[18F]Fluciclovine PET/CT Improves the Clinical Management of Early Recurrence Prostate Cancer Patients
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Population Characteristics
2.2. Imaging Protocol and Analysis
2.3. Data Analysis
2.3.1. [18F]Fluciclovine PET/CT Detection Rate
2.3.2. Follow-Up Data Analysis
- true positive (TP), patients with evidence of [18F]Fluciclovine PET/CT finding(s), confirmed by post-PET anatomical imaging or biopsy examination, and/or biochemical response documented by PSA levels decreasing or stable after therapy or PSA increasing under clinical surveillance;
- true negative (TN), patients with no evidence of [18F]Fluciclovine PET/CT finding(s), confirmed on post-PET anatomical imaging, and/or PSA decreasing without any therapy;
- false positive (FP), patients with evidence of [18F]Fluciclovine PET/CT finding(s), not confirmed by post-PET anatomical imaging, and PSA decreasing without any therapy;
- false negative (FN), patients with no evidence of [18F]Fluciclovine PET/CT finding(s) and positive findings on post-PET anatomical imaging, and/or PSA decreasing after therapy.
2.3.3. [18F]Fluciclovine PET/CT Semiquantitative Analysis
2.3.4. Subpopulation Analysis
2.4. Statistical Analysis
3. Results
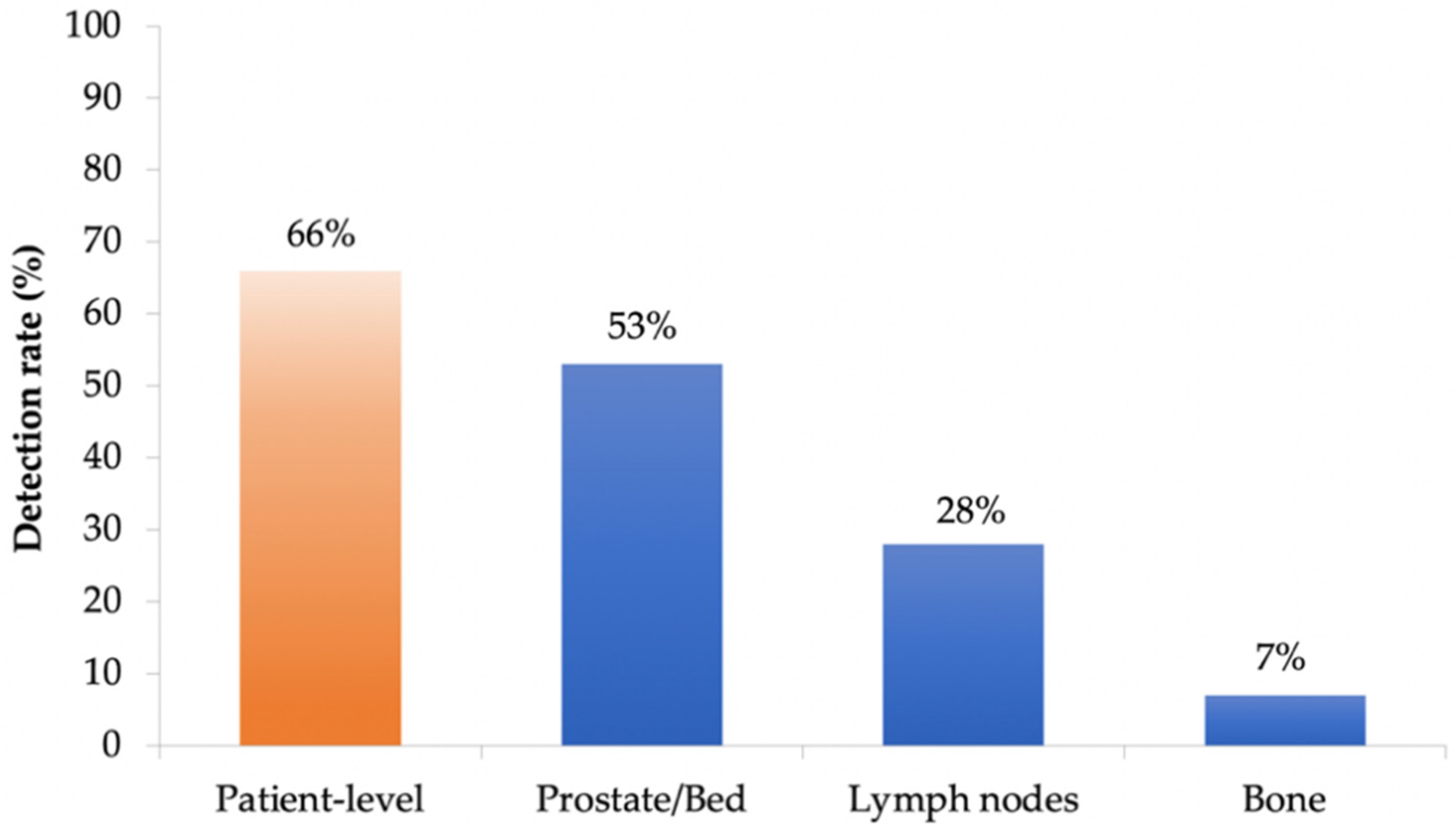
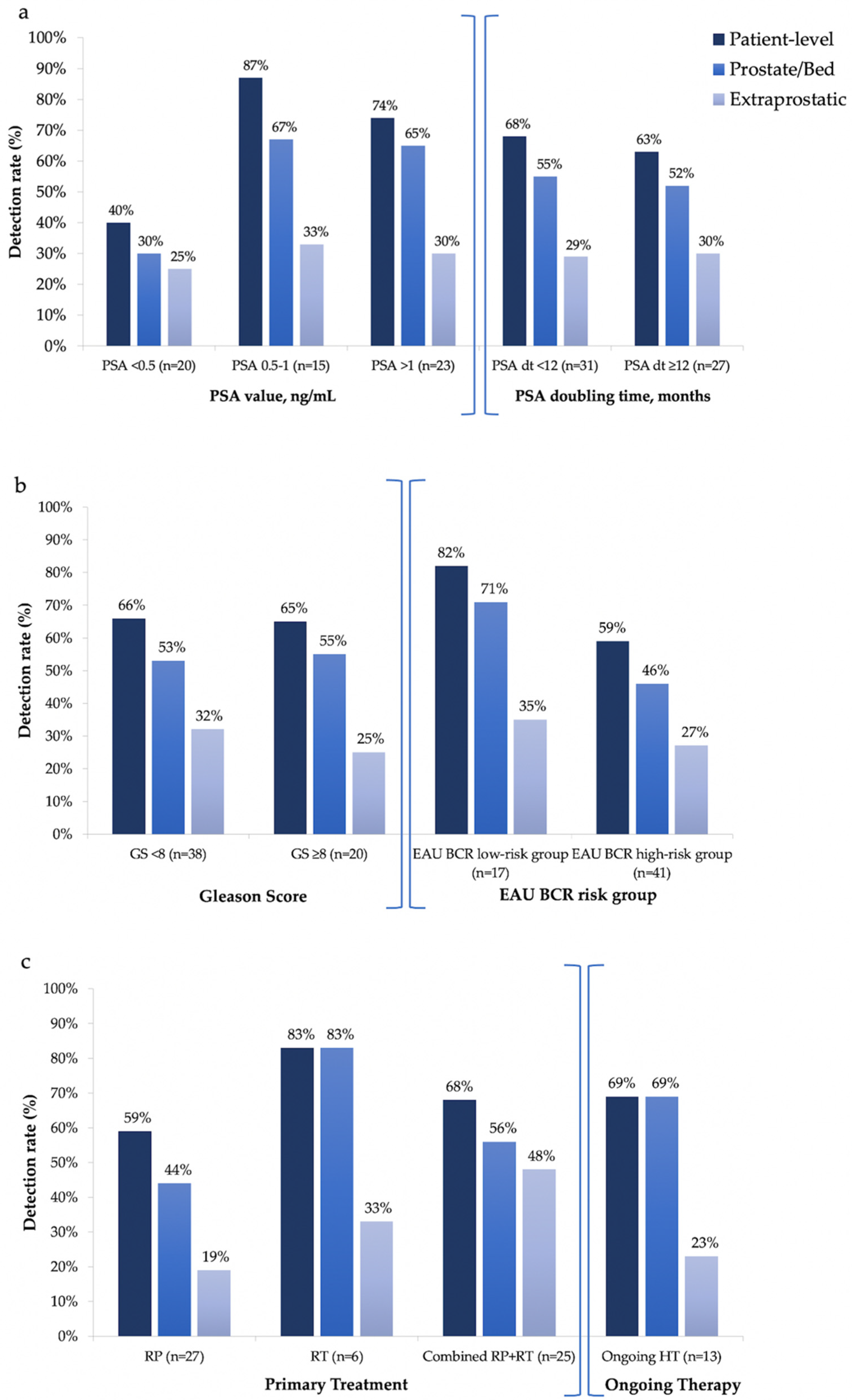
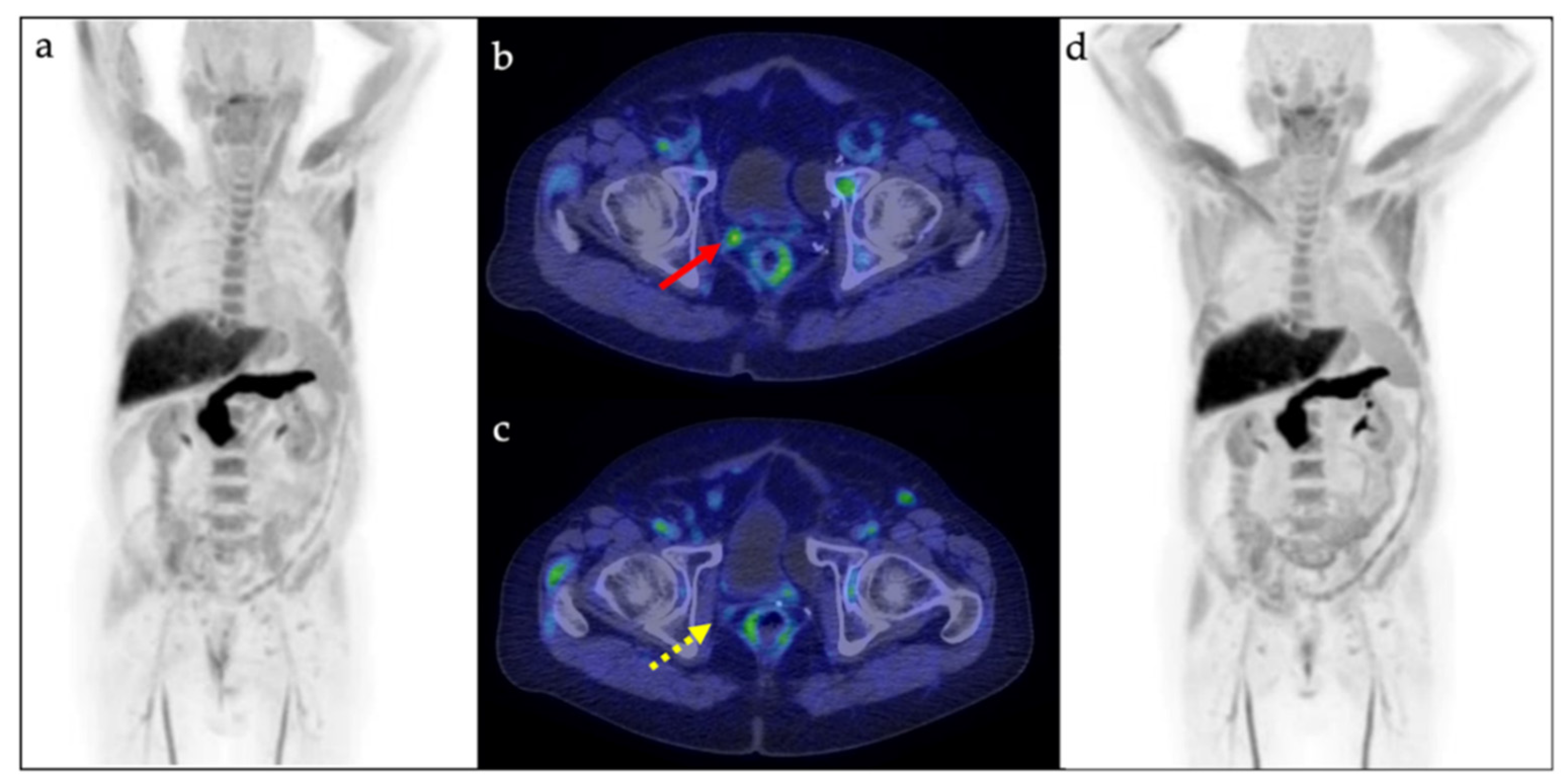
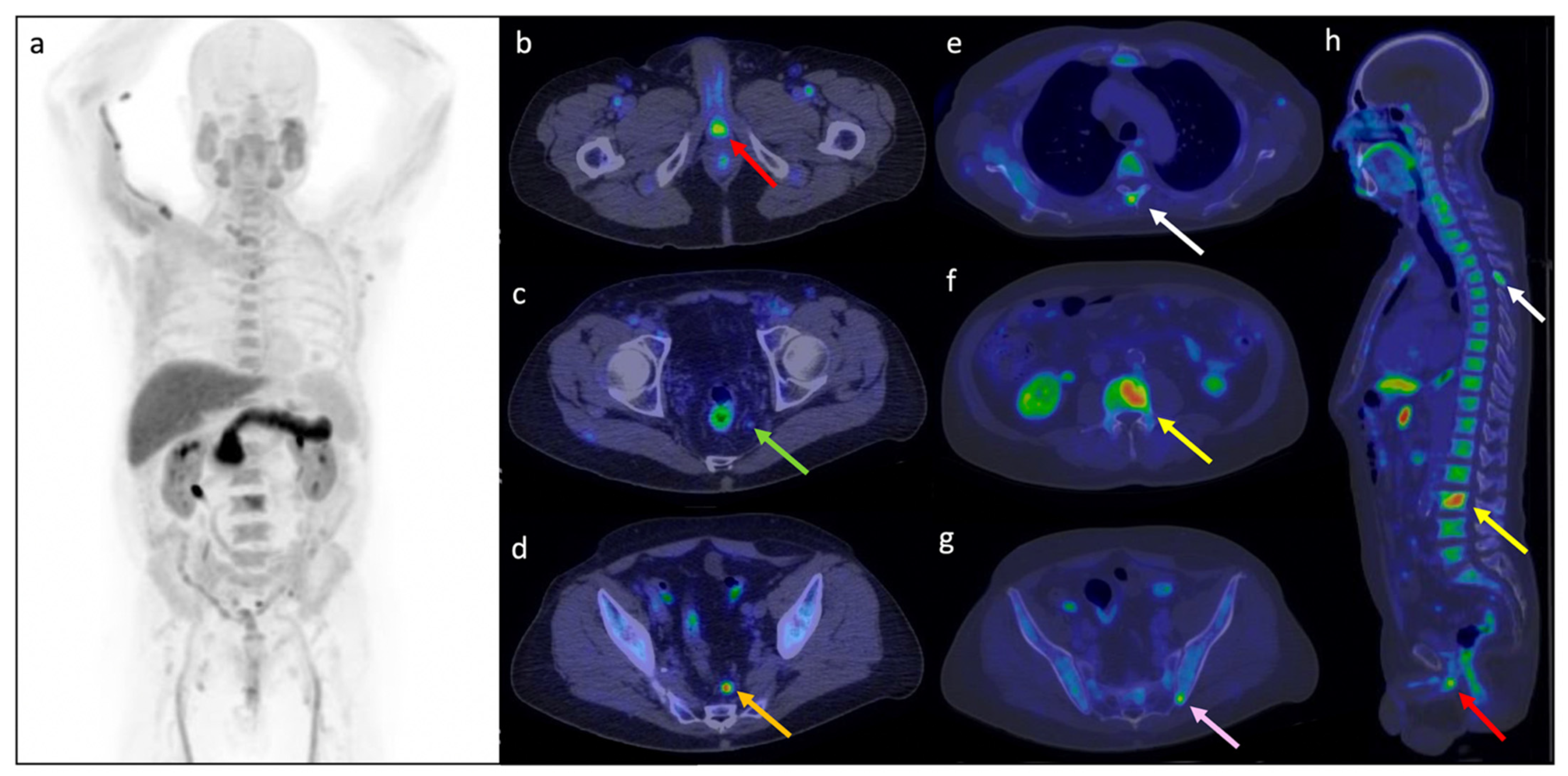
3.1. [18F]Fluciclovine PET/CT Detection Rate
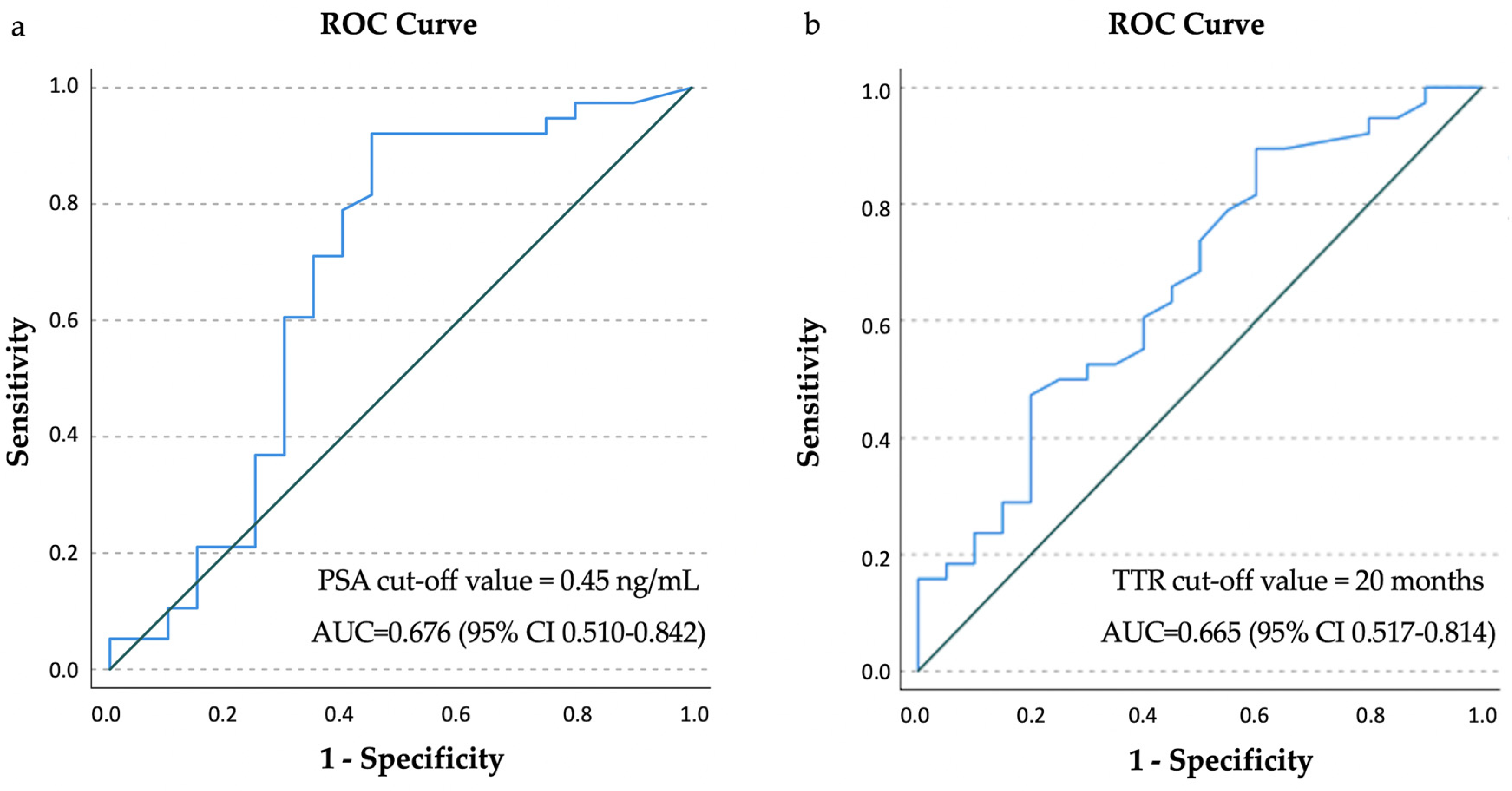
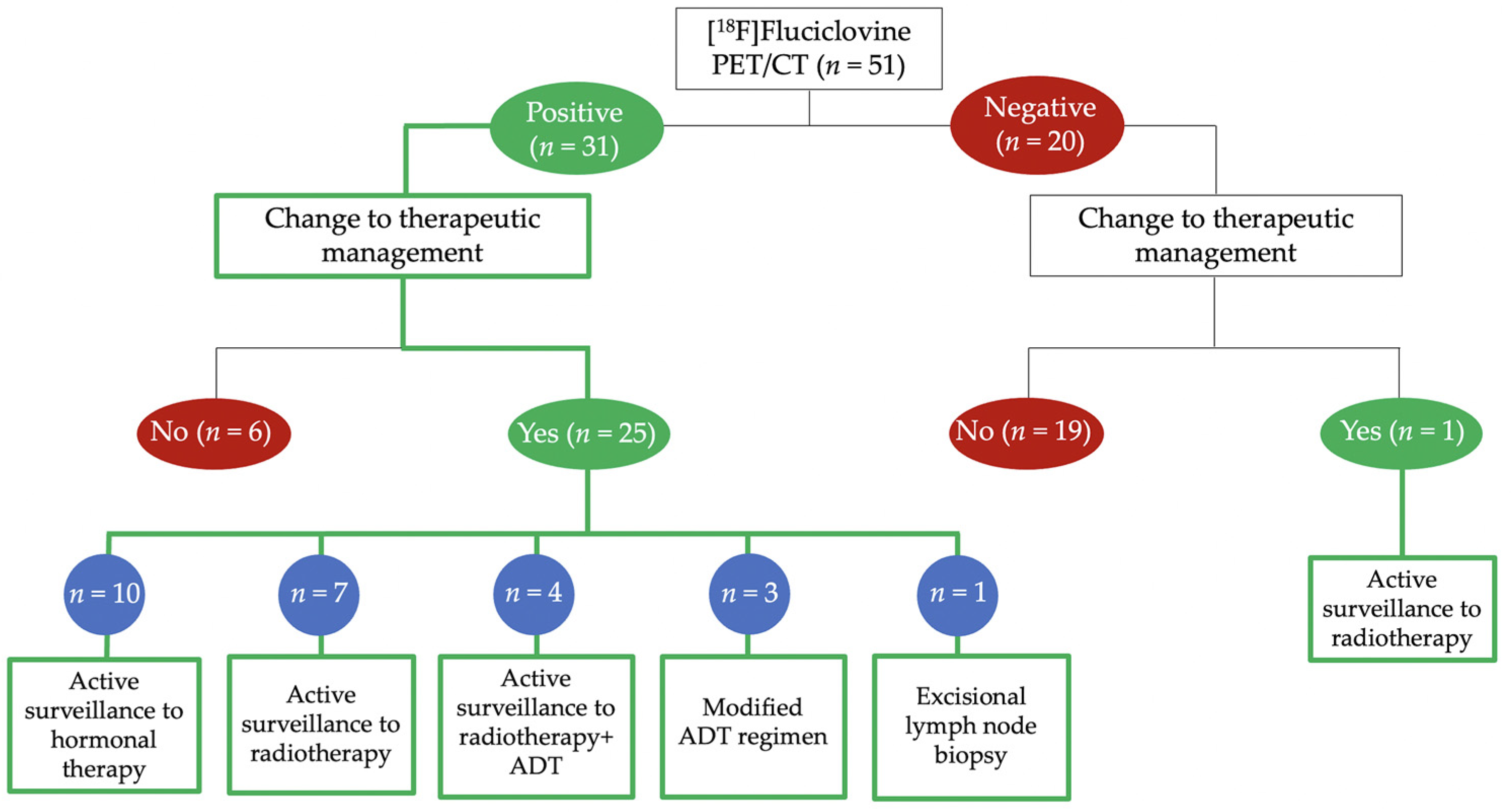
3.2. Follow-Up Data Analysis
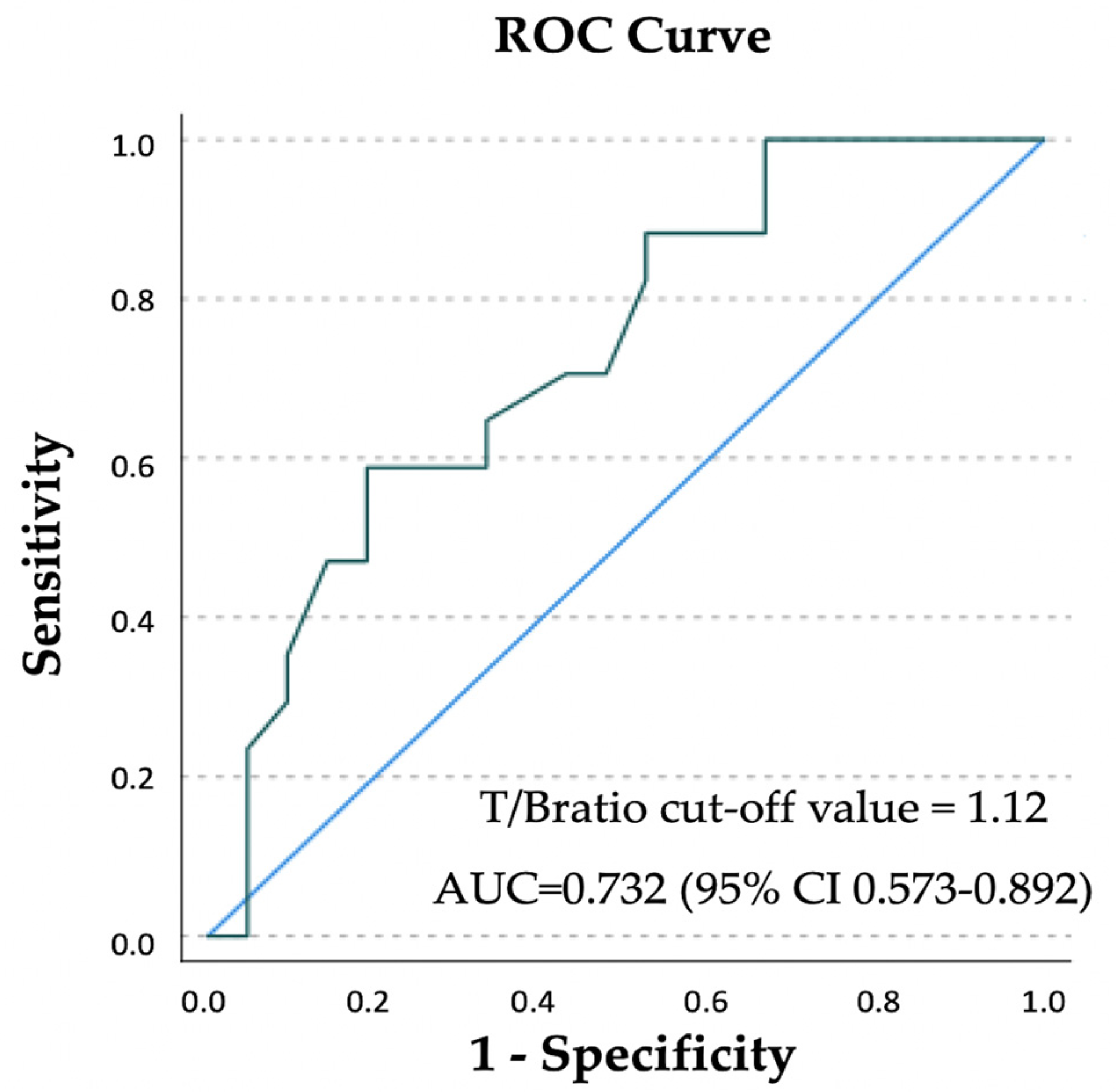
