Detection of Circulating and Disseminated Tumor Cells and Their Prognostic Value under the Influence of Neoadjuvant Therapy in Esophageal Cancer Patients
Abstract
Simple Summary
Abstract
1. Introduction
2. Results
2.1. Characterization of the Analyzed EC Patient Cohort
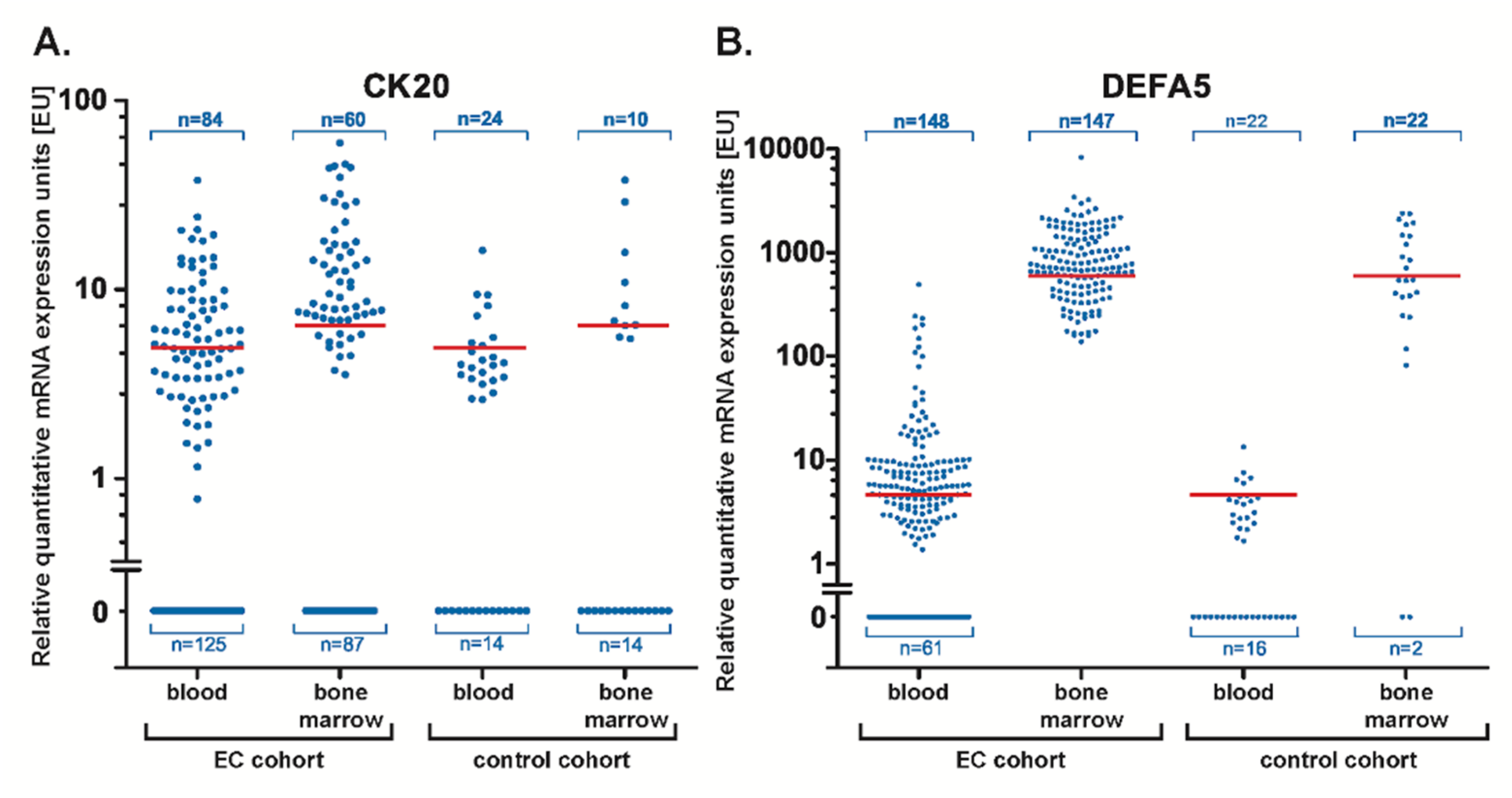
2.2. Quantitative Analysis of CK20 and DEFA5 mRNA Expression by RT-PCR
2.3. Definition of a Diagnostic Cut-Off Threshold of CK20 and DEFA5
2.4. Semi-Quantitative Analysis of CK20 and DEFA5 mRNA Expression by RT-PCR
2.5. Correlation of CK20 and DEFA5 in Liquid Biopsies of EC Patients with Clinical Parameter
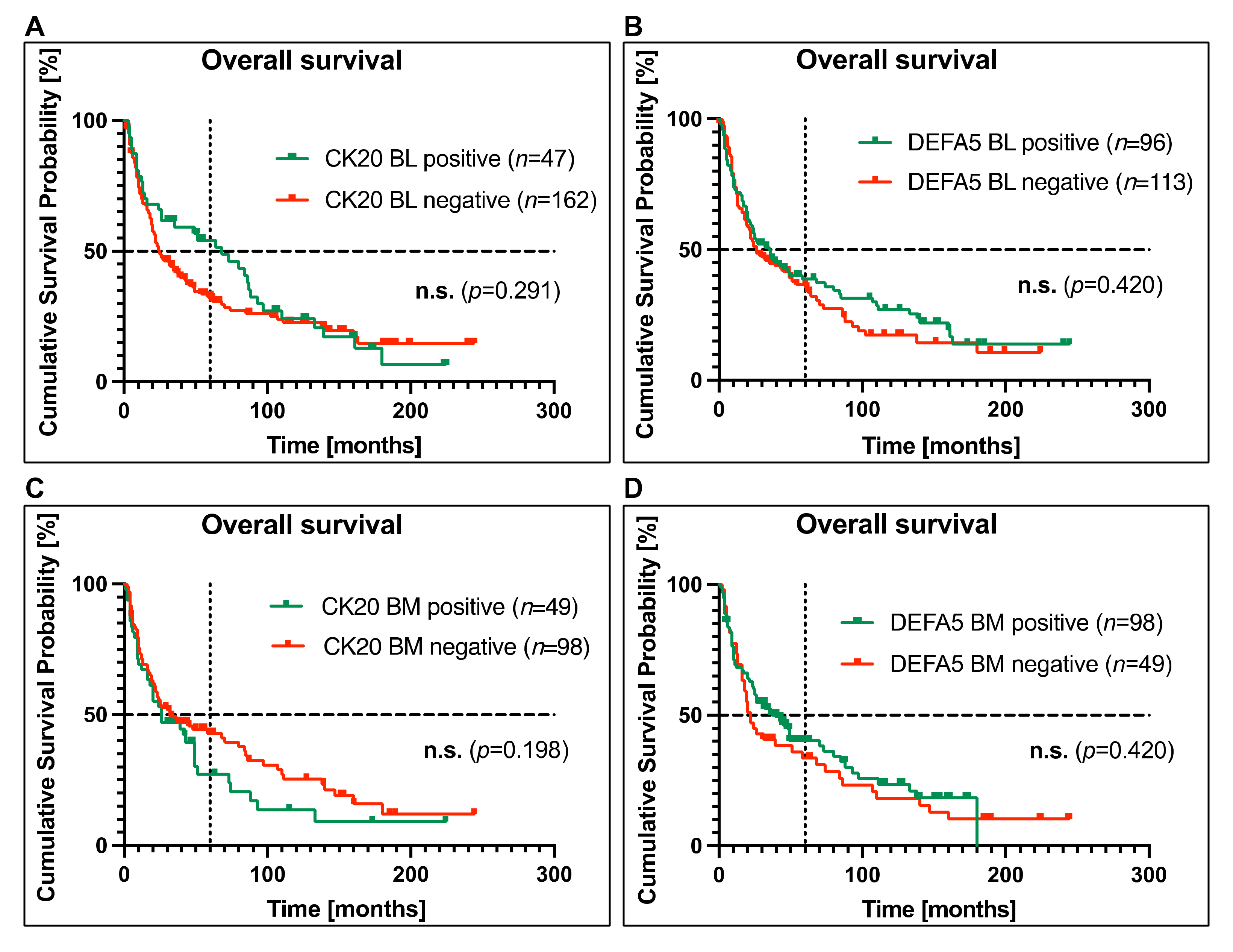
2.6. Correlation of CK20 and DEFA5 Expression in Blood and Bone Marrow with EC Patients’ Survival
2.7. Correlation between CK20 or DEFA5 Detection in Blood or Bone Marrow and Survival in EC Patients without Neoadjuvant Chemotherapy
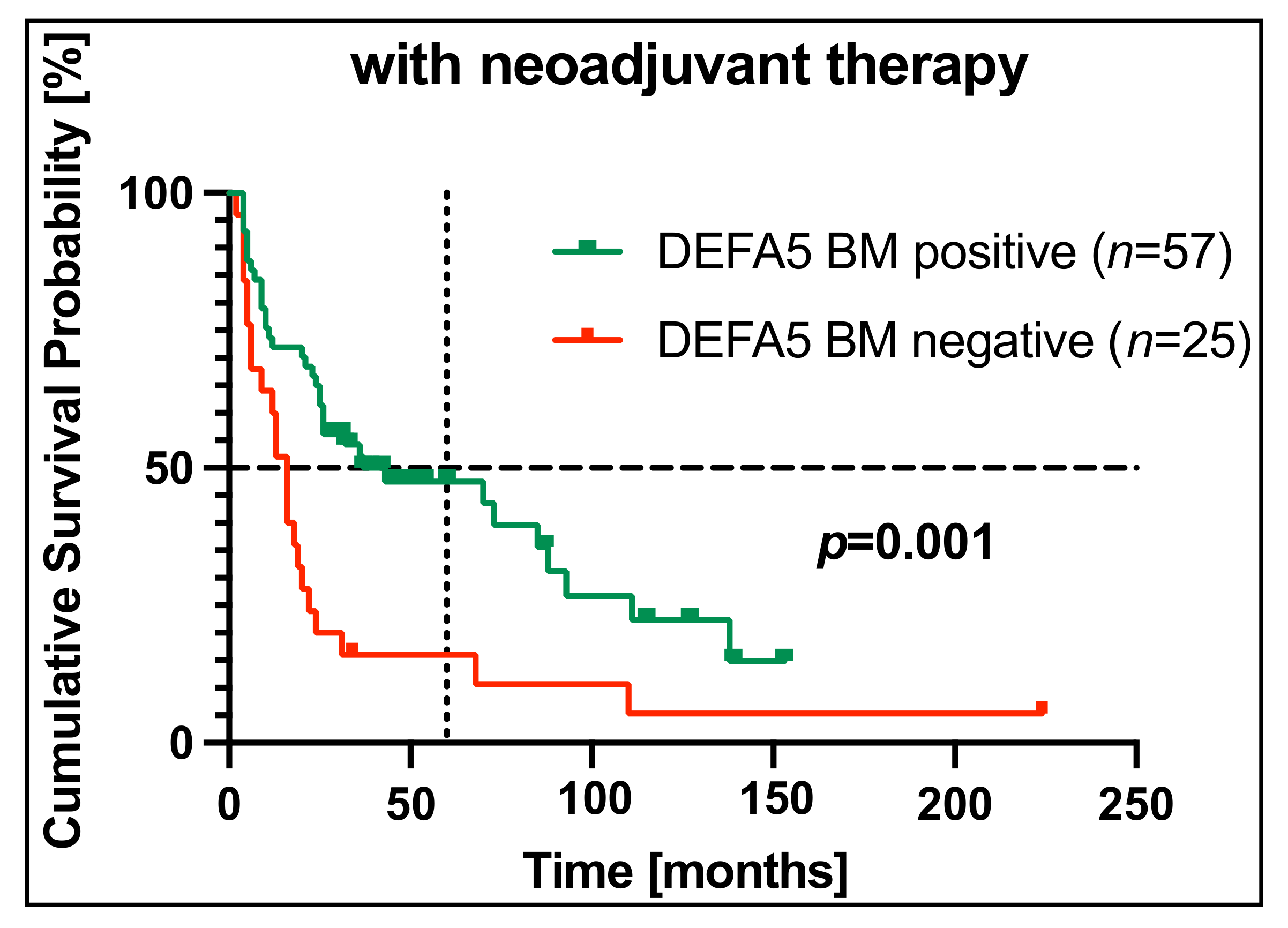
2.8. Correlation of CK20 or DEFA5 Positivity in Blood or Bone Marrow and Survival in EC Patients with Neoadjuvant Chemotherapy
2.9. Multivariate Analyses
3. Materials and Methods
3.1. Patient Cohort
3.2. Control Group
3.3. Sample Collection, Isolation of RNA and RT-PCR
3.4. Statistical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AD | Adenocarcinoma |
| BL | Blood |
| BM | Bone marrow |
| BMB-CCC | Biobank of Comprehensive Cancer Center North |
| cDNA | Complementary deoxyribonucleic acid |
| CI | Confidence interval |
| CK20 | Cytokeratin-20 |
| CRC | Colorectal cancer |
| CT | Computed tomography |
| CTC | Circulating tumor cells |
| DEFA5 | α-defensin 5 |
| DNA | Deoxyribonucleic acid |
| DTC | Disseminated tumor cells |
| EC | Esophageal carcinoma |
| EMT | Epithelial to mesenchymal transition |
| EU | Expression units |
| HER2 | Human epidermal growth factor 2 |
| HR | Hazard ratio |
| LQ | Likelihood quotient |
| MNC | Mononuclear cells |
| MRD | Minimal residual disease |
| mRNA | Messenger ribonucleic acid |
| n.s. | Not significant |
| OS | Overall survival |
| PBS | Phosphate-buffered saline |
| PET | Positron emission tomography |
| P2N | PopGen 2.0 Biobanking Network |
| RNA | Ribonucleic acid |
| ROC | Receiver operating characteristics |
| RT-PCR | Real-time-polymerase chain reaction |
| SCC | Squamous cell carcinoma |
| TCGA | The Cancer Genome Atlas |
| UICC | Union Internationale Contre le Cancer |
| UKSH | University Medical Center Schleswig-Holstein. |
References
- Pennathur, A.; Gibson, M.K.; Jobe, B.A.; Luketich, J.D. Oesophageal carcinoma. Lancet 2013, 381, 400–412. [Google Scholar] [CrossRef]
- Arnold, M.; Soerjomataram, I.; Ferlay, J.; Forman, D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut 2015, 64, 381–387. [Google Scholar] [CrossRef]
- Gao, Y.B.; Chen, Z.L.; Li, J.G.; Hu, X.D.; Shi, X.J.; Sun, Z.M.; Zhang, F.; Zhao, Z.R.; Li, Z.T.; Liu, Z.Y.; et al. Genetic landscape of esophageal squamous cell carcinoma. Nat. Genet. 2014, 46, 1097–1102. [Google Scholar] [CrossRef] [PubMed]
