Management and Outcomes of Pancreatic Cancer in French Real-World Clinical Practice
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Data Set
- (0)
- No chemotherapy (n = 375)
- (1)
- gemcitabine without resection (Gem alone, n = 92),
- (2)
- gemcitabine + oxaliplatin or gemcitabine + nab-paclitaxel without surgical resection (Gem_Ox/Gem_Abra alone, n = 78); these were pooled as patients presented similar clinical features (mostly locally advanced or M1 disease) and similar characteristics,
- (3)
- leucovorine + 5-fluorouracil + irinotecan + oxaliplatin without surgical resection (FOLFIRINOX: FFX alone, n = 255),
- (4)
- FOLFIRINOX followed by surgical resection (FFX induction, n = 14),
- (5)
- gemcitabine (n = 63) or gemcitabine + capecitabine (n = 24) after surgical resection (Gem adjuvant, n = 87). In accordance with ASCO guidelines [9] stating that doublet therapy with gemcitabine and capecitabine or mono-therapy with gemcitabine alone can be offered in adjuvant settings; gemcitabine + capecitabine and gemcitabine alone were pooled.
2.3. Statistical Analysis
3. Results
3.1. Surgical Resection
3.2. Chemotherapy
3.3. Chemotherapy-Related Toxicities
3.4. Progression Free Survival (PFS)
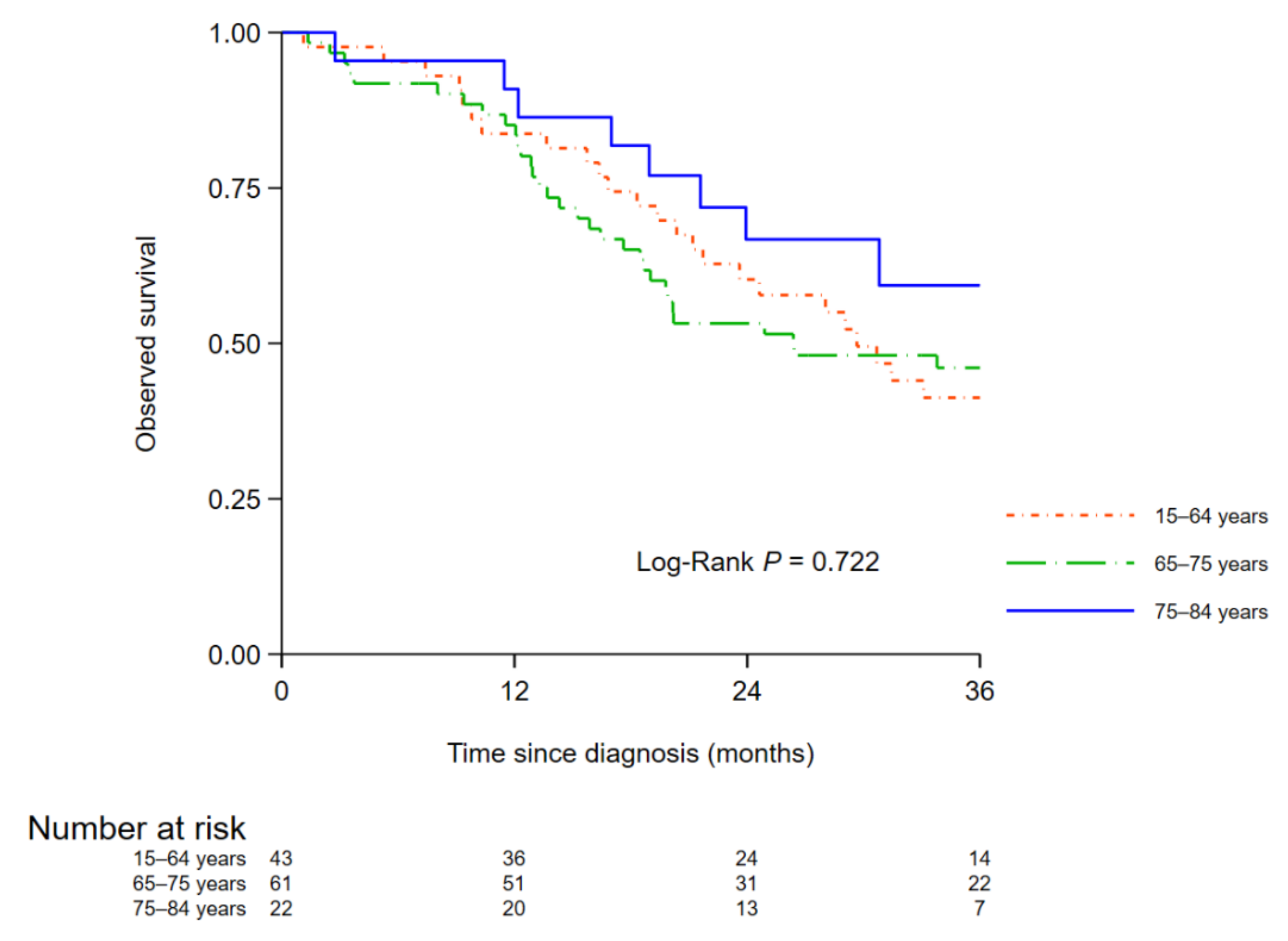
3.5. Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Dyba, T.; Randi, G.; Bettio, M.; Gavin, A.; Visser, O.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur. J. Cancer 2018, 103, 356–387. [Google Scholar] [PubMed]
- Bouvier, A.-M.; Uhry, Z.; Jooste, V.; Drouillard, A.; Remontet, L.; Launoy, G.; Leone, N.; Francim, T.F.N.O.C.R. Focus on an unusual rise in pancreatic cancer incidence in France. Int. J. Epidemiol. 2017, 46, 1764–1772. [Google Scholar] [PubMed] [Green Version]
- Neoptolemos, J.P.; Palmer, D.H.; Ghaneh, P.; Psarelli, E.E.; Valle, J.W.; Halloran, C.M.; Faluyi, O.; O’Reilly, D.A.; Cunningham, D.; Wadsley, J.; et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): A multicentre, open-label, randomised, phase 3 trial. Lancet 2017, 389, 1011–1024. [Google Scholar] [PubMed]
- Ducreux, M.; Cuhna, A.S.; Caramella, C.; Hollebecque, A.; Burtin, P.; Goéré, D.; Seufferlein, T.; Haustermans, K.; Van Laethem, J.L.; Conroy, T.; et al. Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26 (Suppl. S5), v56–v68. [Google Scholar]
- Von Hoff, D.D.; Ervin, T.; Arena, F.P.; Chiorean, E.G.; Infante, J.; Moore, M.; Seay, T.; Tjulandin, S.A.; Ma, W.W.; Saleh, M.N.; et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 2013, 369, 1691–1703. [Google Scholar]
