Current Knowledge on Spinal Meningiomas Epidemiology, Tumor Characteristics and Non-Surgical Treatment Options: A Systematic Review and Pooled Analysis (Part 1)
Abstract
Simple Summary
Abstract
1. Introduction
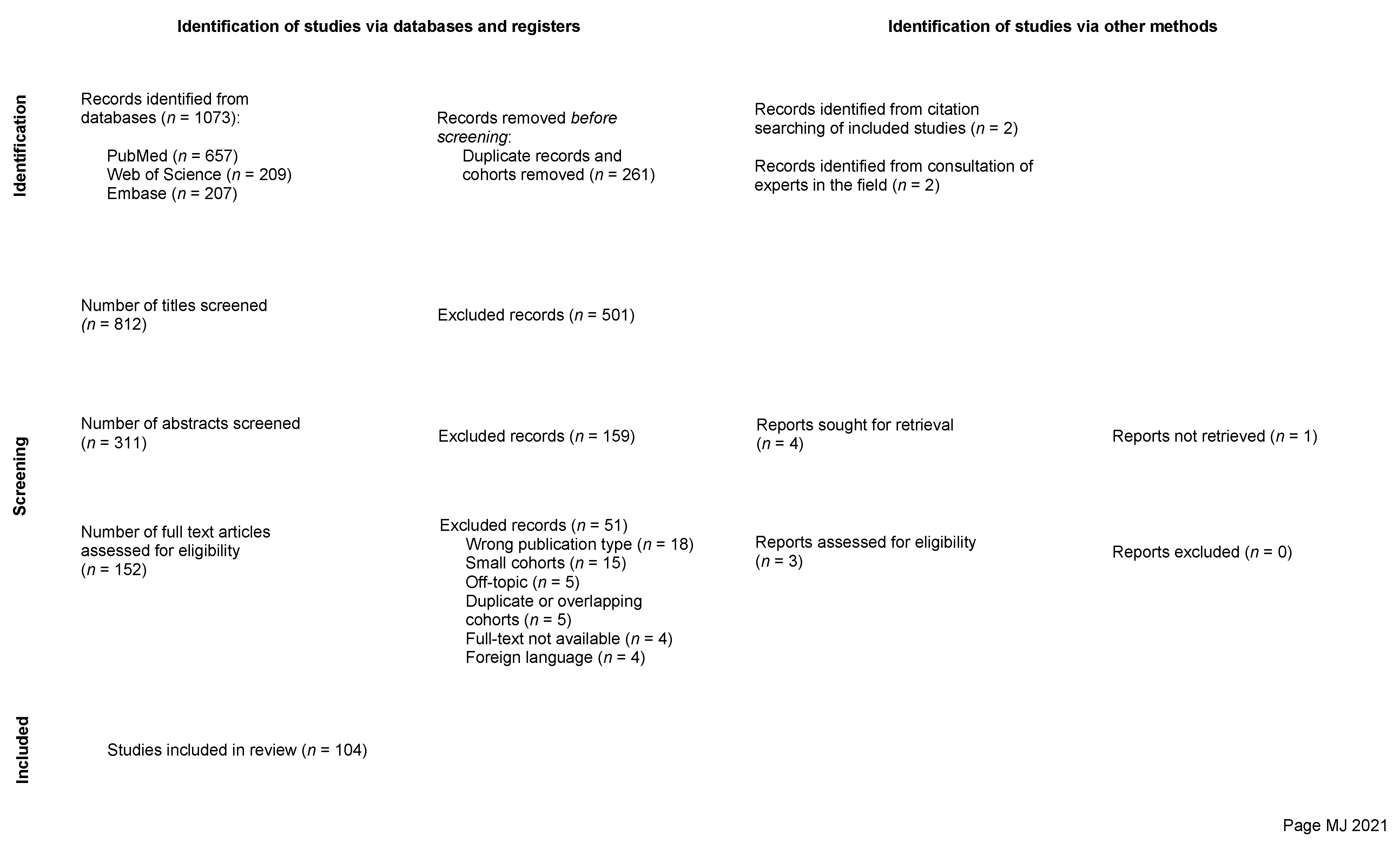
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Databases and Search Strategy
2.3. Study Selection
2.4. Data Extraction
2.5. Individual Evidence Level and Risk of Bias Assessment
2.6. Data Synthesis, Analysis, and Statistics
3. Results and Discussion
3.1. Epidemiology
3.1.1. Sex
3.1.2. Age
3.1.3. Racial Distribution and Interregional Variability
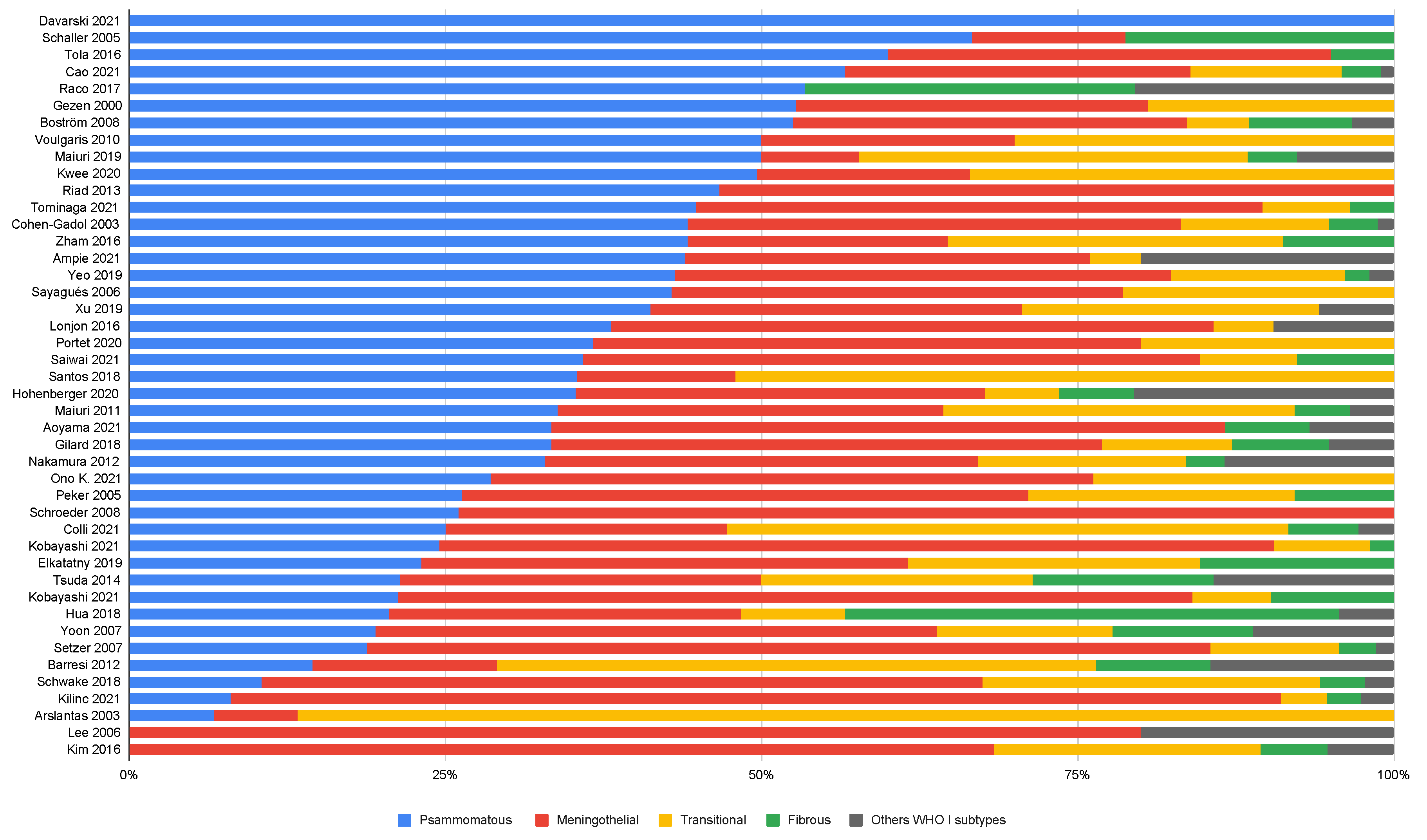
3.2. Histopathology
3.2.1. WHO Grade 1
3.2.2. WHO Grade 2 and 3
3.2.3. Age and WHO Grade
3.3. Tumor Biology
3.3.1. Genomics of Spinal Meningiomas
3.3.2. Receptor Expression
3.3.3. MIB-Index
3.3.4. Neurofibromatosis Type 2 and Other Genetic Conditions
3.4. Tumor Location and Shape
3.4.1. Craniocaudal and Axial Tumor Locations
3.4.2. Dumbbell Formation
3.5. Tumor Presentation
3.5.1. Presenting Symptoms and Symptom Duration
3.5.2. Correlation of Specific Symptoms with Location and Other Factors
3.5.3. Degree of Tumor Compression and Correlation to Symptoms
3.6. Radiological Diagnosis
3.6.1. General Radiological Features and Findings Described
3.6.2. Calcification of Spinal Meningioma
3.6.3. Differences and Similarities between Spinal Meningiomas and Schwannomas
3.7. Non-Surgical Primary, Adjuvant, or Salvage Therapy
3.7.1. Use and Trends Related to Non-Surgical Treatments
3.7.2. Benefits and Risks Associated with Radiotherapy
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ogasawara, C.; Philbrick, B.D.; Adamson, D.C. Meningioma: A Review of Epidemiology, Pathology, Diagnosis, Treatment, and Future Directions. Biomedicines 2021, 9, 319. [Google Scholar] [CrossRef] [PubMed]
- Kshettry, V.R.; Hsieh, J.K.; Ostrom, Q.T.; Kruchko, C.; Benzel, E.C.; Barnholtz-Sloan, J.S. Descriptive Epidemiology of Spinal Meningiomas in the United States. Spine 2015, 40, E886–E889. [Google Scholar] [CrossRef] [PubMed]
- Maiti, T.K.; Bir, S.C.; Patra, D.P.; Kalakoti, P.; Guthikonda, B.; Nanda, A. Spinal Meningiomas: Clinicoradiological Factors Predicting Recurrence and Functional Outcome. Neurosurg. Focus 2016, 41, E6. [Google Scholar] [CrossRef] [PubMed]
