Racial Disparities in Breast Cancer Treatments and Adverse Events in the SEER-Medicare Data
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Generation of Database
2.2. Generation of a Patient Cohort That Met Our Selection Criteria
2.3. Statistical Analysis
3. Results
3.1. Distributions of Patient Characteristics
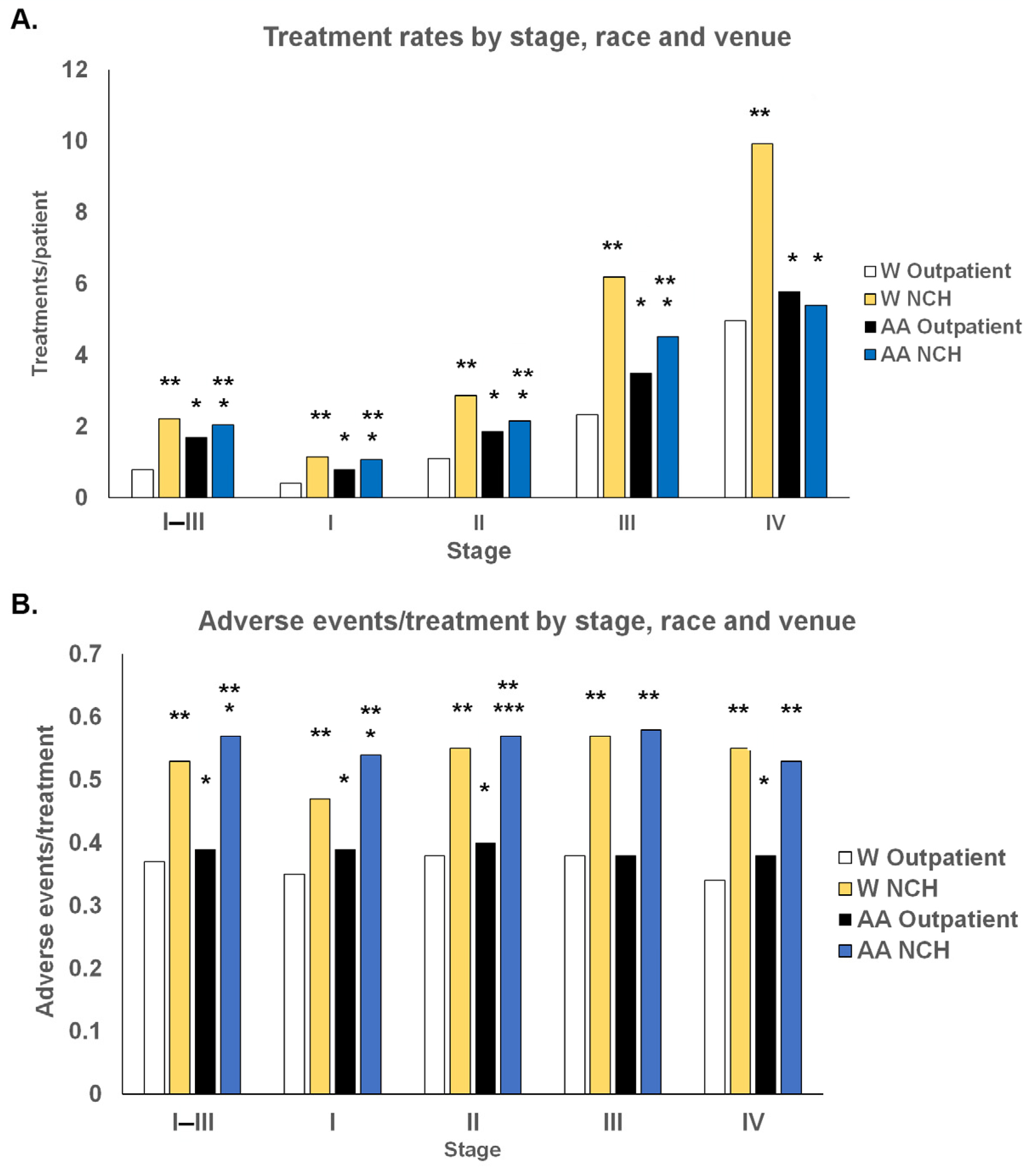
3.2. Treatment and Adverse Events Distributions
3.3. Effects of ER/PR and Her2 Status on Racial Differences in Treatments and AEs
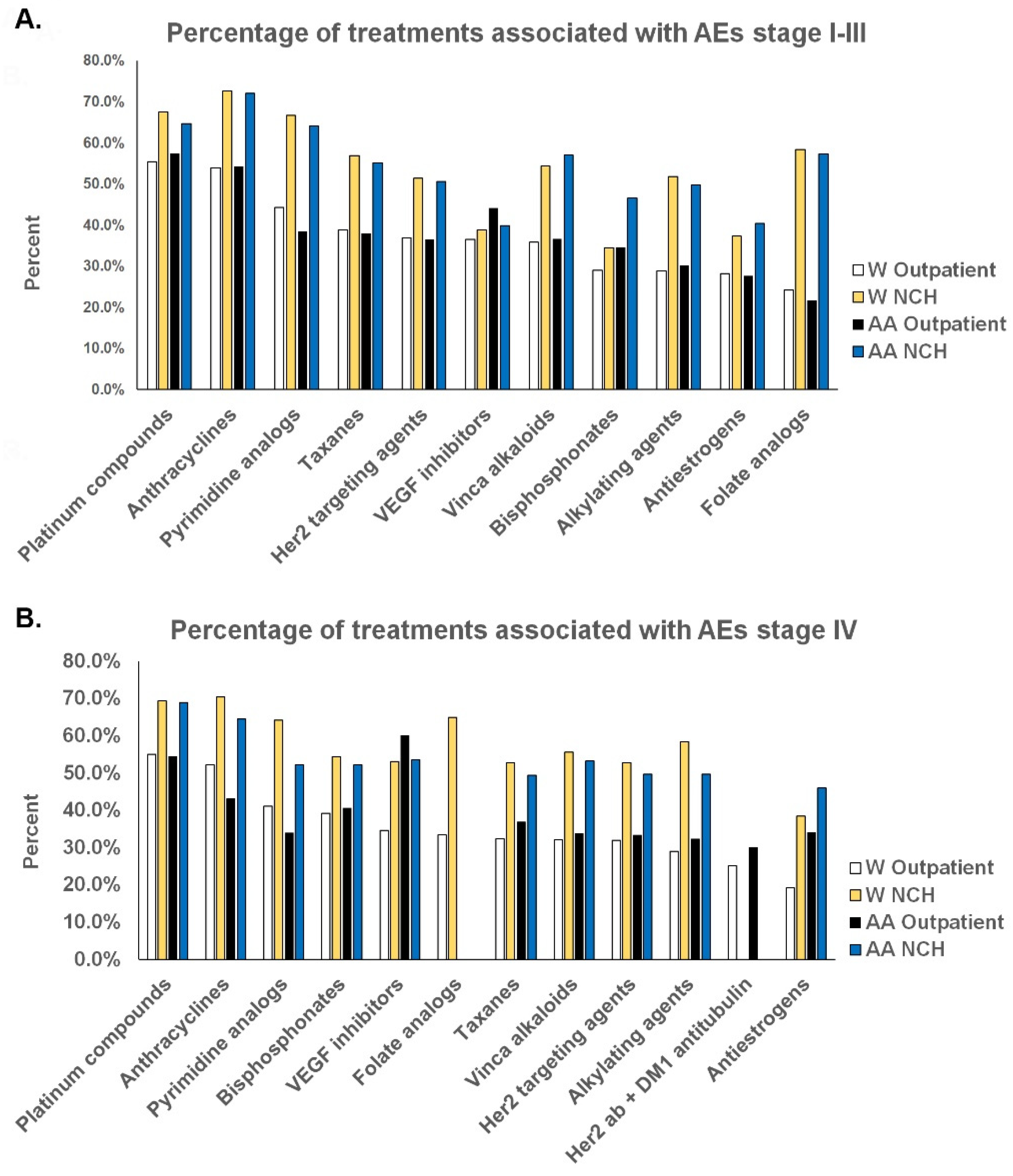
3.4. Treatment Regimens and AEs
3.5. Racial Effects of Treatments and AEs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Inst. Outpt. | PP Office | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stage | All | % in Stage | W | % in Stage | AA | % in Stage | AA/ (W+AA × 100%) | All | % in Stage | W | % in Stage | AA | % in Stage | AA/ (W+AA × 100%) |
| I | 125,391 | 53.1% | 112,023 | 53.9% | 7292 | 42.1% | 6.1% | 129,105 | 53.2% | 115,191 | 54.0% | 7345 | 42.3% | 6.0% |
| II | 71,862 | 30.4% | 62,544 | 30.1% | 5890 | 34.0% | 8.6% | 73,742 | 30.4% | 64,143 | 30.1% | 5924 | 34.1% | 8.5% |
| III | 25,998 | 11.0% | 22,203 | 10.7% | 2675 | 15.4% | 10.8% | 26,603 | 11.0% | 22,758 | 10.7% | 2661 | 15.3% | 10.5% |
| IV | 12,947 | 5.5% | 11,021 | 5.3% | 1483 | 8.6% | 11.9% | 13,148 | 5.4% | 11,261 | 5.3% | 1431 | 8.2% | 11.3% |
| Total | 236,198 | 207,791 | 17,340 | 242,598 | 213,353 | 17,361 | ||||||||
 ), Her2 (
), Her2 ( ) status, and race (
) status, and race ( ) on distribution differences in age, comorbidity index, TR/PT, and AE/TR. The congruence between the Outpatient/NCH and Inst. OP/PP Ofc. datasets (
) on distribution differences in age, comorbidity index, TR/PT, and AE/TR. The congruence between the Outpatient/NCH and Inst. OP/PP Ofc. datasets ( ) was most evident in files that were annotated for ER/PR status and less so in the files annotated for Her2 that had much fewer numbers.
