 432–443. [Google Scholar] [CrossRef]
- Audenet, F.; Yates, D.R.; Cussenot, O.; Roupret, M. The role of chemotherapy in the treatment of urothelial cell carcinoma of the upper urinary tract (UUT-UCC). Urol. Oncol. 2013, 31, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Witjes, J.A.; Bruins, H.M.; Cathomas, R.; Comperat, E.M.; Cowan, N.C.; Gakis, G.; Hernandez, V.; Linares Espinos, E.; Lorch, A.; Neuzillet, Y.; et al. European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur. Urol. 2021, 79, 82–104. [Google Scholar] [CrossRef]
- Grossman, H.B.; Natale, R.B.; Tangen, C.M.; Speights, V.O.; Vogelzang, N.J.; Trump, D.L.; de Vere White, R.W.; Sarosdy, M.F.; Wood, D.P., Jr.; Raghavan, D.; et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N. Engl. J. Med. 2003, 349, 859–866. [Google Scholar] [CrossRef]
- Advanced Bladder Cancer Meta-analysis, C. Neoadjuvant chemotherapy in invasive bladder cancer: Update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration. Eur. Urol. 2005, 48, 202–205, discussion 205–206. [Google Scholar]
- Clements, T.; Messer, J.C.; Terrell, J.D.; Herman, M.P.; Ng, C.K.; Scherr, D.S.; Scoll, B.; Boorjian, S.A.; Uzzo, R.G.; Wille, M.; et al. High-grade ureteroscopic biopsy is associated with advanced pathology of upper-tract urothelial carcinoma tumors at definitive surgical resection. J. Endourol. 2012, 26, 398–402. [Google Scholar] [CrossRef]
- Rojas, C.P.; Castle, S.M.; Llanos, C.A.; Santos Cortes, J.A.; Bird, V.; Rodriguez, S.; Reis, I.M.; Zhao, W.; Gomez-Fernandez, C.; Leveillee, R.J.; et al. Low biopsy volume in ureteroscopy does not affect tumor biopsy grading in upper tract urothelial carcinoma. Urol. Oncol. 2013, 31, 1696–1700. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.A.; Matin, S.F.; Busby, J.E.; Dinney, C.P.; Grossman, H.B.; Pettaway, C.A.; Munsell, M.F.; Kamat, A.M. Ability of clinical grade to predict final pathologic stage in upper urinary tract transitional cell carcinoma: Implications for therapy. Urology 2007, 70, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Seisen, T.; Colin, P.; Roupret, M. Risk-adapted strategy for the kidney-sparing management of upper tract tumours. Nat. Rev. Urol. 2015, 12, 155–166. [Google Scholar] [CrossRef]
- Honda, Y.; Nakamura, Y.; Teishima, J.; Goto, K.; Higaki, T.; Narita, K.; Akagi, M.; Terada, H.; Kaichi, Y.; Fujii, S.; et al. Clinical staging of upper urinary tract urothelial carcinoma for T staging: Review and pictorial essay. Int. J. Urol. 2019, 26, 1024–1032. [Google Scholar] [CrossRef]
- D’Andrea, D.; Matin, S.; Black, P.C.; Petros, F.G.; Zargar, H.; Dinney, C.P.; Cookson, M.S.; Kassouf, W.; Dall’Era, M.A.; McGrath, J.S.; et al. Comparative effectiveness of neoadjuvant chemotherapy in bladder and upper urinary tract urothelial carcinoma. BJU Int. 2021, 127, 528–537. [Google Scholar] [CrossRef]
- Siefker-Radtke, A.O.; Dinney, C.P.; Shen, Y.; Williams, D.L.; Kamat, A.M.; Grossman, H.B.; Millikan, R.E. A phase 2 clinical trial of sequential neoadjuvant chemotherapy with ifosfamide, doxorubicin, and gemcitabine followed by cisplatin, gemcitabine, and ifosfamide in locally advanced urothelial cancer: Final results. Cancer 2013, 119, 540–547. [Google Scholar] [CrossRef]
- Leow, J.J.; Chong, Y.L.; Chang, S.L.; Valderrama, B.P.; Powles, T.; Bellmunt, J. Neoadjuvant and Adjuvant Chemotherapy for Upper Tract Urothelial Carcinoma: A 2020 Systematic Review and Meta-analysis, and Future Perspectives on Systemic Therapy. Eur. Urol. 2021, 79, 635–654. [Google Scholar] [CrossRef]
- Margulis, V.; Puligandla, M.; Trabulsi, E.J.; Plimack, E.R.; Kessler, E.R.; Matin, S.F.; Godoy, G.; Alva, A.; Hahn, N.M.; Carducci, M.A.; et al. Phase II Trial of Neoadjuvant Systemic Chemotherapy Followed by Extirpative Surgery in Patients with High Grade Upper Tract Urothelial Carcinoma. J. Urol. 2020, 203, 690–698. [Google Scholar] [CrossRef]