- Pettersson-Segerlind, J.; Fletcher-Sandersjöö, A.; Tatter, C.; Burström, G.; Persson, O.; Förander, P.; Mathiesen, T.; Bartek, J., Jr.; Edström, E.; Elmi-Terander, A. Long-Term Follow-Up and Predictors of Functional Outcome after Surgery for Spinal Meningiomas: A Population-Based Cohort Study. Cancers 2021, 13, 3244. [Google Scholar] [CrossRef]
- Westwick, H.J.; Shamji, M.F. Effects of Sex on the Incidence and Prognosis of Spinal Meningiomas: A Surveillance, Epidemiology, and End Results Study. J. Neurosurg. Spine 2015, 23, 368–373. [Google Scholar] [CrossRef]
- Hua, L.; Zhu, H.; Deng, J.; Tian, M.; Jiang, X.; Tang, H.; Luan, S.; Wakimoto, H.; Xie, Q.; Gong, Y. Clinical and Prognostic Features of Spinal Meningioma: A Thorough Analysis from a Single Neurosurgical Center. J. Neurooncol. 2018, 140, 639–647. [Google Scholar] [CrossRef]
- El-Hajj, V.G.; Fletcher-Sandersjöö, A.; Pettersson-Segerlind, J.; Edström, E.; Elmi-Terander, A. Unsuccessful External Validation of the MAC-Score for Predicting Increased MIB-1 Index in Patients with Spinal Meningiomas. Front. Oncol. 2022, 12, 6749. [Google Scholar] [CrossRef]
- Cohen-Gadol, A.A.; Zikel, O.M.; Koch, C.A.; Scheithauer, B.W.; Krauss, W.E. Spinal Meningiomas in Patients Younger than 50 Years of Age: A 21-Year Experience. J. Neurosurg. 2003, 98, 258–263. [Google Scholar] [CrossRef]
- Maiuri, F.; Mariniello, G.; de Divitiis, O.; Esposito, F.; Guadagno, E.; Teodonno, G.; Barbato, M.; del Basso De Caro, M. Progesterone Receptor Expression in Meningiomas: Pathological and Prognostic Implications. Front. Oncol. 2021, 11, 2585. [Google Scholar] [CrossRef]
- Yang, X.; Liu, F.; Zheng, J.; Cheng, W.; Zhao, C.; Di, J. Relationship Between Oral Contraceptives and the Risk of Gliomas and Meningiomas: A Dose-Response Meta-Analysis and Systematic Review. World Neurosurg. 2021, 147, e148–e162. [Google Scholar] [CrossRef]
- Antolínez Ayala, V.E.; García Arias, M.D.; Bautista Vargas, S.E.; Báez Cárdenas, L.M.; Castellanos Peñaranda, C. Paraplegia Due to Spinal Meningioma during the Third Trimester of Pregnancy: Case Report and Literature Review. Spinal Cord Ser. Cases 2021, 7, 31. [Google Scholar] [CrossRef] [PubMed]