) was most evident in files that were annotated for ER/PR status and less so in the files annotated for Her2 that had much fewer numbers.| W | AA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % ER/PR- | Age | Comb | TR/PT | AE/TR | % ER/PR- | Age | Comb | TR/PT | AE/TR | |
| Stage I–III | ||||||||||
| Inst. Outpt. | ||||||||||
| ER/PR+ | 85.8 | 75.3 ± 7.2 | 3.0 ± 3.1 | 0.6 | 0.40 | 75.8 a | 75.0 ± 7.2 b | 3.5 ± 3.3 b | 0.9 a | 0.39 |
| ER/PR- | 14.2 | 75.0 ± 7.3 d | 2.7 ± 3.1 d | 1.5 c | 0.43 c | 24.4 a | 74.0 ± 7.0 b,d  | 3.1 ± 3.3 b,d  | 2.2 a,c  | 0.43 c  |
| Her2- | 89.3 | 75.0 ± 7.3 | 3.3 ± 3.0 | 0.9 | 0.42 | 87.4 a | 74.6 ± 7.3 b | 3.8 ± 3.2 b | 1.3 a | 0.43 |
| Her2+ | 10.7 | 74.7 ± 7.5 f | 3.4 ± 3.1 f | 4.7 e | 0.40 e | 12.6 a | 74.3 ± 7.1  | 3.6 ± 3.1  | 5.5 a,e  | 0.36 a,e  |
| PP Office | ||||||||||
| ER/PR+ | 85.8 | 75.3 ± 7.2 | 2.7 ± 2.8 h | 1.8 g | 0.52 g | 75.7 a | 75.0 ± 7.2 b  | 3.1 ± 3.0 b,h  | 1.6 a,g  | 0.58 a,g  |
| ER/PR- | 14.2 | 75.0 ± 7.2 d  | 2.4 ± 2.7 d,h  | 4.2 c,g  | 0.60 c,g  | 24.3 a | 74.0 ± 6.9 b,d   | 2.8 ± 3.0 b,d,h   | 3.4 a,c,g   | 0.59 g   |
| Her2- | 89.3 | 74.9 ± 7.3 h | 3.1 ± 2.8 h | 1.6 g | 0.48 g | 87.5 a | 74.6 ± 7.2 b  | 3.6 ± 3.0 b,h  | 1.4 a  | 0.52 a,g  |
| Her2+ | 10.7 | 74.5 ± 7.5 f  | 3.1 ± 2.8 h  | 7.3 e,g  | 0.49 e,g  | 12.5 a | 74.3 ± 7.1   | 3.4 ± 2.9   | 4.5 a,e,g   | 0.46 a,e,g   |
| Stage IV | ||||||||||
| Inst. Outpt. | ||||||||||
| ER/PR+ | 79.4 | 76.1 ± 7.5 | 2.0 ± 2.8 | 3.0 | 0.37 | 68.0 a | 75.1 ± 7.4 b | 2.1 ± 2.9 | 2.9 | 0.39 |
| ER/PR- | 20.6 | 75.8 ± 7.5 | 1.7 ± 2.8 d | 3.0 | 0.37 | 32.0 a | 74.6 ± 6.8 b  | 1.8 ± 2.9  | 2.8  | 0.42 a  |
| Her2- | 80.6 | 75.9 ± 7.8 | 3.1 ± 3.0 | 4.2 | 0.40 | 79.0 | 75.0 ± 7.6 b | 3.2 ± 3.1 | 3.9 | 0.42 |
| Her2+ | 19.4 | 75.3 ± 7.7 | 3.1 ± 3.1 | 8.4 e | 0.32 e | 21.0 | 74.6 ± 7.6  | 3.1 ± 3.2  | 4.0 a  | 0.25 a,e  |
| PP Office | ||||||||||
| ER/PR+ | 79.2 | 76.2 ± 7.5 | 1.8 ± 2.6 h | 6.4 g | 0.57 g | 68.1 a | 75.2 ± 7.4 b  | 2.0 ± 2.7  | 4.7 a,g  | 0.59 g  |
| ER/PR- | 20.8 | 75.9 ± 7.5  | 1.6 ± 2.6 d  | 7.7 c,g  | 0.6 c,g  | 31.9 a | 75.2 ± 6.8   | 1.6 ± 2.7 d   | 4.3 a,g   | 0.64 g   |
| Her2- | 80.4 | 76.0 ± 7.8 | 2.8 ± 2.8 h | 3.9 g | 0.51 g | 78.7 | 75.2 ± 7.5  | 3.1 ± 2.9  | 3.9  | 0.55 g  |
| Her2+ | 19.6 | 75.3 ± 7.7 f  | 2.8 ± 2.9  | 12.8 e,g  | 0.54 e,g  | 21.3 | 74.8 ± 7.8   | 2.8 ± 2.8   | 3.3 a   | 0.38 a,e,g   |
 /No
/No  ), ER/PR effect (Yes
), ER/PR effect (Yes  /No
/No  ), Her2 effect (Yes
), Her2 effect (Yes  /No
/No  ), and venue effect (Yes
), and venue effect (Yes  /No
/No  ).
