Simple Summary
Epithelial-to-mesenchymal transition (EMT) is a complex program by which epithelial cells lose epithelial characteristics whilst acquiring mesenchymal features. EMT was coined in the 1980s and initially thought to involve a binary switch between epithelial and mesenchymal states. However, mounting work suggests that EMT involves intermediate states or hybrid epithelial/mesenchymal (E/M) phenotypes. In the context of many cancers, such as breast cancers, these hybrid states retain characteristics of both epithelial and mesenchymal cells, and have been linked to poor survival, metastasis, and resistance to treatment. In this Review, the authors examine the complex layers of molecular interactions governing EMT in cancer. The underlying drivers of these states, namely EMT-transcription factors, epigenetic regulators, and non-coding RNAs, as well as the influence of EMT on the immune response, are discussed, and in doing so, this Review outlines valuable mechanistic insights for the reversion of EMT and potential avenues for therapeutic intervention.
Abstract
Cellular plasticity in cancer enables adaptation to selective pressures and stress imposed by the tumor microenvironment. This plasticity facilitates the remodeling of cancer cell phenotype and function (such as tumor stemness, metastasis, chemo/radio resistance), and the reprogramming of the surrounding tumor microenvironment to enable immune evasion. Epithelial plasticity is one form of cellular plasticity, which is intrinsically linked with epithelial–mesenchymal transition (EMT). Traditionally, EMT has been regarded as a binary state. Yet, increasing evidence suggests that EMT involves a spectrum of quasi-epithelial and quasi-mesenchymal phenotypes governed by complex interactions between cellular metabolism, transcriptome regulation, and epigenetic mechanisms. Herein, we review the complex cross-talk between the different layers of epithelial plasticity in cancer, encompassing the core layer of transcription factors, their interacting epigenetic modifiers and non-coding RNAs, and the manipulation of cancer immunogenicity in transitioning between epithelial and mesenchymal states. In examining these factors, we provide insights into promising therapeutic avenues and potential anti-cancer targets.
1. Introduction
Epithelial cells have defined structural features which include the polarized distribution of the plasma membrane components and uniform cell–cell junctions, giving rise to a wide array of cellular states. Intercellular adhesions provide epithelial cells with intrinsic and structural “rigidity”. On the other hand, mesenchymal cells lack such uniformity with decreased structural integrity and adhesions. Unlike their epithelial counterparts, mesenchymal cells exhibit elongated, irregular morphologies, and exhibit an ability to migrate and invade through the extracellular matrix.
The phenomenon by which epithelial cells undergo complex phenotypic changes and acquire mesenchymal features is referred as epithelial-to-mesenchymal transition (EMT). This process was first coined in 1982 by Elizabeth Dexter “Betty” Hay and her team, who described the ability of epithelial cells to switch “off” epithelial genes while acquiring mesenchymal characteristics [1]. This pioneering work observed that cultured chick embryo epithelial cells had a remarkable ability to move and migrate through the collagen matrix in which they were suspended. These migratory cells displayed mesenchymal properties and were described as “transformed”. Further investigation detailed that reverse changes could occur in these migratory cells where they would anchor and regain epithelial-like characteristics.
EMT and its reverse process, mesenchymal-to-epithelial transition (MET), is instrumental in developmental programs, including embryonic association with implantation and embryonic development (type I EMT) and wound healing [2]. However, abnormal activation of EMT programs is induced by conditions such as fibrosis (type II EMT) and cancer (type III EMT) [2,3]. The different types of EMT have been extensively reviewed by Kalluri and Weinberg, 2009 [2]. For decades, EMT was viewed to comprise two distinct cell types—epithelial and mesenchymal—with a binary switch between the two states. However, in 2020, a consensus among EMT researchers established that this biological phenomenon encompasses a spectrum of dynamic intermediate states of bidirectional EMT to MET giving rise to epithelial–mesenchymal plasticity (EMP) [4].
There are several regulatory processes or layers of complexity that modulate EMP. At the core of EMP lies pro-mesenchymal transcription factors (EMT-TFs). EMT-TFs specifically regulate their target genes via consensus DNA-binding domains, which vary across the main families of EMT-TFs. Furthermore, their N- and C-terminal effector domains promote the association with particular partners, and the recruitment of a constellation of different epigenetic modifiers, modulating gene activation and/or repression. Added layers of regulatory mechanisms include non-coding RNAs, such as micro RNAs (miRNAs), many of which are involved in regulatory feedback loops with the EMT-TFs themselves, thus greatly amplifying the scope of targets implicated in EMP. Beyond these molecular processes intrinsic to cancer cells, there are also cross-talk mechanisms established between the cancer cells, the surrounding tumor microenvironment, and the infiltrating immune response, which can further modulate EMP.
Carcinoma cells in the form of transformed cell lines and solid tumors are notoriously heterogeneous, and can be positioned in particular cell states along a continuum of a bi-directional plasticity axis. Importantly, this axis includes a range of quasi-epithelial and quasi-mesenchymal phenotypes existing in equilibrium [5]. Loss of epithelial E-cadherin and gain of mesenchymal N-Cadherin, Fibronectin, and Vimentin have been long considered hallmarks of EMT [6]. Importantly, during tumorigenesis and cancer progression, tumor cells rarely attain a complete mesenchymal phenotype [7]. Instead, cancer cells undergo commonly partial EMT (pEMT) resulting in E/M hybrid states where the same cell co-expresses epithelial and mesenchymal markers [7,8,9]. The positioning of cancer cells along the EMP axis is defined by an interplay of several EMT inducers and regulators, outlined in Figure 1.
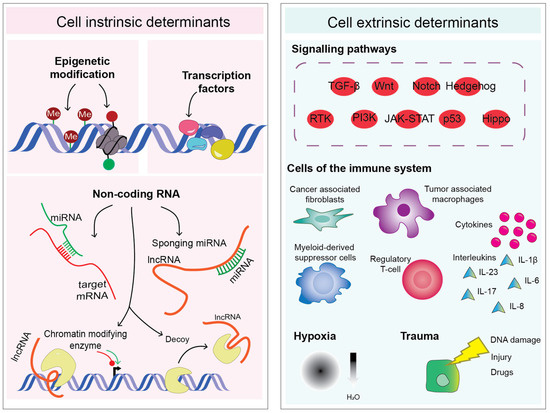
Figure 1.
Schematic diagram displaying the complexity of cancer cell plasticity and regulation, which can be divided into two major categories of triggering factors: cell intrinsic and cell extrinsic determinants. Me: DNA methylation, miRNA: microRNA, lncRNA: long non-coding RNA, TGF-β: transforming growth factor-β, Wnt: Wnt signaling, RTK: receptor tyrosine kinases, PI3K: phosphoinositide 3-kinase, JAK-STAT: Janus kinase-signal transducer and activator of transcription, IL: interleukin.
Much of EMT research has focused on the upregulation of “core” EMT-TFs in cancer cells, such as zinc-finger E-box-binding (ZEB) 1 and 2, snail family transcriptional repressor 1 (SNAI1, SNAIL), snail family transcriptional repressor 2 (SNAI2, SLUG), and twist-related protein (TWIST) 1 and 2 [10]. These EMT regulators cooperate to suppress pro-epithelial genes, particularly those involved in tight junction and adhesion. In addition, several non-coding RNAs, such as pro-epithelial miRNAs [11], are involved in regulatory feedback loops with EMT-TFs, and are key for specifying the different cell states along the EMP axis. One prime example is the double negative feedback loop between members of the microRNA-200 family (miR-200a, miR-200b, miR-200c, miR-429, and miR-141) with the ZEB1/ZEB2 EMT-TFs [12,13].
In addition to the “intrinsic” regulation of EMT-TFs in cancer cells, various extracellular signals and intracellular pathways associated with an aggressive tumor microenvironment (TME) modulate EMT either directly or indirectly, including the cytokine transforming growth factor-β (TGFβ), tumor necrosis factor-α (TNFα), Notch, JAK/STAT, Wnt/β-Catenin, and PI3K/Akt/mTOR [14,15,16,17,18]. These pathways, together with other regulatory cues, can activate EMT-TFs, often in combination with suppression of pro-epithelial miRNA expression, thereby facilitating cancer cell survival and metastasis [19,20].
Not surprisingly, hybrid E/M states, characterized by co-expression of epithelial and mesenchymal markers, have been associated with poor prognosis cancers with the ability to metastasize and resist treatment [7,21,22]. Gene expression profiling has identified several EMT-related gene signatures in numerous cancer types, which facilitate the scoring and positioning of these hybrid cancers along an EM spectrum [23,24,25]. A crucial property of hybrid cancer cell populations is the ability to escape the killing by cytotoxic immune cells. Cancer cells in various states of EMT secrete an array of cytokines, chemokines, and growth factors, which influence the differentiation, homing, and activity of various immune cell populations [26,27,28,29,30]. Below, we discuss the intricate cross-talk between layers of epithelial plasticity in cancer, including the core layer of transcription factors, their interaction with epigenetic modifiers and non-coding RNAs, and the manipulation of tumor immunogenicity during the transition between epithelial and mesenchymal states.
2. Epigenetics and the Transcription Factor Network
Although epigenetic modifications in cancer cells have been implicated in EMT, the extensive epigenetic reprogramming network driving plasticity is not fully understood. By definition, TFs are proteins that respond to stimuli from the extracellular environment and bind to specific DNA sequences with consequent regulation of gene expression. Therefore, TFs can stimulate or inhibit target gene expression during EMT induction and cancer progression [31]. Functionally, TFs involved in regulating epithelial plasticity are collectively referred to as EMT-TFs [32,33]. EMT-TFs bind specifically to their target genes through their different DNA-binding domains (Figure 2). Altered EMT-TF expression is frequently observed in cancers and studies have highlighted their contribution to cancer biology through various mechanisms. In addition to their DNA binding domains, EMT-TFs also vary in structure, as manifested by their different effector domains interacting with various epigenetic modifiers. These “epimodifiers” induce epigenetic modifications and chromatin remodeling in their target DNAs, leading to either gene activation or gene repression, as discussed in detail below (Figure 2).
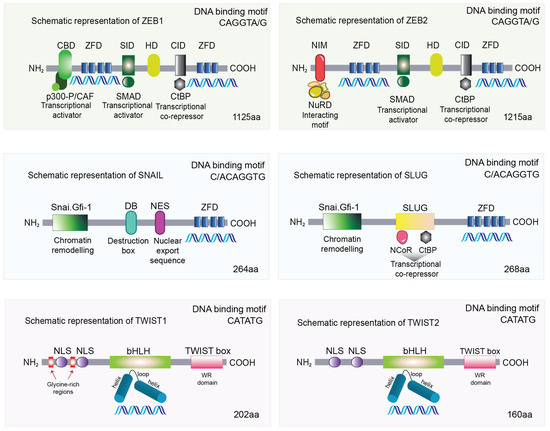
Figure 2.
Human ZEBs, SNAIL, SLUG, and TWISTs protein structure and interacting domains. NH2: N-terminus, COOH: C-terminus, CBD: CAF/P300 binding domain, ZFD: zinc finger domain, SID: Smad interaction domain, HD: Homeodomain, CID: CtBP interaction domain, NIM: NuRD interacting motif, NuRD: nucleosome remodeling and deacetylase complex, Snai.Gfi-1: SNAG domain, DB: destruction box, NES: nuclear export sequence, NCor: nuclear receptor co-repressor, NLS: nuclear localization signals, bHLH: basic helix-loop-helix, aa: amino acids.
2.1. SNAIL and SLUG
The first EMT-TFs molecularly characterized were SNAIL and SLUG [34,35]. Both SNAIL and SLUG contain tandem zinc-finger motifs on the C-terminus and a Snai/Gfi-1 (SNAG) repressor domain on the N-terminus (Figure 2). While differences exist with SNAIL containing four C2H2 zinc-finger motifs (cysteine/histidine, coordinating a zinc ion) and SLUG containing five, both share a high degree of homology and function as DNA-binding motifs targeting consensus E2-box type elements (C/ACAGGTG) [36]. Their SNAG domain is essential for nuclear localization and, on DNA binding, functions as a molecular hook to recruit co-repressors and epigenetic remodeling complexes, thereby exerting their role as transcriptional repressors. SNAG recruits histone lysine specific demethylase 1 (LSD1), which removes mono- and di-methylation at lysine 4 on histone H3 (H3K4me, H3K4me2) [37]. LSD1 is frequently associated with the CoREST ternary complex, which additionally associates with histone deacetylase HDAC1/2. Furthermore, LSD1 may have a dual role since, in addition to repression, it has been shown to alter H3 lysine 9 state by removing mono- and di-methylation, resulting in transcriptional activation [38].
