The Vermiform Appendix and Its Pathologies
Abstract
Simple Summary
Abstract
1. Introduction
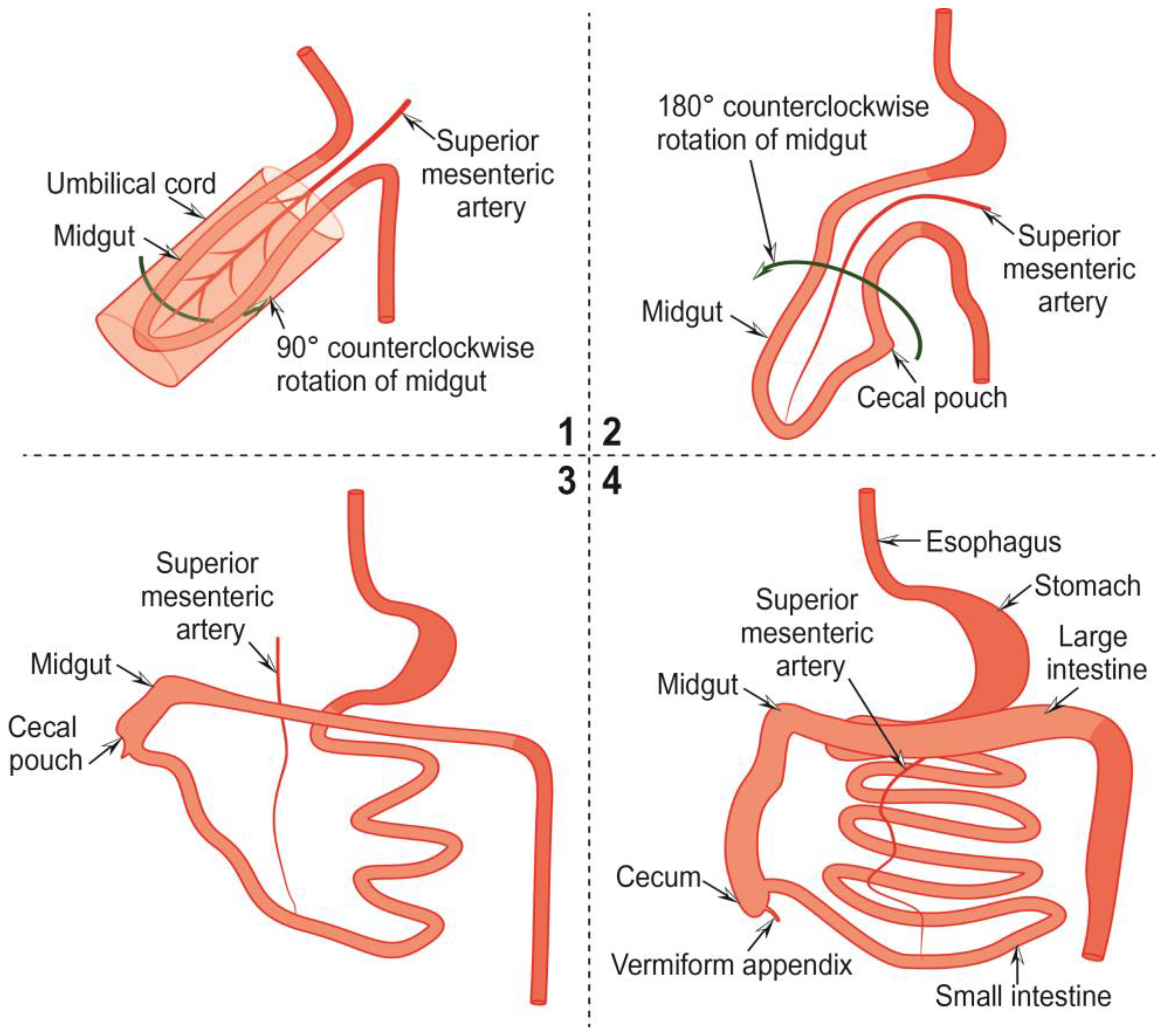
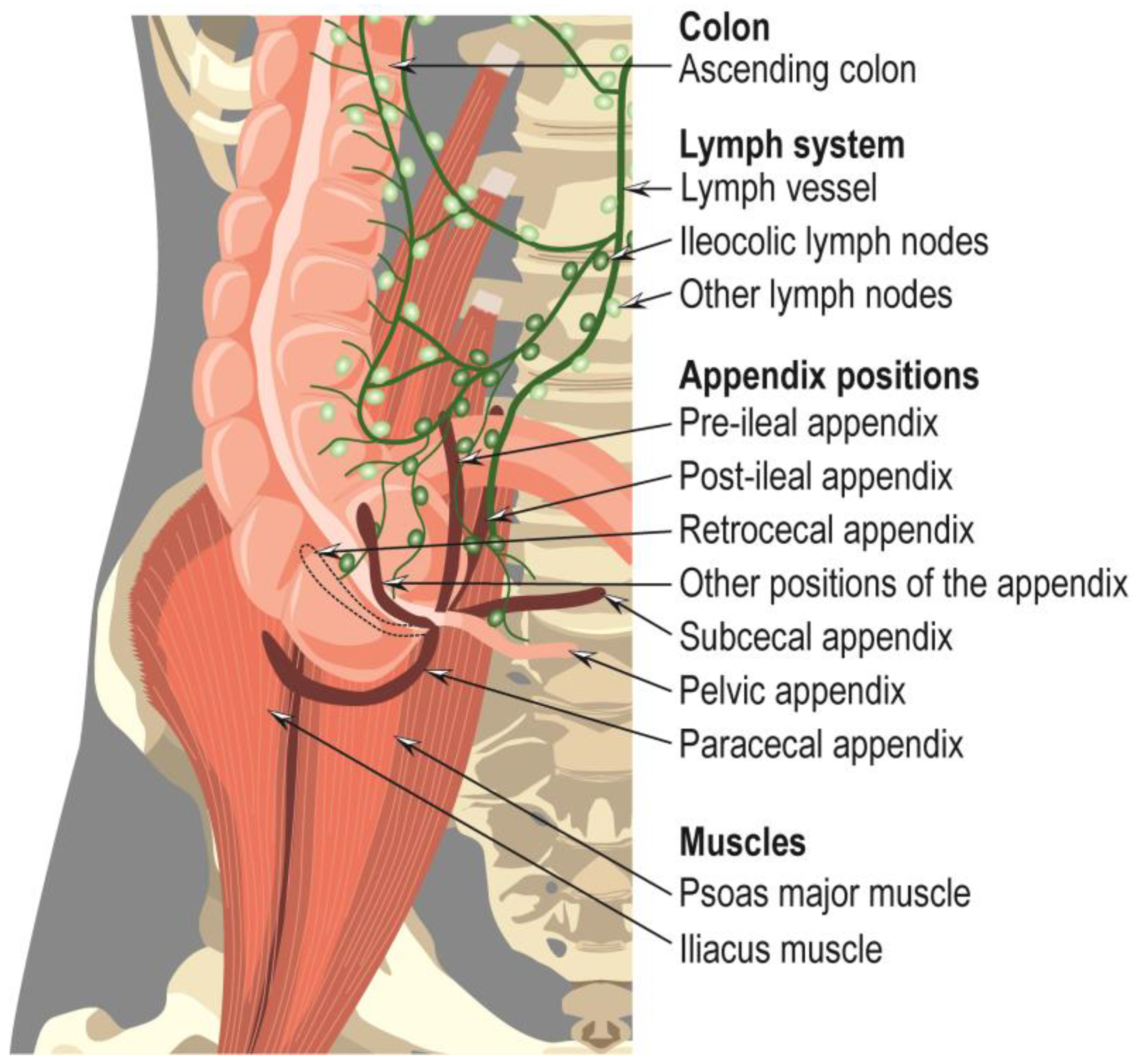
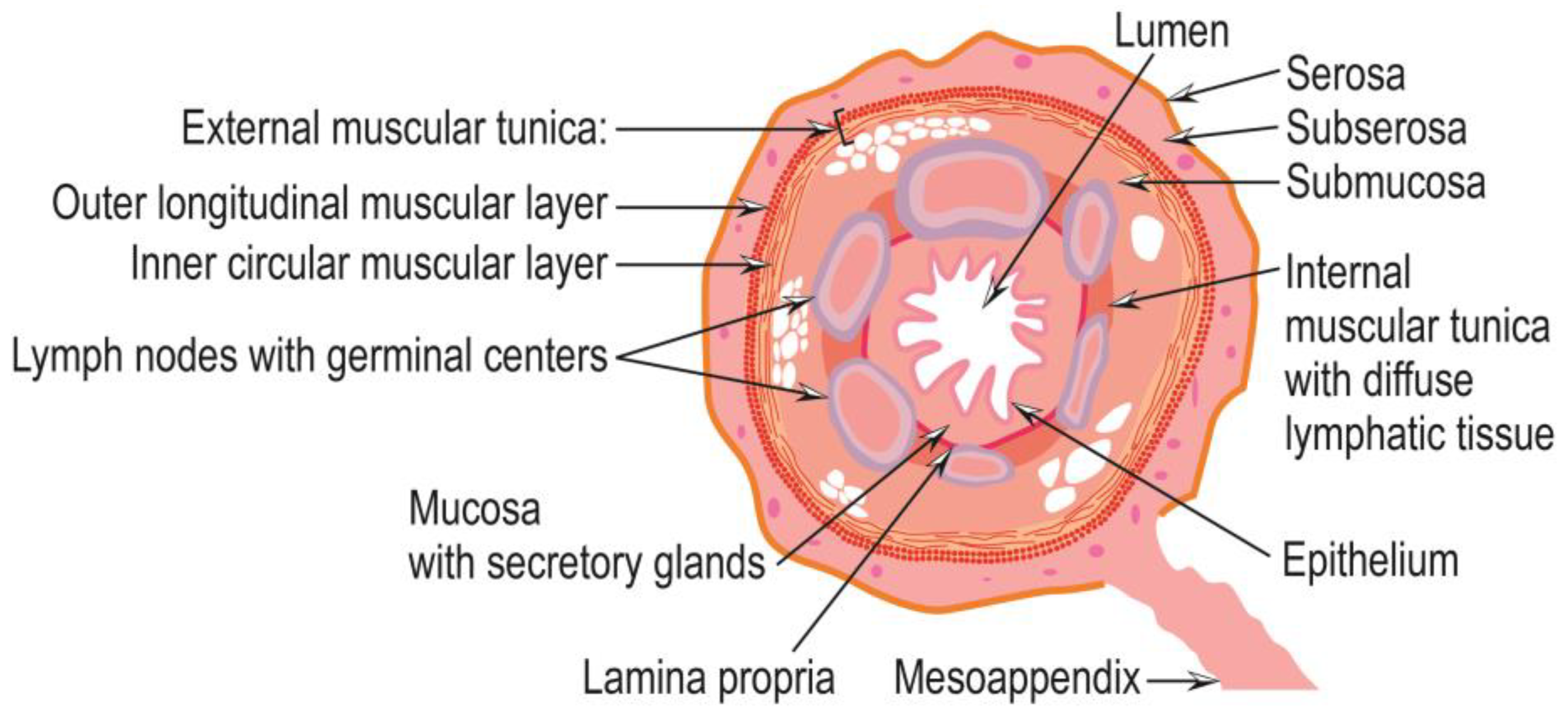
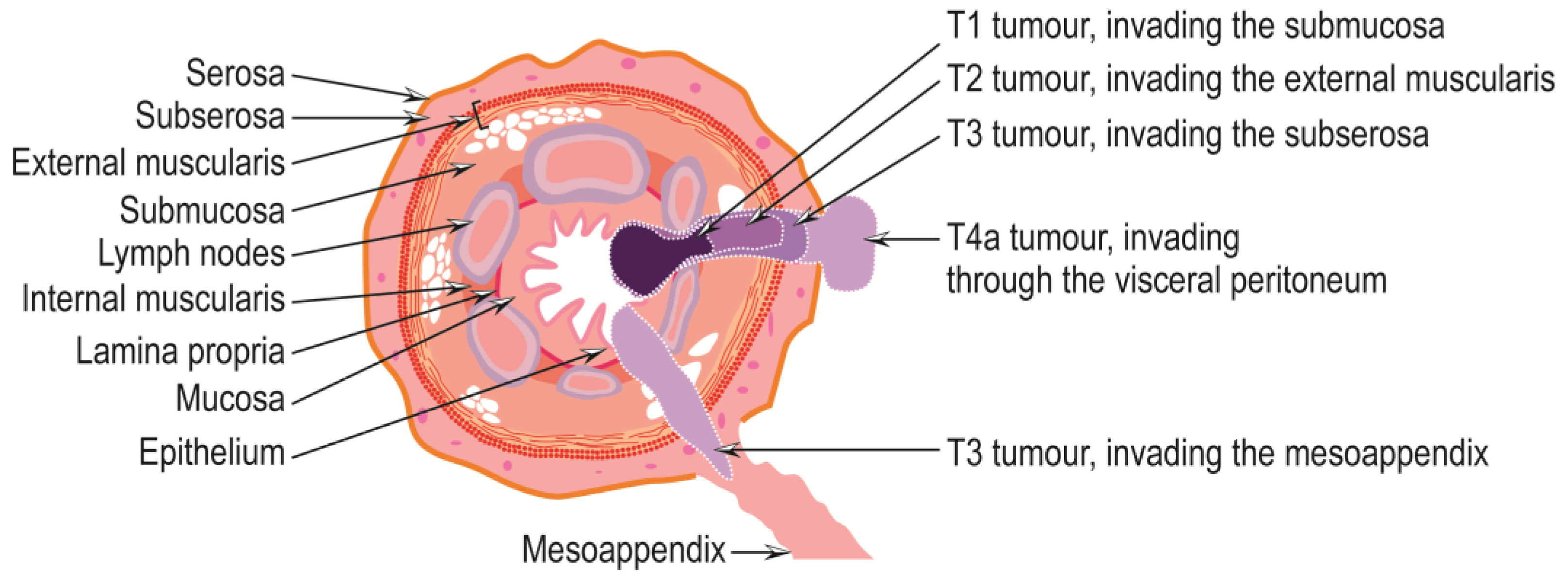
2. The Vermiform Appendix—Anatomy and Embryology
3. Inflammatory Pathologies of the Vermiform Appendix
4. Pathologies Related to Congenital Anomalies of the Appendix and Other Related Diseases
5. Tumors of the Appendix
5.1. Hyperplastic Polyps, Sessile Serrated Lesions without Dysplasia, and Serrated Lesions with Dysplasia
5.2. Appendiceal Mucinous Neoplasms
5.3. Appendiceal Adenocarcinomas NOS and Undifferentiated Carcinomas NOS
5.4. Appendiceal Goblet Cell Adenocarcinoma
5.5. Appendiceal Neuroendocrine Neoplasms
5.6. Therapeutic Approaches for Appendiceal Cancers
| Tumor Type | Therapeutic Approaches |
|---|---|
| Mucinous neoplasms, grade 1 | Appendectomy [34] |
| Mucinous neoplasms, grades 2, 3 | Appendectomy + right hemicolectomy + perioperative systemic chemotherapy [137,141,142] |
| Pseudomyxoma peritonei | Cytoreductive surgery + hyperthermic intraperitoneal chemotherapy [138] |
| Pseudomyxoma peritonei, grades 2, 3 | Cytoreductive surgery + hyperthermic intraperitoneal chemotherapy [138] + perioperative systemic chemotherapy [139,140,142] |
| Mucinous adenocarcinoma | Right hemicolectomy [143] Chemotherapy [144] Cytoreductive surgery + hyperthermic intraperitoneal chemotherapy [145] |
| Goblet cell adenocarcinomas without carcinomatosis | Right hemicolectomy [146] |
| Goblet cell adenocarcinomas with carcinomatosis | Cytoreductive surgery + hyperthermic intraperitoneal chemotherapy [147] |
| Goblet cell adenocarcinomas, stages III, IV | Cytoreductive surgery + adjuvant chemotherapy [148] |
| Nonmucinous appendiceal adenocarcinomas/signet ring adenocarcinomas without metastases | Right hemicolectomy [149] |
| Nonmucinous appendiceal adenocarcinomas/signet ring adenocarcinomas with metastases | Right hemicolectomy [149] + standard systemic chemotherapy (fluorouracil, platinum, and irinotecan [153]) + cytoreductive surgery/hyperthermic intraperitoneal chemotherapy [150,151,152] |
| Localized nonmucinous appendiceal adenocarcinomas/signet ring adenocarcinomas without node involvement | Right hemicolectomy [149] + adjuvant chemotherapy (fluoropyrimidine/oxaliplatin) [153] |
| Neuroendocrine neoplasms < 2 cm | Appendectomy [155] |
| Neuroendocrine neoplasms > 2 cm | Right hemicolectomy [155] |
| Resecable metastatic neuroendocrine neoplasms | Cytoreductive surgery [155,157] |
| Non-resectable metastatic neuroendocrine neoplasms | Bland hepatic artery embolization + intra-arterial chemoembolization with cisplatin or doxorubicin + and 90Y-radioembolization [158] Somatostatin analogue therapies: octreotide (PROMID phase III study)/lanreotide (în CLARINET phase III study) [159] Everolimus (mTOR inhibitor)/Sunitinib (VEGFRs 1–3 inhibitors), and surufatinib (angiogenesis inhibitor) [155] FOLFOX (folinic acid, fluorouracil and oxaliplatin)/XELOX/CAPOX (capecitabine and oxaliplatin) [160,161] CAPTEM (capecitabin and temozolomide) [162] FOLFOX or XELOX/CAPOX + bevacizumab [163,164] |
6. Other Diagnoses Associated with the Vermiform Appendix
7. Discussion
8. Conclusions
9. Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vitetta, L.; Chen, J.; Clarke, S. The vermiform appendix: An immunological organ sustaining a microbiome inoculum. Clin. Sci. 2019, 133, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Krzyzak, M.; Mulrooney, S.M. Acute appendicitis review: Background, epidemiology, diagnosis, and treatment. Cureus 2020, 12, e8562. [Google Scholar] [CrossRef] [PubMed]
- Moris, D.; Paulson, E.K.; Pappas, T.N. Diagnosis and Management of Acute Appendicitis in Adults: A Review. JAMA 2021, 326, 2299–2311. [Google Scholar] [CrossRef] [PubMed]
- Jordan, T.R.; Webb, E.M. Diseases of the Appendix. In Abdominal Imaging; Hamm, B., Ros, P.R., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; pp. 885–904. [Google Scholar]
- Yoo, H.Y.; Choi, J.; Kim, J.; Chai, Y.J.; Shin, R.; Ahn, H.S.; Lim, C.-S.; Lee, H.W.; Hwang, K.-T.; Jung, I.M. Unexpected appendiceal pathologies and their changes with the expanding use of preoperative imaging studies. Ann. Coloproctol. 2017, 33, 99–105. [Google Scholar] [CrossRef][Green Version]
- Jones, M.W.; Lopez, R.A.; Deppen, J.G.; Kendall, B.A. Appendicitis (Nursing). In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Echevarria, S.; Rauf, F.; Hussain, N.; Zaka, H.; Ahsan, N.; Broomfield, A.; Akbar, A.; Khawaja, U.A.; Farwa, U.E. Typical and Atypical Presentations of Appendicitis and Their Implications for Diagnosis and Treatment: A Literature Review. Cureus 2023, 15, e37024. [Google Scholar] [CrossRef] [PubMed]
- Vieira, E.d.P.L.; Bonato, L.M.; Silva, G.G.P.d.; Gurgel, J.L. Congenital abnormalities and anatomical variations of the vermiform appendix and mesoappendix. J. Coloproctol. 2019, 39, 279–287. [Google Scholar] [CrossRef]
- Ahadi, M.; Sokolova, A.; Brown, I.; Chou, A.; Gill, A.J. The 2019 World Health Organization Classification of appendiceal, colorectal and anal canal tumours: An update and critical assessment. Pathology 2021, 53, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, S.; Verde, F.; Johnson, P.T.; Fishman, E.K.; Macura, K.J. Anatomical variants and pathologies of the vermix. Emerg. Radiol. 2014, 21, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Schumpelick, V.; Dreuw, B.; Ophoff, K.; Prescher, A. Appendix and cecum. Embryology, anatomy, and surgical applications. Surg. Clin. N. Am. 2000, 80, 295–318. [Google Scholar] [CrossRef] [PubMed]
- Malone, J.C.; Shah, A.B. Embryology, Midgut. In StatPearls [Internet]; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Souza, S.C.D.; Costa, S.R.M.R.D.; Souza, I.G.S.D. Vermiform appendix: Positions and length-a study of 377 cases and literature review. J. Coloproctol. 2015, 35, 212–216. [Google Scholar] [CrossRef]
- Simonovský, V. Sonographic detection of normal and abnormal appendix. Clin. Radiol. 1999, 54, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Nikolaidis, P.; Hwang, C.M.; Miller, F.H.; Papanicolaou, N. The nonvisualized appendix: Incidence of acute appendicitis when secondary inflammatory changes are absent. AJR Am. J. Roentgenol. 2004, 183, 889–892. [Google Scholar] [CrossRef] [PubMed]
- Spalluto, L.B.; Woodfield, C.A.; DeBenedectis, C.M.; Lazarus, E. MR Imaging Evaluation of Abdominal Pain during Pregnancy: Appendicitis and Other Nonobstetric Causes. RadioGraphics 2012, 32, 317–334. [Google Scholar] [CrossRef] [PubMed]
- Hardin, D.M., Jr. Acute appendicitis: Review and update. Am. Fam. Physician 1999, 60, 2027–2034. [Google Scholar] [PubMed]