).References
- Polite, B.N.; Cirrincione, C.; Fleming, G.F.; Berry, D.A.; Seidman, A.; Muss, H.; Norton, L.; Shapiro, C.; Bakri, K.; Marcom, K.; et al. Racial differences in clinical outcomes from metastatic breast cancer: A pooled analysis of CALGB 9342 and 9840—Cancer and Leukemia Group B. J. Clin. Oncol. 2008, 26, 2659–2665. [Google Scholar] [CrossRef]
- Silber, J.H.; Rosenbaum, P.R.; Clark, A.S.; Giantonio, B.J.; Ross, R.N.; Teng, Y.; Wang, M.; Niknam, B.A.; Ludwig, J.M.; Wang, W.; et al. Characteristics associated with differences in survival among black and white women with breast cancer. JAMA 2013, 310, 389–397. [Google Scholar] [CrossRef]
- Wieder, R.; Shafiq, B.; Adam, N. African American race is an independent risk factor in survival form initially diagnosed localized breast cancer. J. Cancer 2016, 7, 1587–1598. [Google Scholar] [CrossRef][Green Version]
- Lovejoy, L.A.; Shriver, C.D.; Haricharan, S.; Ellsworth, R.E. Survival disparities in us black compared to white women with hormone receptor positive-Her2 negative breast cancer. Int. J. Environ. Res. Public Health 2023, 20, 2903. [Google Scholar] [CrossRef]
- Daly, B.; Olopade, O.I. A perfect storm: How tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J. Clin. 2015, 65, 221–238. [Google Scholar] [CrossRef]
- Roberts, M.C.; Wheeler, S.B.; Reeder-Hayes, K. Racial/ethnic and socioeconomic disparities in endocrine therapy adherence in breast cancer: A systematic review. Am. J. Public Health 2015, 105 (Suppl. S3), e4–e15. [Google Scholar] [CrossRef]
- Dietze, E.C.; Sistrunk, C.; Miranda-Carboni, G.; O’Regan, R.; Seewaldt, V.L. Triple-negative breast cancer in african-american women: Disparities versus biology. Nat. Rev. Cancer 2015, 15, 248–254. [Google Scholar] [CrossRef]
- Keenan, T.; Moy, B.; Mroz, E.A.; Ross, K.; Niemierko, A.; Rocco, J.W.; Isakoff, S.; Ellisen, L.W.; Bardia, A. Comparison of the genomic landscape between primary breast cancer in African American versus White women and the association of racial differences with tumor recurrence. J. Clin. Oncol. 2015, 33, 3621–3627. [Google Scholar] [CrossRef]
- Nalwoga, H.; Ahmed, L.; Arnes, J.B.; Wabinga, H.; Akslen, L.A. Strong expression of Hypoxia-Inducible Factor-1alpha (HIF-1alpha) is associated with Axl expression and features of aggressive tumors in African breast cancer. PLoS ONE 2016, 11, e0146823. [Google Scholar] [CrossRef]
- Sugita, B.; Gill, M.; Mahajan, A.; Duttargi, A.; Kirolikar, S.; Almeida, R.; Regis, K.; Oluwasanmi, O.L.; Marchi, F.; Marian, C.; et al. Differentially expressed miRNAs in triple negative breast cancer between African-American and non-Hispanic White women. Oncotarget 2016, 7, 79274–79291. [Google Scholar] [CrossRef]
- Field, L.A.; Love, B.; Deyarmin, B.; Hooke, J.A.; Shriver, C.D.; Ellsworth, R.E. Identification of differentially expressed genes in breast tumors from African American compared with Caucasian women. Cancer 2011, 118, 1334–1344. [Google Scholar] [CrossRef] [PubMed]
- Pollard, J.; Burns, P.A.; Hughes, T.A.; Ho-Yen, C.; Jones, J.L.; Mukherjee, G.; Omoniyi-Esan, G.O.; Titloye, N.A.; Speirs, V.; Shaaban, A.M. Differential expression of micrornas in breast cancers from four different ethnicities. Pathobiology 2018, 85, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Jiagge, E.; Chitale, D.; Newman, L.A. Triple-negative breast cancer, stem cells, and african ancestry. Am. J. Pathol. 2018, 188, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Telonis, A.G.; Rigoutsos, I. Race disparities in the contribution of mirna isoforms and trna-derived fragments to triple-negative breast cancer. Cancer Res. 2018, 78, 1140–1154. [Google Scholar] [CrossRef]
- Davis, M.; Martini, R.; Newman, L.; Elemento, O.; White, J.; Verma, A.; Datta, I.; Adrianto, I.; Chen, Y.; Gardner, K.; et al. Identification of distinct heterogenic subtypes and molecular signatures associated with African ancestry in triple negative breast cancer using quantified genetic ancestry models in admixed race populations. Cancers 2020, 12, 1220. [Google Scholar] [CrossRef]
- Xing, F.; Zhao, D.; Wu, S.Y.; Tyagi, A.; Wu, K.; Sharma, S.; Liu, Y.; Deshpande, R.; Wang, Y.; Cleary, J.; et al. Epigenetic and posttranscriptional modulation of sos1 can promote breast cancer metastasis through obesity-activated c-met signaling in african-american women. Cancer Res. 2021, 81, 3008–3021. [Google Scholar] [CrossRef] [PubMed]
- Martini, R.; Delpe, P.; Chu, T.R.; Arora, K.; Lord, B.; Verma, A.; Bedi, D.; Karanam, B.; Elhussin, I.; Chen, Y.; et al. African ancestry-associated gene expression profiles in triple-negative breast cancer underlie altered tumor biology and clinical outcome in women of African descent. Cancer Discov. 2022, 12, 2530–2551. [Google Scholar] [CrossRef]
- Joshi, S.; Garlapati, C.; Aneja, R. Epigenetic determinants of racial disparity in breast cancer: Looking beyond genetic alterations. Cancers 2022, 14, 1903. [Google Scholar] [CrossRef]
- Wieder, R. Fibroblasts as turned agents in cancer progression. Cancers 2023, 15, 2014. [Google Scholar] [CrossRef]
- Zhang, H.; Barner, J.C.; Moczygemba, L.R.; Rascati, K.L.; Park, C.; Kodali, D. Comparing survival outcomes between neoadjuvant and adjuvant chemotherapy within breast cancer subtypes and stages among older women: A SEER-Medicare analysis. Breast Cancer 2023, 30, 489–496. [Google Scholar] [CrossRef]
- Wright, N.; Rida, P.C.G.; Aneja, R. Tackling intra- and inter-tumor heterogeneity to combat triple negative breast cancer. Front. Biosci. 2017, 22, 1549–1580. [Google Scholar]
