Calcium Homeostasis in the Development of Resistant Breast Tumors
Abstract
Simple Summary
Abstract
1. Introduction
1.1. Epidemiology and Risk Factors for Breast Cancer
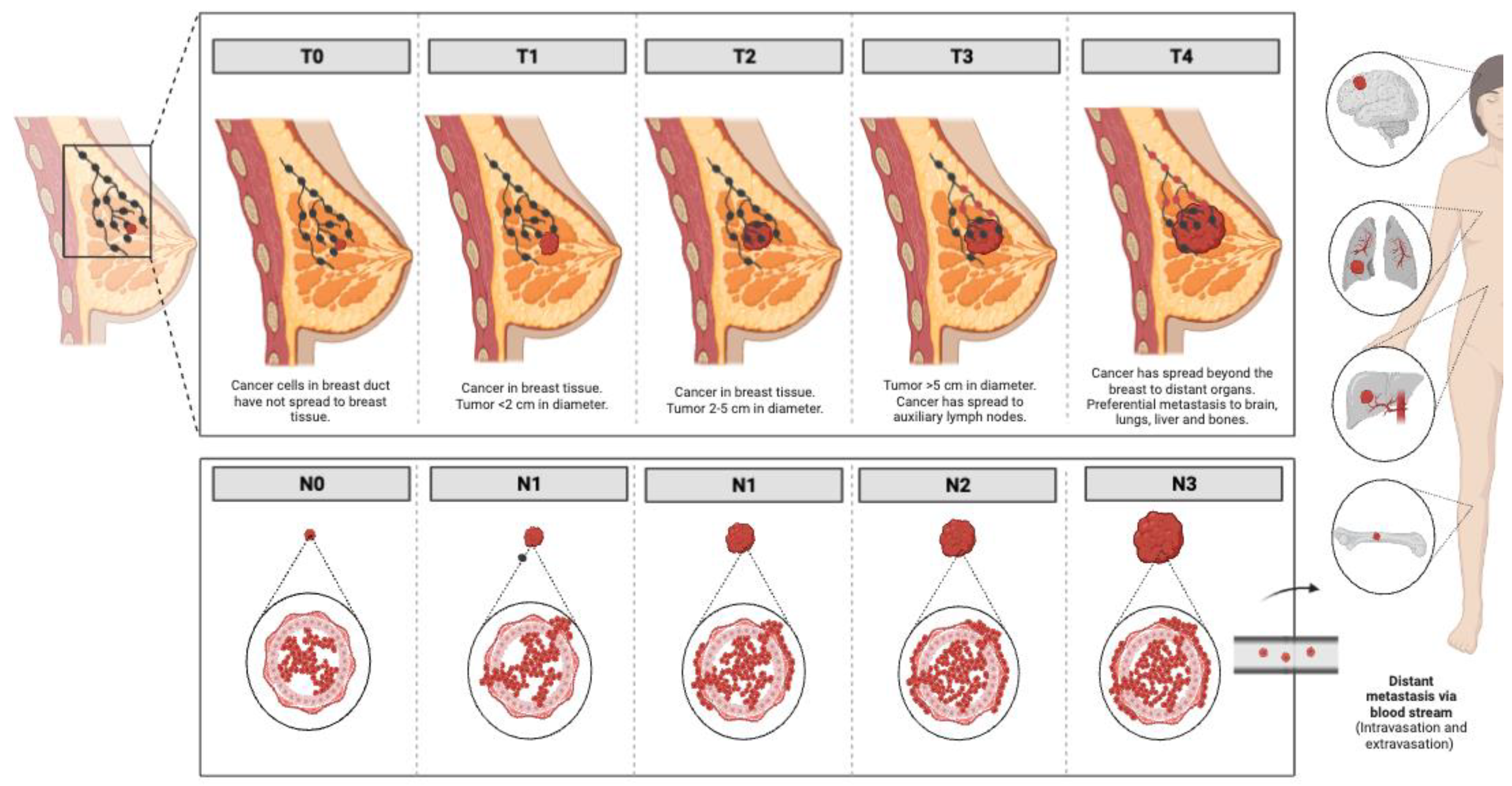
1.2. Heterogeneity of Breast Cancer: Progression of the Disease and Histological and Molecular Classifications
- Hormone-receptor-positive breast tumors, which account for 75% of breast carcinomas, are classified into luminal A breast tumors (50–60% of diagnosed cases)—which are ER-positive and/or PR-positive, HER2-negative and Ki67 < 14% [19] with low histological grade, and have a low mitosis proportion number and good prognosis—and luminal B tumors (15–20% of diagnosed cases)—which are defined as ER-positive and/or PR-positive (PR < 20% + Ki67 ≥ 14%), HER2-negative or ER-positive and/or PR positive/negative (any PR-positive and any Ki67) and HER2-positive. Luminal B tumors usually have a more aggressive phenotype, both by histologic grade and proliferative Ki67 index, and worse prognosis than luminal A tumors [20].
- HER2-enriched tumors, which account for approximately 15–20% of breast tumors, present HER2 overexpression [21]. These tumors do not express estrogen or progesterone receptors and are characterized by the overactivation of signaling pathways involved in increased cell proliferation (Ras/MAPK mitogen-activated protein kinases and PI3K/AKT phosphoinositide 4-kinase/protein kinase B), with increased risk of metastasis and a more aggressive phenotype than luminal tumors [22].
- Basal-like tumors are characterized by a lack of HER2 overexpression and the absence or low levels of ER/PR expression. Among basal-like tumors, the triple-negative subtype, which constitutes approximately 80% of basal-like tumors and 10–15% of breast carcinomas, is defined by the lack of hormone receptors (ER-, PR-), the lack of HER overexpression (HER2-) and being cytokeratin-5/6-positive (CK5/6+) and/or Epidermal-Growth-Factor-Receptor-positive (EGFR+) [23].
1.3. Conventional Treatments for Breast Cancer
1.4. Targeted Therapies for Breast Cancer
2. Role of the Ca2+-Signaling Pathway in Breast Cancer
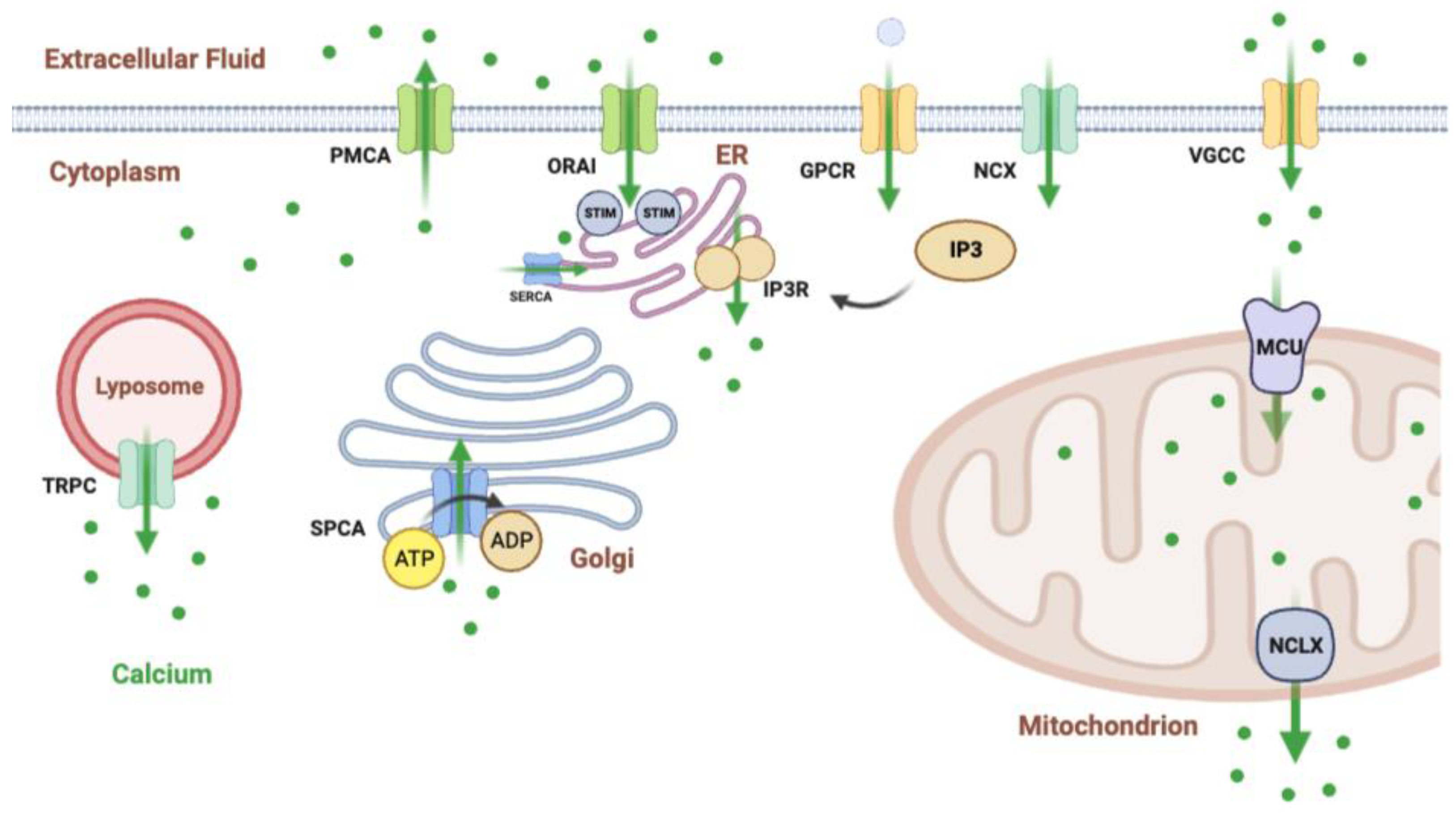
2.1. Proteins Involved in Calcium Homeostasis and Relevance in Breast Cancer
2.1.1. Calcium Ion Channels
2.1.2. Ligand-Dependent Calcium Ion Channels
- Store-operated Ca2+ entry, which is a process that serves to replenish Ca2+ after its release from reserve sites, such as the endoplasmic reticulum.