- Lagergren, J.; Smyth, E.; Cunningham, D.; Lagergren, P. Oesophageal cancer. Lancet 2017, 390, 2383–2396. [Google Scholar] [CrossRef]
- Gupta, B.; Kumar, N. Worldwide incidence, mortality and time trends for cancer of the oesophagus. Eur. J. Cancer Prev. 2017, 26, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Rice, T.W.; Apperson-Hansen, C.; DiPaola, L.M.; Semple, M.E.; Lerut, T.E.; Orringer, M.B.; Chen, L.Q.; Hofstetter, W.L.; Smithers, B.M.; Rusch, V.W.; et al. Worldwide Esophageal Cancer Collaboration: Clinical staging data. Dis. Esophagus 2016, 29, 707–714. [Google Scholar] [CrossRef]
- Mariette, C.; Balon, J.M.; Piessen, G.; Fabre, S.; Van Seuningen, I.; Triboulet, J.P. Pattern of recurrence following complete resection of esophageal carcinoma and factors predictive of recurrent disease. Cancer 2003, 97, 1616–1623. [Google Scholar] [CrossRef]
- Reeh, M.; Effenberger, K.E.; Koenig, A.M.; Riethdorf, S.; Eichstadt, D.; Vettorazzi, E.; Uzunoglu, F.G.; Vashist, Y.K.; Izbicki, J.R.; Pantel, K.; et al. Circulating Tumor Cells as a Biomarker for Preoperative Prognostic Staging in Patients with Esophageal Cancer. Ann. Surg. 2015, 261, 1124–1130. [Google Scholar] [CrossRef]
- Izbicki, J.R.; Hosch, S.B.; Pichlmeier, U.; Rehders, A.; Busch, C.; Niendorf, A.; Passlick, B.; Broelsch, C.E.; Pantel, K. Prognostic value of immunohistochemically identifiable tumor cells in lymph nodes of patients with completely resected esophageal cancer. N. Engl. J. Med. 1997, 337, 1188–1194. [Google Scholar] [CrossRef]
- Vashist, Y.K.; Effenberger, K.E.; Vettorazzi, E.; Riethdorf, S.; Yekebas, E.F.; Izbicki, J.R.; Pantel, K. Disseminated tumor cells in bone marrow and the natural course of resected esophageal cancer. Ann. Surg. 2012, 255, 1105–1112. [Google Scholar] [CrossRef]
- Hoeppner, J.; Kulemann, B. Circulating Tumor Cells in Esophageal Cancer. Oncol. Res. Treat. 2017, 40, 417–422. [Google Scholar] [CrossRef]
- Bardelli, A.; Pantel, K. Liquid Biopsies, What We Do Not Know (Yet). Cancer Cell 2017, 31, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Alix-Panabieres, C.; Pantel, K. Circulating tumor cells: Liquid biopsy of cancer. Clin. Chem. 2013, 59, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Braun, S.; Vogl, F.D.; Naume, B.; Janni, W.; Osborne, M.P.; Coombes, R.C.; Schlimok, G.; Diel, I.J.; Gerber, B.; Gebauer, G.; et al. A pooled analysis of bone marrow micrometastasis in breast cancer. N. Engl. J. Med. 2005, 353, 793–802. [Google Scholar] [CrossRef]
- Cohen, S.J.; Punt, C.J.; Iannotti, N.; Saidman, B.H.; Sabbath, K.D.; Gabrail, N.Y.; Picus, J.; Morse, M.; Mitchell, E.; Miller, M.C.; et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J. Clin. Oncol. 2008, 26, 3213–3221. [Google Scholar] [CrossRef] [PubMed]
