Effectiveness of Nivolumab in Second-Line and Later in Patients with Advanced Non-Small Cell Lung Cancer in Real-Life Practice in France and Germany: Analysis of the ESME-AMLC and CRISP Cohorts
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. ESME-AMLC
2.2. CRISP (AIO-TRK-0315)
2.3. Study Population
2.4. Study Period
2.5. Analyses
3. Results
3.1. Patient Characteristics
3.2. Treatment Response, Treatment Duration and Reasons for Discontinuation
3.3. OS and PFS
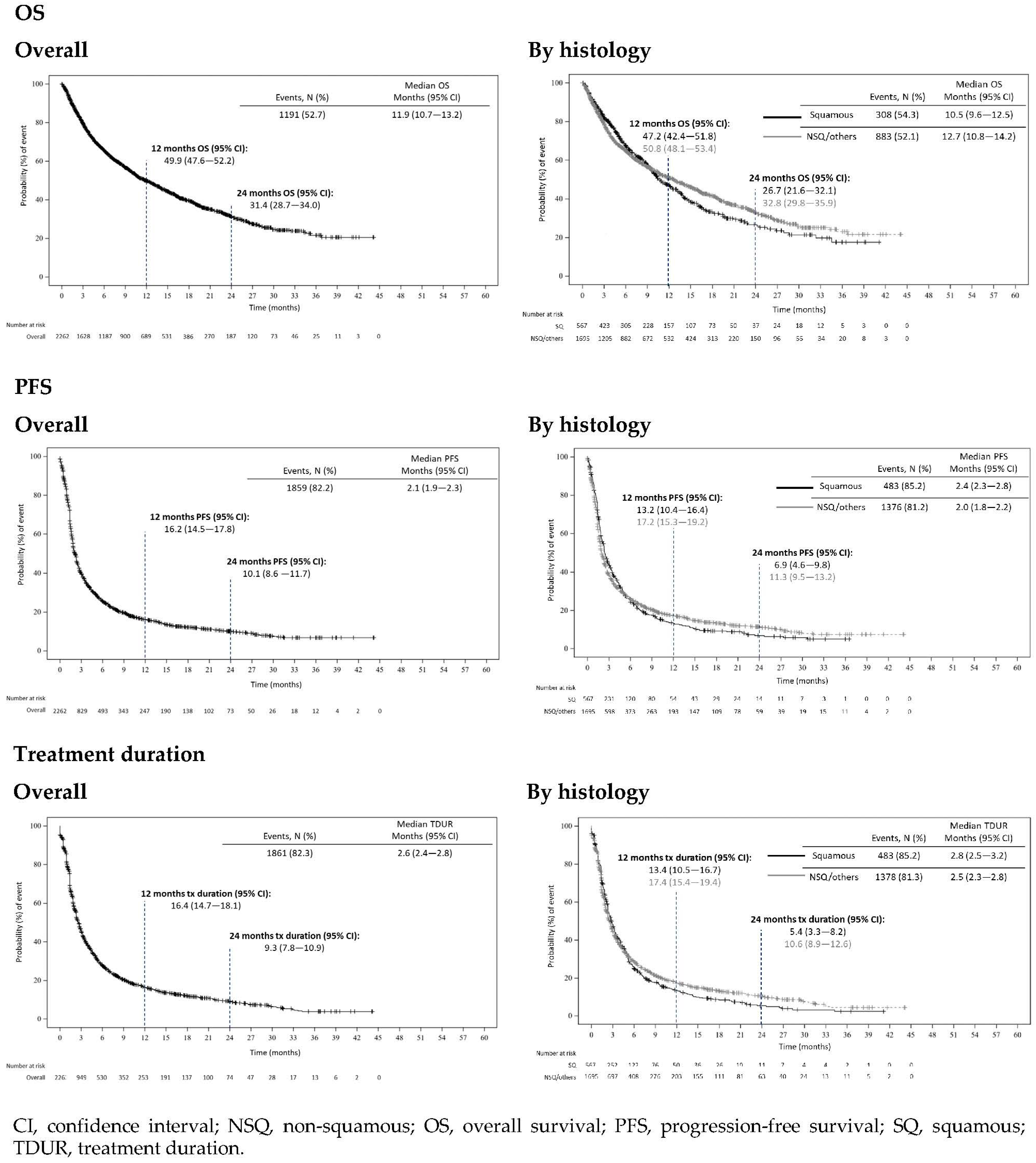
3.3.1. ESME-AMLC
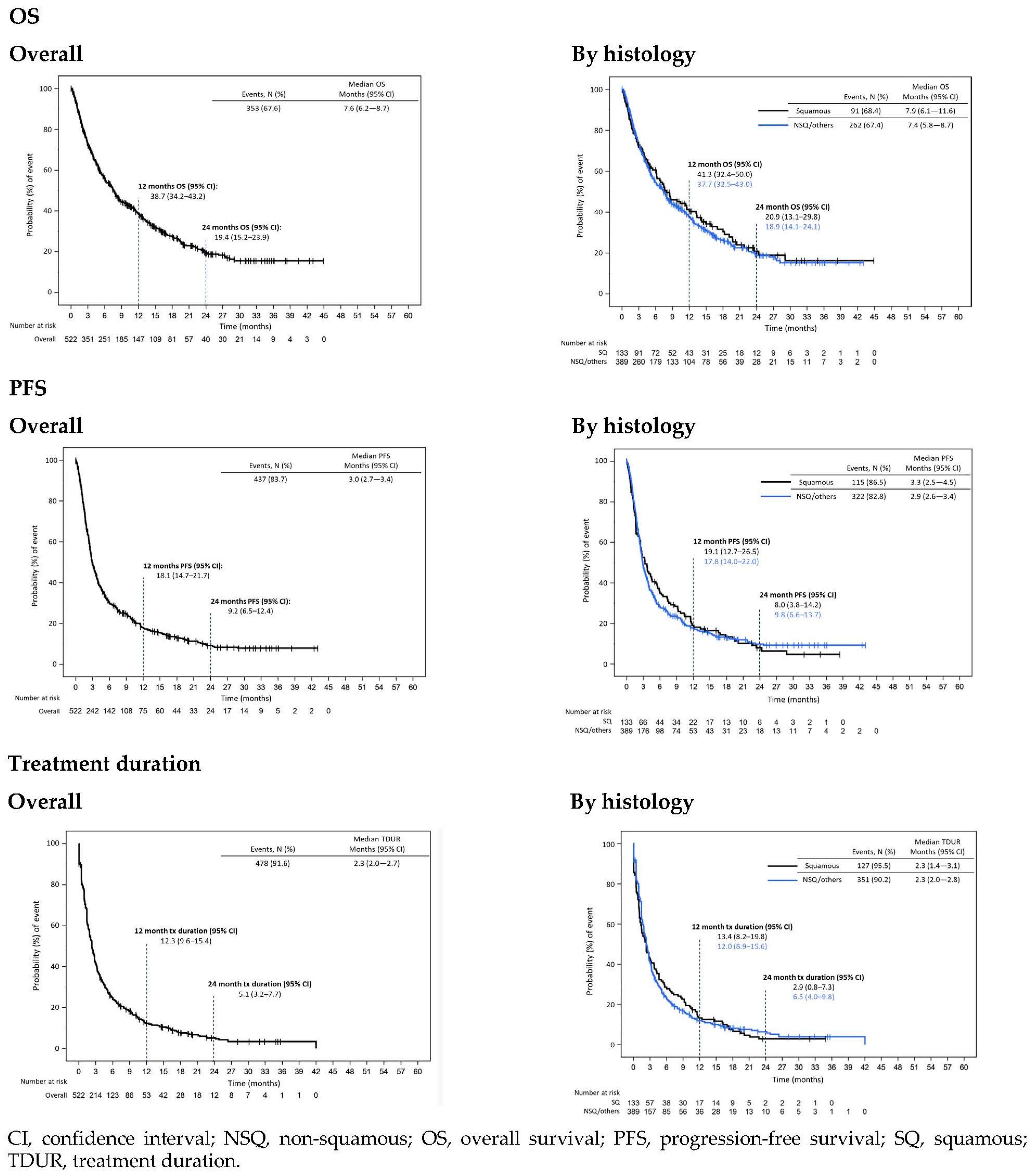
3.3.2. CRISP
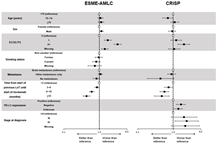
3.4. Factors Associated with Treatment Duration and OS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Globocan, The Global Cancer Observatory. France Fact Sheet. Available online: https://gco.iarc.fr/today/data/factsheets/populations/250-france-fact-sheets.pdf (accessed on 9 December 2022).