3.3. [18F]Fluciclovine PET/CT Semiquantitative Analysis
3.4. Subpopulation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cornford, P.; van den Bergh, R.C.N.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S.; et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. Part II-2020 Update: Treatment of Relapsing and Metastatic Prostate Cancer. Eur. Urol. 2021, 79, 263–282. [Google Scholar] [CrossRef]
- Vargas, H.A.; Martin-Malburet, A.G.; Takeda, T.; Corradi, R.B.; Eastham, J.; Wibmer, A.; Sala, E.; Zelefsky, M.J.; Weber, W.A.; Hricak, H. Localizing sites of disease in patients with rising serum prostate-specific antigen up to 1 ng/ml following prostatectomy: How much information can conventional imaging provide? Urol. Oncol. Semin. Orig. Investig. 2016, 34, 482.e5–482.e10. [Google Scholar] [CrossRef] [Green Version]
- Farkas, A.B.; Green, E.D.; Thaggard, A.L.; Vijayakumar, V.; Henegan, J.C.; Lirette, S.T.; Nittala, M.R.; Vijayakumar, S. Initial Institutional Experience with 18F-Fluciclovine PET-CT in Biochemical Recurrence of Prostate Cancer. South. Med. J. 2021, 114, 703–707. [Google Scholar] [CrossRef]
- Malone, S.; Croke, J.; Roustan-Delatour, N.; Belanger, E.; Avruch, L.; Malone, C.; Morash, C.; Kayser, C.; Underhill, K.; Li, Y.; et al. Postoperative radiotherapy for prostate cancer: A comparison of four consensus guidelines and dosimetric evaluation of 3D-CRT versus tomotherapy IMRT. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 725–732. [Google Scholar] [CrossRef]
