Advances in Genomic Data and Biomarkers: Revolutionizing NSCLC Diagnosis and Treatment
Abstract
Simple Summary
Abstract
1. Introduction
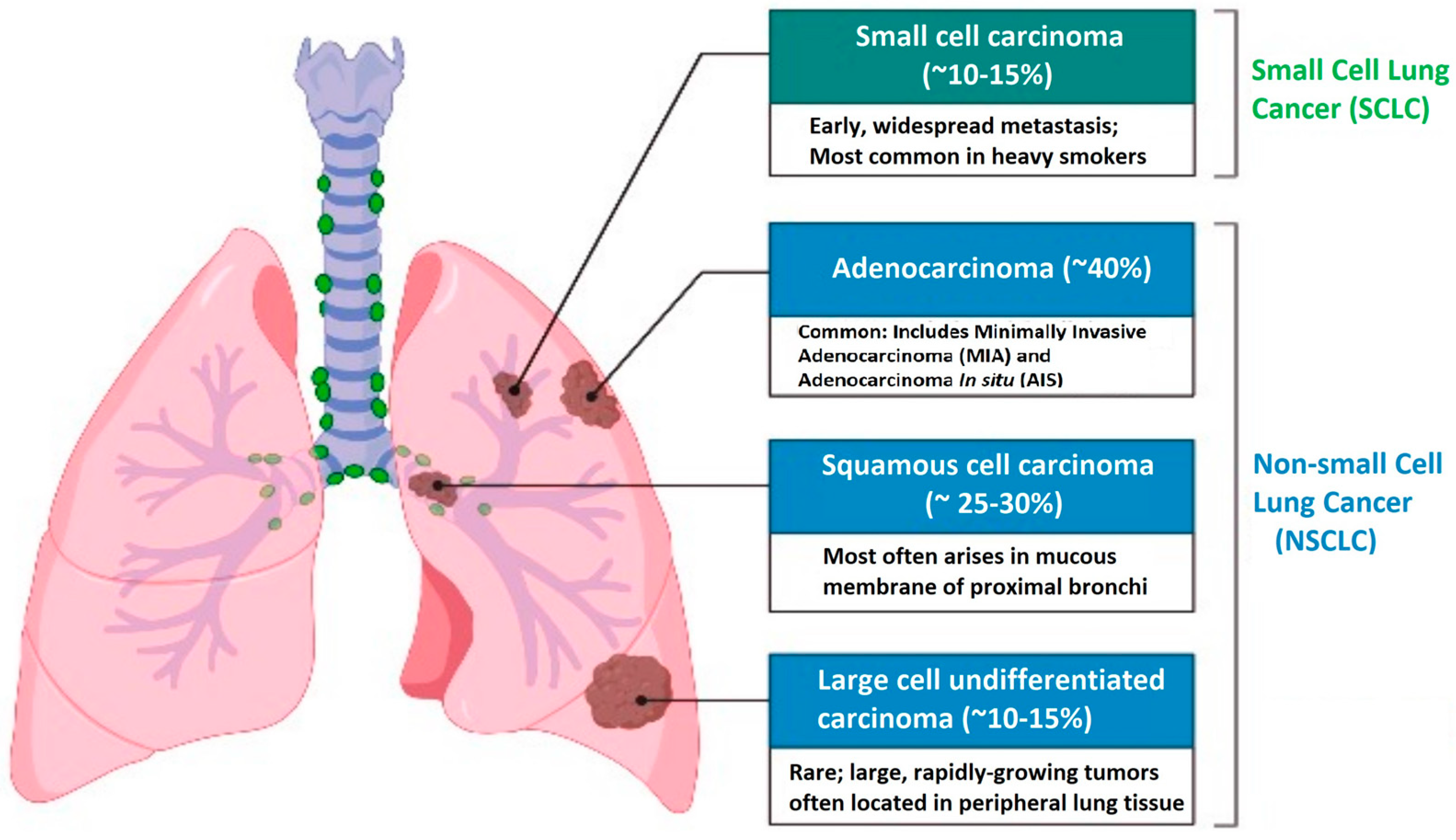
2. Non-Small Cell Lung Cancer
2.1. Risk Factors and Epidemiology
2.2. Pathophysiology, Histology, and Classification
2.3. Resistance to Medications and Immunotherapy in NSCLC: Mechanisms and Therapeutic Strategies
2.4. Diagnosis and Treatment
3. Precision Medicine and Biomarkers
3.1. The Impact of Precision Medicine
3.2. Types of Biomarkers
- Genetic biomarkers: include variations in DNA, such as genetic mutations or single nucleotide polymorphisms (SNPs).
- Protein biomarkers: refer to specific proteins or protein profiles that can be measured in biological samples, such as blood or urine.
- Lipid biomarkers: are related to the lipids or fats present in the body and may be associated with cardiovascular or metabolic diseases.
- Metabolic biomarkers: refer to products or intermediates of metabolism that can be measured in biological samples.
- Diagnostic biomarkers: used to confirm or rule out the presence of a specific disease or medical condition.
- Prognostic biomarkers: used to predict the progression of a disease or response to treatment.
- Treatment response biomarkers: used to evaluate the effectiveness of a specific treatment and adjust its dosage or duration.
- Disease progression biomarkers: used to monitor the advancement of a disease and evaluate its severity.
- Predictive biomarkers: used to predict the likelihood of a patient’s response to a specific treatment before it is administered. These biomarkers are based on biological characteristics or signals that indicate the probability of a patient responding favorably to a particular treatment.
- Blood biomarkers: found in the blood and easily accessible through blood analysis.
- Urinary biomarkers: found in urine and used to assess renal function and detect urinary tract diseases.
- Tissue biomarkers: found in specific tissues and may require biopsies or imaging studies for their retrieval.
3.3. NSCLC Cancer Biomarkers
3.4. Novel NSCLC Cancer Biomarkers
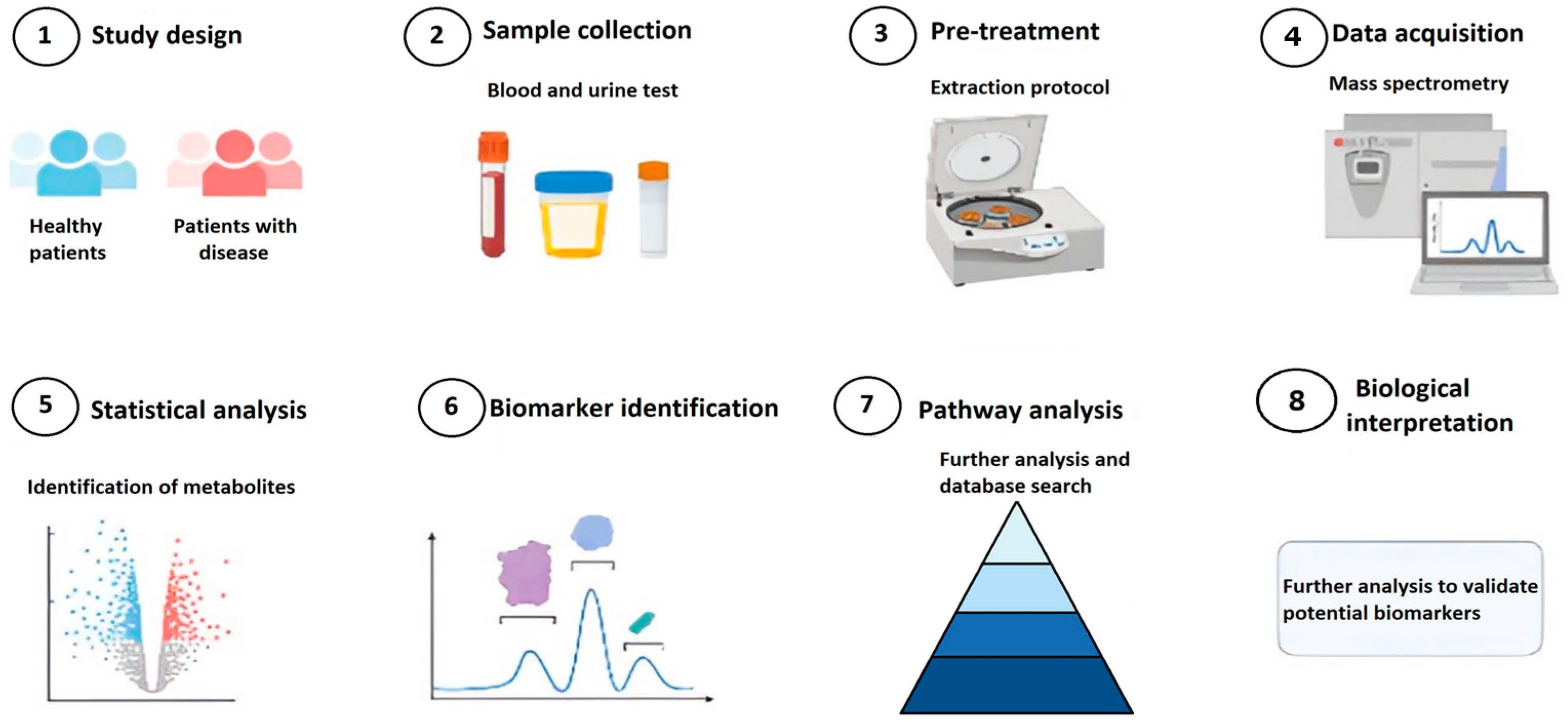
4. Methodology for Discovering Novel Biomarkers
4.1. Artificial Intelligence Algorithms
4.2. Bioinformatics for Biomarkers Prediction
- Genomic data identification: The first step is to gather relevant genomic data for the study. This may include publicly available datasets from genomic databases, such as GenBank or the Human Genome Project Repository, or internally generated data from experiments.