- Cytosolic calcium increases are necessary for cell activation. The entire process of calcium-dependent cell activation is based on ER calcium release combined with capacitative calcium influx and consequent increases in cytosolic calcium levels.
2.1.3. Voltage-Dependent Calcium Channels
2.1.4. G-Protein-Coupled Receptors
2.1.5. Calcium Buffer Proteins
2.2. Ca2+ as a Therapeutic Target in Breast Cancer
3. Preclinical and Clinical Research on Ca2+ in Breast Cancer
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Shulman, L.N.; Willett, W.; Sievers, A.; Knaul, F.M. Breast cancer in developing countries: Opportunities for improved survival. J. Oncol. 2010, 2010, 595167. [Google Scholar] [CrossRef]
- Shemanko, C.S.; Cong, Y.; Forsyth, A. What is the breast in the bone? Int. J. Mol. Sci. 2016, 17, 1764. [Google Scholar] [CrossRef]
- Bloom, A.P.; Jiménez-Andrade, J.M.; Taylor, R.N.; Castañeda-Corral, G.; Kaczmarska, M.J.; Freeman, K.T.; Coughlin, K.A.; Guilardi, J.R.; Kuskowsik, M.A.; Mantyh, P.W. Breast cancer-induced bone remodeling, skeletal pain and tenderness flare nerve fibers. J. Pain. 2011, 12, 698–711. [Google Scholar] [CrossRef]
- Takeshima, H.; Ushijima, T. Accumulation of genetic and epigenetic alterations in normal cells and cancer risk. NPJ Precis. Oncol. 2019, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rodero, S.; Delgado-Álvarez, E.; Fernández, A.F.; Fernández-Morera, J.L.; Menéndez-Torre, E.; Fraga, M.F. Epigenetic alterations in endocrine-related cancer. Endocr. Relat. Cancer. 2014, 21, 319–330. [Google Scholar] [CrossRef]
- Chen, W.Y.; Rosner, B.; Hankinson, S.E.; Colditz, G.A.; Willett, W.C. Moderate adult alcohol consumption, drinking patterns, and breast cancer risk. JAMA 2011, 306, 1884–1890. [Google Scholar] [CrossRef] [PubMed]
- Cancer CGoHFiB. Type and timing of menopausal hormone therapy and breast cancer risk: Individual participant meta-analysis of worldwide epidemiologic evidence. Lancet 2019, 394, 1159–1168. [Google Scholar] [CrossRef]
- Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk: Individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012, 13, 1141–1151. [Google Scholar] [CrossRef]
- Fortner, R.T.; Sisti, J.; Chai, B.; Collins, L.C.; Rosner, B.; Hankinson, S.E.; Tamimi, R.M.; Eliassen, A.H. Parity, breastfeeding, and breast cancer risk by hormone receptor status and molecular phenotype: Results from the Nurses’ Health Studies. Breast Cancer Res. 2019, 21, 40. [Google Scholar] [CrossRef] [PubMed]
- Padilla-Ruiz, M.; Zarcos-Pedrinaci, I.; Rivas-Ruiz, F.; Téllez, T.; García-Gutiérrez, S.; González, N.; Rivero, A.; Sarasqueta, C.; Serrano-Aguilar, P.; Castells, X.; et al. Factors that Influence Treatment Delay for Patients with Breast Cancer. Ann. Surg. Oncol. 2021, 28, 3714–3721. [Google Scholar] [CrossRef] [PubMed]
- Rakha, E.A.; Green, A.R. Molecular classification of breast cancer: What the pathologist needs to know. Pathology 2017, 49, 111–119. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Breast Tumours, 5th ed.; WHO Classification of Tumours; World Health Organization: Geneva, Switzerland, 2019; Volume 2, ISBN-13: 978-92-832-4500-1. [Google Scholar]
- Dillon, D.; Guidi, A.J.; Schnitt, S.J. Pathology of Invasive Breast Cancer. In Diseases of the Breast, 5th ed.; Harris, J.R., Lippman, M.E., Morrow, M., Osborne, C.K., Eds.; Wolters Kluwer Health: Philadelphia, PA, USA, 2014. [Google Scholar]
- Byrd, D.R.; Carducci, M.A.; Compton, C.C.; Fritz, A.; Greene, F. AJCC Cancer Staging Manual; Edge, S.B., Ed.; Springer: New York, NY, USA, 2010; Volume 7, pp. 97–100. [Google Scholar]
- Alkabban, F.M.; Ferguson, T. Cancer, Breast; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Park, Y.H.; Lee, S.J.; Cho, E.Y.; Choi, Y.; Lee, J.E.; Nam, S.J.; Yang, J.H.; Shin, J.H.; Ko, E.Y.; Han, B.K.; et al. Clinical relevance of TNM staging system according to breast cancer subtypes. Ann. Oncol. 2011, 22, 1554–1560, Erratum in Ann. Oncol. 2019, 30, 2011. [Google Scholar] [CrossRef]
- Koh, J.; Kim, M.J. Introduction of a New Staging System of Breast Cancer for Radiologists: An Emphasis on the Prognostic Stage. Korean J. Radiol. 2019, 20, 69–82, Erratum in Korean J. Radiol. 2022, 23, 570. [Google Scholar] [CrossRef]
- Lim, E.; Metzger-Filho, O.; Winer, E.P. The natural history of hormone receptor-positive breast cancer. Oncology 2012, 26, 668–694. [Google Scholar]
- Dai, X.; Li, T.; Bai, Z.; Yang, Y.; Liu, X.; Zhan, J.; Shi, B. Breast cancer intrinsic classification, clinical use and future trends. Am. J. Cancer Res. 2015, 5, 2929–2943. [Google Scholar] [PubMed]
- Sareyeldin, R.M.; Gupta, I.; Al-Hashimi, I.; Al-Thawadi, H.; Al Farsi, H.F.; Vraninc, S.; Al Moustafa, A.E. Gene expression and miRNA profiling: Function and regulation in human epidermal growth factor receptor 2 (HER2) positive Breast cancer. Cancers 2019, 11, 646. [Google Scholar] [CrossRef]
- Harbeckm, N.; Penault-Llorca, F.; Cortes, J.; Gnant, M.; Houssami, N.; Poortmans, P.; Ruddy, K.; Tsang, J.; Cardoso, F. Breast Cancer. Nat. Dis. Rev. Prim. 2019, 5, 66. [Google Scholar] [CrossRef]
- Cheang, M.C.; Voduc, D.; Bajdik, C.; Leung, S.; McKinney, S.; Chia, S.K.; Perou, C.M. Basal-like breast cancer defined by five biomarkers has superior prognostic value to triple-negative phenotype. Clin. Cancer Res. 2008, 14, 1368–1376. [Google Scholar] [CrossRef]
- Joshi, H.; Press, M.F. Molecular Oncology of Breast Cancer. In The Breast; Bland, K.I., Copeland, E.M., Klimberg, V.S., Gradishar, W.J., Eds.; Elsevier: Philadelphia, PA, USA, 2018; Volume 22. [Google Scholar] [CrossRef]
- Chavez-MacGregor, M.; Mittendorf, E.A.; Clarke, C.A.; Lichtensztajn, D.Y.; Hunt, K.K.; Giordano, S.H. Incorporating Tumor Characteristics to the American Joint Committee on Cancer Breast Cancer Staging System. Oncologist 2017, 22, 1292–1300. [Google Scholar] [CrossRef]
- Zhang, W.; Couldwell, W.T.; Song, H.; Takano, T.; Lin, J.H.; Nedergaard, M. Tamoxifen-induced calcium signaling in glioma and MCF-7 breast cancer cells. Cancer Res. 2000, 60, 5395–5400. [Google Scholar]
- Baselga, J.; Norton, L.; Albanell, J.; Kim, Y.M.; Mendelsohn, J. Recombinant humanized anti-HER2 antibody (Herceptin) enhances the antitumor activity of paclitaxel and doxorubicin against HER2/neu overexpressing human breast cancer xenografts. Cancer Res. 1998, 58, 2825–2831. [Google Scholar]