- Cristofanilli, M.; Budd, G.T.; Ellis, M.J.; Stopeck, A.; Matera, J.; Miller, M.C.; Reuben, J.M.; Doyle, G.V.; Allard, W.J.; Terstappen, L.W.; et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N. Engl. J. Med. 2004, 351, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Su, P.J.; Wu, M.H.; Wang, H.M.; Lee, C.L.; Huang, W.K.; Wu, C.E.; Chang, H.K.; Chao, Y.K.; Tseng, C.K.; Chiu, T.K.; et al. Circulating Tumour Cells as an Independent Prognostic Factor in Patients with Advanced Oesophageal Squamous Cell Carcinoma Undergoing Chemoradiotherapy. Sci. Rep. 2016, 6, 31423. [Google Scholar] [CrossRef]
- Zhao, Y.; Han, L.; Zhang, W.; Shan, L.; Wang, Y.; Song, P.; Peng, C.; Zhao, X. Preoperative chemotherapy compared with postoperative adjuvant chemotherapy for squamous cell carcinoma of the thoracic oesophagus with the detection of circulating tumour cells randomized controlled trial. Int. J. Surg. 2020, 73, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Richter, F.; Baratay, A.; Röder, C.; Egberts, J.H.; Kalthoff, H.; Becker, T.; Sebens, S. Comparative Analysis of Blood and Bone Marrow for the Detection of Circulating and Disseminated Tumor Cells and Their Prognostic and Predictive Value in Esophageal Cancer Patients. J. Clin. Med. 2020, 9, 2674. [Google Scholar] [CrossRef]
- Pantel, K.; Alix-Panabieres, C. Bone marrow as a reservoir for disseminated tumor cells: A special source for liquid biopsy in cancer patients. Bonekey Rep. 2014, 3, 584. [Google Scholar] [CrossRef]
- Hinz, S.; Hendricks, A.; Wittig, A.; Schafmayer, C.; Tepel, J.; Kalthoff, H.; Becker, T.; Röder, C. Detection of circulating tumor cells with CK20 RT-PCR is an independent negative prognostic marker in colon cancer patients—A prospective study. BMC Cancer 2017, 17, 53. [Google Scholar] [CrossRef] [PubMed]
- Andergassen, U.; Kolbl, A.C.; Mahner, S.; Jeschke, U. Real-time RT-PCR systems for CTC detection from blood samples of breast cancer and gynaecological tumour patients (Review). Oncol. Rep. 2016, 35, 1905–1915. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.; Petersen, K.; Krüger, W.; Wolf, M.; Wagener, C.; Zander, A.; Neumaier, M. Detection of micrometastasis by cytokeratin 20 RT-PCR is limited due to stable background transcription in granulocytes. Br. J. Cancer 1999, 81, 870–873. [Google Scholar] [CrossRef] [PubMed]
- Vlems, F.A.; Ladanyi, A.; Gertler, R.; Rosenberg, R.; Diepstra, J.H.; Röder, C.; Nekarda, H.; Molnar, B.; Tulassay, Z.; van Muijen, G.N.; et al. Reliability of quantitative reverse-transcriptase-PCR-based detection of tumour cells in the blood between different laboratories using a standardised protocol. Eur. J. Cancer 2003, 39, 388–396. [Google Scholar] [CrossRef]
- Dandachi, N.; Balic, M.; Stanzer, S.; Halm, M.; Resel, M.; Hinterleitner, T.A.; Samonigg, H.; Bauernhofer, T. Critical evaluation of real-time reverse transcriptase-polymerase chain reaction for the quantitative detection of cytokeratin 20 mRNA in colorectal cancer patients. J. Mol. Diagn. 2005, 7, 631–637. [Google Scholar] [CrossRef][Green Version]