- Data preprocessing: Once the genomic data are obtained, they need to undergo preprocessing to ensure data quality and prepare the data for analysis. This may involve data cleaning, normalization, and the removal of irrelevant or noisy data.
- Gene expression analysis: One of the most common ways to discover biomarkers is through gene expression analysis. This involves comparing gene expression levels between different sample groups, such as samples from patients with and without a particular disease. Techniques such as microarrays or RNA sequencing can be used to measure gene expression.
- Genetic variant analysis: Another strategy is to analyze genetic variants, such as mutations or polymorphisms, and their association with a specific condition. This can be achieved through the analysis of DNA sequencing data, where differences in genetic sequences among different sample groups are sought.
- Data mining and statistical analysis: Once the preprocessed data are available, data mining and statistical analysis techniques can be applied to identify significant patterns and associations. This may include correlation analysis, enrichment analysis of biological pathways, gene interaction network analysis, and classification or clustering analysis.
- Experimental validation: Biomarkers identified through bioinformatic analysis need to be experimentally validated to confirm their clinical relevance. This may involve the use of molecular biology techniques such as real-time PCR, Western blotting, or immunohistochemistry to verify the expression of the biomarkers in additional samples.
- Clinical application: Once validated, the new biomarkers can be used in clinical studies to assess their utility in the diagnosis, prognosis, or treatment response of a specific disease. They can also be valuable for developing personalized therapies based on the presence or absence of certain biomarkers.
- ANLN: ANLN is observed to be overexpressed in multiple tumor types, including pancreatic, brain, breast, and lung cancers. It is involved in cell proliferation, and its inhibition can impede cancer cell division, migration, and invasion. Overexpression of ANLN has been associated with lung adenocarcinoma metastasis, making it a potential target for cancer therapy.
- CDKN3: CDKN3 exhibits overexpression in glioma and cervical cancer and is linked to poorer survival outcomes. Its expression levels fluctuate during the cell cycle, peaking during mitosis. High levels of mitotic CDKN3 expression are often observed in various human cancers.
- CCNB1 and CCNB2: These genes play essential roles in meiotic resumption and have been implicated in tumor cell division, proliferation, and tumor growth in several cancer types, including colorectal, pancreatic, breast, hepatocellular carcinoma, and NSCLC.
- KIF4A: KIF4A is involved in DNA replication and repair processes and promotes cell proliferation. It is associated with tumor size in oral carcinoma and has potential prognostic value in various solid tumors.
- KIF11 and MELK: Both KIF11 and MELK have been identified as oncogenes in multiple cancers and are being investigated as potential targets for cancer treatment in ongoing phase I/II clinical trials.
- CEP55: CEP55 is considered a promising cancer vaccine candidate and serves as a marker for predicting cancer invasion risk, metastasis, and therapeutic response.
- HMMR: HMMR is a microtubule-associated protein that regulates mitosis and meiosis. Aberrant expression of HMMR disrupts the cell division process and is associated with cancer risk and progression across various tumor types.
- ASPM: ASPM has emerged as a predictor of tumor aggressiveness and prognosis in bladder, prostate, and endometrial cancers.
- CENPF: CENPF serves as a proliferative marker for malignant tumor cell growth.
- BUB1: BUB1 is a serine/threonine-protein kinase that plays a critical role in oncogenesis, chromosome arrangement, and spindle assembly.
5. Challenges and Future Perspectives
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| NSCLC | Non-Small Cell Lung Cancer |
| PET | Positron Emission Tomography |
| GEO | Gene Expression Omnibus |
| TCGA | The Cancer Genome Atlas |
| MDS | Multidimensional Scaling |
| UMAP | Uniform Manifold Approximation and Projection |
| TP53 | Tumor Protein 53 |
| EGFR | Epidermal Growth Factor Receptor |
| ALK | Anaplastic Lymphoma Kinase |
| MRI | Magnetic Resonance Imaging |
| CT | Computed Tomography |
| FISH | Fluorescence In Situ Hybridization |
| PCR | Polymerase Chain Reaction |
| IHC | Immunohistochemistry |
| TKIs | Tyrosine Kinase Inhibitors |
| OPN | Osteopontin |
| PI3K/AKT/mTOR | Phosphoinositide 3-kinase/Protein Kinase B/Mammalian Target of Rapamycin |
| RET | Rearranged during Transfection |
| JAK-STAT | Janus Kinase-Signal Transducer and Activator of Transcription |
| RAS/MAPK | Rat Sarcoma/Mitogen-Activated Protein Kinase |
| MET | Mesenchymal Epithelial Transition |
| EMT | Epithelial-Mesenchymal Transition |
| HER2 | Human Epidermal Growth Factor Receptor 2 |
| MEK/ERK | Mitogen-Activated Protein Kinase Kinase/Extracellular Signal-Regulated Kinase |
| BRAF | B-Raf Proto-Oncogene, Serine/Threonine Kinase |
| ROS1 | ROS Proto-Oncogene 1, Receptor Tyrosine Kinase |
| KRAS | Kirsten Rat Sarcoma Viral Oncogene Homolog |
| NTRK | Neurotrophic Tropomyosin Receptor Kinase |
| TME | Tumor Microenvironment |
| ICBs | Immune Checkpoint Inhibitors |
| STK11 | Serine/Threonine Kinase 11 |
| NGS | Next-Generation Sequencing |
| TNM | Tumor, Node, Metastasis |
| FDA | U.S. Food and Drug Administration |
| NIH | National Institutes of Health |
| DNA | Deoxyribonucleic Acid |
| SNPs | Single Nucleotide Polymorphisms |
| FDA-NIH | FDA-NIH Biomarker Working Group |
| PD-L1 | Programmed Death-Ligand 1 |
| PD-1 | Programmed Death-1 |
| NKX2-1 | Thyroid Transcription Factor-1 |
| TTF-1 | Thyroid Transcription Factor-1 |
| NAPSA | Napsin A |
| CYFRA 21-1 | Cytokeratin 19 fragment |
| CEA | Carcinoembryonic Antigen |
| SCCA | Squamous cell carcinoma antigen |
| CA125 | Carbohydrate antigen 125 |
| miRNA | microRNA |
| FGFR1 | Fibroblast Growth Factor Receptor 1 |
| DDR2 | Discoidin domain Receptor 2 |
| m6A | N6-methyladenine |
| SFTA2 | Surfactant Protein A2 |
| ROS1 | ROS Proto-Oncogene 1 |
| ALK | Anaplastic Lymphoma Kinase |
| BRAF | B-Raf Proto-Oncogene |
| NTRK | Neurotrophic Tyrosine Kinase Receptor |
| TIM-3 | T-cell Immunoglobulin and Mucin Domain Containing-3 |
| TMB | Tumor Mutational Burden |
| AMP | Association for Molecular Pathology |
| CAP | College of American Pathologists |
| IASLC | International Association for the Study of Lung Cancer |
| ASCO | American Society of Clinical Oncology |
| ESMO | European Society for Medical Oncology |
| NCCN | National Comprehensive Cancer Network |
| VEGF | Vascular Endothelial Growth Factor |
| TUBB3 | Tubulin Beta-3 |
| KIAA1522 | KIAA1522 protein |
| TGF-β | Transforming Growth Factor Beta |
| LAG-3 | Lymphocyte Activation Gene-3 |
| NLR | Neutrophil-to-Lymphocyte Ratio |
| PLR | Platelet-to-Lymphocyte Ratio |
| PCA | Principal Component Analysis |
| t-SNE | t-Distributed Stochastic Neighbor Embedding |
| SVM | Support Vector Machine |
| qPCR | Quantitative Polymerase Chain Reaction |
| RT-PCR | Reverse Transcription Polymerase Chain Reaction |
| R | Programming language/software for statistical computing and graphics |
| LIMMA | Linear Models for Microarray Data Analysis |
| STRING | Search Tool for the Retrieval of Interacting Genes/Proteins |
| Cytoscape | Software platform for visualizing molecular interaction networks |
| DAVID | Database for Annotation, Visualization, and Integrated Discovery |
| KEGG | Kyoto Encyclopedia of Genes and Genomes |
| GO | Gene Ontology |
| GEPIA | Gene Expression Profiling Interactive Analysis |
| HPA | The Human Protein Atlas |
References
- Cancer Today. Available online: http://gco.iarc.fr/today/home (accessed on 31 May 2023).
