Comparative Analyses of the Clinicopathologic Features of Short-Term and Long-Term Survivors of Patients with Pancreatic Ductal Adenocarcinoma Who Received Neoadjuvant Therapy and Pancreatoduodenectomy
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
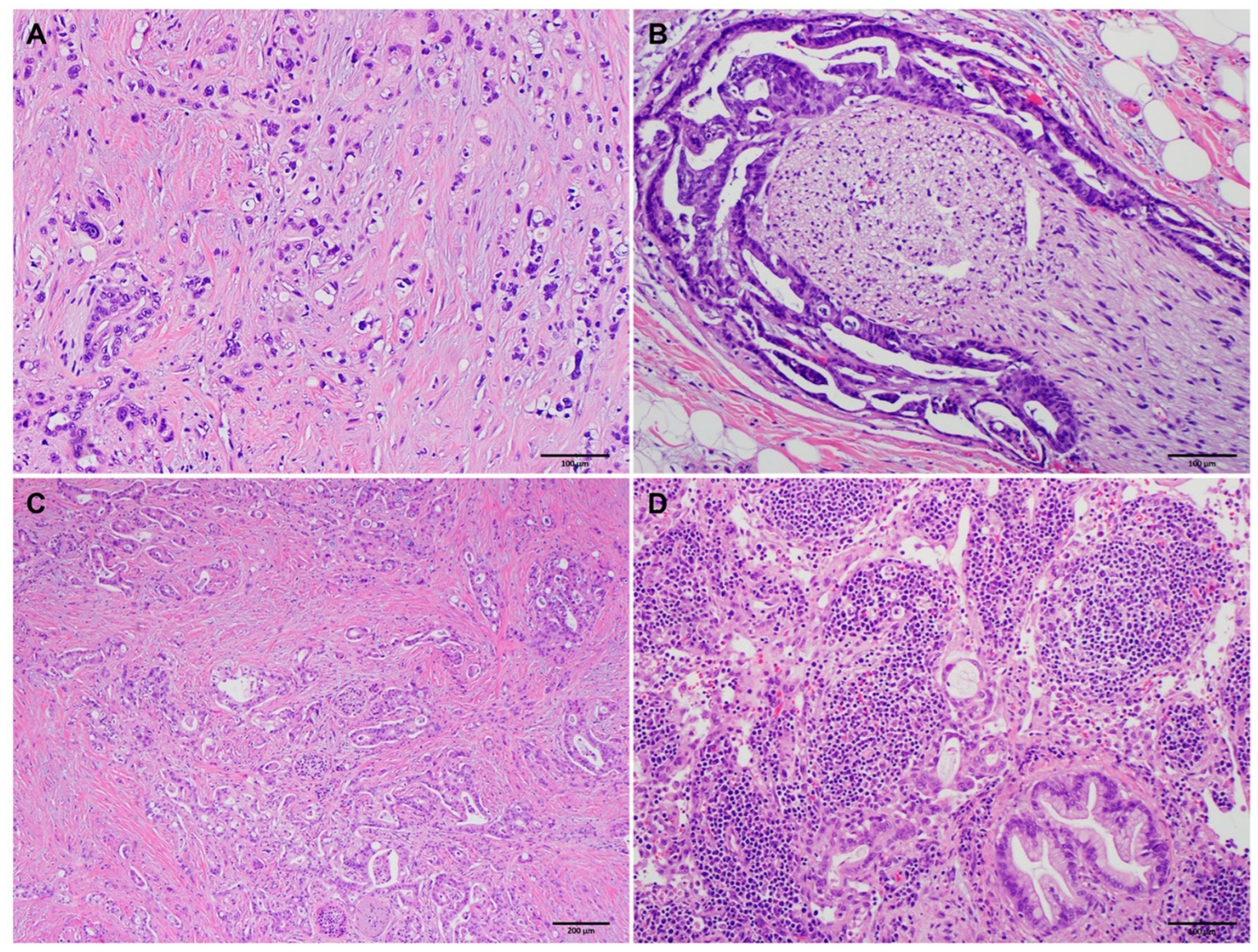
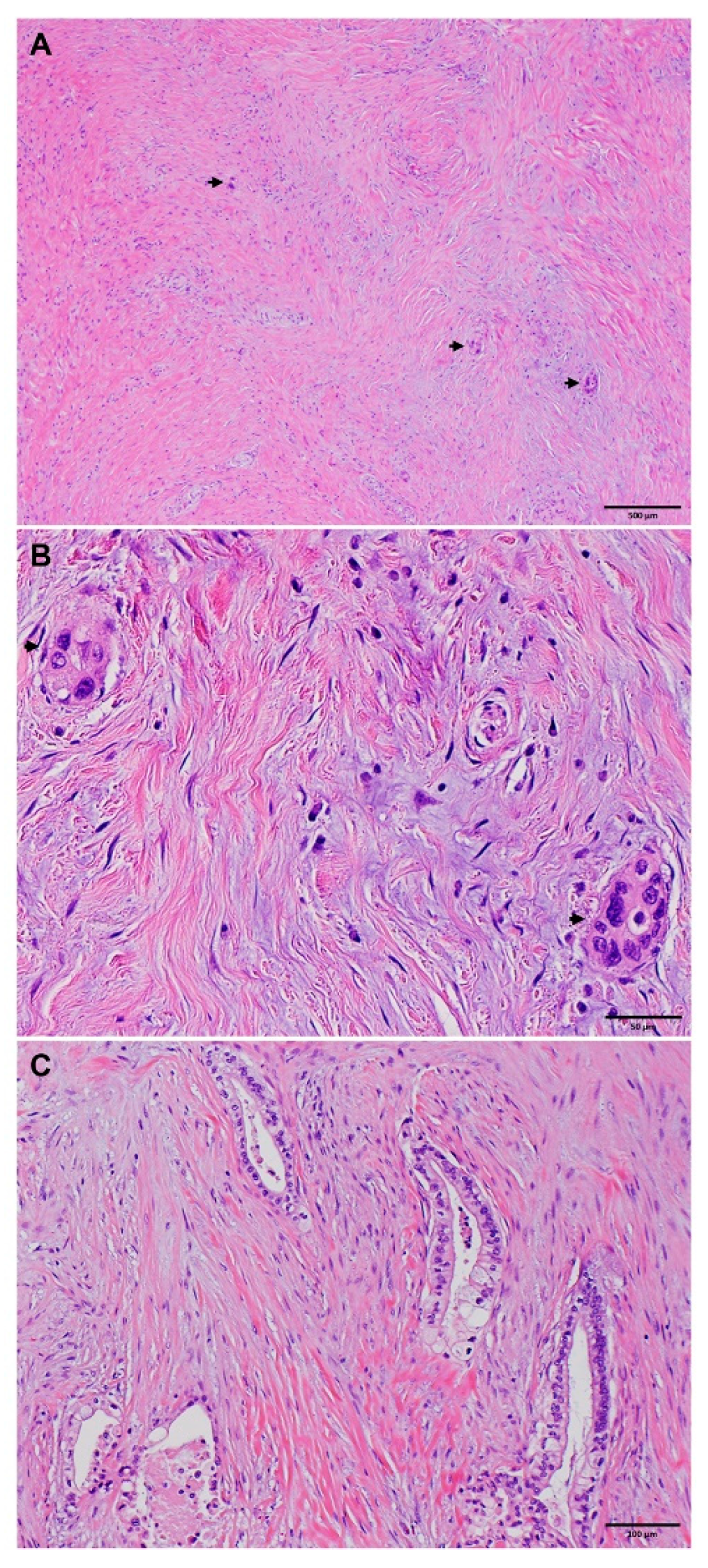
2.2. Pathologic Evaluation
2.3. Clinical and Follow-Up Data
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. The Clinicopathologic Features of Short-Term Survivor Group
3.3. The Clinicopathologic Features of Long-Term Survivor Group
3.4. Comparison of the Clinicopathologic Features of Long-Term Survivor Group with Short-Term Survivor Group
3.5. Multivariate Logistic Regression Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Rahib, L.; Wehner, M.R.; Matrisian, L.M.; Nead, K.T. Estimated Projection of US Cancer Incidence and Death to 2040. JAMA Netw. Open 2021, 4, e214708. [Google Scholar] [CrossRef]
- Tempero, M.A.; Malafa, M.P.; Al-Hawary, M.; Behrman, S.W.; Benson, A.B.; Cardin, D.B.; Chiorean, E.G.; Chung, V.; Czito, B.; Del Chiaro, M.; et al. Pancreatic Adenocarcinoma, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 439–457. [Google Scholar] [CrossRef]
- Springfeld, C.; Ferrone, C.R.; Katz, M.H.G.; Philip, P.A.; Hong, T.S.; Hackert, T.; Buchler, M.W.; Neoptolemos, J. Neoadjuvant therapy for pancreatic cancer. Nat. Rev. Clin. Oncol. 2023, 20, 318–337. [Google Scholar] [CrossRef]
- Tong, Y.T.; Lai, Z.; Katz, M.H.G.; Prakash, L.R.; Wang, H.; Chatterjee, D.; Kim, M.; Tzeng, C.D.; Lee, J.E.; Ikoma, N.; et al. Prognosticators for Patients with Pancreatic Ductal Adenocarcinoma Who Received Neoadjuvant FOLFIRINOX or Gemcitabine/Nab-Paclitaxel Therapy and Pancreatectomy. Cancers 2023, 15, 2608. [Google Scholar] [CrossRef] [PubMed]
- Janssen, Q.P.; van Dam, J.L.; Kivits, I.G.; Besselink, M.G.; van Eijck, C.H.J.; Homs, M.Y.V.; Nuyttens, J.; Qi, H.; van Santvoort, H.J.; Wei, A.C.; et al. Added Value of Radiotherapy Following Neoadjuvant FOLFIRINOX for Resectable and Borderline Resectable Pancreatic Cancer: A Systematic Review and Meta-Analysis. Ann. Surg. Oncol. 2021, 28, 8297–8308. [Google Scholar] [CrossRef]
- Wolfe, A.R.; Prabhakar, D.; Yildiz, V.O.; Cloyd, J.M.; Dillhoff, M.; Abushahin, L.; Alexandra Diaz, D.; Miller, E.D.; Chen, W.; Frankel, W.L.; et al. Neoadjuvant-modified FOLFIRINOX vs nab-paclitaxel plus gemcitabine for borderline resectable or locally advanced pancreatic cancer patients who achieved surgical resection. Cancer Med. 2020, 9, 4711–4723. [Google Scholar] [CrossRef]