- Moll, R.; Zimbelmann, R.; Goldschmidt, M.D.; Keith, M.; Laufer, J.; Kasper, M.; Koch, P.J.; Franke, W.W. The human gene encoding cytokeratin 20 and its expression during fetal development and in gastrointestinal carcinomas. Differentiation 1993, 53, 75–93. [Google Scholar] [CrossRef]
- Hendricks, A.; Eggebrecht, G.L.; Bernsmeier, A.; Geisen, R.; Dall, K.; Trauzold, A.; Becker, T.; Kalthoff, H.; Schafmayer, C.; Röder, C.; et al. Identifying patients with an unfavorable prognosis in early stages of colorectal carcinoma. Oncotarget 2018, 9, 27423–27434. [Google Scholar] [CrossRef][Green Version]
- Lisitsyn, N.A.; Bukurova, Y.A.; Nikitina, I.G.; Krasnov, G.S.; Sykulev, Y.; Beresten, S.F. Enteric alpha defensins in norm and pathology. Ann. Clin. Microbiol. Antimicrob. 2012, 11, 1. [Google Scholar] [CrossRef]
- Nastase, A.; Paslaru, L.; Niculescu, A.M.; Ionescu, M.; Dumitrascu, T.; Herlea, V.; Dima, S.; Gheorghe, C.; Lazar, V.; Popescu, I. Prognostic and predictive potential molecular biomarkers in colon cancer. Chirurgia 2011, 106, 177–185. [Google Scholar]
- Vragniau, C.; Hubner, J.M.; Beidler, P.; Gil, S.; Saydaminova, K.; Lu, Z.Z.; Yumul, R.; Wang, H.; Richter, M.; Sova, P.; et al. Studies on the Interaction of Tumor-Derived HD5 Alpha Defensins with Adenoviruses and Implications for Oncolytic Adenovirus Therapy. J. Virol. 2017, 91, e02030-16. [Google Scholar] [CrossRef]
- Kemik, O.; Kemik, A.S.; Sumer, A.; Begenik, H.; Purisa, S.; Tuzun, S. Human neutrophil peptides 1, 2 and 3 (HNP 1–3): Elevated serum levels in colorectal cancer and novel marker of lymphatic and hepatic metastasis. Hum. Exp. Toxicol. 2013, 32, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Born, J.; Hendricks, A.; Hauser, C.; Egberts, J.H.; Becker, T.; Roder, C.; Sebens, S. Detection of Marker Associated with CTC in Colorectal Cancer in Mononuclear Cells of Patients with Benign Inflammatory Intestinal Diseases. Cancers 2021, 14, 47. [Google Scholar] [CrossRef]
- Lu, W.; de Leeuw, E. Functional intersection of Human Defensin 5 with the TNF receptor pathway. FEBS Lett. 2014, 588, 1906–1912. [Google Scholar] [CrossRef]
- Qiao, Q.; Bai, R.; Song, W.; Gao, H.; Zhang, M.; Lu, J.; Hong, M.; Zhang, X.; Sun, P.; Zhang, Q.; et al. Human alpha-defensin 5 suppressed colon cancer growth by targeting PI3K pathway. Expl. Cell Res. 2021, 407, 112809. [Google Scholar] [CrossRef]
- Wu, Z.; Ding, Z.; Cheng, B.; Cui, Z. The inhibitory effect of human DEFA5 in growth of gastric cancer by targeting BMI1. Cancer Sci. 2021, 112, 1075–1083. [Google Scholar] [CrossRef]
- Nomura, Y.; Tanabe, H.; Moriichi, K.; Igawa, S.; Ando, K.; Ueno, N.; Kashima, S.; Tominaga, M.; Goto, T.; Inaba, Y.; et al. Reduction of E-cadherin by human defensin-5 in esophageal squamous cells. Biochem. Biophys. Res. Commun. 2013, 439, 71–77. [Google Scholar] [CrossRef]