- Guan, L.; Liu, Z.; Pan, G.; Zhang, B.; Wu, Y.; Gan, T.; Ouyang, G. The global, regional, and national burden of appendicitis in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. BMC Gastroenterol. 2023, 23, 44. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Guo, C.; Gu, Z.; Hua, J.; Zhang, J.; Qian, S.; Shi, J. The global burden of appendicitis in 204 countries and territories from 1990 to 2019. Clin Epidemiol. 2022, 14, 1487–1499. [Google Scholar] [CrossRef] [PubMed]
- Simmering, J.E.; Polgreen, L.A.; Talan, D.A.; Cavanaugh, J.E.; Polgreen, P.M. Association of appendicitis incidence with warmer weather independent of season. JAMA Netw. Open 2022, 5, e2234269. [Google Scholar] [CrossRef] [PubMed]
- Dreuw, B.; Truong, S.; Riesener, K.P.; Füzesi, L.; Schumpelick, V. The value of sonography in the diagnosis of appendicitis. A prospective study of 100 patients. Der Chir. Z. Fur Alle Geb. Der Oper. Medizen 1990, 61, 880–886. [Google Scholar]
- Lee, S.D. What patients will have an “atypical” presentation for appendicitis? What are those presentations? In Gastrointestinal Emergencies: Evidence-Based Answers to Key Clinical Questions; Springer: Berlin/Heidelberg, Germany, 2019; pp. 255–258. [Google Scholar]
- Duque, G.A.; Mohney, S. Appendicitis in pregnancy. In StatPearls [Internet]; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Moniruddin, A.B.M.; Chowdhury, S.; Hasan, T.; Ferdous, B.; Khan, M.R. Atypical presentations of appendicitis. KYAMC J. 2021, 12, 101–106. [Google Scholar] [CrossRef]
- Waugh, T.R. Appendix vermiformis duplex. Arch. Surg. 1941, 42, 311–320. [Google Scholar] [CrossRef]
- Altieri, M.L.; Piozzi, G.N.; Salvatori, P.; Mirra, M.; Piccolo, G.; Olivari, N. Appendiceal diverticulitis, a rare relevant pathology: Presentation of a case report and review of the literature. Int. J. Surg. Case Rep. 2017, 33, 31–34. [Google Scholar] [CrossRef]
- D’Souza, G.F.; Abdessalam, S. Volvulus of the appendix: A case report. J. Pediatr. Surg. 2011, 46, e43–e44. [Google Scholar] [CrossRef] [PubMed]
- Fawcitt, R. Appendix situated within the thorax. Br. J. Radiol. 1948, 21, 523–525. [Google Scholar] [CrossRef] [PubMed]
- Vigh, E.; Kopp, M. Appendix in the left thoracic cavity. Orvosi Hetil. 1974, 115, 2623–2624. [Google Scholar]
- Chauhan, S.; Anand, S. Intracecal appendix: An extremely rare anatomical variation. A case report and review of literature. Surg. Radiol. Anat. 2018, 40, 111–114. [Google Scholar] [CrossRef] [PubMed]
- McCusker, M.E.; Coté, T.R.; Clegg, L.X.; Sobin, L.H. Primary malignant neoplasms of the appendix: A population-based study from the surveillance, epidemiology and end-results program, 1973–1998. Cancer 2002, 94, 3307–3312. [Google Scholar] [CrossRef] [PubMed]
- Turaga, K.K.; Pappas, S.G.; Gamblin, T. Importance of histologic subtype in the staging of appendiceal tumors. Ann. Surg. Oncol. 2012, 19, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Hoehn, R.S.; Rieser, C.J.; Choudry, M.H.; Melnitchouk, N.; Hechtman, J.; Bahary, N. Current Management of Appendiceal Neoplasms. Am. Soc. Clin. Oncol. Educ. Book 2021, 41, 118–132. [Google Scholar] [CrossRef] [PubMed]
- Munari, G.; Businello, G.; Mattiolo, P.; Pennelli, G.; Sbaraglia, M.; Borga, C.; Pucciarelli, S.; Spolverato, G.; Mescoli, C.; Galuppini, F.; et al. Molecular profiling of appendiceal serrated lesions, polyps and mucinous neoplasms: A single-centre experience. J. Cancer Res. Clin. Oncol. 2021, 147, 1897–1904. [Google Scholar] [CrossRef] [PubMed]
- Bellizzi, A.M.; Rock, J.; Marsh, W.L.; Frankel, W.L. Serrated lesions of the appendix: A morphologic and immunohistochemical appraisal. Am. J. Clin. Pathol. 2010, 133, 623–632. [Google Scholar] [CrossRef]
- Pai, R.K.; Hartman, D.J.; Gonzalo, D.H.; Lai, K.K.; Downs-Kelly, E.; Goldblum, J.R.; Liu, X.; Patil, D.T.; Bennett, A.E.; Plesec, T.P.; et al. Serrated lesions of the appendix frequently harbor KRAS mutations and not BRAF mutations indicating a distinctly different serrated neoplastic pathway in the appendix. Hum. Pathol. 2014, 45, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Higa, E.; Rosai, J.; Pizzimbono, C.A.; Wise, L. Mucosal hyperplasia, mucinous cystadenoma, and mucinous cystadenocarcinoma of the appendix. A re-evaluation of appendiceal “mucocele”. Cancer 1973, 32, 1525–1541. [Google Scholar] [CrossRef] [PubMed]
- Qizilbash, A.H. Mucoceles of the appendix. Their relationship to hyperplastic polyps, mucinous cystadenomas, and cystadenocarcinomas. Arch. Pathol. 1975, 99, 548–555. [Google Scholar]
- Rubio, C.A. Serrated adenomas of the appendix. J. Clin. Pathol. 2004, 57, 946–949. [Google Scholar] [CrossRef]
- Figueroa-Rivera, I.M.; Santiago-Rivera, L.; Magno, P. Sessile Serrated Adenoma of the Appendix in an Asymptomatic Patient. Clin. Gastroenterol. Hepatol. 2018, 16, A27. [Google Scholar] [CrossRef]
- Yantiss, R.K.; Panczykowski, A.; Misdraji, J.; Hahn, H.P.; Odze, R.D.; Rennert, H.; Chen, Y.T. A comprehensive study of nondysplastic and dysplastic serrated polyps of the vermiform appendix. Am. J. Surg. Pathol. 2007, 31, 1742–1753. [Google Scholar] [CrossRef]
- Misdraji, J. Appendiceal mucinous neoplasms: Controversial issues. Arch. Pathol. Lab. Med. 2010, 134, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Tirumani, S.H.; Fraser-Hill, M.; Auer, R.; Shabana, W.; Walsh, C.; Lee, F.; Ryan, J.G. Mucinous neoplasms of the appendix: A current comprehensive clinicopathologic and imaging review. Cancer Imaging 2013, 13, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Qu, Z.B.; Liu, L.X. Management of pseudomyxoma peritonei. World J. Gastroenterol. 2006, 12, 6124–6127. [Google Scholar] [CrossRef] [PubMed]
- Youssef, H.; Newman, C.; Chandrakumaran, K.; Mohamed, F.; Cecil, T.D.; Moran, B.J. Operative findings, early complications, and long-term survival in 456 patients with pseudomyxoma peritonei syndrome of appendiceal origin. Dis. Colon Rectum 2011, 54, 293–299. [Google Scholar] [CrossRef]
- Carr, N.J.; McCarthy, W.F.; Sobin, L.H. Epithelial noncarcinoid tumors and tumor-like lesions of the appendix. A clinicopathologic study of 184 patients with a multivariate analysis of prognostic factors. Cancer 1995, 75, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Ronnett, B.M.; Yan, H.; Kurman, R.J.; Shmookler, B.M.; Wu, L.; Sugarbaker, P.H. Patients with pseudomyxoma peritonei associated with disseminated peritoneal adenomucinosis have a significantly more favorable prognosis than patients with peritoneal mucinous carcinomatosis. Cancer 2001, 92, 85–91. [Google Scholar] [CrossRef]