- Chen, L.; Li, H.; Xie, L.; Zuo, Z.; Tian, L.; Liu, C.; Guo, X. Editorial: Big Data and Machine Learning in Cancer Genomics. Front. Genet. 2021, 12, 749584. [Google Scholar] [CrossRef]
- Barrett, T.; Wilhite, S.E.; Ledoux, P.; Evangelista, C.; Kim, I.F.; Tomashevsky, M.; Marshall, K.A.; Phillippy, K.H.; Sherman, P.M.; Holko, M.; et al. NCBI GEO: Archive for Functional Genomics Data Sets—Update. Nucleic Acids Res. 2012, 41, D991–D995. [Google Scholar] [CrossRef]
- Meng, L.; Tian, Z.; Long, X.; Diao, T.; Hu, M.; Wang, M.; Zhang, W.; Zhang, Y.; Wang, J.; He, Y. Caspase 4 Overexpression as a Prognostic Marker in Clear Cell Renal Cell Carcinoma: A Study Based on the Cancer Genome Atlas Data Mining. Front. Genet. 2021, 11, 600248. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, J.; Zhuang, J.; Liu, C.; Gao, C.; Li, H.; Ma, X.; Li, J.; Sun, C. A Novel Glycolysis-Related Four-MRNA Signature for Predicting the Survival of Patients with Breast Cancer. Front. Genet. 2021, 12, 606937. [Google Scholar] [CrossRef] [PubMed]
- Becht, E.; McInnes, L.; Healy, J.; Dutertre, C.-A.; Kwok, I.W.H.; Ng, L.G.; Ginhoux, F.; Newell, E.W. Dimensionality Reduction for Visualizing Single-Cell Data Using UMAP. Nat. Biotechnol. 2019, 37, 38–44. [Google Scholar] [CrossRef]
- Lai, G.G.Y.; Guo, R.; Drilon, A.; Shao Weng Tan, D. Refining Patient Selection of MET-Activated Non-Small Cell Lung Cancer through Biomarker Precision. Cancer Treat. Rev. 2022, 110, 102444. [Google Scholar] [CrossRef]
- Yang, S.-R.; Schultheis, A.M.; Yu, H.; Mandelker, D.; Ladanyi, M.; Büttner, R. Precision Medicine in Non-Small Cell Lung Cancer: Current Applications and Future Directions. Semin. Cancer Biol. 2022, 84, 184–198. [Google Scholar] [CrossRef] [PubMed]
- Zappa, C.; Mousa, S.A. Non-Small Cell Lung Cancer: Current Treatment and Future Advances. Transl. Lung Cancer Res. 2016, 5, 288–300. [Google Scholar] [CrossRef]
- Wang, S.; Zimmermann, S.; Parikh, K.; Mansfield, A.S.; Adjei, A.A. Current Diagnosis and Management of Small-Cell Lung Cancer. Mayo Clin. Proc. 2019, 94, 1599–1622. [Google Scholar] [CrossRef]
- Mithoowani, H.; Febbraro, M. Non-Small-Cell Lung Cancer in 2022: A Review for General Practitioners in Oncology. Curr. Oncol. 2022, 29, 1828–1839. [Google Scholar] [CrossRef]
- Herbst, R.S.; Morgensztern, D.; Boshoff, C. The Biology and Management of Non-Small Cell Lung Cancer. Nature 2018, 553, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Molina, J.R.; Yang, P.; Cassivi, S.D.; Schild, S.E.; Adjei, A.A. Non–Small Cell Lung Cancer: Epidemiology, Risk Factors, Treatment, and Survivorship. Mayo Clin. Proc. 2009, 83, 584–594. [Google Scholar] [CrossRef]
- Duma, N.; Santana-Davila, R.; Molina, J.R. Non–Small Cell Lung Cancer: Epidemiology, Screening, Diagnosis, and Treatment. Mayo Clin. Proc. 2019, 94, 1623–1640. [Google Scholar] [CrossRef]
- Clark, S.B.; Alsubait, S. Non Small Cell Lung Cancer. In StatPearls; StatPearls Publishing: Tampa, FL, USA, 2022. [Google Scholar]
- Giraldo-Osorio, A.; Ruano-Ravina, A.; Rey-Brandariz, J.; Arias-Ortiz, N.; Candal-Pedreira, C.; Pérez-Ríos, M. Tendencias en la mortalidad por cáncer de pulmón en Colombia, 1985–2018. Rev. Panam. Salud Pública 2022, 46, 1. [Google Scholar] [CrossRef]
- Alarcón, M.-L.; Brugés, R.; Carvajal, C.; Vallejo, C.; Beltrán, R. Características de los pacientes con cáncer de pulmón de célula no pequeña en el Instituto Nacional de Cancerología de Bogotá. Rev. Colomb. Cancerol. 2021, 25, 103–109. [Google Scholar] [CrossRef]
- Guo, Q.; Liu, L.; Chen, Z.; Fan, Y.; Zhou, Y.; Yuan, Z.; Zhang, W. Current Treatments for Non-Small Cell Lung Cancer. Front. Oncol. 2022, 12, 945102. [Google Scholar] [CrossRef]
- Sosa Iglesias, V.; Giuranno, L.; Dubois, L.J.; Theys, J.; Vooijs, M. Drug Resistance in Non-Small Cell Lung Cancer: A Potential for NOTCH Targeting? Front. Oncol. 2018, 8, 267. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Lin, Z. Non-Small Cell Lung Cancer Targeted Therapy: Drugs and Mechanisms of Drug Resistance. IJMS 2022, 23, 15056. [Google Scholar] [CrossRef]
- Błach, J.; Wojas-Krawczyk, K.; Nicoś, M.; Krawczyk, P. Failure of Immunotherapy-The Molecular and Immunological Origin of Immunotherapy Resistance in Lung Cancer. Int. J. Mol. Sci. 2021, 22, 9030. [Google Scholar] [CrossRef]
- Schubart, C.; Stöhr, R.; Tögel, L.; Fuchs, F.; Sirbu, H.; Seitz, G.; Seggewiss-Bernhardt, R.; Leistner, R.; Sterlacci, W.; Vieth, M.; et al. MET Amplification in Non-Small Cell Lung Cancer (NSCLC)—A Consecutive Evaluation Using Next-Generation Sequencing (NGS) in a Real-World Setting. Cancers 2021, 13, 5023. [Google Scholar] [CrossRef]
- Rosellini, P.; Amintas, S.; Caumont, C.; Veillon, R.; Galland-Girodet, S.; Cuguillière, A.; Nguyen, L.; Domblides, C.; Gouverneur, A.; Merlio, J.-P.; et al. Clinical Impact of STK11 Mutation in Advanced-Stage Non-Small Cell Lung Cancer. Eur. J. Cancer 2022, 172, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Su, C. Emerging Insights to Lung Cancer Drug Resistance. Cancer Drug Resist. 2022, 5, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Sumbly, V.; Landry, I. Unraveling the Role of STK11/LKB1 in Non-Small Cell Lung Cancer. Cureus 2022, 14, e21078. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.C.; Balko, J.M. Mechanisms of MHC-I Downregulation and Role in Immunotherapy Response. Front. Immunol. 2022, 13, 844866. [Google Scholar] [CrossRef] [PubMed]
- Yan, N.; Guo, S.; Zhang, H.; Zhang, Z.; Shen, S.; Li, X. BRAF-Mutated Non-Small Cell Lung Cancer: Current Treatment Status and Future Perspective. Front. Oncol. 2022, 12, 863043. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zheng, L.; Yang, Q.; Sun, J. The Evolution of BRAF Activation in Non-Small-Cell Lung Cancer. Front. Oncol. 2022, 12, 882940. [Google Scholar] [CrossRef]
- Nam, M.-W.; Kim, C.-W.; Choi, K.-C. Epithelial-Mesenchymal Transition-Inducing Factors Involved in the Progression of Lung Cancers. Biomol. Ther. 2022, 30, 213–220. [Google Scholar] [CrossRef]
- Chae, Y.K.; Chang, S.; Ko, T.; Anker, J.; Agte, S.; Iams, W.; Choi, W.M.; Lee, K.; Cruz, M. Epithelial-Mesenchymal Transition (EMT) Signature Is Inversely Associated with T-Cell Infiltration in Non-Small Cell Lung Cancer (NSCLC). Sci. Rep. 2018, 8, 2918. [Google Scholar] [CrossRef]
- Greenspan, B.S. Role of PET/CT for Precision Medicine in Lung Cancer: Perspective of the Society of Nuclear Medicine and Molecular Imaging. Transl. Lung Cancer Res. 2017, 6, 617–620. [Google Scholar] [CrossRef]
- Inamura, K. Update on Immunohistochemistry for the Diagnosis of Lung Cancer. Cancers 2018, 10, 72. [Google Scholar] [CrossRef]
- Ginsburg, G.S.; Phillips, K.A. Precision Medicine: From Science To Value. Health Aff. 2018, 37, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Denny, J.C.; Collins, F.S. Precision Medicine in 2030—Seven Ways to Transform Healthcare. Cell 2021, 184, 1415–1419. [Google Scholar] [CrossRef] [PubMed]