- Versteijne, E.; Vogel, J.A.; Besselink, M.G.; Busch, O.R.C.; Wilmink, J.W.; Daams, J.G.; van Eijck, C.H.J.; Groot Koerkamp, B.; Rasch, C.R.N.; van Tienhoven, G.; et al. Meta-analysis comparing upfront surgery with neoadjuvant treatment in patients with resectable or borderline resectable pancreatic cancer. Br. J. Surg. 2018, 105, 946–958. [Google Scholar] [CrossRef]
- Chatterjee, D.; Katz, M.H.; Rashid, A.; Varadhachary, G.R.; Wolff, R.A.; Wang, H.; Lee, J.E.; Pisters, P.W.; Vauthey, J.N.; Crane, C.; et al. Histologic grading of the extent of residual carcinoma following neoadjuvant chemoradiation in pancreatic ductal adenocarcinoma: A predictor for patient outcome. Cancer 2012, 118, 3182–3190. [Google Scholar] [CrossRef]
- Chou, A.; Ahadi, M.; Arena, J.; Sioson, L.; Sheen, A.; Fuchs, T.L.; Pavlakis, N.; Clarke, S.; Kneebone, A.; Hruby, G.; et al. A Critical Assessment of Postneoadjuvant Therapy Pancreatic Cancer Regression Grading Schemes With a Proposal for a Novel Approach. Am. J. Surg. Pathol. 2021, 45, 394–404. [Google Scholar] [CrossRef]
- Lee, S.M.; Katz, M.H.; Liu, L.; Sundar, M.; Wang, H.; Varadhachary, G.R.; Wolff, R.A.; Lee, J.E.; Maitra, A.; Fleming, J.B.; et al. Validation of a Proposed Tumor Regression Grading Scheme for Pancreatic Ductal Adenocarcinoma After Neoadjuvant Therapy as a Prognostic Indicator for Survival. Am. J. Surg. Pathol. 2016, 40, 1653–1660. [Google Scholar] [CrossRef] [PubMed]
- Nagaria, T.S.; Wang, H.; Chatterjee, D. Pathology of Treated Pancreatic Ductal Adenocarcinoma and Its Clinical Implications. Arch. Pathol. Lab. Med. 2020, 144, 838–845. [Google Scholar] [CrossRef]
- Chatterjee, D.; Katz, M.H.; Rashid, A.; Wang, H.; Iuga, A.C.; Varadhachary, G.R.; Wolff, R.A.; Lee, J.E.; Pisters, P.W.; Crane, C.H.; et al. Perineural and intraneural invasion in posttherapy pancreaticoduodenectomy specimens predicts poor prognosis in patients with pancreatic ductal adenocarcinoma. Am. J. Surg. Pathol. 2012, 36, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, D.; Rashid, A.; Wang, H.; Katz, M.H.; Wolff, R.A.; Varadhachary, G.R.; Lee, J.E.; Pisters, P.W.; Gomez, H.F.; Abbruzzese, J.L.; et al. Tumor invasion of muscular vessels predicts poor prognosis in patients with pancreatic ductal adenocarcinoma who have received neoadjuvant therapy and pancreaticoduodenectomy. Am. J. Surg. Pathol. 