- Hortobágyi, T.; Bencze, J.; Murnyák, B.; Kouhsari, M.C.; Bognár, L.; Marko-Varga, G. Pathophysiology of Meningioma Growth in Pregnancy. Open Med. 2017, 12, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Pettersson-Segerlind, J.; Mathiesen, T.; Elmi-Terander, A.; Edström, E.; Talbäck, M.; Feychting, M.; Tettamanti, G. The Risk of Developing a Meningioma during and after Pregnancy. Sci. Rep. 2021, 11, 9153. [Google Scholar] [CrossRef] [PubMed]
- Abul-Kasim, K.; Thurnher, M.M.; McKeever, P.; Sundgren, P.C. Intradural Spinal Tumors: Current Classification and MRI Features. Neuroradiology 2008, 50, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Watts, J.; Box, G.; Galvin, A.; Brotchie, P.; Trost, N.; Sutherland, T. Magnetic Resonance Imaging of Meningiomas: A Pictorial Review. Insights Imaging 2014, 5, 113–122. [Google Scholar] [CrossRef]
- Kondziolka, D.; Nathoo, N.; Flickinger, J.C.; Niranjan, A.; Maitz, A.H.; Lunsford, L.D.; Piepmeier, J.M.; Berger, M.S.; Loeffler, J.S.; Gutin, P.H. Long-Term Results after Radiosurgery for Benign Intracranial Tumors. Neurosurgery 2003, 53, 815–822. [Google Scholar] [CrossRef]
- Tatter, C.; Fletcher-Sandersjöö, A.; Persson, O.; Burström, G.; Grane, P.; Edström, E.; Elmi-Terander, A. Incidence and Predictors of Kyphotic Deformity Following Resection of Cervical Intradural Tumors in Adults: A Population-Based Cohort Study. Acta Neurochir. 2020, 162, 2905–2913. [Google Scholar] [CrossRef]
- Viereck, M.J.; Ghobrial, G.M.; Beygi, S.; Harrop, J.S. Improved Patient Quality of Life Following Intradural Extramedullary Spinal Tumor Resection. J. Neurosurg. Spine 2016, 25, 640–645. [Google Scholar] [CrossRef]
- El-Hajj, V.G.; Pettersson Segerlind, J.; Burström, G.; Edström, E.; Elmi-Terander, A. Current Knowledge on Spinal Meningiomas: A Systematic Review Protocol. BMJ Open 2022, 12, e061614. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.G.; Swiontkowski, M.F.; Heckman, J.D. Introducing Levels of Evidence to the Journal. J. Bone Jt. Surg. Am. 2003, 85, 1–3. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Pereson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 24 July 2022).
- Lasserson, T.J.; Thomas, J.; Higgins, J.P.T. Chapter 1: Starting a Review. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2021; Available online: www.Training.Cochrane.Org/Handbook (accessed on 10 June 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing; R Core Team: Vienna, Austria, 2020; Available online: https://www.r-project.org/ (accessed on 10 June 2022).