- Davis, M.B.; Newman, L.A. Breast cancer disparities: How can we leverage genomics to improve outcomes? Surg. Oncol. Clin. N. Am. 2018, 27, 217–234. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.J.; Minas, T.Z.; Ambs, S. Analysis of tumor biology to advance cancer health disparity research. Am. J. Pathol. 2018, 188, 304–316. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Haque, I.; Chakraborty, J.; Graff, S.; Banerjee, S.; Banerjee, S.K. Racial disparity in breast cancer: Can it be mattered for prognosis and therapy. J. Cell Commun. Signal. 2018, 12, 119–132. [Google Scholar] [CrossRef]
- Wright, N.; Akinyemiju, T.; Subhedar, P.; Rida, P.; Aneja, R. Targeting risk factors for reducing the racially disparate burden in breast cancer. Front. Biosci. 2019, 11, 136–160. [Google Scholar]
- Freedman, R.A.; He, Y.; Winer, E.P.; Keating, N.L. Racial/ethnic differences in receipt of timely adjuvant therapy for older women with breast cancer: Are delays influenced by the hospitals where patients obtain surgical care? Health Serv. Res. 2013, 48, 1669–1683. [Google Scholar] [CrossRef]
- Jain, U.; Jain, B.; Fayanju, O.M.; Chino, F.; Dee, E.C. Disparities in timely treatment among young women with breast cancer. Am. J. Surg. 2022, 224, 811–815. [Google Scholar] [CrossRef]
- Babatunde, O.A.; Eberth, J.M.; Felder, T.M.; Moran, R.; Hughes-Halbert, C.; Truman, S.; Hebert, J.R.; Heiney, S.; Adams, S.A. Racial disparities and diagnosis-to-treatment time among patients diagnosed with breast cancer in South Carolina. J. Racial Ethn. Health Dispar. 2022, 9, 124–134. [Google Scholar] [CrossRef]
- Smith, K.; Wray, L.; Klein-Cabral, M.; Schuchter, L.; Fox, K.; Glick, J.; DeMichele, A. Ethnic disparities in adjuvant chemotherapy for breast cancer are not caused by excess toxicity in black patients. Clin. Breast Cancer 2005, 6, 260–266; discussion 267–269. [Google Scholar] [CrossRef]
- Knisely, A.T.; Michaels, A.D.; Mehaffey, J.H.; Hassinger, T.E.; Krebs, E.D.; Brenin, D.R.; Schroen, A.T.; Showalter, S.L. Race is associated with completion of neoadjuvant chemotherapy for breast cancer. Surgery 2018, 164, 195–200. [Google Scholar] [CrossRef]
- Nugent, B.D.; Ren, D.; Bender, C.M.; Rosenzweig, M. The impact of age and adjuvant chemotherapy modifications on survival among black women with breast cancer. Clin. Breast Cancer 2019, 19, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Stabellini, N.; Cullen, J.; Cao, L.; Shanahan, J.; Hamerschlak, N.; Waite, K.; Barnholtz-Sloan, J.S.; Montero, A.J. Racial disparities in breast cancer treatment patterns and treatment related adverse events. Sci. Rep. 2023, 13, 1233. [Google Scholar] [CrossRef] [PubMed]
- DeLancey, J.O.; Thun, M.J.; Jemal, A.; Ward, E.M. Recent trends in black-white disparities in cancer mortality. Cancer Epidemiol. Biomark. Prev. 2008, 17, 2908–2912. [Google Scholar] [CrossRef] [PubMed]
- Wieder, R.; Shafiq, B.; Adam, N. Greater Survival Improvement in African American vs. Caucasian Women with Hormone Negative Breast Cancer. J. Cancer 2020, 11, 2808–2820. [Google Scholar] [CrossRef]
- Russo, A.; Autelitano, M.; Bisanti, L. Re: Frequency and cost of chemotherapy-related serious adverse effects in a population sample of women with breast cancer. J. Natl. Cancer Inst. 2006, 98, 1826–1827. [Google Scholar] [CrossRef]
- Rosenzweig, M.Q.; Mazanec, S.R. Racial differences in breast cancer therapeutic toxicity: Implications for practice. Cancer Epidemiol. Biomark. Prev. 2023, 32, 157–158. [Google Scholar] [CrossRef]
- Nyrop, K.A.; Damone, E.M.; Deal, A.M.; Wheeler, S.B.; Charlot, M.; Reeve, B.B.; Basch, E.; Shachar, S.S.; Carey, L.A.; Reeder-Hayes, K.E.; et al. Patient-reported treatment toxicity and adverse events in Black and White women receiving chemotherapy for early breast cancer. Breast Cancer Res. Treatment. 2022, 191, 409–422. [Google Scholar] [CrossRef]
- Simon, N.B.; Danso, M.A.; Alberico, T.A.; Basch, E.; Bennett, A.V. The prevalence and pattern of chemotherapy-induced peripheral neuropathy among women with breast cancer receiving care in a large community oncology practice. Qual. Life Res. 2017, 26, 2763–2772. [Google Scholar] [CrossRef]
- Aldrich, J.; Ekpo, P.; Rupji, M.; Switchenko, J.M.; Torres, M.A.; Kalinsky, K.; Bhave, M.A. Racial disparities in clinical outcomes on investigator-initiated breast cancer clinical trials at an urban medical center. Clin. Breast Cancer 2023, 23, 38–44. [Google Scholar] [CrossRef]
- Han, H.S.; Reis, I.M.; Zhao, W.; Kuroi, K.; Toi, M.; Suzuki, E.; Syme, R.; Chow, L.; Yip, A.Y.; Gluck, S. Racial differences in acute toxicities of neoadjuvant or adjuvant chemotherapy in patients with early-stage breast cancer. Eur. J. Cancer 2011, 47, 2537–2545. [Google Scholar] [CrossRef]
- Reynolds, C.H.; Patel, J.D.; Garon, E.B.; Olsen, M.R.; Bonomi, P.; Govindan, R.; Pennella, E.J.; Liu, J.; Guba, S.C.; Li, S.; et al. Exploratory subset analysis of African Americans from the pointbreak study: Pemetrexed-carboplatin-bevacizumab followed by maintenance pemetrexed-bevacizumab versus paclitaxel-carboplatin-bevacizumab followed by maintenance bevacizumab in patients with stage IIIb/IV nonsquamous non-small-cell lung cancer. Clin. Lung Cancer 2015, 16, 200–208. [Google Scholar] [PubMed]
- Enewold, L.; Parsons, H.; Zhao, L.; Bott, D.; Rivera, D.R.; Barrett, M.J.; Virnig, B.A.; Warren, J.L. Updated overview of the SEER-Medicare data: Enhanced content and applications. JNCI Monogr. 2020, 2020, 3–13. [Google Scholar]