- Nanni, C.; Zanoni, L.; Pultrone, C.; Schiavina, R.; Brunocilla, E.; Lodi, F.; Malizia, C.; Ferrari, M.; Rigatti, P.; Fonti, C.; et al. (18)F-FACBC (anti1-amino-3-(18)F-fluorocyclobutane-1-carboxylic acid) versus (11)C-choline PET/CT in prostate cancer relapse: Results of a prospective trial. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1601–1610. [Google Scholar] [CrossRef]
- Wang, R.; Shen, G.; Huang, M.; Tian, R. The Diagnostic Role of 18 F-Choline, 18 F-Fluciclovine and 18 F-PSMA PET/CT in the Detection of Prostate Cancer With Biochemical Recurrence: A Meta-Analysis. Front. Oncol. 2021, 11. [Google Scholar] [CrossRef]
- Scarsbrook, A.F.; Bottomley, D.; Teoh, E.J.; Bradley, K.M.; Payne, H.; Afaq, A.; Bomanji, J.; van As, N.; Chua, S.; Hoskin, P.; et al. Effect of 18F-Fluciclovine Positron Emission Tomography on the Management of Patients With Recurrence of Prostate Cancer: Results From the FALCON Trial. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 316–324. [Google Scholar] [CrossRef] [Green Version]
- Schuster, D.M.; Nanni, C.; Fanti, S.; Oka, S.; Okudaira, H.; Inoue, Y.; Sörensen, J.; Owenius, R.; Choyke, P.; Turkbey, B.; et al. Anti-1-amino-3-18F-fluorocyclobutane-1-carboxylic acid: Physiologic uptake patterns, incidental findings, and variants that may simulate disease. J. Nucl. Med. 2014, 55, 1986–1992. [Google Scholar] [CrossRef] [Green Version]
- Andriole, G.L.; Kostakoglu, L.; Chau, A.; Duan, F.; Mahmood, U.; Mankoff, D.A.; Schuster, D.M.; Siegel, B.A. The Impact of Positron Emission Tomography with 18F-Fluciclovine on the Treatment of Biochemical Recurrence of Prostate Cancer: Results from the LOCATE Trial. J. Urol. 2019, 201, 322–330. [Google Scholar] [CrossRef]