- Globocan, The Global Cancer Observatory. Germany Fact Sheet. Available online: https://gco.iarc.fr/today/data/factsheets/populations/276-germany-fact-sheets.pdf (accessed on 9 December 2022).
- ESMO. Non-Small-Cell Lung Cancer (NSCLC): An ESMO Guide for Patients. Available online: https://www.esmo.org/for-patients/patient-guides/non-small-cell-lung-cancer (accessed on 9 December 2022).
- ESMO. Metastatic Non-Small Cell Lung Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Available online: https://www.esmo.org/content/download/347819/6934778/1/ESMO-CPG-mNSCLC-15SEPT2020.pdf (accessed on 9 December 2022).
- Guo, L.; Zhang, H.; Chen, B. Nivolumab as Programmed Death-1 (PD-1) Inhibitor for Targeted Immunotherapy in Tumor. J. Cancer 2017, 8, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Velcheti, V.; Schalper, K.A.; Carvajal, D.E.; Anagnostou, V.K.; Syrigos, K.N.; Sznol, M.; Herbst, R.S.; Gettinger, S.N.; Chen, L.; Rimm, D.L. Programmed death ligand-1 expression in non-small cell lung cancer. Lab. Investig. 2014, 94, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Brahmer, J.; Reckamp, K.L.; Baas, P.; Crinò, L.; Eberhardt, W.E.; Poddubskaya, E.; Antonia, S.; Pluzanski, A.; Vokes, E.E.; Holgado, E.; et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 373, 123–135. [Google Scholar] [CrossRef]
- Borghaei, H.; Paz-Ares, L.; Horn, L.; Spigel, D.R.; Steins, M.; Ready, N.E.; Chow, L.Q.; Vokes, E.E.; Felip, E.; Holgado, E.; et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 373, 1627–1639. [Google Scholar] [CrossRef]
- Borghaei, H.; Gettinger, S.; Vokes, E.E.; Chow, L.Q.M.; Burgio, M.A.; de Castro Carpeno, J.; Pluzanski, A.; Arrieta, O.; Frontera, O.A.; Chiari, R.; et al. Five-Year Outcomes From the Randomized, Phase III Trials CheckMate 017 and 057: Nivolumab Versus Docetaxel in Previously Treated Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2021, 39, 723–733. [Google Scholar] [CrossRef]
- Horn, L.; Spigel, D.R.; Vokes, E.E.; Holgado, E.; Ready, N.; Steins, M.; Poddubskaya, E.; Borghaei, H.; Felip, E.; Paz-Ares, L.; et al. Nivolumab Versus Docetaxel in Previously Treated Patients with Advanced Non-Small-Cell Lung Cancer: Two-Year Outcomes From Two Randomized, Open-Label, Phase III Trials (CheckMate 017 and CheckMate 057). J. Clin. Oncol. 2017, 35, 3924–3933. [Google Scholar] [CrossRef] [PubMed]
- The European Medicines Agency. OPDIVO: Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/opdivo-epar-product-information_en.pdf (accessed on 9 December 2022).
