Novel Adaption of the SARC-F Score to Classify Pediatric Hemato-Oncology Patients with Functional Sarcopenia
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. PED-SARC-F
2.3. Physiotherapy Assessment
2.4. Structural and Functional Sarcopenia Definition
2.5. Statistical Analyses
3. Results
3.1. Patients
3.2. PED-SARC-F Scores and Physiotherapy Assessment
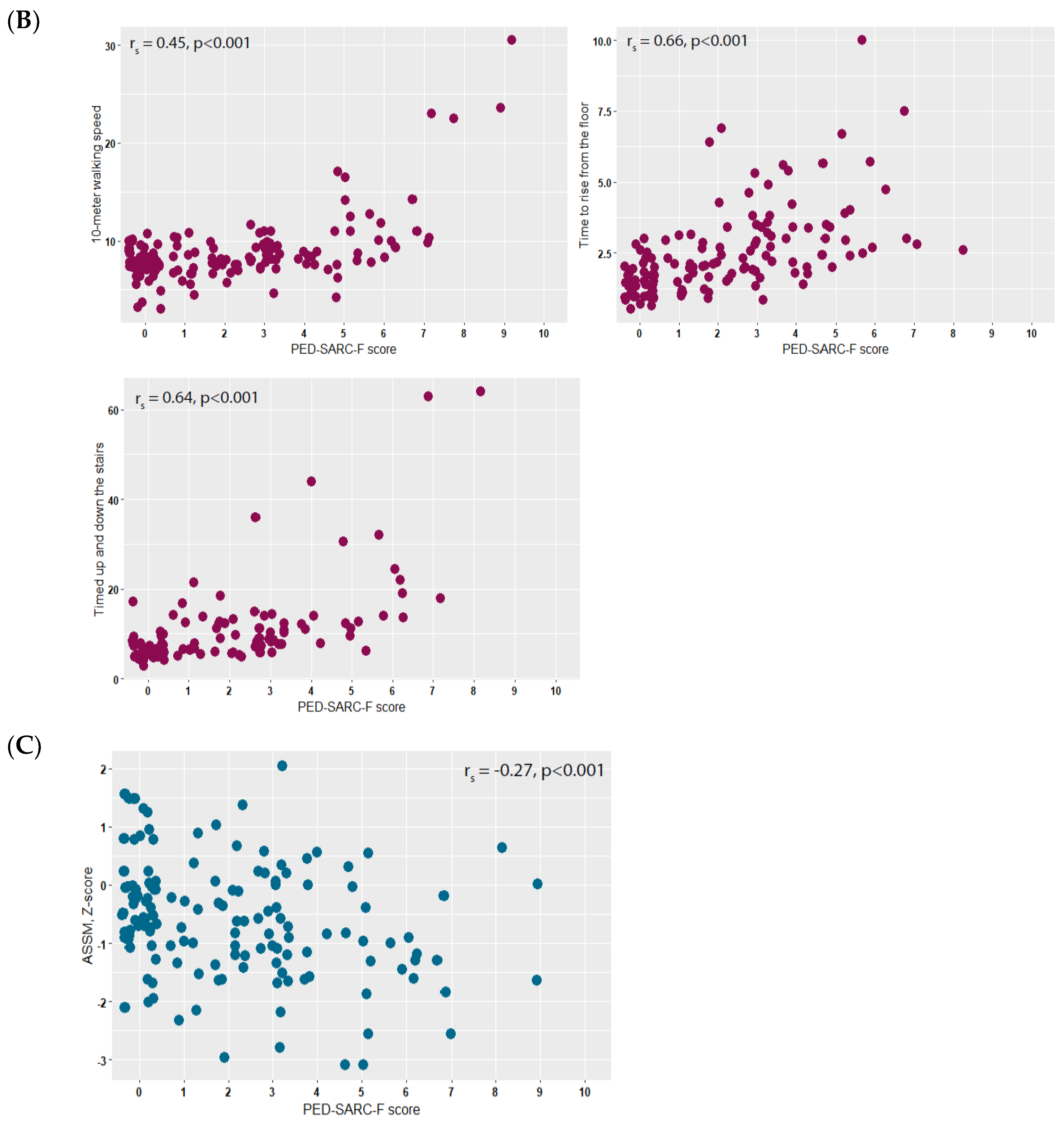
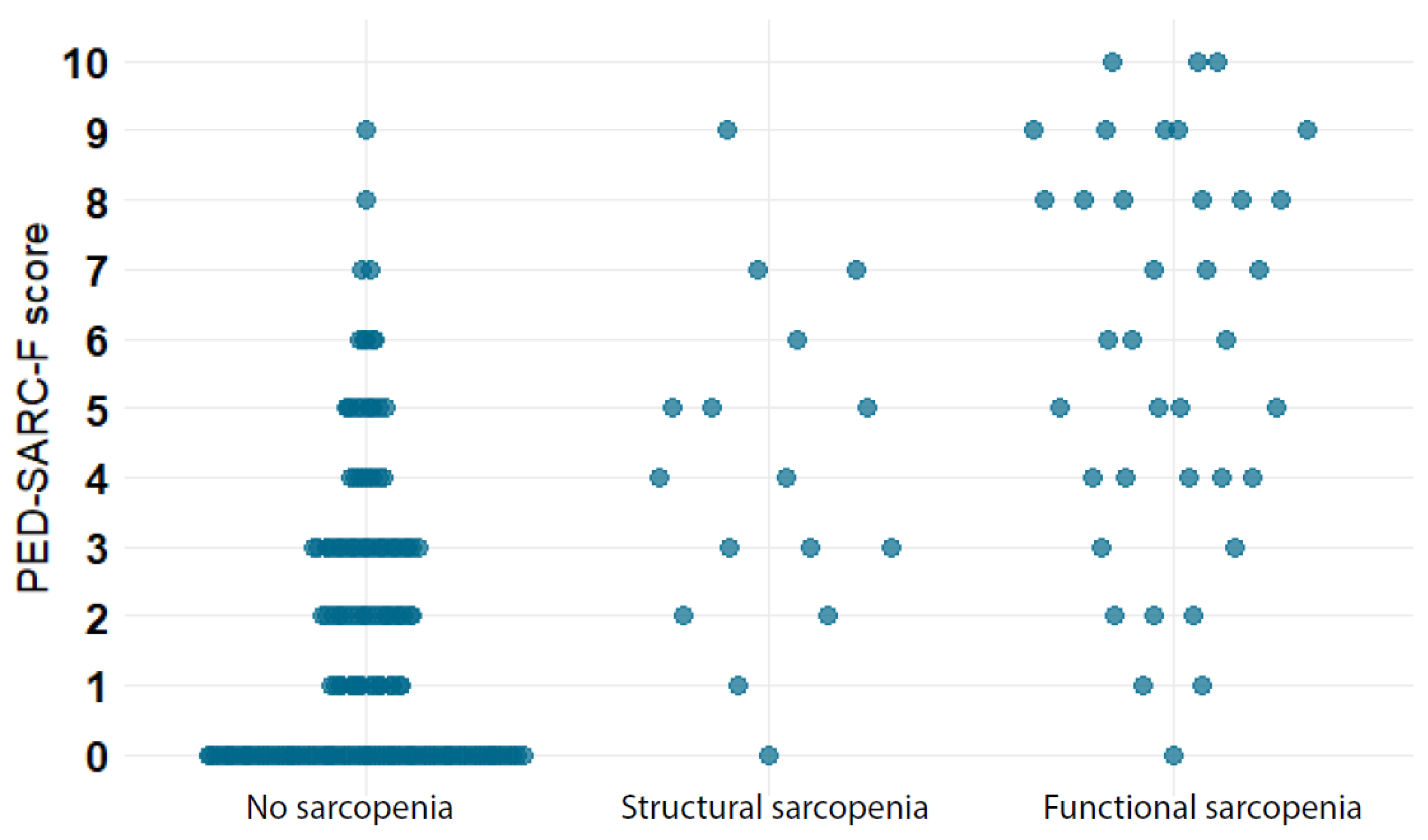
3.3. Correlations of PED-SARC-F with Muscle Strength, Physical Performance and ASMM
3.4. Diagnostic Accuracy of the PED-SARC-F for Structural and Functional Sarcopenia
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bodine, S.C.; Furlow, J.D. Glucocorticoids and Skeletal Muscle. Adv. Exp. Med. Biol. 2015, 872, 145–176. [Google Scholar] [CrossRef] [PubMed]
- Inaba, H.; Pui, C.-H. Glucocorticoid use in acute lymphoblastic leukaemia. Lancet Oncol. 2010, 11, 1096–1106. [Google Scholar] [CrossRef] [PubMed]
- van de Velde, M.E.; Kaspers, G.L.; Abbink, F.C.; Wilhelm, A.J.; Ket, J.C.F.; van den Berg, M.H. Vincristine-induced peripheral neuropathy in children with cancer: A systematic review. Crit. Rev. Oncol. Hematol. 2017, 114, 114–130. [Google Scholar] [CrossRef] [PubMed]
- van de Velde, M.E.; Berg, M.H.v.D.; Kaspers, G.J.L.; Abbink, F.C.H.; Twisk, J.W.R.; van der Sluis, I.M.; Bos, C.V.D.; Heuvel-Eibrink, M.M.V.D.; Segers, H.; Chantrain, C.; et al. The association between vincristine-induced peripheral neuropathy and health-related quality of life in children with cancer. Cancer Med. 2021, 10, 8172–8181. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A. Sarcopenia, the last organ insufficiency. Eur. Geriatr. Med. 2016, 7, 195–196. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.-Y.; Bruyère, O. Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef]
- Ooi, P.H.; Thompson-Hodgetts, S.; Pritchard-Wiart, L.; Gilmour, S.M.; Mager, D.R. Pediatric Sarcopenia: A Paradigm in the Overall Definition of Malnutrition in Children? J. Parenter. Enter. Nutr. 2020, 44, 407–418. [Google Scholar] [CrossRef]
