Transient Enlargement in Meningiomas Treated with Stereotactic Radiotherapy
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Radiation Therapy
2.3. Follow-Up and Imaging
2.4. Volumetric Analysis
2.5. Statistical Analysis
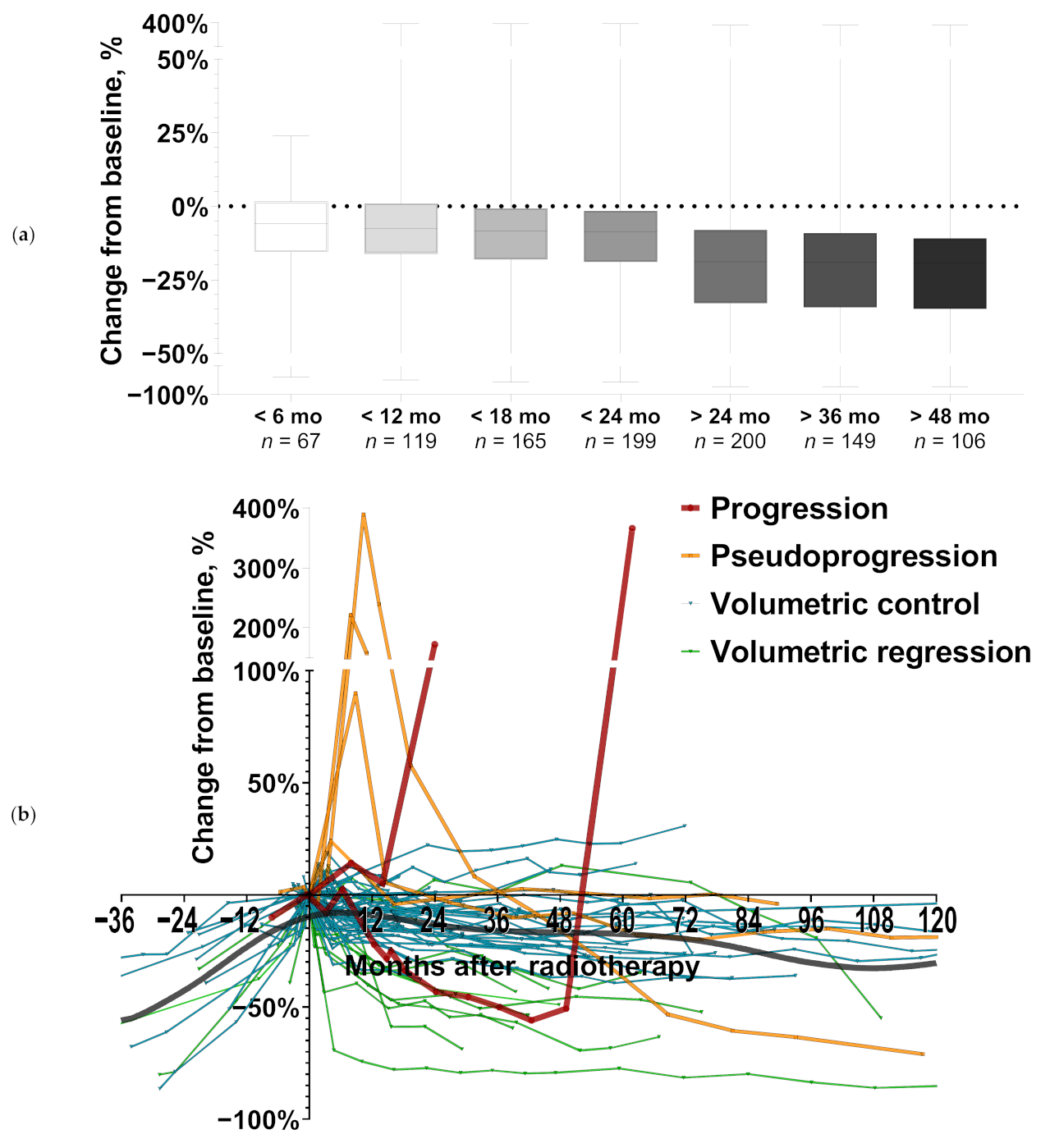
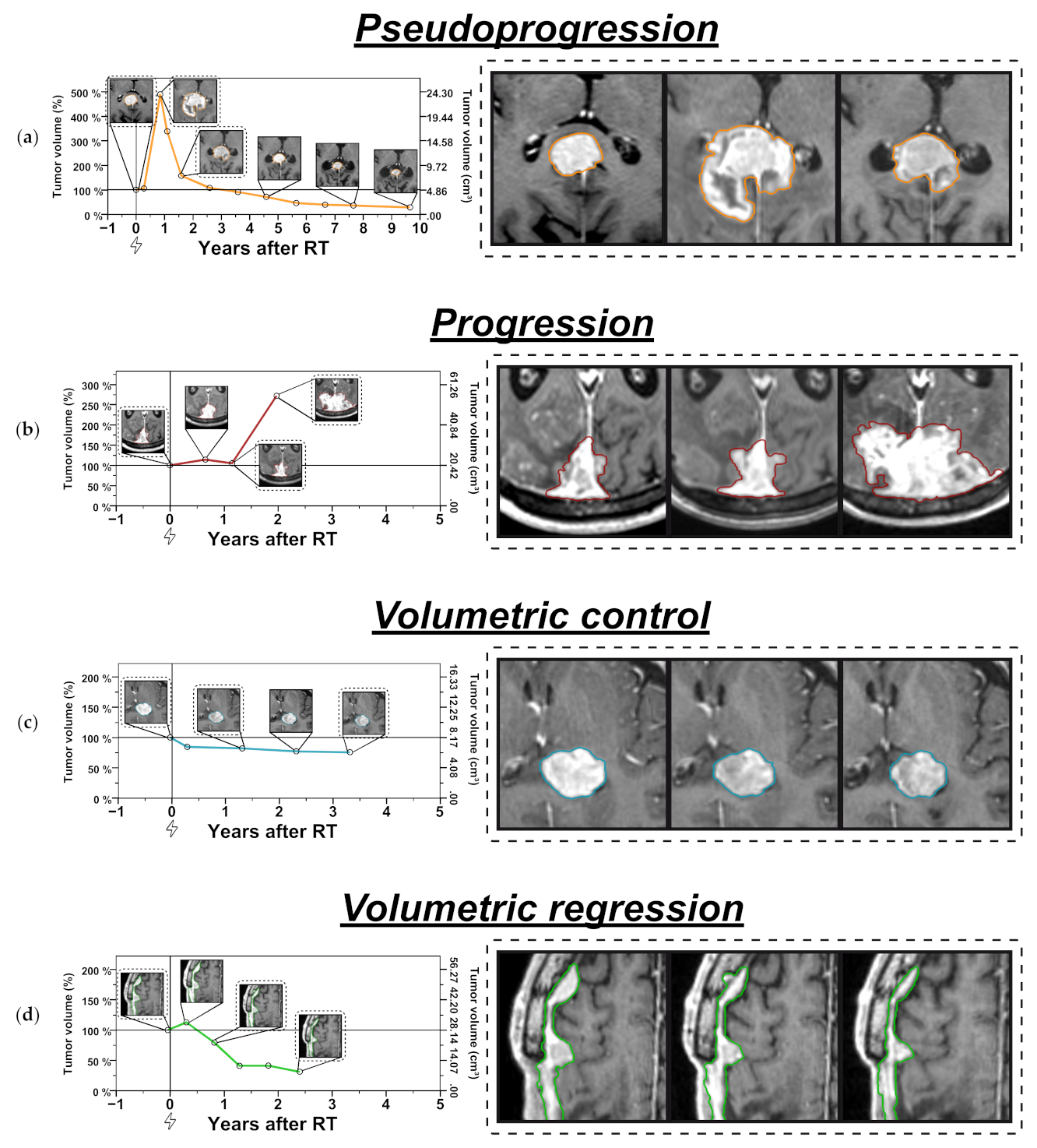
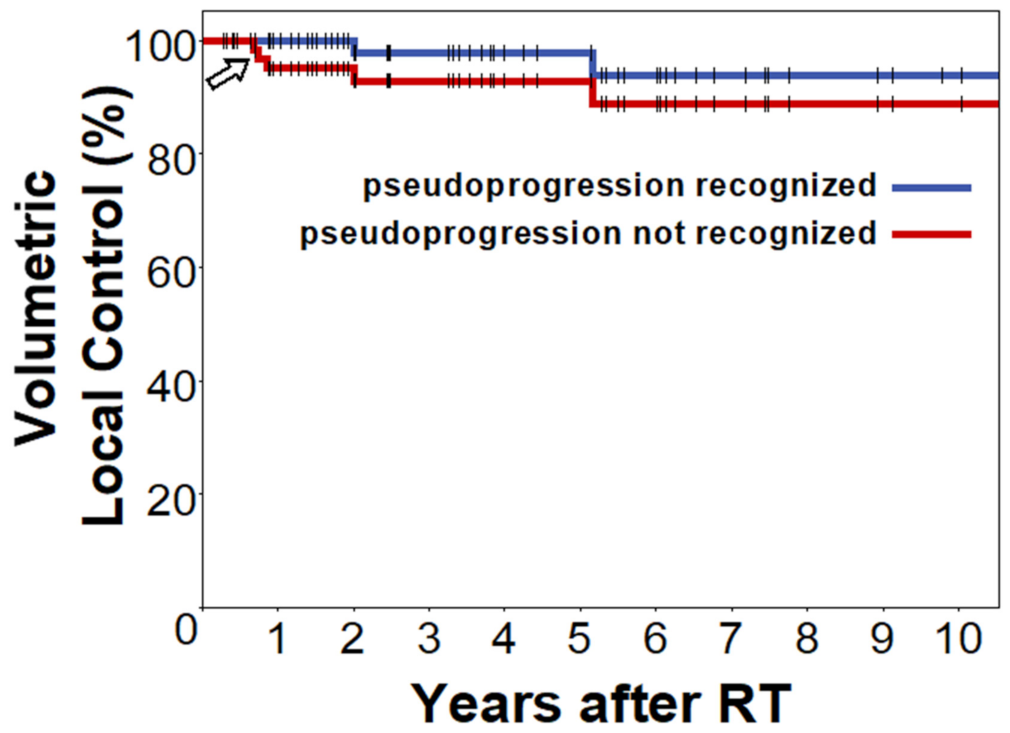
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Cioffi, G.; Gittleman, H.; Patil, N.; Waite, K.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016. Neuro-Oncology 2019, 21, v1–v100. [Google Scholar] [CrossRef] [PubMed]
- van Alkemade, H.; de Leau, M.; Dieleman, E.M.T.; Kardaun, J.W.P.F.; van Os, R.; Vandertop, W.P.; van Furth, W.R.; Stalpers, L.J.A. Impaired survival and long-term neurological problems in benign meningioma. Neuro-Oncology 2012, 14, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Nassiri, F.; Price, B.; Shehab, A.; Au, K.; Cusimano, M.D.; Jenkinson, M.D.; Jungk, C.; Mansouri, A.; Santarius, T.; Suppiah, S.; et al. Life after surgical resection of a meningioma: A prospective cross-sectional study evaluating health-related quality of life. Neuro-Oncology 2019, 21, i32–i43. [Google Scholar] [CrossRef] [Green Version]
- Pettersson-Segerlind, J.; Orrego, A.; Lönn, S.; Mathiesen, T. Long-term 25-year follow-up of surgically treated parasagittal meningiomas. World Neurosurg. 2011, 76, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Goldbrunner, R.; Minniti, G.; Preusser, M.; Jenkinson, M.D.; Sallabanda, K.; Houdart, E.; von Deimling, A.; Stavrinou, P.; Lefranc, F.; Lund-Johansen, M.; et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol. 2016, 17, e383–e391. [Google Scholar] [CrossRef] [Green Version]
- Weber, D.C.; Ares, C.; Villa, S.; Peerdeman, S.M.; Renard, L.; Baumert, B.G.; Lucas, A.; Veninga, T.; Pica, A.; Jefferies, S.; et al. Adjuvant postoperative high-dose radiotherapy for atypical and malignant meningioma: A phase-II parallel non-randomized and observation study (EORTC 22042-26042). Radiother. Oncol. 2018, 128, 260–265. [Google Scholar] [CrossRef] [Green Version]