- Soeth, E.; Vogel, I.; Röder, C.; Juhl, H.; Marxsen, J.; Krüger, U.; Henne-Bruns, D.; Kremer, B.; Kalthoff, H. Comparative analysis of bone marrow and venous blood isolates from gastrointestinal cancer patients for the detection of disseminated tumor cells using reverse transcription PCR. Cancer Res. 1997, 57, 3106–3110. [Google Scholar]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Konczalla, L.; Ghadban, T.; Effenberger, K.E.; Wostemeier, A.; Riethdorf, S.; Uzunoglu, F.G.; Izbicki, J.R.; Pantel, K.; Bockhorn, M.; Reeh, M. Prospective Comparison of the Prognostic Relevance of Circulating Tumor Cells in Blood and Disseminated Tumor Cells in Bone Marrow of a Single Patient’s Cohort with Esophageal Cancer. Ann. Surg. 2021, 273, 299–305. [Google Scholar] [CrossRef]
- Uhlen, M.; Oksvold, P.; Fagerberg, L.; Lundberg, E.; Jonasson, K.; Forsberg, M.; Zwahlen, M.; Kampf, C.; Wester, K.; Hober, S.; et al. Towards a knowledge-based Human Protein Atlas. Nat. Biotechnol. 2010, 28, 1248–1250. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Genome Atlas Research Network. Integrated genomic characterization of oesophageal carcinoma. Nature 2017, 541, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, S.; Natsugoe, S.; Matsumoto, M.; Miyazono, F.; Nakajo, A.; Uchikura, K.; Tokuda, K.; Ishigami, S.; Baba, M.; Takao, S.; et al. Clinical significance of circulating tumor cells in blood by molecular detection and tumor markers in esophageal cancer. Surgery 2003, 133, 162–169. [Google Scholar] [CrossRef]
- Pantel, K.; Brakenhoff, R.H. Dissecting the metastatic cascade. Nat. Rev. Cancer 2004, 4, 448–456. [Google Scholar] [CrossRef]
- Ghosh, D.; Porter, E.; Shen, B.; Lee, S.K.; Wilk, D.; Drazba, J.; Yadav, S.P.; Crabb, J.W.; Ganz, T.; Bevins, C.L. Paneth cell trypsin is the processing enzyme for human defensin-5. Nat. Immunol. 2002, 3, 583–590. [Google Scholar] [CrossRef]
- Bevins, C.L.; Salzman, N.H. Paneth cells, antimicrobial peptides and maintenance of intestinal homeostasis. Nat. Rev. Microbiol. 2011, 9, 356–368. [Google Scholar] [CrossRef]
- Droin, N.; Hendra, J.B.; Ducoroy, P.; Solary, E. Human defensins as cancer biomarkers and antitumour molecules. J. Proteom. 2009, 72, 918–927. [Google Scholar] [CrossRef]
- Ganz, T. Defensins: Antimicrobial peptides of innate immunity. Nat. Rev. Immunol. 2003, 3, 710–720. [Google Scholar] [CrossRef]
- Lehrer, R.I.; Lu, W. alpha-Defensins in human innate immunity. Immunol. Rev. 2012, 245, 84–112. [Google Scholar] [CrossRef]
- Cowland, J.B.; Borregaard, N. The individual regulation of granule protein mRNA levels during neutrophil maturation explains the heterogeneity of neutrophil granules. J. Leukoc. Biol. 1999, 66, 989–995. [Google Scholar] [CrossRef]
- Yount, N.Y.; Wang, M.S.; Yuan, J.; Banaiee, N.; Ouellette, A.J.; Selsted, M.E. Rat neutrophil defensins. Precursor structures and expression during neutrophilic myelopoiesis. J. Immunol. 1995, 155, 4476–4484. [Google Scholar]