- Pernthaler, B.; Kulnik, R.; Gstettner, C.; Salamon, S.; Aigner, R.M.; Kvaternik, H. A Prospective Head-to-Head Comparison of 18F-Fluciclovine with 68Ga-PSMA-11 in Biochemical Recurrence of Prostate Cancer in PET/CT. Clin. Nucl. Med. 2019, 44, E566–E573. [Google Scholar] [CrossRef]
- El Bulbul, J.; Grybowski, D.; Lovrec, P.; Solanki, A.A.; Gabriel, M.S.; Wagner, R.H.; Savir-Baruch, B. Positivity Rate of [18F]Fluciclovine PET/CT in Patients with Suspected Prostate Cancer Recurrence at PSA Levels Below 1 ng/mL. Mol. Imaging Biol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Crocerossa, F.; Carbonara, U.; Parekh, J.; Urdaneta, A.; Weprin, S.; Damiano, R.; Grob, M.B.; Hampton, L.J.; Paul, A.; Autorino, R.; et al. PSA and PSA Kinetics as Predictors for 18F-Fluciclovine PET/CT Positivity in Biochemically Recurrent Prostate Cancer. Urol. Int. 2021, 21, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jani, A.B.; Schreibmann, E.; Goyal, S.; Halkar, R.; Hershatter, B.; Rossi, P.J.; Shelton, J.W.; Patel, P.R.; Xu, K.M.; Goodman, M.; et al. 18 F-fluciclovine-PET/CT imaging versus conventional imaging alone to guide postprostatectomy salvage radiotherapy for prostate cancer (EMPIRE-1): A single centre, open-label, phase 2/3 randomised controlled trial. Lancet 2021, 397, 1895–1904. [Google Scholar] [CrossRef]
- Kim, E.H.; Siegel, B.A.; Teoh, E.J.; Andriole, G.L. Prostate cancer recurrence in patients with negative or equivocal conventional imaging: A role for 18F-fluciclovine-PET/CT in delineating sites of recurrence and identifying patients with oligometastatic disease. Urol. Oncol. Semin. Orig. Investig. 2021, 39, 365.e9–365.e16. [Google Scholar] [CrossRef] [PubMed]