- Garrido-Castro, A.C.; Lin, N.U.; Polyak, K. Insights into Molecular Classifications of Triple-Negative Breast Cancer: Improving Patient Selection for Treatment. Cancer Discov. 2019, 9, 176–198. [Google Scholar] [CrossRef] [PubMed]
- Schneider, B.P.; Winer, E.P.; Foulkes, W.D.; Garber, J.; Perou, C.M.; Richardson, A.; Sledge, G.W.; Carey, L.A. Triple-negative breast cancer: Risk factors to potential targets. Clin. Cancer Res. 2008, 14, 8010–8018. [Google Scholar] [CrossRef]
- Redig, A.J.; McAllister, S.S. Breast cancer as a systemic disease: A view of metastasis. J. Intern. Med. 2013, 274, 113–126. [Google Scholar] [CrossRef]
- Sheikh, A.; Hussain, S.A.; Ghori, Q.; Naeem, N.; Fazil, A.; Giri, S.; Sathian, B.; Mainali, P.; Al Tamimi, D.M. The spectrum of genetic mutations in breast cancer. Asian Pac. J. Cancer Prev. 2015, 16, 2177–2185. [Google Scholar] [CrossRef]
- Paul, A.; Paul, S. The breast cancer susceptibility genes (BRCA) in breast and ovarian cancers. Front. Biosci. 2014, 19, 605–618. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wu, A.; Bean, G.R.; Hagemann, I.S.; Lin, C.Y. Molecular Testing in Breast Cancer: Current Status and Future Directions. J. Mol. Diagn. 2021, 23, 1422–1432. [Google Scholar] [CrossRef] [PubMed]
- Nicolini, A.; Ferrari, P.; Duffy, M.J. Prognostic and predictive biomarkers in breast cancer: Past, present and future. Semin. Cancer Biol. 2018, 52, 56–73. [Google Scholar] [CrossRef]
- Wöckel, A.; Albert, U.S.; Janni, W.; Scharl, A.; Kreienberg, R.; Stüber, T. The Screening, Diagnosis, Treatment, and Follow-Up of Breast Cancer. Dtsch. Arztebl. Int. 2018, 115, 316–323. [Google Scholar] [CrossRef]
- Lyman, G.H.; Somerfield, M.R.; Bosserman, L.D.; Perkins, C.L.; Weaver, D.L.; Giuliano, A.E. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J. Clin. Oncol. 2017, 35, 561–564. [Google Scholar] [CrossRef]
- Detailed Guide: Radiation Therapy of Breast Cancer. American Cancer Society. 2009. Available online: http://www.cancer.org/docroot/CRI/content/CRI_2_4_4X_Radiation_Therapy_5.asp?sitearea (accessed on 17 November 2022).
- Wells, B.G. Breast Cancer, Pharmacotherapy Manual, 5th ed.; Tata McGraw Hill Publisher Company Limited: New Delhi, India, 2004. [Google Scholar]
- Goldhirsch, A.; Wood, W.C.; Coates, A.S.; Gelber, R.D.; Trürlimann, B.; Senn, H.J.; Panel members. Strategies for subtypes—Dealing with the diversity of breast cancer: Highlights of the St. Gallen International Expert. Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann. Oncol. 2011, 22, 1736–1747. [Google Scholar] [CrossRef] [PubMed]
- Zirlik, K.; Duyster, J. Anti-Angiogenics: Current Situation and Future Perspectives. Oncol. Res. Treat. 2018, 41, 166–171. [Google Scholar] [CrossRef]
- McDonald, E.S.; Clark, A.S.; Tchou, J.; Zhang, P.; Freedman, G.M. Clinical Diagnosis and Management of Breast Cancer. J. Nucl. Med. 2016, 57 (Suppl. 1), 9–16. [Google Scholar] [CrossRef]
- Early Breast Cancer Trialists’ Collaborative Group. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: Patient-level meta-analysis of randomised trials. Lancet 2011, 378, 771–784. [Google Scholar] [CrossRef] [PubMed]
- Drăgănescu, M.; Carmocan, C. Hormone Therapy in Breast Cancer. Chirurgia 2017, 112, 413–417. [Google Scholar] [CrossRef]
- Dowsett, M.; Cuzick, J.; Ingle, J.; Coates, A.; Forbes, J.; Bliss, J.; Buyse, M.; Baum, M.; Buzdar, A.; Colleoni, M.; et al. Meta-analysis of breast cancer outcomes in adjuvant trials of aromatase inhibitors versus tamoxifen. J. Clin. Oncol. 2010, 28, 509–518. [Google Scholar] [CrossRef]
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Aromatase inhibitors versus tamoxifen in early breast cancer: Patient-level meta-analysis of the randomised trials. Lancet 2015, 386, 1341–1352. [Google Scholar] [CrossRef]
- Singh, H.; Walker, A.J.; Amiri-Kordestani, L.; Cheng, J.; Tang, S.; Balcazar, P.; Barnett-Ringgold, K.; Palmby, T.R.; Cao, X.; Zheng, N.; et al. U.S. food and drug administration approval: Neratinib for the extended adjuvant treatment of early-stage HER2-positive breast cancer. Clin. Cancer Res. 2018, 24, 3486–3491. [Google Scholar] [CrossRef]
- Ben Dhia, S.; Loap, P.; Loirat, D.; Vincent-Salomon, A.; Cao, K.; Escalup, L.; Fourquet, A.; Kirova, Y. Concurrent radiation therapy and dual HER2 blockade in breast cancer: Assessment of toxicity. Cancer Radiother. 2021, 25, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Royce, M.; Osgood, C.L.; Amatya, A.K.; Kiero, M.H.; Chang, C.J.G.; Ricks, T.K.; Shetty, K.A.; Kraft, J.; Qiu, J.; Song, P.; et al. FDA approval summary: Margetuximab plus chemotherapy for advanced or metastatic HER2-positive breast cancer. Clin. Cancer Res. 2022, 28, 1487–1492. [Google Scholar] [CrossRef]
- Markham, A. Margetuximab: First approval. Drugs 2021, 81, 599–604. [Google Scholar] [CrossRef]
- MacroGenics. MARGENZA (Margetuximab-cmkb): Highlights of Prescribing Information; MacroGenics: Rockville, MD, USA, 2020. [Google Scholar]
- Wahdan-Alaswad, R.; Liu, B.; Thor, A.D. Targeted lapatinib anti-HER2/ErbB2 therapy resistance in breast cancer: Opportunities to overcome a difficult problem. Cancer Drug. Resist. 2020, 3, 179–198. [Google Scholar] [CrossRef]
- Moy, B.; Kirkpatrick, P.; Kar, S.; Goss, P. Lapatinib. Nat. Rev. Drug. Discov. 2007, 6, 431–432. [Google Scholar] [CrossRef]
- Paranjpe, R.; Basatneh, D.; Tao, G.; De Angelis, C.; Noormohammed, S.; Ekinci, E.; Abugshosh, S.; Ghose, R.; Trivedi, M.V. Neratinib in HER2-positive breast cancer patients. Ann. Pharmacother. 2019, 53, 612–620. [Google Scholar] [CrossRef]
- Lee, A. Tucatinib: First approval. Drug. 2020, 80, 1033–1038. [Google Scholar] [CrossRef]
- Blair, H.A. Pyrotinib: First global approval. Drugs. 2018, 78, 1751–1755. [Google Scholar] [CrossRef]
- Yu, J.; Fang, T.; Yun, C.; Liu, X.; Cai, X. Antibody-drug conjugates targeting the human epidermal growth factor receptor family in cancers. Front. Mol. Biosci. 2022, 9, 847835. [Google Scholar] [CrossRef]
- Corrigan, P.A.; Cicci, T.A.; Auten, J.J.; Lowe, D.K. Ado-trastuzumab Emtansine: A HER2-positive targeted antibody-drug conjugate. Ann. Pharmacother. 2014, 48, 1484–1493. [Google Scholar] [CrossRef]
