Physical Activity and Long-Term Risk of Breast Cancer, Associations with Time in Life and Body Composition in the Prospective Malmö Diet and Cancer Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
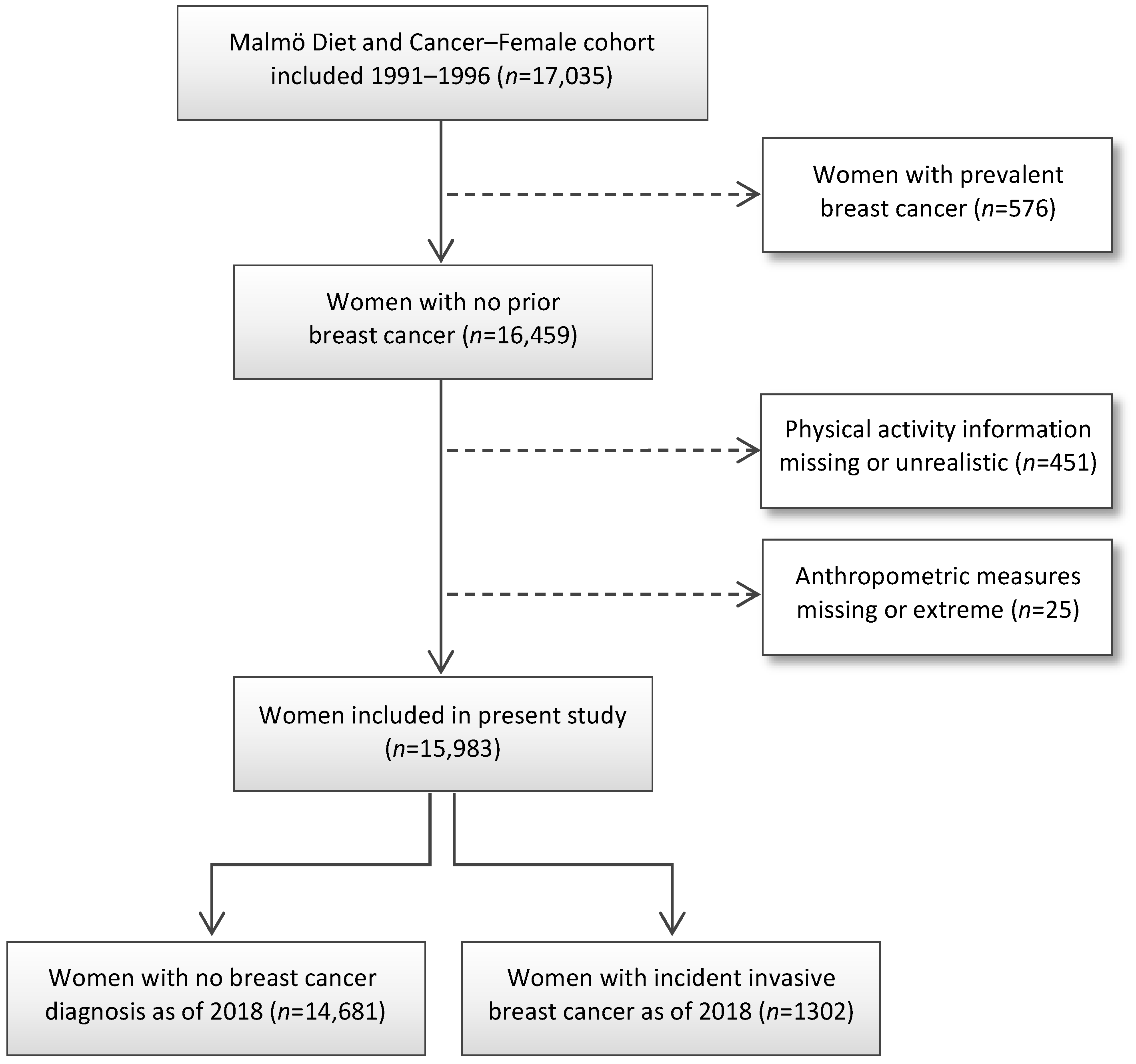
2.1. Study Population
2.2. Eligibility and Exclusion Criteria
2.3. Physical Activity Assessment