The SNAG domain of SNAIL has also been shown to interact with HDAC1, HDAC2, and the co-repressor SIN3 transcription regulator homolog A (mSin3A) [39]. Further, in human breast cancer, SNAIL has been shown to interact with histone methyltransferase G9a inducing H3K9me2, and further recruit both G9a and DMNTs to the CDH1 promoter to induce DNA methylation and gene silencing [40].
In breast cancer, SLUG forms a complex with LSD1 and protein arginine methyltransferase 5 (PRMT5), which facilitates cancer invasion [41]. In addition, SNAIL can induce the repressive H3K27me3 mark via the recruitment of PRC2 together with the co-regulators LIM protein AJUBA and PRMT5 [42].
Differences between SNAIL and SLUG lie in the inclusion of a SLUG domain, an additional unique 28-amino acid sequence only present in the latter. Functional studies have found that SLUG interacts with the co-repressors NCoR and CtBP1, and deletion of the SLUG domain fully abolishes interaction with CtBP1 [43]. While the exact mechanism of the SLUG domain binding to epimodifiers is yet to be uncovered, this additional sequence renders the SLUG protein susceptible to post-translational modifications affecting proteolytic function and/or cellular localization [44].
The most notable target of both SNAIL and SLUG is the promoter of the CDH1 gene, which encodes the quintessentially epithelial protein, E-cadherin. Interaction between SNAIL and SLUG with epimodifiers through their SNAG domain is essential for repression of E-cadherin (CDH1). SNAIL and SLUG also bind to E-boxes in other key target epithelial genes in human breast cancer including claudin-1 [45], Muc1 [46,47], Vitamin D receptor [48], integrins [49], cytokeratins, and occludins [50,51].
In addition to epithelial proteins, SNAIL and SLUG are involved in the epigenetic repression of tumor suppressor genes involved in EMT. For example, SNAIL and SLUG have been shown to bind to E boxes (enhancer box) in the PTEN promoter, thereby negatively regulating PTEN expression [52,53,54]. Repression of PTEN contributes to the development of tumorigenesis, and resistance to PI3Kα inhibitors and targeted therapies, such as trastuzumab or doxorubicin [52,55,56,57]. Furthermore, PTEN exerts its tumor suppressive functions by inhibiting the PI3K-AKT pathway, which also controls EMT [52]. In contrast, SLUG is a negative regulator of BRCA2 in human breast cancer via recruitment of CtBP1 and HDAC1 at E boxes in the BRCA2 promoter [58].
2.2. TWIST1 and TWIST2
The basic helix-loop-helix (bHLH) family of proteins include a range of TFs containing a conserved domain characterized by two α-helices connected by a short inter-helical loop (Figure 2) [59]. These proteins are further classified into three subfamilies: classes A, B, and C. Class A proteins are ubiquitously expressed, whereas class B proteins have tissue specificity. In many instances, class B proteins form dimers with proteins of class A through interactions mediated by α-helices. This dimerization permits the binding to specific hexanucleotide E-box sequences (CATATG) leading to transcriptional regulation of target genes [60]. Twist-related proteins 1 and 2 (TWIST1 and TWIST2) fall into class B as they form dimers with class A proteins, particularly E proteins such as E12 and E47, which are critical regulators of B cell development [61]. Additionally, class B members form dimers with proteins belonging to the same class. Within the bHLH domain of class B TWIST lies a Thr-Gln-Ser (TQS) motif vital for promoting metastasis [62]. Upon phosphorylation, this motif modulates binding affinities with partner proteins specifying cell fate [63].
The TWIST1 and TWIST2 TFs have 100% structural similarity in the C-terminus Twist box, and 95% similarity in the bHLH region, while only 54% similarity in the N-terminus. The N-terminus contains two nuclear localization signals (NLS), mediating effective translocation to the nucleus required for DNA binding. The traditional view of mammalian TWIST function is that of inhibiting differentiation of mesenchymal cell lineages such as inhibition of myogenesis and osteogenesis. TWIST1 and TWIST2 display a bifunctional role as activators or repressors depending on the binding partner choice, chromatin accessibility and specific cell type. Overall, target promoters for TWIST1 and TWIST2 have multiple E-boxes suggesting combinations of several dimers could influence binding, thereby controlling transcriptional outcome.
The C-terminus 20 residue Twist box (also known as WR domain) is critical for TWIST transcriptional activity [64]. The TWIST1 N-terminal region contains an additional two glycine rich tracks rendering TWIST1 protein larger than TWIST2. Physical interaction between TWIST1 and p300, cAMP-response element binding protein (CREB), CREB-binding protein (CBP), and p300/CBP-associated factor (PCAF) is mediated by this N-terminal glycine-rich tracks that block histone acetyltransferase (HAT) activity [65]. TWIST2, lacking these additional glycine-rich tracks, does not have the ability to block HAT. Yet, both TWIST1 and TWIST2 have the ability to recruit HDACs, with TWIST1 previously shown to interact with several components of the Mi2/nucleosome remodeling and deacetylase (Mi2/NuRD) complex and Rb-associated protein 46 [66,67,68]. Of note, it has been demonstrated that TWIST1 in complex with E12 recruits Mi2/NuRD/MTA2 complex and directly interacts with MTA2 to repress CDH1 expression [66,69].
Both TWIST1 and TWIST2 also interact with other TFs including SMAD4, MyoD, MEF2, RUNX1/1, CEBP-α, and NF-ĸB [68,70,71,72,73,74,75]. Furthermore, TWIST1/2 proteins have the potential to interfere with the transcriptional activity of MyoB and MEF2 TFs, thereby inhibiting myogenic differentiation.
2.3. ZEB1 and ZEB2
The zinc-finger E homeobox-binding (ZEB) family of TFs contains two members, ZEB1 and ZEB2, which play a central role in cancer cell plasticity. ZEB proteins not only control global (genome-wide) reprogramming of plasticity [32,76,77], but also specific pathways including Hippo [78], Notch [79], and NF-κB [80].
Structurally, the ZEB proteins are highly homologous in the two C2H2 zinc-finger motifs located at the N- and C- termini (Figure 2). Both ZEB members bind to the paired E2-box type elements (CAGGTA/G) [81]. Along with the centrally located homeodomain, the zinc fingers mediate ZEB1 and ZEB2 binding at various target genes. Further, the interaction with repressive epimodifiers occurs via protein–protein binding domains including the SMAD binding domain and the CtBP interaction domain, both near the N-terminus of the ZEB TFs (Figure 2). Interestingly, ZEB1 contains binding domains for both p300 and P/CAF (close to the C-terminus) as well as an activation domain (N-terminus) rendering the protein a potential transcriptional activator. Interestingly, binding of ZEB1 with P/CAF acetylates lysine resides close to the N-terminal CtBP interaction domain, switching it from a transcriptional repressor to an activator, a feature which is not observed with the ZEB2 TFs.
Through its CtBP interaction domain, ZEB TFs are capable of interacting with the CtBP transcriptional co-repressor [82], which recruits histone deacetylases HDAC1/2. Depending on the chromatin context, in addition to HDAC1/2, CtBP-associated proteins also include histone methyltransferases G9a and EuHMT, chromodomain-containing proteins HPC2 and CDYL and CoREST [83]. While CtBP plays a key role in the ZEB1/2-mediated repression of CDH1, ZEB1 specifically acts as a transcriptional repressor via its interaction with BRG1 (BRM/SWI2 related gene 1), a component of the SWItch/sucrose non-fermentable (mSWI/SNF) chromatin remodeling complex. This complex has the capacity to bind to the minor grooves in DNA and utilize ATP to perturb histone–DNA interactions affecting the target chromatin structure [84].
SMADs are a group of intracellular proteins which are the main transducers of TGFβ signaling receptors, and are able to regulate gene transcription. The differential recruitment by ZEBs by SMAD proteins is evidenced by their powerful role as regulators of the TGFβ and BMP signaling pathways, which are involved in several cellular processes including cancer progression [85,86]. Members of the secretory TGFβ cytokine family, including TGFβ and BMP, stimulate the induction of SMAD proteins leading to nuclear translocation. Both ZEB1 and ZEB2 proteins bind to receptor regulated SMADs through their SMAD binding domain; however, ZEB1/2 have been shown to have antagonistic effects [87]. Once in complex, ZEB1 synergizes with SMAD-mediated transcriptional activation of downstream targets while ZEB2 represses it.
The ZEBs are best known as key drivers of EMT by repressing CDH1 and the pro-epithelial miR-200 family members. Downstream targets of ZEB1 and ZEB2 have been well studied in the context of breast cancer and include key genes involved in epithelial plasticity and cellular polarity genes [88,89,90]. By targeting promoters of pro-epithelial genes, ZEBs are dominant regulators of EMT and tumor progression. High ZEB expression is associated with poor prognosis, metastasis, and resistance to chemotherapy in a variety of cancer types [91]. Furthermore, there is increasing evidence of ZEB-mediated regulation of inflammatory responses, thereby supporting the TME and potentiating tumor growth [92].
3. Transcription Factor Cooperative Regulation
The EMT-TFs regulate important genes controlling cancer initiation, development, therapy resistance, and metastasis [93]. They have also been shown to functionally cooperate and regulate one another (Figure 3A). For example, in melanoma, ChIP assays identified SLUG as a direct activator of ZEB1 with the ability to bind to E-boxes within the ZEB1 promoter [94]. Whereas in hepatocellular carcinoma, SNAIL can both directly and indirectly activate ZEB1 transcription [95]. Similarly, in mouse breast epithelial cells treated with TGF-β to induce EMT, SNAIL, and TWIST cooperate in inducing ZEB1 transcription [96]. In the same study, SNAIL was able to increase both TWIST1 protein expression and stability.
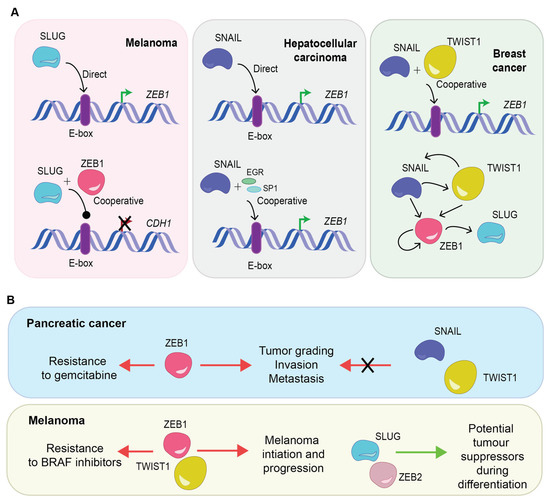
Figure 3.
(A) Schematic diagram demonstrating the interaction between EMT-TFs in different cancers with direct, indirect, and cooperative interactions observed. (B) Examples of the differential roles EMT-TFs can play in resistance with oncogenic functions, but may have the potential to act as tumor suppressors. E-box: enhancer box, EGR: transcription factor early growth response factor 1, SP1: transcription factor specificity protein 1.
Although EMT-TFs broadly converge to induce EMT programs, recent data supports the notion that each EMT-TF is involved in specialized, non-redundant and/or tissue-specific roles, orchestrating different functions in cancer pathobiology [97,98,99]. This intricate involvement, which remains elusive in many cancer types, fuels carcinoma cells with the plasticity to differentially activate many transcriptional programs and epigenetic landscapes. This is particularly important in the context of resistance and adaptation to particular insults, such as metabolic stress, DNA damage caused by chemotherapies and radiation, as well as other mechanisms of therapy-induced resistance [4,97,100].
It has been proposed that the capacity of carcinoma cells to exist in hybrid E/M phenotypes is controlled by the differing molecular roles and thus the differential expression of each EMT-TF [97,98]. For example, to drive hybrid E/M tumors to a fully mesenchymal phenotype in breast carcinoma cells requires ZEB1 expression. Not surprisingly, in breast tumors, ZEB1 expression levels are highly elevated in mesenchymal cell states [98]. In contrast, the highly tumorigenic hybrid E/M cell state is driven by SNAIL with more than five-fold protein increase in hybrid E/M states compared to mesenchymal cells. Whereas TWIST levels were elevated in both hybrid and mesenchymal populations as compared to epithelial cell states [98].