- Bradley, R.F.; Stewart, J.H.t.; Russell, G.B.; Levine, E.A.; Geisinger, K.R. Pseudomyxoma peritonei of appendiceal origin: A clinicopathologic analysis of 101 patients uniformly treated at a single institution, with literature review. Am. J. Surg. Pathol. 2006, 30, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Cummins, K.A.; Russell, G.B.; Votanopoulos, K.I.; Shen, P.; Stewart, J.H.; Levine, E.A. Peritoneal dissemination from high-grade appendiceal cancer treated with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). J. Gastrointest. Oncol. 2016, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Mouabbi, J.A.; Malapati, S.J.; Abdalla, A.; Biedny, A.; Hayward, D.; Szpunar, S.; Hadid, T.H.; Berri, R.N.; Kafri, Z. A new prognostic model for high-grade appendiceal mucinous neoplasms with peritoneal carcinomatosis. J. Clin. Oncol. 2020, 38, e16718. [Google Scholar] [CrossRef]
- Overman, M.J.; Asare, E.A.; Compton, C.C.; Hanna, N.N.; Kakar, S.; Kosinski, L.A. Appendix–carcinoma. In AJCC Cancer Staging Manual, 8th ed.; AJCC: Chicago, IL, USA, 2017; pp. 237–250. [Google Scholar]
- Singhi, A.D.; Davison, J.M.; Choudry, H.A.; Pingpank, J.F.; Ahrendt, S.A.; Holtzman, M.P.; Zureikat, A.H.; Zeh, H.J.; Ramalingam, L.; Mantha, G.; et al. GNAS is frequently mutated in both low-grade and high-grade disseminated appendiceal mucinous neoplasms but does not affect survival. Hum. Pathol. 2014, 45, 1737–1743. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Mody, K.; de Abreu, F.B.; Pipas, J.M.; Peterson, J.D.; Gallagher, T.L.; Suriawinata, A.A.; Ripple, G.H.; Hourdequin, K.C.; Smith, K.D.; et al. Molecular profiling of appendiceal epithelial tumors using massively parallel sequencing to identify somatic mutations. Clin. Chem. 2014, 60, 1004–1011. [Google Scholar] [CrossRef]
- Pengelly, R.J.; Rowaiye, B.; Pickard, K.; Moran, B.; Dayal, S.; Tapper, W.; Mirnezami, A.; Cecil, T.; Mohamed, F.; Carr, N.; et al. Analysis of Mutation and Loss of Heterozygosity by Whole-Exome Sequencing Yields Insights into Pseudomyxoma Peritonei. J. Mol. Diagn. 2018, 20, 635–642. [Google Scholar] [CrossRef]
- Alakus, H.; Babicky, M.L.; Ghosh, P.; Yost, S.; Jepsen, K.; Dai, Y.; Arias, A.; Samuels, M.L.; Mose, E.S.; Schwab, R.B.; et al. Genome-wide mutational landscape of mucinous carcinomatosis peritonei of appendiceal origin. Genome Med. 2014, 6, 43. [Google Scholar] [CrossRef]
- Carr, N.J.; Cecil, T.D.; Mohamed, F.; Sobin, L.H.; Sugarbaker, P.H.; González-Moreno, S.; Taflampas, P.; Chapman, S.; Moran, B.J. A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: The results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am. J. Surg. Pathol. 2016, 40, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Cerame, M.A. A 25-year review of adenocarcinoma of the appendix: A frequently perforating carcinoma. Dis. Colon Rectum 1988, 31, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Grover, A.S.; Mittal, S.; Singla, P.; Singh, P.; Kapoor, W. Case Report-Cystadenocarcinoma of appendix with cutaneous fistula-An unusual case presentation. Indian J. Surg. 2005, 67, 267–269. [Google Scholar]
- Karakaya, K.; Barut, F.; Emre, A.U.; Ucan, H.B.; Cakmak, G.K.; Irkorucu, O.; Tascilar, O.; Ustundag, Y.; Comert, M. Appendiceal mucocele: Case reports and review of current literature. World J. Gastroenterol. 2008, 14, 2280–2283. [Google Scholar] [CrossRef]
- Balint, I.; Nad, M.; Kiraly, A.; Bali, O.; Rashed, A.; Vizsy, L. Giant appendix or an appendiceal mucocele? Case report of an 11-year-old child. Interv. Med. Appl. Sci. 2014, 6, 187–190. [Google Scholar] [CrossRef]
- Rosat, A.; Pérez, E.; Sánchez, J.M.; González, O.B.H.; Barrera, M. Vesico-appendiceal fistula secondary to adenocarcinoma of the appendix: A case report and literature review. Pan Afr. Med. J. 2020, 37, 97. [Google Scholar] [CrossRef]
- Ailenei, M.-C.; Călin, R.; Prună, M.; Mitru, C.; Jinga, M.; Ioniţă-Radu, F.; Sandu, C.; Bucurică, S. Silent and Surprising Pathology: Appendix Tumors-Incidental Finding of a Rare Mucinous Appendiceal Adenocarcinoma. Intern. Med. 2019, 16, 67–72. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- Chang, P.; Attiyeh, F.F. Adenocarcinoma of the appendix. Dis. Colon Rectum 1981, 24, 176–180. [Google Scholar] [CrossRef]
- Nitecki, S.S.; Wolff, B.G.; Schlinkert, R.; Sarr, M.G. The natural history of surgically treated primary adenocarcinoma of the appendix. Ann. Surg. 1994, 219, 51–57. [Google Scholar] [CrossRef]
- Cortina, R.; McCormick, J.; Kolm, P.; Perry, R.R. Management and prognosis of adenocarcinoma of the appendix. Dis. Colon Rectum 1995, 38, 848–852. [Google Scholar] [CrossRef] [PubMed]
- Turner, K.M.; Patel, S.H. Low-Risk Non-mucinous Adenocarcinoma of the Appendix: When Is an Appendectomy Enough? Ann. Surg. Oncol. 2022, 29, 2144–2145. [Google Scholar] [CrossRef] [PubMed]
- Kabbani, W.; Houlihan, P.S.; Luthra, R.; Hamilton, S.R.; Rashid, A. Mucinous and nonmucinous appendiceal adenocarcinomas: Different clinicopathological features but similar genetic alterations. Mod. Pathol. 2002, 15, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Taggart, M.W.; Galbincea, J.; Mansfield, P.F.; Fournier, K.F.; Royal, R.E.; Overman, M.J.; Rashid, A.; Abraham, S.C. High-level microsatellite instability in appendiceal carcinomas. Am. J. Surg. Pathol. 2013, 37, 1192–1200. [Google Scholar] [CrossRef]
- Abuoğlu, H.; Yıldız, M.K.; Kaya, B.; Odabaşı, M. Clinicopathological analysis of patients operated for appendiceal mucocele. Turk. J. Trauma Emerg. Surg. 2017, 23, 230–234. [Google Scholar] [CrossRef]
- Mikaeel, R.R.; Young, J.P.; Tapia Rico, G.; Hewett, P.J.; Hardingham, J.E.; Uylaki, W.; Horsnell, M.; Price, T.J. Immunohistochemistry features and molecular pathology of appendiceal neoplasms. Crit. Rev. Clin. Lab. Sci. 2021, 58, 369–384. [Google Scholar] [CrossRef]
- Noguchi, R.; Yano, H.; Gohda, Y.; Suda, R.; Igari, T.; Ohta, Y.; Yamashita, N.; Yamaguchi, K.; Terakado, Y.; Ikenoue, T.; et al. Molecular profiles of high-grade and low-grade pseudomyxoma peritonei. Cancer Med. 2015, 4, 1809–1816. [Google Scholar] [CrossRef]
- Morales-Miranda, A.; Rosado, I.D.; Núñez, C.C.; Montero, F.C. Appendiceal carcinoma associated with microsatellite instability. Mol. Clin. Oncol. 2018, 8, 694–698. [Google Scholar] [CrossRef]
- McDonald, S.J.; Lee, F.; Dean, N.; Ridley, L.J.; Stewart, P. Fistulae involving the appendix: A systematic review of the literature. ANZ J. Surg. 2020, 90, 1878–1887. [Google Scholar] [CrossRef]
- Shetty, S.; Natarajan, B.; Thomas, P.; Govindarajan, V.; Sharma, P.; Loggie, B. Proposed Classification of Pseudomyxoma Peritonei: Influence of Signet Ring Cells on Survival. Am. Surg. 2013, 79, 1171–1176. [Google Scholar] [CrossRef]
- Benesch, M.G.K.; Mathieson, A. Epidemiology of signet ring cell adenocarcinomas. Cancers 2020, 12, 1544. [Google Scholar] [CrossRef] [PubMed]
- Davison, J.M.; Choudry, H.A.; Pingpank, J.F.; Ahrendt, S.A.; Holtzman, M.P.; Zureikat, A.H.; Zeh, H.J.; Ramalingam, L.; Zhu, B.; Nikiforova, M.; et al. Clinicopathologic and molecular analysis of disseminated appendiceal mucinous neoplasms: Identification of factors predicting survival and proposed criteria for a three-tiered assessment of tumor grade. Mod. Pathol. 2014, 27, 1521–1539. [Google Scholar] [CrossRef] [PubMed]