2.4. Definition of Subgroups by Menopausal Status and Body Composition
2.5. Endpoint
2.6. Statistical Analysis
Covariate Adjustments
3. Results
3.1. Baseline Characteristics Based on Physical Activity Levels
3.2. Physical Activity Levels in Relation to Breast Cancer Status
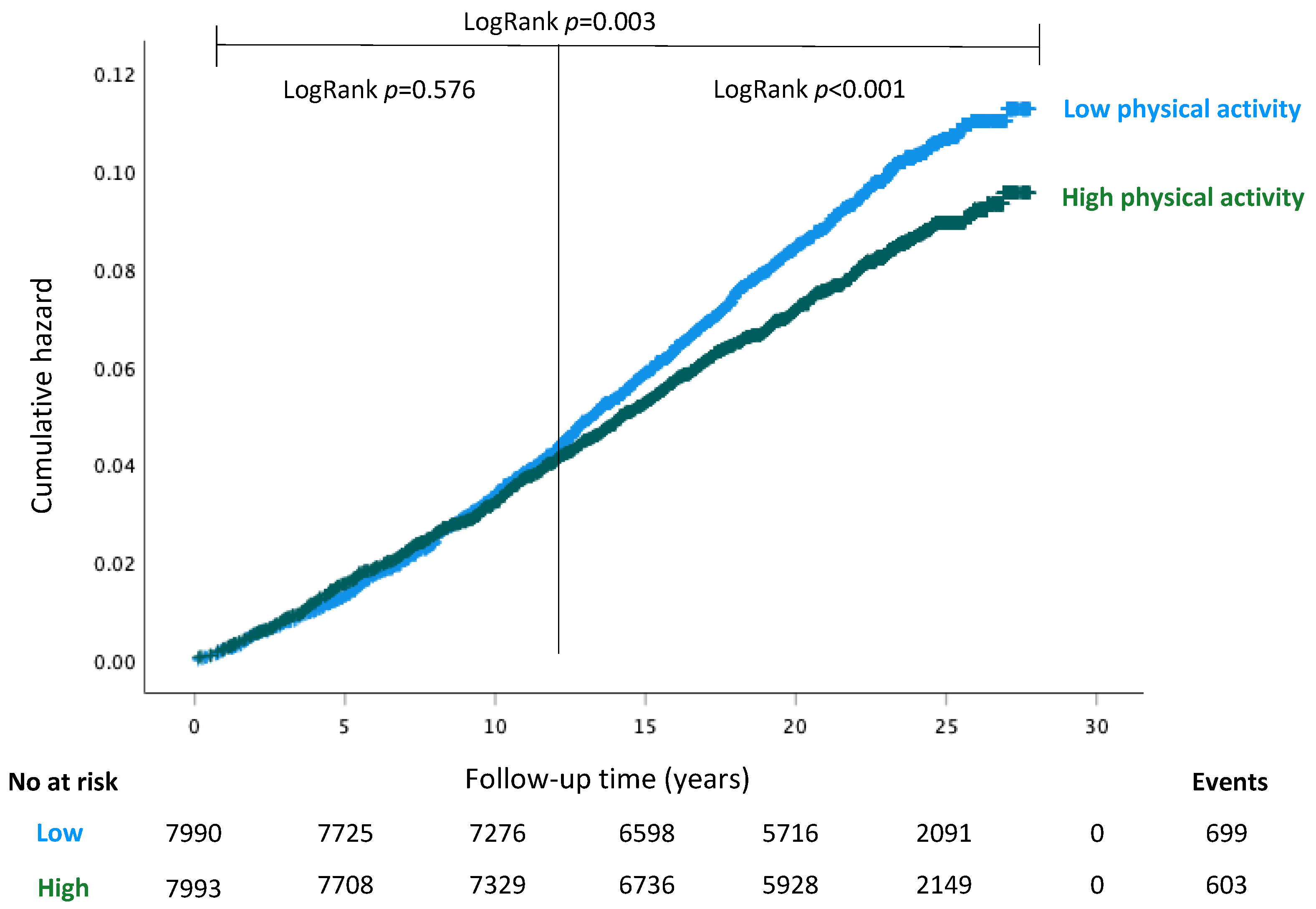
3.3. Breast Cancer Incidence Based on Physical Activity Levels
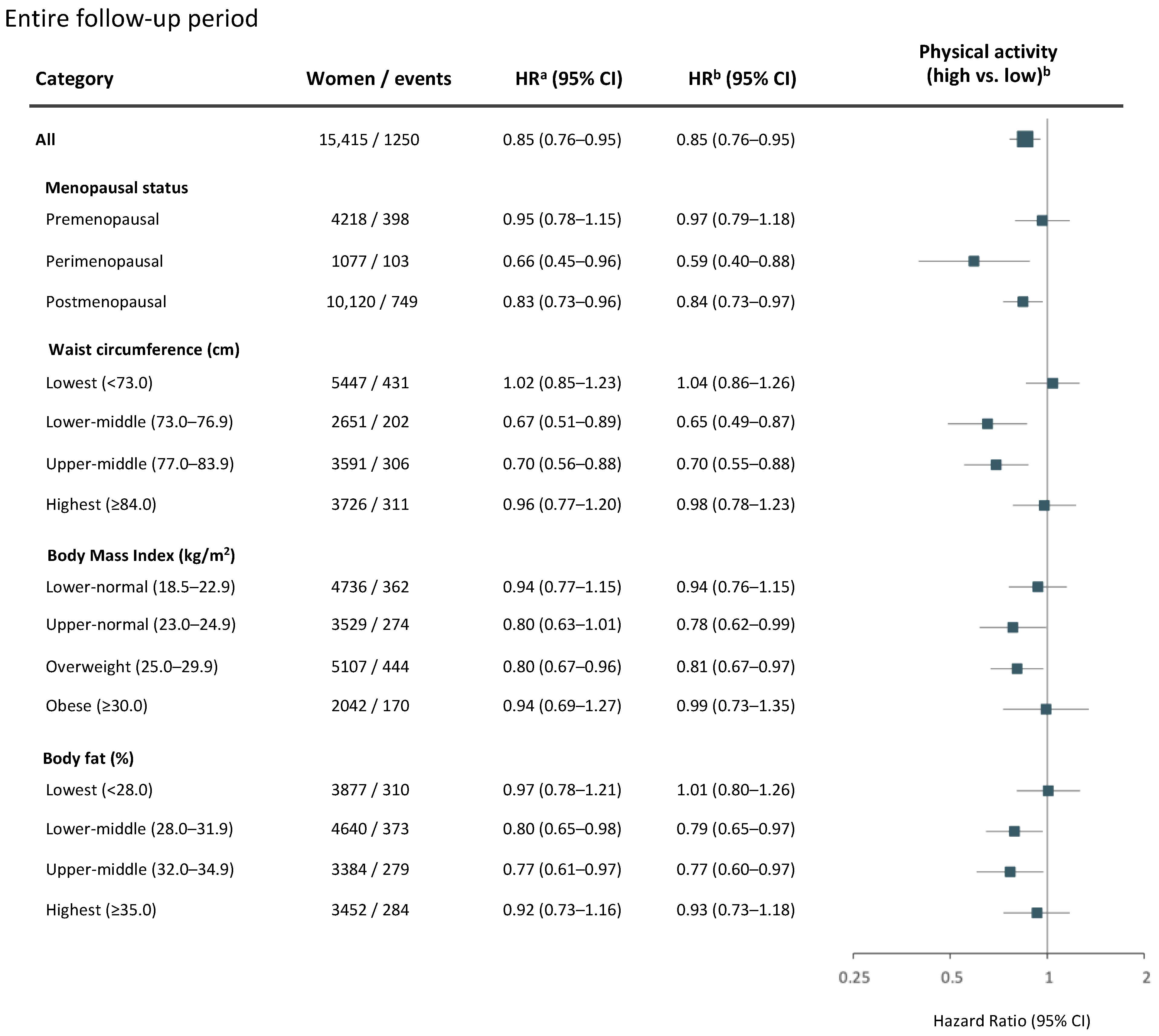