Importantly, there are specialized roles EMT-TFs play in resistance to a range of chemotherapies. In ovarian cancer, upregulation of SNAIL and SLUG has been directly correlated with resistance to cisplatin [101], paclitaxel [102], and radiation [102], as well as gefitinib resistance in lung cancer cell lines [103]. ZEB1 induces resistance to epirubicin in breast cancer [104], oxaliplatin in esophageal cancer [105], docetaxel in prostate cancer [106], and gemcitabine in pancreatic cancer [107]. In addition to resistance to particular agents, EMT can be induced after various treatments in a bid to adapt to cellular stress induced by treatments including chemo-, radio- and immune-based therapies [108].
While individual signals that trigger EMT have been identified, our understanding of the impact of the differential EMT-TF expression in the different cancer phenotypes remains elusive. However, some nuances have been characterized, as outlined in Figure 3B. In pancreatic cancer, depletion of ZEB1 affected tumor grading, invasion, and, importantly, metastasis in contrast with SNAIL and TWIST1 [32]. In breast cancer, however, SNAIL may also trigger metastasis [109]. During melanocytic differentiation, both SLUG and ZEB2 act as tumor suppressor proteins whereas ZEB1 and TWIST1 are oncogenic proteins driving melanoma initiation and progression [110]. This demonstrates the enormous flexibility of the biological effects of EMT-TFs in inducing metastasis and resistance to particular agents, depending on the cancer type. This flexibility could also be explained by tissue specific expression of EMT-TF partner proteins and the vast array of epigenetic modifiers each TF can recruit.
4. EMT-TFs Are Induced by Proinflammatory Mediators
In the same way that cellular plasticity provides cancer cells with the ability to adapt to the TME, this characteristic additionally confers the capacity to escape immune detection and elimination. EMT-TFs are central to the deployment of immune evasion mechanisms in cancer cells, which can be induced in the presence of chronic inflammation—a hallmark of cancer. In this context, further to the aforementioned TGF-β interaction [111,112], activation of EMT-TFs have been shown to be closely associated with other key pro-inflammatory mediators, including IFNγ [113,114], IL-1β [115,116], IL-6 [117,118,119], IL-8 [119,120], IL-1 [121], IL-23 [122], CCL2 [123,124], CCL5 [125,126], and CCL18 [127]. Together, these molecules promote chronic inflammation in the TME, and ultimately, foster the acquisition of EMT-like features in cancer cells. The origin of these inflammatory mediators varies within the tumor and may arise from various cell types, including polarized “M2-like” (Arg1high/CD206high/IL-10high) pro-tumoral macrophages (tumor-associated macrophages; TAMs) [128], myeloid-derived suppressor cells (MDSCs) [129], CD4+Foxp3+ regulatory T cells (Tregs) [130], and/or the tumor cells themselves [112]. Importantly, the persistent inflammatory environment within the tumor produced by these cells attracts additional immunosuppressive cells into the TME, promoting continued expression of EMT-TFs, and results in a detrimental positive feedback loop that drives tumor progression and inhibits anti-tumor immunity. For example, work by Su and colleagues [131], has shown that mesenchymal-like breast cancer cell lines have the capacity to polarize macrophages to an “M2-like” phenotype via their secretion of granulocyte-macrophage colony-stimulating factor (GM-CSF). These TAMs, in turn, produce elevated levels of CCL18, which induces EMT in breast cancer cells via the phosphatidylinositol 3-kinase (PI3K)/Akt/glycogen synthase kinase 3β (GSK3β)/SNAIL signaling pathway. This then initiates a positive feedback loop between GM-CSF from breast cancer cells and CCL18 from TAMs that was shown in their humanized mouse model to drive tumor metastasis in vivo. Furthermore, other studies have shown that sustained production of GM-CSF by tumor cells also promotes the induction or recruitment of MDSCs, which inhibit CD8+ T cell function and detrimentally impact the overall anti-tumor immune response [132,133]. These studies highlight that interactions between tumor cells and other cells in the TME are highly complex and have the capacity to significantly impact the anti-tumor immune response.
5. EMT-TFs Facilitate Immune Evasion
In recent years, major advancements have been made in the development and application of cancer immunotherapies, including immune checkpoint inhibitors (ICIs) and adoptive cell therapy (ACT). However, despite these breakthroughs, low response rates and therapeutic resistance remain major obstacles to achieving clinical benefit across patients, particularly in solid cancer types. The poor response and acquired resistance seen in some patients is, in part, due to EMT-driven immune evasion and tumor-related immunosuppression. Although current cancer immunotherapies have the capacity to target major immune checkpoints such as PD-1, PD-L1, or CTLA-4 to galvanize the anti-cancer T cell response [134,135,136], numerous other immune regulatory checkpoints are also upregulated on the surface of EMT cancers, including CD73 [137], CD155 [138], PD-L2 [139], and HVEM [140], which are not addressed by current ICI therapies. Activation of these alternative immune checkpoints hinders effective anti-tumor immune responses.
Moreover, EMT-TFs have been shown to be associated with reduced expression of major histocompatibility complex (MHC) Class I [141,142], which plays a pivotal role in the presentation of tumor antigens on the tumor cell surface for recognition by CD8+ T cells and activation of cytotoxic T cell responses [143]. In addition to reduced MHC Class I expression, Tripathi and colleagues [144] showed that EMT in lung cancer cell lines results in reduced expression of various immunoproteasome components (IRF1, STAT1, PSMB8, PSMB9, and PSMB10), which are required for efficient antigen processing and presentation by MHC Class I. This depletion of the immunoproteasome was found to reduce the repertoire of MHC Class I-bound peptides and impede cancer cell recognition and killing by CD8+ T cells. Interestingly, immunoproteasome deficiency and lack of MHC Class I was restored in this study by treatment with the inhibitor of DNA methylation 5-aza-2′-deoxycytidine, suggesting an epigenetic mechanism of repression in EMT to facilitate immune evasion. Alternatively, other studies have shown that direct knockout of EMT-TFs can abrogate tumor immunosuppression, improve local infiltration of CD8+ T cells, and induce systemic anti-tumor immune responses [112].
Aside from MHC Class I, EMT-TFs have previously been shown to activate the inhibitory immune receptors killer Ig-like receptors (KIR) KIR3DL1, KIR2DL1, KIR2DL3, and KIR2DL4 [145], and repress activating immune-receptor natural killer group member D (NKG2D) ligands UL-16 binding protein (ULBP) 1 [146] and ULBP2 [147] on the tumor cell surface. Interestingly, Lopez-Soto and colleagues [147] showed that induction of EMT in colorectal cancer cells via SNAIL overexpression induced upregulation of the NKG2D ligands MICA/B and ULBP2, suggesting an avenue for NKG2D-mediated natural killer (NK) cell immunotherapy [148]. However, follow-up experiments identified that levels of soluble MICA were also elevated in the SNAIL-activated tumors, which act as a decoy to limit anti-cancer surveillance by NK cells. This highlights the potential for different evasion mechanisms to be simultaneously involved in the context of EMT.
6. Non-Coding RNAs Add Another Layer of Intricacy
Until recently, the role of non-coding RNAs (ncRNAs) in EMT was limited. With the realization of their involvement in numerous diseases, such as cancer, there has been a plethora of interest in their role and functions in epithelial plasticity. Non-coding RNAs are functional RNA moieties that do not require translation into protein for their action [149].
Although there are several categories of ncRNAs, they are loosely divided into two main groups based on their length. One of the most studied groups of ncRNAs are microRNAs (miRNAs), which are small, single-stranded non-coding RNAs approximately 18–22 nucleotides in length. MicroRNAs play a crucial regulatory role in the behavior of every biological process as they contain a “seed sequence” complementary to the 3′UTR (untranslated region) of target mRNA, which in most cases facilitates binding and degradation. Under certain conditions, miRNAs have also been shown to induce gene expression [150,151,152].
There are over 2600 known mature miRNAs (miRBase v2.2 [153]) which are involved in the regulation of >60% of human protein coding genes. In cancer, they have been shown to act as either oncogenes or tumor suppressors. Numerous miRNA signatures have been described for various stages of cancer initiation and progression. Therefore, in-depth research has been directed to understanding the role of miRNAs in cancer progression and metastasis. The role of miRNAs in EMT-TF regulation is well established and many of them participate in feedback loops with EMT-TFs [11,19,154]. Therefore, miRNAs’ regulatory interaction with TFs are crucial contributors of cancer cell plasticity.
In particular, the negative feedback loop of members of the miR-200 family with the ZEBs has been extensively investigated [13,155]. Members from the miR-200 and miR-205 families can repress expression of ZEB1 and ZEB2 by binding to 3′ untranslated regions of mRNA, thus preventing translation [12,13]. There is also a feedback loop between miR-34 and SNAIL. In the SNAIL 3′UTR lies a conserved seed sequence facilitating binding of miR-34a/b/c. Ectopic miR-34a results in direct downregulation of SNAIL mRNA and protein resulting in the induction of MET [156]. Other well-established interactions include miR-137/SNAIL, let-7/SNAIL, miR-218/SLUG, miR-218/ZEB2, miR-203/SNAIL, and miR-203/SLUG (extensively reviewed in [19,154,157,158]).
Considering their role in both tumor pathogenesis and EMT modulation, miRNAs are emerging as epigenetic players in cancer immune evasion. Multiple miRNA (>50) regulate the expression of PD-L1, such as miR-142 in pancreatic cancer [159], miR-138 in colorectal cancer [160], and miR-570 in hepatocellular carcinoma [161]. Similarly, in lung cancer, regulation of PD-L1 expression has been linked to the miR-200/ZEB1 axis [134]. Additionally, indirect epigenetic regulation of PD-L1 expression by miRNAs occurs through regulation of signaling pathways, including activation of STATs, PI3K/Akt, and suppression of PTEN [162]. A direct inhibitor of SNAIL and EMT in breast and ovarian cancers, miR-34a inhibits the expression of PD-L1 in acute myeloid leukemia [163].
Unlike their smaller ncRNA counterparts, long non-coding RNAs (lncRNA) are underexplored and remain an untapped resource in cancer therapeutics. With advancement in transcriptomic profiling, there is mounting evidence of lncRNA contribution in modulating EMT-TFs, thereby affecting regulation of cancer cell plasticity [164,165,166,167,168,169]. LncRNAs vary in length, ranging from 200 nucleotides up to ~100 kilobases and do not translate into proteins. In prostate cancer, antisense lncRNA ZEB1-AS1, which is co-expressed with ZEB1, epigenetically activates ZEB1 by recruiting the histone methyltransferase MLL1 [170]. Interestingly, lncRNA ZEB2-AS1 contains a complementary sequence to a splice site located in the 5′UTR ZEB2 intron. This particular region in the intron contains an internal ribosome entry site. Upon ZEB2-AS1 binding, splicing of this region is disrupted, thereby improving ZEB2 translation efficiency and increasing overall ZEB2 protein levels [171].
Evidence exists of interactions between lncRNAs and miRNAs affecting PD-L1 expression. In prostate cancer, lncRNA KCNQ1OT1 negatively regulates miR-15a by direct binding, which in turn affects PD-L1 expression, thus promoting immune evasion [172]. In hepatocellular carcinoma, lncRNA-ATB binds to IL11 mRNA, increasing its stability and triggering the oncogenic STAT3 signaling [173]. Competitively binding with miR-200 family members, lncRNA-ATB is also able to increase ZEB1 and ZEB2 expression levels. One of the most well-studied lncRNAs is the HOX transcript antisense RNA (HOTAIR), upregulated in several cancers including cervical cancer [174], gastric cancer [175], lung cancer [176], and breast cancer [177]. Knockdown of HOTAIR directly impairs EMT in cancer cells, reducing migration and invasion [178]. In colorectal cancer cells, HOTAIR directly binds and recruits SNAIL to regulate a transcription factor, HNF-4α [178]. However, it can also act indirectly by downregulating miRNAs, such as miR-7 a regulator of the SETDB1 and STAT3 pathway in breast cancer [177].
7. Conclusions
The traditional binary view of EMT has been challenged by the concept of epithelial-mesenchymal plasticity, suggesting that tumor cells can exist in intermediate hybrid E/M states (Figure 4). The expression of particular EMT-TF combinations by tumor cells determines their capacity to reside in different cell states (or hybrid E/M phenotypes). Increasingly, these intermediary states are being understood as essential for the activation of metastasis and resistance to particular agents in different cancers. Mounting research has also identified that, in addition to differential expression of EMT-TFs, the presence of particular co-factors and epigenetic regulators, miRNAs, and lncRNAs, provide additional layers of regulation to shape epithelial plasticity. Moreover, pro-inflammatory mediators such as IFNγ, IL-1β, and IL-6 also induce EMT-TFs, leading to chronic inflammation in the tumor microenvironment, immune escape, and the acquisition of EMT-like features in tumor cells. Altogether, understanding these regulatory processes provides mechanistic insights into tumor development and progression, and opens avenues for therapeutic intervention and treatment.