2012, 36, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Fischer, L.K.; Katz, M.H.; Lee, S.M.; Liu, L.; Wang, H.; Varadhachary, G.R.; Wolff, R.A.; Lee, J.E.; Maitra, A.; Roland, C.L.; et al. The number and ratio of positive lymph nodes affect pancreatic cancer patient survival after neoadjuvant therapy and pancreaticoduodenectomy. Histopathology 2016, 68, 210–220. [Google Scholar] [CrossRef]
- Liu, L.; Katz, M.H.; Lee, S.M.; Fischer, L.K.; Prakash, L.; Parker, N.; Wang, H.; Varadhachary, G.R.; Wolff, R.A.; Lee, J.E.; et al. Superior Mesenteric Artery Margin of Posttherapy Pancreaticoduodenectomy and Prognosis in Patients With Pancreatic Ductal Adenocarcinoma. Am. J. Surg. Pathol. 2015, 39, 1395–1403. [Google Scholar] [CrossRef]
- Estrella, J.S.; Rashid, A.; Fleming, J.B.; Katz, M.H.; Lee, J.E.; Wolf, R.A.; Varadhachary, G.R.; Pisters, P.W.; Abdalla, E.K.; Vauthey, J.N.; et al. Post-therapy pathologic stage and survival in patients with pancreatic ductal adenocarcinoma treated with neoadjuvant chemoradiation. Cancer 2012, 118, 268–277. [Google Scholar] [CrossRef]
- Sohn, A.J.; Taherian, M.; Katz, M.H.G.; Prakash, L.R.; Chatterjee, D.; Wang, H.; Kim, M.; Tzeng, C.D.; Lee, J.E.; Ikoma, N.; et al. Integrated Pathologic Score Effectively Stratifies Patients With Pancreatic Ductal Adenocarcinoma Who Received Neoadjuvant Therapy and Pancreaticoduodenectomy. Am. J. Surg. Pathol. 2023, 47, 421–430. [Google Scholar] [CrossRef]
- Varadhachary, G.R.; Tamm, E.P.; Abbruzzese, J.L.; Xiong, H.Q.; Crane, C.H.; Wang, H.; Lee, J.E.; Pisters, P.W.; Evans, D.B.; Wolff, R.A. Borderline resectable pancreatic cancer: Definitions, management, and role of preoperative therapy. Ann. Surg. Oncol. 2006, 13, 1035–1046. [Google Scholar] [CrossRef]
- Chatterjee, D.; Katz, M.H.; Foo, W.C.; Sundar, M.; Wang, H.; Varadhachary, G.R.; Wolff, R.A.; Lee, J.E.; Maitra, A.; Fleming, J.B.; et al. Prognostic Significance of New AJCC Tumor Stage in Patients With Pancreatic Ductal Adenocarcinoma Treated With Neoadjuvant Therapy. Am. J. Surg. Pathol. 2017, 41, 1097–1104. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- Belfiori, G.; Crippa, S.; Francesca, A.; Pagnanelli, M.; Tamburrino, D.; Gasparini, G.; Partelli, S.; Andreasi, V.; Rubini, C.; Zamboni, G.; et al. Long-Term Survivors after Upfront Resection for Pancreatic Ductal Adenocarcinoma: An Actual 5-Year Analysis of Disease-Specific and Post-Recurrence Survival. Ann. Surg. Oncol. 2021, 28, 8249–8260. [Google Scholar] [CrossRef] [PubMed]
