The Use of miRNAs in Predicting Response to Neoadjuvant Therapy in Oesophageal Cancer
Abstract
Simple Summary
Abstract
1. Introduction
1.1. Oesophageal Cancer Epidemiology
1.2. Pathophysiology of OAC and OSCC
1.3. Current Pathways of Screening
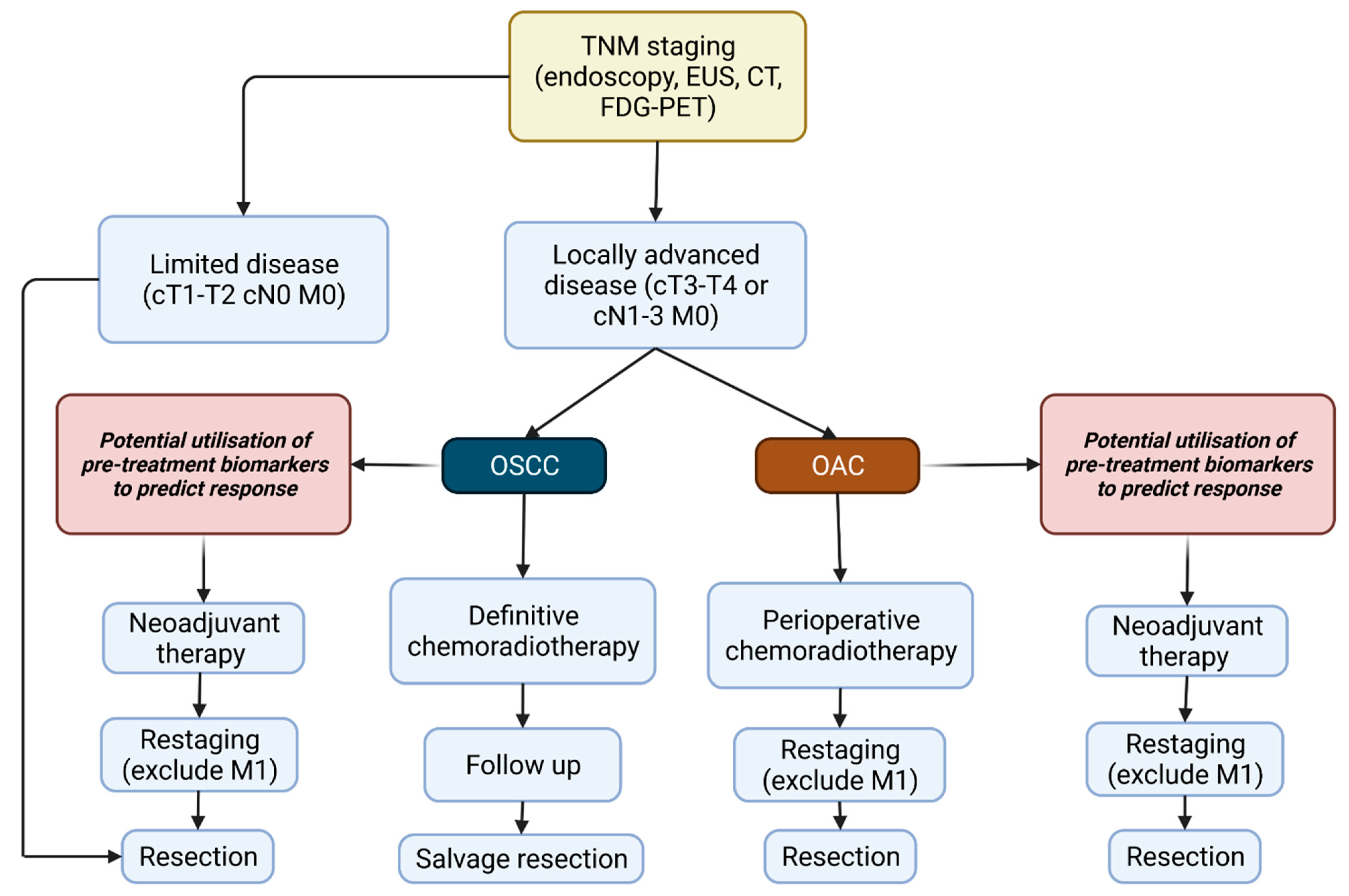
1.4. Treatment of Oesophageal Cancer
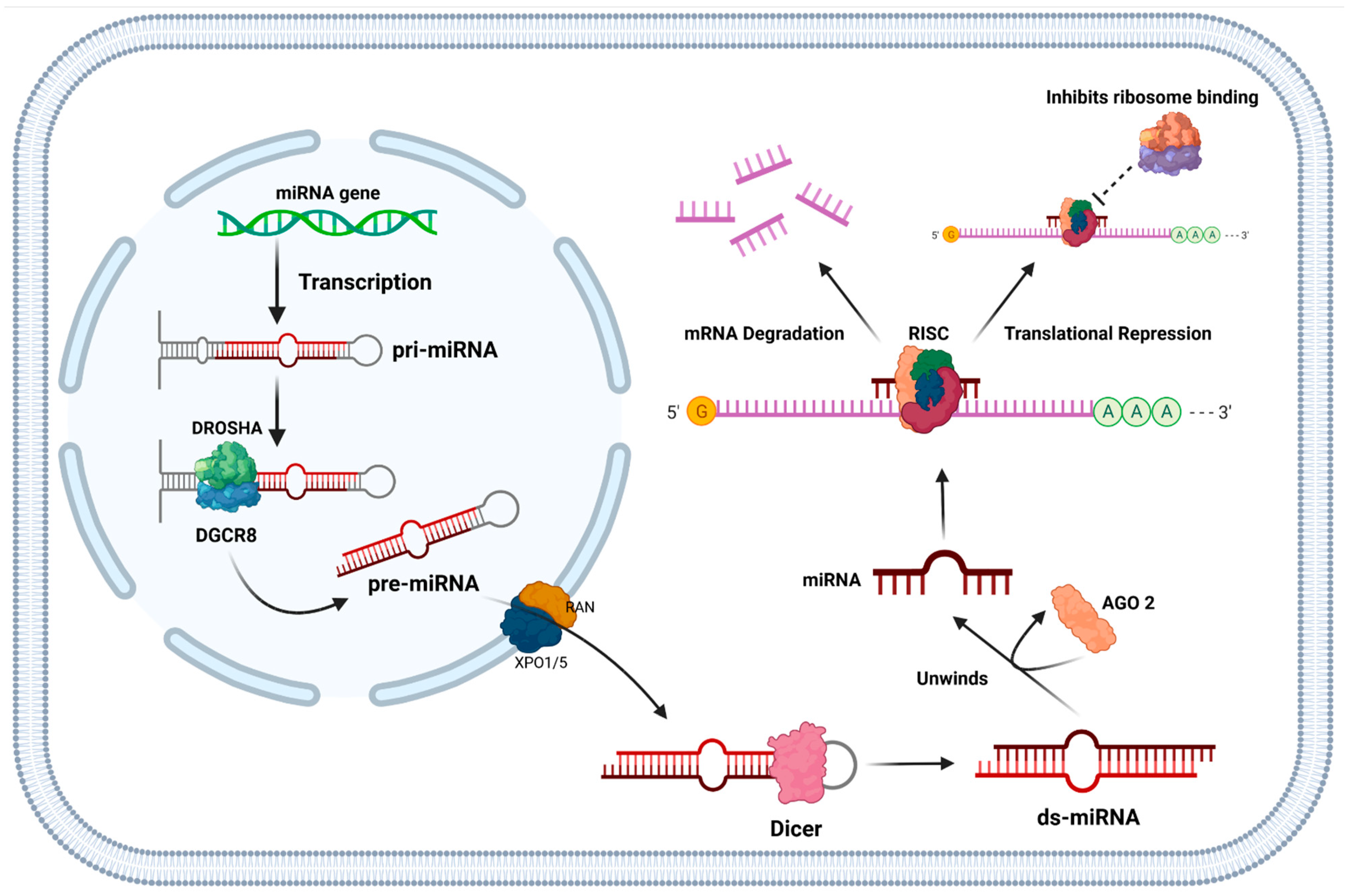
1.5. Function of miRNAs and Their Role in Cancer
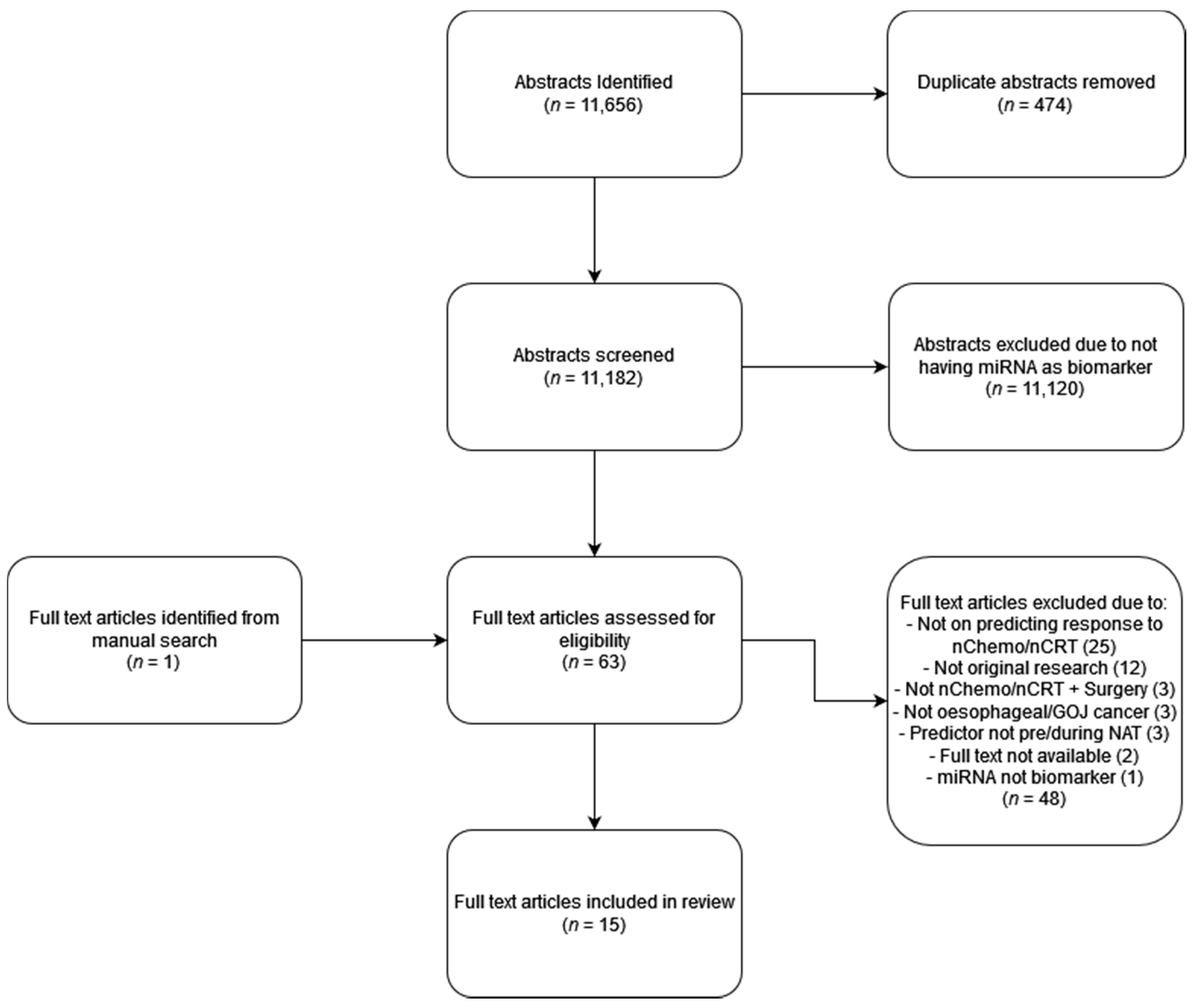
2. Materials and Methods
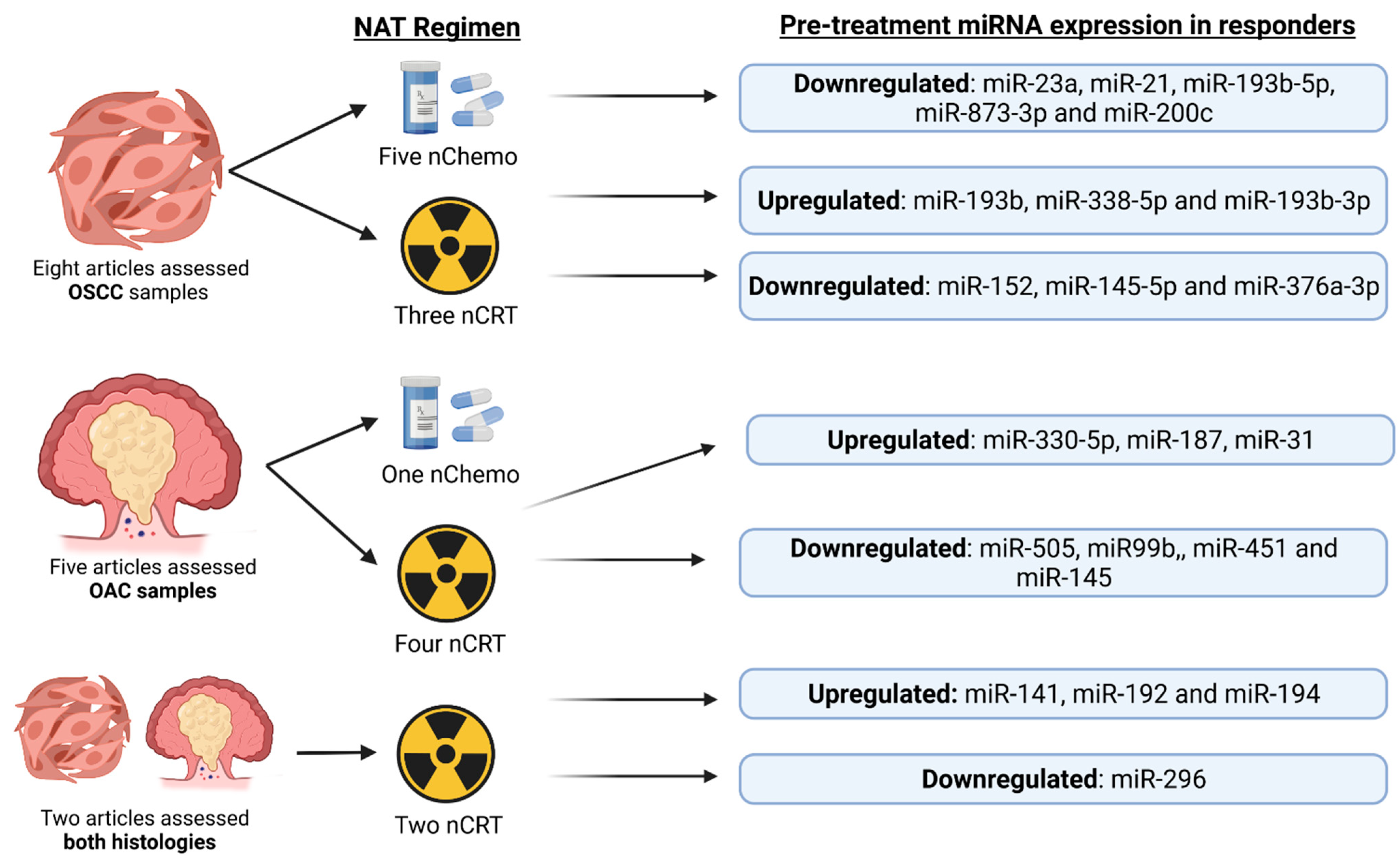
3. Results
3.1. MiRNAs Used to Identify Response in OAC Patients
3.1.1. Articles Studying Response to nChemo Only in OAC Patients
3.1.2. Article Studying Response to nCRT in OAC Patients
3.2. MiRNAs Used to Identify Response in OSCC Patients
3.2.1. Articles Studying Response to nCRT in OSCC Patients
3.2.2. Articles Studying Response to nChemo in OSCC Patients
3.3. MiRNAs Used to Identify Response in Both OAC and OSCC Patients
3.3.1. Articles Studying Response to nChemo in Both OAC and OSCC Patients
3.3.2. Article Studying Response to nCRT in Both OAC and OSCC Patients
3.4. Evidence from In Vitro Functional Studies and Animal Models to Investigate the Utility of miRNAs in Predicting Response to NAT in OAC and OSCC
4. Discussion
4.1. Current Use of miR-21, miR-193b and miR-200c in Cancers and Their Functional Roles
4.2. Strengths and Limitations of the Included Articles
5. Recommendations for Future Research