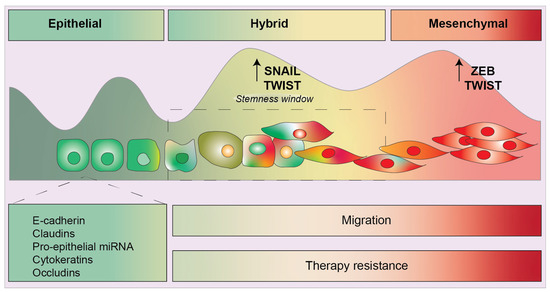
Figure 4.
Schematic diagram displaying the several phenotypes along the epithelial to mesenchymal spectrum. Epithelial characteristics include expression of cadherins, cytokeratins, pro-epithelial miRNA, and occludins. Hybrid phenotypes give rise to a stemness/plasticity window where cells contain equal expression of epithelial and mesenchymal features. Recent studies have shown that SNAIL is important to maintain this hybrid feature whereas ZEB1 is required to fully push hybrid cells to a completely mesenchymal phenotype.
Author Contributions
Conceptualization, C.W. and P.B.; writing—original draft preparation, C.W. and E.A.; writing—review and editing, C.W., E.A., R.M., R.D., E.W.T., A.R. and P.B.; visualization, C.W.; funding acquisition, P.B. All authors have read and agreed to the published version of the manuscript.
Funding
P.B. is the recipient of the following Fellowships and Awards: Australian Research Council Future Fellowship FT130101767; a Cancer Council of Western Australia Research Fellowship; a Wesfarmers Fellowship in Women’s Cancers and Future Health Research and Innovation (FHRI); NHMRC APP1147528 (with A.R. and E.W.T.), APP1165208, and APP1187328 (with R.M. and R.D.); CBCF-NBCF Brain and Breast Cancer Research Collaboration Initiative 19-009, National Breast Cancer Foundation IIRS-22-044; Cancer Council New South Wales APP2013068 and Cancer Council Western Australia 2022/RPG0057 (with A.R. and C.W.). E.A. is a recipient of an Australian Government Research Training Program Scholarship at The University of Western Australia, BioZone PhD Scholarship at the University of Western Australia, Cancer Council WA PhD Top Up Scholarship and Tour de Cure PhD Support Scholarship.
Acknowledgments
P.B. and C.W. would like to acknowledge the Brenkley family for their family donation supporting breast cancer research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Greenburg, G.; Hay, E.D. Epithelia Suspended in Collagen Gels Can Lose Polarity and Express Characteristics of Migrating Mesenchymal Cells. J. Cell Biol. 1982, 95, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Kalluri, R.; Weinberg, R.A. The basics of epithelial-mesenchymal transition. J. Clin. Investig. 2009, 119, 1420–1428. [Google Scholar] [CrossRef]
- Lachat, C.; Peixoto, P.; Hervouet, E. Epithelial to Mesenchymal Transition History: From Embryonic Development to Cancers. Biomolecules 2021, 11, 782. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Antin, P.; Berx, G.; Blanpain, C.; Brabletz, T.; Bronner, M.; Campbell, K.; Cano, A.; Casanova, J.; Christofori, G.; et al. Guidelines and definitions for research on epithelial-mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2020, 21, 341–352. [Google Scholar] [CrossRef]
- San Juan, B.P.; Garcia-Leon, M.J.; Rangel, L.; Goetz, J.G.; Chaffer, C.L. The Complexities of Metastasis. Cancers 2019, 11, 1575. [Google Scholar] [CrossRef] [PubMed]
- Jolly, M.K.; Boareto, M.; Huang, B.; Jia, D.; Lu, M.; Ben-Jacob, E.; Onuchic, J.N.; Levine, H. Implications of the Hybrid Epithelial/Mesenchymal Phenotype in Metastasis. Front. Oncol. 2015, 5, 155. [Google Scholar] [CrossRef] [PubMed]
- Jolly, M.K.; Murphy, R.J.; Bhatia, S.; Whitfield, H.J.; Redfern, A.; Davis, M.J.; Thompson, E.W. Measuring and Modelling the Epithelial- Mesenchymal Hybrid State in Cancer: Clinical Implications. Cells Tissues Organs 2022, 211, 110–133. [Google Scholar] [CrossRef]
- Shibue, T.; Weinberg, R.A. EMT, CSCs, and drug resistance: The mechanistic link and clinical implications. Nat. Rev. Clin. Oncol. 2017, 14, 611–629. [Google Scholar] [CrossRef]
- Grosse-Wilde, A.; D’hérouël, A.F.; McIntosh, E.; Ertaylan, G.; Skupin, A.; Kuestner, R.E.; del Sol, A.; Walters, K.-A.; Huang, S. Stemness of the hybrid Epithelial/Mesenchymal State in Breast Cancer and Its Association with Poor Survival. PLoS ONE 2015, 10, e0126522. [Google Scholar] [CrossRef]
- Lamouille, S.; Xu, J.; Derynck, R. Molecular mechanisms of epithelial-mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2014, 15, 178–196. [Google Scholar] [CrossRef]
- Cursons, J.; Pillman, K.A.; Scheer, K.G.; Gregory, P.A.; Foroutan, M.; Hediyeh-Zadeh, S.; Toubia, J.; Crampin, E.J.; Goodall, G.J.; Bracken, C.P.; et al. Combinatorial Targeting by MicroRNAs Co-ordinates Post-transcriptional Control of EMT. Cell Syst. 2018, 7, 77–91.e77. [Google Scholar] [CrossRef]
- Gregory, P.A.; Bert, A.G.; Paterson, E.L.; Barry, S.C.; Tsykin, A.; Farshid, G.; Vadas, M.A.; Khew-Goodall, Y.; Goodall, G.J. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat. Cell Biol. 2008, 10, 593–601. [Google Scholar] [CrossRef]
- Bracken, C.P.; Gregory, P.A.; Kolesnikoff, N.; Bert, A.G.; Wang, J.; Shannon, M.F.; Goodall, G.J. A double-negative feedback loop between ZEB1-SIP1 and the microRNA-200 family regulates epithelial-mesenchymal transition. Cancer Res. 2008, 68, 7846–7854. [Google Scholar] [CrossRef] [PubMed]
- Mani, S.A.; Guo, W.; Liao, M.-J.; Eaton, E.N.; Ayyanan, A.; Zhou, A.Y.; Brooks, M.; Reinhard, F.; Zhang, C.C.; Shipitsin, M.; et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 2008, 133, 704–715. [Google Scholar] [CrossRef] [PubMed]
- Gregory, P.A.; Bracken, C.P.; Bert, A.G.; Goodall, G.J. MicroRNAs as regulators of epithelial-mesenchymal transition. Cell Cycle 2008, 7, 3112–3118. [Google Scholar] [CrossRef]
- Zhan, T.; Rindtorff, N.; Boutros, M. Wnt signaling in cancer. Oncogene 2017, 36, 1461–1473. [Google Scholar] [CrossRef] [PubMed]
- Thiery, J.P.; Sleeman, J.P. Complex networks orchestrate epithelial-mesenchymal transitions. Nat. Rev. Mol. Cell Biol. 2006, 7, 131–142. [Google Scholar] [CrossRef]
- Sahlgren, C.; Gustafsson, M.V.; Jin, S.; Poellinger, L.; Lendahl, U. Notch signaling mediates hypoxia-induced tumor cell migration and invasion. Proc. Natl. Acad. Sci. USA 2008, 105, 6392–6397. [Google Scholar] [CrossRef]
- Pan, G.; Liu, Y.; Shang, L.; Zhou, F.; Yang, S. EMT-associated microRNAs and their roles in cancer stemness and drug resistance. Cancer Commun. 2021, 41, 199–217. [Google Scholar] [CrossRef]
- Drak Alsibai, K.; Meseure, D. Tumor microenvironment and noncoding RNAs as co-drivers of epithelial-mesenchymal transition and cancer metastasis. Dev. Dyn. 2018, 247, 405–431. [Google Scholar] [CrossRef]
- Pastushenko, I.; Blanpain, C. EMT Transition States during Tumor Progression and Metastasis. Trends Cell Biol. 2019, 29, 212–226. [Google Scholar] [CrossRef] [PubMed]
- Pastushenko, I.; Brisebarre, A.; Sifrim, A.; Fioramonti, M.; Revenco, T.; Boumahdi, S.; Van Keymeulen, A.; Brown, D.; Moers, V.; Lemaire, S.; et al. Identification of the tumour transition states occurring during EMT. Nature 2018, 556, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Murakami, R.; Matsumura, N.; Mandai, M.; Yoshihara, K.; Tanabe, H.; Nakai, H.; Yamanoi, K.; Abiko, K.; Yoshioka, Y.; Hamanishi, J.; et al. Establishment of a Novel Histopathological Classification of High-Grade Serous Ovarian Carcinoma Correlated with Prognostically Distinct Gene Expression Subtypes. Am. J. Pathol. 2016, 186, 1103–1113. [Google Scholar] [CrossRef] [PubMed]
- Chae, Y.K.; Chang, S.; Ko, T.; Anker, J.; Agte, S.; Iams, W.; Choi, W.M.; Lee, K.; Cruz, M. Epithelial-mesenchymal transition (EMT) signature is inversely associated with T-cell infiltration in non-small cell lung cancer (NSCLC). Sci. Rep. 2018, 8, 2918. [Google Scholar] [CrossRef]
- Vasaikar, S.V.; Deshmukh, A.P.; Hollander, P.D.; Addanki, S.; Kuburich, N.A.; Kudaravalli, S.; Joseph, R.; Chang, J.T.; Soundararajan, R.; Mani, S.A. EMTome: A resource for pan-cancer analysis of epithelial-mesenchymal transition genes and signatures. Br. J. Cancer 2021, 124, 259–269. [Google Scholar] [CrossRef]
- Ray, I.; Michael, A.; Meira, L.B.; Ellis, P.E. The Role of Cytokines in Epithelial-Mesenchymal Transition in Gynaecological Cancers: A Systematic Review. Cells 2023, 12, 416. [Google Scholar] [CrossRef]
- Adekoya, T.O.; Richardson, R.M. Cytokines and Chemokines as Mediators of Prostate Cancer Metastasis. Int. J. Mol. Sci. 2021, 21, 4449. [Google Scholar] [CrossRef]
- Bhat, A.A.; Nisar, S.; Singh, M.; Ashraf, B.; Masoodi, T.; Prasad, C.P.; Sharma, A.; Maacha, S.; Karedath, T.; Hashem, S.; et al. Cytokine- and chemokine-induced inflammatory colorectal tumor microenvironment: Emerging avenue for targeted therapy. Cancer Commun. 2022, 42, 689–715. [Google Scholar] [CrossRef]
- Bhat, A.A.; Nisar, S.; Maacha, S.; Carneiro-Lobo, T.C.; Akhtar, S.; Siveen, K.S.; Wani, N.A.; Rizwan, A.; Bagga, P.; Singh, M.; et al. Cytokine-chemokine network driven metastasis in esophageal cancer; promising avenue for targeted therapy. Mol. Cancer 2021, 20, 2. [Google Scholar] [CrossRef]
- Sistigu, A.; Di Modugno, F.; Manic, G.; Nistico, P. Deciphering the loop of epithelial-mesenchymal transition, inflammatory cytokines and cancer immunoediting. Cytokine Growth Factor Rev. 2017, 36, 67–77. [Google Scholar] [CrossRef]
- Chaffer, C.L.; San Juan, B.P.; Lim, E.; Weinberg, R.A. EMT, cell plasticity and metastasis. Cancer Metastasis Rev. 2016, 35, 645–654. [Google Scholar] [CrossRef]