- Subbuswamy, S.G.; Gibbs, N.M.; Ross, C.F.; Morson, B.C. Goblet cell carcinoid of the appendix. Cancer 1974, 34, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Kanthan, R.; Saxena, A.; Kanthan, S.C. Goblet cell carcinoids of the appendix: Immunophenotype and ultrastructural study. Arch. Pathol. Lab. Med. 2001, 125, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Taggart, M.W.; Abraham, S.C.; Overman, M.J.; Mansfield, P.F.; Rashid, A. Goblet cell carcinoid tumor, mixed goblet cell carcinoid-adenocarcinoma, and adenocarcinoma of the appendix: Comparison of clinicopathologic features and prognosis. Arch. Pathol. Lab. Med. 2015, 139, 782–790. [Google Scholar] [CrossRef]
- Yozu, M.; Johncilla, M.E.; Srivastava, A.; Ryan, D.P.; Cusack, J.C.; Doyle, L.; Setia, N.; Yang, M.; Lauwers, G.Y.; Odze, R.D.; et al. Histologic and outcome study supports reclassifying appendiceal goblet cell carcinoids as goblet cell adenocarcinomas, and grading and staging similarly to colonic adenocarcinomas. Am. J. Surg. Pathol. 2018, 42, 898–910. [Google Scholar] [CrossRef] [PubMed]
- Burke, A.P.; Sobin, L.H.; Federspiel, B.H.; Shekitka, K.M.; Helwig, E.B. Goblet cell carcinoids and related tumors of the vermiform appendix. Am. J. Clin. Pathol. 1990, 94, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Blessing, K.; Kerr, K.; Chetty, U.; Gilmour, H. Goblet cell carcinoid of the appendix. Gut 1990, 31, 322–324. [Google Scholar] [CrossRef]
- Holt, N.; Grønbæk, H. Goblet cell carcinoids of the appendix. Sci. World J. 2013, 2013, 543696. [Google Scholar] [CrossRef]
- Roy, P.; Chetty, R. Goblet cell carcinoid tumors of the appendix: An overview. World J. Gastrointest. Oncol. 2010, 2, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Sigley, K.; Franklin, M.; Welch, S. Appendiceal goblet cell adenocarcinoma case report and review of the literature. Cureus 2021, 13, e13511. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, G.; Jensen, K.; Saligram, S.; Sachdev, T.P.; Arekapudi, S.R. Goblet cell carcinoid of the appendix - diagnostic challenges and treatment updates: A case report and review of the literature. J. Med. Case Rep. 2018, 12, 275. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.H.; Shia, J.; Soslow, R.A.; Dhall, D.; Wong, W.D.; O’Reilly, E.; Qin, J.; Paty, P.; Weiser, M.R.; Guillem, J.; et al. Pathologic classification and clinical behavior of the spectrum of goblet cell carcinoid tumors of the appendix. Am. J. Surg. Pathol. 2008, 32, 1429–1443. [Google Scholar] [CrossRef] [PubMed]
- Radomski, M.; Pai, R.K.; Shuai, Y.; Ramalingam, L.; Jones, H.; Holtzman, M.P.; Ahrendt, S.A.; Pingpank, J.F.; Zeh, H.J.; Bartlett, D.L.; et al. Curative Surgical Resection as a Component of Multimodality Therapy for Peritoneal Metastases from Goblet Cell Carcinoids. Ann. Surg. Oncol. 2016, 23, 4338–4343. [Google Scholar] [CrossRef] [PubMed]
- Reid, M.D.; Basturk, O.; Shaib, W.L.; Xue, Y.; Balci, S.; Choi, H.J.; Akkas, G.; Memis, B.; Robinson, B.S.; El-Rayes, B.F.; et al. Adenocarcinoma ex-goblet cell carcinoid (appendiceal-type crypt cell adenocarcinoma) is a morphologically distinct entity with highly aggressive behavior and frequent association with peritoneal/intra-abdominal dissemination: An analysis of 77 cases. Mod. Pathol. 2016, 29, 1243–1253. [Google Scholar] [CrossRef]
- Johncilla, M.; Stachler, M.; Misdraji, J.; Lisovsky, M.; Yozu, M.; Lindeman, N.; Lauwers, G.Y.; Odze, R.D.; Srivastava, A. Mutational landscape of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids of the appendix is distinct from typical carcinoids and colorectal adenocarcinomas. Mod. Pathol. 2018, 31, 989–996. [Google Scholar] [CrossRef] [PubMed]
- Arai, H.; Baca, Y.; Battaglin, F.; Kawanishi, N.; Wang, J.; Soni, S.; Zhang, W.; Millstein, J.; Johnston, C.; Goldberg, R.M.; et al. Molecular Characterization of Appendiceal Goblet Cell Carcinoid. Mol. Cancer Ther. 2020, 19, 2634–2640. [Google Scholar] [CrossRef] [PubMed]
- Ramnani, D.M.; Wistuba, I.I.; Behrens, C.; Gazdar, A.F.; Sobin, L.H.; Albores-Saavedra, J. K-ras and p53 mutations in the pathogenesis of classical and goblet cell carcinoids of the appendix. Cancer 1999, 86, 14–21. [Google Scholar] [CrossRef]
- Jesinghaus, M.; Konukiewitz, B.; Foersch, S.; Stenzinger, A.; Steiger, K.; Muckenhuber, A.; Groß, C.; Mollenhauer, M.; Roth, W.; Detlefsen, S.; et al. Appendiceal goblet cell carcinoids and adenocarcinomas ex-goblet cell carcinoid are genetically distinct from primary colorectal-type adenocarcinoma of the appendix. Mod. Pathol. 2018, 31, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Zhan, T.; Rindtorff, N.; Boutros, M. Wnt signaling in cancer. Oncogene 2017, 36, 1461–1473. [Google Scholar] [CrossRef]
- Wen, K.W.; Grenert, J.P.; Joseph, N.M.; Shafizadeh, N.; Huang, A.; Hosseini, M.; Kakar, S. Genomic profile of appendiceal goblet cell carcinoid is distinct compared to appendiceal neuroendocrine tumor and conventional adenocarcinoma. Hum. Pathol. 2018, 77, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Volante, M.; Grillo, F.; Massa, F.; Maletta, F.; Mastracci, L.; Campora, M.; Ferro, J.; Vanoli, A.; Papotti, M. Neuroendocrine neoplasms of the appendix, colon and rectum. Pathologica 2021, 113, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Shibahara, Y.; Krzyzanowska, M.; Vajpeyi, R. Appendiceal Well-Differentiated Neuroendocrine Tumors: A Single-Center Experience and New Insights into the Effective Use of Immunohistochemistry. Int. J. Surg. Pathol. 2023, 31, 252–259. [Google Scholar] [CrossRef]
- Pape, U.F.; Niederle, B.; Costa, F.; Gross, D.; Kelestimur, F.; Kianmanesh, R.; Knigge, U.; Öberg, K.; Pavel, M.; Perren, A.; et al. ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (excluding goblet cell carcinomas). Neuroendocrinology 2016, 103, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- de Lambert, G.; Lardy, H.; Martelli, H.; Orbach, D.; Gauthier, F.; Guérin, F. Surgical management of neuroendocrine tumors of the appendix in children and adolescents: A retrospective french multicenter study of 114 cases. Pediatr. Blood Cancer 2016, 63, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Henderson, L.; Fehily, C.; Folaranmi, S.; Kelsey, A.; McPartland, J.; Jawaid, W.B.; Craigie, R.; Losty, P.D. Management and outcome of neuroendocrine tumours of the appendix-a two centre UK experience. J. Pediatr. Surg. 2014, 49, 1513–1517. [Google Scholar] [CrossRef]
- Morais, C.; Silva, E.; Brandão, P.N.; Correia, R.; Foreid, S.; Valente, V. Neuroendocrine tumor of the appendix—A case report and review of the literature. J. Surg. Case Rep. 2019, 2019, rjz086. [Google Scholar] [CrossRef]
- Panek, M.; Szymczak, M.; Stepaniuk, M.; Górecki, W.; Gawłowska-Marciniak, A.; Wolak, P.; Zbyrad, D.; Rybkiewicz, M.; Chrobak, K.; Noparlik, R. Radical surgical treatment of neuroendocrine tumors of the appendix in children—A Polish multicenter study. Arch. Med. Sci. 2021, 17, 1128–1131. [Google Scholar] [CrossRef] [PubMed]