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Esophageal Cancer: Practice Essentials, Background, Anatomy. 2020. Available online: https://emedicine.medscape.com/article/277930-overview (accessed on 9 November 2020).
- Kamangar, F.; Nasrollahzadeh, D.; Safiri, S.; Sepanlou, S.G.; Fitzmaurice, C.; Ikuta, K.S.; Bisignano, C.; Islami, F.; Roshandel, G.; Lim, S.S.; et al. The Global, Regional, and National Burden of Oesophageal Cancer and Its Attributable Risk Factors in 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 582–597. [Google Scholar] [CrossRef]
- Roser, M.; Ritchie, H. Cancer. Our World Data. 2015. Available online: https://ourworldindata.org/cancer (accessed on 9 November 2020).
- Oesophageal Cancer Statistics. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/oesophageal-cancer (accessed on 9 November 2020).
- Cancer Survival Rates. Available online: https://www.nuffieldtrust.org.uk/resource/cancer-survival-rates (accessed on 9 November 2020).
- Early Diagnosis. Available online: https://crukcancerintelligence.shinyapps.io/EarlyDiagnosis/ (accessed on 16 January 2022).
- Smyth, E.C.; Lagergren, J.; Fitzgerald, R.C.; Lordick, F.; Shah, M.A.; Lagergren, P.; Cunningham, D. Oesophageal Cancer. Nat. Rev. Dis. Primers 2017, 3, 17048. [Google Scholar] [CrossRef] [PubMed]
- Runge, T.M.; Abrams, J.A.; Shaheen, N.J. Epidemiology of Barrett’s Esophagus and Esophageal Adenocarcinoma. Gastroenterol. Clin. N. Am. 2015, 44, 203–231. [Google Scholar] [CrossRef]
- Wong, I.; Law, S. The CROSS Road in Neoadjuvant Therapy for Esophageal Cancer: Long-Term Results of CROSS Trial. Transl. Cancer Res. 2016, 3, S415–S419. [Google Scholar] [CrossRef]