- McConkey, D.J.; Choi, W.; Shen, Y.; Lee, I.L.; Porten, S.; Matin, S.F.; Kamat, A.M.; Corn, P.; Millikan, R.E.; Dinney, C.; et al. A Prognostic Gene Expression Signature in the Molecular Classification of Chemotherapy-naive Urothelial Cancer is Predictive of Clinical Outcomes from Neoadjuvant Chemotherapy: A Phase 2 Trial of Dose-dense Methotrexate, Vinblastine, Doxorubicin, and Cisplatin with Bevacizumab in Urothelial Cancer. Eur. Urol. 2016, 69, 855–862. [Google Scholar]
- Youssef, R.F.; Shariat, S.F.; Lotan, Y.; Wood, C.G.; Sagalowsky, A.I.; Zigeuner, R.; Kikuchi, E.; Weizer, A.; Raman, J.D.; Remzi, M.; et al. Upper urinary tract urothelial carcinoma with loco-regional nodal metastases: Insights from the Upper Tract Urothelial Carcinoma Collaboration. BJU Int. 2011, 108, 1286–1291. [Google Scholar] [CrossRef]
- Meng, X.; Chao, B.; Vijay, V.; Silver, H.; Margolin, E.J.; Balar, A.; Taneja, S.S.; Shah, O.; Bjurlin, M.A.; Anderson, C.B.; et al. High Response Rates to Neoadjuvant Chemotherapy in High-Grade Upper Tract Urothelial Carcinoma. Urology 2019, 129, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Coleman, J.A.; Yip, W.; Wong, N.C.; Sjoberg, D.D.; Bochner, B.H.; Dalbagni, G.; Donat, S.M.; Herr, H.W.; Cha, E.K.; Donahue, T.F.; et al. Multicenter Phase II Clinical Trial of Gemcitabine and Cisplatin as Neoadjuvant Chemotherapy for Patients With High-Grade Upper Tract Urothelial Carcinoma. J. Clin. Oncol. 2023, 41, 1618–1625. [Google Scholar] [CrossRef] [PubMed]
- Birtle, A.; Johnson, M.; Chester, J.; Jones, R.; Dolling, D.; Bryan, R.T.; Harris, C.; Winterbottom, A.; Blacker, A.; Catto, J.W.F.; et al. Adjuvant chemotherapy in upper tract urothelial carcinoma (the POUT trial): A phase 3, open-label, randomised controlled trial. Lancet 2020, 395, 1268–1277. [Google Scholar] [CrossRef]
- Adibi, M.; McCormick, B.; Economides, M.P.; Petros, F.; Xiao, L.; Guo, C.; Shah, A.; Kamat, A.M.; Dinney, C.; Navai, N.; et al. Five and Ten-Year Outcomes of Neoadjuvant Chemotherapy and Surgery for High-Risk Upper Tract Urothelial Carcinoma. Clin. Genitourin. Cancer 2022, 20, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Necchi, A.; Martini, A.; Raggi, D.; Cucchiara, V.; Colecchia, M.; Luciano, R.; Villa, L.; Mazzone, E.; Basile, G.; Scuderi, S.; et al. A feasibility study of preoperative pembrolizumab before radical nephroureterectomy in patients with high-risk, upper tract urothelial carcinoma: PURE-02. Urol. Oncol. 2022, 40, 10.e11–10.e16. [Google Scholar] [CrossRef] [PubMed]
- Teo, M.; Guercio, B.; Pietzak, E.J. Neoadjuvant nivolumab (N) + ipilimumab (I) in cisplatin-ineligible patients with upper tract urothelial cancer (UTUC). J. Clin. Oncol. 2023, 41, 511. [Google Scholar] [CrossRef]
- Szabados, B.; Kockx, M.; Assaf, Z.J.; van Dam, P.J.; Rodriguez-Vida, A.; Duran, I.; Crabb, S.J.; Van Der Heijden, M.S.; Pous, A.F.; Gravis, G.; et al. Final Results of Neoadjuvant Atezolizumab in Cisplatin-ineligible Patients with Muscle-invasive Urothelial Cancer of the Bladder. Eur. Urol. 2022, 82, 212–222. [Google Scholar] [CrossRef]
- Gao, J.; Navai, N.; Alhalabi, O.; Siefker-Radtke, A.; Campbell, M.T.; Tidwell, R.S.; Guo, C.C.; Kamat, A.M.; Matin, S.F.; Araujo, J.C.; et al. Neoadjuvant PD-L1 plus CTLA-4 blockade in patients with cisplatin-ineligible operable high-risk urothelial carcinoma. Nat. Med. 2020, 26, 1845–1851. [Google Scholar] [CrossRef]
- National Cancer Institute. Testing the Addition of MEDI4736 (Durvalumab) to Chemotherapy Before Surgery for Patients with High-Grade Upper Urinary Tract Cancer. ClinicalTrials.gov Identifier: NCT04628767. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT04628767 (accessed on 26 June 2023).