- Guillaume, E.; Pornet, C.; Dejardin, O.; Launay, L.; Lillini, R.; Vercelli, M.; Marí-Dell’Olmo, M.; Fontelo, A.F.; Borrell, C.; Ribeiro, A.I.; et al. Development of a cross-cultural deprivation index in five European countries. J. Epidemiol. Community Health 2015, 70, 493–499. [Google Scholar]
- Pornet, C.; Delpierre, C.; Dejardin, O.; Grosclaude, P.; Launay, L.; Guittet, L.; Lang, T.; Launoy, G. Construction of an adaptable European transnational ecological deprivation index: The French version. J. Epidemiol. Community Health 2012, 66, 982–989. [Google Scholar]
- L-Hawary, M.M.; Francis, I.R.; Chari, S.T.; Fishman, E.; Hough, D.M.; Lu, D.S.; Macari, M.; Megibow, A.; Miller, F.H.; Mortele, K.J.; et al. Pancreatic Ductal Adenocarcinoma Radiology Reporting Template: Consensus Statement of the Society of Abdominal Radiology and the American Pancreatic Association. Gastroenterology 2014, 146, 291–304.e1. [Google Scholar]
- Khorana, A.A.; McKernin, S.E.; Berlin, J.; Hong, T.S.; Maitra, A.; Moravek, C.; Mumber, M.; Schulick, R.; Zeh, H.J.; Katz, M.H.G. Potentially Curable Pancreatic Adenocarcinoma: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2019, 37, 2082–2088. [Google Scholar]
- Estève, J.; Benhamou, E.; Croasdale, M.; Raymond, L. Relative survival and the estimation of net survival: Elements for further discussion. Stat. Med. 1990, 9, 529–538. [Google Scholar]
- Nelson, C.P.; Lambert, P.; Squire, I.B.; Jones, D.R. Flexible parametric models for relative survival, with application in coronary heart disease. Stat. Med. 2007, 26, 5486–5498. [Google Scholar] [PubMed] [Green Version]
- Uang, L.; Jansen, L.; Balavarca, Y.; Van Der Geest, L.; Lemmens, V.; Van Eycken, L.; De Schutter, H.; Johannesen, T.B.; Primic-Žakelj, M.; Zadnik, V.; et al. Nonsurgical therapies for resected and unresected pancreatic cancer in Europe and USA in 2003-2014: A large international population-based study. Int. J. Cancer 2018, 143, 3227–3239. [Google Scholar]
- Ilgrim, C.H.C.; Marvelde, L.T.; Stuart, E.; Croagh, D.; Deutscher, D.; Nikfarjam, M.; Lee, B.; Christophi, C. Population-based analysis of treatment patterns and outcomes for pancreas cancer in Victoria. ANZ J. Surg. 2020, 90, 1677–1682. [Google Scholar]
- Van Erning, F.N.; Mackay, T.M.; van der Geest, L.G.; Groot Koerkamp, B.; van Laarhoven, H.W.; Bonsing, B.A.; Wilmink, J.W.; van Santvoort, H.C.; de Vos-Geelen, J.; van Eijck, C.H.; et al. Association of the location of pancreatic ductal adenocarcinoma (head, body, tail) with tumor stage, treatment, and survival: A population-based analysis. Acta Oncol. 2018, 57, 1655–1662. [Google Scholar]