- Barok, M.; Joensuu, H.; Isola, J. Trastuzumab emtansine: Mechanisms of action and drug resistance. Breast Cancer Res. 2014, 16, 209. [Google Scholar] [CrossRef]
- So, C.L.; Saunus, J.M.; Roberts-Thomson, S.J.; Monteith, G.R. Calcium signalling and breast cancer. Semin. Cell. Dev. Biol. 2019, 94, 74–83. [Google Scholar] [CrossRef]
- Modi, S.; Saura, C.; Yamashita, T.; Park, Y.H.; Kim, S.B.; Tamura, K.; Andre, F.; Iwata, H.; Ito, Y.; Tsurutani, J.; et al. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N. Engl. J. Med. 2020, 382, 610–621. [Google Scholar] [CrossRef] [PubMed]
- Tajada, S.; Villalobos, C. Calcium-permeable channels in cancer characteristics. Front. Pharmacol. 2020, 11, 968. [Google Scholar] [CrossRef] [PubMed]
- Aalders, K.C.; Tryfonidis, K.; Senkus, E.; Cardoso, F. Anti-angiogenic treatment in breast cancer: Facts, successes, failures and future perspectives. Cancer Treat. Rev. 2017, 53, 98–110. [Google Scholar] [CrossRef]
- Miyashita, M.; Hattori, M.; Takano, T.; Toyama, T.; Iwata, H. Risks and benefits of bevacizumab combined with chemotherapy for advanced or metastatic breast cancer: A meta-analysis of randomized controlled trials. Breast Cancer. 2020, 27, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Ueda, S.; Saeki, T.; Osaki, A.; Yamane, T.; Kuji, I. Bevacizumab induces acute hypoxia and cancer progression in patients with refractory breast cancer: Multimodal functional imaging and multiplex cytokine analysis. Clin. Cancer Res. 2017, 23, 5769–5778. [Google Scholar] [CrossRef]
- Kazazi-Hysen, F.; Beijnen, J.H.; Schellens, J.H. Bevacizumab. Oncologist 2010, 15, 819. [Google Scholar] [CrossRef]
- Krüger, K.; Silwal-Pandit, L.; Wik, E.; Straume, O.; Stefansson, I.M.; Borgen, E.; Garred, O.; Naume, B.; Engebraaten, O.; Akslen, L.A. Baseline microvessel density predicts response to neoadjuvant bevacizumab treatment of locally advanced breast cancer. Sci. Rep. 2021, 11, 3388. [Google Scholar] [CrossRef]
- Spring, L.M.; Wander, S.A.; Zangardi, M.; Bardia, A. CDK 4/6 inhibitors in breast cancer: Current controversies and future directions. Curr. Oncol. Rep. 2019, 21, 25. [Google Scholar] [CrossRef]
- Ciruelos, E.; Villagrasa, P.; Pascual, T.; Oliveira, M.; Pernas, S.; Paré, L.; Escrivá-de-Romaní, S.; Manso, L.; Adamo, B.; Martínez, E.; et al. Palbociclib and trastuzumab in HER2-positive advanced breast cancer: Results from the phase II SOLTI-1303 PATRICIA trial. Clin. Cancer Res. 2020, 26, 5820–5829. [Google Scholar] [CrossRef]
- Bahrami, A.; Khazaei, M.; Shahidsales, S.; Hassanian, S.M.; Hasanzadeh, M.; Maftouh, M.; Ferns, G.A.; Avan, A. The therapeutic potential of PI3K/Akt/mTOR inhibitors in. J. Cell. Biochem. 2018, 119, 213–222. [Google Scholar] [CrossRef]
- Cidado, J.; Park, B.H. Targeting the PI3K/Akt/mTOR pathway for breast cancer therapy. J. Mammary Gland. Biol. Neoplasia. 2012, 17, 205–216. [Google Scholar] [CrossRef]
- Verret, B.; Cortes, J.; Bachelot, T.; Andre, F.; Arnedos, M. Efficacy of PI3K inhibitors in advanced breast cancer. Ann. Oncol. 2019, 30 (Suppl. S10), x12–x20. [Google Scholar] [CrossRef]
- Roskoski, R. Properties of FDA-approved small molecule phosphatidylinositol 3-kinase inhibitors prescribed for the treatment of malignancies. Pharmacol. Res. 2021, 168, 105579. [Google Scholar] [CrossRef]
- Paplomata, E.; Zelnak, A.; O’Regan, R. Everolimus: Side effect profile and management of toxicities in breast cancer. Breast Cancer Res. Treat. 2013, 140, 453–462. [Google Scholar] [CrossRef]
- Lin, J.; Sampath, D.; Nannini, M.A.; Lee, B.B.; Degtyarev, M.; Oeg, J.; Savage, H.; Guan, Z.; Hong, R.; Kassees, R.; et al. Targeting activated Akt with GDC-0068, a novel selective Akt inhibitor that is efficacious in multiple tumor models. Clin. Cáncer Res. 2013, 19, 1760–1772. [Google Scholar] [CrossRef]
- Isakoff, S.J.; Tabernero, J.; Molife, L.R.; Soria, J.C.; Cervantes, A.; Volgelzang, N.J.; Patel, M.R.; Hussain, M.; Baron, A.; Argilés, G.; et al. Antitumor activity of ipatasertib combined with chemotherapy: Results from a phase Ib study in solid tumors. Ann. Oncol. 2020, 31, 626–633. [Google Scholar] [CrossRef]
- Kim, S.B.; Dent, R.; Im, S.A.; Espié, M.; Blau, S.; Tan, A.R.; Isakoff, S.J.; Oliveira, M.; Saura, C.; LOTUS Investigators; et al. Ipatasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer (LOTUS): A multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2017, 18, 1360–1372. [Google Scholar] [CrossRef]
- Dent, R.; Oliveira, M.; Isakoff, S.J.; LOTUS Investigators. Final results of the double-blind placebo-controlled randomized phase 2 LOTUS trial of first-line ipatasertib plus paclitaxel for inoperable locally advanced/metastatic triple-negative breast cancer. Breast Cancer Res. Treat. 2021, 189, 377–386. [Google Scholar] [CrossRef]
- Turner, N.; Dent, R.A.; O’Shaughnessy, J.; Kim, S.B.; Isakoff, S.J.; Barrios, C.; Saji, S.; Bondarenko, I.; Noweckin, Z.; Lian, Q.; et al. Ipatasertib plus paclitaxel for PIK3CA/AKT1/PTEN-altered hormone receptor-positive HER2-negative advanced breast cancer: Primary results from cohort B of the IPATunity130 randomized phase 3 trial. Breast Cancer Res. Treat. 2022, 191, 565–576. [Google Scholar] [CrossRef]
- Cortesi, L.; Rugo, H.S.; Jackisch, C. An overview of PARP inhibitors for the treatment of breast cancer. Target. Oncol. 2021, 16, 255–282. [Google Scholar] [CrossRef] [PubMed]
- Livraghi, L.; Garber, J.E. PARP inhibitors in the management of breast cancer: Current data and future prospects. BMC Med. 2015, 13, 188. [Google Scholar] [CrossRef] [PubMed]
- Schwartzberg, L.S.; Kiedrowski, L.A. Olaparib in hormone receptor-positive, HER2-negative metastatic breast cancer with a somatic BRCA2 mutation. Ther. Adv. Med. Oncol. 2021, 13, 17588359211006962. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. FDA Approves Olaparib Germline BRCA Mutated Metastatic Breast Cancer; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2018.
- Hoy, S.M. Talazoparib: First global approval. Drugs 2018, 78, 1939–1946. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. FDA Approves Talazoparib gBRCAm her2 Negative Locally Advanced or Metastatic Breast Cancer; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2018.