- Krebs, A.M.; Mitschke, J.; Lasierra Losada, M.; Schmalhofer, O.; Boerries, M.; Busch, H.; Boettcher, M.; Mougiakakos, D.; Reichardt, W.; Bronsert, P.; et al. The EMT-activator Zeb1 is a key factor for cell plasticity and promotes metastasis in pancreatic cancer. Nat. Cell Biol. 2017, 19, 518–529. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Tam, W.L.; Shibue, T.; Kaygusuz, Y.; Reinhardt, F.; Eaton, E.N.; Weinberg, R.A. Distinct EMT programs control normal mammary stem cells and tumour-initiating cells. Nature 2015, 525, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Nieto, M.A.; Bennett, M.F.; Sargent, M.G.; Wilkinson, D.G. Cloning and developmental expression of Sna, a murine homologue of the Drosophila snail gene. Development 1992, 116, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.E.; Franco del Amo, F.; Gridley, T. Isolation of Sna, a mouse gene homologous to the Drosophila genes snail and escargot: Its expression pattern suggests multiple roles during postimplantation development. Development 1992, 116, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Prokop, J.W.; Liu, Y.; Milsted, A.; Peng, H.; Rauscher, F.J., 3rd. A method for in silico identification of SNAIL/SLUG DNA binding potentials to the E-box sequence using molecular dynamics and evolutionary conserved amino acids. J. Mol. Model. 2013, 19, 3463–3469. [Google Scholar] [CrossRef]
- Lin, Y.; Wu, Y.; Li, J.; Dong, C.; Ye, X.; Chi, Y.-I.; Evers, B.M.; Zhou, B.P. The SNAG domain of Snail1 functions as a molecular hook for recruiting lysine-specific demethylase 1. EMBO J. 2010, 29, 1803–1816. [Google Scholar] [CrossRef]
- Metzger, E.; Wissmann, M.; Yin, N.; Müller, J.M.; Schneider, R.; Peters, A.H.F.M.; Günther, T.; Buettner, R.; Schüle, R. LSD1 demethylates repressive histone marks to promote androgen-receptor-dependent transcription. Nature 2005, 437, 436–439. [Google Scholar] [CrossRef]
- Peinado, H.; Ballestar, E.; Esteller, M.; Cano, A. Snail mediates E-cadherin repression by the recruitment of the Sin3A/histone deacetylase 1 (HDAC1)/HDAC2 complex. Mol. Cell Biol. 2004, 24, 306–319. [Google Scholar] [CrossRef]
- Dong, C.; Wu, Y.; Yao, J.; Wang, Y.; Yu, Y.; Rychahou, P.; Evers, B.M.; Zhou, B.P. G9a interacts with Snail and is critical for Snail-mediated E-cadherin repression in human breast cancer. J. Clin. Investig. 2012, 122, 1469–1486. [Google Scholar] [CrossRef]
- Zhang, J.; Fan, X.; Zhou, Y.; Chen, L.; Rao, H. The PRMT5-LSD1 axis confers Slug dual transcriptional activities and promotes breast cancer progression. J. Exp. Clin. Cancer Res. 2022, 41, 191. [Google Scholar] [CrossRef]
- Hou, Z.; Peng, H.; Ayyanathan, K.; Yan, K.-P.; Langer, E.M.; Longmore, G.D.; Rauscher, F.J. The LIM protein AJUBA recruits protein arginine methyltransferase 5 to mediate SNAIL-dependent transcriptional repression. Mol. Cell. Biol. 2008, 28, 3198–3207. [Google Scholar] [CrossRef] [PubMed]
- Molina-Ortiz, P.; Villarejo, A.; MacPherson, M.; Santos, V.; Montes, A.; Souchelnytskyi, S.; Portillo, F.; Cano, A. Characterization of the SNAG and SLUG domains of Snail2 in the repression of E-cadherin and EMT induction: Modulation by serine 4 phosphorylation. PLoS ONE 2012, 7, e36132. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Gross, K.M.; Kuperwasser, C. Molecular regulation of Snai2 in development and disease. J. Cell Sci. 2019, 132, jcs235127. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Estrada, O.M.; Cullerés, A.; Soriano, F.X.; Peinado, H.; Bolós, V.; Martínez, F.O.; Reina, M.; Cano, A.; Fabre, M.; Vilaró, S. The transcription factors Slug and Snail act as repressors of Claudin-1 expression in epithelial cells. Biochem. J. 2006, 394, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Guaita, S.; Puig, I.; Francí, C.; Garrido, M.; Domínguez, D.; Batlle, E.; Sancho, E.; Dedhar, S.; de Herreros, A.G.; Baulida, J. Snail induction of epithelial to mesenchymal transition in tumor cells is accompanied by MUC1 repression and ZEB1 expression. J. Biol. Chem. 2002, 277, 39209–39216. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.; Kuperwasser, C. SLUG: Critical regulator of epithelial cell identity in breast development and cancer. Cell Adh. Migr. 2014, 8, 578–587. [Google Scholar] [CrossRef]
- Mittal, M.K.; Myers, J.N.; Misra, S.; Bailey, C.K.; Chaudhuri, G. In vivo binding to and functional repression of the VDR gene promoter by SLUG in human breast cells. Biochem. Biophys. Res. Commun. 2008, 372, 30–34. [Google Scholar] [CrossRef]
- Turner, F.E.; Broad, S.; Khanim, F.L.; Jeanes, A.; Talma, S.; Hughes, S.; Tselepis, C.; Hotchin, N. Slug regulates integrin expression and cell proliferation in human epidermal keratinocytes. J. Biol. Chem. 2006, 281, 21321–21331. [Google Scholar] [CrossRef]
- Tripathi, M.K.; Misra, S.; Chaudhuri, G. Negative regulation of the expressions of cytokeratins 8 and 19 by SLUG repressor protein in human breast cells. Biochem. Biophys. Res. Commun. 2005, 329, 508–515. [Google Scholar] [CrossRef]
- Ikenouchi, J.; Matsuda, M.; Furuse, M.; Tsukita, S. Regulation of tight junctions during the epithelium-mesenchyme transition: Direct repression of the gene expression of claudins/occludin by Snail. J. Cell Sci. 2003, 116, 1959–1967. [Google Scholar] [CrossRef]
- Moses, C.; Nugent, F.; Waryah, C.B.; Garcia-Bloj, B.; Harvey, A.R.; Blancafort, P. Activating PTEN Tumor Suppressor Expression with the CRISPR/dCas9 System. Mol. Ther. Nucleic Acids 2019, 14, 287–300. [Google Scholar] [CrossRef]
- Escriva, M.; Peiró, S.; Herranz, N.; Villagrasa, P.; Dave, N.; Montserrat-Sentís, B.; Murray, S.A.; Francí, C.; Gridley, T.; Virtanen, I.; et al. Repression of PTEN phosphatase by Snail1 transcriptional factor during gamma radiation-induced apoptosis. Mol. Cell. Biol. 2008, 28, 1528–1540. [Google Scholar] [CrossRef]
- Uygur, B.; Abramo, K.; Leikina, E.; Vary, C.; Liaw, L.; Wu, W.-S. SLUG is a direct transcriptional repressor of PTEN tumor suppressor. Prostate 2015, 75, 907–916. [Google Scholar] [CrossRef]
- Costa, C.; Wang, Y.; Ly, A.; Hosono, Y.; Murchie, E.; Walmsley, C.S.; Huynh, T.; Healy, C.; Peterson, R.; Yanase, S.; et al. PTEN Loss Mediates Clinical Cross-Resistance to CDK4/6 and PI3Kalpha Inhibitors in Breast Cancer. Cancer Discov. 2020, 10, 72–85. [Google Scholar] [CrossRef] [PubMed]
- Nagata, Y.; Lan, K.-H.; Zhou, X.; Tan, M.; Esteva, F.J.; Sahin, A.A.; Klos, K.S.; Li, P.; Monia, B.P.; Nguyen, N.T.; et al. PTEN activation contributes to tumor inhibition by trastuzumab, and loss of PTEN predicts trastuzumab resistance in patients. Cancer Cell 2004, 6, 117–127. [Google Scholar] [CrossRef]
- Steelman, L.S.; Navolanic, P.M.; Sokolosky, M.L.; Taylor, J.R.; Lehmann, B.D.; Chappell, W.H.; Abrams, S.L.; Wong, E.W.T.; Stadelman, K.M.; Terrian, D.M.; et al. Suppression of PTEN function increases breast cancer chemotherapeutic drug resistance while conferring sensitivity to mTOR inhibitors. Oncogene 2008, 27, 4086–4095. [Google Scholar] [CrossRef]
- Tripathi, M.K.; Misra, S.; Khedkar, S.V.; Hamilton, N.; Irvin-Wilson, C.; Sharan, C.; Sealy, L.; Chaudhuri, G. Regulation of BRCA2 gene expression by the SLUG repressor protein in human breast cells. J. Biol. Chem. 2005, 280, 17163–17171. [Google Scholar] [CrossRef]
- Murre, C.; McCaw, P.S.; Vaessin, H.; Caudy, M.; Jan, L.; Jan, Y.; Cabrera, C.V.; Buskin, J.N.; Hauschka, S.D.; Lassar, A.B.; et al. Interactions between heterologous helix-loop-helix proteins generate complexes that bind specifically to a common DNA sequence. Cell 1989, 58, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Ledent, V.; Vervoort, M. The basic helix-loop-helix protein family: Comparative genomics and phylogenetic analysis. Genome Res. 2001, 11, 754–770. [Google Scholar] [CrossRef] [PubMed]
- Beck, K.; Peak, M.M.; Ota, T.; Nemazee, D.; Murre, C. Distinct roles for E12 and E47 in B cell specification and the sequential rearrangement of immunoglobulin light chain loci. J. Exp. Med. 2009, 206, 2271–2284. [Google Scholar] [CrossRef] [PubMed]
- Gajula, R.P.; Chettiar, S.T.; Williams, R.D.; Nugent, K.; Kato, Y.; Wang, H.; Malek, R.; Taparra, K.; Cades, J.; Annadanam, A.; et al. Structure-function studies of the bHLH phosphorylation domain of TWIST1 in prostate cancer cells. Neoplasia 2015, 17, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Firulli, A.B.; Conway, S.J. Phosphoregulation of Twist1 provides a mechanism of cell fate control. Curr. Med. Chem. 2008, 15, 2641–2647. [Google Scholar] [CrossRef]
- Gajula, R.P.; Chettiar, S.T.; Williams, R.D.; Thiyagarajan, S.; Kato, Y.; Aziz, K.; Wang, R.; Gandhi, N.; Wild, A.T.; Vesuna, F.; et al. The twist box domain is required for Twist1-induced prostate cancer metastasis. Mol. Cancer Res. 2013, 11, 1387–1400. [Google Scholar] [CrossRef]
- Hamamori, Y.; Sartorelli, V.; Ogryzko, V.; Puri, P.L.; Wu, H.-Y.; Wang, J.Y.; Nakatani, Y.; Kedes, L. Regulation of histone acetyltransferases p300 and PCAF by the bHLH protein twist and adenoviral oncoprotein E1A. Cell 1999, 96, 405–413. [Google Scholar] [CrossRef]
- Fu, J.; Qin, L.; He, T.; Qin, J.; Hong, J.; Wong, J.; Liao, L.; Xu, J. The TWIST/Mi2/NuRD protein complex and its essential role in cancer metastasis. Cell Res. 2011, 21, 275–289. [Google Scholar] [CrossRef]
- Koh, H.S.; Lee, C.; Lee, K.S.; Park, E.J.; Seong, R.H.; Hong, S.; Jeon, S.H. Twist2 regulates CD7 expression and galectin-1-induced apoptosis in mature T-cells. Mol. Cells 2009, 28, 553–558. [Google Scholar] [CrossRef]
- Gong, X.Q.; Li, L. Dermo-1, a multifunctional basic helix-loop-helix protein, represses MyoD transactivation via the HLH domain, MEF2 interaction, and chromatin deacetylation. J. Biol. Chem. 2002, 277, 12310–12317. [Google Scholar] [CrossRef]
- Kim, J.Y.; Park, M.; Ohn, J.; Seong, R.H.; Chung, J.H.; Kim, K.H.; Jo, S.J.; Kwon, O. Twist2-driven chromatin remodeling governs the postnatal maturation of dermal fibroblasts. Cell Rep. 2022, 39, 110821. [Google Scholar] [CrossRef]
- Li, C.W.; Xia, W.; Huo, L.; Lim, S.-O.; Wu, Y.; Hsu, J.L.; Chao, C.-H.; Yamaguchi, H.; Yang, N.-K.; Ding, Q.; et al. Epithelial-mesenchymal transition induced by TNF-alpha requires NF-kappaB-mediated transcriptional upregulation of Twist1. Cancer Res. 2012, 72, 1290–1300. [Google Scholar] [CrossRef] [PubMed]