- Van Roest, M.H.; van der Aa, M.A.; van der Geest, L.G.; de Jong, K.P. The Impact of Socioeconomic Status, Surgical Resection and Type of Hospital on Survival in Patients with Pancreatic Cancer. A Population-Based Study in the Netherlands. PLoS ONE 2016, 11, e0166449. [Google Scholar]
- Huang, L.; Jansen, L.; Balavarca, Y.; Molina-Montes, E.; Babaei, M.; Van Der Geest, L.; Lemmens, V.; Van Eycken, L.; De Schutter, H.; Johannesen, T.B.; et al. Resection of pancreatic cancer in Europe and USA: An international large-scale study highlighting large variations. Gut 2019, 68, 130–139. [Google Scholar] [PubMed]
- Burmeister, E.A.; Waterhouse, M.; Jordan, S.J.; O’Connell, D.L.; Merrett, N.D.; Goldstein, D.; Wyld, D.; Beesley, V.; Gooden, H.; Janda, M.; et al. Determinants of survival and attempted resection in patients with non-metastatic pancreatic cancer: An Australian population-based study. Pancreatology 2016, 16, 873–881. [Google Scholar] [PubMed] [Green Version]
- Shaib, W.L.; Jones, J.S.; Goodman, M.; Sarmiento, J.M.; Maithel, S.K.; Cardona, K.; Kane, S.; Wu, C.; Alese, O.B.; El-Rayes, B.F. Evaluation of Treatment Patterns and Survival Outcomes in Elderly Pancreatic Cancer Patients: A Surveillance, Epidemiology, and End Results-Medicare Analysis. Oncologist 2018, 23, 704–711. [Google Scholar]
- Pamoukdjian, F.; Canoui-Poitrine, F.; Longelin-Lombard, C.; Aparicio, T.; Ganne, N.; Wind, P.; Martinez-Tapia, C.; Audureau, E.; Sebbane, G.; Zelek, L.; et al. Diagnostic performance of gait speed, G8 and G8 modified indices to screen for vulnerability in older cancer patients: The prospective PF-EC cohort study. Oncotarget 2017, 8, 50393–50402. [Google Scholar]
- Booth, C.M.; Mackillop, W.J. Translating new medical therapies into societal benefit: The role of population-based outcome studies. JAMA 2008, 300, 2177–2179. [Google Scholar]
- Conroy, T.; Hammel, P.; Hebbar, M.; Ben Abdelghani, M.; Wei, A.C.; Raoul, J.-L.; Choné, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [PubMed]
- Engberg, H.; Steding-Jessen, M.; Øster, I.; Jensen, J.W.; Fristrup, C.W.; Møller, H. Regional and socio-economic variation in survival after a pancreatic cancer diagnosis in Denmark. Dan. Med. J. 2020, 67, A08190438. [Google Scholar] [PubMed]

| Total | <65 y n (%) | 65–74 y n (%) | 75–84 y n (%) | ≥85 y n (%) | pa | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Men | 481 | 152 (68) | 160 (60) | 114 (45) | 55 (33) | |
| Women | 431 | 73 (32) | 108 (40) | 139 (55) | 111 (67) | <0.001 |
| Charlson index | ||||||
| 0–1 | 660 | 184 (82) | 192 (73) | 170 (68) | 114 (70) | |
| 2 | 146 | 28 (13) | 41 (16) | 49 (20) | 28 (17) | |
| 3+ | 95 | 12 (5) | 31 (12) | 32 (13) | 20 (12) | 0.019 |