- Morandi, X.; Haegelen, C.; Riffaud, L.; Amlashi, S.; Adn, M.; Brassier, G. Results in the Operative Treatment of Elderly Patients with Spinal Meningiomas. Spine 2004, 29, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Iacoangeli, M.; Gladi, M.; Di Rienzo, A.; Dobran, M.; Alvaro, L.; Nocchi, N.; Maria, L.G.; Somma, D.; Colasanti, R.; Scerrati, M. Minimally Invasive Surgery for Benign Intradural Extramedullary Spinal Meningiomas: Experience of a Single Institution in a Cohort of Elderly Patients and Review of the Literature. Clin. Interv. Aging 2012, 7, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Sacko, O.; Haegelen, C.; Mendes, V.; Brenner, A.; Sesay, M.; Brauge, D.; Lagarrigue, J.; Loiseau, H.; Roux, F.E. Spinal Meningioma Surgery in Elderly Patients with Paraplegia or Severe Paraparesis: A Multicenter Study. Neurosurgery 2009, 64, 503–509; discussion 509–510. [Google Scholar] [CrossRef]
- Ambekar, S.; Sharma, M.; Kukreja, S.; Nanda, A. Complications and Outcomes of Surgery for Spinal Meningioma: A Nationwide Inpatient Sample Analysis from 2003 to 2010. Clin. Neurol. Neurosurg. 2014, 118, 65–68. [Google Scholar] [CrossRef]
- Wang, X.Q.; Zeng, X.W.; Zhang, B.Y.; Dou, Y.F.; Wu, J.S.; Jiang, C.C.; Zhong, P.; Chen, H. Spinal Meningioma in Childhood: Clinical Features and Treatment. Childs Nerv. Syst. 2012, 28, 129–136. [Google Scholar] [CrossRef]
- Wu, L.; Yang, C.; Liu, T.; Fang, J.; Yang, J.; Xu, Y. Clinical Features and Long-Term Outcomes of Pediatric Spinal Meningiomas. J. Neurooncol. 2017, 133, 347–355. [Google Scholar] [CrossRef]
- Cao, Y.; Jiang, Y.; Liu, C.; Jin, R.; Jin, Z.; Hong, X.; Zhao, L.; Zhao, G.; Wang, Y. Epidemiology and Survival of Patients with Spinal Meningiomas: A {SEER} Analysis. Eur. J. Surg. Oncol. 2021, 47, 2340–2345. [Google Scholar] [CrossRef]
- Sahm, F.; Reuss, D.E.; Giannini, C. WHO 2016 Classification: Changes and Advancements in the Diagnosis of Miscellaneous Primary CNS Tumours. Neuropathol. Appl. Neurobiol. 2018, 44, 163–171. [Google Scholar] [CrossRef]
- Maiuri, F.; De Caro, M.D.B.; de Divitiis, O.; Vergara, P.; Mariniello, G. Spinal Meningiomas: Age-Related Features. Clin. Neurol. Neurosurg. 2011, 113, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, S.; Wang, Q.; Cheng, J.; Deng, X.; Wang, Y.; Hui, X. Spinal Clear Cell Meningioma: Clinical Study with Long-Term Follow-Up in 12 Patients. World Neurosurg. 2019, 122, e415–e426. [Google Scholar] [CrossRef] [PubMed]
- Krauss, W.E.; Yolcu, Y.U.; Alvi, M.A.; Moinuddin, F.M.; Goyal, A.; Clarke, M.J.; Marsh, W.R.; Bydon, M. Clinical Characteristics and Management Differences for Grade II and III Spinal Meningiomas. J. Neurooncol. 2021, 153, 313–320. [Google Scholar] [CrossRef]
- Ye, J.; Lv, G.; Qian, J.; Zhu, J.; Han, R.; Luo, C. Clinical Features and Prognostic Factors of WHO II and III Adult Spinal Meningiomas: Analysis of 25 Cases in a Single Center. J. Neurooncol. 2016, 128, 349–356. [Google Scholar] [CrossRef]
- Noh, S.H.; Kim, K.H.; Shin, D.A.; Park, J.Y.; Yi, S.; Kuh, S.U.; Kim, K.N.; Chin, D.K.; Kim, K.S.; Yoon, D.H.; et al. Treatment Outcomes of 17 Patients with Atypical Spinal Meningioma, Including 4 with Metastases: A Retrospective Observational Study. Spine J. 2019, 19, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Sayagués, J.M.; Tabernero, M.D.; Maíllo, A.; Trelles, O.; Espinosa, A.B.; Sarasquete, M.E.; Merino, M.; Rasillo, A.; Vera, J.F.; Santos-Briz, A.; et al. Microarray-Based Analysis of Spinal versus Intracranial Meningiomas: Different Clinical, Biological, and Genetic Characteristics Associated with Distinct Patterns of Gene Expression. J. Neuropathol. Exp. Neurol. 2006, 65, 445–454. [Google Scholar] [CrossRef]
- Arslantas, A.; Artan, S.; Oner, U.; Durmaz, R.; Müslümanoglu, H.; Atasoy, M.A.; Başaran, N.; Tel, E. Detection of Chromosomal Imbalances in Spinal Meningiomas by Comparative Genomic Hybridization. Neurol. Med. Chir. 2003, 43, 12–18; discussion 19. [Google Scholar] [CrossRef] [PubMed]