- de Nova, J.L.M.; Hernando, J.; Núñez, M.S.; Benítez, G.T.V.; Ibáñez, E.M.T.; del Olmo García, M.I.; Barriuso, J.; Capdevila, J.; Martín-Pérez, E. Management of incidentally discovered appendiceal neuroendocrine tumors after an appendicectomy. World J. Gastroenterol. 2022, 28, 1304–1314. [Google Scholar] [CrossRef] [PubMed]
- Clementi, M.; Pietroletti, R.; Ciarrocchi, A.; d’Ascanio, F.; Rindi, G.; Carlei, F. Appendiceal Neuroendocrine Tumors and Anorectal Melanoma. In Tumor Progression and Metastasis; Ahmed, L., Karine, C.-S., Eds.; IntechOpen: Rijeka, Croatia, 2020; p. 5. [Google Scholar]
- Modlin, I.M.; Sandor, A. An analysis of 8305 cases of carcinoid tumors. Cancer 1997, 79, 813–829. [Google Scholar] [CrossRef]
- Murray, S.E.; Lloyd, R.V.; Sippel, R.S.; Chen, H.; Oltmann, S.C. Postoperative surveillance of small appendiceal carcinoid tumors. Am. J. Surg. 2014, 207, 342–345, discussion 345. [Google Scholar] [CrossRef]
- Sarshekeh, A.M.; Advani, S.; Halperin, D.M.; Conrad, C.; Shen, C.; Yao, J.C.; Dasari, A. Regional lymph node involvement and outcomes in appendiceal neuroendocrine tumors: A SEER database analysis. Oncotarget 2017, 8, 99541–99551. [Google Scholar] [CrossRef] [PubMed]
- Landry, J.P.; Voros, B.A.; Ramirez, R.A.; Boudreaux, J.P.; Woltering, E.A.; Thiagarajan, R. Management of Appendiceal Neuroendocrine Tumors: Metastatic Potential of Small Tumors. Ann. Surg. Oncol. 2021, 28, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Rault-Petit, B.; Cao, C.D.; Guyétant, S.; Guimbaud, R.; Rohmer, V.; Julié, C.; Baudin, E.; Goichot, B.; Coriat, R.; Tabarin, A.; et al. Current Management and Predictive Factors of Lymph Node Metastasis of Appendix Neuroendocrine Tumors: A National Study from the French Group of Endocrine Tumors (GTE). Ann. Surg. 2019, 270, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Alexandraki, K.I.; Kaltsas, G.A.; Grozinsky-Glasberg, S.; Chatzellis, E.; Grossman, A.B. Appendiceal neuroendocrine neoplasms: Diagnosis and management. Endocr.-Relat. Cancer 2016, 23, R27–R41. [Google Scholar] [CrossRef]
- Moris, D.; Tsilimigras, D.I.; Vagios, S.; Ntanasis-Stathopoulos, I.; Karachaliou, G.S.; Papalampros, A.; Alexandrou, A.; Blazer, D.G., 3rd; Felekouras, E. Neuroendocrine Neoplasms of the Appendix: A Review of the Literature. Anticancer Res. 2018, 38, 601–611. [Google Scholar] [CrossRef]
- Onyemkpa, C.; Davis, A.; McLeod, M.; Oyasiji, T. Typical carcinoids, goblet cell carcinoids, mixed adenoneuroendocrine carcinomas, neuroendocrine carcinomas and adenocarcinomas of the appendix: A comparative analysis of survival profile and predictors. J. Gastrointest. Oncol. 2019, 10, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Amyand, C. Of an Inguinal rupture, with a pin in the appendix coeci, incrusted stone; and some observations on wounds in the guts. Philos. Trans. R. Soc. 1736, 39, 329–342. [Google Scholar] [CrossRef]
- Podda, M.; Gerardi, C.; Cillara, N.; Fearnhead, N.; Gomes, C.A.; Birindelli, A.; Mulliri, A.; Davies, R.J.; Di Saverio, S. Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: A systematic review and meta-analysis. Ann. Surg. 2019, 270, 1028–1040. [Google Scholar] [CrossRef] [PubMed]
- Herrod, P.J.J.; Kwok, A.T.; Lobo, D.N. Randomized clinical trials comparing antibiotic therapy with appendicectomy for uncomplicated acute appendicitis: Meta-analysis. BJS Open 2022, 6, zrac100. [Google Scholar] [CrossRef]
- Jaschinski, T.; Mosch, C.; Eikermann, M.; Neugebauer, E.A. Laparoscopic versus open appendectomy in patients with suspected appendicitis: A systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015, 15, 48. [Google Scholar] [CrossRef] [PubMed]
- Nakhamiyayev, V.; Galldin, L.; Chiarello, M.; Lumba, A.; Gorecki, P.J. Laparoscopic appendectomy is the preferred approach for appendicitis: A retrospective review of two practice patterns. Surg. Endosc. 2010, 24, 859–864. [Google Scholar] [CrossRef] [PubMed]
- Di Saverio, S.; Podda, M.; De Simone, B.; Ceresoli, M.; Augustin, G.; Gori, A.; Boermeester, M.; Sartelli, M.; Coccolini, F.; Tarasconi, A.; et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J. Emerg. Surg. 2020, 15, 27. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, S.; Granström, L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br. J. Surg. 1995, 82, 166–169. [Google Scholar] [CrossRef]
- Yadao, S.; Lamture, Y.; Huse, S. Uses of antibiotics alone in case of uncomplicated appendicitis. Cureus 2022, 14, e28488. [Google Scholar] [CrossRef]
- Gorter, R.R.; van der Lee, J.H.; Cense, H.A.; Kneepkens, C.M.; Wijnen, M.H.; In ‘t Hof, K.H.; Offringa, M.; Heij, H.A.; APAC Study Group. Initial antibiotic treatment for acute simple appendicitis in children is safe: Short-term results from a multicenter, prospective cohort study. Surgery 2015, 157, 916–923. [Google Scholar] [CrossRef]
- Tanaka, Y.; Uchida, H.; Kawashima, H.; Fujiogi, M.; Takazawa, S.; Deie, K.; Amano, H. Long-term outcomes of operative versus nonoperative treatment for uncomplicated appendicitis. J. Pediatr. Surg. 2015, 50, 1893–1897. [Google Scholar] [CrossRef]
- Salminen, P.; Tuominen, R.; Paajanen, H.; Rautio, T.; Nordström, P.; Aarnio, M.; Rantanen, T.; Hurme, S.; Mecklin, J.P.; Sand, J.; et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the appac randomized clinical trial. JAMA 2018, 320, 1259–1265. [Google Scholar] [CrossRef]
- CODA Collaborative; Flum, D.R.; Davidson, G.H.; Monsell, S.E.; Shapiro, N.I.; Odom, S.R.; Sanchez, S.E.; Drake, F.T.; Fischkoff, K.; Johnson, J.; et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N. Engl. J. Med. 2020, 383, 1907–1919. [Google Scholar] [CrossRef]
- Coccolini, F.; Fugazzola, P.; Sartelli, M.; Cicuttin, E.; Sibilla, M.G.; Leandro, G.; De’ Angelis, G.L.; Gaiani, F.; Mario, F.D.; Tomasoni, M.; et al. Conservative treatment of acute appendicitis. Acta Biomed. 2018, 89, 119–134. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.; Du, Z.; Zhou, X. Endoscopic retrograde appendicitis therapy for management of acute appendicitis. Surg. Endosc. 2022, 36, 2480–2487. [Google Scholar] [CrossRef]
- Ullah, S.; Ali, F.S.; Shi, M.; Zhang, J.-Y.; Liu, B.-R. Is it time for global adoption endoscopic retrograde appendicitis therapy of acute appendicitis? Clin. Res. Hepatol. Gastroenterol. 2022, 46, 102049. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Sun, P.; Jiang, M.; Zhen, Z.; Liu, J.; Ye, M.; Huang, W. Endoscopic retrograde appendicitis therapy versus laparoscopic appendectomy versus open appendectomy for acute appendicitis: A pilot study. BMC Gastroenterol. 2022, 22, 63. [Google Scholar] [CrossRef]
- Enblad, M.; Birgisson, H.; Ekbom, A.; Sandin, F.; Graf, W. Increased incidence of bowel cancer after non-surgical treatment of appendicitis. Eur. J. Surg. Oncol. 2017, 43, 2067–2075. [Google Scholar] [CrossRef] [PubMed]