- Ritchie, H.; Roser, M. Smoking. Our World Data. 2013. Available online: https://ourworldindata.org/smoking#:~:text=Smoking%20is%20one%20the%20leading,1%2Din%2D5%20deaths.&text=Nearly%20one%2Din%2Dfour%20adults%20in%20the%20world%20smoke%20tobacco (accessed on 9 November 2020).
- Ramachandran, A.; Chamukuttan, S.; Shetty, S.A.; Arun, N.; Susairaj, P. Obesity in Asia—Is It Different from Rest of the World. Diabetes Metab. Res. Rev. 2012, 28, 47–51. [Google Scholar] [CrossRef]
- Oesophageal Cancers Country Data. Available online: https://digestivecancers.eu/oesophageal-cancer-map/ (accessed on 9 November 2020).
- di Pietro, M.; Alzoubaidi, D.; Fitzgerald, R.C. Barrett’s Esophagus and Cancer Risk: How Research Advances Can Impact Clinical Practice. Gut Liver 2014, 8, 356–370. [Google Scholar] [CrossRef]
- Fléjou, J.-F. Barrett’s Oesophagus: From Metaplasia to Dysplasia and Cancer. Gut 2005, 54, i6–i12. [Google Scholar] [CrossRef]
- Weaver, J.M.J.; Ross-Innes, C.S.; Shannon, N.; Lynch, A.G.; Forshew, T.; Barbera, M.; Murtaza, M.; Ong, C.-A.J.; Lao-Sirieix, P.; Dunning, M.J.; et al. Ordering of Mutations in Preinvasive Disease Stages of Esophageal Carcinogenesis. Nat. Genet. 2014, 46, 837–843. [Google Scholar] [CrossRef]
- Esophageal Cancer—Symptoms and Causes. Available online: https://www.mayoclinic.org/diseases-conditions/esophageal-cancer/symptoms-causes/syc-20356084 (accessed on 3 December 2020).