- Barresi, V.; Alafaci, C.; Caffo, M.; Barresi, G.; Tuccari, G. Clinicopathological Characteristics, Hormone Receptor Status and Matrix Metallo-Proteinase-9 (MMP-9) Immunohistochemical Expression in Spinal Meningiomas. Pathol. Res. Pract. 2012, 208, 350–355. [Google Scholar] [CrossRef]
- Smith, M.J.; O’Sullivan, J.; Bhaskar, S.S.; Hadfield, K.D.; Poke, G.; Caird, J.; Sharif, S.; Eccles, D.; Fitzpatrick, D.; Rawluk, D.; et al. Loss-of-Function Mutations in SMARCE1 Cause an Inherited Disorder of Multiple Spinal Meningiomas. Nat. Genet. 2013, 45, 295–298. [Google Scholar] [CrossRef]
- Smith, M.J.; Wallace, A.J.; Bennett, C.; Hasselblatt, M.; Elert-Dobkowska, E.; Evans, L.T.; Hickey, W.F.; van Hoff, J.; Bauer, D.; Lee, A.; et al. Germline SMARCE1 Mutations Predispose to Both Spinal and Cranial Clear Cell Meningiomas. J. Pathol. 2014, 234, 436–440. [Google Scholar] [CrossRef]
- Karsy, M.; Guan, J.; Sivakumar, W.; Neil, J.A.; Schmidt, M.H.; Mahan, M.A. The Genetic Basis of Intradural Spinal Tumors and Its Impact on Clinical Treatment. Neurosurg. Focus 2015, 39, E3. [Google Scholar] [CrossRef] [PubMed]
- Shu, J.; Lee Joung, H.; Harwalkar, J.A.; Oh-Siskovic, S.; Stacey, D.W.; Golubic, M. Adenovirus-Mediated Gene Transfer of Dominant Negative Ha-Ras Inhibits Proliferation of Primary Meningioma Cells. Neurosurgery 1999, 44, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Tummalapalli, P.; Spomar, D.; Gondi, C.S.; Olivero, W.C.; Gujrati, M.; Dinh, D.H.; Rao, J.S. RNAi-Mediated Abrogation of Cathepsin B and MMP-9 Gene Expression in a Malignant Meningioma Cell Line Leads to Decreased Tumor Growth, Invasion and Angiogenesis. Int. J. Oncol. 2007, 31, 1039–1050. [Google Scholar] [CrossRef]
- Dey, M.; Auffinger, B.; Lesniak, M.S.; Ahmed, A.U. Antiglioma Oncolytic Virotherapy: Unattainable Goal or a Success Story in the Making? Futur. Virol. 2013, 8, 675–693. [Google Scholar] [CrossRef] [PubMed]
- De La Garza-Ramos, R.; Flores-Rodríguez, J.V.; Martínez-Gutiérrez, J.C.; Ruiz-Valls, A.; Caro-Osorio, E. Current Standing and Frontiers of Gene Therapy for Meningiomas. Neurosurg. Focus 2013, 35, E4. [Google Scholar] [CrossRef]
- Hawasli, A.H.; Rubin, J.B.; Tran, D.D.; Adkins, D.R.; Waheed, S.; Hullar, T.E.; Gutmann, D.H.; Evans, J.; Leonard, J.R.; Zipfel, G.J.; et al. Antiangiogenic Agents for Nonmalignant Brain Tumors. J. Neurol. Surg. Part B Skull Base 2013, 74, 136–141. [Google Scholar] [CrossRef]
- Lou, E.; Sumrall, A.L.; Turner, S.; Peters, K.B.; Desjardins, A.; Vredenburgh, J.J.; McLendon, R.E.; Herndon, J.E.; McSherry, F.; Norfleet, J.; et al. Bevacizumab Therapy for Adults with Recurrent/Progressive Meningioma: A Retrospective Series. J. Neurooncol. 2012, 109, 63–70. [Google Scholar] [CrossRef]
- Nayak, L.; Iwamoto, F.M.; Rudnick, J.D.; Norden, A.D.; Lee, E.Q.; Drappatz, J.; Omuro, A.; Kaley, T.J. Atypical and Anaplastic Meningiomas Treated with Bevacizumab. J. Neurooncol. 2012, 109, 187–193. [Google Scholar] [CrossRef]
- Maiuri, F.; Mariniello, G.; Guadagno, E.; Barbato, M.; Corvino, S.; del Basso De Caro, M. WHO Grade, Proliferation Index, and Progesterone Receptor Expression Are Different According to the Location of Meningioma. Acta Neurochir. 2019, 161, 2553–2561. [Google Scholar] [CrossRef]
- Sun, S.Q.; Cai, C.; Ravindra, V.M.; Gamble, P.; Yarbrough, C.K.; Dacey, R.G.; Dowling, J.L.; Zipfel, G.J.; Wright, N.M.; Santiago, P.; et al. Simpson Grade I-III Resection of Spinal Atypical (World Health Organization Grade II) Meningiomas Is Associated With Symptom Resolution and Low Recurrence. Neurosurgery 2015, 76, 739–746. [Google Scholar] [CrossRef]
- Pemov, A.; Dewan, R.; Hansen, N.F.; Chandrasekharappa, S.C.; Ray-Chaudhury, A.; Jones, K.; Luo, W.; Heiss, J.D.; Mullikin, J.C.; Chittiboina, P.; et al. Comparative Clinical and Genomic Analysis of Neurofibromatosis Type 2-Associated Cranial and Spinal Meningiomas. Sci. Rep. 2020, 10, 12563. [Google Scholar] [CrossRef] [PubMed]