- Cleary, S.P.; Gryfe, R.; Guindi, M.; Greig, P.; Smith, L.; Mackenzie, R.; Strasberg, S.; Hanna, S.; Taylor, B.; Langer, B.; et al. Prognostic factors in resected pancreatic adenocarcinoma: Analysis of actual 5-year survivors. J. Am. Coll. Surg. 2004, 198, 722–731. [Google Scholar] [CrossRef]
- Conlon, K.C.; Klimstra, D.S.; Brennan, M.F. Long-term survival after curative resection for pancreatic ductal adenocarcinoma. Clinicopathologic analysis of 5-year survivors. Ann. Surg. 1996, 223, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Ferrone, C.R.; Pieretti-Vanmarcke, R.; Bloom, J.P.; Zheng, H.; Szymonifka, J.; Wargo, J.A.; Thayer, S.P.; Lauwers, G.Y.; Deshpande, V.; Mino-Kenudson, M.; et al. Pancreatic ductal adenocarcinoma: Long-term survival does not equal cure. Surgery 2012, 152, S43–S49. [Google Scholar] [CrossRef]
- Han, S.S.; Jang, J.Y.; Kim, S.W.; Kim, W.H.; Lee, K.U.; Park, Y.H. Analysis of long-term survivors after surgical resection for pancreatic cancer. Pancreas 2006, 32, 271–275. [Google Scholar] [CrossRef]
- Schnelldorfer, T.; Ware, A.L.; Sarr, M.G.; Smyrk, T.C.; Zhang, L.; Qin, R.; Gullerud, R.E.; Donohue, J.H.; Nagorney, D.M.; Farnell, M.B. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: Is cure possible? Ann. Surg. 2008, 247, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Strobel, O.; Lorenz, P.; Hinz, U.; Gaida, M.; Konig, A.K.; Hank, T.; Niesen, W.; Kaiser, J.O.R.; Al-Saeedi, M.; Bergmann, F.; et al. Actual Five-year Survival After Upfront Resection for Pancreatic Ductal Adenocarcinoma: Who Beats the Odds? Ann. Surg. 2022, 275, 962–971. [Google Scholar] [CrossRef]
- Yamamoto, T.; Yagi, S.; Kinoshita, H.; Sakamoto, Y.; Okada, K.; Uryuhara, K.; Morimoto, T.; Kaihara, S.; Hosotani, R. Long-term survival after resection of pancreatic cancer: A single-center retrospective analysis. World J. Gastroenterol. 2015, 21, 262–268. [Google Scholar] [CrossRef]
- Paniccia, A.; Hosokawa, P.; Henderson, W.; Schulick, R.D.; Edil, B.H.; McCarter, M.D.; Gajdos, C. Characteristics of 10-Year Survivors of Pancreatic Ductal Adenocarcinoma. JAMA Surg. 2015, 150, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K.; Amano, R.; Nakata, B.; Yamazoe, S.; Hirata, K.; Murata, A.; Miura, K.; Nishio, K.; Hirakawa, T.; Ohira, M.; et al. Clinical and pathological features of five-year survivors after pancreatectomy for pancreatic adenocarcinoma. World J. Surg. Oncol. 2014, 12, 360. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, M.; Kondo, S.; Sugiura, H.; Katoh, H. Pre-operative predictors of short-term survival after pancreatic cancer resection. Hepatogastroenterology 1998, 45, 2399–2403. [Google Scholar] [PubMed]