- Ioannou, M.; Kouvaras, E.; Papamichali, R.; Samara, M.; Chiotoglou, I.; Koukoulis, G. Smad4 and epithelial-mesenchymal transition proteins in colorectal carcinoma: An immunohistochemical study. J. Mol. Histol. 2018, 49, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Chen, K.; Zhang, Y.; Barnes, S.D.; Jaichander, P.; Zheng, Y.; Hassan, M.; Malladi, V.S.; Skapek, S.X.; Xu, L.; et al. Twist2 amplification in rhabdomyosarcoma represses myogenesis and promotes oncogenesis by redirecting MyoD DNA binding. Genes Dev. 2019, 33, 626–640. [Google Scholar] [CrossRef]
- Cripps, R.M.; Black, B.L.; Zhao, B.; Lien, C.-L.; Schulz, R.A.; Olson, E.N. The myogenic regulatory gene Mef2 is a direct target for transcriptional activation by Twist during Drosophila myogenesis. Genes Dev. 1998, 12, 422–434. [Google Scholar] [CrossRef] [PubMed]
- Sharabi, A.B.; Aldrich, M.; Šošić, A.; Olson, E.N.; Friedman, A.D.; Lee, S.-H.; Chen, S.-Y. Twist-2 controls myeloid lineage development and function. PLoS Biol. 2008, 6, e316. [Google Scholar] [CrossRef] [PubMed]
- Pham, C.G.; Bubici, C.; Zazzeroni, F.; Knabb, J.R.; Papa, S.; Kuntzen, C.; Franzoso, G. Upregulation of Twist-1 by NF-kappaB blocks cytotoxicity induced by chemotherapeutic drugs. Mol. Cell Biol. 2007, 27, 3920–3935. [Google Scholar] [CrossRef]
- Chaffer, C.L.; Marjanovic, N.D.; Lee, T.; Bell, G.; Kleer, C.G.; Reinhardt, F.; D’Alessio, A.C.; Young, R.A.; Weinberg, R.A. Poised chromatin at the ZEB1 promoter enables breast cancer cell plasticity and enhances tumorigenicity. Cell 2013, 154, 61–74. [Google Scholar] [CrossRef]
- Drapela, S.; Bouchal, J.; Jolly, M.K.; Culig, Z.; Soucek, K. ZEB1: A Critical Regulator of Cell Plasticity, DNA Damage Response, and Therapy Resistance. Front. Mol. Biosci. 2020, 7, 36. [Google Scholar] [CrossRef]
- Lehmann, W.; Mossmann, D.; Kleemann, J.; Mock, K.; Meisinger, C.; Brummer, T.; Herr, R.; Brabletz, S.; Stemmler, M.P.; Brabletz, T. ZEB1 turns into a transcriptional activator by interacting with YAP1 in aggressive cancer types. Nat. Commun. 2016, 7, 10498. [Google Scholar] [CrossRef]
- Brabletz, S.; Bajdak-Rusinek, K.; Meidhof, S.; Burk, U.; Niedermann, G.; Firat, E.; Wellner, U.; Dimmler, A.; Faller, G.; Schubert, J.; et al. The ZEB1/miR-200 feedback loop controls Notch signalling in cancer cells. EMBO J. 2011, 30, 770–782. [Google Scholar] [CrossRef]
- Gu, K.; Li, M.M.; Shen, J.; Liu, F.; Cao, J.Y.; Jin, S.; Yu, Y. Interleukin-17-induced EMT promotes lung cancer cell migration and invasion via NF-kappaB/ZEB1 signal pathway. Am. J. Cancer Res. 2015, 5, 1169–1179. [Google Scholar]
- Vandewalle, C.; Van Roy, F.; Berx, G. The role of the ZEB family of transcription factors in development and disease. Cell Mol. Life Sci. 2009, 66, 773–787. [Google Scholar] [CrossRef] [PubMed]
- Postigo, A.A.; Dean, D.C. ZEB represses transcription through interaction with the corepressor CtBP. Proc. Natl. Acad. Sci. USA 1999, 96, 6683–6688. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Sawada, J.-I.; Sui, G.; Affar, E.B.; Whetstine, J.R.; Lan, F.; Ogawa, H.; Luke, M.P.-S.; Nakatani, Y.; Shi, Y. Coordinated histone modifications mediated by a CtBP co-repressor complex. Nature 2003, 422, 735–738. [Google Scholar] [CrossRef]
- Wang, W.; Chi, T.; Xue, Y.; Zhou, S.; Kuo, A.; Crabtree, G.R. Architectural DNA binding by a high-mobility-group/kinesin-like subunit in mammalian SWI/SNF-related complexes. Proc. Natl. Acad. Sci. USA 1998, 95, 492–498. [Google Scholar] [CrossRef]
- Feldker, N.; Ferrazzi, F.; Schuhwerk, H.; Widholz, S.A.; Guenther, K.; Frisch, I.; Jakob, K.; Kleemann, J.; Riegel, D.; Bönisch, U.; et al. Genome-wide cooperation of EMT transcription factor ZEB1 with YAP and AP-1 in breast cancer. EMBO J. 2020, 39, e103209. [Google Scholar] [CrossRef] [PubMed]
- Hugo, H.J.; Pereira, L.; Suryadinata, R.; Drabsch, Y.; Gonda, T.J.; Gunasinghe, N.P.A.D.; Pinto, C.; Soo, E.T.L.; Van Denderen, B.J.W.; Hill, P.; et al. Direct repression of MYB by ZEB1 suppresses proliferation and epithelial gene expression during epithelial-to-mesenchymal transition of breast cancer cells. Breast Cancer Res. 2013, 15, R113. [Google Scholar] [CrossRef]
- Postigo, A.A. Opposing functions of ZEB proteins in the regulation of the TGFbeta/BMP signaling pathway. EMBO J. 2003, 22, 2443–2452. [Google Scholar] [CrossRef]
- Burks, H.E.; Matossian, M.D.; Rhodes, L.V.; Phamduy, T.; Elliott, S.; Buechlein, A.; Rusch, D.B.; Miller, D.F.B.; Nephew, K.P.; Chrisey, D.; et al. ZEB2 regulates endocrine therapy sensitivity and metastasis in luminal a breast cancer cells through a non-canonical mechanism. Breast Cancer Res. Treat. 2021, 189, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Sun, Y.; Ma, L. ZEB1: At the crossroads of epithelial-mesenchymal transition, metastasis and therapy resistance. Cell Cycle 2015, 14, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Waryah, C.; Cursons, J.; Foroutan, M.; Pflueger, C.; Wang, E.; Molania, R.; Woodward, E.; Sorolla, A.; Wallis, C.; Moses, C.; et al. Synthetic Epigenetic Reprogramming of Mesenchymal to Epithelial States Using the CRISPR/dCas9 Platform in Triple Negative Breast Cancer. Adv. Sci. 2023, 2301802. [Google Scholar] [CrossRef]
- Perez-Oquendo, M.; Gibbons, D.L. Regulation of ZEB1 Function and Molecular Associations in Tumor Progression and Metastasis. Cancers 2022, 14, 1864. [Google Scholar] [CrossRef] [PubMed]
- Katsura, A.; Tamura, Y.; Hokari, S.; Harada, M.; Morikawa, M.; Sakurai, T.; Takahashi, K.; Mizutani, A.; Nishida, J.; Yokoyama, Y.; et al. ZEB1-regulated inflammatory phenotype in breast cancer cells. Mol. Oncol. 2017, 11, 1241–1262. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Kang, Y. Epithelial-Mesenchymal Plasticity in Cancer Progression and Metastasis. Dev. Cell 2019, 49, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Wels, C.; Joshi, S.; Koefinger, P.; Bergler, H.; Schaider, H. Transcriptional activation of ZEB1 by Slug leads to cooperative regulation of the epithelial-mesenchymal transition-like phenotype in melanoma. J. Investig. Dermatol. 2011, 131, 1877–1885. [Google Scholar] [CrossRef]
- Wu, W.S.; You, R.-I.; Cheng, C.-C.; Lee, M.-C.; Lin, T.-Y.; Hu, C.-T. Snail collaborates with EGR-1 and SP-1 to directly activate transcription of MMP 9 and ZEB1. Sci. Rep. 2017, 7, 17753. [Google Scholar] [CrossRef] [PubMed]
- Dave, N.; Guaita-Esteruelas, S.; Gutarra, S.; Frias, Á.; Beltran, M.; Peiró, S.; de Herreros, A.G. Functional cooperation between Snail1 and twist in the regulation of ZEB1 expression during epithelial to mesenchymal transition. J. Biol. Chem. 2011, 286, 12024–12032. [Google Scholar] [CrossRef]
- Stemmler, M.P.; Eccles, R.L.; Brabletz, S.; Brabletz, T. Non-redundant functions of EMT transcription factors. Nat. Cell Biol. 2019, 21, 102–112. [Google Scholar] [CrossRef]
- Kroger, C.; Afeyan, A.; Mraz, J.; Eaton, E.N.; Reinhardt, F.; Khodor, Y.L.; Thiru, P.; Bierie, B.; Ye, X.; Burge, C.B.; et al. Acquisition of a hybrid E/M state is essential for tumorigenicity of basal breast cancer cells. Proc. Natl. Acad. Sci. USA 2019, 116, 7353–7362. [Google Scholar] [CrossRef]
- Vazquez-Martin, A.; Anatskaya, O.V.; Giuliani, A.; Erenpreisa, J.; Huang, S.; Salmina, K.; Inashkina, I.; Huna, A.; Nikolsky, N.N.; Vinogradov, A.E. Somatic polyploidy is associated with the upregulation of c-MYC interacting genes and EMT-like signature. Oncotarget 2016, 7, 75235–75260. [Google Scholar] [CrossRef]
- Huang, Y.; Hong, W.; Wei, X. The molecular mechanisms and therapeutic strategies of EMT in tumor progression and metastasis. J. Hematol. Oncol. 2022, 15, 129. [Google Scholar] [CrossRef]
- Haslehurst, A.M.; Koti, M.; Dharsee, M.; Nuin, P.; Evans, K.; Geraci, J.; Childs, T.; Chen, J.; Li, J.; Weberpals, J.; et al. EMT transcription factors snail and slug directly contribute to cisplatin resistance in ovarian cancer. BMC Cancer 2012, 12, 91. [Google Scholar] [CrossRef]
- Kurrey, N.K.; Jalgaonkar, S.P.; Joglekar, A.V.; Ghanate, A.D.; Chaskar, P.D.; Doiphode, R.Y.; Bapat, S.A. Snail and slug mediate radioresistance and chemoresistance by antagonizing p53-mediated apoptosis and acquiring a stem-like phenotype in ovarian cancer cells. Stem Cells 2009, 27, 2059–2068. [Google Scholar] [CrossRef]
- Lee, A.F.; Chen, M.-C.; Chen, C.-J.; Yang, C.-J.; Huang, M.-S.; Liu, Y.-P. Reverse epithelial-mesenchymal transition contributes to the regain of drug sensitivity in tyrosine kinase inhibitor-resistant non-small cell lung cancer cells. PLoS ONE 2017, 12, e0180383. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, Z.; Zhang, Q.; Zhang, Q.; Sun, P.; Xiang, R.; Ren, G.; Yang, S. ZEB1 confers chemotherapeutic resistance to breast cancer by activating ATM. Cell Death Dis. 2018, 9, 57. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liao, W.; Wu, Q.; Huang, X.; Pan, Z.; Chen, W.; Gu, S.; Huang, Z.; Wang, Y.; Tang, X.; et al. LINC00152 upregulates ZEB1 expression and enhances epithelial-mesenchymal transition and oxaliplatin resistance in esophageal cancer by interacting with EZH2. Cancer Cell Int. 2020, 20, 569. [Google Scholar] [CrossRef]
- Hanrahan, K.; O’Neill, A.; Prencipe, M.; Bugler, J.; Murphy, L.; Fabre, A.; Puhr, M.; Culig, Z.; Murphy, K.; Watson, R.W. The role of epithelial-mesenchymal transition drivers ZEB1 and ZEB2 in mediating docetaxel-resistant prostate cancer. Mol. Oncol. 2017, 11, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Chen, Y.; Lin, Y.; Wang, X.; Cui, X.; Zhang, Z.; Xian, G.; Qin, C. Novel crosstalk between KLF4 and ZEB1 regulates gemcitabine resistance in pancreatic ductal adenocarcinoma. Int. J. Oncol. 2017, 51, 1239–1248. [Google Scholar] [CrossRef]