- Rayar, M.; Webber, C.E.; Nayiager, T.; Sala, A.; Barr, R.D. Sarcopenia in Children with Acute Lymphoblastic Leukemia. J. Pediatr. Hematol. Oncol. 2013, 35, 98–102. [Google Scholar] [CrossRef]
- Suzuki, D.; Kobayashi, R.; Sano, H.; Hori, D.; Kobayashi, K. Sarcopenia after induction therapy in childhood acute lymphoblastic leukemia: Its clinical significance. Int. J. Hematol. 2018, 107, 486–489. [Google Scholar] [CrossRef]
- Hoed, M.A.H.D.; Pluijm, S.M.F.; De Groot-Kruseman, H.A.; Winkel, M.L.T.; Fiocco, M.; Akker, E.V.D.; Hoogerbrugge, P.; Berg, H.V.D.; Leeuw, J.; Bruin, M.; et al. The negative impact of being underweight and weight loss on survival of children with acute lymphoblastic leukemia. Haematologica 2015, 100, 62–69. [Google Scholar] [CrossRef]
- Malmstrom, T.K.; Morley, J.E. SARC-F: A Simple Questionnaire to Rapidly Diagnose Sarcopenia. J. Am. Med. Dir. Assoc. 2013, 14, 531–532. [Google Scholar] [CrossRef]
- Malmstrom, T.K.; Miller, D.K.; Simonsick, E.M.; Ferrucci, L.; Morley, J.E. SARC-F: A symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J. Cachexia Sarcopenia Muscle 2016, 7, 28–36. [Google Scholar] [CrossRef]
- Fu, X.; Tian, Z.; Thapa, S.; Sun, H.; Wen, S.; Xiong, H.; Yu, S. Comparing SARC-F with SARC-CalF for screening sarcopenia in advanced cancer patients. Clin. Nutr. 2020, 39, 3337–3345. [Google Scholar] [CrossRef]
- Lu, J.-L.; Ding, L.-Y.; Xu, Q.; Zhu, S.-Q.; Xu, X.-Y.; Hua, H.-X.; Chen, L.; Xu, H. Screening Accuracy of SARC-F for Sarcopenia in the Elderly: A Diagnostic Meta-Analysis. J. Nutr. Health Aging 2021, 25, 172–182. [Google Scholar] [CrossRef]
- Ida, S.; Kaneko, R.; Murata, K. SARC-F for Screening of Sarcopenia Among Older Adults: A Meta-analysis of Screening Test Accuracy. J. Am. Med. Dir. Assoc. 2018, 19, 685–689. [Google Scholar] [CrossRef]
- Beenakker, E.; van der Hoeven, J.; Fock, J.; Maurits, N. Reference values of maximum isometric muscle force obtained in 270 children aged 4–16 years by hand-held dynamometry. Neuromuscul. Disord. 2001, 11, 441–446. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Wang, Y.-C.; Bubela, D.; Gershon, R.C. Handgrip Strength: A Population-Based Study of Norms and Age Trajectories for 3- to 17-Year-Olds. Pediatr. Phys. Ther. 2017, 29, 118–123. [Google Scholar] [CrossRef]