- Tilki, D.; Preisser, F.; Graefen, M.; Huland, H.; Pompe, R.S. External Validation of the European Association of Urology Biochemical Recurrence Risk Groups to Predict Metastasis and Mortality After Radical Prostatectomy in a European Cohort. Eur. Urol. 2019, 75, 896–900. [Google Scholar] [CrossRef] [PubMed]
- Nanni, C.; Zanoni, L.; Bach-Gansmo, T.; Minn, H.; Willoch, F.; Bogsrud, T.V.; Edward, E.P.; Savir-Baruch, B.; Teoh, E.; Ingram, F.; et al. [18F]Fluciclovine PET/CT: Joint EANM and SNMMI procedure guideline for prostate cancer imaging—version 1.0. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 579–591. [Google Scholar] [CrossRef] [PubMed]
- Graziani, T.; Ceci, F.; Castellucci, P.; Polverari, G.; Lima, G.M.; Lodi, F.; Morganti, A.G.; Ardizzoni, A.; Schiavina, R.; Fanti, S. 11C-Choline PET/CT for restaging prostate cancer. Results from 4,426 scans in a single-centre patient series. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1971–1979. [Google Scholar] [CrossRef] [PubMed]
- Payne, H.; Bomanji, J.; Bottomley, D.; Scarsbrook, A.F.; Teoh, E.J. Impact of 18 F-fluciclovine PET/CT on salvage radiotherapy plans for men with recurrence of prostate cancer postradical prostatectomy. Nucl. Med. Commun. 2022, 43, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Freedman-Cass, D.; Berardi, R.; Shead, D.A. NCCN Guidelines Version 2.2022 Prostate Cancer. 2021. Available online: http://nccndd.qitian-med.tech/nccn-his/%E5%89%8D%E5%88%97%E8%85%BA%E7%99%8C/%E5%89%8D%E5%88%97%E8%85%BA%E7%99%8C2022.2%E7%89%88.pdf (accessed on 12 January 2022).