- Naithani, N.; Sinha, S.; Misra, P.; Vasudevan, B.; Sahu, R. Precision Medicine: Concept and Tools. Med. J. Armed Forces India 2021, 77, 249–257. [Google Scholar] [CrossRef] [PubMed]
- König, I.R.; Fuchs, O.; Hansen, G.; Von Mutius, E.; Kopp, M.V. What Is Precision Medicine? Eur. Respir. J. 2017, 50, 1700391. [Google Scholar] [CrossRef]
- George, A.P.; Kuzel, T.M.; Zhang, Y.; Zhang, B. The Discovery of Biomarkers in Cancer Immunotherapy. Comput. Struct. Biotechnol. J. 2019, 17, 484–497. [Google Scholar] [CrossRef]
- Ielapi, N.; Andreucci, M.; Licastro, N.; Faga, T.; Grande, R.; Buffone, G.; Mellace, S.; Sapienza, P.; Serra, R. Precision Medicine and Precision Nursing: The Era of Biomarkers and Precision Health. IJGM 2020, 13, 1705–1711. [Google Scholar] [CrossRef]
- Slikker, W. Biomarkers and Their Impact on Precision Medicine. Exp. Biol. Med. 2018, 243, 211–212. [Google Scholar] [CrossRef]
- Hulsen, T.; Jamuar, S.S.; Moody, A.R.; Karnes, J.H.; Varga, O.; Hedensted, S.; Spreafico, R.; Hafler, D.A.; McKinney, E.F. From Big Data to Precision Medicine. Front. Med. 2019, 6, 34. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision Medicine, AI, and the Future of Personalized Health Care. Clin. Transl. Sci. 2021, 14, 86–93. [Google Scholar] [CrossRef]
- Califf, R.M. Biomarker Definitions and Their Applications. Exp. Biol. Med. 2018, 243, 213–221. [Google Scholar] [CrossRef]
- Henry, N.L.; Hayes, D.F. Cancer Biomarkers. Mol. Oncol. 2012, 6, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Grimberg, D.C.; Inman, B.A. Classification of Molecular Biomarkers. Société Int. Urol. J. 2020, 1, 8–15. [Google Scholar] [CrossRef]
- Berk, M. The Classification of Biomarkers. JAMA Psychiatry 2015, 72, 1056–1057. [Google Scholar] [CrossRef] [PubMed]
- Rifai, N.; Gillette, M.A.; Carr, S.A. Protein Biomarker Discovery and Validation: The Long and Uncertain Path to Clinical Utility. Nat. Biotechnol. 2006, 24, 971–983. [Google Scholar] [CrossRef]
- Qiu, S.; Cai, Y.; Yao, H.; Lin, C.; Xie, Y.; Tang, S.; Zhang, A. Small Molecule Metabolites: Discovery of Biomarkers and Therapeutic Targets. Signal Transduct. Target. Ther. 2023, 8, 132. [Google Scholar] [CrossRef]
- Hoseok, I.; Cho, J.-Y. Lung Cancer Biomarkers. In Advances in Clinical Chemistry; Elsevier: Amsterdam, The Netherlands, 2015; Volume 72, ISBN 978-0-12-803314-2. [Google Scholar]
- Gong, K.; Zhou, H.; Liu, H.; Xie, T.; Luo, Y.; Guo, H.; Chen, J.; Tan, Z.; Yang, Y.; Xie, L. Identification and Integrate Analysis of Key Biomarkers for Diagnosis and Prognosis of Non-Small Cell Lung Cancer Based on Bioinformatics Analysis. Technol. Cancer Res. Treat. 2021, 20, 107–170. [Google Scholar] [CrossRef]
- Román, M.; Baraibar, I.; López, I.; Nadal, E.; Rolfo, C.; Vicent, S.; Gil-Bazo, I. KRAS Oncogene in Non-Small Cell Lung Cancer: Clinical Perspectives on the Treatment of an Old Target. Mol. Cancer 2018, 17, 33. [Google Scholar] [CrossRef]
- Gendarme, S.; Bylicki, O.; Chouaid, C.; Guisier, F. ROS-1 Fusions in Non-Small-Cell Lung Cancer: Evidence to Date. Curr. Oncol. 2022, 29, 641–658. [Google Scholar] [CrossRef]
- Grigg, C.; Rizvi, N.A. PD-L1 Biomarker Testing for Non-Small Cell Lung Cancer: Truth or Fiction? J. Immunother. Cancer 2016, 4, 48. [Google Scholar] [CrossRef]
- Affandi, K.A.; Tizen, N.M.S.; Mustangin, M.; Zin, R.R.M.R.M. P40 Immunohistochemistry Is an Excellent Marker in Primary Lung Squamous Cell Carcinoma. J. Pathol. Transl. Med. 2018, 52, 283–289. [Google Scholar] [CrossRef]
- Pan, J.; Zhou, C.; Zhao, X.; He, J.; Tian, H.; Shen, W.; Han, Y.; Chen, J.; Fang, S.; Meng, X.; et al. A Two-MiRNA Signature (MiR-33a-5p and MiR-128-3p) in Whole Blood as Potential Biomarker for Early Diagnosis of Lung Cancer. Sci. Rep. 2018, 8, 16699. [Google Scholar] [CrossRef]
- Xu, Y.; Chai, B.; Wang, X.; Wu, Z.; Gu, Z.; Liu, X.; Zhao, Y.; Chen, T.; Ma, Z.; Sun, Q. MiRNA-199a-5p/SLC2A1 Axis Regulates Glucose Metabolism in Non-Small Cell Lung Cancer. J. Cancer 2022, 13, 2352–2361. [Google Scholar] [CrossRef] [PubMed]
- Pennell, N.A.; Arcila, M.E.; Gandara, D.R.; West, H. Biomarker Testing for Patients with Advanced Non–Small Cell Lung Cancer: Real-World Issues and Tough Choices. Am. Soc. Clin. Oncol. Educ. Book 2019, 531–542. [Google Scholar] [CrossRef]
- Ettinger, D.S.; Wood, D.E.; Aisner, D.L.; Akerley, W.; Bauman, J.R.; Bharat, A.; Bruno, D.S.; Chang, J.Y.; Chirieac, L.R.; D’Amico, T.A.; et al. NCCN Guidelines Insights: Non–Small Cell Lung Cancer, Version 2.2021: Featured Updates to the NCCN Guidelines. J. Natl. Compr. Cancer Netw. 2021, 19, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-L.; Planchard, D.; Lu, S.; Sun, H.; Yamamoto, N.; Kim, D.-W.; Tan, D.S.W.; Yang, J.C.-H.; Azrif, M.; Mitsudomi, T.; et al. Pan-Asian Adapted Clinical Practice Guidelines for the Management of Patients with Metastatic Non-Small-Cell Lung Cancer: A CSCO–ESMO Initiative Endorsed by JSMO, KSMO, MOS, SSO and TOS. Ann. Oncol. 2019, 30, 171–210. [Google Scholar] [CrossRef]
- Moes-Sosnowska, J.; Skupinska, M.; Lechowicz, U.; Szczepulska-Wojcik, E.; Skronska, P.; Rozy, A.; Stepniewska, A.; Langfort, R.; Rudzinski, P.; Orlowski, T.; et al. FGFR1–4 RNA-Based Gene Alteration and Expression Analysis in Squamous Non-Small Cell Lung Cancer. IJMS 2022, 23, 10506. [Google Scholar] [CrossRef] [PubMed]
- Dhakar, R.; Dakal, T.C.; Sharma, A. Genetic Determinants of Lung Cancer: Understanding the Oncogenic Potential of Somatic Missense Mutations. Genomics 2022, 114, 110401. [Google Scholar] [CrossRef]
- Uy, N.F.; Merkhofer, C.M.; Baik, C.S. HER2 in Non-Small Cell Lung Cancer: A Review of Emerging Therapies. Cancers 2022, 14, 4155. [Google Scholar] [CrossRef]
- Wang, N.; Song, X. Research Advances of Immunotherapy of Exosome PD-L1 in Non-Small Cell Lung Cancer. Chin. J. Lung Cancer 2022, 25, 689–695. [Google Scholar] [CrossRef]
- Qiu, F.-S.; He, J.-Q.; Zhong, Y.-S.; Guo, M.-Y.; Yu, C.-H. Implications of M6A Methylation and Microbiota Interaction in Non-Small Cell Lung Cancer: From Basics to Therapeutics. Front. Cell. Infect. Microbiol. 2022, 12, 972655. [Google Scholar] [CrossRef]
- Li, N.; Zhai, Z.; Chen, Y.; Li, X. Transcriptomic and Immunologic Implications of the Epithelial–Mesenchymal Transition Model Reveal a Novel Role of SFTA2 in Prognosis of Non-Small-Cell Lung Carcinoma. Front. Genet. 2022, 13, 911801. [Google Scholar] [CrossRef]
- Tutar, Y. MiRNA and Cancer; Computational and Experimental Approaches. Curr. Pharm. Biotechnol. 2014, 15, 429. [Google Scholar] [CrossRef]
- Wang, N.; Zhang, H.; Li, D.; Jiang, C.; Zhao, H.; Teng, Y. Identification of Novel Biomarkers in Breast Cancer via Integrated Bioinformatics Analysis of Potential Biomarkers for Pancreatic Cancer and Experimental Validation. Bioengineered 2021, 12, 12431–12446. [Google Scholar] [CrossRef]