- Kaganoi, J.; Shimada, Y.; Kano, M.; Okumura, T.; Watanabe, G.; Imamura, M. Detection of circulating oesophageal squamous cancer cells in peripheral blood and its impact on prognosis. Br. J. Surg. 2004, 91, 1055–1060. [Google Scholar] [CrossRef]
- Setoyama, T.; Natsugoe, S.; Okumura, H.; Matsumoto, M.; Uchikado, Y.; Ishigami, S.; Owaki, T.; Takao, S.; Aikou, T. Carcinoembryonic antigen messenger RNA expression in blood predicts recurrence in esophageal cancer. Clin. Cancer Res. 2006, 12, 5972–5977. [Google Scholar] [CrossRef]
- Wang, S.; Du, H.; Li, G. Significant prognostic value of circulating tumor cells in esophageal cancer patients: A meta-analysis. Oncotarget 2017, 8, 15815–15826. [Google Scholar] [CrossRef]
- Joosse, S.A.; Hannemann, J.; Spotter, J.; Bauche, A.; Andreas, A.; Muller, V.; Pantel, K. Changes in keratin expression during metastatic progression of breast cancer: Impact on the detection of circulating tumor cells. Clin. Cancer Res. 2012, 18, 993–1003. [Google Scholar] [CrossRef]
- Marth, C.; Kisic, J.; Kaern, J.; Trope, C.; Fodstad, O. Circulating tumor cells in the peripheral blood and bone marrow of patients with ovarian carcinoma do not predict prognosis. Cancer 2002, 94, 707–712. [Google Scholar] [CrossRef]
- Chen, S.B.; Su, X.D.; Ma, G.W.; Lin, P.; Wen, J.; Wang, F.X.; Zhang, H.; Fu, J.H.; Zhang, X. Prognostic value of bone marrow micrometastasis in patients with operable esophageal squamous cell carcinoma: A long-term follow-up study. J. Thorac. Oncol. 2014, 9, 1207–1213. [Google Scholar] [CrossRef] [PubMed][Green Version]
- D’Oronzo, S.; Brown, J.; Coleman, R. The role of biomarkers in the management of bone-homing malignancies. J. Bone Oncol. 2017, 9, 1–9. [Google Scholar] [CrossRef]
- Ryan, P.; Furlong, H.; Murphy, C.G.; O’Sullivan, F.; Walsh, T.N.; Shanahan, F.; O’Sullivan, G.C. Prognostic significance of prospectively detected bone marrow micrometastases in esophagogastric cancer: 10-year follow-up confirms prognostic significance. Cancer Med. 2015, 4, 1281–1288. [Google Scholar] [CrossRef]
- Engel, H.; Kleespies, C.; Friedrich, J.; Breidenbach, M.; Kallenborn, A.; Schondorf, T.; Kolhagen, H.; Mallmann, P. Detection of circulating tumour cells in patients with breast or ovarian cancer by molecular cytogenetics. Br. J. Cancer 1999, 81, 1165–1173. [Google Scholar] [CrossRef]
- Guan, X.; Ma, F.; Li, C.; Wu, S.; Hu, S.; Huang, J.; Sun, X.; Wang, J.; Luo, Y.; Cai, R.; et al. The prognostic and therapeutic implications of circulating tumor cell phenotype detection based on epithelial-mesenchymal transition markers in the first-line chemotherapy of HER2-negative metastatic breast cancer. Cancer Commun. 2019, 39, 1–10. [Google Scholar] [CrossRef]
- Porschen, R.; Buck, A.; Fischbach, W.; Gockel, I.; Gorling, U.; Grenacher, L.; Hollerbach, S.; Holscher, A.; Korber, J.; Messmann, H.; et al. S3-Leitlinie Diagnostik und Therapie der Plattenepithelkarzinome und Adenokarzinome des Ösophagus (Langversion 1.0—September 2015, AWMF-Registernummer: 021/023OL). Z. Gastroenterol. 2015, 53, 1288–1347. [Google Scholar] [CrossRef]