- Bailey, H. The Ochsner-Sherren (delayed) treatment of acute appendicitis: Indications and technique. Br. Med. J. 1930, 1, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Coldrey, E. Five years of conservative treatment of acute appendicitis. J. Int. Coll. Surg. 1959, 32, 255–261. [Google Scholar]
- Harper, M.M.; Kim, J.; Pandalai, P.K. Current trends in cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal disease from appendiceal and colorectal malignancies. J. Clin. Med. 2022, 11, 2840. [Google Scholar] [CrossRef]
- de Bree, E.; Michelakis, D.; Stamatiou, D.; Romanos, J.; Zoras, O. Pharmacological principles of intraperitoneal and bidirectional chemotherapy. Pleura Peritoneum. 2017, 2, 47–62. [Google Scholar] [CrossRef]
- Yantiss, R.K.; Shia, J.; Klimstra, D.S.; Hahn, H.P.; Odze, R.D.; Misdraji, J. Prognostic significance of localized extra-appendiceal mucin deposition in appendiceal mucinous neoplasms. Am. J. Surg. Pathol. 2009, 33, 248–255. [Google Scholar] [CrossRef]
- Lin, Y.L.; Xu, D.Z.; Li, X.B.; Yan, F.C.; Xu, H.B.; Peng, Z.; Li, Y. Consensuses and controversies on pseudomyxoma peritonei: A review of the published consensus statements and guidelines. Orphanet J. Rare Dis. 2021, 16, 85. [Google Scholar] [CrossRef] [PubMed]
- Bijelic, L.; Kumar, A.S.; Stuart, O.A.; Sugarbaker, P.H. Systemic chemotherapy prior to cytoreductive surgery and HIPEC for carcinomatosis from appendix cancer: Impact on perioperative outcomes and short-term survival. Gastroenterol. Res. Pract. 2012, 2012, 163284. [Google Scholar] [CrossRef]
- Blackham, A.U.; Swett, K.; Eng, C.; Sirintrapun, J.; Bergman, S.; Geisinger, K.R.; Votanopoulos, K.; Stewart, J.H.; Shen, P.; Levine, E.A. Perioperative systemic chemotherapy for appendiceal mucinous carcinoma peritonei treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J. Surg. Oncol. 2014, 109, 740–745. [Google Scholar] [CrossRef]
- Lu, P.; Fields, A.C.; Meyerhardt, J.A.; Davids, J.S.; Shabat, G.; Bleday, R.; Goldberg, J.E.; Nash, G.M.; Melnitchouk, N. Systemic chemotherapy and survival in patients with metastatic low-grade appendiceal mucinous adenocarcinoma. J. Surg. Oncol. 2019, 120, 446–451. [Google Scholar] [CrossRef]
- Chicago Consensus Working Group. The Chicago Consensus on peritoneal surface malignancies: Management of appendiceal neoplasms. Cancer 2020, 126, 2525–2533. [Google Scholar] [CrossRef] [PubMed]
- Turaga, K.K.; Pappas, S.; Gamblin, T.C. Right hemicolectomy for mucinous adenocarcinoma of the appendix: Just right or too much? Ann. Surg. Oncol. 2013, 20, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Li, Q.; Chen, W. Chemotherapy in the treatment of different histological types of appendiceal cancers: A SEER based study. BMC Cancer 2021, 21, 778. [Google Scholar] [CrossRef]
- Kaakour, D.; Ward, G.; Senthil, M.; Dayyani, F. Durable response after repeat cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) in a patient with extensive mucinous adenocarcinoma of the appendix. Diseases 2023, 11, 60. [Google Scholar] [CrossRef]
- Boudreaux, J.P.; Klimstra, D.S.; Hassan, M.M.; Woltering, E.A.; Jensen, R.T.; Goldsmith, S.J.; Nutting, C.; Bushnell, D.L.; Caplin, M.E.; Yao, J.C.; et al. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: Well-differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas 2010, 39, 753–766. [Google Scholar] [CrossRef]
- Yu, H.H.; Yonemura, Y.; Hsieh, M.C.; Mizumoto, A.; Wakama, S.; Lu, C.Y. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for appendiceal goblet cell carcinomas with peritoneal carcinomatosis: Results from a single specialized center. Cancer Manag. Res. 2017, 9, 513–523. [Google Scholar] [CrossRef]
- AlMasri, S.; Nassour, I.; Kowalsky, S.J.; Hrebinko, K.; Singhi, A.D.; Lee, K.K.; Choudry, H.A.; Bartlett, D.; Zureikat, A.; Paniccia, A. The Role of adjuvant chemotherapy in non-metastatic goblet cell carcinoid of the appendix: An 11-year experience from the national cancer database. Ann. Surg. Oncol. 2021, 28, 3873–3881. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, S.C.; Gaertner, W.; Stewart, D.; Davids, J.; Alavi, K.; Paquette, I.M.; Steele, S.R.; Feingold, D.L. The American Society of Colon and Rectal Surgeons, Clinical Practice Guidelines for the Management of Appendiceal Neoplasms. Dis. Colon Rectum 2019, 62, 1425–1438. [Google Scholar] [CrossRef] [PubMed]
- Grotz, T.E.; Overman, M.J.; Eng, C.; Raghav, K.P.; Royal, R.E.; Mansfield, P.F.; Mann, G.N.; Robinson, K.A.; Beaty, K.A.; Rafeeq, S.; et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for moderately and poorly differentiated appendiceal adenocarcinoma: Survival outcomes and patient selection. Ann. Surg. Oncol. 2017, 24, 2646–2654. [Google Scholar] [CrossRef]
- Aziz, O.; Jaradat, I.; Chakrabarty, B.; Selvasekar, C.R.; Fulford, P.E.; Saunders, M.P.; Renehan, A.G.; Wilson, M.S.; O’Dwyer, S.T. Predicting survival after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for appendix adenocarcinoma. Dis. Colon Rectum 2018, 61, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Ramirez, F.; Gushchin, V.; Sittig, M.; King, M.C.; Baron, E.; Nikiforchin, A.; Nieroda, C.; Sardi, A. Iterative cytoreduction and hyperthermic intraperitoneal chemotherapy for recurrent mucinous adenocarcinoma of the appendix. Ann. Surg. Oncol. 2022, 29, 3390–3401. [Google Scholar] [CrossRef]
- Lieu, C.H.; Lambert, L.A.; Wolff, R.A.; Eng, C.; Zhang, N.; Wen, S.; Rafeeq, S.; Taggart, M.; Fournier, K.; Royal, R.; et al. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann. Oncol. 2012, 23, 652–658. [Google Scholar] [CrossRef]
- Kelly, K.J. Management of appendix cancer. Clin. Colon Rectal Surg. 2015, 28, 247–255. [Google Scholar] [CrossRef]
- Mohamed, A.; Wu, S.; Hamid, M.; Mahipal, A.; Cjakrabarti, S.; Bajor, D.; Selfridge, J.E.; Asa, S.L. Management of appendix neuroendocrine neoplasms: Insights on the current guidelines. Cancers 2022, 15, 295. [Google Scholar] [CrossRef]
- Pavel, M.; Baudin, E.; Couvelard, A.; Krenning, E.; Öberg, K.; Steinmüller, T.; Anlauf, M.; Wiedenmann, B.; Salazar, R.; Barcelona Consensus Conference participants. ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2012, 95, 157–176. [Google Scholar] [CrossRef]
- Howe, J.R. It may not be too little or too late: Resecting primary small bowel neuroendocrine tumors in the presence of metastatic disease. Ann. Surg. Oncol. 2020, 27, 2583–2585. [Google Scholar] [CrossRef]
- Kessler, J.; Singh, G.; Ituarte, P.H.G.; Allen, R.; Chang, S.; Li, D. A comparison of liver-directed therapy and systemic therapy for the treatment of liver metastases in patients with gastrointestinal neuroendocrine tumors: Analysis of the california cancer registry. J. Vasc. Interv. Radiol. 2021, 32, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Rinke, A.; Müller, H.H.; Schade-Brittinger, C.; Klose, K.J.; Barth, P.; Wied, M.; Mayer, C.; Aminossadati, B.; Pape, U.F.; Bläker, M.; et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: A report from the PROMID Study Group. J. Clin. Oncol. 2009, 27, 4656–4663. [Google Scholar] [CrossRef]