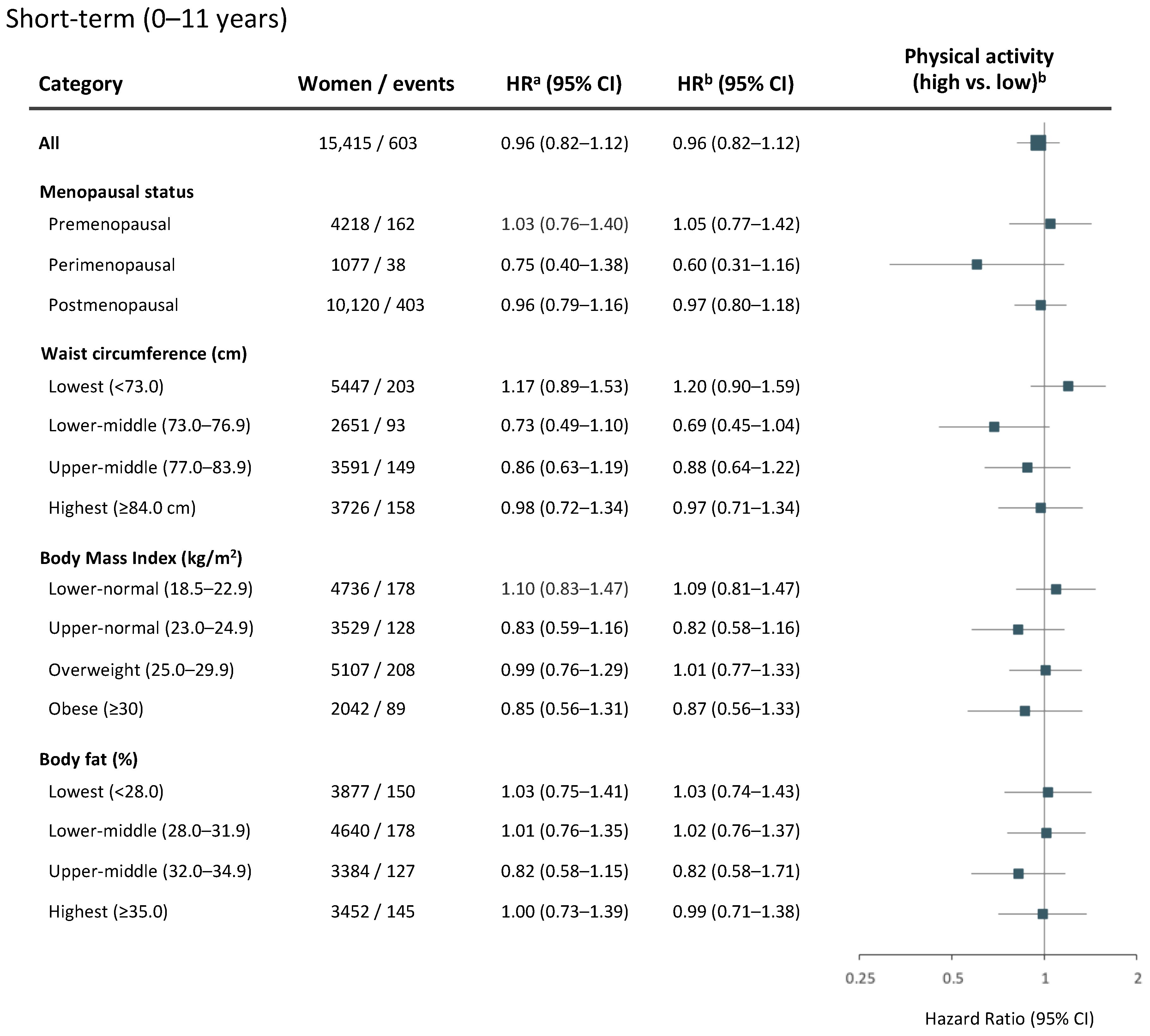
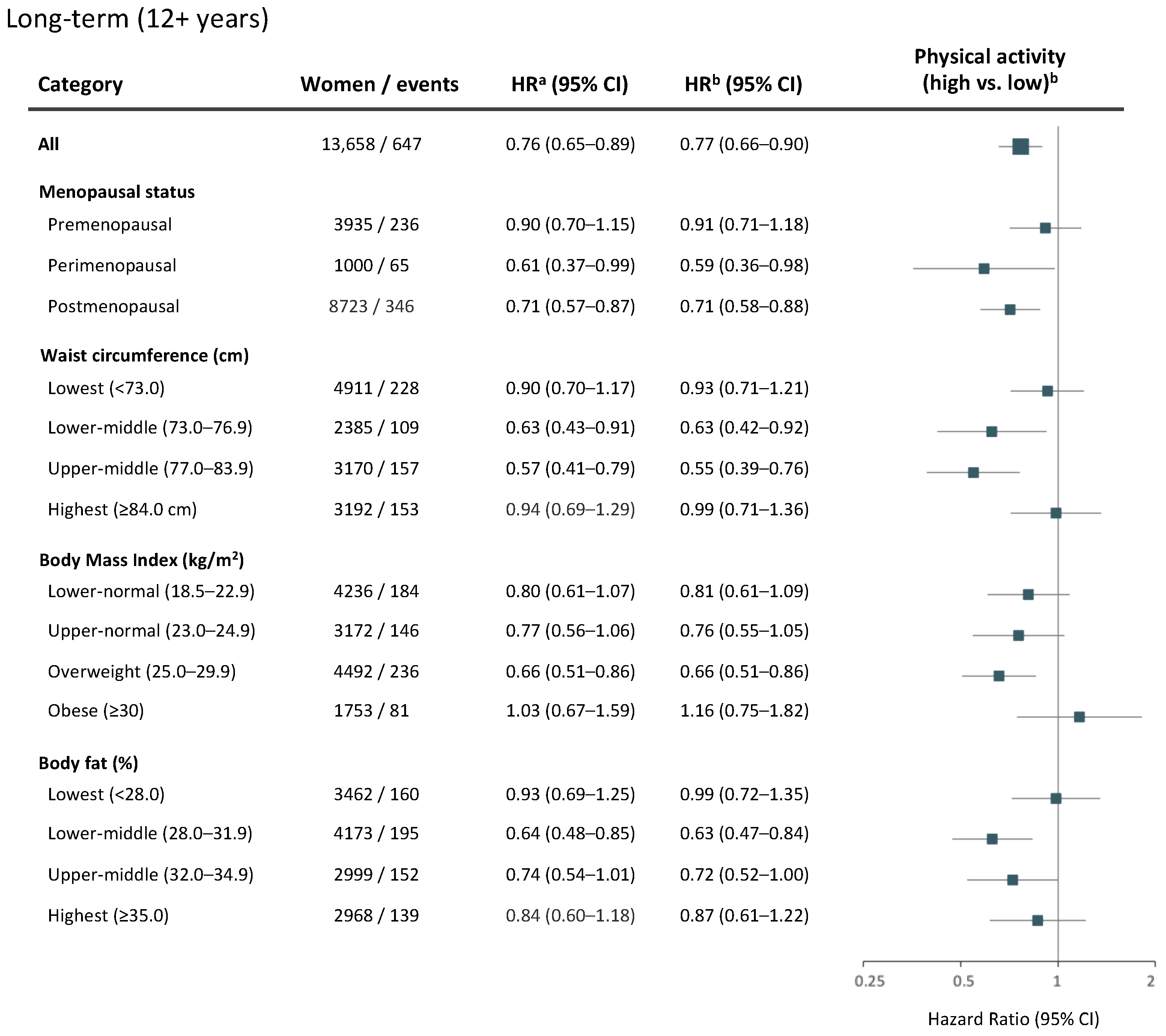
3.4. Physical Activity and Breast Cancer Risk Overall, and Based on Menopausal Status and Body Composition
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: Globocan Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Thun, M.J.; Linet, M.S.; Cerhan, J.R.; Haiman, C.; Schottenfeld, D. Cancer Epidemiology and Prevention, 4th ed.; Oxford University Press: New York, NY, USA, 2018; 1308p. [Google Scholar]
- Kopp, W. How Western Diet and Lifestyle Drive the Pandemic of Obesity and Civilization Diseases. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2221–2236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 15 March 2022).
- Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; Naghavi, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [PubMed]
- Gray, N.; Picone, G.; Sloan, F.; Yashkin, A. Relation between BMI and diabetes mellitus and its complications among US older adults. South Med. J. 2015, 108, 29–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casanova, F.; O’Loughlin, J.; Martin, S.; Beaumont, R.N.; Wood, A.R.; Watkins, E.R.; Freathy, R.M.; Hagenaars, S.P.; Frayling, T.M.; Yaghootkar, H.; et al. Higher adiposity and mental health: Causal inference using Mendelian randomization. Hum. Mol. Genet. 2021, 30, 2371–2382. [Google Scholar] [CrossRef]
- Lauby-Secretan, B.; Scoccianti, C.; Loomis, D.; Grosse, Y.; Bianchini, F.; Straif, K. Body Fatness and Cancer—Viewpoint of the IARC Working Group. N. Engl. J. Med. 2016, 375, 794–798. [Google Scholar] [CrossRef] [Green Version]
- Meseguer, A.; Puche, C.; Cabero, A. Sex steroid biosynthesis in white adipose tissue. Horm. Metab. Res. 2002, 34, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Van den Brandt, P.A.; Spiegelman, D.; Yaun, S.S.; Adami, H.O.; Beeson, L.; Folsom, A.R.; Fraser, G.; Goldbohm, R.A.; Graham, S.; Kushi, L.; et al. Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am. J. Epidemiol. 2000, 152, 514–527. [Google Scholar] [CrossRef] [Green Version]
- The Premenopausal Breast Cancer Collaborative Group. Association of Body Mass Index and Age with Subsequent Breast Cancer Risk in Premenopausal Women. JAMA Oncol. 2018, 4, e181771. [Google Scholar] [CrossRef]
- Pierobon, M.; Frankenfeld, C.L. Obesity as a risk factor for triple-negative breast cancers: A systematic review and meta-analysis. Breast Cancer Res. Treat. 2013, 137, 307–314. [Google Scholar] [CrossRef]
- Moore, S.C.; Lee, I.M.; Weiderpass, E.; Campbell, P.T.; Sampson, J.N.; Kitahara, C.M.; Keadle, S.K.; Arem, H.; Berrington de Gonzalez, A.; Hartge, P.; et al. Association of Leisure-Time Physical Activity with Risk of 26 Types of Cancer in 1.44 Million Adults. JAMA Intern. Med. 2016, 176, 816–825. [Google Scholar] [CrossRef] [PubMed]
- De Roon, M.; May, A.M.; McTiernan, A.; Scholten, R.; Peeters, P.H.M.; Friedenreich, C.M.; Monninkhof, E.M. Effect of exercise and/or reduced calorie dietary interventions on breast cancer-related endogenous sex hormones in healthy postmenopausal women. Breast Cancer Res. 2018, 20, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, A.V.; Friedenreich, C.M.; Moore, S.C.; Hayes, S.C.; Silver, J.K.; Campbell, K.L.; Winters-Stone, K.; Gerber, L.H.; George, S.M.; Fulton, J.E.; et al. American College of Sports Medicine Roundtable Report on Physical Activity, Sedentary Behavior, and Cancer Prevention and Control. Med. Sci. Sports Exerc. 2019, 51, 2391–2402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, W.; Fensom, G.K.; Reeves, G.K.; Key, T.J. Physical activity and breast cancer risk: Results from the UK Biobank prospective cohort. Br. J. Cancer 2020, 122, 726–732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, D.S.M.; Abar, L.; Cariolou, M.; Nanu, N.; Greenwood, D.C.; Bandera, E.V.; McTiernan, A.; Norat, T. World Cancer Research Fund International: Continuous Update Project-systematic literature review and meta-analysis of observational cohort studies on physical activity, sedentary behavior, adiposity, and weight change and breast cancer risk. Cancer Causes Control 2019, 30, 1183–1200. [Google Scholar] [CrossRef] [Green Version]
- Neilson, H.K.; Farris, M.S.; Stone, C.R.; Vaska, M.M.; Brenner, D.R.; Friedenreich, C.M. Moderate-vigorous recreational physical activity and breast cancer risk, stratified by menopause status: A systematic review and meta-analysis. Menopause 2017, 24, 322–344. [Google Scholar] [CrossRef]
- Lynch, B.M.; Neilson, H.K.; Friedenreich, C.M. Physical activity and breast cancer prevention. Recent Results Cancer Res. 2011, 186, 13–42. [Google Scholar]
- Maliniak, M.L.; Gapstur, S.M.; McCullough, L.E.; Rees-Punia, E.; Gaudet, M.M.; Um, C.Y.; Guinter, M.A.; Flanders, W.D.; Patel, A.V. Joint associations of physical activity and body mass index with the risk of established excess body fatness-related cancers among postmenopausal women. Cancer Causes Control 2021, 32, 127–138. [Google Scholar] [CrossRef]
- Minihan, A.K.; Patel, A.V.; Flanders, W.D.; Sauer, A.G.; Jemal, A.; Islami, F. Proportion of Cancer Cases Attributable to Physical Inactivity by US State, 2013–2016. Med. Sci. Sports Exerc. 2022, 54, 417–423. [Google Scholar] [CrossRef]
- Breast Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed on 15 March 2022).
- Taylor, H.L.; Jacobs, D.R., Jr.; Schucker, B.; Knudsen, J.; Leon, A.S.; Debacker, G. A questionnaire for the assessment of leisure time physical activities. J. Chronic. Dis. 1978, 31, 741–755. [Google Scholar] [CrossRef]
- Li, C.; Aronsson, C.A.; Hedblad, B.; Gullberg, B.; Wirfalt, E.; Berglund, G. Ability of physical activity measurements to assess health-related risks. Eur. J. Clin. Nutr. 2009, 63, 1448–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R., Jr.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, Y.; Zhang, D.; Kang, S. Physical activity and risk of breast cancer: A meta-analysis of prospective studies. Breast Cancer Res. Treat. 2013, 137, 869–882. [Google Scholar] [CrossRef] [PubMed]
- WHO Guidelines on Physical Activity and Sedentary Behaviour. 2020. Available online: https://apps.who.int/iris/handle/10665/337001 (accessed on 8 April 2022).