| Performance Status | ||||||
| 0–1 | 588 | 179 (83) | 207 (82) | 150 (66) | 52 (38) | |
| 2 | 174 | 29 (13) | 36 (14) | 57 (25) | 52 (38) | |
| 3–4 | 72 | 7 (3) | 10 (4) | 22 (10) | 33 (24) | <0.001 |
| Deprivation | ||||||
| Quintile 1 | 168 | 38 (17) | 61 (23) | 48 (19) | 21 (13) | |
| Quintile 2 | 171 | 48 (22) | 57 (22) | 40 (16) | 26 (16) | |
| Quintile 3 | 154 | 37 (17) | 43 (16) | 39 (16) | 35 (21) | |
| Quintile 4 | 227 | 58 (26) | 60 (23) | 66 (26) | 43 (26) | |
| Quintile 5 | 179 | 41 (18) | 41 (16) | 58 (23) | 39 (24) | 0.104 |
| Clinical features b | ||||||
| M0 resectable tumor | 180 | 49 (22) | 70 (27) | 43 (18) | 18 (12) | |
| Locally advanced | 217 | 46 (21) | 53 (21) | 60 (25) | 58 (38) | |
| M1 | 476 | 127 (57) | 135 (52) | 137 (57) | 77 (50) | <0.001 |
| Treatment | ||||||
| Surgical resection without chemotherapy | 21 | 6 (3) | 12 (5) | 3 (1) | 0 (0) | |
| Best supportive care | 354 | 43 (19) | 49 (18) | 109 (44) | 153 (93) | |
| Chemotherapy | 528 | 173 (78) | 204 (77) | 139 (55) | 12 (7) | <0.001 |
| 1st line regimenc: | ||||||
| Gem alone | 92 | 8 (4) | 22 (8) | 51 (20) | 11 (7) | |
| Gem_Ox/Gem_Abra alone | 78 | 13 (6) | 26 (10) | 38 (15) | 1 (1) | |
| FFX alone | 255 | 116 (52) | 108 (41) | 31 (12) | 0 (0) | |
| FFX induction | 14 | 9 (4) | 5 (2) | 0 (0) | 0 (0) | |
| Gem adjuvant | 87 | 26 (13) | 42 (16) | 19 (8) | 0 (0) | <0.001 |
| Surgical Resection | Multivariate Analysis c | |||||
|---|---|---|---|---|---|---|
| Total | n (%) | pa | AOR | (95%CI) | p | |
| Age | ||||||
| <65 years | 49 | 43 (88) | 1 | |||
| 65–74 years | 70 | 61 (87) | 1.58 | (0.47–5.35) | ||
| 75–84 years | 43 | 22 (51) | 0.22 | (0.07–0.66) | <0.001 | |
| ≥85 years | 18 | 0 (0) | <0.001 | - | ||
| Sex | ||||||
| Men | 97 | 75 (77) | 1 | |||
| Women | 83 | 51 (61) | 0.021 | 0.58 | (0.24–1.39) | 0.221 |
| Charlson index | ||||||
| 0–1 | 125 | 88 (70) | - | |||
| 2 | 31 | 23 (74) | - | |||
| 3+ | 21 | 12 (57) | 0.390 | - | ||
| Deprivation | ||||||
| Quintile 1 | 29 | 19 (66) | - | |||
| Quintile 2 | 43 | 30 (70) | - | |||
| Quintile 3 | 27 | 18 (67) | - | |||
| Quintile 4 | 54 | 39 (72) | - | |||
| Quintile 5 | 24 | 17 (71) | 0.971 | - | ||
| Performance Status | ||||||
| 0–1 | 152 | 118 (78) | 1 | |||
| 2 | 17 | 3 (18) | 0.08 | (0.02–0.40) | ||
| 3–4 | 8 | 2 (25) | <0.001 b | 0.10 | (0.01–0.93) | <0.001 |
| Location | ||||||
| Head | 146 | 102 (70) | - | |||
| Other | 34 | 24 (71) | 0.934 | - | ||
| Chemotherapy | Multivariate Analysis c | |||||
|---|---|---|---|---|---|---|
| Total | n (%) | p a | AOR | (95%CI) | p | |
| Age | ||||||
| <65 years | 222 | 173 (78) | 1 | |||