- Pereira, A.C.; Ribeiro, M.G.; Araújo, A.P.D.Q.C.; AnaBarta, L.M.; Sossai, B.; Vasconcelos, C.; Sampaio, I.; Campos, I.P.D.Q.; Da Costa, A.C.; De Novaes, B.M.; et al. Timed motor function tests capacity in healthy children. Arch. Dis. Child. 2016, 101, 147–151. [Google Scholar] [CrossRef]
- McCarthy, H.D.; Samani-Radia, D.; Jebb, S.A.; Prentice, A.M. Skeletal muscle mass reference curves for children and adolescents. Pediatr. Obes. 2014, 9, 249–259. [Google Scholar] [CrossRef]
- Webber, C.E.; Barr, R.D. Age- and gender-dependent values of skeletal muscle mass in healthy children and adolescents. J. Cachex- Sarcopenia Muscle 2012, 3, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Zaino, C.A.; Marchese, V.G.; Westcott, S.L. Timed Up and Down Stairs Test: Preliminary Reliability and Validity of a New Measure of Functional Mobility. Pediatr. Phys. Ther. 2004, 16, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Ness, K.K.; Krull, K.R.; Jones, K.E.; Mulrooney, D.A.; Armstrong, G.T.; Green, D.M.; Chemaitilly, W.; A Smith, W.; Wilson, C.L.; Sklar, C.A.; et al. Physiologic Frailty as a Sign of Accelerated Aging Among Adult Survivors of Childhood Cancer: A Report from the St Jude Lifetime Cohort Study. J. Clin. Oncol. 2013, 31, 4496–4503. [Google Scholar] [CrossRef] [PubMed]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S. Assessing the Fit of the Model; Wiley: New York, NY, USA, 2000; pp. 143–202. [Google Scholar]
- Shreffler, J.; Huecker, M.R. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive Values and Likelihood Ratios; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- RStudio Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Larsson, L.; Degens, H.; Li, M.; Salviati, L.; Lee, Y.I.; Thompson, W.; Kirkland, J.L.; Sandri, M. Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol. Rev. 2019, 99, 427–511. [Google Scholar] [CrossRef]