- Rogers, L.; Zhang, P.; Vogelbaum, M.A.; Perry, A.; Ashby, L.S.; Modi, J.M.; Alleman, A.M.; Galvin, J.; Brachman, D.; Jenrette, J.M.; et al. Intermediate-risk meningioma: Initial outcomes from NRG Oncology RTOG 0539. J. Neurosurg. 2018, 129, 35–47. [Google Scholar] [CrossRef] [Green Version]
- Jenkinson, M.D.; Javadpour, M.; Haylock, B.J.; Young, B.; Gillard, H.; Vinten, J.; Bulbeck, H.; Das, K.; Farrell, M.; Looby, S.; et al. The ROAM/EORTC-1308 trial: Radiation versus Observation following surgical resection of Atypical Meningioma: Study protocol for a randomised controlled trial. Trials 2015, 16, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Huang, R.Y.; Bi, W.L.; Weller, M.; Kaley, T.; Blakeley, J.; Dunn, I.; Galanis, E.; Preusser, M.; McDermott, M.; Rogers, L.; et al. Proposed response assessment and endpoints for meningioma clinical trials: Report from the Response Assessment in Neuro-Oncology Working Group. Neuro-Oncology 2019, 21, 26–36. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Sade, B. The Novel “CLASS” Algorithmic Scale for Patient Selection in Meningioma Surgery. In Meningiomas; Lee, J.H., Ed.; Springer: London, UK, 2009; pp. 217–221. [Google Scholar]
- Koca, S.; Distel, L.; Lubgan, D.; Weissmann, T.; Lambrecht, U.; Lang-Welzenbach, M.; Eyupoglu, I.; Bischoff, B.; Buchfelder, M.; Semrau, S.; et al. Time course of pain response and toxicity after whole-nerve-encompassing LINAC-based stereotactic radiosurgery for trigeminal neuralgia-a prospective observational study. Strahlenther. Onkol. 2019, 195, 745–755. [Google Scholar] [CrossRef]
- Putz, F.; Muller, J.; Wimmer, C.; Goerig, N.; Knippen, S.; Iro, H.; Grundtner, P.; Eyupoglu, I.; Rossler, K.; Semrau, S.; et al. Stereotactic radiotherapy of vestibular schwannoma: Hearing preservation, vestibular function, and local control following primary and salvage radiotherapy. Strahlenther. Onkol. 2017, 193, 200–212. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, D.; Blanck, O.; Gauer, T.; Fix, M.K.; Brunner, T.B.; Fleckenstein, J.; Loutfi-Krauss, B.; Manser, P.; Werner, R.; Wilhelm, M.L.; et al. Technological quality requirements for stereotactic radiotherapy: Expert review group consensus from the DGMP Working Group for Physics and Technology in Stereotactic Radiotherapy. Strahlenther. Onkol. 