- Matthews, C.E.; Moore, S.C.; Arem, H.; Cook, M.B.; Trabert, B.; Hakansson, N.; Larsson, S.C.; Wolk, A.; Gapstur, S.M.; Lynch, B.M.; et al. Amount and Intensity of Leisure-Time Physical Activity and Lower Cancer Risk. J. Clin. Oncol. 2020, 38, 686–697. [Google Scholar] [CrossRef] [PubMed]
- Peters, T.M.; Schatzkin, A.; Gierach, G.L.; Moore, S.C.; Lacey, J.V., Jr.; Wareham, N.J.; Ekelund, U.; Hollenbeck, A.R.; Leitzmann, M.F. Physical activity and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Cancer Epidemiol. Biomark. Prev. 2009, 18, 289–296. [Google Scholar] [CrossRef] [Green Version]
- Peters, T.M.; Moore, S.C.; Gierach, G.L.; Wareham, N.J.; Ekelund, U.; Hollenbeck, A.R.; Schatzkin, A.; Leitzmann, M.F. Intensity and timing of physical activity in relation to postmenopausal breast cancer risk: The prospective NIH-AARP diet and health study. BMC Cancer 2009, 9, 349. [Google Scholar] [CrossRef] [Green Version]
- Colditz, G.A.; Feskanich, D.; Chen, W.Y.; Hunter, D.J.; Willett, W.C. Physical activity and risk of breast cancer in premenopausal women. Br. J. Cancer 2003, 89, 847–851. [Google Scholar] [CrossRef] [Green Version]
- Neil-Sztramko, S.E.; Boyle, T.; Milosevic, E.; Nugent, S.F.; Gotay, C.C.; Campbell, K.L. Does obesity modify the relationship between physical activity and breast cancer risk? Breast Cancer Res. Treat. 2017, 166, 367–381. [Google Scholar] [CrossRef]
- Iyengar, N.M.; Zhou, X.K.; Mendieta, H.; Giri, D.D.; El-Hely, O.; Winston, L.; Falcone, D.J.; Wang, H.; Meng, L.; Landa, J.; et al. Effects of Adiposity and Exercise on Breast Tissue and Systemic Metabo-Inflammatory Factors in Women at High Risk or Diagnosed with Breast Cancer. Cancer Prev. Res. 2021, 14, 541–550. [Google Scholar] [CrossRef]
| Physical Activity Level | ||||
|---|---|---|---|---|
| All | Low | High | Not Included | |
| (n = 17,035) | (n = 7990) | (n = 7993) | (n = 1052) | |
| Age at baseline | 56.7 (50–63.8) | 56.6 (50.0–63.3) | 56.3 (49.8–63.8) | 61 (53.8–66) |
| Age at diagnosis | 64.6 (56.2–72) | 68.5 (62.4–74.2) | 67.2 (61.6–74.0) | 52.7 (46.7–60.4) |
| ANTHROPOMETRY | ||||
| Weight (kg) | 66 (60–74) | 67 (60–75) | 66 (60–73) | 68 (61–77) |
| Height (cm) | 164 (160–168) | 163 (159–168) | 164 (160–168) | 163 (159–167) |
| Waist (cm) | 76 (70–83) | 77 (71–85) | 75 (70–82) | 78 (72–87) |
| Hip (cm) | 97 (91–103) | 97 (92–104) | 96 (91–102) | 98 (93–106) |
| BMI (kg/m2) | 24.7 (22.5–27.7) | 24.9 (22.7–28.0) | 24.4 (22.3–27.1) | 25.5 (22.9–28.7) |
| Body fat (%) | 31 (28–34) | 31 (28–35) | 30 (27–34) | 32 (29–35) |
| SOCIOECONOMY | ||||
| Occupation | ||||
| Manual worker | 6430 (38.1) | 3098 (39.2) | 2879 (36.3) | 453 (44.2) |
| Nonmanual worker | 9156 (54.3) | 4226 (53.4) | 4434 (55.9) | 496 (48.4) |
| Employer/self-employed | 1276 (7.6) | 587 (7.4) | 614 (7.7) | 75 (7.3) |
| Missing | 173 (1.0) | 79 (1.0) | 66 (0.8) | 28 (2.7) |
| LIFESTYLE AND REPRODUCTIVE FACTORS | ||||
| Age at menarche | ||||
| ≤12 years | 3726 (22) | 1778 (22.4) | 1739 (21.9) | 209 (20.3) |
| 13–14 years | 9013 (53.3) | 4203 (52.9) | 4275 (53.9) | 535 (51.8) |
| >15 years | 4171 (24.7) | 1963 (24.7) | 1920 (24.2) | 288 (27.9) |
| Missing | 125 (0.7) | 46 (0.6) | 59 (0.7) | 20 (1.9) |
| Parity | ||||
| 0 | 2184 (13.0) | 968 (12.3) | 1046 (13.3) | 170 (16.5) |
| 1 | 3640 (21.7) | 1729 (22.0) | 1635 (20.8) | 276 (26.8) |
| 2 | 6990 (41.7) | 3283 (41.8) | 3350 (42.6) | 357 (34.7) |