- Stewart, B.W.; Wild, C.P. (Eds.) World Cancer Report 2014; World Health Organization: Geneva, Switzerland, 2014; ISBN 978-92-832-0432-9. [Google Scholar]
- Testa, U.; Castelli, G.; Pelosi, E. Esophageal Cancer: Genomic and Molecular Characterization, Stem Cell Compartment and Clonal Evolution. Medicines 2017, 4, 67. [Google Scholar] [CrossRef]
- Screening | Oesophageal Cancer | Cancer Research, UK. Available online: https://www.cancerresearchuk.org/about-cancer/oesophageal-cancer/getting-diagnosed/screening (accessed on 16 December 2020).
- Bollschweiler, E.; Boettcher, K.; Hoelscher, A.H.; Sasako, M.; Kinoshita, T.; Maruyama, K.; Siewert, J.R. Is the Prognosis for Japanese and German Patients with Gastric Cancer Really Different? Cancer 1993, 71, 2918–2925. [Google Scholar] [CrossRef]
- Zakko, L.; Lutzke, L.; Wang, K.K. Screening and Preventive Strategies in Esophagogastric Cancer. Surg. Oncol. Clin. 2017, 26, 163–178. [Google Scholar] [CrossRef] [PubMed]
- Ben-Menachem, T.; Decker, G.A.; Early, D.S.; Evans, J.; Fanelli, R.D.; Fisher, D.A.; Fisher, L.; Fukami, N.; Hwang, J.H.; Ikenberry, S.O.; et al. Adverse Events of Upper GI Endoscopy. Gastrointest. Endosc. 2012, 76, 707–718. [Google Scholar] [CrossRef]
- Chen, R.; Liu, Y.; Song, G.; Li, B.; Zhao, D.; Hua, Z.; Wang, X.; Li, J.; Hao, C.; Zhang, L.; et al. Effectiveness of One-Time Endoscopic Screening Programme in Prevention of Upper Gastrointestinal Cancer in China: A Multicentre Population-Based Cohort Study. Gut 2020, 70, 251–260. [Google Scholar] [CrossRef]
- Ross-Innes, C.S.; Debiram-Beecham, I.; O’Donovan, M.; Walker, E.; Varghese, S.; Lao-Sirieix, P.; Lovat, L.; Griffin, M.; Ragunath, K.; Haidry, R.; et al. Evaluation of a Minimally Invasive Cell Sampling Device Coupled with Assessment of Trefoil Factor 3 Expression for Diagnosing Barrett’s Esophagus: A Multi-Center Case-Control Study. PLoS Med. 2015, 12, e1001780. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, R.C.; Di Pietro, M.; O’Donovan, M.; Maroni, R.; Muldrew, B.; Debiram-Beecham, I.; Gehrung, M.; Offman, J.; Tripathi, M.; Smith, S.G.; et al. Cytosponge-Trefoil Factor 3 versus Usual Care to Identify Barrett’s Oesophagus in a Primary Care Setting: A Multicentre, Pragmatic, Randomised Controlled Trial. Lancet 2020, 396, 333–344. [Google Scholar] [CrossRef]
- Oesophageal and Gastric Cancer Overview—NICE Pathways. Available online: https://pathways.nice.org.uk/pathways/oesophageal-and-gastric-cancer#content=view-node%3Anodes-staging (accessed on 3 December 2020).
- Lordick, F.; Mariette, C.; Haustermans, K.; Obermannová, R.; Arnold, D. Oesophageal Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2016, 27, v50–v57. [Google Scholar] [CrossRef]
- Cunningham, D.; Allum, W.H.; Stenning, S.P.; Thompson, J.N.; Van de Velde, C.J.H.; Nicolson, M.; Scarffe, J.H.; Lofts, F.J.; Falk, S.J.; Iveson, T.J.; et al. Perioperative Chemotherapy versus Surgery Alone for Resectable Gastroesophageal Cancer. N. Engl. J. Med. 2006, 355, 11–20. [Google Scholar] [CrossRef]
- van Hagen, P.; Hulshof, M.C.C.M.; van Lanschot, J.J.B.; Steyerberg, E.W.; Henegouwen, M.V.B.; Wijnhoven, B.P.L.; Richel, D.J.; Nieuwenhuijzen, G.A.P.; Hospers, G.A.P.; Bonenkamp, J.J.; et al. Preoperative Chemoradiotherapy for Esophageal or Junctional Cancer. N. Engl. J. Med. 2012, 366, 2074–2084. [Google Scholar] [CrossRef]
- Zhang, B.; Pan, X.; Cobb, G.P.; Anderson, T.A. MicroRNAs as Oncogenes and Tumor Suppressors. Dev. Biol. 2007, 302, 1–12. [Google Scholar] [CrossRef]
- Noble, F.; Lloyd, M.A.; Turkington, R.; Griffiths, E.; O’Donovan, M.; O’Neill, J.R.; Mercer, S.; Parsons, S.L.; Fitzgerald, R.C.; Underwood, T.J.; et al. Multicentre Cohort Study to Define and Validate Pathological Assessment of Response to Neoadjuvant Therapy in Oesophagogastric Adenocarcinoma. Br. J. Surg. 2017, 104, 1816–1828. [Google Scholar] [CrossRef]
- Lordick, F.; Gockel, I. Chances, Risks and Limitations of Neoadjuvant Therapy in Surgical Oncology. Innov. Surg. Sci. 2016, 1, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Barbour, A.P.; Walpole, E.T.; Mai, G.T.; Barnes, E.H.; Watson, D.I.; Ackland, S.P.; Martin, J.M.; Burge, M.; Finch, R.; Karapetis, C.S.; et al. Preoperative Cisplatin, Fluorouracil, and Docetaxel with or without Radiotherapy after Poor Early Response to Cisplatin and Fluorouracil for Resectable Oesophageal Adenocarcinoma (AGITG DOCTOR): Results from a Multicentre, Randomised Controlled Phase II Trial. Ann. Oncol. 2020, 31, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Pathologic Assessment of Tumor Regression after Preoperative Chemoradiotherapy of Esophageal Carcinoma. Clinicopathologic Correlations—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/8194005/ (accessed on 26 January 2022).