- Agalianos, C.; Gouvas, N.; Papaparaskeva, K.; Dervenis, C. Positive para-aortic lymph nodes following pancreatectomy for pancreatic cancer. Systematic review and meta-analysis of impact on short term survival and association with clinicopathologic features. HPB 2016, 18, 633–641. [Google Scholar] [CrossRef]
- Wang, H.; Chetty, R.; Hosseini, M.; Allende, D.S.; Esposito, I.; Matsuda, Y.; Deshpande, V.; Shi, J.; Dhall, D.; Jang, K.T.; et al. Pathologic Examination of Pancreatic Specimens Resected for Treated Pancreatic Ductal Adenocarcinoma: Recommendations From the Pancreatobiliary Pathology Society. Am. J. Surg. Pathol. 2022, 46, 754–764. [Google Scholar] [CrossRef]
- Yamaguchi, J.; Yokoyama, Y.; Fujii, T.; Yamada, S.; Takami, H.; Kawashima, H.; Ohno, E.; Ishikawa, T.; Maeda, O.; Ogawa, H.; et al. Results of a Phase II Study on the Use of Neoadjuvant Chemotherapy (FOLFIRINOX or GEM/nab-PTX) for Borderline-resectable Pancreatic Cancer (NUPAT-01). Ann. Surg. 2022, 275, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Short-Term | Intermediate-Term | p Value |
|---|---|---|---|
| Mean age ± SD (years) | 66.0 ± 9.8 | 63.5 ± 9.3 | 0.06 |
| Sex | 0.03 | ||
| Female | 18 | 159 | |
| Male | 42 | 193 | |
| Neoadjuvant therapy | 0.214 | ||
| FP-based chemo + radiation | 16 | 119 | |
| Gem-based chemo + radiation | 41 | 193 | |
| Gem-based chemo | 2 | 30 | |
| FOLFIRINOX | 1 | 10 | |
| Resectability | 0.04 | ||
| Potentially resectable | 50 | 235 | |
| Borderline resectable | 8 | 92 | |
| Locally advanced | 2 | 25 | |
| Differentiation | 0.006 | ||
| Well-moderate | 26 | 221 | |
| Poor | 34 | 131 | |
| Mean tumor size ± SD (cm) | 2.9 ± 1.2 | 2.7 ± 1.3 | 0.13 |
| ypT stage | 0.36 | ||
| ypT0/ypT1 | 21 | 115 | |
| ypT2 | 28 | 193 | |
| ypT3 | 11 | 44 | |
| Lymphovascular invasion | 0.12 | ||
| Negative | 22 | 169 | |
| Positive | 38 | 183 | |
| Perineural invasion | 0.052 | ||
| Negative | 6 | 73 | |
| Positive | 54 | 279 | |
| ypN stage | 0.002 | ||
| ypN0 | 12 | 153 | |
| ypN1 | 31 | 119 | |
| ypN2 | 17 | 80 | |
| Mean number of positive nodes ± SD | 3.1 ± 3.7 | 2.1 ± 3.3 | 0.04 |
| Mean total number of nodes ± SD | 23.8 ± 9.6 | 25.9 ± 10.3 | 0.14 |