- Ratto, G.M.; Payne, R.; Owen, W.G.; Tsien, R.Y. The concentration of cytosolic free calcium in vertebrate rod outer segments measured with fura-2. J. Neurosci. 1988, 8, 3240–3246. [Google Scholar] [CrossRef]
- O’Grady, S.; Morgan, M.P. Calcium transport and signalling in breast cancer: Functional and prognostic significance. Semin. Cancer Biol. 2021, 72, 19–26. [Google Scholar] [CrossRef]
- Cox, R.F.; Morgan, M.P. Microcalcifications in breast cancer: Lessons from physiological mineralization. Bone 2013, 53, 437–450. [Google Scholar] [CrossRef]
- Carruthers, C.; Suntzeff, V. The Role of Calcium in Carcinogenesis Summary. Science 1944, 99, 245–247. [Google Scholar] [CrossRef]
- Pedriali, G.; Rimessi, A.; Sbano, L.; Giorgi, C.; Wieckowski, M.R.; Previati, M.; Pinton, P. Regulation of Endoplasmic Reticulum-Mitochondria Ca2+ Transfer and Its Importance for Anti-Cancer Therapies. Front. Oncol. 2017, 7, 180. [Google Scholar] [CrossRef]
- Petersen, O.H.; Michalak, M.; Verkhratsky, A. Calcium signalling: Past, present and future. Cell Calcium 2005, 38, 161–169. [Google Scholar] [CrossRef]
- Capiod, T.; Shuba, Y.; Skryma, R.; Prevarskaya, N. Calcium signalling and cancer cell growth. Subcell. Biochem. 2007, 45, 405–427. [Google Scholar] [CrossRef] [PubMed]
- Neville, M.C. Calcium secretion into milk. J. Mammary Gland. Biol. Neoplasia. 2005, 10, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Neville, M.C.; Keller, R.P.; Casey, C.; Allen, J.C. Calcium partitioning in human and bovine milk. J. Dairy Sci. 1994, 77, 1964–1975. [Google Scholar] [CrossRef] [PubMed]
- Pratt, S.; Hernández-Ochoa, E.; Martin, S.S. Calcium signaling breast cancer’s approach to manipulation of cellular circuitry. Biophys. Rev. 2020, 12, 1343–1359. [Google Scholar] [CrossRef]
- Berridge, M.J. The AM and FM of calcium signalling. Nature 1997, 386, 759–760. [Google Scholar] [CrossRef]
- Parekh, A.B. Decoding cytosolic Ca2+ oscillations. Trends Biochem. Sci. 2011, 36, 78–87. [Google Scholar] [CrossRef]
- Samanta, K.; Parekh, A.B. Spatial Ca2+ profiling: Decrypting the universal cytosolic Ca2+ oscillation. J. Physiol. 2017, 595, 3053–3062. [Google Scholar] [CrossRef]
- Cyrus, K.; Wang, Q.; Sharawi, Z.; Noguchi, G.; Kaushal, M.; Chang, T.; Rydzewiski, W.; Yeguech, W.; Gibrel, F.; Psaltis, J.B.; et al. Role of calcium in hormone-independent and -resistant breast cancer. Int. J. Cancer. 2021, 149, 1817–1827. [Google Scholar] [CrossRef]
- Lee, W.J.; Monteith, G.R.; Roberts-Thomson, S.J. Calcium transport and signaling in the mammary gland: Targets for breast cancer. Biochim. Biophys. Acta. 2006, 1765, 235–255. [Google Scholar] [CrossRef]
- Kanwar, N.; Carmine-Simmen, K.; Nair, R.; Wang, C.; Moghadas-Jafari, S.; Blaser, H.; Tran-Tranh, D.; Wang, D.; Wang, P.; Wang, J.; et al. Amplification of a calcium channel subunit CACNG4 increases breast cancer metastasis. eBioMedicine 2020, 52, 102646. [Google Scholar] [CrossRef]
- Jacquemet, G.; Baghirov, H.; Georgiadou, M.; Sihto, H.; Peuhu, E.; Cettour-Janet, P.; He, T.; Perälä, M.; Kronqvist, P.; Joensuu, H.; et al. L-type calcium channels regulate filopodia stability and cancer cell invasion downstream of integrin signaling. Nat. Commun. 2016, 7, 13297. [Google Scholar] [CrossRef]
- Bon, R.; Beech, D.J. In pursuit of small molecule chemistry for calcium-permeable non-selective TRPC channels—Mirage or pot of gold? Br. J. Pharmacol. 2013, 170, 459–474. [Google Scholar] [CrossRef] [PubMed]
- Schwab, A.; Hanley, P.; Fabian, A.; Stock, C. Potassium channels keep mobile cells on the go. Physiology 2008, 23, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Asghar, M.Y.; Törnquist, K. Transient receptor potential canonical (TRPC) channels as modulators of migration and invasion. Int. J. Mol. Sci. 2020, 21, 1739. [Google Scholar] [CrossRef] [PubMed]
- Storch, U.; Forst, A.L.; Philipp, M.; Gudermann, T.; y Schnitzler, M.M. Transient receptor potential channel 1 (TRPC1) reduces calcium permeability in heteromeric channel complexes. J. Biol. Chem. 2012, 287, 3530–3540. [Google Scholar] [CrossRef]
- Bhargava, A.; Saha, S. T-type voltage-dependent calcium channels: A target in breast cancer? Breast Cancer Res. Treat. 2019, 173, 11–21. [Google Scholar] [CrossRef]
- Perez-Reyes, E. Molecular physiology of low-voltage-activated t-type calcium channels. Physiol. Rev. 2003, 83, 117–161. [Google Scholar] [CrossRef] [PubMed]
- Bertolesi, G.E.; Shi, C.; Elbaum, L.; Jollimore, C.; Rozenberg, G.; Barnes, S.; Kelly, M.E. The Ca2+ channel antagonists mibefradil and pimozide inhibit cell growth via different cytotoxic mechanisms. Mol. Pharmacol. 2002, 62, 210–219. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, H.; Qian, Z.; Feng, B.; Zhao, X.; Jiang, X.; Tao, J. Low-voltage-activated T-type Ca2+ channel inhibitors as new tools in the treatment of glioblastoma: The role of endostatin. Pflug. Arch. 2014, 466, 811–818. [Google Scholar] [CrossRef]
- Wee, P.; Wang, Z. Epidermal Growth Factor Receptor Cell Proliferation Signaling Pathways. Cancers 2017, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Haugh, J.M.; Schooler, K.; Wells, A.; Wiley, H.S.; Lauffenburger, D.A. Effect of epidermal growth factor receptor internalization on regulation of the phospholipase C-gamma1 signaling pathway. J. Biol. Chem. 1999, 274, 8958–8965. [Google Scholar] [CrossRef] [PubMed]
- Roskoski, R., Jr. The role of small molecule platelet-derived growth factor receptor (PDGFR) inhibitors in the treatment of neoplastic disorders. Pharmacol. Res. 2018, 129, 65–83. [Google Scholar] [CrossRef] [PubMed]
- Carafoli, E.; Santella, L.; Branca, D.; Brini, M. Generation, control, and processing of cellular calcium signals. Crit. Rev. Biochem. Mol. Biol. 2001, 36, 107–260. [Google Scholar] [CrossRef]
- Terrié, E.; Coronas, V.; Constantin, B. Role of the calcium toolkit in cancer stem cells. Cell Calcium 2019, 80, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Immler, R.; Simon, S.I.; Sperandio, M. Calcium signalling and related ion channels in neutrophil recruitment and function. Eur. J. Clin. Investig. 2018, 48 (Suppl. 2), 12964. [Google Scholar] [CrossRef] [PubMed]
- Weaver, C.M.; Peacock, M. Calcium. Adv. Nutr. 2019, 10, 546–548. [Google Scholar] [CrossRef]