- Wang, D.; Smit, J.K.; Zwaan, E.; Muijs, C.T.; Groen, H.; Hollema, H.; Plukker, J.T. Neoadjuvant Therapy Reduces the Incidence of Nodal Micrometastases in Esophageal Adenocarcinoma. Am. J. Surg. 2013, 206, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Hiraki, Y.; Kimura, Y.; Imano, M.; Kato, H.; Iwama, M.; Shiraishi, O.; Yasuda, A.; Shinkai, M.; Makino, T.; Motoori, M.; et al. Controlling Lymph Node Micrometastases by Neoadjuvant Chemotherapy Affects the Prognosis in Advanced Esophageal Squamous Cell Carcinoma. Surg. Today 2021, 51, 118–126. [Google Scholar] [CrossRef]
- Ameres, S.L.; Zamore, P.D. Diversifying MicroRNA Sequence and Function. Nat. Rev. Mol. Cell Biol. 2013, 14, 475–488. [Google Scholar] [CrossRef]
- Lai, E.C. Micro RNAs Are Complementary to 3′ UTR Sequence Motifs That Mediate Negative Post-Transcriptional Regulation. Nat. Genet. 2002, 30, 363–364. [Google Scholar] [CrossRef]
- Zhang, Y. RNA-Induced Silencing Complex (RISC). In Encyclopedia of Systems Biology; Dubitzky, W., Wolkenhauer, O., Cho, K.-H., Yokota, H., Eds.; Springer: New York, NY, USA, 2013; p. 1876. ISBN 978-1-4419-9863-7. [Google Scholar]
- Ding, L.; Lan, Z.; Xiong, X.; Ao, H.; Feng, Y.; Gu, H.; Yu, M.; Cui, Q. The Dual Role of MicroRNAs in Colorectal Cancer Progression. Int. J. Mol. Sci. 2018, 19, 2791. [Google Scholar] [CrossRef]
- MacFarlane, L.-A.; Murphy, P.R. MicroRNA: Biogenesis, Function and Role in Cancer. Curr. Genom. 2010, 11, 537–561. [Google Scholar] [CrossRef]
- Essakly, A.; Loeser, H.; Kraemer, M.; Alakus, H.; Chon, S.-H.; Zander, T.; Buettner, R.; Hillmer, A.M.; Bruns, C.J.; Schroeder, W.; et al. PIK3CA and KRAS Amplification in Esophageal Adenocarcinoma and Their Impact on the Inflammatory Tumor Microenvironment and Prognosis. Transl. Oncol. 2019, 13, 157–164. [Google Scholar] [CrossRef]
- Xu, J.; Lv, H.; Zhang, B.; Xu, F.; Zhu, H.; Chen, B.; Zhu, C.; Shen, J. MiR-30b-5p Acts as a Tumor Suppressor MicroRNA in Esophageal Squamous Cell Carcinoma. J. Thorac. Dis. 2019, 11, 3015–3029. [Google Scholar] [CrossRef]
- Cui, X.-B.; Peng, H.; Li, R.-R.; Mu, J.-Q.; Yang, L.; Li, N.; Liu, C.-X.; Hu, J.-M.; Li, S.-G.; Wei, Y.; et al. MicroRNA-34a Functions as a Tumor Suppressor by Directly Targeting Oncogenic PLCE1 in Kazakh Esophageal Squamous Cell Carcinoma. Oncotarget 2017, 8, 92454–92469. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Skinner, H.D.; Lee, J.H.; Bhutani, M.S.; Weston, B.; Hofstetter, W.; Komaki, R.; Shiozaki, H.; Wadhwa, R.; Sudo, K.; Elimova, E.; et al. A Validated MiRNA Profile Predicts Response to Therapy in Esophageal Adenocarcinoma. Cancer 2014, 120, 3635–3641. [Google Scholar] [CrossRef] [PubMed]
- Lindholm, E.M.; Aure, M.R.; Haugen, M.H.; Sahlberg, K.K.; Kristensen, V.N.; Nebdal, D.; Børresen-Dale, A.-L.; Lingjærde, O.C.; Engebraaten, O. MiRNA Expression Changes during the Course of Neoadjuvant Bevacizumab and Chemotherapy Treatment in Breast Cancer. Mol. Oncol. 2019, 13, 2278–2296. [Google Scholar] [CrossRef] [PubMed]
- Kheirelseid, E.A.H.; Miller, N.; Chang, K.H.; Curran, C.; Hennessey, E.; Sheehan, M.; Newell, J.; Lemetre, C.; Balls, G.; Kerin, M.J. MiRNA Expressions in Rectal Cancer as Predictors of Response to Neoadjuvant Chemoradiation Therapy. Int. J. Colorectal Dis. 2013, 28, 247–260. [Google Scholar] [CrossRef]
- Gao, S.; Zhao, Z.-Y.; Zhang, Z.-Y.; Zhang, Y.; Wu, R. Prognostic Value of MicroRNAs in Esophageal Carcinoma: A Meta-Analysis. Clin. Transl. Gastroenterol. 2018, 9, 203. [Google Scholar] [CrossRef]
- Bibby, B.A.S.; Reynolds, J.V.; Maher, S.G. MicroRNA-330-5p as a Putative Modulator of Neoadjuvant Chemoradiotherapy Sensitivity in Oesophageal Adenocarcinoma. PLoS ONE 2015, 10, e0134180. [Google Scholar] [CrossRef] [PubMed]
- Lynam-Lennon, N.; Bibby, B.A.S.; Mongan, A.M.; Marignol, L.; Paxton, C.N.; Geiersbach, K.; Bronner, M.P.; O’Sullivan, J.; Reynolds, J.V.; Maher, S.G. Low MiR-187 Expression Promotes Resistance to Chemoradiation Therapy In Vitro and Correlates with Treatment Failure in Patients with Esophageal Adenocarcinoma. Mol. Med. 2016, 22, 388–397. [Google Scholar] [CrossRef]
- Lynam-Lennon, N.; Reynolds, J.V.; Marignol, L.; Sheils, O.M.; Pidgeon, G.P.; Maher, S.G. MicroRNA-31 Modulates Tumour Sensitivity to Radiation in Oesophageal Adenocarcinoma. J. Mol. Med. 2012, 90, 1449–1458. [Google Scholar] [CrossRef]
- Ilhan-Mutlu, A.; Tezcan, G.; Schoppmann, S.F.; Preusser, M.; Spyridoula, K.; Karanikas, G.; Birner, P. MicroRNA-21 Expression Is Elevated in Esophageal Adenocarcinoma After Neoadjuvant Chemotherapy. Cancer Investig. 2015, 33, 246–250. [Google Scholar] [CrossRef]
- Wen, J.; Luo, K.; Liu, H.; Liu, S.; Lin, G.; Hu, Y.; Zhang, X.; Wang, G.; Chen, Y.; Chen, Z.; et al. MiRNA Expression Analysis of Pretreatment Biopsies Predicts the Pathological Response of Esophageal Squamous Cell Carcinomas to Neoadjuvant Chemoradiotherapy. Ann. Surg. 2016, 263, 942–948. [Google Scholar] [CrossRef]