| 65–74 years | 265 | 204 (77) | 1.10 | (0.67–1.81) | ||
| 75–84 years | 251 | 139 (55) | 0.46 | (0.29–0.75) | ||
| ≥85 years | 165 | 12 (7) | <0.001 | 0.03 | (0.01–0.07) | <0.001 |
| Sex | ||||||
| Men | 475 | 292 (61) | 1 | |||
| Women | 428 | 236 (55) | 0.054 | 1.38 | (0.94–2.03) | 0.103 |
| Charlson index | ||||||
| 0–1 | 657 | 409 (62) | 1 | |||
| 2 | 145 | 81 (56) | 1.27 | (0.75–2.13) | ||
| 3+ | 95 | 36 (38) | <0.001 | 0.47 | (0.26–0.84) | 0.016 |
| Performance Status | ||||||
| 0–1 | 585 | 440 (75) | 1 | |||
| 2 | 174 | 64 (37) | 0.30 | (0.19–0.46) | ||
| 3–4 | 72 | 8 (11) | <0.001 | 0.07 | (0.03–0.15) | <0.001 |
| Deprivation | ||||||
| Quintile 1 | 168 | 105 (63) | 1 | (0.80–2.72) | ||
| Quintile 2 | 170 | 119 (70) | 1.47 | (0.80–2.72) | ||
| Quintile 3 | 154 | 88 (57) | 1.02 | (0.55–1.89) | ||
| Quintile 4 | 221 | 124 (56) | 0.79 | (0.46–1.38) | ||
| Quintile 5 | 177 | 83 (47) | <0.001 | 0.59 | (0.33–1.05) | 0.033 |
| Clinical Feature b | ||||||
| M0 resectable tumor | 176 | 122 (69) | 1 | |||
| Locally advanced | 216 | 127 (59) | 1.76 | (0.98–3.15) | ||
| M1 | 474 | 265 (56) | 0.008 | 1.01 | (0.63–1.63) | 0.055 |
| Severe Toxicity | Multivariate Analysis c | |||||
|---|---|---|---|---|---|---|
| Total | n (%) | pa | AOR | (95%CI) | p | |
| Age | ||||||
| <65 years | 173 | 51 (29) | 1 | |||
| 65–74 years | 204 | 58 (28) | 1.17 | (0.73–1.87) | ||
| 75–84 years | 139 | 52 (37) | 2.59 | (1.44–4.63) | ||
| ≥85 years | 12 | 8 (67) | 0.017 | 12.40 | (3.05–50.44) | <0.001 |
| Sex | ||||||
| Men | 292 | 81 (28) | 1 | |||
| Women | 236 | 88 (37) | 0.019 | 1.42 | (0.96–2.12) | 0.082 |
| Charlson index | ||||||
| 0–1 | 409 | 141 (34) | - | |||
| 2 | 81 | 21 (26) | - | |||
| 3+ | 36 | 7 (19) | 0.077 | - | ||
| Performance Status | ||||||
| 0–1 | 440 | 141 (32) | - | |||
| 2 | 64 | 23 (36) | - | |||
| 3–4 | 8 | 2 (25) | 0.744 | - | ||
| Deprivation | ||||||
| Quintile 1 | 105 | 30 (29) | - | |||
| Quintile 2 | 119 | 32 (27) | - | |||
| Quintile 3 | 88 | 31 (35) | - | |||
| Quintile 4 | 124 | 42 (34) | - | |||
| Quintile 5 | 83 | 33 (40) | 0.303 | - | ||
| 1st line regimen b | ||||||
| Gem alone | 92 | 24 (26) | 1 | |||
| Gem_Ox/Gem_Abra alone | 78 | 26 (33) | 2.24 | (1.07–4.68) | ||
| FFX alone or induction | 269 | 107 (40) | 4.31 | (2.17–8.53) | ||
| Gem adjuvant | 87 | 12 (14) | <0.001 | 0.92 | (0.39–2.15) | <0.001 |
| 6 Months | 1 Year | 3 Years | p | AHR (95% CI) | p | |
|---|---|---|---|---|---|---|
| Age | ||||||
| <65 years | 69 (62–74) | 47 (40–53) | 12 (8–17) | 1 | ||
| 65–74 years | 70 (64–75) | 53 (46–59) | 17 (13–22) | 0.9 (0.74–1.09) | ||