| 3 | 2813 (16.8) | 1339 (17.0) | 1329 (16.9) | 145 (14.1) |
| 4 or more | 1118 (6.7) | 540 (6.9) | 498 (6.3) | 80 (7.8) |
| Missing | 290 (1.7) | 131 (1.6) | 135 (1.7) | 24 (2.3) |
| Age at first childbirth | ||||
| Nulliparous | 2184 (13.1) | 968 (12.3) | 1046 (13.3) | 170 (16.6) |
| ≤20 years | 2832 (16.9) | 1379 (17.6) | 1278 (16.3) | 175 (17.1) |
| 21–25 years | 5970 (35.7) | 2772 (35.3) | 2856 (36.4) | 342 (33.4) |
| 26–30 years | 4151 (24.8) | 1952 (24.9) | 1962 (25.0) | 237 (23.1) |
| >30 years | 1596 (9.5) | 783 (10.0) | 712 (9.5) | 101 (9.9) |
| Missing | 302 (1.8) | 136 (1.7) | 139 (1.7) | 27 (2.6) |
| Oral contraceptive use | ||||
| Never | 8665 (50.9) | 4016 (50.3) | 4022 (50.4) | 627 (60.1) |
| Ever | 8354 (49.1) | 3972 (49.7) | 3966 (49.6) | 416 (39.9) |
| Menopausal status | ||||
| Premenopausal | 4452 (26.1) | 2110 (26.4) | 2189 (27.4) | 153 (14.5) |
| Perimenopausal | 1195 (7.0) | 553 (6.9) | 581 (7.3) | 61 (5.8) |
| Postmenopausal | 11,388 (66.9) | 5327 (66.7) | 5223 (65.3) | 838 (79.7) |
| Current HRT use | ||||
| No | 13,111 (77.2) | 6138 (77.0) | 6064 (76.1) | 909 (86.6) |
| Yes | 3877 (22.8) | 1829 (23.0) | 1907 (23.9) | 141 (13.4) |
| Alcohol | ||||
| Nothing last year | 1947 (11.5) | 966 (12.1) | 768 (9.6) | 213 (20.6) |
| Something last year | 2054 (12.1) | 966 (12.1) | 917 (11.5) | 171 (16.5) |
| Something last month | 12,997 (76.5) | 6046 (75.8) | 6299 (78.9) | 652 (62.9) |
| Missing | 37 (0.2) | 12 (0.2) | 9 (0.1) | 16 (1.5) |
| Physical activity | ||||
| Activity time (min/week) | 376 (225–576) | 228 (150–301) | 578 (463–760) | 368 (214–543) |
| MET-hours/week | 28.3 (17.3–43.5) | 17.3 (11.4–22.8) | 43.7 (35.0–57.4) | 27.5 (16.1–41.3) |
| All Women | No Breast Cancer | Breast Cancer | ||||
|---|---|---|---|---|---|---|
| min/Week | MET-h/Week | min/Week | MET-h/Week | min/Week | MET-h/Week | |
| All | 377 (228–578) | 28.5 (17.3–43.7) | 380 (228–580) | 28.6 (17.3–43–8) | 353 (222–555) | 26.7 (17.0–41.9) |
| Menopausal status | ||||||
| Premenopausal | 371 (228–558) | 28.9 (17.8–43.4) | 372 (228–555) | 29.0 (17.7–43.2) | 368 (230–582) | 28.2 (18.7–44.6) |
| Perimenopausal | 367 (227–562) | 29.0 (17.8–42.8) | 373 (230–564) | 29.4 (17.9–43.4) | 328 (210–501) | 24.6 (15.4–39.1) |
| Postmenopausal | 383 (226–590) | 28.1 (17.0–43.9) | 385 (228–593) | 28.3 (17.0–44.1) | 348 (220–548) | 26.1 (16.3–41.0) |
| Waist circumference (cm) | ||||||
| Lowest (≤73.0) | 408 (253–605) | 31.0 (19.4–46.0) | 408 (253–605) | 31.0 (19.5–46.0) | 416 (248–601) | 31.0 (19.3–46.5) |
| Lower-middle (73.0–76.9) | 380 (233–576) | 29.0 (18.0–43.5) | 385 (235–585) | 29.4 (18.2–44.0) | 330 (213–509) | 24.9 (16.8–39.1) |
| Upper-middle (77.0–83.9) | 370 (222–569) | 28.0 (17.0–43.0) | 376 (223–575) | 28.0 (17.1–43.3) | 328 (206–508) | 24.4 (15.4–38.4) |
| Highest (≥84.0) | 343 (195–536) | 25.4 (14.6–40.2) | 343 (195–538) | 25.5 (14.4–40.2) | 338 (212–530) | 25.0 (15.7–40.3) |
| Body Mass Index (kg/m2) | ||||||
| Lower-normal (<23.0) | 393 (240–595) | 30.0 (18.7–45.0) | 393 (240–595) | 30.1 (18.7–45.2) | 378 (229–585) | 29.1 (18.3–44.1) |
| Upper-normal (23.0–24.9) | 390 (240–575) | 29.3 (18.4–43.8) | 393 (240–576) | 29.6 (18.4–43.9) | 354 (240–553) | 26.9 (18.0–41.9) |
| Overweight (25.0–29.9) | 375 (225–588) | 28.0 (17.0–44.0) | 379 (225–595) | 28.1 (17.0–44.5) | 343 (215–525) | 26.0 (16.3–40.8) |
| Obese (≥30.0) | 330 (183–522) | 24.2 (14.0–39.0) | 330 (181–520) | 24.3 (13.8–38.9) | 333 (203–535) | 23.7 (15.0–40.3) |