- Chan, C.; Lai, K.; Ng, E.; Kiang, M.; Kwok, T.; Wang, H.; Chan, K.; Law, T.; Tong, D.; Chan, K.; et al. Serum MicroRNA-193b as a Promising Biomarker for Prediction of Chemoradiation Sensitivity in Esophageal Squamous Cell Carcinoma Patients. Oncol. Lett. 2017, 15, 3273–3280. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Cui, D.; Li, B.; Xu, W.W.; Lam, A.K.Y.; Chan, K.T.; Zhu, Y.; Lee, N.P.Y.; Law, S.Y.K.; Guan, X.Y.; et al. MicroRNA-338-5p Reverses Chemoresistance and Inhibits Invasion of Esophageal Squamous Cell Carcinoma Cells by Targeting Id-1. Cancer Sci. 2019, 110, 3677–3688. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, S.; Ichikawa, D.; Kawaguchi, T.; Takeshita, H.; Miyamae, M.; Ohashi, T.; Okajima, W.; Imamura, T.; Kiuchi, J.; Arita, T.; et al. Plasma MicroRNA Profiles: Identification of MiR-23a as a Novel Biomarker for Chemoresistance in Esophageal Squamous Cell Carcinoma. Oncotarget 2016, 7, 62034–62048. [Google Scholar] [CrossRef] [PubMed]
- Kurashige, J.; Kamohara, H.; Watanabe, M.; Tanaka, Y.; Kinoshita, K.; Saito, S.; Hiyoshi, Y.; Iwatsuki, M.; Baba, Y.; Baba, H. Serum MicroRNA-21 Is a Novel Biomarker in Patients with Esophageal Squamous Cell Carcinoma. J. Surg. Oncol. 2012, 106, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Niwa, Y.; Yamada, S.; Sonohara, F.; Kurimoto, K.; Hayashi, M.; Tashiro, M.; Iwata, N.; Kanda, M.; Tanaka, C.; Kobayashi, D.; et al. Identification of a Serum-Based MiRNA Signature for Response of Esophageal Squamous Cell Carcinoma to Neoadjuvant Chemotherapy. J. Transl. Med. 2019, 17, 1. [Google Scholar] [CrossRef]
- Tanaka, K.; Miyata, H.; Yamasaki, M.; Sugimura, K.; Takahashi, T.; Kurokawa, Y.; Nakajima, K.; Takiguchi, S.; Mori, M.; Doki, Y. Circulating MiR-200c Levels Significantly Predict Response to Chemotherapy and Prognosis of Patients Undergoing Neoadjuvant Chemotherapy for Esophageal Cancer. Ann. Surg. Oncol. 2013, 20, 607–615. [Google Scholar] [CrossRef]
- Komatsu, S.; Ichikawa, D.; Kawaguchi, T.; Miyamae, M.; Okajima, W.; Ohashi, T.; Imamura, T.; Kiuchi, J.; Konishi, H.; Shiozaki, A.; et al. Circulating MiR-21 as an Independent Predictive Biomarker for Chemoresistance in Esophageal Squamous Cell Carcinoma. Am. J. Cancer Res. 2016, 6, 1511–1523. [Google Scholar]
- MIR193B Gene—GeneCards | MIR193B RNA Gene. Available online: https://www.genecards.org/cgi-bin/carddisp.pl?gene=MIR193B (accessed on 15 December 2020).
- Ko, M.A.; Zehong, G.; Virtanen, C.; Guindi, M.; Waddell, T.K.; Keshavjee, S.; Darling, G.E. MicroRNA Expression Profiling of Esophageal Cancer Before and After Induction Chemoradiotherapy. Ann. Thorac. Surg. 2012, 94, 1094–1103. [Google Scholar] [CrossRef]
- Odenthal, M.; Bollschweiler, E.; Grimminger, P.P.; Schröder, W.; Brabender, J.; Drebber, U.; Hölscher, A.H.; Metzger, R.; Vallböhmer, D. MicroRNA Profiling in Locally Advanced Esophageal Cancer Indicates a High Potential of MiR-192 in Prediction of Multimodality Therapy Response. Int. J. Cancer 2013, 133, 2454–2463. [Google Scholar] [CrossRef]
- Hummel, R.; Sie, C.; Watson, D.I.; Wang, T.; Ansar, A.; Michael, M.Z.; Van der Hoek, M.; Haier, J.; Hussey, D.J. MicroRNA Signatures in Chemotherapy Resistant Esophageal Cancer Cell Lines. World J. Gastroenterol. WJG 2014, 20, 14904–14912. [Google Scholar] [CrossRef]
- Hiyoshi, Y.; Kamohara, H.; Karashima, R.; Sato, N.; Imamura, Y.; Nagai, Y.; Yoshida, N.; Toyama, E.; Hayashi, N.; Watanabe, M.; et al. MicroRNA-21 Regulates the Proliferation and Invasion in Esophageal Squamous Cell Carcinoma. Clin. Cancer Res. 2009, 15, 1915–1922. [Google Scholar] [CrossRef]
- Mahawongkajit, P.; Tomtitchong, P. Expression of MiRNA in 5-FU Resistant Esophageal Cancer. Mol. Clin. Oncol. 2020, 13, 221–227. [Google Scholar] [CrossRef]
- Longley, D.B.; Harkin, D.P.; Johnston, P.G. 5-Fluorouracil: Mechanisms of Action and Clinical Strategies. Nat. Rev. Cancer 2003, 3, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Kozak, J.; Jonak, K.; Maciejewski, R. The Function of MiR-200 Family in Oxidative Stress Response Evoked in Cancer Chemotherapy and Radiotherapy. Biomed. Pharmacother. 2020, 125, 110037. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.A.; Walker, R.C.; Lloyd, M.A.; Grace, B.L.; van Boxel, G.I.; Kingma, B.F.; Ruurda, J.P.; van Hillegersberg, R.; Harris, S.; Parsons, S.; et al. Machine Learning to Predict Early Recurrence after Oesophageal Cancer Surgery. Br. J. Surg. 2020, 107, 1042–1052. [Google Scholar] [CrossRef] [PubMed]
- Pilonis, N.D.; Killcoyne, S.; Tan, W.K.; O’Donovan, M.; Malhotra, S.; Tripathi, M.; Miremadi, A.; Debiram-Beecham, I.; Evans, T.; Phillips, R.; et al. Use of a Cytosponge Biomarker Panel to Prioritise Endoscopic Barrett’s Oesophagus Surveillance: A Cross-Sectional Study Followed by a Real-World Prospective Pilot. Lancet Oncol. 2022, 23, 270–278. [Google Scholar] [CrossRef]
- Drucker, E.; Krapfenbauer, K. Pitfalls and Limitations in Translation from Biomarker Discovery to Clinical Utility in Predictive and Personalised Medicine. EPMA J. 2013, 4, 7. [Google Scholar] [CrossRef]
- Brown, R.A.M.; Epis, M.R.; Horsham, J.L.; Kabir, T.D.; Richardson, K.L.; Leedman, P.J. Total RNA Extraction from Tissues for MicroRNA and Target Gene Expression Analysis: Not All Kits Are Created Equal. BMC Biotechnol. 2018, 18, 16. [Google Scholar] [CrossRef]
- Moldovan, L.; Batte, K.E.; Trgovcich, J.; Wisler, J.; Marsh, C.B.; Piper, M. Methodological Challenges in Utilizing MiRNAs as Circulating Biomarkers. J. Cell. Mol. Med. 2014, 18, 371–390. [Google Scholar] [CrossRef]