- Wu, Q.; Zhang, B.; Sun, Y.; Xu, R.; Hu, X.; Ren, S.; Ma, Q.; Chen, C.; Shu, J.; Qi, F.; et al. Identification of Novel Biomarkers and Candidate Small Molecule Drugs in Non-Small-Cell Lung Cancer by Integrated Microarray Analysis. OncoTargets Ther. 2019, 12, 3545–3563. [Google Scholar] [CrossRef]
- Canale, M.; Andrikou, K.; Priano, I.; Cravero, P.; Pasini, L.; Urbini, M.; Delmonte, A.; Crinò, L.; Bronte, G.; Ulivi, P. The Role of TP53 Mutations in EGFR-Mutated Non-Small-Cell Lung Cancer: Clinical Significance and Implications for Therapy. Cancers 2022, 14, 1143. [Google Scholar] [CrossRef]
- McCarroll, J.A.; Gan, P.P.; Erlich, R.B.; Liu, M.; Dwarte, T.; Sagnella, S.S.; Akerfeldt, M.C.; Yang, L.; Parker, A.L.; Chang, M.H.; et al. TUBB3/ΒIII-Tubulin Acts through the PTEN/AKT Signaling Axis to Promote Tumorigenesis and Anoikis Resistance in Non–Small Cell Lung Cancer. Cancer Res. 2015, 75, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.-Q.; Huang, Y.-X.; Li, J.-L.; Zhang, X.-Q.; Peng, Q.-Q.; Tang, L.-R.; Wu, J.-X. Prognostic Value of Vascular Endothelial Growth Factor Receptor 1 and Class III β-Tubulin in Survival for Non-Metastatic Rectal Cancer. WJGO 2018, 10, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Šutić, M.; Vukić, A.; Baranašić, J.; Försti, A.; Džubur, F.; Samaržija, M.; Jakopović, M.; Brčić, L.; Knežević, J. Diagnostic, Predictive, and Prognostic Biomarkers in Non-Small Cell Lung Cancer (NSCLC) Management. JPM 2021, 11, 1102. [Google Scholar] [CrossRef] [PubMed]
- Villaruz, L.C.; Socinski, M.A. The Role of Anti-Angiogenesis in Non-Small-Cell Lung Cancer: An Update. Curr. Oncol. Rep. 2015, 17, 26. [Google Scholar] [CrossRef]
- Liu, Y.-Z.; Yang, H.; Cao, J.; Jiang, Y.-Y.; Hao, J.-J.; Xu, X.; Cai, Y.; Wang, M.-R. KIAA1522 Is a Novel Prognostic Biomarker in Patients with Non-Small Cell Lung Cancer. Sci. Rep. 2016, 6, 24786. [Google Scholar] [CrossRef]
- Hung, C.-Y.; Wang, Y.-C.; Chuang, J.-Y.; Young, M.-J.; Liaw, H.; Chang, W.-C.; Hung, J.-J. Nm23-H1-Stabilized HnRNPA2/B1 Promotes Internal Ribosomal Entry Site (IRES)-Mediated Translation of Sp1 in the Lung Cancer Progression. Sci. Rep. 2017, 7, 9166. [Google Scholar] [CrossRef]
- Lai, Y.-H.; Chen, W.-N.; Hsu, T.-C.; Lin, C.; Tsao, Y.; Wu, S. Overall Survival Prediction of Non-Small Cell Lung Cancer by Integrating Microarray and Clinical Data with Deep Learning. Sci. Rep. 2020, 10, 4679. [Google Scholar] [CrossRef]
- Chen, J.H.; Asch, S.M. Machine Learning and Prediction in Medicine—Beyond the Peak of Inflated Expectations. N. Engl. J. Med. 2017, 376, 2507–2509. [Google Scholar] [CrossRef] [PubMed]
- Hammad, A.; Elshaer, M.; Tang, X. Identification of Potential Biomarkers with Colorectal Cancer Based on Bioinformatics Analysis and Machine Learning. Math. Biosci. Eng. 2021, 18, 8997–9015. [Google Scholar] [CrossRef] [PubMed]
- Arslan, S.; Mehrotra, D.; Schmidt, J.; Geraldes, A.; Singhal, S.; Hense, J.; Li, X.; Bass, C.; Kather, J.N.; Pandya, P.; et al. Deep Learning Can Predict Multi-Omic Biomarkers from Routine Pathology Images: A Systematic Large-Scale Study. bioRxiv 2022. preprint. [Google Scholar]
- Wang, F.; Su, Q.; Li, C. Identidication of Novel Biomarkers in Non-Small Cell Lung Cancer Using Machine Learning. Sci. Rep. 2022, 12, 16693. [Google Scholar] [CrossRef]
- Handelman, G.S.; Kok, H.K.; Chandra, R.V.; Razavi, A.H.; Lee, M.J.; Asadi, H. EDoctor: Machine Learning and the Future of Medicine. J. Intern. Med. 2018, 284, 603–619. [Google Scholar] [CrossRef]
- Margolis, R.; Derr, L.; Dunn, M.; Huerta, M.; Larkin, J.; Sheehan, J.; Guyer, M.; Green, E.D. The National Institutes of Health’s Big Data to Knowledge (BD2K) Initiative: Capitalizing on Biomedical Big Data. J. Am. Med. Inform. Assoc. 2014, 21, 957–958. [Google Scholar] [CrossRef]
- Podolsky, M.D.; Barchuk, A.A.; Kuznetcov, V.I.; Gusarova, N.F.; Gaidukov, V.S.; Tarakanov, S.A. Evaluation of Machine Learning Algorithm Utilization for Lung Cancer Classification Based on Gene Expression Levels. Asian Pac. J. Cancer Prev. 2016, 17, 835–838. [Google Scholar] [CrossRef]
- Yang, Y.; Xu, L.; Sun, L.; Zhang, P.; Farid, S.S. Machine Learning Application in Personalised Lung Cancer Recurrence and Survivability Prediction. Comput. Struct. Biotechnol. J. 2022, 20, 1811–1820. [Google Scholar] [CrossRef]
- Huang, Y.; Huang, S.; Liu, Z. Multi-Task Learning-Based Feature Selection and Classification Models for Glioblastoma and Solitary Brain Metastases. Front. Oncol. 2022, 12, 1000471. [Google Scholar] [CrossRef] [PubMed]
- Batra, U.; Nathany, S.; Sharma, M.; Mehta, A.; Dhanda, S.; Jose, J.T. Machine Learning-Based Algorithm Demonstrates Differences in Del19 and L858R EGFR Subgroups in Non-Small Cell Lung Cancer: A Single Center Experience. Am. J. Transl. Res. 2022, 14, 2677. [Google Scholar]
- Yang, J.; Yee, P.L.; Khan, A.A.; Khan, M.S.; Karamti, H.; Aldweesh, A.; Hussain, L.; Omar, A. Improving Lungs Cancer Detection Based on Hybrid Features and Employing Machine Learning Techniques. Res. Sq. 2023. preprint. [Google Scholar] [CrossRef]
- Lian, J.; Deng, J.; Hui, E.S.; Koohi-Moghadam, M.; She, Y.; Chen, C.; Vardhanabhuti, V. Early Stage NSCLS Patients’ Prognostic Prediction with Multi-Information Using Transformer and Graph Neural Network Model. eLife 2022, 11, e80547. [Google Scholar] [CrossRef] [PubMed]
- Civit-Masot, J.; Bañuls-Beaterio, A.; Domínguez-Morales, M.; Rivas-Pérez, M.; Muñoz-Saavedra, L.; Rodríguez Corral, J.M. Non-Small Cell Lung Cancer Diagnosis Aid with Histopathological Images Using Explainable Deep Learning Techniques. Comput. Methods Programs Biomed. 2022, 226, 107108. [Google Scholar] [CrossRef]
- Huang, Z.; Wang, S.; Zhang, H.-J.; Zhou, Y.L.; Tang, X.; Shi, J.-H. Characteristics of Hypoxic Tumor Microenvironment in Non-Small Cell Lung Cancer, Involving Molecular Patterns and Prognostic Signature. Transl. Lung Cancer Res. 2021, 10, 2132–2147. [Google Scholar] [CrossRef]
- Shin, H.; Jeong, H.; Park, J.; Hong, S.; Choi, Y. Correlation between Cancerous Exosomes and Protein Markers Based on Surface-Enhanced Raman Spectroscopy (SERS) and Principal Component Analysis (PCA). ACS Sens. 2018, 3, 2637–2643. [Google Scholar] [CrossRef]
- Islam, M.T.; Xing, L. Geometry and Statistics-Preserving Manifold Embedding for Nonlinear Dimensionality Reduction. Pattern Recognit. Lett. 2021, 151, 155–162. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, Y.; Hao, Y.; Li, X.; Qi, Y.; Xin, M.; Xiao, Q.; Wang, P. Characterizing the Metabolic and Immune Landscape of Non-Small Cell Lung Cancer Reveals Prognostic Biomarkers Through Omics Data Integration. Front. Cell Dev. Biol. 2021, 9, 702112. [Google Scholar] [CrossRef]
- Nascimben, M.; Rimondini, L.; Corà, D.; Venturin, M. Polygenic Risk Modeling of Tumor Stage and Survival in Bladder Cancer. BioData Min. 2022, 15, 23. [Google Scholar] [CrossRef]