- Bach-Gansmo, T.; Nanni, C.; Nieh, P.T.; Zanoni, L.; Bogsrud, T.V.; Sletten, H.; Korsan, K.A.; Kieboom, J.; Tade, F.I.; Odewole, O.; et al. Multisite Experience of the Safety, Detection Rate and Diagnostic Performance of Fluciclovine (18 F) Positron Emission Tomography/Computerized Tomography Imaging in the Staging of Biochemically Recurrent Prostate Cancer. J. Urol. 2017, 197, 676–683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dreyfuss, A.D.; Ahn, G.S.; Barsky, A.R.; Gillman, J.A.; Vapiwala, N.; Pantel, A.R. 18F-Fluciclovine PET/CT in Therapeutic Decision Making for Prostate Cancer: A Large Single-Center Practice-Based Analysis. Clin. Nucl. Med. 2021, 46, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Odewole, O.A.; Tade, F.I.; Nieh, P.T.; Savir-Baruch, B.; Jani, A.B.; Master, V.A.; Rossi, P.J.; Halkar, R.K.; Osunkoya, A.O.; Akin-Akintayo, O.; et al. Recurrent prostate cancer detection with anti-3-[(18)F]FACBC PET/CT: Comparison with CT. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1773–1783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teyateeti, A.; Teyateeti, A.; Macapinlac, H.A.; Lu, Y. Is There Any Role for 18F-Fluciclovine PET/CT in the Presence of Undetectable PSA in Prostate Cancer Patients After Definitive Treatment? Clin. Nucl. Med. 2020, 45, 672–678. [Google Scholar] [CrossRef] [PubMed]
- England, J.R.; Paluch, J.; Ballas, L.K.; Jadvar, H. 18F-Fluciclovine PET/CT Detection of Recurrent Prostate Carcinoma in Patients With Serum PSA ≤ 1 ng/mL After Definitive Primary Treatment. Clin. Nucl. Med. 2019, 44, e128–e132. [Google Scholar] [CrossRef]
- Quartuccio, N.; Marrale, M.; Laudicella, R.; Alongi, P.; Siracusa, M.; Sturiale, L.; Arnone, G.; Cutaia, G.; Salvaggio, G.; Midiri, M.; et al. The role of PET radiomic features in prostate cancer: A systematic review. Clin. Transl. Imaging 2021, 9, 579–588. [Google Scholar] [CrossRef]
- Teyateeti, A.; Teyateeti, A.; Ravizzini, G.C.; Xu, G.; Tang, C.; Tu, S.-M.; Macapinlac, H.A.; Lu, Y. Diagnostic performance of 18 F-fluciclovine PET/CT in prostate cancer patients with rising PSA level ≤ 0.5 ng/ml after multiple treatment failures. Am. J. Nucl. Med. Mol. Imaging 2021, 11, 87–98. [Google Scholar]
- Selnæs, K.M.; Krüger-Stokke, B.; Elschot, M.; Johansen, H.; Steen, P.A.; Langørgen, S.; Aksnessæther, B.Y.; Indrebø, G.; Sjøbakk, T.A.E.; Tessem, M.B.; et al. Detection of Recurrent Prostate Cancer With 18F-Fluciclovine PET/MRI. Front. Oncol. 2020, 10, 2930. [Google Scholar] [CrossRef]
- Malviya, G.; Patel, R.; Salji, M.; Martinez, R.S.; Repiscak, P.; Mui, E.; Champion, S.; Mrowinska, A.; Johnson, E.; AlRasheedi, M.; et al. 18F-Fluciclovine PET metabolic imaging reveals prostate cancer tumour heterogeneity associated with disease resistance to androgen deprivation therapy. EJNMMI Res. 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Zanoni, L.; Mei, R.; Bianchi, L.; Giunchi, F.; Maltoni, L.; Pultrone, C.V.; Nanni, C.; Bossert, I.; Matti, A.; Schiavina, R.; et al. The role of [18f]fluciclovine PET/CT in the characterization of high-risk primary prostate cancer: Comparison with [11c]choline PET/CT and histopathological analysis. Cancers 2021, 13, 1575. [Google Scholar] [CrossRef]
- Parent, E.E.; Schuster, D.M. Update on 18 F-Fluciclovine PET for Prostate Cancer Imaging. J. Nucl. Med. 2018, 59, 733–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schuster, D.M.; Nieh, P.T.; Jani, A.B.; Amzat, R.; Bowman, F.D.; Halkar, R.K.; Master, V.A.; Nye, J.A.; Odewole, O.A.; Osunkoya, A.O.; et al. Anti-3-[18F]FACBC positron emission tomography-computerized tomography and 111In-capromab pendetide single photon emission computerized tomography-computerized tomography for recurrent prostate carcinoma: Results of a prospective clinical trial. J. Urol. 2014, 191, 1446–1453. [Google Scholar] [CrossRef] [Green Version]
- Nanni, C.; Schiavina, R.; Brunocilla, E.; Boschi, S.; Borghesi, M.; Zanoni, L.; Pettinato, C.; Martorana, G.; Fanti, S. 18F-Fluciclovine PET/CT for the Detection of Prostate Cancer Relapse: A Comparison to 11C-Choline PET/CT. Clin. Nucl. Med. 2015, 40, e386–e391. [Google Scholar] [CrossRef] [PubMed]
- Nanni, C.; Schiavina, R.; Brunocilla, E.; Borghesi, M.; Ambrosini, V.; Zanoni, L.; Gentile, G.; Vagnoni, V.; Romagnoli, D.; Martorana, G.; et al. 18F-FACBC compared with 11C-choline PET/CT in patients with biochemical relapse after radical prostatectomy: A prospective study in 28 patients. Clin. Genitourin. Cancer 2014, 12, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Andriole, G.L. What is the best PET target for early biochemical recurrence of prostate cancer? Lancet. Oncol. 2019, 20, e608. [Google Scholar] [CrossRef] [Green Version]