| Mean positive lymph node ratio ± SD | 0.12 ± 0.13 | 0.09 ± 0.12 | 0.03 |
| MDA Tumor Response Grade | 0.46 | ||
| MDA grade 0 | 0 | 7 | |
| MDA grade 1 | 7 | 32 | |
| MDA grade 2 | 53 | 313 | |
| CAP Tumor Response Grade | 0.50 | ||
| Grade 0 | 0 | 7 | |
| Grade 1 | 7 | 32 | |
| Grade 2 | 31 | 203 | |
| Grade 3 | 22 | 110 | |
| Margin status | 0.70 | ||
| Negative | 52 | 296 | |
| Positive | 8 | 56 | |
| Recurrence/metastasis | 0.15 | ||
| None | 8 | 63 | |
| Local | 8 | 77 | |
| Distant | 44 | 212 |
| Long-Term | Intermediate-Term | p Value | |
|---|---|---|---|
| Mean age ± SD (years) | 63.0 ± 9.6 | 63.5 ± 9.3 | 0.59 |
| Sex | 0.63 | ||
| Female | 71 | 159 | |
| Male | 78 | 193 | |
| Neoadjuvant therapy | 0.08 | ||
| FP-based chemo + radiation | 47 | 119 | |
| Gem-based chemo + radiation | 94 | 193 | |
| Gem-based chemo | 4 | 30 | |
| FOLFIRINOX | 4 | 10 | |
| Resectability | 0.86 | ||
| Potentially resectable | 101 | 235 | |
| Borderline resectable | 36 | 92 | |
| Locally advanced | 12 | 25 | |
| Differentiation | 0.19 | ||
| Well-moderate | 103 | 221 | |
| Poor | 46 | 131 | |
| Mean tumor size ± SD (cm) | 2.24 ± 1.52 | 2.67 ± 1.27 | 0.001 |
| ypT stage | 0.001 | ||
| ypT0/ypT1 | 74 | 115 | |
| ypT2 | 63 | 193 | |
| ypT3 | 12 | 44 | |
| Lymphovascular invasion | 0.001 | ||
| Negative | 96 | 169 | |
| Positive | 53 | 183 | |
| Perineural invasion | <0.001 | ||
| Negative | 59 | 73 | |
| Positive | 90 | 279 | |
| ypN stage | <0.001 | ||
| ypN0 | 94 | 153 | |
| ypN1 | 44 | 119 | |
| ypN2 | 11 | 80 | |
| Mean number of positive nodes ± SD | 1.04 ± 2.53 | 2.14 ± 3.30 | <0.001 |
| Mean total number of nodes ± SD | 25.58 ± 10.49 | 25.88 ± 10.29 | 0.77 |
| Mean positive lymph node ratio ± SD | 0.036 ± 0.068 | 0.087 ± 0.124 | <0.001 |
| MDA Tumor Response Grade | <0.001 | ||
| MDA grade 0 | 9 | 7 | |
| MDA grade 1 | 30 | 32 | |
| MDA grade 2 | 110 | 313 | |
| CAP Tumor Response Grade | <0.001 | ||
| Grade 0 | 9 | 7 | |
| Grade 1 | 30 | 32 | |
| Grade 2 | 70 | 203 | |
| Grade 3 | 40 | 110 | |
| Margin status | 0.07 | ||
| Negative | 135 | 296 | |
| Positive | 14 | 56 | |
| Recurrence/metastasis | <0.001 | ||
| None | 97 | 63 | |
| Local | 13 | 77 | |
| Distant | 39 | 212 |
| Characteristics | Short-Term | Long-Term | p Value |
|---|---|---|---|
| Mean age ± SD (years) | 66.0 ± 9.8 | 63.0 ± 9.6 | 0.04 |
| Sex | 0.02 | ||
| Female | 18 | 71 | |
| Male | 42 | 78 | |
| Neoadjuvant therapy | 0.86 | ||
| FP-based chemo + radiation | 16 | 47 | |