- Spada, F.; Antonuzzo, L.; Marconcini, R.; Radice, D.; Antonuzzo, A.; Ricci, S.; Di Costanzo, F.; Fontana, A.; Gelsomino, F.; Luppi, G.; et al. Oxaliplatin-based chemotherapy in advanced neuroendocrine tumors: Clinical outcomes and preliminary correlation with biological factors. Neuroendocrinology 2016, 103, 806–814. [Google Scholar] [CrossRef]
- Faure, M.; Niccoli, P.; Autret, A.; Cavaglione, G.; Mineur, L.; Raoul, J.L. Systemic chemotherapy with FOLFOX in metastatic grade 1/2 neuroendocrine cancer. Mol. Clin. Oncol. 2017, 6, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Sahu, A.; Jefford, M.; Lai-Kwon, J.; Thai, A.; Hicks, R.J.; Michael, M. CAPTEM in metastatic well-differentiated intermediate to high grade neuroendocrine tumors: A single centre experience. J. Oncol. 2019, 2019, 9032753. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, G.; Mitsuma, A.; Sunagawa, Y.; Ishigure, K.; Yokoyama, H.; Matsui, T.; Nakayama, H.; Nakata, K.; Ishiyama, A.; Asada, T.; et al. Randomized phase ii trial of capox plus bevacizumab and capiri plus bevacizumab as first-line treatment for japanese patients with metastatic colorectal cancer (CCOG-1201 study). Oncologist 2018, 23, 919–927. [Google Scholar] [CrossRef]
- Maiello, E.; Di Maggio, G.; Cordio, S.; Cinieri, S.; Giuliani, F.; Pisconti, S.; Rinaldi, A.; Febbraro, A.; Latiano, T.P.; Aieta, M.; et al. Bevacizumab in combination with either folfox-4 or xelox-2 in first-line treatment of patients with metastatic colorectal cancer: A multicenter randomized phase ii trial of the gruppo oncologico dell’italia meridionale (GOIM 2802). Clin. Colorectal Cancer 2020, 19, 109–115. [Google Scholar] [CrossRef]
- Patel, B.K.; Singh, A.R.; Umamahesweran, S.; Badhe, B.A.; Singh, A. Vermiform appendix and the potential for missed pathologies. Cureus 2022, 14, e25055. [Google Scholar] [CrossRef]
- Al-Tamimi, S.N.A.; Al-Bayati, N.Y. Investigate the appendicitis companied with parasitic infection in patients attending the baquba teaching hospital undergoing an appendix removal, diyala province. Biochem. Cell. Arch. 2022, 22, 431–434. [Google Scholar]
- Chitnis, A.; Yousefi Azimi, D.; Sabri, S.; Dhebri, A. Enterobius vermicularis: A parasitic cause of appendicular colic. Cureus 2020, 12, e8524. [Google Scholar] [CrossRef]
- Zarbaliyev, E.; Celik, S. Parasitic appendicitis: A novel laparoscopic approach for the prevention of peritoneal contamination. Can. J. Infect. Dis. Med. Microbiol. 2018, 2018, 3238061. [Google Scholar] [CrossRef]
- Alshihmani, S.H.A. Acute appendicitis due to infection with Enterobius vermicularis, A case report. Ann. Med. Surg. 2022, 80, 104094. [Google Scholar] [CrossRef] [PubMed]
- Mishra, P.P.; Hota, S.; Panda, P.; Satpathi, S. Fungal appendicitis: A case report and review of the literature. J. Cardiovasc. Dis. Res. 2022, 13, 45–50. [Google Scholar]
- Larbcharoensub, N.; Boonsakan, P.; Kanoksil, W.; Wattanatranon, D.; Phongkitkarun, S.; Molagool, S.; Watcharananan, S.P. Fungal appendicitis: A case series and review of the literature. Southeast Asian J. Trop. Med. Public Health 2013, 44, 681–689. [Google Scholar]
- Jung, K.U.; Yoon, K.W.; Do, I.-G.; Lee, D. Aspergillus appendicitis complicating chemotherapy of leukemia: A case report and review of the literature. Int. J. Surg. Case Rep. 2022, 100, 107738. [Google Scholar] [CrossRef] [PubMed]
- Allahqoli, L.; Mazidimoradi, A.; Momenimovahed, Z.; Günther, V.; Ackermann, J.; Salehiniya, H.; Alkatout, I. Appendiceal endometriosis: A comprehensive review of the literature. Diagnostics 2023, 13, 1827. [Google Scholar] [CrossRef]
- Aragone, L.; Pasquini, M.T.; Rebzda, V.S.; Talarico, M.S.; Mihura, M. Appendiceal endometriosis: Case report of a rare differential diagnosis of acute appendicitis. Int. J. Surg. Case Rep. 2023, 105, 107993. [Google Scholar] [CrossRef]
- Samuk, I.; Dlugy, E.; Seguier-Lipszyc, E.; Rootman, M.S.; Nica, A.; Kravarusic, D. Not only appendicitis: Rare appendix disorders manifesting as surgical emergencies in children. Eur. J. Pediatr. 2021, 180, 407–413. [Google Scholar] [CrossRef]
- Ali, A.K.; Ibrahim, H.M.; Sabra, T.A. Appendiceal intussusception requiring ileocecectomy. J. Pediatr. Surg. Case Rep. 2023, 88, 102535. [Google Scholar] [CrossRef]
- Furlong, S.A.; Hart, A.; Lobeck, I.; Furman, M. Recurrent ileocolic intussusception with appendiceal lead point in a 2-year-old child: An etiology to be aware of on ultrasound. Radiol. Case Rep. 2022, 17, 1951–1954. [Google Scholar] [CrossRef]
- Bakrin, N.; Deraco, M.; Glehen, O.; Morris, D.L.; Van der Speeten, K. Cytoreductive Surgery & Perioperative Chemotherapy for Peritoneal Surface Malignancy: Textbook and Video Atlas, 2; Ciné-Med: Woodbury, CT, USA, 2017. [Google Scholar]
- Omohwo, C.; Nieroda, C.A.; Studeman, K.D.; Thieme, H.; Kostuik, P.; Ross, A.S.; Holter, D.R.; Gushchin, V.; Merriman, B.; Sardi, A. Complete cytoreduction offers longterm survival in patients with peritoneal carcinomatosis from appendiceal tumors of unfavorable histology. J. Am. Coll. Surg. 2009, 209, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Klaver, C.E.L.; Wisselink, D.D.; Punt, C.J.A.; Snaebjornsson, P.; Crezee, J.; Aalbers, A.G.J.; Brandt, A.; Bremers, A.J.A.; Burger, J.W.A.; Fabry, H.F.J.; et al. Adjuvant hyperthermic intraperitoneal chemotherapy in patients with locally advanced colon cancer (COLOPEC): A multicentre, open-label, randomised trial. Lancet Gastroenterol. Hepatol. 2019, 4, 761–770. [Google Scholar] [CrossRef] [PubMed]
- Goéré, D.; Glehen, O.; Quenet, F.; Guilloit, J.M.; Bereder, J.M.; Lorimier, G.; Thibaudeau, E.; Ghouti, L.; Pinto, A.; Tuech, J.J.; et al. Second-look surgery plus hyperthermic intraperitoneal chemotherapy versus surveillance in patients at high risk of developing colorectal peritoneal metastases (PROPHYLOCHIP-PRODIGE 15): A randomised, phase 3 study. Lancet Oncol. 2020, 21, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Quénet, F.; Elias, D.; Roca, L.; Goéré, D.; Ghouti, L.; Pocard, M.; Facy, O.; Arvieux, C.; Lorimier, G.; Pezet, D.; et al. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy versus cytoreductive surgery alone for colorectal peritoneal metastases (PRODIGE 7): A multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 256–266. [Google Scholar] [CrossRef]
- Faron, M.; Macovei, R.; Goéré, D.; Honoré, C.; Benhaim, L.; Elias, D. Linear relationship of peritoneal cancer index and survival in patients with peritoneal metastases from colorectal cancer. Ann. Surg. Oncol. 2016, 23, 114–119. [Google Scholar] [CrossRef]
| T Category | T Criteria |
|---|---|