- Lombe, C.P.; Meyer, M.; Pretorius, A. Bioinformatics Prediction and Analysis of MicroRNAs and Their Targets as Biomarkers for Prostate Cancer: A Preliminary Study. Mol. Biotechnol. 2022, 64, 401–412. [Google Scholar] [CrossRef]
- Sarafidis, M.; Lambrou, G.I.; Zoumpourlis, V.; Koutsouris, D. An Integrated Bioinformatics Analysis towards the Identification of Diagnostic, Prognostic, and Predictive Key Biomarkers for Urinary Bladder Cancer. Cancers 2022, 14, 3358. [Google Scholar] [CrossRef]
- Pandi, J.; Arulprakasam, A.; Dhandapani, R.; Ramanathan, S.; Thangavelu, S.; Chinnappan, J.; Vidhya Rajalakshmi, V.; Alghamdi, S.; Shesha, N.T.; Prasath, S. Biomarkers for Breast Adenocarcinoma Using In Silico Approaches. Evid.-Based Complement. Altern. Med. 2022, 2022, 825272. [Google Scholar] [CrossRef]
- Lvu, W.; Fei, X.; Chen, C.; Zhang, B. In Silico Identification of the Prognostic Biomarkers and Therapeutic Targets Associated with Cancer Stem Cell Characteristics of Glioma. Biosci. Rep. 2020, 40, BSR20201037. [Google Scholar] [CrossRef]
- Yuan, L.; Cao, X.; Chen, L.; Zhu, Y.; Qian, G.; Xiao, Y. Identification of Potential Biomarkers in Human Prostate Cancer Using Bioinform. Anal. 2017, 1, 6. [Google Scholar]
- Chen, J.; Cai, Y.; Xu, R.; Pan, J.; Zhou, J.; Mei, J. Identification of Four Hub Genes as Promising Biomarkers to Evaluate the Prognosis of Ovarian Cancer in Silico. Cancer Cell. Int. 2020, 20, 270. [Google Scholar] [CrossRef]
- Wu, L.; Shang, W.; Zhao, H.; Rong, G.; Zhang, Y.; Xu, T.; Zhang, J.; Huang, P.; Wang, F. In Silico Screening of Circulating MicroRNAs as Potential Biomarkers for the Diagnosis of Ovarian Cancer. Dis. Markers 2019, 2019, 1–12. [Google Scholar] [CrossRef]
- Lai, L.-T.; Ren, Y.-H.; Huai, Y.-J.; Liu, Y.; Liu, Y.; Wang, S.-S.; Mei, J.-H. Identification and Validation of Novel Prognostic Biomarkers and Therapeutic Targets for Non-Small Cell Lung Cancer. Front. Genet. 2023, 14, 1139994. [Google Scholar] [CrossRef]
- Lavanya, C.; Pooja, S.; Kashyap, A.H.; Rahaman, A.; Niranjan, S.; Niranjan, V. Novel Biomarker Prediction for Lung Cancer Using Random Forest Classifiers. Cancer Inform. 2023, 22, 117693512311679. [Google Scholar] [CrossRef]
- Zhang, C.; Berndt-Paetz, M.; Neuhaus, J. Bioinformatics Analysis Identifying Key Biomarkers in Bladder Cancer. Data 2020, 5, 38. [Google Scholar] [CrossRef]
- Xu, Y.; Niu, C. Screening of Breast Cancer Biomarkers Based on Bioinformatics Analysis. Res. Sq. 2022. preprint. [Google Scholar] [CrossRef]
- Wu, Z.; Wan, J.; Wang, J.; Meng, X.; Qian, H. Identification of Prognostic Biomarkers for Breast Cancer Brain Metastases Based on the Bioinformatics Analysis. Biochem. Biophys. Rep. 2022, 29, 101203. [Google Scholar] [CrossRef]
- Fadaka, A.O.; Klein, A.; Pretorius, A. In Silico Identification of MicroRNAs as Candidate Colorectal Cancer Biomarkers. Tumour Biol. 2019, 41, 101042831988372. [Google Scholar] [CrossRef]
- Dai, G.; Wang, L.; Wen, Y.; Ren, X.; Zuo, S. Identification of Key Genes for Predicting Colorectal Cancer Prognosis by Integrated Bioinformatics Analysis. Oncol. Lett. 2019, 19, 388–398. [Google Scholar] [CrossRef]
- Li, H.; Liu, L.; Jiang, Y.; Jiang, H.; Niu, C.; Xia, J.; Liu, Z.; Guo, Y. Integrated Bioinformatics Revealed 2 Novel Prognostic Biomarkers in Colorectal Cancer. Int. J. Clin. Exp. Med. 2021, 14, 2250–2258. [Google Scholar]
- Paksoy, N.; Yağin, F.H. Artificial Intelligence-Based Colon Cancer Prediction by Identifying Genomic Biomarkers. Med. Rec. 2022, 4, 196–202. [Google Scholar] [CrossRef]
- Wang, W.; Min, K.; Chen, G.; Zhang, H.; Deng, J.; Lv, M.; Cao, Z.; Zhou, Y. Use of Bioinformatic Database Analysis and Specimen Verification to Identify Novel Biomarkers Predicting Gastric Cancer Metastasis. J. Cancer 2021, 12, 5967–5976. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, D.-X.; Wan, X.-J.; Meng, X.-H. Identification of Candidate Biomarkers Associated with Gastric Cancer Prognosis Based on an Integrated Bioinformatics Analysis. J. Gastrointest. Oncol. 2022, 13, 1690–1700. [Google Scholar] [CrossRef]
- Liao, Y.; Xiao, H.; Cheng, M.; Fan, X. Bioinformatics Analysis Reveals Biomarkers with Cancer Stem Cell Characteristics in Lung Squamous Cell Carcinoma. Front. Genet. 2020, 11, 427. [Google Scholar] [CrossRef]
- Zahra, A.; Hall, M.; Chatterjee, J.; Sisu, C.; Karteris, E. In Silico Study to Predict the Structural and Functional Consequences of SNPs on Biomarkers of Ovarian Cancer (OC) and BPA Exposure-Associated OC. IJMS 2022, 23, 1725. [Google Scholar] [CrossRef]
- Shi, H.; Xu, H.; Chai, C.; Qin, Z.; Zhou, W. Integrated Bioinformatics Analysis of Potential Biomarkers for Pancreatic Cancer. J. Clin. Lab. Anal. 2022, 36, e24381. [Google Scholar] [CrossRef]
- Van Den Broek, D.; Hiltermann, T.J.N.; Biesma, B.; Dinjens, W.N.M.; ’T Hart, N.A.; Hinrichs, J.W.J.; Leers, M.P.G.; Monkhorst, K.; Van Oosterhout, M.; Scharnhorst, V.; et al. Implementation of Novel Molecular Biomarkers for Non-Small Cell Lung Cancer in the Netherlands: How to Deal with Increasing Complexity. Front. Oncol. 2020, 9, 1521. [Google Scholar] [CrossRef]
- Hofman, P. The Challenges of Evaluating Predictive Biomarkers Using Small Biopsy Tissue Samples and Liquid Biopsies from Non-Small Cell Lung Cancer Patients. J. Thorac. Dis. 2019, 11, S57–S64. [Google Scholar] [CrossRef]
- Mandair, D.; Reis-Filho, J.S.; Ashworth, A. Biological Insights and Novel Biomarker Discovery through Deep Learning Approaches in Breast Cancer Histopathology. NPJ Breast Cancer 2023, 9, 21. [Google Scholar] [CrossRef]
| Diagnostic Method | Advantages | Disadvantages |
|---|---|---|
| MRI | No ionizing radiation exposure | Limited availability and restricted access |
| Detailed imaging of soft tissues | Lower sensitivity for detecting small lesions | |
| PET | Detects metabolic and molecular changes | Higher cost and limited availability |
| High sensitivity for detecting metastasis | Potential for false positives due to FDG accumulation | |
| CT | Widely available and rapid access | Exposes the patient to ionizing radiation |
| High spatial resolution and early tumor detection | Potential for false positives due to benign lesions | |
| FISH Biomarkers | Provides genetic information about specific cancer subtypes | Requires specialized laboratory analysis |
| PCR Biomarkers | Provides genetic information about specific cancer subtypes, | Requires specialized laboratory analysis |
| IHC Biomarkers | Provides protein expression information, Helps differentiate cancer subtypes | Requires specialized personnel and equipment, results may vary depending on the method used |
| Next Generation Sequencing Biomarkers | Provides comprehensive genetic information | Requires specialized laboratory analysis |
| Liquid Biopsy | Non-invasive and lower risk for the patient | Lower sensitivity compared to tissue biopsy |