- Sarfati, D.; Gurney, J.; Stanley, J.; Salmond, C.; Crampton, P.; Dennett, E.; Koea, J.; Pearce, N. Cancer-specific administrative data–based comorbidity indices provided valid alternative to Charlson and National Cancer Institute Indices. J. Clin. Epidemiol. 2014, 67, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.; Murphy, C.C.; Pruitt, S.L.; Rashdan, S.; Rahimi, A.; Gerber, D.E. Potential impact of revised NCI eligibility criteria guidance: Prior malignancy exclusion in breast cancer clinical trials. J. Natl. Compr. Canc. Netw. 2022, 20, 792–799. [Google Scholar] [CrossRef]
- Du, X.L.; Osborne, C.; Goodwin, J.S. Population-based assessment of hospitalizations for toxicity from chemotherapy in older women with breast cancer. J. Clin. Oncol. 2002, 20, 4636–4642. [Google Scholar] [CrossRef]
- Hassett, M.J.; O’Malley, A.J.; Pakes, J.R.; Newhouse, J.P.; Earle, C.C. Frequency and cost of chemotherapy-related serious adverse effects in a population sample of women with breast cancer. J. Natl. Cancer Inst. 2006, 98, 1108–1117. [Google Scholar] [CrossRef]
- Rashid, N.; Koh, H.A.; Baca, H.C.; Li, Z.; Malecha, S.; Abidoye, O.; Masaquel, A. Clinical impact of chemotherapy-related adverse events in patients with metastatic breast cancer in an integrated health care system. J. Managed Care Spec. Pharm. 2015, 21, 863–871. [Google Scholar] [CrossRef]
- Kawasumi, K.; Kujirai, A.; Matsui, R.; Kawano, Y.; Yamaguchi, M.; Aoyama, T. Survey of serious adverse events and safety evaluation of oral anticancer drug treatment in Japan: A retrospective study. Mol. Clin. Oncol. 2021, 14, 12. [Google Scholar] [CrossRef]
- Kuter, D.J. Treatment of chemotherapy-induced thrombocytopenia in patients with non-hematologic malignancies. Haematologica 2022, 107, 1243–1263. [Google Scholar] [CrossRef]
- Ingrand, I.; Defossez, G.; Lafay-Chebassier, C.; Chavant, F.; Ferru, A.; Ingrand, P.; Pérault-Pochat, M.C. Serious adverse effects occurring after chemotherapy: A general cancer registry-based incidence survey. Br. J. Clin. Pharmacol. 2020, 86, 711–722. [Google Scholar] [CrossRef]
- Ghasemi, A.; Zahediasl, S. Normality tests for statistical analysis: A guide for non-statisticians. Int. J. Endocrinol. Metab. 2012, 10, 486–489. [Google Scholar] [CrossRef] [PubMed]
- Hershman, D.; Weinberg, M.; Rosner, Z.; Alexis, K.; Tiersten, A.; Grann, V.R.; Troxel, A.; Neugut, A.I. Ethnic neutropenia and treatment delay in african american women undergoing chemotherapy for early-stage breast cancer. J. Natl. Cancer Inst. 2003, 95, 1545–1548. [Google Scholar] [CrossRef] [PubMed]
- Jemal, A.; Robbins, A.S.; Lin, C.C.; Flanders, W.D.; DeSantis, C.E.; Ward, E.M.; Freedman, R.A. Factors that contributed to black-white disparities in survival among nonelderly women with breast cancer between 2004 and 2013. J. Clin. Oncol. 2018, 36, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Doose, M.; Steinberg, M.B.; Xing, C.Y.; Lin, Y.; Cantor, J.C.; Hong, C.C.; Demissie, K.; Bandera, E.V.; Tsui, J. Comorbidity management in black women diagnosed with breast cancer: The role of primary care in shared care. J. Gen. Intern. Med. 2021, 36, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Doose, M.; Sanchez, J.I.; Cantor, J.C.; Plascak, J.J.; Steinberg, M.B.; Hong, C.C.; Demissie, K.; Bandera, E.V.; Tsui, J. Fragmentation of care among black women with breast cancer and comorbidities: The role of health systems. JCO Oncol. Pract. 2021, 17, e637–e644. [Google Scholar] [CrossRef] [PubMed]
- Wallner, L.P.; Chen, L.H.; Hogan, T.A.; Brasfield, F.M.; Haque, R. The influence of medical comorbidities on survival disparities in a multiethnic group of patients with de novo metastatic breast cancer. Cancer Epidemiol. Biomark. Prev. 2022, 31, 1935–1943. [Google Scholar] [CrossRef]
- Shariff-Marco, S.; Ellis, L.; Yang, J.; Koo, J.; John, E.M.; Keegan, T.H.M.; Cheng, I.; Monroe, K.R.; Vigen, C.; Kwan, M.L.; et al. Hospital characteristics and breast cancer survival in the california breast cancer survivorship consortium. JCO Oncol. Pract. 2020, 16, e517–e528. [Google Scholar] [CrossRef]
- Song, J.H.; Kantor, O.; Mittendorf, E.A.; King, T.A.; Minami, C.A. Race and site of care impact treatment delays in older women with non-metastatic breast cancer. Ann. Surg. Oncol. 2022, 29, 4103–4114. [Google Scholar] [CrossRef]
- Goel, N.; Hernandez, A.; Thompson, C.; Choi, S.; Westrick, A.; Stoler, J.; Antoni, M.H.; Rojas, K.; Kesmodel, S.; Figueroa, M.E.; et al. Neighborhood disadvantage and breast cancer-specific survival. JAMA Netw. Open 2023, 6, e238908. [Google Scholar] [CrossRef]
- Jung, J.; Feldman, R.; Kalidindi, Y. The impact of integration on outpatient chemotherapy use and spending in Medicare. Health Econ. 2019, 28, 517–528. [Google Scholar] [CrossRef]
- Fisher, M.D.; Punekar, R.; Yim, Y.M.; Small, A.; Singer, J.R.; Schukman, J.; McAneny, B.L.; Luthra, R.; Malin, J. Differences in health care use and costs among patients with cancer receiving intravenous chemotherapy in physician offices versus in hospital outpatient settings. J. Oncol. Pract. 2017, 13, e37–e46. [Google Scholar] [CrossRef] [PubMed]
| Stage | AA + W PTs | % in Stage | Outpatient | NCH | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| W | % in Stage | AA | % in Stage | AA/(W + AA) × 100% | W | % in Stage | AA | % in Stage | AA/(W + AA) × 100% | |||
| I | 275,428 | 54.0 | 117,716 | 55.5 | 10,819 | 41.7 | 8.4 | 134,616 | 55.5 | 12,277 | 42.0 | 8.4 |
| II | 163,589 | 32.1 | 66,410 | 31.3 | 9949 | 38.3 | 13.0 | 76,118 | 31.4 | 11,112 | 38.0 | 12.7 |
| III | 53,486 | 10.5 | 21,202 | 10.0 | 3896 | 15.0 | 15.5 | 24,034 | 9.9 | 4354 | 14.9 | 15.3 |