- Champeaux-Depond, C.; Penet, N.; Weller, J.; Le Huec, J.-C.; Jecko, V. Functional Outcome After Spinal Meningioma Surgery. A Nationwide Population-Based Study. Neurospine 2022, 19, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Baro, V.; Moiraghi, A.; Carlucci, V.; Paun, L.; Anglani, M.; Ermani, M.; Saladino, A.; Chioffi, F.; D’Avella, D.; Landi, A. Spinal Meningiomas: Influence of Cord Compression and Radiological Features on Preoperative Functional Status and Outcome. Cancers 2021, 13, 4183. [Google Scholar] [CrossRef]
- Yoon, S.H.; Chung, C.K.; Jahng, T.A. Surgical Outcome of Spinal Canal Meningiomas. J. Korean Neurosurg. Soc. 2007, 42, 300–304. [Google Scholar] [CrossRef] [PubMed]
- Hohenberger, C.; Gugg, C.; Schmidt, N.O.; Zeman, F.; Schebesch, K.M. Functional Outcome after Surgical Treatment of Spinal Meningioma. J. Clin. Neurosci. 2020, 77, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Ampie, L.; Snyder, M.H.; Dominguez, J.F.; Buchholz, A.; Yen, C.P.; Shaffrey, M.E.; Syed, H.R.; Shaffrey, C.I.; Smith, J.S. Clinical Characteristics and Long-Term Outcomes for Patients Who Undergo Cytoreductive Surgery for Thoracic Meningiomas: A Retrospective Analysis. Neurosurg. Focus 2021, 50, E18. [Google Scholar] [CrossRef]
- Onken, J.; Obermüller, K.; Staub-Bartelt, F.; Meyer, B.; Vajkoczy, P.; Wostrack, M. Surgical Management of Spinal Meningiomas: Focus on Unilateral Posterior Approach and Anterior Localization. J. Neurosurg. Spine 2018, 30, 308–313. [Google Scholar] [CrossRef]
- Han, B.; Zhang, L.; Jia, W.; Yang, J. Clinical Features and Surgical Outcomes of High-Grade Spinal Meningiomas: Report of 19 Cases and Literature Review. J. Clin. Neurosci. 2020, 72, 264–269. [Google Scholar] [CrossRef]
- Schaller, B. Spinal Meningioma: Relationship between Histological Subtypes and Surgical Outcome? J. Neurooncol. 2005, 75, 157–161. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Menezes, A.H.; Shimizu, K.; Woodroffe, R.W.; Helland, L.C.; Hitchon, P.W.; Howard, M.A. Differences and Characteristics of Symptoms by Tumor Location, Size, and Degree of Spinal Cord Compression: A Retrospective Study on 53 Surgically Treated, Symptomatic Spinal Meningiomas. J. Neurosurg. Spine 2020, 32, 931–940. [Google Scholar] [CrossRef]
- Postalci, L.; Tugcu, B.; Gungor, A.; Guclu, G. Spinal Meningiomas: Recurrence in Ventrally Located Individuals on Long-Term Follow-up, A Review of 46 Operated Cases. Turk. Neurosurg. 2011, 21, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Schwake, M.; Adeli, A.; Sporns, P.; Ewelt, C.; Schmitz, T.; Sicking, J.; Hess, K.; Spille, D.C.; Paulus, W.; Stummer, W.; et al. Spinal Meningiomas—Risks and Potential of an Increasing Age at the Time of Surgery. J. Clin. Neurosci. 2018, 57, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Abdelmonam Abdelaziz Mostafa Elkatatny, A.; Ramadan, M.; Gouda, A.H.; MHamdy, T.; Samir Fahmy, R.; Farid El Emady, M.; Salaheldin, A. Surgical Outcome of Spinal Meningioma, Single Institute Experience. Pharmacophore 2019, 10, 7–17. [Google Scholar]
- Setzer, M.; Vatter, H.; Marquardt, G.; Seifert, V.; Vrionis, F.D. Management of Spinal Meningiomas: Surgical Results and a Review of the Literature. Neurosurg. Focus 2007, 23, E14. [Google Scholar] [CrossRef] [PubMed]
- Davies, S.; Gregson, B.; Mitchell, P. Spinal Meningioma: Relationship between Degree of Cord Compression and Outcome. Br. J. Neurosurg. 2017, 31, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Corell, A.; Cerbach, C.; Hoefling, N.; Björkman-Burtscher, I.M.; Jakola, A.S. Spinal Cord Compression in Relation to Clinical Symptoms in Patients with Spinal Meningiomas. Clin. Neurol. Neurosurg. 2021, 211, 107018. [Google Scholar] [CrossRef]
- Ono, K.; Shimizu, T.; Fujibayashi, S.; Otsuki, B.; Murata, K.; Sakamoto, A.; Matsuda, S. Predictive Value of Heterogeneously Enhanced Magnetic Resonance Imaging Findings With Computed Tomography Evidence of Calcification for Severe Motor Deficits in Spinal Meningioma. Neurospine 2021, 18, 163–169. [Google Scholar] [CrossRef]
- Bayoumi, A.B.; Laviv, Y.; Yokus, B.; Efe, I.E.; Toktas, Z.O.; Kilic, T.; Demir, M.K.; Konya, D.; Kasper, E.M. Proposal of a New Radiological Classification System for Spinal Meningiomas as a Descriptive Tool and Surgical Guide. Clin. Neurol. Neurosurg. 2017, 162, 118–126. [Google Scholar] [CrossRef]