| 75–84 years | 48 (42–54) | 30 (24–36) | 10 (7–15) | 1.31 (1.07–1.61) | ||
| ≥85 years | 27 (20–34) | 12 (7–18) | - | <0.001 | 2.19 (1.70–2.81) | <0.001 |
| Sex | ||||||
| Men | 58 (53–62) | 40 (36–45) | 13 (10–16) | 1 | ||
| Women | 53 (48–58) | 34 (29–39) | 9 (6–12) | 0.065 | 0.97 (0.84–1.13) | 0.706 |
| Charlson index | ||||||
| 0–1 | 59 (55–63) | 40 (36–43) | 10 (8–13) | 1 | ||
| 2 | 48 (40–56) | 36 (28–44) | 12 (7–19) | 1.06 (0.87–1.30) | ||
| 3+ | 44 (34–54) | 26 (18–35) | 9 (4–16) | 0.029 | 1.28 (1.00–1.63) | 0.166 |
| Performance Status | ||||||
| 0–1 | 71 (67–74) | 50 (45–54) | 16 (13–19) | 1 | ||
| 2 | 36 (29–43) | 18 (13–24) | 2 (1–6) | 1.7 (1.41–2.06) | ||
| 3–4 | 16 (8–25) | 9 (4–17) | 0 - | <0.001 | 2.2 (1.65–2.92) | <0.001 |
| Deprivation | ||||||
| Quintile 1 | 58 (50–65) | 38 (31–46) | 16 (10–22) | 1 | ||
| Quintile 2 | 66 (58–72) | 49 (41–56) | 11 (7–17) | 0.96 (0.76–1.21) | ||
| Quintile 3 | 52 (44–60) | 35 (27–42) | 6 (3–11) | 1.09 (0.86–1.38) | ||
| Quintile 4 | 53 (47–60) | 36 (30–43) | 14 (9–19) | 1.16 (0.93–1.45) | ||
| Quintile 5 | 48 (40–55) | 28 (21–35) | 5 (2–10) | 0.01 | 1.06 (0.84–1.33) | 0.465 |
| Clinical features b | ||||||
| M0 resectable tumor | 84 (77–88) | 69 (62–76) | 35 (28–42) | 1 | ||
| Locally advanced | 66 (59–72) | 48 (41–55) | 8 (5–13) | 1.43 (1.13–1.80) | ||
| M1 | 41 (37–46) | 21 (17–25) | 3 (2–5) | <0.001 | 3.31 (2.69–4.09) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jooste, V.; Bengrine-Lefevre, L.; Manfredi, S.; Quipourt, V.; Grosclaude, P.; Facy, O.; Lepage, C.; Ghiringhelli, F.; Bouvier, A.-M. Management and Outcomes of Pancreatic Cancer in French Real-World Clinical Practice. Cancers 2022, 14, 1675. https://doi.org/10.3390/cancers14071675
Jooste V, Bengrine-Lefevre L, Manfredi S, Quipourt V, Grosclaude P, Facy O, Lepage C, Ghiringhelli F, Bouvier A-M. Management and Outcomes of Pancreatic Cancer in French Real-World Clinical Practice. Cancers. 2022; 14(7):1675. https://doi.org/10.3390/cancers14071675
Chicago/Turabian StyleJooste, Valérie, Leila Bengrine-Lefevre, Sylvain Manfredi, Valérie Quipourt, Pascale Grosclaude, Olivier Facy, Côme Lepage, François Ghiringhelli, and Anne-Marie Bouvier. 2022. "Management and Outcomes of Pancreatic Cancer in French Real-World Clinical Practice" Cancers 14, no. 7: 1675. https://doi.org/10.3390/cancers14071675
APA StyleJooste, V., Bengrine-Lefevre, L., Manfredi, S., Quipourt, V., Grosclaude, P., Facy, O., Lepage, C., Ghiringhelli, F., & Bouvier, A.-M. (2022). Management and Outcomes of Pancreatic Cancer in French Real-World Clinical Practice. Cancers, 14(7), 1675. https://doi.org/10.3390/cancers14071675