| IV | 17,650 | 3.5 | 6947 | 3.3 | 1293 | 5.0 | 15.7 | 7942 | 3.3 | 1468 | 5.0 | 15.6 |
| Total | 510,153 | 212,275 | 25,957 | 242,710 | 29,211 | |||||||
| Outpatient | NCH | |||||||
|---|---|---|---|---|---|---|---|---|
| Age ± SD | Comorb. Index ± SD | Age + SD | Comorb. Index ± SD | |||||
| Stage | W | AA | W | AA | W | AA | W | AA |
| I–III | 68.0 ± 10.8 | 64.6 ± 12.3 1 | 4.2 ± 2.8 | 4.5 ± 2.9 1 | 67.8 ± 10.8 | 64.6 ± 12.2 1 | 3.6 ± 2.7 4 | 4.0 ± 2.9 1,4 |
| I | 68.4 + 10.0 | 66.0 + 10.9 1 | 4.2 + 2.7 | 4.5 + 2.9 1 | 68.2 + 10.1 | 66.0 + 10.8 1 | 3.6 + 2.6 4 | 4.1 + 2.8 1,4 |
| II | 67.7 + 11.4 | 63.9 + 13.0 1 | 4.2 + 2.8 | 4.5 + 3.0 1 | 67.5 + 11.4 | 63.9 + 12.8 1 | 3.7 + 2.7 4 | 4.1 + 2.9 1,4 |
| III | 66.5 + 12.2 | 62.2 + 13.9 1 | 4.1 + 2.8 | 4.2 + 3.0 2 | 66.4 + 12.2 | 62.3 + 13.8 1 | 3.6 + 2.7 4 | 3.9 + 2.9 1,4 |
| IV | 69.4 + 12.1 | 65.3 + 13.3 1 | 3.8 + 2.8 | 4.0 + 2.9 3 | 69.5 + 12.0 | 65.6 + 13.1 1 | 3.5 + 2.7 4 | 3.7 + 2.8 1,4 |
| % | Age ± SD | Comb. Index ± SD | TR/PT | AE/TR | % | Age ± SD | Comb. Index ± SD | TR/PT | AE/TR | |
|---|---|---|---|---|---|---|---|---|---|---|
| W | AA | |||||||||
| Stage I–III | ||||||||||
| Outpatient | ||||||||||
| ER/PR+ | 84.6% | 68.6 ± 10.5 | 4.2 ± 2.8 | 0.75 | 0.37 | 71.1% a | 65.9 ± 12.1 b | 4.5 ± 2.9 b | 1.40 a | 0.38 |
| ER/PR- | 15.4% | 65.8 ± 11.4 d | 4.0 ± 2.8 d | 1.56 c | 0.40 c | 28.9% a | 61.8 ± 12.3 b,d | 4.2 ± 2.9 b,d | 2.45 a,c | 0.41 c |
| Her2- | 88.3% | 71.8 ± 9.2 | 4.1 ± 2.8 | 0.92 | 0.40 | 85.3% a | 68.0 ± 11.4 b | 4.4 ± 3.0 b | 1.69 a | 0.41 |
| Her2+ | 11.7% | 70.2 ± 10.2 f | 4.0 ± 2.9 f | 4.31 e | 0.38 e | 14.7% a | 65.4 ± 12.1 b,f | 4.1 ± 3.0 f | 5.51 a,e | 0.38 e |
| NCH | ||||||||||
| ER/PR+ | 84.6% | 68.4 ± 10.5 h | 3.6 ± 2.7 h | 1.96 g | 0.52 g | 71.2% a | 65.9 ± 11.9 b | 4.1 ± 2.9 b,h | 1.70 a,g | 0.56 a,g |
| ER/PR- | 15.4% | 65.6 ± 11.4 d,h | 3.5 ± 2.6 d,h | 3.84 c,g | 0.57 c,g | 28.8% a | 61.9 ± 12.2 b,d | 3.9 ± 2.8 b,d,h | 2.85 a,c,g | 0.57 g |
| Her2- | 88.4% | 71.7 ± 9.1 | 3.6 ± 2.7 h | 1.54 g | 0.50 g | 85.5% a | 68.0 ± 11.2 b | 4.0 ± 3.0 b,h | 1.37 a,g | 0.53 a,g |
| Her2+ | 11.6% | 70.2 ± 10.0 f | 3.5 ± 2.8 f,h | 6.57 e,g | 0.49 g | 14.5% a | 65.7 ± 11.8 b,f | 3.8 ± 2.9 b,f,h | 3.70 a,e,g | 0.45 a,e,g |
| Stage IV | ||||||||||
| Outpatient | ||||||||||
| ER/PR+ | 81.6% | 69.3 ± 12.0 | 3.8 ± 2.8 | 5.09 | 0.34 | 72.3% a | 65.1 ± 13.6 b | 3.9 ± 2.9 | 6.08 a | 0.40 a |
| ER/PR- | 18.4% | 68.6 ± 12.3 | 3.8 ± 3.0 | 5.48 c | 0.35 | 27.7% a | 65.2 ± 13.1 b | 4.2 ± 3.1 b | 6.85 a | 0.34 c |
| Her2- | 77.3% | 71.4 ± 11.0 | 4.0 ± 2.9 | 4.43 | 0.38 | 73.7% a | 68.0 ± 12.2 b | 4.3 ± 3.1 b | 4.55 | 0.42 a |
| Her2+ | 22.7% | 68.3 ± 12.4 f | 3.6 ± 2.9 f | 8.52 e | 0.28 e | 26.3% a | 63.4 ± 14.0 b,f | 3.5 ± 2.7 f | 8.38 e | 0.29 e |
| NCH | ||||||||||
| ER/PR+ | 81.6% | 69.5 ± 11.9 | 3.4 ± 2.7 h | 9.79 g | 0.56 g | 72.7% a | 65.4 ± 13.3 | 3.5 ± 2.8 h | 5.31 a,g | 0.52 a,g |
| ER/PR- | 18.4% | 69.0 ± 12.1 | 3.5 ± 2.8 h | 10.92 c,g | 0.55 g | 27.3% a | 65.6 ± 12.8 b | 3.9 ± 2.9 b,d | 6.43 a,c | 0.54 g |
| Her2- | 77.9% | 71.6 ± 10.9 | 3.5 ± 2.8 h | 4.08 g | 0.53 g | 74.4% a | 68.1 ± 11.9 b | 3.9 ± 3.0 b,h | 3.85 g | 0.53 g |
| Her2+ | 22.1% | 68.7 ± 12.2 f | 3.3 ± 2.8 h | 13.09 e,g | 0.52 g | 25.6% a | 64.0 ± 13.8 b,f,h | 3.4 ± 2.7 | 3.29 a,g | 0.49 g |
| Stage I–III | ||||||
|---|---|---|---|---|---|---|
| Treatment | Patient TRs | % of All TRs | % TRs with AEs | % AEs/TR | Age ± SD | Comorbidity Index ± SD |
| Outpatient | ||||||
| Taxanes | 54,178 | 24.1% | 38.3% | 9.2% | 63.8 ± 10.5 | 3.9 ± 2.5 |
| Her2 targeting agents | 41,037 | 18.2% | 36.4% | 6.6% | 64.5 ± 11.2 | 4.0 ± 2.6 |
| Bisphosphonates | 25,976 | 11.5% | 30.0% | 3.5% | 65.5 ± 11.1 | 4.3 ± 2.6 |
| Alkylating agents | 23,921 | 10.6% | 29.1% | 3.1% | 65.5 ± 9.5 | 4.2 ± 2.5 |
| Anthracyclines | 17,380 | 7.7% | 54.2% | 4.2% | 63.9 ± 9.4 | 4.0 ± 2.3 |
| Pyrimidine analogs | 13,960 | 6.2% | 42.7% | 2.7% | 61.9 ± 12.2 | 4.1 ± 2.6 |
| Antiestrogens | 13,723 | 6.1% | 27.8% | 1.7% | 63.3 ± 12.5 | 4.4 ± 2.7 |
| Platinum cmpds. | 13,557 | 6.0% | 55.6% | 3.4% | 62.7 ± 11.0 | 3.9 ± 2.4 |
| Vinca alkaloids | 6427 | 2.9% | 36.0% | 1.0% | 57.5 ± 12.6 | 3.5 ± 2.5 |
| Folate antagonists | 5325 | 2.4% | 23.7% | 0.6% | 66.3 ± 10.8 | 4.7 ± 2.6 |
| VEGF inhibitors | 3696 | 1.6% | 37.9% | 0.6% | 60.7 ± 13.2 | 3.8 ± 2.5 |
| Non chemother. | 2781 | 1.2% | 41.3% | 0.5% | 67.2 ± 11.3 | 5.3 ± 2.8 |
| Total tallied | 221,961 | 98.7% | 37.0% | 63.6 ± 11.3 | 4.2 ± 2.6 | |
| NCH | ||||||
| Taxanes | 130,739 | 21.2% | 57.0% | 12.1% | 65.6 ± 9.6 | 4.0 ± 2.4 |
| Her2 targeting agents | 98,222 | 15.9% | 51.7% | 8.2% | 66.4 ± 10.4 | 4.0 ± 2.5 |
| Anthracyclines | 63,847 | 10.4% | 72.5% | 7.5% | 66.1 ± 8.5 | 4.2 ± 2.3 |
| Pyrimidine analogs | 57,783 | 9.4% | 66.5% | 6.2% | 65.9 ± 10.6 | 4.5 ± 2.5 |
| Bisphosphonates | 55,761 | 9.1% | 35.1% | 3.2% | 67.1 ± 10.5 | 4.4 ± 2.5 |
| VEGF inhibitors | 49,015 | 8.0% | 29.5% | 2.3% | 71.2 ± 11.1 | 5.2 ± 2.5 |
| Alkylating agents | 47,241 | 7.7% | 51.8% | 4.0% | 67.0 ± 8.6 | 4.1 ± 2.4 |
| Platinum cmpds. | 35,885 | 5.8% | 67.7% | 3.9% | 64.8 ± 10.2 | 4.0 ± 2.4 |
| Antiestrogens | 25,883 | 4.2% | 37.5% | 1.6% | 65.4 ± 11.5 | 4.4 ± 2.5 |
| Folate antagonists | 23,502 | 3.8% | 57.9% | 2.2% | 68.9 ± 8.9 | 5.1 ± 2.4 |
| Vinca alkaloids | 22,480 | 3.7% | 55.3% | 2.0% | 61.5 ± 12.4 | 3.8 ± 2.4 |
| Total tallied | 610,358 | 98.1% | 53.3% | 66.4 ± 10.2 | 4.3 ± 2.4 | |
| Significance Outpatient/NCH t-test | p = 0 | p = 0 | ||||
| Stage IV | ||||||
|---|---|---|---|---|---|---|