2020, 196, 421–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinter, C.; Lasso, A.; Wang, A.; Jaffray, D.; Fichtinger, G. SlicerRT: Radiation therapy research toolkit for 3D Slicer. Med. Phys. 2012, 39, 6332–6338. [Google Scholar] [CrossRef]
- Weissmann, T.; Lettmaier, S.; Roesch, J.; Mengling, V.; Bert, C.; Iro, H.; Hornung, J.; Janka, R.; Semrau, S.; Fietkau, R.; et al. Paragangliomas of the Head and Neck: Local Control and Functional Outcome Following Fractionated Stereotactic Radiotherapy. Am. J. Clin. Oncol. 2019, 42, 818–823. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Kolesov, I.; Gao, Y.; Kikinis, R.; Tannenbaum, A. An Effective Interactive Medical Image Segmentation Method using Fast GrowCut. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention. Workshop on Interactive Methods, Boston, MA, USA, 14–18 September 2014. [Google Scholar]
- Zhao, B.; Tan, Y.; Tsai, W.Y.; Qi, J.; Xie, C.; Lu, L.; Schwartz, L.H. Reproducibility of radiomics for deciphering tumor phenotype with imaging. Sci. Rep. 2016, 6, 23428. [Google Scholar] [CrossRef] [Green Version]
- Balagurunathan, Y.; Kumar, V.; Gu, Y.; Kim, J.; Wang, H.; Liu, Y.; Goldgof, D.B.; Hall, L.O.; Korn, R.; Zhao, B.; et al. Test-retest reproducibility analysis of lung CT image features. J. Digit. Imaging 2014, 27, 805–823. [Google Scholar] [CrossRef] [Green Version]
- Odland, A.; Server, A.; Saxhaug, C.; Breivik, B.; Groote, R.; Vardal, J.; Larsson, C.; Bjørnerud, A. Volumetric glioma quantification: Comparison of manual and semi-automatic tumor segmentation for the quantification of tumor growth. Acta Radiol. 2015, 56, 1396–1403. [Google Scholar] [CrossRef]
- Yang, D.Y.; Sheehan, J.; Liu, Y.S.; ChangLai, S.P.; Pan, H.C.; Chen, C.J.; Chou, M.C. Analysis of factors associated with volumetric data errors in gamma knife radiosurgery. Stereotact. Funct. Neurosurg. 2009, 87, 1–7. [Google Scholar] [CrossRef]