- Marchi, S.; Pinton, P. The mitochondrial calcium uniporter complex: Molecular components, structure and physiopathological implications. J. Physiol. 2014, 592, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Patron, M.; Raffaello, A.; Granatiero, V.; Tosatto, A.; Merli, G.; De Stefani, D.; Wright, L.; Pallafacchina, G.; Terrin, A.; Mammucari, C.; et al. The mitochondrial calcium uniporter (MCU): Molecular identity and physiological roles. J. Biol. Chem. 2013, 288, 10750–10758. [Google Scholar] [CrossRef]
- Stewart, T.; Yapa, K.T.; Monteith, G.R. Altered calcium signaling in cancer cells. Biochim. Biophys. Acta 2015, 1848, 2502–2511. [Google Scholar] [CrossRef]
- Roderick, H.L.; Cook, S.J. Ca2+ signaling checkpoints in cancer: Ca2+ remodeling for cancer cell proliferation and survival. Nat. Rev. Cancer 2008, 8, 361. [Google Scholar] [CrossRef]
- Marchi, S.; Pinton, P. Alterations of calcium homeostasis in cancer cells. Curr. Opin. Pharmacol. 2016, 29, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rivera, E.; Gomez, H. Chemotherapy resistance in metastatic breast cancer: The evolving role of ixabepilone. Breast Cancer Res. 2010, 12, S2. [Google Scholar] [CrossRef] [PubMed]
- Castronovo, V.; Bellahcene, A. Evidence that breast cancer-associated microcalcifications are mineralized malignant cells. Int. J. Oncol. 1998, 12, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Kratz, A.; Ferraro, M.; Sluss, P.M.; Lewandrowski, K.B. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Laboratory reference values. N. Engl. J. Med. 2004, 351, 1548–1563. [Google Scholar] [CrossRef] [PubMed]
- McDonough, P.M.; Button, D.C. Measurement of cytoplasmic calcium concentration in cell suspensions: Correction for extracellular Fura-2 through use of Mn2+ and probenecid. Cell Calcium 1989, 10, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Cruz Morales, R.A.; Villaseñor Navarro, Y.; Pavón Hernández, C.M.; Pérez Badillo, M.P.; Aguilar Cortázar, L.O.; Pérez Zúñiga, I. Microcalcificaciones de la mama: Un reto para el diagnóstico. Gac. Mex. De Oncol. 2012, 11, 251–259. [Google Scholar]
- Lang, F.; Stournaras, C. Ion channels in cancer: Future perspectives and clinical potential. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2014, 369, 20130108. [Google Scholar] [CrossRef]
- Henrot, P.; Leroux, A.; Barlier, C.; Génin, P. Breast microcalcifications: The lesions in anatomical pathology. Diagn. Interv. Imaging 2014, 95, 141–152. [Google Scholar] [CrossRef]
- Clemenceau, A.; Michou, L.; Diorio, C.; Durocher, F. Breast Cancer and Microcalcifications: An Osteoimmunological Disorder? Int. J. Mol. Sci. 2020, 21, 8613. [Google Scholar] [CrossRef]
- Peters, A.A.; Milevskiy, M.J.; Lee, W.C.; Curry, M.C.; Smart, C.E.; Saunus, J.M.; Reid, L.; da Silva, L.; Marcial, D.L.; Dray, E.; et al. The calcium pump plasma membrane Ca2+-ATPase 2 (PMCA2) regulates breast cancer cell proliferation and sensitivity to doxorubicin. Sci. Rep. 2016, 6, 25505. [Google Scholar] [CrossRef]
- Faddy, H.M.; Smart, C.E.; Xu, R.; Lee, G.Y.; Kenny, P.A.; Feng, M.; Rao, R.; Brown, M.A.; Bissel, M.J.; Roberts-Thomson, S.J.; et al. Localization of plasma membrane and secretory calcium pumps in the mammary gland. Biochem. Biophys. Res. Commun. 2008, 369, 977–981. [Google Scholar] [CrossRef]
- Makena, M.R.; Ko, M.; Mekile, A.X.; Senoo, N.; Dang, D.K.; Warrington, J.; Buckhaults, P.; Talbot, C.C.; Chaypool, S.M.; Rao, R. Secretory pathway Ca2+-ATPase SPCA2 regulates mitochondrial respiration and DNA damage response through store-independent calcium entry. Redox Biol. 2022, 50, 102240. [Google Scholar] [CrossRef] [PubMed]
- Feng, M.; Grice, D.M.; Faddy, H.M.; Nguyen, N.; Leitch, S.; Wang, Y.; Muend, S.; Kenny, P.A.; Sukumar, S.; Roberts-Thomson, S.J.; et al. Store-independent activation of Orai1 by SPCA2 in mammary tumors. Cell 2010, 143, 84–98. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, S.B.; Monteith, G.R. ORAI channels and cancer. Cell Calcium 2018, 74, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Azimi, I.; Milevskiy, M.J.; Chalmers, S.B.; Yapa, K.T.D.S.; Robitaille, M.; Henry, C.; Baillie, G.J.; Thompson, E.W.; Roberts-Thomson, S.J.; Monteith, G.R. ORAI1 and ORAI3 in Breast Cancer Molecular Subtypes and the Identification of ORAI3 as a Hypoxia Sensitive Gene and a Regulator of Hypoxia Responses. Cancers 2019, 11, 208. [Google Scholar] [CrossRef]
- Faouzi, M.; Hague, F.; Potier, M.; Ahidouch, A.; Sevestre, H.; Ouadid-Ahidouch, H. Down-regulation of Orai3 arrests cell-cycle progression and induces apoptosis in breast cancer cells but not in normal breast epithelial cells. J. Cell Phys. 2011, 226, 542–551. [Google Scholar] [CrossRef]
- McAndrew, D.; Grice, D.M.; Peters, A.A.; Davis, F.M.; Stewart, T.; Rice, M.; Smart, C.E.; Brown, M.A.; Kenny, P.A.; Roberts-Thomson, S.J.; et al. ORAI1-mediated calcium influx in lactation and in breast cancer. Mol. Cancer Ther. 2011, 10, 448–460. [Google Scholar] [CrossRef]
- Yang, S.; Zhang, J.J.; Huang, X.Y. Orai1 and STIM1 are critical for breast tumor cell migration and metastasis. Cancer Cell. 2009, 15, 124–134. [Google Scholar] [CrossRef]
- Yang, Y.; Jiang, Z.; Wang, B.; Chang, L.; Liu, J.; Zhang, L.; Gu, L. Expression of STIM1 is associated with tumor aggressiveness and poor prognosis in breast cancer. Pathol. Res. Pract. 2017, 213, 1043–1047. [Google Scholar] [CrossRef]
- Motiani, R.K.; Abdullaev, I.F.; Trebak, M. A Novel Native Store-operated Calcium Channel Encoded by Orai3. J. Biol. Chem. 2010, 285, 19173–19183. [Google Scholar] [CrossRef]
- Jardin, I.; Diez-Bello, R.; Lopez, J.J.; Redondo, P.C.; Salido, G.M.; Smani, T.; Rosado, J.A. TRPC6 Channels are Required for Proliferation, Migration and Invasion of Breast Cancer Cell Lines by Modulation of Orai1 and Orai3 Surface Exposure. Cancers 2018, 10, 331. [Google Scholar] [CrossRef] [PubMed]
- Chodon, D.; Guilbert, A.; Dhennin-Duthille, I.; Gautier, M.; Telliez, M.S.; Sevestre, H.; Ouadid-Ahidouch, H. Estrogen regulation of TRPM8 expression in breast cancer cells. BMC Cancer 2010, 10, 212. [Google Scholar] [CrossRef] [PubMed]
- Dhennin-Duthille, I.; Gautier, M.; Faouzi, M.; Guilbert, A.; Brevet, M.; Vaudry, D.; Ahidrouch, A.; Sevestre, H.; Ouadid-Ahidouch, H. High expression of transient receptor potential channels in human breast cancer epithelial cells and tissues: Correlation with pathological parameters. Cell. Phys. Biochem. 2011, 28, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Motiani, R.K.; Zhang, X.; Harmon, K.E.; Keller, R.S.; Matrougui, K.; Bennett, J.A.; Trebak, M. Orai3 is an estrogen receptor α-regulated Ca2+ channel that promotes tumorigenesis. FASEB J. 2013, 27, 63–75. [Google Scholar] [CrossRef]