- Atarod, S.; Smith, H.; Dickinson, A.; Wang, X.-N. MicroRNA Levels Quantified in Whole Blood Varies from PBMCs. F1000Research 2014, 3, 183. [Google Scholar] [CrossRef]
- Jiang, W.; de Jong, J.M.; van Hillegersberg, R.; Read, M. Predicting Response to Neoadjuvant Therapy in Oesophageal Adenocarcinoma. Cancers 2022, 14, 996. [Google Scholar] [CrossRef]
- Li, F.; Lv, J.-H.; Liang, L.; Wang, J.; Li, C.-R.; Sun, L.; Li, T. Downregulation of MicroRNA-21 Inhibited Radiation-Resistance of Esophageal Squamous Cell Carcinoma. Cancer Cell Int. 2018, 18, 39. [Google Scholar] [CrossRef] [PubMed]
- Nouraee, N.; Van Roosbroeck, K.; Vasei, M.; Semnani, S.; Samaei, N.M.; Naghshvar, F.; Omidi, A.A.; Calin, G.A.; Mowla, S.J. Expression, Tissue Distribution and Function of MiR-21 in Esophageal Squamous Cell Carcinoma. PLoS ONE 2013, 8, e73009. [Google Scholar] [CrossRef] [PubMed]
- Kestens, C.; Siersema, P.D.; van Baal, J.W. Current Understanding of the Functional Roles of Aberrantly Expressed MicroRNAs in Esophageal Cancer. World J. Gastroenterol. 2016, 22, 1–7. [Google Scholar] [CrossRef]
- Ourô, S.; Mourato, C.; Velho, S.; Cardador, A.; Ferreira, M.P.; Albergaria, D.; Castro, R.E.; Maio, R.; Rodrigues, C.M.P. Potential of MiR-21 to Predict Incomplete Response to Chemoradiotherapy in Rectal Adenocarcinoma. Front. Oncol. 2020, 10, 2212. [Google Scholar] [CrossRef]
- Liu, B.; Su, F.; Lv, X.; Zhang, W.; Shang, X.; Zhang, Y.; Zhang, J. Serum MicroRNA-21 Predicted Treatment Outcome and Survival in HER2-Positive Breast Cancer Patients Receiving Neoadjuvant Chemotherapy Combined with Trastuzumab. Cancer Chemother. Pharmacol. 2019, 84, 1039–1049. [Google Scholar] [CrossRef]
- Fang, Z.; Li, C.; Li, S. MicroRNA-193b Acts as a Tumor Suppressor in Colon Cancer Progression via Targeting RAB22A. Exp. Ther. Med. 2019, 17, 3921–3928. [Google Scholar] [CrossRef]
- Nyhan, M.J.; O’Donovan, T.R.; Boersma, A.W.M.; Wiemer, E.A.C.; McKenna, S.L. MiR-193b Promotes Autophagy and Non-Apoptotic Cell Death in Oesophageal Cancer Cells. BMC Cancer 2016, 16, 101. [Google Scholar] [CrossRef]
- Czochor, J.R.; Glazer, P.M. MicroRNAs in Cancer Cell Response to Ionizing Radiation. Antioxid. Redox Signal. 2014, 21, 293–312. [Google Scholar] [CrossRef]
- Sulaiman, S.A.; Ab Mutalib, N.-S.; Jamal, R. MiR-200c Regulation of Metastases in Ovarian Cancer: Potential Role in Epithelial and Mesenchymal Transition. Front. Pharmacol. 2016, 7, 271. [Google Scholar] [CrossRef]
- Smith, C.M.; Watson, D.I.; Leong, M.P.; Mayne, G.C.; Michael, M.Z.; Wijnhoven, B.P.; Hussey, D.J. MiR-200 Family Expression Is Downregulated upon Neoplastic Progression of Barrett’s Esophagus. World J. Gastroenterol. WJG 2011, 17, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Hamano, R.; Miyata, H.; Yamasaki, M.; Kurokawa, Y.; Hara, J.; Moon, J.H.; Nakajima, K.; Takiguchi, S.; Fujiwara, Y.; Mori, M.; et al. Overexpression of MiR-200c Induces Chemoresistance in Esophageal Cancers Mediated Through Activation of the Akt Signaling Pathway. Clin. Cancer Res. 2011, 17, 3029–3038. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, T.; Nishizuka, S.S.; Ishida, K.; Endo, F.; Katagiri, H.; Kume, K.; Ikeda, M.; Koeda, K.; Wakabayashi, G. Evaluation of Chemosensitivity Prediction Using Quantitative Dose–Response Curve Classification for Highly Advanced/Relapsed Gastric Cancer. World J. Surg. Oncol. 2013, 11, 11. [Google Scholar] [CrossRef] [PubMed]
| Authors | Sample Size (N) | Gender M, F (N (%)) | Age (Years); Median (Range) | Cancer Type (Storage) | Pre-Treatment Stage | NAT Regimen | miRNA Quantification Method | Key Results of Predictive miRNA Expression in Responders |
|---|---|---|---|---|---|---|---|---|
| Bibby et al. (2015) [49] | 18 | 16/18 (89) 2/18 (11) | 65 (37–75) | OAC (Frozen) | Tis–T4 N0–N1 Mx–M0 | nCRT: Cisplatin and 5-FU 1.87 Gy/min | qPCR | ↑ miR-330-5p miR-330-5p downregulated in non—responders Responders = Pt with TRG 1-2 |
| Ilhan–mutlu et al. (2015) [52] | 36 | 32/36 (89) 4/26 (11) | * 62 ± 9 | OAC (FFPE) | Not specified | nChemo only: Docetaxel (n = 8) Mitomycin/Cisplatin/5-FU (n = 8) Cisplatin/5-FU (n = 10) Epirubicin/Oxaliplatin/Capecitabine (n = 1) Others (n = 6) | RT-qPCR | No predictive value miR-21 and miR-148a not associated with response prediction pCR = Mandards TRG 1 |
| Lynam–lennon et al. (2016) [50] | 18 | 16/18 (89) 2/18 (11) | * 63 (37–75) | OAC (Frozen) | Stage IIa, IIb and III | nCRT: Cisplatin and 5-FU 40.05 Gy in 15 daily fractions | TaqMan miRNA assay RT-PCR | ↑ miR-187 miR-187 expression significantly decreased in pre-treatment biopsies in responders Responders = Pt with TRG 1-2 |
| Lynam–lennon et al. (2012) [51] | 19 | 17/19 (89) 2/19 (11) | * 63 (37–75) | OAC (Frozen) | Stage IIa, IIb and III | nCRT: Cisplatin and 5-FU 40.05 Gy in 15 daily fractions | TaqMan miRNA assay qPCR | ↑ miR-31 miR-31 expression is significantly higher in good responders. ‘Good’ responders = Pt with TRG 1-2 |
| Skinner et al. (2014) [45] | Discovery cohort 10 Model Cohort 43 Validation Cohort 65 | Discovery cohort 9/10 (90) 1/10 (10) Model Cohort 40/43 (93) 3/43 (7) Validation Cohort M = 63/65 (97) F = 2/65 (3) | Not specified | OAC | Stage II, III and IV | nCRT: Cisplatin and 5-FU 50.4 Gy total dose | Taqman array Fluidigm array Illumina array | ↓ miR-505 ↓ miR-99b ↓ miR-451 ↓ miR-145 miR-505/99b/451/145 all showed reduced expression in tumour specimens patients achieving pCR pCR = Complete absence of tumour cells in resected specimen |