- Silleras, B.D.M.; de la Cruz, S.; Alonso-Izquierdo, L.; Camina-Martín, M.A.; Marugán-De-Miguelsanz, J.M.; Redondo-Del-Río, M.P. Bioelectrical impedance vector analysis in obese and overweight children. PLoS ONE 2019, 14, e0211148. [Google Scholar] [CrossRef]
- de Castro, J.A.C.; de Lima, T.R.; Silva, D.A.S. Body composition estimation in children and adolescents by bioelectrical impedance analysis: A systematic review. J. Bodyw. Mov. Ther. 2018, 22, 134–146. [Google Scholar] [CrossRef]
- Barbosa-Silva, T.G.; Menezes, A.M.B.; Bielemann, R.M.; Malmstrom, T.K.; Gonzalez, M.C.; Grupo de Estudos em Composição Corporal e Nutrição (COCONUT). Enhancing SARC-F: Improving Sarcopenia Screening in the Clinical Practice. J. Am. Med. Dir. Assoc. 2016, 17, 1136–1141. [Google Scholar] [CrossRef]
- Marini, A.C.B.; Perez, D.R.S.; Fleuri, J.A.; Pimentel, G.D. SARC-F Is Better Correlated with Muscle Function Indicators Than Muscle Mass in Older Hemodialysis Patients. J. Nutr. Health Aging 2020, 24, 1–4. [Google Scholar] [CrossRef]
- Siqueira, J.M.; de Oliveira, I.C.; Soares, J.D.; Pimentel, G.D. SARC-F has low correlation and reliability with skeletal muscle mass index in older gastrointestinal cancer patients. Clin. Nutr. 2021, 40, 890–894. [Google Scholar] [CrossRef]
- Voelker, S.N.; Michalopoulos, N.; Maier, A.B.; Reijnierse, E.M. Reliability and Concurrent Validity of the SARC-F and Its Modified Versions: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2021, 22, 1864–1876.e16. [Google Scholar] [CrossRef]
- Nielsen, M.K.; Larsen, H.B.; Schmiegelow, K.; Christensen, J.F. Muscle Dysfunction in Childhood Cancer: Biological Mechanisms and Implications for Long-Term Survivorship. EMJ Oncol. 2016, 4, 78–85. [Google Scholar] [CrossRef]
- Coombs, A.; Schilperoort, H.; Sargent, B. The effect of exercise and motor interventions on physical activity and motor outcomes during and after medical intervention for children and adolescents with acute lymphoblastic leukemia: A systematic review. Crit. Rev. Oncol. Hematol. 2020, 152, 103004. [Google Scholar] [CrossRef]