- Calais, J.; Ceci, F.; Eiber, M.; Hope, T.A.; Hofman, M.S.; Rischpler, C.; Bach-Gansmo, T.; Nanni, C.; Savir-Baruch, B.; Elashoff, D.; et al. 18 F-fluciclovine PET-CT and 68 Ga-PSMA-11 PET-CT in patients with early biochemical recurrence after prostatectomy: A prospective, single-centre, single-arm, comparative imaging trial. Lancet. Oncol. 2019, 20, 1286–1294. [Google Scholar] [CrossRef]
| Characteristic | Value |
|---|---|
| No. patients | 58 |
| Age, y | |
| Mean (SD) | 71 ± 7.17 |
| Median (range) | 72 (50–83) |
| Time from primary treatment to BRC, months | |
| Mean (SD) | 60.24 ± 54.09 |
| Median (range) | 43 (1–219) |
| PSA level, ng/mL | |
| Mean (SD) | 1.25 ± 1.18 |
| Median (range) | 0.92 (0.05–5.67) |
| PSA value, n (%) | |
| <0.5 ng/mL | 20/58 (34%) |
| 0.5–1 ng/mL | 15/58 (26%) |
| >1 ng/mL | 23/58 (40%) |
| PSA Doubling Time, months | |
| Mean | 52 |
| Median (range) | 9 (4.20–2241.10) |
| PSA Doubling Time, n (%) | |
| <12 months | 31/58 (53%) |
| ≥12 months | 27/58 (47%) |
| Gleason Score, n (%) | |
| <8 | 38/58 (66%) |
| ≥8 | 20/58 (34%) |
| EAU BCR Risk Group, n (%) | |
| Low-Risk | 17/58 (29%) |
| High-Risk | 41/58 ((71%) |
| Primary treatment, n (%) | |
| RP | 27/58 (47%) |
| RT | 6/58 (10%) |
| RP + RT | 25/58 (43%) |
| Ongoing hormonal therapy, n (%) | |
| Yes | 13/58 (22%) |
| No | 45/58 (78%) |
| [18F]Fluciclovine PET/CT Diagnostic Performance | ||
|---|---|---|
| Value | 95% CI | |
| Sensitivity | 87.10% | 70.17% to 96.37% |
| Specificity | 80.00% | 56.34% to 94.27% |
| PPV | 87.10% | 73.55% to 94.25% |
| NPV | 80.00% | 60.96% to 91.11% |
| Accuracy | 84.31% | 71.41% to 92.98% |
| [18F]Fluciclovine PET Parameters | Mean SUVmaxRL (Range) | p | Mean T/BratioRL (Range) | p | Mean MTVRL (Range) | p | Mean TLARL (Range) | p | Mean SUVmeanRL (Range) | p |
|---|---|---|---|---|---|---|---|---|---|---|
| PSA Value, ng/mL | ||||||||||
| <0.5 | 3.85 | 0.149 | 1.74 | 0.106 | 6.44 | 0.416 | 16,683.44 | 0.618 | 2.35 | 0.195 |
| (2.90–5.24) | (0.70–2.60) | (2.03–15.43) | (3392.10–44,146.60) | (1.63–3.34) | ||||||
| 0.5–1 | 3.93 | 1.2 | 5.3 | 16,111.94 | 2.51 | |||||
| (1.6–9.00) | (0.70–2.20) | (0.66–16.87) | (1089.20–81,840.10) | (0.93–5.90) | ||||||
| >1 | 5.03 | 1.82 | 4.32 | 13,529.53 | 3.05 | |||||
| (2.20–12.20) | (0.60–5.23) | (1.75–11.99) | (3708.10–34,779.60) | (1.29–7.90) | ||||||
| PSA doubling time, months | ||||||||||
| <12 | 5.00 | 0.45 | 1.77 | 0.128 | 4.58 | 0.601 | 15,519.87 | 0.954 | 2.88 | 0.504 |
| (1.90–12.20) | (0.70–5.23) | (0.66–15.43) | (1089.20–81,840.10) | (1.16–7.90) | ||||||
| ≥12 | 3.96 | 1.3 | 5.51 | 13,479.49 | 2.46 | |||||
| (1.60–7.90) | (0.60–2.60) | (1.10–16.87) | (1952.90–38,385.20) | (0.93–4.81) | ||||||
| Gleason Score | ||||||||||
| <8 | 4.49 | 0.952 | 1.61 | 0.627 | 4.82 | 0.259 | 14,511.89 | 0.3 | 2.81 | 0.927 |
| (2.00–12.20) | (0.60–5.23) | (0.66–16.87) | (1089.20–81,840.10) | (1.20–7.90) | ||||||
| ≥8 | 4.14 | 1.54 | 5.72 | 16,239 | 2.51 | |||||
| (1.60–7.50) | (0.90–2.90) | (2.24–15.43) | (2079.90–44,146.60) | (0.93–4.30) | ||||||
| EAU BCR Risk Group | ||||||||||
| Low-Risk | 4.15 | 0.917 | 1.22 | 0.058 | 5.1 | 0.846 | 12,605.06 | 0.846 | 2.5 | 0.964 |
| (2.10–7.90) | (0.60–1.80) | (1.10–16.87) | (1952.90–38,385.20) | (1.29–4.81) | ||||||
| High-Risk | 4.58 | 1.8 | 5.22 | 16,861.75 | 2.82 | |||||
| (1.60–12.20) | (0.70–5.23) | (0.66–15.43) | (1089.20–81,840.10) | (0.93–7.90) | ||||||
| TTR, months | ||||||||||
| ≤20 | 5.65 | 0.982 | 1.97 | 0.505 | 6.49 | 0.63 | 22,583.48 | 0.505 | 3.65 | 0.697 |
| (3.1–12.20) | (0.80–3.80) | (2.37–15.43) | (4384.30–44,146.60) | (1.90–7.90) | ||||||
| >20 | 4.25 | 1.55 | 4.92 | 14,093.1 | 2.62 | |||||
| (1.60–9.00) | (0.60–5.23) | (0.66–16.87) | (1089.20–81,840.10) | (0.93–5.90) | ||||||
| Primary treatment | ||||||||||
| RP | 4.16 | 0.835 | 1.29 | 0.141 | 4.1 | 0.237 | 10,219.34 | 0.197 | 2.53 | 0.913 |
| (1.60–7.90) | (0.60–2.20) | (0.66–16.87) | (1089.20–38,385.20) | (0.93–4.81) | ||||||
| RT | 3.82 | 1.25 | 8.45 | 22,677.74 | 2.59 | |||||
| (2.10–5.00) | (0.70–1.79) | (1.10–15.43) | (1952.90–44,146.60) | (1.80–3.40) | ||||||
| RP + RT | 4.69 | 1.99 | 4.81 | 16,444.07 | 2.88 | |||||
| (2.40–12.20) | (0.70–5.23) | (1.75–13.98) | (3392.10–81,840.10) | (1.63–7.90) | ||||||
| Ongoing hormonal therapy | ||||||||||
| Yes | 4.73 | 0.521 | 1.85 | 0.1 | 6.81 | 0.325 | 22,207.29 | 0.124 | 2.88 | 0.436 |
| (1.90–9.00) | (0.70–5.23) | (1.75–15.43) | (4531.70–81,840.10) | (1.16–5.90) | ||||||
| No | 4.28 | 1.44 | 3.98 | 10,744.88 | 2.67 | |||||
| (1.60–12.20) | (0.60–3.80) | (0.66–16.87) | (1089.20–38,385.20) | (0.93–7.90) |
| Characteristic | Overall Positivity (n = 38) | Prostate/Bed Disease (n = 21) | Extraprostatic Disease (n = 17) | p Value | Oligometastatic Disease (n = 36) | Polymetastatic Disease (n = 2) | p Value |
|---|---|---|---|---|---|---|---|
| PSA Value, ng/mL | |||||||
| Mean (SD) | 1.38 ± 1.20 | 1.35 ± 1.20 | 1.35 ± 1.23 | 0.706 | 1.43 ± 1.21 | 0.61 ± 0.21 | 0.182 |