- Ouadid-Ahidouch, H.; Dhennin-Duthille, I.; Gautier, M.; Sevestre, H.; Ahidouch, A. Canaux cationiques TRP dans le cancer du sein: Expression, rôle et corrélation avec des paramètres cliniques [TRP calcium channel and breast cancer: Expression, role and correlation with clinical parameters]. Bull. Cancer 2012, 99, 655–664. [Google Scholar] [CrossRef]
- Azimi, I.; Milevskiy, M.J.; Kaemmerer, E.; Turner, D.; Yapa, K.T.D.S.; Brown, M.A.; Thompson, E.W.; Roberts-Thomson, S.J.; Monteith, G.R. TRPC1 is a differential regulator of hypoxia-mediated events and Akt signalling in PTEN-deficient breast cancer cells. J. Cell Sci. 2017, 130, 2292–2305. [Google Scholar] [CrossRef]
- Pera, E.; Kaemmerer, E.; Milevskiy, M.J.G.; Yapa, K.T.D.S.; O’Donnell, J.S.; Brown, M.A.; Simpson, F.; Peters, A.A.; Roberts-Thomson, S.J.; Monteith, G.R. The Ca2+-dependent voltage-gated Ca v 3.2 channel and therapeutic responses in breast cancer. Cancer Cell Int. 2016, 16, 24. [Google Scholar] [CrossRef]
- Phan, N.N.; Wang, C.Y.; Chen, C.F.; Sun, Z.; Lai, M.D.; Lin, Y.C. Voltage-gated calcium channels: Novel targets for cancer therapy. Oncol. Lett. 2017, 14, 2059–2074. [Google Scholar] [CrossRef]
- Dang, D.; Prasad, H.; Rao, R. Secretory pathway Ca2+-ATPases promote in vitro microcalcifications in breast cancer cells. BMC Cancer 2017, 56, 2474–2485. [Google Scholar] [CrossRef]
- Varga, K.; Hollósi, A.; Pászty, K.; Hegedús, L.; Szakács, G.; Tímár, J.; Papp, B.; Enyedi, Á.; Padányi, R. Expression of calcium pumps is differentially regulated by histone deacetylase inhibitors and estrogen receptor alpha in breast cancer cells. BMC Cancer 2018, 18, 1029. [Google Scholar] [CrossRef]
- Mahdi, S.H.; Cheng, H.; Li, J.; Feng, R. The effect of TGF-beta-induced epithelial-mesenchymal transition on the expression of intracellular calcium-handling proteins in T47D and MCF-7 human breast cancer cells. Arch. Biochem. Biophys. 2015, 583, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Reinhardt, T.A.; Lippolis, J.D.; Shull, G.E.; Horst, R.L. Null mutation in the gene encoding plasma membrane Ca2+-ATPase isoform 2 impairs calcium transport into milk. J. Biol. Chem. 2004, 279, 42369–42373. [Google Scholar] [CrossRef]
- Curry, M.C.; Luk, N.A.; Kenny, P.A.; Roberts-Thomson, S.J.; Monteith, G.R. Distinct regulation of cytoplasmic calcium signals and cell death pathways by different plasma membrane calcium ATPase isoforms in MDA-MB-231 breast cancer cells. J. Biol. Chem. 2012, 287, 28598–28608. [Google Scholar] [CrossRef]
- Hegedüs, L.; Padányi, R.; Molnár, J.; Pászty, K.; Varga, K.; Kenessey, I.; Sárközy, E.; Wolf, M.; Grusch, M.; Hegyi, Z.; et al. Histone Deacetylase Inhibitor Treatment Increases the Expression of the Plasma Membrane Ca2+ Pump PMCA4b and Inhibits the Migration of Melanoma Cells Independent of ERK. Front. Oncol. 2017, 7, 95. [Google Scholar] [CrossRef] [PubMed]
- Varga, K.; Pászty, K.; Padányi, R.; Hegedús, L.; Brouland, J.P.; Papp, B.; Enyedi, A. Histone deacetylase inhibitor- and PMA-induced upregulation of PMCA4b enhances Ca2+ clearance from MCF-7 breast cancer cells. Cell Calcium 2014, 55, 78–92. [Google Scholar] [CrossRef]
- Wu, L.; Weidong, L.; Liang, Z. Calcium signaling in cancer progression and therapy. FEBS J. 2021, 288, 6187–6205. [Google Scholar] [CrossRef]
- Bong, A.H.L.; Hua, T.; So, C.L.; Peters, A.A.; Robitaille, M.; Tan, Y.Y.; Roberts-Thomson, S.J.; Monteith, G.R. AKT Regulation of ORAI1-Mediated Calcium Influx in Breast Cancer Cells. Cancers 2022, 14, 4794. [Google Scholar] [CrossRef]
- Wang, Y.; Qi, Y.X.; Qi, Z.; Tsang, S.Y. TRPC3 Regulates the Proliferation and Apoptosis Resistance of Triple Negative Breast Cancer Cells through the TRPC3/RASA4/MAPK Pathway. Cancers 2019, 11, 558. [Google Scholar] [CrossRef]
- Frezza, M.; Hindo, S.; Chen, D.; Davenport, A.; Schmitt, S.; Tomco, D.; Ping Dou, Q. Novel metals and metal complexes as platforms for cancer therapy. Curr. Pharm. Des. 2010, 16, 1813–1825. [Google Scholar] [CrossRef] [PubMed]
- Florea, A.M.; Büsselberg, D. Anti-cancer drugs interfere with intracellular calcium signaling. Neurotoxicology 2009, 30, 803–810. [Google Scholar] [CrossRef]
- Varghese, E.; Büsselberg, D. Auranofin, an anti-rheumatic gold compound, modulates apoptosis by elevating the intracellular calcium concentration ([Ca2+]i) in MCF-7 breast cancer cells. Cancers 2014, 6, 2243–2258. [Google Scholar] [CrossRef] [PubMed]
- Florea, A.M.; Büsselberg, D. Metals and breast cancer: Risk factors or healing agents? J. Toxicol. 2011, 2011, 159619. [Google Scholar] [CrossRef] [PubMed]
- Hanigan, M.H.; Devarajan, P. Cisplatin nephrotoxicity: Molecular mechanisms. Cancer Ther. 2003, 1, 47–61. [Google Scholar]
- Dai, J.; Inscho, E.W.; Yuan, L.; Hill, S.M. Modulation of intracellular calcium and calmodulin by melatonin in MCF-7 human breast cancer cells. J. Pineal Res. 2002, 32, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.H.; Chen, C.H.; Gau, R.J.; Lin, C.C.; Tsai, C.L.; Tsai, K.; Lu, F.J. Effect of baicalein on apoptosis of the human Hep G2 cell line was induced by mitochondrial dysfunction. Planta Med. 2002, 68, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Tong, W.; Ding, X.; Adrian, T. The mechanisms of lipoxygenase inhibitor-induced apoptosis in human breast cancer cells. Biochem. Biophys. Res. Commun. 2002, 296, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Pidgeon, G.P.; Kandouz, M.; Meram, A.; Honn, K.V. Mechanisms controlling cell cycle arrest and induction of apoptosis after 12-lipoxygenase inhibition in prostate cancer cells. Cancer Res. 2002, 62, 2721–2727. [Google Scholar]
- Wong, B.C.; Wang, W.P.; Cho, C.H.; Fan, X.M.; Lin, M.C.M.; Kung, H.F.; Lam, S.K. 12-Lipoxygenase inhibition induced apoptosis in human gastric cancer cells. Carcinogenesis 2001, 22, 1349–1354. [Google Scholar] [CrossRef]
- Lee, J.H.; Li, Y.C.; Ip, S.W.; Chang, N.W.; Tang, N.Y.; Yu, C.S.; Chou, S.T.; Lin, S.S.; Lino, C.C.; Yang, J.S.; et al. The role of Ca2+ in baicalein-induced apoptosis in human breast MDA-MB-231 cancer cells through mitochondria- and caspase-3-dependent pathway. Anticancer. Res. 2008, 28, 1701–1711. [Google Scholar]