- van de Langenberg, R.; de Bondt, B.J.; Nelemans, P.J.; Baumert, B.G.; Stokroos, R.J. Follow-up assessment of vestibular schwannomas: Volume quantification versus two-dimensional measurements. Neuroradiology 2009, 51, 517–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brandes, A.A.; Franceschi, E.; Tosoni, A.; Blatt, V.; Pession, A.; Tallini, G.; Bertorelle, R.; Bartolini, S.; Calbucci, F.; Andreoli, A.; et al. MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J. Clin. Oncol. 2008, 26, 2192–2197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, P.Y.; Macdonald, D.R.; Reardon, D.A.; Cloughesy, T.F.; Sorensen, A.G.; Galanis, E.; Degroot, J.; Wick, W.; Gilbert, M.R.; Lassman, A.B.; et al. Updated response assessment criteria for high-grade gliomas: Response assessment in neuro-oncology working group. J. Clin. Oncol. 2010, 28, 1963–1972. [Google Scholar] [CrossRef] [PubMed]
- Back, M.; Jayamanne, D.; Brazier, D.; Newey, A.; Bailey, D.; Schembri, G.; Hsiao, E.; Khasraw, M.; Wong, M.; Kastelan, M.; et al. Pattern of failure in anaplastic glioma patients with an IDH1/2 mutation. Strahlenther. Onkol. 2020, 196, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Meijer, O.W.; Weijmans, E.J.; Knol, D.L.; Slotman, B.J.; Barkhof, F.; Vandertop, W.P.; Castelijns, J.A. Tumor-volume changes after radiosurgery for vestibular schwannoma: Implications for follow-up MR imaging protocol. AJNR Am. J. Neuroradiol. 2008, 29, 906–910. [Google Scholar] [CrossRef] [Green Version]
- Aoyama, H.; Onodera, S.; Takeichi, N.; Onimaru, R.; Terasaka, S.; Sawamura, Y.; Shirato, H. Symptomatic outcomes in relation to tumor expansion after fractionated stereotactic radiation therapy for vestibular schwannomas: Single-institutional long-term experience. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 329–334. [Google Scholar] [CrossRef]
- Miyatake, S.; Kawabata, S.; Nonoguchi, N.; Yokoyama, K.; Kuroiwa, T.; Matsui, H.; Ono, K. Pseudoprogression in boron neutron capture therapy for malignant gliomas and meningiomas. Neuro-Oncology 2009, 11, 430–436. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.; Lee, D.H.; Kim Rn, H.J.; Cho, Y.H.; Kim, J.H.; Kwon, D.H. Analysis of the results of recurrent intracranial meningiomas treated with re-radiosurgery. Clin. Neurol. Neurosurg. 2017, 153, 93–101. [Google Scholar] [CrossRef]