- Redfern, A.D.; Spalding, L.J.; Thompson, E.W. The Kraken Wakes: Induced EMT as a driver of tumour aggression and poor outcome. Clin. Exp. Metastasis 2018, 35, 285–308. [Google Scholar] [CrossRef]
- Tran, H.D.; Luitel, K.; Kim, M.; Zhang, K.; Longmore, G.D.; Tran, D.D. Transient SNAIL1 expression is necessary for metastatic competence in breast cancer. Cancer Res. 2014, 74, 6330–6340. [Google Scholar] [CrossRef]
- Caramel, J.; Papadogeorgakis, E.; Hill, L.; Browne, G.J.; Richard, G.; Wierinckx, A.; Saldanha, G.; Osborne, J.; Hutchinson, P.; Tse, G.; et al. A switch in the expression of embryonic EMT-inducers drives the development of malignant melanoma. Cancer Cell 2013, 24, 466–480. [Google Scholar] [CrossRef]
- Asiedu, M.K.; Ingle, J.N.; Behrens, M.D.; Radisky, D.C.; Knutson, K.L. TGFbeta/TNF(alpha)-mediated epithelial-mesenchymal transition generates breast cancer stem cells with a claudin-low phenotype. Cancer Res. 2011, 71, 4707–4719. [Google Scholar] [CrossRef] [PubMed]
- Kudo-Saito, C.; Shirako, H.; Takeuchi, T.; Kawakami, Y. Cancer metastasis is accelerated through immunosuppression during Snail-induced EMT of cancer cells. Cancer Cell 2009, 15, 195–206. [Google Scholar] [CrossRef]
- Yang, J.; Wang, X.; Huang, B.; Liu, R.; Xiong, H.; Ye, F.; Zeng, C.; Fu, X.; Li, L. An IFNgamma/STAT1/JMJD3 Axis Induces ZEB1 Expression and Promotes Aggressiveness in Lung Adenocarcinoma. Mol. Cancer Res. 2021, 19, 1234–1246. [Google Scholar] [CrossRef]
- Lo, U.G.; Pong, R.-C.; Yang, D.; Gandee, L.; Hernandez, E.; Dang, A.; Lin, C.-J.; Santoyo, J.; Ma, S.; Sonavane, R.; et al. IFNgamma-Induced IFIT5 Promotes Epithelial-to-Mesenchymal Transition in Prostate Cancer via miRNA Processing. Cancer Res. 2019, 79, 1098–1112. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, L.; Pappan, L.; Galliher-Beckley, A.; Shi, J. IL-1beta promotes stemness and invasiveness of colon cancer cells through Zeb1 activation. Mol. Cancer 2012, 11, 87. [Google Scholar] [CrossRef]
- Lee, C.H.; Chang, J.S.; Syu, S.; Wong, T.; Chan, J.Y.; Tang, Y.; Yang, Z.; Yang, W.; Chen, C.; Lu, S.; et al. IL-1beta promotes malignant transformation and tumor aggressiveness in oral cancer. J. Cell Physiol. 2015, 230, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, N.J.; Sasser, A.K.; Axel, A.; Vesuna, F.; Raman, V.; Ramirez, N.; Oberyszyn, T.M.; Hall, B.M. Interleukin-6 induces an epithelial-mesenchymal transition phenotype in human breast cancer cells. Oncogene 2009, 28, 2940–2947. [Google Scholar] [CrossRef]
- Yadav, A.; Kumar, B.; Datta, J.; Teknos, T.N.; Kumar, P. IL-6 promotes head and neck tumor metastasis by inducing epithelial-mesenchymal transition via the JAK-STAT3-SNAIL signaling pathway. Mol. Cancer Res. 2011, 9, 1658–1667. [Google Scholar] [CrossRef]
- Hwang, W.L.; Yang, M.; Tsai, M.; Lan, H.; Su, S.; Chang, S.; Teng, H.; Yang, S.; Lan, Y.; Chiou, S.; et al. SNAIL regulates interleukin-8 expression, stem cell-like activity, and tumorigenicity of human colorectal carcinoma cells. Gastroenterology 2011, 141, 279–291.e5. [Google Scholar] [CrossRef]
- Visciano, C.; Liotti, F.; Prevete, N.; Cali’, G.; Franco, R.; Collina, F.; De Paulis, A.; Marone, G.; Santoro, M.; Melillo, R.M. Mast cells induce epithelial-to-mesenchymal transition and stem cell features in human thyroid cancer cells through an IL-8-Akt-Slug pathway. Oncogene 2015, 34, 5175–5186. [Google Scholar] [CrossRef]
- Zhang, Q.; Liu, S.; Parajuli, K.R.; Zhang, W.; Zhang, K.; Mo, Z.; Liu, J.; Chen, Z.; Yang, S.; Wang, A.R.; et al. Interleukin-17 promotes prostate cancer via MMP7-induced epithelial-to-mesenchymal transition. Oncogene 2017, 36, 687–699. [Google Scholar] [CrossRef]
- Chen, D.; Li, W.; Liu, S.; Su, Y.; Han, G.; Xu, C.; Liu, H.; Zheng, T.; Zhou, Y.; Mao, C. Interleukin-23 promotes the epithelial-mesenchymal transition of oesophageal carcinoma cells via the Wnt/beta-catenin pathway. Sci. Rep. 2015, 5, 8604. [Google Scholar] [CrossRef]
- Izumi, K.; Fang, L.Y.; Mizokami, A.; Namiki, M.; Li, L.; Lin, W.J.; Chang, C. Targeting the androgen receptor with siRNA promotes prostate cancer metastasis through enhanced macrophage recruitment via CCL2/CCR2-induced STAT3 activation. EMBO Mol. Med. 2013, 5, 1383–1401. [Google Scholar] [CrossRef]
- Rao, Q.; Chen, Y.; Yeh, C.-R.; Ding, J.; Li, L.; Chang, C.; Yeh, S. Recruited mast cells in the tumor microenvironment enhance bladder cancer metastasis via modulation of ERbeta/CCL2/CCR2 EMT/MMP9 signals. Oncotarget 2016, 7, 7842–7855. [Google Scholar] [CrossRef] [PubMed]
- Long, H.; Xiang, T.; Qi, W.; Huang, J.; Chen, J.; He, L.; Liang, Z.; Guo, B.; Li, Y.; Xie, R.; et al. CD133+ ovarian cancer stem-like cells promote non-stem cancer cell metastasis via CCL5 induced epithelial-mesenchymal transition. Oncotarget 2015, 6, 5846–5859. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhao, J.; Li, J.; Zhu, Z.; Cui, Z.; Liu, R.; Lu, R.; Yao, Z.; Xu, Q. Cancer associated fibroblast-derived CCL5 promotes hepatocellular carcinoma metastasis through activating HIF1alpha/ZEB1 axis. Cell Death Dis. 2022, 13, 478. [Google Scholar] [CrossRef]
- Zhang, B.; Yin, C.; Li, H.; Shi, L.; Liu, N.; Sun, Y.; Lu, S.; Liu, Y.; Sun, L.; Li, X.; et al. Nir1 promotes invasion of breast cancer cells by binding to chemokine (C-C motif) ligand 18 through the PI3K/Akt/GSK3beta/Snail signalling pathway. Eur. J. Cancer 2013, 49, 3900–3913. [Google Scholar] [CrossRef]
- Bonde, A.K.; Tischler, V.; Kumar, S.; Soltermann, A.; Schwendener, R.A. Intratumoral macrophages contribute to epithelial-mesenchymal transition in solid tumors. BMC Cancer 2012, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Toh, B.; Wang, X.; Keeble, J.; Sim, W.J.; Khoo, K.; Wong, W.-C.; Kato, M.; Prevost-Blondel, A.; Thiery, J.-P.; Abastado, J.-P. Mesenchymal transition and dissemination of cancer cells is driven by myeloid-derived suppressor cells infiltrating the primary tumor. PLoS Biol. 2011, 9, e1001162. [Google Scholar] [CrossRef]
- Camisaschi, C.; Casati, C.; Rini, F.; Perego, M.; De Filippo, A.; Triebel, F.; Parmiani, G.; Belli, F.; Rivoltini, L.; Castelli, C. LAG-3 expression defines a subset of CD4(+)CD25(high)Foxp3(+) regulatory T cells that are expanded at tumor sites. J. Immunol. 2010, 184, 6545–6551. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Liu, Q.; Chen, J.; Chen, J.; Chen, F.; He, C.; Huang, D.; Wu, W.; Lin, L.; Huang, W.; et al. A positive feedback loop between mesenchymal-like cancer cells and macrophages is essential to breast cancer metastasis. Cancer Cell 2014, 25, 605–620. [Google Scholar] [CrossRef]
- Bronte, V.; Chappell, D.B.; Apolloni, E.; Cabrelle, A.; Wang, M.; Hwu, P.; Restifo, N.P. Unopposed production of granulocyte-macrophage colony-stimulating factor by tumors inhibits CD8+ T cell responses by dysregulating antigen-presenting cell maturation. J. Immunol. 1999, 162, 5728–5737. [Google Scholar] [CrossRef] [PubMed]
- Nagaraj, S.; Gupta, K.; Pisarev, V.; Kinarsky, L.; Sherman, S.; Kang, L.; Herber, D.L.; Schneck, J.; Gabrilovich, D.I. Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer. Nat. Med. 2007, 13, 828–835. [Google Scholar] [CrossRef]
- Chen, L.; Gibbons, D.L.; Goswami, S.; Cortez, M.A.; Ahn, Y.-H.; Byers, L.A.; Zhang, X.; Yi, X.; Dwyer, D.; Lin, W.; et al. Metastasis is regulated via microRNA-200/ZEB1 axis control of tumour cell PD-L1 expression and intratumoral immunosuppression. Nat. Commun. 2014, 5, 5241. [Google Scholar] [CrossRef] [PubMed]
- Ock, C.Y.; Kim, S.; Keam, B.; Kim, M.; Kim, T.M.; Kim, J.-H.; Jeon, Y.K.; Lee, J.-S.; Kwon, S.K.; Hah, J.H.; et al. PD-L1 expression is associated with epithelial-mesenchymal transition in head and neck squamous cell carcinoma. Oncotarget 2016, 7, 15901–15914. [Google Scholar] [CrossRef]
- Alsuliman, A.; Colak, D.; Al-Harazi, O.; Fitwi, H.; Tulbah, A.; Al-Tweigeri, T.; Al-Alwan, M.; Ghebeh, H. Bidirectional crosstalk between PD-L1 expression and epithelial to mesenchymal transition: Significance in claudin-low breast cancer cells. Mol. Cancer 2015, 14, 149. [Google Scholar] [CrossRef] [PubMed]
- Dongre, A.; Rashidian, M.; Eaton, E.N.; Reinhardt, F.; Thiru, P.; Zagorulya, M.; Nepal, S.; Banaz, T.; Martner, A.; Spranger, S.; et al. Direct and Indirect Regulators of Epithelial-Mesenchymal Transition-Mediated Immunosuppression in Breast Carcinomas. Cancer Discov. 2021, 11, 1286–1305. [Google Scholar] [CrossRef]
- Zheng, Q.; Gao, J.; Yin, P.; Wang, W.; Wang, B.; Li, Y.; Zhao, C. CD155 contributes to the mesenchymal phenotype of triple-negative breast cancer. Cancer Sci. 2020, 111, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Mak, M.P.; Tong, P.; Diao, L.; Cardnell, R.J.; Gibbons, D.L.; William, W.N.; Skoulidis, F.; Parra, E.R.; Rodriguez-Canales, J.; Wistuba, I.I.; et al. A Patient-Derived, Pan-Cancer EMT Signature Identifies Global Molecular Alterations and Immune Target Enrichment Following Epithelial-to-Mesenchymal Transition. Clin. Cancer Res. 2016, 22, 609–620. [Google Scholar] [CrossRef]
- Lou, Y.; Diao, L.; Cuentas, E.R.P.; Denning, W.L.; Chen, L.; Fan, Y.H.; Byers, L.A.; Wang, J.; Papadimitrakopoulou, V.A.; Behrens, C.; et al. Epithelial-Mesenchymal Transition Is Associated with a Distinct Tumor Microenvironment Including Elevation of Inflammatory Signals and Multiple Immune Checkpoints in Lung Adenocarcinoma. Clin. Cancer Res. 2016, 22, 3630–3642. [Google Scholar] [CrossRef]