- Aoyama, T.; Ogiwara, T.; Ito, K.; Miyaoka, Y.; Fujii, Y.; Hanaoka, Y.; Hasegawa, T.; Watanabe, G.; Seguchi, T.; Hongo, K. Correlations Among Consistency, Computed Tomography Values, and Histopathological Subtypes of Spinal Meningioma. Acta Med. Okayama 2021, 75, 713–718. [Google Scholar]
- Ono, H.; Kumagai, G.; Wada, K.; Ono, A.; Asari, T.; Aoki, M.; Ishibashi, Y. Assessing the Utility of 18F-Fluorodeoxyglucose Positron Emission Tomography in the Differential Diagnosis Between Spinal Schwannomas and Meningiomas. Cureus 2021, 13, e18890. [Google Scholar] [CrossRef]
- Kobayashi, K.; Ando, K.; Nakashima, H.; Machino, M.; Kanbara, S.; Ito, S.; Inoue, T.; Yamaguchi, H.; Koshimizu, H.; Segi, N.; et al. Characteristics of Cases with and without Calcification in Spinal Meningiomas. J. Clin. Neurosci. 2021, 89, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Davarski, A.; Kitov, B.; Apostolov, G.; Kehayov, I.; Stoyanova, R. Correlations between Preoperative Clinical Factors and Treatment Outcome of Spinal Meningiomas—A Retrospective Study of a Series of 31 Cases. Surg. Neurol. Int. 2021, 12, 236. [Google Scholar] [CrossRef] [PubMed]
- Pompili, A.; Caroli, F.; Crispo, F.; Giovannetti, M.; Raus, L.; Vidiri, A.; Telera, S. Unilateral Laminectomy Approach for the Removal of Spinal Meningiomas and Schwannomas: Impact on Pain, Spinal Stability, and Neurologic Results. World Neurosurg. 2016, 85, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Iwata, E.; Shigematsu, H.; Yamamoto, Y.; Kawasaki, S.; Tanaka, M.; Okuda, A.; Morimoto, Y.; Masuda, K.; Koizumi, M.; Akahane, M.; et al. Preliminary Algorithm for Differential Diagnosis between Spinal Meningioma and Schwannoma Using Plain Magnetic Resonance Imaging. J. Orthop. Sci. 2018, 23, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Takashima, H.; Takebayashi, T.; Yoshimoto, M.; Onodera, M.; Terashima, Y.; Iesato, N.; Tanimoto, K.; Ogon, I.; Morita, T.; Yamashita, T. Differentiating Spinal Intradural-Extramedullary Schwannoma from Meningioma Using MRI T(2) Weighted Images. Br. J. Radiol. 2018, 91, 20180262. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, H.S.; Yoon, Y.C.; Cha, M.J.; Lee, S.H.; Kim, E.S. Differentiating between Spinal Schwannomas and Meningiomas Using MRI: A Focus on Cystic Change. PLoS ONE 2020, 15, e0233623. [Google Scholar] [CrossRef]
- Liu, W.C.; Choi, G.; Lee, S.H.; Han, H.; Lee, J.Y.; Jeon, Y.H.; Park, H.S.; Park, J.Y.; Paeng, S.S. Radiological Findings of Spinal Schwannomas and Meningiomas: Focus on Discrimination of Two Disease Entities. Eur. Radiol. 2009, 19, 2707–2715. [Google Scholar] [CrossRef]
- De Verdelhan, O.; Haegelen, C.; Carsin-Nicol, B.; Riffaud, L.; Amlashi, S.; Brassier, G.; Carsin, M.; Morandi, X. MR Imaging Features of Spinal Schwannomas and Meningiomas. J. Neuroradiol. 2005, 32, 42–49. [Google Scholar] [CrossRef]
- Yolcu, Y.U.; Goyal, A.; Alvi, M.A.; Moinuddin, F.M.; Bydon, M. Trends in the Utilization of Radiotherapy for Spinal Meningiomas: Insights from the 2004-2015 National Cancer Database. Neurosurg. Focus 2019, 46, E6. [Google Scholar] [CrossRef]
- Lee, M.E.; Hwang, Y.J.; Sohn, M.J.; Lee, B.H.; Kim, S.Y. Assessment of the Treatment Response of Spinal Meningiomas after Radiosurgery Focusing on Serial MRI Findings. Jpn. J. Radiol. 2015, 33, 547–558. [Google Scholar] [CrossRef]
- Kufeld, M.; Wowra, B.; Muacevic, A.; Zausinger, S.; Tonn, J.C. Radiosurgery of Spinal Meningiomas and Schwannomas. Technol. Cancer Res. Treat. 2012, 11, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.L.; Fujimoto, D.; Kumar, K.A.; Tupper, L.; Mansour, S.; Chang, S.D.; Adler, J.R.; Gibbs, I.C.; Hancock, S.L.; Dodd, R.; et al. Long-Term Update of Stereotactic Radiosurgery for Benign Spinal Tumors. Neurosurgery 2019, 85, 708–716. [Google Scholar] [CrossRef] [PubMed]
- Gerszten, P.C.; Burton, S.A.; Ozhasoglu, C.; McCue, K.J.; Quinn, A.E. Radiosurgery for Benign Intradural Spinal Tumors. Neurosurgery 2008, 62, 887–895. [Google Scholar] [CrossRef] [PubMed]