- Fega, K.R.; Fletcher, G.P.; Waddle, M.R.; Peterson, J.L.; Ashman, J.B.; Barrs, D.M.; Bendok, B.R.; Patel, N.P.; Porter, A.B.; Vora, S.A. Analysis of MRI Volumetric Changes After Hypofractionated Stereotactic Radiation Therapy for Benign Intracranial Neoplasms. Adv. Radiat. Oncol. 2019, 4, 43–49. [Google Scholar] [CrossRef] [Green Version]
- Lee, N.K.; Kim, C.Y.; Yoon, W.S.; Chung, Y.G.; Lee, N.J. Quantitative analysis of tumor volume reduction after three-dimensional conformal radiation therapy for intracranial meningiomas. J. Neuro-Oncol. 2015, 121, 195–199. [Google Scholar] [CrossRef]
- Sadik, Z.H.A.; Lie, S.T.; Leenstra, S.; Hanssens, P.E.J. Volumetric changes and clinical outcome for petroclival meningiomas after primary treatment with Gamma Knife radiosurgery. J. Neurosurg. 2018, 129, 1623–1629. [Google Scholar] [CrossRef]
- Speckter, H.; Bido, J.; Hernandez, G.; Rivera, D.; Suazo, L.; Valenzuela, S.; Miches, I.; Oviedo, J.; Gonzalez, C.; Stoeter, P. Pretreatment texture analysis of routine MR images and shape analysis of the diffusion tensor for prediction of volumetric response after radiosurgery for meningioma. J. Neurosurg. 2018, 129, 31–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrison, G.; Kano, H.; Lunsford, L.D.; Flickinger, J.C.; Kondziolka, D. Quantitative tumor volumetric responses after Gamma Knife radiosurgery for meningiomas. J. Neurosurg. 2016, 124, 146–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Astner, S.T.; Theodorou, M.; Dobrei-Ciuchendea, M.; Auer, F.; Kopp, C.; Molls, M.; Grosu, A.L. Tumor shrinkage assessed by volumetric MRI in the long-term follow-up after stereotactic radiotherapy of meningiomas. Strahlenther. Onkol. 