- Lee, J.H.; Shklovskaya, E.; Lim, S.Y.; Carlino, M.S.; Menzies, A.M.; Stewart, A.; Pedersen, B.; Irvine, M.; Alavi, S.; Yang, J.Y.H.; et al. Transcriptional downregulation of MHC class I and melanoma de- differentiation in resistance to PD-1 inhibition. Nat. Commun. 2020, 11, 1897. [Google Scholar] [CrossRef]
- Chen, X.H.; Liu, Z.-C.; Zhang, G.; Wei, W.; Wang, X.-X.; Wang, H.; Ke, H.-P.; Zhang, F.; Wang, H.-S.; Cai, S.-H.; et al. TGF-beta and EGF induced HLA-I downregulation is associated with epithelial-mesenchymal transition (EMT) through upregulation of snail in prostate cancer cells. Mol. Immunol. 2015, 65, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Alves, E.; Taifour, S.; Dolcetti, R.; Chee, J.; Nowak, A.K.; Gaudieri, S.; Blancafort, P. Reprogramming the anti-tumor immune response via CRISPR genetic and epigenetic editing. Mol. Ther. Methods Clin. Dev. 2021, 21, 592–606. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, S.C.; Peters, H.L.; Taguchi, A.; Katayama, H.; Wang, H.; Momin, A.; Jolly, M.K.; Celiktas, M.; Rodriguez-Canales, J.; Liu, H.; et al. Immunoproteasome deficiency is a feature of non-small cell lung cancer with a mesenchymal phenotype and is associated with a poor outcome. Proc. Natl. Acad. Sci. USA 2016, 113, E1555–E1564. [Google Scholar] [CrossRef]
- He, Y.; Bunn, P.A.; Zhou, C.; Chan, D. KIR 2D (L1, L3, L4, S4) and KIR 3DL1 protein expression in non-small cell lung cancer. Oncotarget 2016, 7, 82104–82111. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Tian, X.; Li, Y.; Liu, Y.; Yang, T.; Han, Z.; An, J.; Kong, L.; Li, Y. Epithelial-mesenchymal transition may be involved in the immune evasion of circulating gastric tumor cells via downregulation of ULBP1. Cancer Med. 2020, 9, 2686–2697. [Google Scholar] [CrossRef]
- Lopez-Soto, A.; Huergo-Zapico, L.; Galvan, J.A.; Rodrigo, L.; de Herreros, A.G.; Astudillo, A.; Gonzalez, S. Epithelial-mesenchymal transition induces an antitumor immune response mediated by NKG2D receptor. J. Immunol. 2013, 190, 4408–4419. [Google Scholar] [CrossRef]
- Alves, E.; McLeish, E.; Blancafort, P.; Coudert, J.D.; Gaudieri, S. Manipulating the NKG2D Receptor-Ligand Axis Using CRISPR: Novel Technologies for Improved Host Immunity. Front. Immunol. 2021, 12, 712722. [Google Scholar] [CrossRef]
- Anastasiadou, E.; Jacob, L.S.; Slack, F.J. Non-coding RNA networks in cancer. Nat. Rev. Cancer 2018, 18, 5–18. [Google Scholar] [CrossRef]
- Lin, C.C.; Liu, L.-Z.; Addison, J.B.; Wonderlin, W.F.; Ivanov, A.V.; Ruppert, J.M. A KLF4-miRNA-206 autoregulatory feedback loop can promote or inhibit protein translation depending upon cell context. Mol. Cell Biol. 2011, 31, 2513–2527. [Google Scholar] [CrossRef]
- Ma, F.; Liu, X.; Li, D.; Wang, P.; Li, N.; Lu, L.; Cao, X. MicroRNA-466l upregulates IL-10 expression in TLR-triggered macrophages by antagonizing RNA-binding protein tristetraprolin-mediated IL-10 mRNA degradation. J. Immunol. 2010, 184, 6053–6059. [Google Scholar] [CrossRef]
- Vasudevan, S.; Tong, Y.; Steitz, J.A. Switching from repression to activation: microRNAs can up-regulate translation. Science 2007, 318, 1931–1934. [Google Scholar] [CrossRef]
- Kozomara, A.; Birgaoanu, M.; Griffiths-Jones, S. miRBase: From microRNA sequences to function. Nucleic Acids Res. 2019, 47, D155–D162. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ma, L. MicroRNA control of epithelial-mesenchymal transition and metastasis. Cancer Metastasis Rev. 2012, 31, 653–662. [Google Scholar] [CrossRef]
- Burk, U.; Schubert, J.; Wellner, U.; Schmalhofer, O.; Vincan, E.; Spaderna, S.; Brabletz, T. A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep. 2008, 9, 582–589. [Google Scholar] [CrossRef]
- Siemens, H.; Jackstadt, R.; Hünten, S.; Kaller, M.; Menssen, A.; Götz, U.; Hermeking, H. miR-34 and SNAIL form a double-negative feedback loop to regulate epithelial-mesenchymal transitions. Cell Cycle 2011, 10, 4256–4271. [Google Scholar] [CrossRef]
- Zaravinos, A. The Regulatory Role of MicroRNAs in EMT and Cancer. J. Oncol. 2015, 2015, 865816. [Google Scholar] [CrossRef]
- Davis-Dusenbery, B.N.; Hata, A. MicroRNA in Cancer: The Involvement of Aberrant MicroRNA Biogenesis Regulatory Pathways. Genes Cancer 2010, 1, 1100–1114. [Google Scholar] [CrossRef] [PubMed]
- Jia, L.; Xi, Q.; Wang, H.; Zhang, Z.; Liu, H.; Cheng, Y.; Guo, X.; Zhang, J.; Zhang, Q.; Zhang, L.; et al. miR-142-5p regulates tumor cell PD-L1 expression and enhances anti-tumor immunity. Biochem. Biophys. Res. Commun. 2017, 488, 425–431. [Google Scholar] [CrossRef]
- Zhao, L.; Yu, H.; Yi, S.; Peng, X.; Su, P.; Xiao, Z.; Liu, R.; Tang, A.; Li, X.; Liu, F.; et al. The tumor suppressor miR-138-5p targets PD-L1 in colorectal cancer. Oncotarget 2016, 7, 45370–45384. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Tan, W.; Liu, S.; Huang, X.; Lin, J.; Liang, R.; Su, L.; Su, Q.; Wang, C. MiR-570 inhibited the cell proliferation and invasion through directly targeting B7-H1 in hepatocellular carcinoma. Tumour Biol. 2015, 36, 9049–9057. [Google Scholar] [CrossRef] [PubMed]
- Omar, H.A.; El-Serafi, A.T.; Hersi, F.; Arafa, E.A.; Zaher, D.M.; Madkour, M.; Arab, H.H.; Tolba, M.F. Immunomodulatory MicroRNAs in cancer: Targeting immune checkpoints and the tumor microenvironment. FEBS J. 2019, 286, 3540–3557. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, J.; Dong, K.; Lin, F.; Long, M.; Ouyang, Y.; Wei, J.; Chen, X.; Weng, Y.; He, T.; et al. Tumor suppressor miR-34a targets PD-L1 and functions as a potential immunotherapeutic target in acute myeloid leukemia. Cell Signal. 2015, 27, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Pavlic, A.; Hauptman, N.; Bostjancic, E.; Zidar, N. Long Non-Coding RNAs as Potential Regulators of EMT-Related Transcription Factors in Colorectal Cancer-A Systematic Review and Bioinformatics Analysis. Cancers 2022, 14, 2280. [Google Scholar] [CrossRef] [PubMed]
- Xiong, H.G.; Li, H.; Xiao, Y.; Yang, Q.-C.; Yang, L.-L.; Chen, L.; Bu, L.-L.; Zhang, W.F.; Zhang, J.L.; Sun, Z.-J. Long noncoding RNA MYOSLID promotes invasion and metastasis by modulating the partial epithelial-mesenchymal transition program in head and neck squamous cell carcinoma. J. Exp. Clin. Cancer Res. 2019, 38, 278. [Google Scholar] [CrossRef]
- Xu, Q.; Deng, F.; Qin, Y.; Zhao, Z.; Wu, Z.; Xing, Z.; Ji, A.; Wang, Q.J. Long non-coding RNA regulation of epithelial-mesenchymal transition in cancer metastasis. Cell Death Dis. 2016, 7, e2254. [Google Scholar] [CrossRef]
- Xue, M.; Pang, H.; Li, X.; Li, H.; Pan, J.; Chen, W. Long non-coding RNA urothelial cancer-associated 1 promotes bladder cancer cell migration and invasion by way of the hsa-miR-145-ZEB1/2-FSCN1 pathway. Cancer Sci. 2016, 107, 18–27. [Google Scholar] [CrossRef]
- Li, H.; Zhu, L.; Xu, L.; Qin, K.; Liu, C.; Yu, Y.; Su, D.; Wu, K.; Sheng, Y. Long noncoding RNA linc00617 exhibits oncogenic activity in breast cancer. Mol. Carcinog. 2017, 56, 3–17. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, J.; Shen, B.; Yin, K.; Xu, J.; Gao, W.; Zhang, L. Long noncoding RNA lncTCF7, induced by IL-6/STAT3 transactivation, promotes hepatocellular carcinoma aggressiveness through epithelial-mesenchymal transition. J. Exp. Clin. Cancer Res. 2015, 34, 116. [Google Scholar] [CrossRef]
- Su, W.; Xu, M.; Chen, X.; Ni Chen, N.; Gong, J.; Nie, L.; Li, L.; Li, X.; Zhang, M.; Zhou, Q. Long noncoding RNA ZEB1-AS1 epigenetically regulates the expressions of ZEB1 and downstream molecules in prostate cancer. Mol. Cancer 2017, 16, 142. [Google Scholar] [CrossRef]
- Beltran, M.; Puig, I.; Peña, C.; García, J.M.; Álvarez, A.B.; Peña, R.; Bonilla, F.; de Herreros, A.G. A natural antisense transcript regulates Zeb2/Sip1 gene expression during Snail1-induced epithelial-mesenchymal transition. Genes Dev. 2008, 22, 756–769. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.H.; Li, B.; Liu, D.-G.; Zhang, B.; Yang, X.; Tu, Y.-L. LncRNA KCNQ1OT1 sponges miR-15a to promote immune evasion and malignant progression of prostate cancer via up-regulating PD-L1. Cancer Cell Int. 2020, 20, 394. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.H.; Yang, F.; Wang, F.; Ma, J.-Z.; Guo, Y.-J.; Tao, Q.-F.; Liu, F.; Pan, W.; Wang, T.-T.; Zhou, C.-C.; et al. A long noncoding RNA activated by TGF-beta promotes the invasion-metastasis cascade in hepatocellular carcinoma. Cancer Cell 2014, 25, 666–681. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Lee, D.W.; Yim, G.W.; Nam, E.J.; Kim, S.; Kim, S.W.; Kim, Y.T. Long non-coding RNA HOTAIR is associated with human cervical cancer progression. Int. J. Oncol. 2015, 46, 521–530. [Google Scholar] [CrossRef]
- Liu, Y.W.; Sun, M.; Xia, R.; Zhang, E.-B.; Liu, X.-H.; Zhang, Z.-H.; Xu, T.-P.; De, W.; Liu, B.-R.; Wang, Z.-X. LincHOTAIR epigenetically silences miR34a by binding to PRC2 to promote the epithelial-to-mesenchymal transition in human gastric cancer. Cell Death Dis. 2015, 6, e1802. [Google Scholar] [CrossRef]
- Liu, M.; Zhang, H.; Li, Y.; Wang, R.; Li, Y.; Zhang, H.; Ren, D.; Liu, H.; Kang, C.; Chen, J. HOTAIR, a long noncoding RNA, is a marker of abnormal cell cycle regulation in lung cancer. Cancer Sci. 2018, 109, 2717–2733. [Google Scholar] [CrossRef]
- Zhang, H.; Cai, K.; Wang, J.; Wang, X.; Cheng, K.; Shi, F.; Jiang, L.; Zhang, Y.; Dou, J. MiR-7, inhibited indirectly by lincRNA HOTAIR, directly inhibits SETDB1 and reverses the EMT of breast cancer stem cells by downregulating the STAT3 pathway. Stem Cells 2014, 32, 2858–2868. [Google Scholar] [CrossRef]
- Jin, L.; Pan, Y.L.; Zhang, J.; Cao, P.G. LncRNA HOTAIR recruits SNAIL to inhibit the transcription of HNF4alpha and promote the viability, migration, invasion and EMT of colorectal cancer. Transl Oncol. 2021, 14, 101036. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).