- Allum, W.H.; Blazeby, J.M.; Griffin, S.M.; Cunningham, D.; Jankowski, J.A.; Wong, R.; The Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland; The British Society of Gastroenterology; The British Association of Surgical Oncology. Guidelines for the management of oesophageal and gastric cancer. Gut 2011, 60, 1449–1472. [Google Scholar] [CrossRef] [PubMed]
- Stahl, M.; Budach, W.; Meyer, H.J.; Cervantes, A.; The ESMO Guidelines Working Group. Esophageal cancer: Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2010, 21, v46–v49. [Google Scholar] [CrossRef]
- Braun, S.; Kentenich, C.; Janni, W.; Hepp, F.; de Waal, J.; Willgeroth, F.; Sommer, H.; Pantel, K. Lack of effect of adjuvant chemotherapy on the elimination of single dormant tumor cells in bone marrow of high-risk breast cancer patients. J. Clin. Oncol. 2000, 18, 80–86. [Google Scholar] [CrossRef]

| Category | n (%) | 5y-OS (%) | p-Value | |
|---|---|---|---|---|
| All | 216 (100) | 38 | ||
| Gender | Male | 182 (84.3) | 37 | 0.95 |
| Female | 34 (15.7) | 43 | ||
| Age [years] | <70 | 160 (74.1) | 42 | 0.003 |
| >70 | 56 (25.9) | 26 | ||
| Histotype | Adenocarcinoma | 162 (75) | 35 | 0.141 |
| Squamous cell carcinoma | 54 (25) | 42 | ||
| pT category (n = 200) | T1 | 55 (27.5) | 65 | <0.001 |
| T2 | 50 (25) | 19 | ||
| T3 | 93 (46.5) | 28 | ||
| T4 | 2 (1) | 0 | ||
| pN category | N0 | 105 (48.6) | 58 | <0.001 |
| N1 | 73 (33.8) | 23 | ||
| N2 | 29 (13.4) | 13 | ||
| N3 | 9 (4.2) | 0 | ||
| pM category | M0 | 201 (93.1) | 40 | 0.001 |
| M1 | 15 (6.9) | 7 | ||
| UICC stage (n = 200) | I | 48 (24) | 65 | <0.001 |
| II | 52 (26) | 37 | ||
| III | 77 (38.5) | 29 | ||
| IV | 23 (11.5) | 4 | ||
| Neoadjuvant therapy | Yes | 115 (53.2) | 39 | 0.323 |
| No | 101 (46.8) | 38 | ||
| Adjuvant therapy | Yes | 57 (26.4) | 41 | 0.107 |
| No | 138 (63.9) | 37 | ||
| Unknown | 21 (9.7) |
| Variables | Blood Samples (n = 209) (%) | Bone Marrow Samples (n = 147) (%) | ||
|---|---|---|---|---|
| Positive (%) | Negative (%) | Positive (%) | Negative (%) | |
| CK20 | 47 (22.5) | 162 (77.5) | 49 (33.3) | 98 (66.7) |
| DEFA5 | 96 (45.9) | 113 (54.1) | 98 (66.7) | 49 (33.3) |
| Variable | CK20 + BL (%) | p | DEFA5 + BL (%) | p | CK20 + BM (%) | p | DEFA5 + BM (%) | p | |
|---|---|---|---|---|---|---|---|---|---|
| Gender | Male | 38 (21.5) | 0.40 | 83 (46.9) | 0.51 | 44 (34.6) | 0.39 | 85 (66.9) | 0.86 |
| Female | 9 (28.1) | 13 (40.6) | 5 (25) | 13 (65) | |||||
| Age [years] | <70 | 32 (20.6) | 0.28 | 72 (46.5) | 0.79 | 34 (30.9) | 0.28 | 74 (67.3) | 0.79 |
| >70 | 15 (27.8) | 24 (44.4) | 15 (40.5) | 24 (64.9) | |||||
| Histotype | AC | 35 (22.6) | 0.78 | 70 (45.2) | 0.71 | 39 (34.5) | 0.50 | 78 (69) | 0.25 |
| SCC | 12 (22.2) | 26 (48.1) | 10 (29.4) | 20 (58.8) | |||||
| pT category | T1 | 12 (22.2) | 0.81 | 29 (53.7) | 0.30 | 12 (33.3) | 0.54 | 23 (63.9) | 0.24 |