2010, 186, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Henzel, M.; Gross, M.W.; Hamm, K.; Surber, G.; Kleinert, G.; Failing, T.; Strassmann, G.; Engenhart-Cabillic, R. Significant tumor volume reduction of meningiomas after stereotactic radiotherapy: Results of a prospective multicenter study. Neurosurgery 2006, 59, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- Fuks, Z.; Kolesnick, R. Engaging the vascular component of the tumor response. Cancer Cell 2005, 8, 89–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thiagarajan, A.; Yamada, Y. Radiobiology and radiotherapy of brain metastases. Clin. Exp. Metastasis 2017, 34, 411–419. [Google Scholar] [CrossRef] [PubMed]
| Meningioma Characteristic | Total Cohort (N = 69) |
|---|---|
| Patient age, years | |
| Median (IQR) | 63.0 (49.5–72.0) |
| Mean (range) | 61.0 (36–86) |
| Sex, n (%) | |
| Male | 17 (25%) |
| Female | 52 (75%) |
| Primary indication for radiotherapy, n (%) | |
| Tumor progression/recurrence on imaging | 33 (48%) |
| Tumor-related signs/symptoms | 28 (41%) |
| Residual tumor after preceding surgery | 5 (7%) |
| Patient request | 3 (4%) |
| Primary diagnosis vs. recurrence, n (%) | |
| Primary diagnosis | 57 (83%) |
| Recurrence after prior resection | 12 (17%) |
| Preceding surgery, n (%) | |
| Preceding Simpson grade IV/V resection | 5 (7%) |
| No preceding resection | 64 (93%) |
| Histology, n (%) | |
| WHO I | 10 (15%) |
| WHO II | 7 (10%) |
| Imaging diagnosis of low-grade meningioma | 52 (75%) |
| Meningioma CLASS score group, n (%) | |
| Group I | 3 (4%) |
| Group II | 23 (33%) |
| Group III | 43 (62%) |
| Location, n (%) | |
| Parasellar | 21 (30%) |
| Convexity | 18 (26%) |
| Tentorial | 14 (20%) |
| Olfactory | 5 (7%) |
| Sphenoid Wing | 5 (7%) |
| Falcine | 2 (3 %) |
| Parasagittal | 2 (3 %) |
| Foramen magnum | 1 (1%) |
| Ventricular | 1 (1%) |
| Pre-RT baseline volume, cm3 | |
| Median (IQR) | 4.7 (1.3–9.0) |
| Mean (range) | 7.7 (0.2–43.1) |
| RT fractionation scheme, n (%) | |
| Conventional fractionation in single doses of 1.8 Gy | 57 (83%) |
| 10 × 4.0 Gy | 1 (1%) |
| 7 × 5.0 Gy | 1 (1%) |
| 1 × 13.0 Gy | 5 (7%) |
| 1 × 14.0 Gy | 5 (7%) |
| Conventional fractionation total dose, Gy | |
| Median (IQR) | 54.0 (54.0–54.0) |
| Mean (range) | 53.8 (50.4–59.4) |