| Treatment | Patient TRs | % of all TRs | % TRs with AEs | % AEs/TR | Age ± SD | Comorbidity Index ± SD |
| Outpatient | ||||||
| Taxanes | 9687 | 22.0% | 33.5% | 7.4% | 63.1 ± 11.8 | 3.3 ± 2.5 |
| Her2 targeting agents | 8729 | 19.8% | 31.4% | 6.2% | 62.2 ± 12.5 | 3.2 ± 2.7 |
| Bisphosphonates | 8559 | 19.4% | 30.6% | 5.9% | 65.5 ± 12.0 | 3.6 ± 2.7 |
| Antiestrogens | 4897 | 11.1% | 21.1% | 2.3% | 67.1 ± 11.0 | 3.8 ± 2.7 |
| Pyrimidine analogs | 3077 | 7.0% | 39.1% | 2.7% | 62.1 ± 11.8 | 3.4 ± 2.6 |
| Vinca alkaloids | 2179 | 4.9% | 32.9% | 1.6% | 61.0 ± 11.6 | 3.2 ± 2.6 |
| Platinum cmpds. | 1760 | 4.0% | 54.8% | 2.2% | 61.4 ± 12.3 | 3.1 ± 2.4 |
| Anthracyclines | 1374 | 3.1% | 50.5% | 1.6% | 62.1 ± 11.1 | 3.3 ± 2.5 |
| Alkylating agents | 1350 | 3.1% | 30.1% | 0.9% | 63.0 ± 11.4 | 3.5 ± 2.6 |
| VEGF inhibitors | 1094 | 2.5% | 37.0% | 0.9% | 61.3 ± 11.1 | 2.7 ± 2.1 |
| Her2 ab + DM1 antitubulin | 593 | 1.3% | 25.8% | 0.3% | 58.9 ± 13.1 | 2.8 ± 2.7 |
| Total tallied | 43,299 | 98.2% | 32.1% | 62.5 ± 11.8 | 3.3 ± 2.5 | |
| NCH | ||||||
| Taxanes | 21,747 | 23.9% | 52.6% | 12.6% | 65.5 ± 10.6 | 3.6 + 2.5 |
| Her2 targeting agents | 18,898 | 20.7% | 52.9% | 11.0% | 64.7 + 11.9 | 3.4 ± 2.5 |
| Bisphosphonates | 12,422 | 13.6% | 54.2% | 7.4% | 66.9 ± 11.5 | 3.8 ± 2.6 |
| Pyrimidine analogs | 8856 | 9.7% | 62.8% | 6.1% | 64.4 ± 11.1 | 3.6 ± 2.5 |
| Antiestrogens | 5879 | 6.5% | 38.9% | 2.5% | 68.1 ± 11.3 | 3.9 ± 2.6 |
| Vinca alkaloids | 5264 | 5.8% | 55.1% | 3.2% | 64.2 ± 12.1 | 3.5 ± 2.4 |
| Platinum cmpds. | 4626 | 5.1% | 69.4% | 3.5% | 64.8 ± 10.6 | 3.4 ± 2.4 |
| VEGF inhibitors | 4613 | 5.1% | 53.8% | 2.7% | 66.6 ± 12.0 | 3.9 ± 2.6 |
| Anthracyclines | 3054 | 3.4% | 69.9% | 2.3% | 65.1 ± 10.2 | 3.5 ± 2.2 |
| Alkylating agents | 2737 | 3.0% | 57.4% | 1.7% | 65.5 ± 10.0 | 3.5 ± 2.5 |
| Folate analogs | 2116 | 2.3% | 64.6% | 1.5% | 65.7 ± 11.0 | 4.0 ± 2.8 |
| Total tallied | 90,212 | 99.0% | 54.5% | 65.6 ± 11.1 | 3.7 ± 2.5 | |
| Significance Outpatient/NCH t-test | p = 0 | p = 0 | ||||
| AEs | AEs with TRs | % of all TR AEs | AEs | AEs with TRs | % of all TR AEs |
|---|---|---|---|---|---|
| Outpatient | NCH | ||||
| Stage I–III | |||||
| Nausea/vomiting | 22,058 | 26.1% | Nausea/vomiting | 176,989 | 53.4% |
| Weakness/malaise, delirium | 19,781 | 23.4% | Electrolyte abnormalities | 30,892 | 9.3% |
| Neutropenia/Leukopenia | 13,273 | 15.7% | Weakness/malaise, delirium | 29,611 | 8.9% |
| Respiratory symptoms. | 6470 | 7.7% | Neutropenia/Leukopenia | 29,329 | 8.8% |
| Anemias | 4518 | 5.4% | Anemias | 26,208 | 7.9% |
| Infection/fever | 4185 | 5.0% | Respiratory symptoms | 11,771 | 3.5% |
| Electrolyte abnormalities | 3814 | 4.5% | Infection/fever | 10,400 | 3.1% |
| Diarrhea | 2882 | 3.4% | Thrombophilia | 5647 | 1.7% |
| Thrombophilia | 2531 | 3.0% | Diarrhea | 3242 | 1.0% |
| Constipation | 2214 | 2.6% | |||
| Pulm. Embolus | 1163 | 1.4% | |||
| Weight loss/malnutrition | 859 | 1.0% | |||
| Total tallied | 83,748 | 99.2% | Total tallied | 324,089 | 97.7% |
| Stage IV | |||||
| Weakness/malaise, delirium | 3731 | 24.5% | Nausea/vomiting | 22,939 | 45.7% |
| Nausea/vomiting | 3342 | 22.0% | Electrolyte abnormalities | 6492 | 12.9% |
| Neutropenia/Leukopenia | 1828 | 12.0% | Weakness/malaise, delirium | 5994 | 11.9% |
| Respiratory symptoms | 1412 | 9.3% | Anemias | 4588 | 9.1% |
| Anemias | 1095 | 7.2% | Neutropenia/Leukopenia | 3588 | 7.2% |
| Infection/fever | 850 | 5.6% | Respiratory symptoms | 2497 | 5.0% |
| Thrombophilia | 801 | 5.3% | Infection/fever | 1154 | 2.3% |
| Electrolyte abnormalities | 627 | 4.1% | Thrombophilia | 1047 | 2.1% |
| Constipation | 461 | 3.0% | Pulmonary Embolus | 623 | 1.2% |
| Diarrhea | 410 | 2.7% | Diarrhea | 536 | 1.1% |
| Pulmonary Embolus | 407 | 2.7% | |||
| Weight loss/malnutrition | 156 | 1.0% | |||
| Total tallied | 15,120 | 99.5% | Total tallied | 49,458 | 98.6% |
| (A) | ||||||||||
| Stage I–III | ||||||||||
| Treatment | Patient TRs | % of All TRs | % AEs/TR | Age ± SD | Comorb. Ind. ± SD | Patient TRs | % of All TRs | % AEs/TR | Age ± SD | Comorb. Ind. ± SD |
| Outpatient | NCH | |||||||||
| White patients | ||||||||||
| Taxanes | 40,541 | 23.6% | 9.1% | 64.7 ± 10.0 | 3.8 ± 2.5 | 109,345 | 20.9% | 11.9% | 66.1 ± 9.2 | 4.0 ± 2.4 |
| Her2 target. agts | 31,093 | 18.1% | 6.7% | 65.4 ± 10.8 | 3.9 ± 2.6 | 82,328 | 15.7% | 8.1% | 66.9 ± 10.1 | 4.0 ± 2.5 |
| Bisphosphonates | 21,771 | 12.6% | 3.7% | 66.1 ± 10.5 | 4.3 ± 2.6 | 49,594 | 9.5% | 3.3% | 67.3 ± 10.4 | 4.4 ± 2.5 |
| Alkylating agents | 18,036 | 10.5% | 3.0% | 66.3 ± 9.0 | 4.1 ± 2.5 | 39,253 | 7.5% | 3.9% | 67.4 ± 8.2 | 4.0 ± 2.4 |
| Anthracyclines | 12,865 | 7.5% | 4.0% | 64.8 ± 8.7 | 3.9 ± 2.2 | 52,960 | 10.1% | 7.3% | 66.5 ± 8.2 | 4.2 ± 2.3 |
| Antiestrogens | 11,392 | 6.6% | 1.9% | 64.1 ± 12.1 | 4.4 ± 2.7 | 23,246 | 4.4% | 1.7% | 65.8 ± 11.2 | 4.4 ± 2.4 |
| Pyrimidine anlgs. | 10,120 | 5.9% | 2.6% | 63.1 ± 11.5 | 4.1 ± 2.6 | 48,948 | 9.3% | 6.2% | 66.4 ± 10.2 | 4.5 ± 2.5 |
| Platinum cmpds. | 9835 | 5.7% | 3.2% | 63.8 ± 10.2 | 3.8 ± 2.4 | 29,312 | 5.6% | 3.8% | 65.3 ± 9.8 | 4.0 ± 2.4 |
| Vinca alkaloids | 4958 | 2.9% | 1.0% | 58.5 ± 12.6 | 3.6 ± 2.5 | 18,548 | 3.5% | 1.9% | 62.1 ± 12.2 | 3.8 ± 2.4 |
| Folate analogs | 4296 | 2.5% | 0.6% | 66.9 ± 10.2 | 4.6 ± 2.6 | 20,416 | 3.9% | 2.3% | 69.2 ± 8.6 | 5.0 ± 2.4 |
| VEGF inhibitors | 2706 | 1.6% | 0.6% | 62.1 ± 12.8 | 3.9 ± 2.5 | 45,219 | 8.6% | 3.4% | 71.9 ± 10.8 | 5.2 ± 2.5 |
| Non chemother. | 2284 | 1.3% | 0.5% | 67.7 ± 11.0 | 5.1 ± 2.8 | |||||