| Gem-based chemo + radiation | 41 | 94 | |
| Gem-based chemo | 2 | 4 | |
| FOLFIRINOX | 1 | 4 | |
| Resectability | 0.07 | ||
| Potentially resectable | 50 | 101 | |
| Borderline resectable | 8 | 36 | |
| Locally advanced | 2 | 12 | |
| Differentiation | 0.001 | ||
| Well-moderate | 26 | 103 | |
| Poor | 34 | 46 | |
| Mean tumor size ± SD (cm) | 2.93 ± 1.23 | 2.24 ± 1.52 | 0.002 |
| ypT stage | 0.04 | ||
| ypT0/ypT1 | 21 | 74 | |
| ypT2 | 28 | 63 | |
| ypT3 | 11 | 12 | |
| Lymphovascular invasion | <0.001 | ||
| Negative | 22 | 96 | |
| Positive | 38 | 53 | |
| Perineural invasion | <0.001 | ||
| Negative | 6 | 59 | |
| Positive | 54 | 90 | |
| ypN stage | <0.001 | ||
| ypN0 | 12 | 94 | |
| ypN1 | 31 | 44 | |
| ypN2 | 17 | 11 | |
| Mean number of positive nodes ± SD | 3.12 ± 3.65 | 1.04 ± 2.53 | <0.001 |
| Mean total number of nodes ± SD | 23.75 ± 9.62 | 25.58 ± 10.49 | 0.24 |
| Mean positive lymph node ratio ± SD | 0.124 ± 0.134 | 0.036 ± 0.068 | <0.001 |
| MDA Tumor Response Grade | 0.04 | ||
| MDA grade 0 | 0 | 9 | |
| MDA grade 1 | 7 | 30 | |
| MDA grade 2 | 53 | 110 | |
| CAP Tumor Response Grade | 0.07 | ||
| Grade 0 | 0 | 9 | |
| Grade 1 | 7 | 30 | |
| Grade 2 | 31 | 70 | |
| Grade 3 | 22 | 40 | |
| Margin status | 0.46 | ||
| Negative | 52 | 135 | |
| Positive | 8 | 14 | |
| Recurrence | <0.001 | ||
| None | 8 | 97 | |
| Local | 8 | 13 | |
| Distant | 44 | 39 |
| Characteristics | Number of Patients | OR (95% CI) | p Value |
|---|---|---|---|
| Sex | |||
| Female | 177 | 1.00 | |
| Male | 235 | 1.57 (0.85–2.90) | 0.15 |
| Resectability | 0.07 | ||
| Potentially resectable | 285 | 1.00 | |
| Borderline resectable | 100 | 3.22 (0.72–14.49) | 0.13 |
| Locally advanced | 27 | 1.48 (0.29–7.61) | 0.64 |
| Tumor differentiation | |||
| Well-moderate | 247 | 1.00 | |
| Poor | 165 | 2.09 (1.18–3.72) | 0.01 |
| ypN stage | 0.006 | ||
| ypN0 | 165 | 1.00 | |
| ypN1 | 150 | 3.33 (1.59–6.97) | 0.001 |
| ypN2 | 97 | 2.67 (1.15–6.18) | 0.02 |
| Tumor response grading | |||
| MDA grade 0 or 1 | 46 | 1.00 | |
| MDA grade 2 | 366 | 3.02 (0.97–9.45) | 0.06 |
| Perineural Invasion | |||
| Negative | 79 | 1.00 | |
| Present | 333 | 2.87 (0.95–8.64) | 0.06 |
| Characteristics | Number of Patients | OR (95% CI) | p Value |
|---|---|---|---|
| Neoadjuvant therapy | 0.41 | ||
| FP-based chemo + radiation | 166 | 1.00 | |
| Gem-based chemo + radiation | 287 | 1.21 (0.78–1.86) | 0.40 |
| Gem-based chemo | 34 | 0.50 (0.16–1.53) | 0.22 |