| Number of post-RT imaging studies excluding baseline | |
| Median (IQR) | 5 (3.0–8.0) |
| Mean (range) | 5.8 (1.0–15.0) |
| Parameter | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR | p-Value | OR | p-Value | |
| SRS/hypofractionation vs. conventional fractionation | 18.67 | 0.016 | 22.53 | 0.041 |
| Baseline tumor volume, ≥4.7 vs. <4.7 cm3 | 0.29 | 0.289 | 1.40 | 0.831 |
| WHO grade (atypical vs. benign) | 3.28 | 0.335 | Not included because of p ≥ 0.300 | |
| Patient age, ≥63 vs. <63 years | 0.91 | 0.929 | Not included because of p ≥ 0.300 | |
| Recurrence vs. primary diagnosis | 1.64 | 0.682 | Not included because of p ≥ 0.300 | |
| Patient sex (male vs. female) | 1.02 | 0.986 | Not included because of p ≥ 0.300 | |
| Preceding surgery | 0.00 | 0.999 | Not included because of p ≥ 0.300 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maksoud, Z.; Schmidt, M.A.; Huang, Y.; Rutzner, S.; Mansoorian, S.; Weissmann, T.; Bert, C.; Distel, L.; Semrau, S.; Lettmaier, S.; et al. Transient Enlargement in Meningiomas Treated with Stereotactic Radiotherapy. Cancers 2022, 14, 1547. https://doi.org/10.3390/cancers14061547
Maksoud Z, Schmidt MA, Huang Y, Rutzner S, Mansoorian S, Weissmann T, Bert C, Distel L, Semrau S, Lettmaier S, et al. Transient Enlargement in Meningiomas Treated with Stereotactic Radiotherapy. Cancers. 2022; 14(6):1547. https://doi.org/10.3390/cancers14061547
Chicago/Turabian StyleMaksoud, Ziad, Manuel Alexander Schmidt, Yixing Huang, Sandra Rutzner, Sina Mansoorian, Thomas Weissmann, Christoph Bert, Luitpold Distel, Sabine Semrau, Sebastian Lettmaier, and et al. 2022. "Transient Enlargement in Meningiomas Treated with Stereotactic Radiotherapy" Cancers 14, no. 6: 1547. https://doi.org/10.3390/cancers14061547
APA StyleMaksoud, Z., Schmidt, M. A., Huang, Y., Rutzner, S., Mansoorian, S., Weissmann, T., Bert, C., Distel, L., Semrau, S., Lettmaier, S., Eyüpoglu, I., Fietkau, R., & Putz, F. (2022). Transient Enlargement in Meningiomas Treated with Stereotactic Radiotherapy. Cancers, 14(6), 1547. https://doi.org/10.3390/cancers14061547