- Grimshaw, S.L.; Taylor, N.F.; Shields, N. The Feasibility of Physical Activity Interventions During the Intense Treatment Phase for Children and Adolescents with Cancer: A Systematic Review. Pediatr. Blood Cancer 2016, 63, 1586–1593. [Google Scholar] [CrossRef]


| No. | % | |
| Sex | ||
| Boy | 134 | 62.3 |
| Girl | 81 | 37.7 |
| Type of hematological disease | ||
| Acute lymphoblastic leukemia | 129 | 60 |
| Acute myeloid leukemia | 24 | 11.2 |
| Chronic myeloid leukemia | 6 | 2.8 |
| Hodgkin lymphoma | 8 | 3.7 |
| Non-Hodgkin lymphoma | 16 | 7.4 |
| Myelodysplastic syndrome | 8 | 3.7 |
| Fanconi anemia | 14 | 6.5 |
| Aplastic anemia | 3 | 1.4 |
| Other * | 7 | 3.3 |
| Treatment phase | ||
| Intensive chemotherapy | 54 | 25.1 |
| Maintenance chemotherapy | 57 | 26.5 |
| 1–12 months after chemotherapy cessation | 19 | 8.9 |
| Pre SCT conditioning phase | 31 | 14.4 |
| 3–12 months post SCT | 54 | 25.1 |
| Assessment performed during | ||
| Clinical admission | 36 | 16.7 |
| Daycare admission/Outpatient clinic visit | 179 | 83.3 |
| Body Mass Index, categories | ||
| Underweight | 18 | 8.4 |
| Normal Weight | 141 | 65.6 |
| Overweight | 41 | 19 |
| Obesity | 15 | 7 |
| Mean | Median [IQR] | |
| Age, years | 12.1 | 12.9 [8.5 to 15.8] |
| Height, SDS | −0.31 | −0.27 [−0.8 to 1.2] |
| Weight, SDS | 0.25 | 0.13 [−0.8 to 1.2] |
| Body Mass Index, SDS | 0.33 | 0.33 [−0.8 to 1.6] |
| N | Median | Interquartile Range | Measurement Not Performed | ||
|---|---|---|---|---|---|
| Incapable | Other I | ||||
| Muscle strength measurements | |||||
| Handgrip strength | 100 | 14 | 101 | ||
| Dominant hand, kilograms | 17.4 | 8.7 to 27.5 | |||
| Dominant hand, Z-score II | −0.75 | 1.0 | |||
| Hip flexion, strength | 123 | 23 | 69 | ||
| Left hip, Newton | 126 | 101 to 192 | |||
| Right hip, Newton | 133 | 98 to 177 | |||
| Mean Left + Right hip, Z-score II | −2.3 | 1.2 | |||
| Knee extension strength | 139 | 19 | 57 | ||
| Left leg, Newton | 184 | 131 to 259 | |||
| Right leg, Newton | 186 | 128 to 269 | |||
| Mean Left + Right leg, Z-score II | −1.5 | 1.2 | |||
| Physical performance measurements | |||||
| 10 m Walk Test | 144 | 11 | 60 | ||
| Time, seconds | 8.1 | 7.4 to 9.5 | |||
| Meters per second | 1.23 | 1.0 to 1.4 | |||