| Enables monitoring of genetic changes over time | Potential for false negatives due to low concentration | |
| Tissue Biopsy | Provides tissue samples for histopathological analysis | Invasive procedure with associated risks |
| High precision and detection of genetic mutations | Potential complications such as bleeding or infection |
| Biomarkers in Nsclc | |||||
|---|---|---|---|---|---|
| Diagnostic Biomarkers in NSCLC | |||||
| Immunohistochemistry | Circulating tumor proteins | ||||
| TTF-1 (Thyroid Transcription Factor-1) | Cytokeratin 19 fragment (CYFRA 21-1) | ||||
| p40 | Carcinoembryonic Antigen (CEA) | ||||
| Napsin A | Squamous cell carcinoma antigen (SCCA) | ||||
| Carbohydrate antigen 125 (CA125) | |||||
| microRNA (miRNA) | |||||
| miR-205 | miR-106a | miR-29b | |||
| miR-375 | miR-125a-5p | miR-375 | |||
| miR-93 | miR-129-3p | miR-7 | |||
| miR-221 | miR-205 | miR-19b-3p | |||
| miR-100 | miR-21 | miR-199a-5p | |||
| Predictive Biomarkers in NSCLC | |||||
| Targeted Therapy | For Inmunotherapy | Novel predictive biomarkers | |||
| Biomarker | Therapy | Biomarker | Antibody | Targered therapy | Inmunotherapy |
| EGFR | Afatinib | PD-1 | Atezolizumab | KRAS | Exosome PD-L1 |
| Erlotinib | Pembrolizumab | FGFR1 | m6A methylation | ||
| Gefitinib | Durvalumab | DDR2 | SFTA2 | ||
| Osimertinib | Nivolumab | HER2 | TIL’s | ||
| TIM-3 | |||||
| ROS1 | Entrectinib | TMB | |||
| Ceritinib | |||||
| Crizotinib | |||||
| ALK | Alectinib | ||||
| Crizotinib | |||||
| Lorlatinib | |||||
| MET | Tepotinib | ||||
| Capmatinib | |||||
| RET | Selpercatinib | ||||
| Praseltinib | |||||
| BRAF | Trametinib | ||||
| Dabrafenib+ | |||||
| NTRK (1,2,3) | Larotrectinib | ||||
| Biomarker | Outcome |
|---|---|
| TP53 | Resistance to Therapy increased. |
| VEGF | Poor prognosis, metastasis, tumor recurrence. |
| TUBB3 | Poor prognosis |
| KIAA1522 | Poor prognosis and lower response rate |
| nm23-H1 | Low levels poor prognosis |
| TGF-β | Poor prognosis |
| LAG-3 | Better survival |
| NLR&PLR | Worse overall survival |
| Ki-67 | Poor prognosis |
| Algorithm | Advantages | Limitations | References |
|---|---|---|---|
| Supervised Algorithms | |||
| Logistic Regression | High power for supervised classification with a dichotomous variable | Not useful for continuous variables | Yang, 2022 [83] |
| Support Vector Machine | Applied in non-linear models and survival prediction in cancer and demographic studies, among others. Good control of overfitting and good classifier | Complex algorithm structure. Training is slower. | Huang, 2022 [84] |
| Decision Trees | Easy algorithm for data training. Used in diagnostic protocols | Can have overfitting problems, especially when there is a significant increase in branching in internal nodes | Lai, 2020 [75]; Batra, 2022 [85], 2022 [7] |
| Random Forest | Good predictive algorithm used in medicine in different imaging studies and recently in biomarker studies | May have overfitting problems | Batra, 2022 [85]; Handelman, 2018 [80] |
| Naïve Bayes | Still used in symptom characterization, complication prediction, imaging data, and demographic data. | As it is based on probabilistic statistical models, it can assume that attributes are independent. Redundant attributes can induce classification errors | Yang, 2023 [86] |
| K-Nearest Neighbor | Used as a classification and prediction algorithm in demographic models and genomic data, among others. Tolerant to noisy and missing data | Can assume that data attributes are equally important and may have similar classifications. Computationally complex with increasing data and attributes | Podolsky, 2016 [82] |
| Artificial Neural Networks | Algorithmic model capable of classifying and predicting based on a combination of parameters and applying it at the same time. | May have overfitting with too many attributes, and the optimal network structure is determined for experimentation | Lian, 2022 [87]; Civit-Masot, 2022 [88] |
| Unsupervised Algorithms | |||
| K-Means | Widely used algorithm in biological and medical research and is easy to adapt and understand. Performs well on large datasets | The number of K needs to be manually assigned. Outliers can generate incorrect clusters. Scaling issues with the number of dimensions | Huang, 2021 [89] |
| Principal Component Analysis (PCA) | Linear dimensionality reduction algorithm that allows pattern observation and generates independent variables called principal components. Widely used in biological and genomic data observation | Does not allow non-linear dimensionality reduction. Lack of data standardization can be detrimental to results and information loss | Shin, 2018 [90] |
| t-SNE | Algorithm that enables visualization of high-dimensional datasets. Frequently used with PCA in biological and life sciences, primarily in omics analysis | Some issues when applied to non-linear parameter dimensionality reduction | Islam, 2021 [91]; Wang, 2021 [92] |
| UMAP | Next-generation algorithm that, similar to t-SNE, enables visualization of high-dimensional datasets. Offers higher accuracy when working with non-linear structures. Widely used in omics analysis | Currently limited to dimensional reduction due to its relative lack of familiarity | Islam, 2021 [91]; Nascimben, 2022 [93] |
| Author | Type of Cancer | Type of Data | Database | Data Preprocessing and Differentially Expressed Genes (DEGs) | MicroRNA Target Prediction | Protein–Protein Interaction (PPI) | Functional Enrichment Analysis | Validation |
|---|---|---|---|---|---|---|---|---|
| Zhang et al., 2020 [103] | Bladder | Gene | TCGA-BLCA, GEO | R software | Not Realized | CytoHubba, STRING | GO, KEGG, FUNRICH, DAVID | Oncomine database, GEPIA |
| Sarafidis et al., 2022 [95] | Bladder | Gene | GEO (metanalysis) | Affy, LIMMA R packages, outlier removal quality control | Not Realized | STRING, Cytoscape | GO, KEGG, Disease Ontology (DO), Reactome | GEPIA2, TCGA, Human Protein Atlas (proteomics, RNA-Seq), survival analysis |
| Pandi et al., 2022 [96] | Breast | Gene | GEO | R LIMMA package, GEO2R | Not Realized | STRING, Cytoscape | Enrichr, KEGG | TCGA-BRCA, GEPIA, survival analysis |
| Xu et al., 2022 [104] | Breast | Gene | GEO | R LIMMA package | Not Realized | STRING | GO, KEGG | GEPIA, survival analysis |
| Wu et al., 2022 [105] | Breast | Gene | TCGA | R LIMMA package | Not Realized | STRING | GO, clusterProfiler R package | Breast Cancer Gene-Expression Miner v4.8 (bc-GenExMiner v4.8), survival analysis |
| Fadaka et al., 2019 [106] | Colon | microRNA | miRBase (https://www.mirbase.org/ accessed on 20 March 2023), miR2Disease (http://www.mir2disease.org/ accessed on 20 March 2023), HMDD (http://www.cuilab.cn/hmdd accessed on 20 March 2023), y miRCancer (http://mircancer.ecu.edu/ accessed on 20 March 2023), BLAST | R software | miRDB (http://www.mirdb.org/index.html accessed on 20 March 2023), TargetScan (https://www.targetscan.org/vert_72/ accessed on 20 March 2023) y mirDIP (http://ophid.utoronto.ca/mirDIP/index.jsp accessed on 20 March 2023) | STRING, Cytoscape | DAVID, GO, KEGG | Gene correlation (gbCRC) at http://gbcrc.bioinfo-minzhao.org/ accessed on 20 March 2023 |