| Total tallied | 169,897 | 98.7% | 36.9% | 64.5 ± 10.8 | 4.1 ± 2.5 | 519,169 | 99.1% | 53.7% | 66.8 ± 9.9 | 4.3 ± 2.4 |
| African American Patients | ||||||||||
| Taxanes | 10,768 | 26.3% | 10.0% | 60.2 ± 11.6 | 4.3 ± 2.6 | 13.603 | 23.9% | 13.2% | 61.7 ± 11.3 | 4.4 ± 2.6 |
| Her2 target. agts. | 7551 | 18.4% | 6.8% | 60.7 ± 12.0 | 4.3 ± 2.7 | 8.750 | 15.4% | 7.8% | 62.0 ± 12.1 | 4.2 ± 2.5 |
| Alkylating agents | 4772 | 11.7% | 3.5% | 62.1 ± 10.5 | 4.6 ± 2.6 | 5366 | 9.4% | 4.7% | 63.6 ± 10.3 | 4.5 ± 2.6 |
| Anthracyclines | 3794 | 9.3% | 5.0% | 60.8 ± 10.7 | 4.5 ± 2.5 | 7947 | 13.9% | 10.1% | 62.9 ± 9.6 | 4.7 ± 2.5 |
| Pyrimidine anlgs. | 3062 | 7.5% | 2.9% | 57.4 ± 13.1 | 4.1 ± 2.6 | 5524 | 9.7% | 6.2% | 63.0 ± 12.2 | 4.9 ± 2.6 |
| Platinum cmpds. | 3044 | 7.4% | 4.3% | 58.5 ± 12.3 | 4.1 ± 2.5 | 3852 | 6.8% | 4.4% | 60.5 ± 12.0 | 4.4 ± 2.6 |
| Bisphosphonates | 2691 | 6.6% | 2.3% | 59.6 ± 13.8 | 4.2 ± 2.8 | 3012 | 5.3% | 2.5% | 63.3 ± 12.2 | 4.7 ± 2.8 |
| Antiestrogens | 1678 | 4.1% | 1.1% | 59.2 ± 13.9 | 4.4 ± 2.7 | 1320 | 2.3% | 0.9% | 61.1 ± 14.1 | 4.6 ± 2.7 |
| Vinca alkaloids | 1122 | 2.7% | 1.0% | 53.1 ± 12.0 | 3.3 ± 2.4 | 2829 | 5.0% | 2.8% | 57.5 ± 13.6 | 3.7 ± 2.5 |
| VEGF inhibitors | 783 | 1.9% | 0.8% | 55.0 ± 13.0 | 3.8 ± 2.6 | 2023 | 3.6% | 1.4% | 64.2 ± 12.4 | 5.5 ± 2.8 |
| Folate analogs | 755 | 1.8% | 0.4% | 62.8 ± 12.8 | 5.1 ± 2.7 | 2047 | 3.6% | 2.1% | 66.6 ± 10.8 | 5.8 ± 2.5 |
| Total tallied | 40,020 | 97.8% | 38.1% | 59.0 ± 12.3 | 4.3 ± 2.6 | 56,273 | 98.8% | 56.0% | 62.4 ± 11.9 | 4.7 ± 2.6 |
| Significance W/AA t-test | p = 0 | p = 0 | p = 0 | p = 0 | ||||||
| (B) | ||||||||||
| Stage IV | ||||||||||
| Treatment | Patient TRs | % of all TRs | % AEs/TR | Age ± SD | Comorb. Ind. ± SD | Patient TRs | % of All TRs | % AEs/TR | Age ± SD | Comorb. Ind. ± SD |
| Outpatient | NCH | |||||||||
| White patients | ||||||||||
| Taxanes | 7229 | 21.0% | 6.8% | 64.0 ± 11.4 | 3.3 ± 2.5 | 18,954 | 24.1% | 12.7% | 65.9 ± 10.2 | 3.6 ± 2.4 |
| Bisphosphonates | 7001 | 20.3% | 8.0% | 66.4 ± 11.6 | 3.7 ± 2.7 | 10,674 | 13.5% | 7.4% | 67.7 ± 11.2 | 3.9 ± 2.6 |
| Her2 target. agts. | 6653 | 19.3% | 6.2% | 63.4 ± 12.1 | 3.3 ± 2.8 | 16,209 | 20.6% | 10.9% | 65.4 ± 11.8 | 3.4 ± 2.6 |
| Antiestrogens | 4113 | 11.9% | 2.3% | 67.8 ± 10.8 | 3.8 ± 2.7 | 5157 | 6.5% | 2.5% | 68.6 ± 11.1 | 4.0 ± 2.6 |
| Pyrimidine anlgs. | 2445 | 7.1% | 2.9% | 63.3 ± 11.5 | 3.5 ± 2.6 | 7867 | 10.0% | 6.4% | 64.9 ± 10.6 | 3.6 ± 2.5 |
| Vinca alkaloids | 1712 | 5.0% | 1.6% | 61.7 ± 11.5 | 3.3 ± 2.6 | 4532 | 5.8% | 3.2% | 64.6 ± 11.6 | 3.6 ± 2.4 |
| Platinum cmpds. | 1378 | 4.0% | 2.2% | 62.3 ± 11.4 | 3.1 ± 2.3 | 3688 | 4.7% | 3.2% | 65.6 ± 9.9 | 3.5 ± 2.5 |
| Anthracyclines | 1055 | 3.1% | 1.6% | 63.5 ± 10.4 | 3.2 ± 2.4 | 2649 | 3.4% | 2.4% | 65.4 ± 9.9 | 3.5 ± 2.2 |
| Alkylating agents | 1013 | 2.9% | 0.8% | 64.1 ± 11.0 | 3.4 ± 2.1 | 2364 | 3.0% | 1.7% | 65.4 ± 9.7 | 3.5 ± 2.5 |
| VEGF inhibitors | 799 | 2.3% | 0.8% | 62.0 ± 10.9 | 2.8 ± 2.1 | 3939 | 5.0% | 2.6% | 67.2 ± 11.6 | 3.9 ± 2.6 |
| Her2 ab+DM1 | 386 | 1.1% | 0.3% | 61.5 ± 12.8 | 3.1 ± 3.1 | 0 | 0 | 0 | 0 | 0 |
| Folate analogs | 341 | 1.0% | 0.3% | 63.5 ± 12.2 | 3.6 ± 2.7 | 2062 | 2.6% | 1.7% | 65.6 ± 10.5 | 4.0 ± 2.9 |
| Total tallied | 34,125 | 99.0% | 33.8% | 63.6 ± 11.4 | 3.3 ± 2.6 | 78,095 | 99.1% | 54.7% | 66.0 ± 10.7 | 3.7 ± 2.5 |
| African American Patients | ||||||||||
| Taxanes | 2052 | 27.4% | 10.1% | 60.0 ± 12.7 | 3.7 ± 2.7 | 1933 | 24.4% | 12.0% | 63.1 ± 12.9 | 4.0 ± 2.8 |
| Her2 target. agts. | 1483 | 19.8% | 6.6% | 57.0 ± 13.7 | 3.2 ± 2.3 | 1313 | 16.6% | 8.2% | 60.3 ± 12.2 | 3.1 ± 2.2 |
| Bisphosphonates | 1174 | 15.7% | 6.4% | 61.3 ± 13.1 | 3.5 ± 2.7 | 1117 | 14.1% | 7.3% | 62.3 ± 12.4 | 4.1 ± 2.6 |
| Antiestrogens | 585 | 7.8% | 2.7% | 63.5 ± 12.0 | 3.9 ± 2.7 | 494 | 6.2% | 2.9% | 63.1 ± 13.7 | 4.0 ± 2.6 |
| Pyrimidine anlgs. | 445 | 5.9% | 2.0% | 58.6 ± 12.2 | 3.5 ± 2.7 | 709 | 8.9% | 4.7% | 60.5 ± 13.6 | 3.2 ± 2.5 |
| Vinca alkaloids | 374 | 5.0% | 1.7% | 59.6 ± 11.6 | 3.1 ± 2.5 | 571 | 7.2% | 3.8% | 59.0 ± 15.3 | 3.0 ± 2.3 |
| Platinum cmpds. | 310 | 4.1% | 2.3% | 59.2 ± 14.0 | 3.8 ± 2.8 | 783 | 9.9% | 6.8% | 61.2 ± 12.8 | 3.3 ± 2.3 |
| Anthracyclines | 267 | 3.6% | 1.5% | 58.5 ± 11.8 | 3.7 ± 2.8 | 298 | 3.8% | 2.4% | 64.5 ± 10.2 | 3.6 ± 2.3 |
| VEGF inhibitors | 260 | 3.5% | 2.1% | 57.4 ± 12.8 | 2.6 ± 2.2 | 286 | 3.6% | 1.9% | 58.9 ± 13.9 | 3.0 ± 1.9 |
| Alkylating agents | 257 | 3.4% | 1.1% | 59.4 ± 11.6 | 4.2 ± 3.1 | 260 | 3.3% | 1.6% | 66.7 ± 11.2 | 3.7 ± 2.4 |
| Her2 ab + DM1 | 170 | 2.3% | 0.7% | 50.0 ± 11.4 | 2.5 ± 1.8 | 0 | 0 | 0 | 0 | 0 |
| Total tallied | 7377 | 98.6% | 37.1% | 58.6 ± 12.5 | 3.4 ± 2.6 | 7764 | 97.9% | 51.8% | 62.0 ± 12.8 | 3.5 ± 2.4 |
| Significance W/AA t-test | p = 0 | p = 0.003 | p = 0 | p = 0 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wieder, R.; Adam, N. Racial Disparities in Breast Cancer Treatments and Adverse Events in the SEER-Medicare Data. Cancers 2023, 15, 4333. https://doi.org/10.3390/cancers15174333
Wieder R, Adam N. Racial Disparities in Breast Cancer Treatments and Adverse Events in the SEER-Medicare Data. Cancers. 2023; 15(17):4333. https://doi.org/10.3390/cancers15174333
Chicago/Turabian StyleWieder, Robert, and Nabil Adam. 2023. "Racial Disparities in Breast Cancer Treatments and Adverse Events in the SEER-Medicare Data" Cancers 15, no. 17: 4333. https://doi.org/10.3390/cancers15174333
APA StyleWieder, R., & Adam, N. (2023). Racial Disparities in Breast Cancer Treatments and Adverse Events in the SEER-Medicare Data. Cancers, 15(17), 4333. https://doi.org/10.3390/cancers15174333