- Centre Hospitalier Universitaire de Nīmes. Safety & Efficacy of Durvalumab+Neoadjuvant Chemotherapy for High-Risk Urothelial Carcinoma of the Upper Urinary Tract (iNDUCT). ClinicalTrials.gov Identifier: NCT04617756. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT04617756 (accessed on 25 June 2023).
- Bajorin, D.F.; Witjes, J.A.; Gschwend, J.E.; Schenker, M.; Valderrama, B.P.; Tomita, Y.; Bamias, A.; Lebret, T.; Shariat, S.F.; Park, S.H.; et al. Adjuvant Nivolumab versus Placebo in Muscle-Invasive Urothelial Carcinoma. N. Engl. J. Med. 2021, 384, 2102–2114. [Google Scholar] [CrossRef]
- Bellmunt, J.; Hussain, M.; Gschwend, J.E.; Albers, P.; Oudard, S.; Castellano, D.; Daneshmand, S.; Nishiyama, H.; Majchrowicz, M.; Degaonkar, V.; et al. Adjuvant atezolizumab versus observation in muscle-invasive urothelial carcinoma (IMvigor010): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2021, 22, 525–537. [Google Scholar] [CrossRef]
- Apolo, A.B. ASCO GU 2019: Pembrolizumab in Muscle-Invasive and Locally Advanced Urothelial Carcinoma—AMBASSADOR versus Observation. 2019. Available online: urotoday.com (accessed on 5 August 2023).
- Knowles, M.A.; Hurst, C.D. Molecular biology of bladder cancer: New insights into pathogenesis and clinical diversity. Nat. Rev. Cancer 2015, 15, 25–41. [Google Scholar] [CrossRef] [PubMed]
- Loriot, Y.; Necchi, A.; Park, S.H.; Garcia-Donas, J.; Huddart, R.; Burgess, E.; Fleming, M.; Rezazadeh, A.; Mellado, B.; Varlamov, S.; et al. Erdafitinib in Locally Advanced or Metastatic Urothelial Carcinoma. N. Engl. J. Med. 2019, 381, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Lyou, Y.; Rosenberg, J.E.; Hoffman-Censits, J.; Quinn, D.I.; Petrylak, D.; Galsky, M.; Vaishampayan, U.; De Giorgi, U.; Gupta, S.; Burris, H.; et al. Infigratinib in Early-Line and Salvage Therapy for FGFR3-Altered Metastatic Urothelial Carcinoma. Clin. Genitourin. Cancer 2022, 20, 35–42. [Google Scholar] [CrossRef]
- Iwata, T.; Kimura, S.; Abufaraj, M.; Janisch, F.; Karakiewicz, P.I.; Seebacher, V.; Roupret, M.; Nasu, Y.; Shariat, S.F. The role of adjuvant radiotherapy after surgery for upper and lower urinary tract urothelial carcinoma: A systematic review. Urol. Oncol. 2019, 37, 659–671. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolawa, A.; D’Souza, A.; Tulpule, V. Overview, Diagnosis, and Perioperative Systemic Therapy of Upper Tract Urothelial Carcinoma. Cancers 2023, 15, 4813. https://doi.org/10.3390/cancers15194813
Kolawa A, D’Souza A, Tulpule V. Overview, Diagnosis, and Perioperative Systemic Therapy of Upper Tract Urothelial Carcinoma. Cancers. 2023; 15(19):4813. https://doi.org/10.3390/cancers15194813
Chicago/Turabian StyleKolawa, Adam, Anishka D’Souza, and Varsha Tulpule. 2023. "Overview, Diagnosis, and Perioperative Systemic Therapy of Upper Tract Urothelial Carcinoma" Cancers 15, no. 19: 4813. https://doi.org/10.3390/cancers15194813
APA StyleKolawa, A., D’Souza, A., & Tulpule, V. (2023). Overview, Diagnosis, and Perioperative Systemic Therapy of Upper Tract Urothelial Carcinoma. Cancers, 15(19), 4813. https://doi.org/10.3390/cancers15194813