- Golanov, A.V.; Konovalov, N.A.; Antipina, N.A.; Vetlova, E.R.; Zolotova, S.V.; Galkin, M.V.; Arutyunov, N.V.; Chamorsov, Y.; Krasnyanskiy, S.A.; Nazarenko, A.G.; et al. Stereotactic Radiotherapy for Spinal Meningiomas and Neurinomas. Vopr. Istor. 2015, 79, 4–13. [Google Scholar] [CrossRef]
- Gezen, F.; Kahraman, S.; Canakci, Z.; Bedük, A. Review of 36 Cases of Spinal Cord Meningioma. Spine 2000, 25, 727–731. [Google Scholar] [CrossRef] [PubMed]
- Aboul-Enein, H.A.; Khidr, W.M.; Abdeen, K.M.; Madawi, A.A. Surgical Management of Ventrally Based Lower Cervical (Subaxial) Meningiomas through the Lateral Approach: Report on 16 Cases. Clin. Neurol. Neurosurg. 2015, 139, 152–158. [Google Scholar] [CrossRef]
- Kobayashi, K.; Ando, K.; Matsumoto, T.; Sato, K.; Kato, F.; Kanemura, T.; Yoshihara, H.; Sakai, Y.; Hirasawa, A.; Nakashima, H.; et al. Clinical Features and Prognostic Factors in Spinal Meningioma Surgery from a Multicenter Study. Sci. Rep. 2021, 11, 11630. [Google Scholar] [CrossRef]
- Cramer, P.; Thomale, U.W.; Okuducu, A.F.; Lemke, A.J.; Stockhammer, F.; Woiciechowsky, C. An Atypical Spinal Meningioma with CSF Metastasis: Fatal Progression despite Aggressive Treatment. Case Report. J. Neurosurg. Spine 2005, 3, 153–158. [Google Scholar] [CrossRef]
- Read, W.L.; Williams, F. Recurrent Meningioma of the Cervical Spine, Successfully Treated with Liposomal Doxorubicin. Case Rep. Oncol. 2017, 10, 656–659. [Google Scholar] [CrossRef]
- Epstein, N. Nursing Review of Spinal Meningiomas. Surg. Neurol. Int. 2018, 9, 41. [Google Scholar] [CrossRef]
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Study type | Observational/experimental, peer-reviewed, human studies | Case report, review, editorial, letters, and conference abstracts |
| Publication date | From 1 January 2000 to 1 January 2022 | n/a |
| Language | English | All other languages |
| Population | All sorts of cohorts with at least ten patients | Studies with less than ten patients |
| Intervention | All interventions for both treatment and diagnosis of the tumor | n/a |
| Comparator | n/a | n/a |
| Outcome | Any outcome clearly reported | n/a |
| Most Common Symptom (n = Number of Studies) | 2nd Most Common Symptom (n) | 3rd Most Common Symptom (n) | Times Mentioned in the Top 3 (% among Studies) | |
|---|---|---|---|---|
| Motor dysfunction | 19 | 16 | 11 | 46 (92%) |
| Sensory dysfunction | 17 | 16 | 6 | 39 (78%) |
| Pain | 18 | 10 | 10 | 38 (76%) |
| Gait disturbance | 2 | 11 | 8 | 21 (42%) |
| Bladder and/or bowel dysfunction | 1 | 2 | 11 | 14 (28%) |
| Data not available | 0 | 2 | 5 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Hajj, V.G.; Pettersson-Segerlind, J.; Fletcher-Sandersjöö, A.; Edström, E.; Elmi-Terander, A. Current Knowledge on Spinal Meningiomas Epidemiology, Tumor Characteristics and Non-Surgical Treatment Options: A Systematic Review and Pooled Analysis (Part 1). Cancers 2022, 14, 6251. https://doi.org/10.3390/cancers14246251
El-Hajj VG, Pettersson-Segerlind J, Fletcher-Sandersjöö A, Edström E, Elmi-Terander A. Current Knowledge on Spinal Meningiomas Epidemiology, Tumor Characteristics and Non-Surgical Treatment Options: A Systematic Review and Pooled Analysis (Part 1). Cancers. 2022; 14(24):6251. https://doi.org/10.3390/cancers14246251
Chicago/Turabian StyleEl-Hajj, Victor Gabriel, Jenny Pettersson-Segerlind, Alexander Fletcher-Sandersjöö, Erik Edström, and Adrian Elmi-Terander. 2022. "Current Knowledge on Spinal Meningiomas Epidemiology, Tumor Characteristics and Non-Surgical Treatment Options: A Systematic Review and Pooled Analysis (Part 1)" Cancers 14, no. 24: 6251. https://doi.org/10.3390/cancers14246251
APA StyleEl-Hajj, V. G., Pettersson-Segerlind, J., Fletcher-Sandersjöö, A., Edström, E., & Elmi-Terander, A. (2022). Current Knowledge on Spinal Meningiomas Epidemiology, Tumor Characteristics and Non-Surgical Treatment Options: A Systematic Review and Pooled Analysis (Part 1). Cancers, 14(24), 6251. https://doi.org/10.3390/cancers14246251