| T2 | 12 (25.5) | 21 (44.7) | 15 (39.5) | 30 (78.9) | |||||
| T3 | 19 (20.9) | 38 (41.8) | 18 (29) | 37 (59.7) | |||||
| T4 | 0 | 0 | 0 | 1 (50) | |||||
| pN category | N0 | 25 (24.8) | 0.73 | 52 (51.5) | 0.24 | 22 (31.4) | 0.79 | 49 (70) | 0.55 |
| N1 | 13 (18.1) | 32 (44.4) | 19 (38) | 32 (64) | |||||
| N2 | 7 (25.9) | 10 (37) | 7 (31.8) | 15 (68.2) | |||||
| N3 | 2 (22.2) | 2 (22.2) | 1 (20) | 2 (40) | |||||
| pM category | M0 | 45 (23.2) | 0.38 | 88 (45.4) | 0.55 | 47 (34.6) | 0.27 | 91 (66.9) | 0.82 |
| M1 | 2 (13.3) | 8 (53.3) | 2 (18.2) | 7 (63.6) | |||||
| UICC stage | I | 11 (23.4) | 0.91 | 27 (57.4) | 0.30 | 11 (35.5) | 0.91 | 21 (67.7) | 0.79 |
| II | 10 (20) | 21 (42) | 12 (32.4) | 26 (70.3) | |||||
| III | 18 (24) | 31 (41.3) | 18 (33.3) | 35 (64.8) | |||||
| IV | 4 (18.2) | 9 (40.9) | 4 (25) | 9 (56.3) | |||||
| Neoadjuvant therapy | Yes | 21 (18.9) | 0.19 | 53 (47.7) | 0.57 | 25 (30.5) | 0.41 | 57 (69.5) | 0.41 |
| No | 26 (26.5) | 43 (43.9) | 24 (36.9) | 41 (63.1) | |||||
| Adjuvant therapy | Yes | 8 (14.8) | 0.08 | 21 (38.9) | 0.31 | 13 (31.7) | 0.73 | 32 (78) | 0.07 |
| No | 36 (26.9) | 63 (47) | 32 (34.8) | 57 (62) | |||||
| Variables | Overall Survival | |
|---|---|---|
| Univariate | Multivariate | |
| p-Value | HR (95% CI) p-Value | |
| Without neoadjuvant therapy | ||
| CK20 detection in BM | 0.006 | 2.28 (1.24–4.22) 0.008 |
| DEFA5 detection in BL | 0.047 | 0.74 (0.41–1.34) 0.318 |
| UICC | <0.001 | 1.60 (1.19–2.17) 0.002 |
| With neoadjuvant therapy | ||
| DEFA5 detection in BM | 0.001 | 0.46 (0.26–0.80) 0.006 |
| UICC | <0.001 | 1.53 (1.10–2.13) 0.012 |
| DEFA5 detection in BM | 0.001 | 0.46 (0.26–0.80) 0.006 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Richter, F.; Röder, C.; Möller, T.; Egberts, J.-H.; Becker, T.; Sebens, S. Detection of Circulating and Disseminated Tumor Cells and Their Prognostic Value under the Influence of Neoadjuvant Therapy in Esophageal Cancer Patients. Cancers 2022, 14, 1279. https://doi.org/10.3390/cancers14051279
Richter F, Röder C, Möller T, Egberts J-H, Becker T, Sebens S. Detection of Circulating and Disseminated Tumor Cells and Their Prognostic Value under the Influence of Neoadjuvant Therapy in Esophageal Cancer Patients. Cancers. 2022; 14(5):1279. https://doi.org/10.3390/cancers14051279
Chicago/Turabian StyleRichter, Florian, Christian Röder, Thorben Möller, Jan-Hendrik Egberts, Thomas Becker, and Susanne Sebens. 2022. "Detection of Circulating and Disseminated Tumor Cells and Their Prognostic Value under the Influence of Neoadjuvant Therapy in Esophageal Cancer Patients" Cancers 14, no. 5: 1279. https://doi.org/10.3390/cancers14051279
APA StyleRichter, F., Röder, C., Möller, T., Egberts, J.-H., Becker, T., & Sebens, S. (2022). Detection of Circulating and Disseminated Tumor Cells and Their Prognostic Value under the Influence of Neoadjuvant Therapy in Esophageal Cancer Patients. Cancers, 14(5), 1279. https://doi.org/10.3390/cancers14051279