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| Tis | Carcinoma in situ (intramucosal carcinoma; invasion of the lamina propria or extension into but not through the muscularis mucosae) |
| Tis (LAMN) | Low-grade appendiceal mucinous neoplasm confined by the muscularis propria. Acellular mucin or mucinous epithelium may invade the muscularis propria. T1 and T2 are not applicable to LAMN. Acellular mucin or mucinous epithelium that extends into the subserosa or serosa should be classified as T3 or T4a, respectively. |
| T1 | Tumor invades the submucosa (through the muscularis mucosa but not into the muscularis propria) |
| T2 | Tumor invades the muscularis propria |
| T3 | Tumor invades through the muscularis propria into the subserosa or the mesoappendix |
| T4 | Tumor invades the visceral peritoneum, including the acellular mucin or mucinous epithelium involving the serosa of the appendix or mesoappendix, and/or directly invades adjacent organs or structures |
| T4a | Tumor invades through the visceral peritoneum, including the acellular mucin or mucinous epithelium involving the serosa of the appendix or serosa of the mesoappendix |
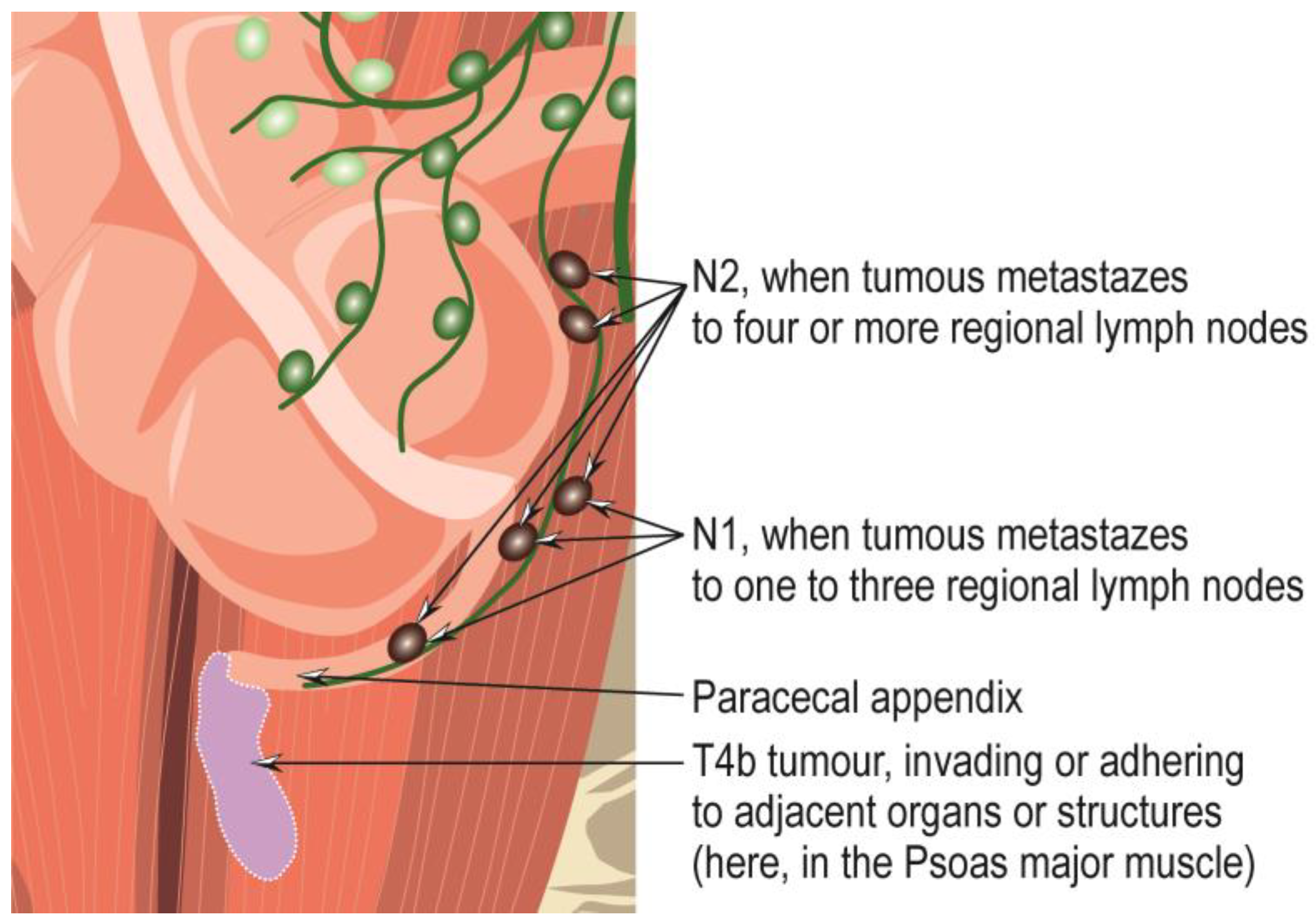
| T4b | Tumor directly invades or adheres to adjacent organs or structures |
| N Category | N Criteria |
|---|---|
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | One to three regional lymph nodes are positive (tumor in lymph node measuring ≥ 0.2 mm), or any number of tumor deposits is present, and all identifiable lymph nodes are negative |
| N1a | One regional lymph node is positive |
| N1b | Two or three regional lymph nodes are positive |
| N1c | No regional lymph nodes are positive, but there are tumor deposits in the subserosa or mesentery |
| N2 | Four or more regional lymph nodes are positive |
| M Category | M Criteria |
|---|---|
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| M1a | Intraperitoneal acellular mucin, without identifiable tumor cells in the disseminated peritoneal mucinous deposits |
| M1b | Intraperitoneal metastasis only, including peritoneal mucinous deposits containing tumor cells |
| M1c | Metastasis to sites other than the peritoneum |
| G | G Definition |
|---|---|
| GX | Grade cannot be assessed |
| G1 | Well-differentiated |
| G2 | Moderately differentiated |
| G3 | Poorly differentiated |
| TNM | Grade | Stage Group |
|---|---|---|
| Tis N0 M0 | - | 0 |
| Tis(LAMN) N0 M0 | - | 0 |
| T1 N0 M0 | - | I |
| T2 N0 M0 | - | I |
| T3 N0 M0 | - | IIA |
| T4a N0 M0 | - | IIB |
| T4b N0 M0 | - | IIC |
| T1 N1 M0 | - | IIIA |
| T2 N1 M0 | - | IIIA |
| T3 N1 M0 | - | IIIB |
| T4 N1 M0 | - | IIIB |
| T(any) N2 M0 | - | IIIC |
| T(any) N(any) M1a | - | IVA |
| T(any) N(any) M1b | G1 | IVA |
| T(any) N(any) M1b | G2, G3, or GX | IVB |
| T(any) N(any) M1c | Any G | IVC |
| T Category | T Criteria |
|---|---|
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| T1 | Tumor 2 cm or less in greatest dimension |
| T2 | Tumor more than 2 cm but less than or equal to 4 cm |
| T3 | Tumor more than 4 cm or with subserosal invasion or involvement of the mesoappendix |
| T4 | Tumor perforates the peritoneum or directly invades other adjacent organs or structures (excluding direct mural extension to adjacent subserosa of adjacent bowel), e.g., abdominal wall and skeletal muscle |
| N Category | N Criteria |
|---|---|
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Regional lymph node metastasis |
| M Category | M Criteria |
|---|---|
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| M1a | Metastasis confined to liver |
| M1b | Metastases in at least one extrahepatic site (e.g., lung, ovary, nonregional lymph node, peritoneum, bone) |
| M1c | Both hepatic and extrahepatic metastases |
| TNM | Stage Group |
|---|---|
| T(X, 0) N(X, 0, 1) M1 | IV |
| T1 N0 M0 | I |
| T1 N1 M0 | III |
| T1 N(X, 0, 1) M1 | IV |
| T2 N0 M0 | II |
| T2 N1 M0 | III |
| T2 N(X, 0, 1) M1 | IV |
| T3 N0 M0 | II |
| T3 N1 M0 | III |
| T3 N(X, 0, 1) M1 | IV |
| T4 N0 M0 | III |
| T4 N1 M0 | III |
| T4 N(X, 0, 1) M1 | IV |
| Therapy | Recurrence Rate | Benefits | Limitations/Complications |
|---|---|---|---|
| Surgical resection (open appendectomy) | None [119] | Effectiveness and safety in preventing occurrence [119] | Limitations: - Complications: postoperative bleeding, wound infection, intra-abdominal abscess, and paralytic ileus, with a rate of 11.1% [120,121] |
| Surgical resection (laparoscopic appendectomy) | None [119] | Effectiveness and safety in preventing occurrence [119] | Limitations: - Complications: postoperative bleeding, wound infection, intra-abdominal abscess, and paralytic ileus, with a rate of 8.7% [120,121] |
| Antibiotic administration | High [122] 5% during the one-year follow-up period [123] 2–14% for initial antibiotic treatment, during follow-up [124] 28.6% % after an average of 4.3 years of follow-up, especially when appendicoliths are present [125] 34.0% at 2 years, 35.2% at 3 years, 37.1% at 4 years, and 39.1% at 5 years [126] | Avoiding surgical approach in most cases [122,123,126,127] Less pain, less analgesia [122] Low hospitalization rate [127] Effectiveness in about 60% of cases of simple appendicitis [123] | Limitations: applies only to uncomplicated cases [128] Complications: perforation and pelvic sepsis [126], occurring in 8.1 per 100 participants, being higher for those with appendicoliths (20.2 per 100 participants) compared to those with no appendicoliths (3.7 per 100 participants) [127] Some cases (29%) need appendectomy after 90 days [127] |
| Endoscopic retrograde appendicitis therapy | 2.86% during the first six months of postoperative follow-up [129] 5 to 6.2% [130] | Nonoperative and minimally invasive, safe, and effective endoscopic treatment [129,131] | Limitations: applies to uncomplicated cases [131] Complications: increased risk of bowel cancer [132] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Constantin, M.; Petrescu, L.; Mătanie, C.; Vrancianu, C.O.; Niculescu, A.-G.; Andronic, O.; Bolocan, A. The Vermiform Appendix and Its Pathologies. Cancers 2023, 15, 3872. https://doi.org/10.3390/cancers15153872
Constantin M, Petrescu L, Mătanie C, Vrancianu CO, Niculescu A-G, Andronic O, Bolocan A. The Vermiform Appendix and Its Pathologies. Cancers. 2023; 15(15):3872. https://doi.org/10.3390/cancers15153872
Chicago/Turabian StyleConstantin, Marian, Livia Petrescu, Cristina Mătanie, Corneliu Ovidiu Vrancianu, Adelina-Gabriela Niculescu, Octavian Andronic, and Alexandra Bolocan. 2023. "The Vermiform Appendix and Its Pathologies" Cancers 15, no. 15: 3872. https://doi.org/10.3390/cancers15153872
APA StyleConstantin, M., Petrescu, L., Mătanie, C., Vrancianu, C. O., Niculescu, A.-G., Andronic, O., & Bolocan, A. (2023). The Vermiform Appendix and Its Pathologies. Cancers, 15(15), 3872. https://doi.org/10.3390/cancers15153872