| FOLFIRINOX | 14 | 1.02 (0.29–3.62) | 0.97 |
| ypT stage | 0.44 | ||
| ypT0/ypT1 | 189 | 1.00 | |
| ypT2 | 256 | 0.76 (0.48–1.20) | 0.24 |
| ypT3 | 56 | 0.71 (0.33–1.51) | 0.37 |
| ypN stage | 0.003 | ||
| ypN0 | 247 | 1.00 | |
| ypN1 | 163 | 0.72 (0.46–1.12) | 0.14 |
| ypN2 | 91 | 0.30 (0.15–0.60) | 0.001 |
| Tumor Response Grading | |||
| MDA grade 0 or 1 | 78 | 1.00 | |
| MDA grade 2 | 423 | 0.55 (0.32–0.97) | 0.04 |
| Lymphovascular invasion | |||
| Negative | 265 | 1.00 | |
| Positive | 236 | 0.86 (0.54–1.37) | 0.52 |
| Perineural invasion | |||
| Negative | 132 | 1.00 | |
| Positive | 369 | 0.61 (0.38–0.98) | 0.04 |
| Margin | |||
| Negative | 431 | 1.00 | |
| Positive | 70 | 0.92 (0.47–1.81) | 0.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, T.Z.; Katz, M.H.G.; Prakash, L.R.; Chatterjee, D.; Wang, H.; Kim, M.; Tzeng, C.-W.D.; Ikoma, N.; Wolff, R.A.; Zhao, D.; et al. Comparative Analyses of the Clinicopathologic Features of Short-Term and Long-Term Survivors of Patients with Pancreatic Ductal Adenocarcinoma Who Received Neoadjuvant Therapy and Pancreatoduodenectomy. Cancers 2023, 15, 3231. https://doi.org/10.3390/cancers15123231
Liang TZ, Katz MHG, Prakash LR, Chatterjee D, Wang H, Kim M, Tzeng C-WD, Ikoma N, Wolff RA, Zhao D, et al. Comparative Analyses of the Clinicopathologic Features of Short-Term and Long-Term Survivors of Patients with Pancreatic Ductal Adenocarcinoma Who Received Neoadjuvant Therapy and Pancreatoduodenectomy. Cancers. 2023; 15(12):3231. https://doi.org/10.3390/cancers15123231
Chicago/Turabian StyleLiang, Tom Z., Matthew H. G. Katz, Laura R. Prakash, Deyali Chatterjee, Hua Wang, Michael Kim, Ching-Wei D. Tzeng, Naruhiko Ikoma, Robert A. Wolff, Dan Zhao, and et al. 2023. "Comparative Analyses of the Clinicopathologic Features of Short-Term and Long-Term Survivors of Patients with Pancreatic Ductal Adenocarcinoma Who Received Neoadjuvant Therapy and Pancreatoduodenectomy" Cancers 15, no. 12: 3231. https://doi.org/10.3390/cancers15123231
APA StyleLiang, T. Z., Katz, M. H. G., Prakash, L. R., Chatterjee, D., Wang, H., Kim, M., Tzeng, C.-W. D., Ikoma, N., Wolff, R. A., Zhao, D., Koay, E. J., Maitra, A., Kundu, S., & Wang, H. (2023). Comparative Analyses of the Clinicopathologic Features of Short-Term and Long-Term Survivors of Patients with Pancreatic Ductal Adenocarcinoma Who Received Neoadjuvant Therapy and Pancreatoduodenectomy. Cancers, 15(12), 3231. https://doi.org/10.3390/cancers15123231