| Time To Rise from the Floor | 141 | 2 | 1.4 to 2.9 | 26 | 48 |
| Time, seconds | |||||
| Timed Up and Down Stairs | 115 | 27 | 103 | ||
| Time, seconds | 7.8 | 5.8 to 12.4 | |||
| Step per second | 0.4 | 0.3 to 0.6 | |||
| Muscle mass measurement | |||||
| Bio-electrical impedance analysis | 175 | NR | 70 | ||
| ASMM, kg | 14.5 | 8.4 to 19.8 | |||
| ASMM, % II | 28.4 | 25.4 to 30.7 | |||
| ASMM, Z-score II | −0.60 | −1.2 to 0.0 | |||
| OR | 95% CI | AUC (95% CI) | |
|---|---|---|---|
| Functional sarcopenia | 0.90 (0.84 to 0.95) | ||
| PED-SARC-F, per point | 2.07 | 1.68 to 2.55 | |
| Sex, boy vs. girl | 0.71 | 0.28 to 1.78 | |
| Age, years | 0.98 | 0.89 to 1.08 | |
| Structural sarcopenia | 0.79 (0.68 to 0.90) | ||
| PED-SARC-F, per point | 1.54 | 1.23 to 1.93 | |
| Age, years | 0.99 | 0.87 to 1.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verwaaijen, E.J.; van der Torre, P.; Vormoor, J.; Pieters, R.; Fiocco, M.; Hartman, A.; van den Heuvel-Eibrink, M.M. Novel Adaption of the SARC-F Score to Classify Pediatric Hemato-Oncology Patients with Functional Sarcopenia. Cancers 2023, 15, 320. https://doi.org/10.3390/cancers15010320
Verwaaijen EJ, van der Torre P, Vormoor J, Pieters R, Fiocco M, Hartman A, van den Heuvel-Eibrink MM. Novel Adaption of the SARC-F Score to Classify Pediatric Hemato-Oncology Patients with Functional Sarcopenia. Cancers. 2023; 15(1):320. https://doi.org/10.3390/cancers15010320
Chicago/Turabian StyleVerwaaijen, Emma J., Patrick van der Torre, Josef Vormoor, Rob Pieters, Marta Fiocco, Annelies Hartman, and Marry M. van den Heuvel-Eibrink. 2023. "Novel Adaption of the SARC-F Score to Classify Pediatric Hemato-Oncology Patients with Functional Sarcopenia" Cancers 15, no. 1: 320. https://doi.org/10.3390/cancers15010320
APA StyleVerwaaijen, E. J., van der Torre, P., Vormoor, J., Pieters, R., Fiocco, M., Hartman, A., & van den Heuvel-Eibrink, M. M. (2023). Novel Adaption of the SARC-F Score to Classify Pediatric Hemato-Oncology Patients with Functional Sarcopenia. Cancers, 15(1), 320. https://doi.org/10.3390/cancers15010320