| Dai et al., 2019 [107] | Colon | Gene | GEO (systematic review) | R software, BRB array tools | Not Realized | STRING, Cytoscape | FunRich (http://www.funrich.org/ accessed on 20 March 2023), KEGG, DAVID | The Human Protein Atlas (HPA), The Cancer Genome Atlas (TCGA), survival analysis |
| Li et al., 2021 [108] | Colon | Gene | GEO | R limma package | Not Realized | STRING, Cytoscape | KEGG, DAVID | TCGA, GEPIA, survival analysis |
| Hammad et al., 2021 [77] | Colon | Gene | GEO | R software | Not Realized | STRING, Cytoscape | KEGG, DAVID | GEPIA, survival analysis (PROGgene) |
| Paksoy and Hilal, 2022 [109] | Colon | Gene | https://figshare.com/articles/dataset/The_microarray_dataset_of_colon_cancer_in_csv_format_/13658790/1 accessed on 20 March 2023 | Synthetic Minority Oversampling Technique, or SMOTE method | Not Realized | Not Realized | Not Realized | Not Realized |
| Wang et al., 2021 [110] | Gastric | Gene | TCGA | R limma package | Not Realized | Cytoscape | GO, KEGG | GEPIA, survival analysis, Jiangsu Province Yixing People’s Hospital |
| Liu et al., 2022 [111] | Gastric | Gene | GEO, TCGA | R limma package, clustering analysis (Bioconductor) | Not Realized | STRING, Cytoscape | KEGG, DAVID | TCGA, survival analysis |
| Lvu et al., 2020 [97] | Glioma | mRNAsi | TCGA | EdgeR method | Not Realized | Not Realized | GO, KEGG | Survival analysis, Chinese Glioma Genome Atlas (CGGA) (http://www.cgga.org.cn/ accessed on 20 March 2023) |
| Liao et al., 2020 [112] | Lung | mRNAsi | TCGA | R LIMMA package | Not Realized | STRING, Cytoscape | GO, KEGG, DAVID | GEPIA, survival analysis |
| Gong et al., 2021 [49] | NSCLC | Gene | GEO | GEO2R | Not Realized | STRING, Cytoscape | KEGG, DAVID | GEPIA, survival analysis, Oncomine database |
| Wu et al., 2019 [100] | Ovarian | microRNA | GEO (Systematic review and Metanalysis) | edgeR package of R | Not Realized | GO, KEGG, DAVID | Survival analysis | |
| Chen et al., 2020 [99] | Ovarian | Gene | GEO | R software | Not Realized | GeneMANIA (https://genemania.org/ accessed on 20 March 2023) | KEGG, DAVID | Survival analysis, Dataset GSE9891 |
| Zahra et al., 2022 [113] | Ovarian | Gene | TCGA, UK BioBank, cBioPortal | R software | Not Realized | Not Realized | Not Realized | Not Realized |
| Shi et al., 2022 [114] | Pancreas | Gene | GEO | GEO2R | STRING, Cytoscape | GO, KEGG, DAVID | GEPIA, Survival analysis | |
| Yuan et al., 2017 [98] | Prostate | Gene | GEO | Affy, LIMMA R packages | STRING, Cytoscape | GO, DAVID | Protein Atlas Database, Oncomine database | |
| Lombe et al., 2022 [94] | Prostate | microRNA | GEO | GENT2 (http://gent2.appex.kr/gent2/ accessed on 20 March 2023) | TargetScan Human, miRDB, DIANA microT | STRING, Cytoscape | GO, KEGG, DAVID | GEPIA, survival analysis |
| Author | Prediction of drug-gene interaction | Evaluation of pronostic biomarkers | Protein acquisition, 3D modeling and protein visualizer | In vitro Validation | ||||
| Zhang et al., 2020 [103] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Sarafidis et al., 2022 [95] | Not Realized | Least Absolute Shrinkage and Selection Operator (LASSO) regression | Not Realized | Not Realized | ||||
| Pandi et al., 2022 [96] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Xu et al., 2022 [104] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Wu et al., 2022 [105] | DrugBank, Cytoscape | Not Realized | Not Realized | Not Realized | ||||
| Fadaka et al., 2019 [106] | Not Realized | PrognoScan (http://dna00.bio.kyutech.ac.jp/PrognoScan/ accessed on 20 March 2023) | Not Realized | Not Realized | ||||
| Dai et al., 2020 [107] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Li et al., 2021 [108] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Hammad et al., 2021 [77] | Not Realized | Prediction model with Support Vector Machine (SVM classifier) | Not Realized | Not Realized | ||||
| Paksoy and Hilal, 2022 [109] | Not Realized | Random Forest, Desicion Trees, Gaussian Bayes | Not Realized | Not Realized | ||||
| Wang et al., 2021 [110] | Not Realized | Not Realized | Not Realized | Gastric cell lines (AGS, HGC27 and MKN45) and normal gastric mucosa cells, FISH, RNA extraction, qRT-PCR | ||||
| Liu et al., 2022 [111] | Drug-Gene Interaction database (DGIdb), Cytoscape | Not Realized | Not Realized | Not Realized | ||||
| Lvu et al., 2020 [97] | Not Realized | Estimation of mRNAsi using one-class logistic regressionmachine learning (OCLR), Least Absolute Shrinkage and Selection Operator (LASSO) regression | Not Realized | Not Realized | ||||
| Liao et al., 2020 [112] | Not Realized | Estimation of mRNAsi using one-class logistic regressionmachine learning (OCLR) | Not Realized | Not Realized | ||||
| Gong et al., 2021 [49] | Not Realized | Not Realized | Not Realized | A549 and HBE normall cells, via qPCR | ||||
| Wu et al., 2019 [100] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Chen et al., 2020 [99] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Zahra et al., 2022 [113] | Not Realized | Not Realized | Uniprot, RSCB PDB (Protein Data Bank),Phyre2, Swissmodel, Alpha fold, Missense3D tool, YASARA, PYMOL, PROVEAN | Not Realized | ||||
| Shi et al., 2022 [114] | Not Realized | Not Realized | Not Realized | Four PDA cell lines (AsPC-1, SW1990, PANC-1, and BxPC-3) and a normal human pancreatic ductal epithelial cell line (HPDE), qRT-CPR | ||||
| Yuan et al., 2017 [98] | Not Realized | Not Realized | Not Realized | Not Realized | ||||
| Lombe et al., 2022 [94] | Not Realized | Not Realized | Not Realized | MicroRNAs via qPCR | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Restrepo, J.C.; Dueñas, D.; Corredor, Z.; Liscano, Y. Advances in Genomic Data and Biomarkers: Revolutionizing NSCLC Diagnosis and Treatment. Cancers 2023, 15, 3474. https://doi.org/10.3390/cancers15133474
Restrepo JC, Dueñas D, Corredor Z, Liscano Y. Advances in Genomic Data and Biomarkers: Revolutionizing NSCLC Diagnosis and Treatment. Cancers. 2023; 15(13):3474. https://doi.org/10.3390/cancers15133474
Chicago/Turabian StyleRestrepo, Juan Carlos, Diana Dueñas, Zuray Corredor, and Yamil Liscano. 2023. "Advances in Genomic Data and Biomarkers: Revolutionizing NSCLC Diagnosis and Treatment" Cancers 15, no. 13: 3474. https://doi.org/10.3390/cancers15133474
APA StyleRestrepo, J. C., Dueñas, D., Corredor, Z., & Liscano, Y. (2023). Advances in Genomic Data and Biomarkers: Revolutionizing NSCLC Diagnosis and Treatment. Cancers, 15(13), 3474. https://doi.org/10.3390/cancers15133474