| Authors | Sample Size (N) | Gender M, F (N (%)) | Age (Years); Median (Range) | Cancer Type (Storage) | Pre-Treatment Stage | NAT Regimen | miRNA Quantification Method | Key Results of Predictive miRNAs in Responders |
|---|---|---|---|---|---|---|---|---|
| Chan C et al. (2017) [54] | 47 | 44/47 (94) 3/47 (6) | 44–82 | OSCC | T1–4 N0–N1 M0–M1 | nCRT Cisplatin and 5-FU 40 Gy at 2 Gy per fraction | TaqMan Low Density Array RT-PCR | ↑ miR-193b High pre-treatment serum miR-193b associated with pCR pCR = Pt with 0% viable tumour cells. |
| Han et al. (2019) [55] | 104 | 93/104 (89) 11/104 (11) | 21 Pt ≤ 55 yrs 83 Pt > 55 yrs | OSCC | T1–4 N0–N3 M0–M1 | nCRT Cisplatin and 5-FU [Radiation dose not specified] | RT-qPCR | ↑ miR-338-5p High pre-treatment serum miR-338-5p predicts pCR pCR = Pt with JES Grade 1 (ypT0N0M0) |
| Komatsu et al. (2016) [56] | 37 | 30/37 (81) 7/37 (19) | 19 Pt < 65 yrs 18 Pt ≥ 65 yrs | OSCC | Stage I, II, III and IV | nChemo only Cisplatin and 5-FU | Toray® 3D-Gene miRNA array RT-PCR | ↓ miR-23a Pre-treatment plasma concentrations of miR-21 were significantly higher in Pt with a low pathological response. Low histopathological response = Pt with JES system TRG 0-1a |
| Komatsu et al. (2016) [60] | 37 | 30/37 (93) 7/37 (19) | 19 Pt < 65 yrs 18 Pt ≥ 65 yrs | OSCC | cT0-4 cN0-3 CM0-1 | nChemo only Cisplatin and 5-FU | RT-PCR | ↑ miR-21 Expression significantly higher in Pt with low histopathological response Low response = JES TRG 0-1a |
| Kurashige et al. (2012) [57] | 71 | 66/71 (93) 5/71 (7) | 35 Pt < 70 yrs 36 Pt ≥ 70 yrs | OSCC | Stage I, II, III and IV | nChemo only Docetaxel/Cisplatin/ 5-FU (DCF) (n = 38) Others (n = 33) | TaqMan microRNAs assay qRT-PCR | ↓ miR-21 Significant decrease in serum miR-21 was noted in the responders during nChemo. pCR = According to RECIST 1.0 criteria, disappearance of all tumour lesions |
| Niwa et al. (2019) [58] | 84 | 70/84 (83) 14/84 (17) | 65 (30–77) | OSCC | pT0-4 pN0–3 pM0-1 | nChemo only Cisplatin plus 5FU or S-1. | Toray 3D-Gene miRNA array RT-PCR | ↓ miR-193b-5p ↓ miR-873-3p Pre-treatment serum expression of miR-193b-5p and miR-873-3p were significantly higher in non-responders Responders = Pt with JES Grade 2-3 |
| Tanaka et al. (2013) [59] | 64 | M = 49/64 (77) F = 15/64 (23) | (67.5) 45–80 | OSCC | Stage II, III and IV | nChemo only Adriamycin, Cisplatin and 5-fluorouracil (ACF) OR Docetaxel, Cisplatin and 5-fluorouracil (DCF) | TaqMan Array qPCR | ↓ miR-200c Pre-treatment serum levels of miR-200c were significantly lower in responders pCR = Total regression of the tumour |
| Wen et al. (2016) [53] | 106 | M = 90/106 (85) F = 16/106 (15) | 55 49 Pt < 55 yrs; 57 Pt ≥ 55 yrs | OSCC (Frozen and FFPE) | Stage IIB and III | nCRT only | qPCR | ↑ miR-193b-3p ↓ miR-152 ↓ miR-145-5p ↓ miR-376a-3p miR-193-3p was downregulated in pre-treatment biopsies of non-responders. miR-152/145-5p/376a-3p were upregulated in non-responders pCR = 0% residual cancer |
| Authors | Sample Size (N) | Gender M, F (N (%)) | Age (Years); Median | Cancer Type (Storage) | Pre-Treatment Stage | NAT Regimen | miRNA Quantification Method | Key Results of Predictive miRNAs in Responders |
|---|---|---|---|---|---|---|---|---|
| Ko et al. (2012) [62] | 25 | Not specified | Not specified | OAC (FFPE) 80% OSCC (FFPE) 20% | T1N1M0 or T2-3N0-1 | nCRT Cisplatin and Irinotecan 50.4 Gy | Illumina miRNA BeOAChip microarray | ↓ miR-296 ↑ miR-141 Pre-treatment specimen levels of miR-296 were significantly lower in Pt achieving pCR. Pre-treatment levels of miR-141 were upregulated in Pt achieving pCR. pCR = 0% viable tumour cells remaining. |
| Odenthal et al. (2013) [63] | 80 | M = 68/80 (85) F = 12/80 (15) | 59 | OSCC (FFPE) 47.5% OAC (FFPE) 52.5% | Not specified | nCRT Cisplatin and 5-FU 40 Gy dose total | TaqManVR Human microRNAs Array RT–P|CR | ↑ miR-192 ↑ miR-194 Pretherapeutic intratumoral expression of miR-192 and miR-194 was higher in major responders. Major response = CRG Grades III and IV |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lang, C.C.J.; Lloyd, M.; Alyacoubi, S.; Rahman, S.; Pickering, O.; Underwood, T.; Breininger, S.P. The Use of miRNAs in Predicting Response to Neoadjuvant Therapy in Oesophageal Cancer. Cancers 2022, 14, 1171. https://doi.org/10.3390/cancers14051171
Lang CCJ, Lloyd M, Alyacoubi S, Rahman S, Pickering O, Underwood T, Breininger SP. The Use of miRNAs in Predicting Response to Neoadjuvant Therapy in Oesophageal Cancer. Cancers. 2022; 14(5):1171. https://doi.org/10.3390/cancers14051171
Chicago/Turabian StyleLang, Cameron C. J., Megan Lloyd, Said Alyacoubi, Saqib Rahman, Oliver Pickering, Tim Underwood, and Stella P. Breininger. 2022. "The Use of miRNAs in Predicting Response to Neoadjuvant Therapy in Oesophageal Cancer" Cancers 14, no. 5: 1171. https://doi.org/10.3390/cancers14051171
APA StyleLang, C. C. J., Lloyd, M., Alyacoubi, S., Rahman, S., Pickering, O., Underwood, T., & Breininger, S. P. (2022). The Use of miRNAs in Predicting Response to Neoadjuvant Therapy in Oesophageal Cancer. Cancers, 14(5), 1171. https://doi.org/10.3390/cancers14051171