| Body fat (%) | ||||||
| Lowest (≤28.0) | 414 (255–607) | 31.7 (20.0–46.6) | 414 (255–609) | 31.8 (20.0–46.6) | 420 (240–603) | 31.0 (19.5–46.0) |
| Lower-middle (28.0–31.9) | 388 (240–585) | 29.3 (18.4–44.3) | 390 (240–588) | 29.5 (18.5–44.5) | 348 (231–563) | 27.1 (18.2–42.2) |
| Upper-middle (32.0–34.9) | 368 (225–564) | 27.5 (16.6–43.0) | 371 (225–570) | 27.8 (16.7–43.6) | 338 (213–500) | 25.5 (16.2–37.7) |
| Highest (≥35.0) | 340 (188–535) | 24.8 (14.0–40.0) | 340 (188–535) | 25.0 (14.0–40.0) | 332 (185–530) | 24.2 (14.8–40.6) |
| All Women | Low Physical Activity | High Physical Activity | Relative Risk | ||||
|---|---|---|---|---|---|---|---|
| Women/Events (n) | BCs/100,000 py | Women/Events (n) | BCs/100,000 py | Women/Events (n) | BCs/100,000 py | (%) | |
| All | 15,983/1302 | 387 | 7990/699 | 418 | 7993/603 | 356 | –14.9 |
| Menopausal status | |||||||
| Premenopausal | 4299/405 | 423 | 2110/205 | 435 | 2189/200 | 412 | –5.3 |
| Perimenopausal | 1134/109 | 424 | 553/64 | 516 | 581/45 | 339 | –34.4 |
| Postmenopausal | 10,550/788 | 366 | 5327/430 | 399 | 5223/358 | 332 | –16.7 |
| Waist circumference (cm) | |||||||
| Lowest (≤73.0) | 5626/453 | 373 | 2496/199 | 370 | 3130/254 | 376 | 1.6 |
| Lower-middle (73.0–76.9) | 2749/210 | 356 | 1353/124 | 429 | 1396/86 | 287 | –33.1 |
| Upper-middle (77.0–83.9) | 3728/316 | 403 | 1930/190 | 472 | 1798/126 | 331 | –30.0 |
| Highest (≥84.0) | 3880/323 | 414 | 2211/186 | 420 | 1669/137 | 405 | –3.6 |
| Body Mass Index (kg/m2) | |||||||
| Lower-normal (<23.0) | 4935/383 | 362 | 2295/184 | 375 | 2640/199 | 351 | –6.3 |
| Upper-normal (23.0–24.9) | 3660/288 | 369 | 1755/154 | 413 | 1905/134 | 328 | –20.6 |
| Overweight (25.0–29.9) | 5272/456 | 415 | 2696/257 | 460 | 2576/199 | 369 | –19.7 |
| Obese (≥30.0) | 2116/175 | 406 | 1244/104 | 416 | 872/71 | 393 | –5.6 |
| Body fat (%) | |||||||
| Lowest (≤28.0) | 4024/329 | 383 | 1722/144 | 391 | 2302/185 | 377 | –3.7 |
| Lower-middle (28.0–31.9) | 4791/381 | 371 | 2311/204 | 415 | 2480/177 | 331 | –20.2 |
| Upper-middle (32.0–34.9) | 3510/294 | 399 | 1843/173 | 449 | 1667/121 | 345 | –23.1 |
| Highest (≥35.0) | 3595/293 | 400 | 2082/174 | 414 | 1513/119 | 382 | –7.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boraka, Ö.; Klintman, M.; Rosendahl, A.H. Physical Activity and Long-Term Risk of Breast Cancer, Associations with Time in Life and Body Composition in the Prospective Malmö Diet and Cancer Study. Cancers 2022, 14, 1960. https://doi.org/10.3390/cancers14081960
Boraka Ö, Klintman M, Rosendahl AH. Physical Activity and Long-Term Risk of Breast Cancer, Associations with Time in Life and Body Composition in the Prospective Malmö Diet and Cancer Study. Cancers. 2022; 14(8):1960. https://doi.org/10.3390/cancers14081960
Chicago/Turabian StyleBoraka, Öykü, Marie Klintman, and Ann H. Rosendahl. 2022. "Physical Activity and Long-Term Risk of Breast Cancer, Associations with Time in Life and Body Composition in the Prospective Malmö Diet and Cancer Study" Cancers 14, no. 8: 1960. https://doi.org/10.3390/cancers14081960
APA StyleBoraka, Ö., Klintman, M., & Rosendahl, A. H. (2022). Physical Activity and Long-Term Risk of Breast Cancer, Associations with Time in Life and Body Composition in the Prospective Malmö Diet and Cancer Study. Cancers, 14(8), 1960. https://doi.org/10.3390/cancers14081960