| Median (range) | 1 (0.05–5.67) | 0.96 (0.26–5.67) | 1.00 (0.05–5.23) | 1.00 (0.05–5.67) | 0.61 (0.46–0.76) | ||
| PSA Value, ng/mL | |||||||
| <0.5 | 8/38 (21%) | 3/21 (14%) | 5/17 (29%) | 0.518 | 7/38 (18%) | 1/2 (50%) | 0.379 |
| 0.5–1 | 13/38 (34%) | 8/21 (38%) | 5/17 (29%) | 12/36 (33%) | 1/2 (50%) | ||
| >1 | 17/38 (45%) | 10/21 (48%) | 7/17 (41%) | 17/36 (47%) | 0/2 (0%) | ||
| PSA doubling time, months | |||||||
| <12 | 21/38 (55%) | 12/21 (57%) | 9/17 (53%) | 0.527 | 19/36 (53%) | 2/2 (100%) | 0.299 |
| ≥12 | 17/38 (45%) | 9/21 (43%) | 8/17 (47%) | 17/36 (47%) | 0/2 (0%) | ||
| Gleason Score | |||||||
| <8 | 25/38 (66%) | 13/21 (62%) | 12/17 (71%) | 0.416 | 24/36 (67%) | 1/2 (50%) | 0.573 |
| ≥8 | 13/38 (34%) | 8/21 (38%) | 5/17 (29%) | 12/36 (33%) | 1/2 (50%) | ||
| EAU BCR Risk Group | |||||||
| Low-Risk | 14/38 (37%) | 8/21 (38%) | 6/17 (35%) | 0.565 | 14/36 (39%) | 0/2 (0%) | 0.393 |
| High-Risk | 24/38 (63%) | 13/21 (62%) | 11/17 (65%) | 22/36 (61%) | 2/2 (100%) | ||
| TTR, months | |||||||
| Mean (SD) | 69.18 ± 56.63 | 74.76 ± 62.52 | 62.29 ± 49.40 | 0.642 | 71.92 ± 56.86 | 20 ± 19.80 | 0.205 |
| Median (range) | 53.5 (5–219) | 58 (5–219) | 38 (6–178) | 56.5 (5–219) | 20 (6–34) | ||
| RP Alone, n (%) | |||||||
| Yes | 16/38 (42%) | 11/21 (52%) | 5/17 (29%) | 0.137 | 16/36 (44%) | 0/2 (0%) | 0.329 |
| No | 22/38 (58%) | 10/21 (48%) | 12/17 (71%) | 20/36 (56%) | 2/2 (100%) | ||
| RT Alone, n (%) | |||||||
| Yes | 20/38 (53%) | 5/21 (24%) | 0/17 (0%) | 0.051 | 5/36 (14%) | 0/2 (0%) | 0.751 |
| No | 18/38 (47%) | 16/21 (76%) | 17/17 (100%) | 31/36 (86%) | 2/2 (100%) | ||
| Combined RP + RT, n (%) | |||||||
| Yes | 17/38 (45%) | 5/21 (24%) | 12/17 (71%) | 0.005 | 15/36 (42%) | 2/2 (100%) | 0.193 |
| No | 21/38 (55%) | 16/21 (76%) | 5/17 (29%) | 21/36 (58%) | 0/2 (0%) | ||
| Ongoing HT, n (%) | |||||||
| Yes | 9/38 (24%) | 6/21 (29%) | 3/17 (18%) | 0.346 | 9/36 (25%) | 0/2 (0%) | 0.578 |
| No | 29/38 (76%) | 15/21 (71%) | 14/17 (82%) | 27/36 (75%) | 2/2 (100%) |
| [18F]Fluciclovine PET Parameters | Overall Positivity (n = 38) | Prostate/Bed Disease (n = 21) | Extraprostatic Disease (n = 17) | p Value | Oligometastatic Disease (n = 36) | Polymetastatic Disease (n = 2) | p Value |
|---|---|---|---|---|---|---|---|
| SUVmaxRL | |||||||
| Mean (SD) | 4.37 ± 2.18 | 4.24 ± 1.80 | 4.205 ± 2.74 | 4.31 ± 2.04 | 6.10 ± 4.10 | ||
| Median | 4 | 4.1 | 3.16 | 0.862 | 4.1 | 6.1 | 0.597 |
| Range | 1.60–12.2 | 1.9–7.9 | 1.60–12.20 | 1.60–12.20 | 3.20–9.00 | ||
| T/BratioRL | |||||||
| Mean (SD) | 1.59 ± 0.91 | 1.39 ± 0.97 | 1.785 ± 0.82 | 1.57 ± 0.92 | 2.00 ± 0.28 | ||
| Median | 1.3 | 1.2 | 1.75 | 0.014 | 1.3 | 2 | 0.159 |
| Range | 0.60–5.23 | 0.6–5.23 | 0.70–3.80 | 0.60–5.23 | 1.80–2.20 | ||
| MTVRL | |||||||
| Mean (SD) | 5.15 ± 4.04 | 4.9 ± 3.67 | 4.375 ± 4.54 | 4.91 ± 3.79 | 8.18 ± 8.21 | ||
| Median | 3.88 | 3.88 | 2.58 | 1 | 3.85 | 8.18 | 0.774 |
| Range | 0.66–16.87 | 1.1–15.43 | 0.658–16.87 | 0.66–16.87 | 2.37–13.98 | ||
| TLARL | |||||||
| Mean (SD) | 15,118.79 ± 15,635.73 | 12,804.89 ± 10,867.18 | 14,943.725 ± 21,128.58 | 13,424.30 ± 10,896.86 | 43,112.20 ± 54,769.52 | ||
| Median | 10,024.8 | 8312.7 | 5647.6 | 0.622 | 10,064.45 | 43,112.2 | 0.774 |
| Range | 1089.20–81,840.10 | 1952.90–44,146.60 | 1089.20–81,840.10 | 1089.20–44,146.60 | 4384.30–81,840.10 | ||
| SUVmeanRL | |||||||
| Mean (SD) | 2.76 ± 1.35 | 2.62 ± 1.04 | 2.625 ± 1.79 | 2.66 ± 1.26 | 3.90 ± 2.83 | ||
| Median | 2.4 | 2.6 | 1.97 | 0.977 | 2.5 | 3.9 | 0.597 |
| Range | 0.93–7.90 | 1.16–4.81 | 0.93–7.90 | 0.93–7.90 | 1.90–5.90 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nappi, A.G.; Ferrari, C.; Mammucci, P.; Rubini, D.; Lavelli, V.; Sardaro, A.; Pisani, A.R.; Rubini, G. [18F]Fluciclovine PET/CT Improves the Clinical Management of Early Recurrence Prostate Cancer Patients. Cancers 2022, 14, 1461. https://doi.org/10.3390/cancers14061461
Nappi AG, Ferrari C, Mammucci P, Rubini D, Lavelli V, Sardaro A, Pisani AR, Rubini G. [18F]Fluciclovine PET/CT Improves the Clinical Management of Early Recurrence Prostate Cancer Patients. Cancers. 2022; 14(6):1461. https://doi.org/10.3390/cancers14061461
Chicago/Turabian StyleNappi, Anna Giulia, Cristina Ferrari, Paolo Mammucci, Dino Rubini, Valentina Lavelli, Angela Sardaro, Antonio Rosario Pisani, and Giuseppe Rubini. 2022. "[18F]Fluciclovine PET/CT Improves the Clinical Management of Early Recurrence Prostate Cancer Patients" Cancers 14, no. 6: 1461. https://doi.org/10.3390/cancers14061461
APA StyleNappi, A. G., Ferrari, C., Mammucci, P., Rubini, D., Lavelli, V., Sardaro, A., Pisani, A. R., & Rubini, G. (2022). [18F]Fluciclovine PET/CT Improves the Clinical Management of Early Recurrence Prostate Cancer Patients. Cancers, 14(6), 1461. https://doi.org/10.3390/cancers14061461