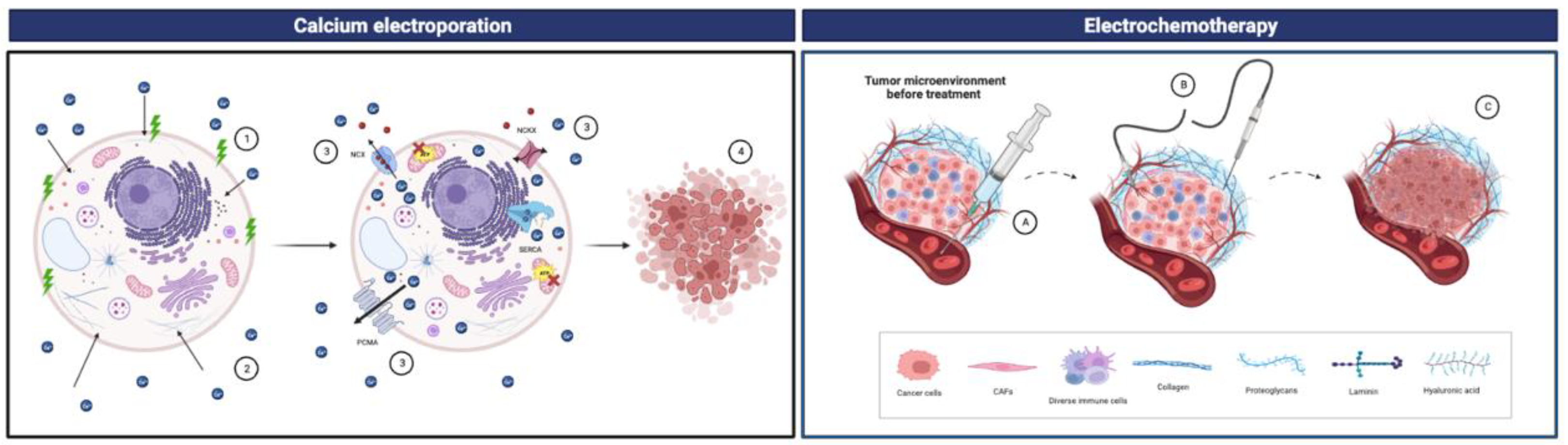
- Hoejholt, K.L.; Mužić, T.; Jensen, S.D.; Dalgaard, L.T.; Bilgin, M.; Nylandsted, J.; Heimburg, T.; Frandsen, S.K.; Gehl, J. Calcium electroporation and electrochemotherapy for cancer treatment: Importance of cell membrane composition investigated by lipidomics, calorimetry and in vitro efficacy. Sci. Rep. 2019, 9, 4758. [Google Scholar] [CrossRef]
- Frandsen, S.K.; Gibot, L.; Madi, M.; Gehl, J.; Rols, M.P. Calcium Electroporation: Evidence for Differential Effects in Normal and Malignant Cell Lines, Evaluated in a 3D Spheroid Model. PLoS ONE 2015, 1, 0144028. [Google Scholar] [CrossRef]
- Belehradek, M.; Domenge, C.; Luboinski, B.; Orlowski, S.; Belehradek, J.; Mir, L.M. Electrochemotherapy, a new antitumor treatment. First clinical phase I-II trial. Cancer 1993, 72, 3694–3700. [Google Scholar] [CrossRef] [PubMed]
- Sersa, G.; Cufer, T.; Paulin, S.M.; Cemazar, M.; Snoj, M. Electrochemotherapy of chest wall breast cancer recurrence. Cancer Treat. Rev. 2012, 38, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Matthiessen, L.W.; Johannesen, H.H.; Hendel, H.W.; Moss, T.; Kamby, C.; Gehl, J. Electrochemotherapy for large cutaneous recurrence of breast cancer: A phase II clinical trial. Acta Oncol. 2012, 51, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Falk, H.; Matthiessen, L.W.; Wooler, G.; Gehl, J. Calcium electroporation for treatment of cutaneous metastases; a randomized double-blinded phase II study, comparing the effect of calcium electroporation with electrochemotherapy. Acta Oncol. 2018, 57, 311–319. [Google Scholar] [CrossRef]
- Frandsen, S.K.; Gissel, H.; Hojmanm, P.; Tramm, T.; Eriksen, J.; Gehl, J. Direct therapeutic applications of calcium electroporation to effectively induce tumor necrosis. Cancer Res. 2012, 72, 1336–1341. [Google Scholar] [CrossRef]
- Cvetković, D.M.; Živanović, M.N.; Milutinović, M.G.; Djukic, T.R.; Radivic, M.D.; Cvetkovic, A.M.; Filipovic, N.D.; Zdravkovic, N.D. Real-time monitoring of cytotoxic effects of electroporation on breast and colon cancer cell lines. Bioelectrochemistry 2017, 113, 85–94. [Google Scholar] [CrossRef]
- Łapińska, Z.; Szwedowicz, U.; Choromańska, A.; Saczko, J. Electroporation and Electrochemotherapy in Gynecological and Breast Cancer Treatment. Molecules 2022, 27, 2476. [Google Scholar] [CrossRef]
- Łapińska, Z.; Saczko, J. Novel electroporation-based treatments for breast cancer. Adv. Clin. Exp. Med. 2022, 31, 1183–1186. [Google Scholar] [CrossRef]
- Jensen, K.B.; Lonkvist, C.K.; Gehl, J.; Vissing, M. Calcium Electroporation for Management of Cutaneous Metastases in HER2-Positive Breast Cancer: A Case Report. Case Rep. Dermatol. 2022, 14, 330–338. [Google Scholar] [CrossRef]
- Belpomme, D.; Gauthier, S.; Pujade-Lauraine, E.; Facchini, T.; Goudier, M.J.; Krakowski, I.; Netter-Pinon, G.; Frenay, M.; Gousset, C.; Marié, F.N.; et al. Verapamil increases the survival of patients with anthracycline-resistant metastatic breast carcinoma. Ann. Oncol. 2000, 11, 1471–1476. [Google Scholar] [CrossRef] [PubMed]
- Rotshild, V.; Hirsh Raccah, B.; Gazawe, M.; Matok, I. Calcium Channel Blocker Use and the Risk for Breast Cancer: A Population-Based Nested Case-Control Study. Cancers 2022, 14, 2344. [Google Scholar] [CrossRef] [PubMed]
- Li, C.I.; Daling, J.R.; Tang, M.-T.C.; Haugen, K.L.; Porter, P.L.; Malone, K.E. Use of antihypertensive medications and breast cancer risk among women aged 55 to 74 years. JAMA Intern. Med. 2013, 173, 1629. [Google Scholar] [CrossRef] [PubMed]
| Type | Molecular Target | Immunotherapeutics | Type of Patient |
|---|---|---|---|
| Tyrosine kinase inhibitors (TKIs) | ATP-binding side of HER2 and EGFR tyrosine kinase | Lapatinib | HER2+ |
| Tyrosine kinase domain of HER2 | Neratinib | HER2+ treated with adjuvant Trastazumab therapy | |
| Tyrosine kinase domain of HER2 and HER3 | Tucatinib | Advanced-stage HER2+ | |
| Human epidermal growth factor receptor type 1 (EGFR) specific tyrosine kinase domain | Pyrotinib | Advanced-stage HER2+ previously treated with chemotherapy | |
| HER2 | Extracellular domain of HER2 | Trastazumab | HER2+ |
| Pertuzumab | HER2+ with risk of relapse | ||
| Margetuximab | HER2+ in metastasis stage | ||
| Drug–antibody conjugates | Extracellular domain of HER2+ microtubule depolymerizer | Trastazumab emtansine (T-DM1) | HER2+ in metastasic stage |
| HER2 extracellular domain + maleimide + topoisomerase inhibitor | Trastazumab deruxtecan (DS-821a) | HER2+ |
| Type | Molecular Target | Chemotherapeutic | Type of Patient |
|---|---|---|---|
| Angiogenic | VEGF-A | Bevacizumab | HER2- |
| CDK4/6 inhibitor | CDK4/6 | Palbociclib Ribociclib Abemaciclib | HER2+ or HER2- |
| PI3K/Akt/mTOR pathway inhibitors | PI3K | Alpelisib | Hormone-receptor-positive and HER2-positive |
| mTORC1 | Everolimus | Advanced hormone-receptor-positive and HER2-positive | |
| PARP inhibitors | PARP | Olaparib | HER2- and BRCA-mutated breast cancer |
| Talazoparib | HER2- and locally advanced tumors or with mutations in BRCA |
| Ion Channel | Member | Overview |
|---|---|---|
| ORAI protein | ORAI1 and ORAI3 |
|
| STIM protein | STIM1 and STIM2 |
|
| Transient Receptor Potential Canonical (TRPC) channels | TRPC6 |
|
| Channel TRP | TRPC1 and TRPM2 |
|
| VGCC type T | CAV3.2 and CACNA1G |
|
| Ca2+ Pumps | Member | Overview |
|---|---|---|
| SERCA-ATPases of the endoplasmic reticulum | SERCA3 |
|
| ATPases of the plasma membrane | PMCA2 |
|
| PMCA4 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin-García, D.; Téllez, T.; Redondo, M.; García-Aranda, M. Calcium Homeostasis in the Development of Resistant Breast Tumors. Cancers 2023, 15, 2872. https://doi.org/10.3390/cancers15112872
Martin-García D, Téllez T, Redondo M, García-Aranda M. Calcium Homeostasis in the Development of Resistant Breast Tumors. Cancers. 2023; 15(11):2872. https://doi.org/10.3390/cancers15112872
Chicago/Turabian StyleMartin-García, Desirée, Teresa Téllez, Maximino Redondo, and Marilina García-Aranda. 2023. "Calcium Homeostasis in the Development of Resistant Breast Tumors" Cancers 15, no. 11: 2872. https://doi.org/10.3390/cancers15112872
APA StyleMartin-García, D., Téllez, T., Redondo, M., & García-Aranda, M. (2023). Calcium Homeostasis in the Development of Resistant Breast Tumors. Cancers, 15(11), 2872. https://doi.org/10.3390/cancers15112872