- Ekman, S.; Griesinger, F.; Baas, P.; Chao, D.; Chouaid, C.; O’Donnell, J.C.; Penrod, J.R.; Daumont, M.; Lacoin, L.; McKenney, A.; et al. I-O Optimise: A novel multinational real-world research platform in thoracic malignancies. Future Oncol. 2019, 15, 1551–1563. [Google Scholar] [CrossRef]
- Griesinger, F.; Pérol, M.; Girard, N.; Durand-Zaleski, I.; Zacharias, S.; Bosquet, L.; Jänicke, M.; Quantin, X.; Groth, A.; Fleitz, A.; et al. Impact of immune checkpoint inhibitors on the management of locally advanced or metastatic non-small cell lung cancer in real-life practice in patients initiating treatment between 2015 and 2018 in France and Germany. Lung Cancer 2022, 172, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Barlesi, F.; Dixmier, A.; Debieuvre, D.; Raspaud, C.; Auliac, J.B.; Benoit, N.; Bombaron, P.; Moro-Sibilot, D.; Audigier-Valette, C.; Asselain, B.; et al. Effectiveness and safety of nivolumab in the treatment of lung cancer patients in France: Preliminary results from the real-world EVIDENS study. Oncoimmunology 2020, 9, 1744898. [Google Scholar] [CrossRef]
- Giaj Levra, M.; Cotté, F.E.; Corre, R.; Calvet, C.; Gaudin, A.F.; Penrod, J.R.; Grumberg, V.; Jouaneton, B.; Jolivel, R.; Assié, J.B.; et al. Immunotherapy rechallenge after nivolumab treatment in advanced non-small cell lung cancer in the real-world setting: A national data base analysis. Lung Cancer 2020, 140, 99–106. [Google Scholar] [CrossRef]
- Sebastian, M.; Gröschel, A.; Gütz, S.; Schulz, H.; Müller-Huesmann, H.; Liersch, R.; von der Heyde, E.; Wiegand, J.; Ukena, D.; Bargon, J.; et al. Prospective, Noninterventional Study of Nivolumab in Real-world Patients With Locally Advanced or Metastatic Non-small Cell Lung Cancer After Prior Chemotherapy (ENLARGE-Lung). J. Immunother. 2022, 45, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Areses Manrique, M.C.; Mosquera Martínez, J.; García González, J.; Afonso Afonso, F.J.; Lázaro Quintela, M.; Fernández Núñez, N.; Azpitarte Raposeiras, C.; Amenedo Gancedo, M.; Santomé Couto, L.; García Campelo, M.R.; et al. Real world data of nivolumab for previously treated non-small cell lung cancer patients: A Galician lung cancer group clinical experience. Transl. Lung Cancer Res. 2018, 7, 404–415. [Google Scholar] [CrossRef] [PubMed]
- Dudnik, E.; Moskovitz, M.; Daher, S.; Shamai, S.; Hanovich, E.; Grubstein, A.; Shochat, T.; Wollner, M.; Bar, J.; Merimsky, O.; et al. Effectiveness and safety of nivolumab in advanced non-small cell lung cancer: The real-life data. Lung Cancer 2018, 126, 217–223. [Google Scholar] [CrossRef]
- Grossi, F.; Genova, C.; Crinò, L.; Delmonte, A.; Turci, D.; Signorelli, D.; Passaro, A.; Soto Parra, H.; Catino, A.; Landi, L.; et al. Real-life results from the overall population and key subgroups within the Italian cohort of nivolumab expanded access program in non-squamous non-small cell lung cancer. Eur. J. Cancer 2019, 123, 72–80. [Google Scholar] [CrossRef]
- Juergens, R.A.; Mariano, C.; Jolivet, J.; Finn, N.; Rothenstein, J.; Reaume, M.N.; Faghih, A.; Labbé, C.; Owen, S.; Shepherd, F.A.; et al. Real-world benefit of nivolumab in a Canadian non-small-cell lung cancer cohort. Curr. Oncol. 2018, 25, 384–392. [Google Scholar] [CrossRef]
- Merino Almazán, M.; Duarte Pérez, J.M.; Marín Pozo, J.F.; Ortega Granados, A.L.; Muros De Fuentes, B.; Quesada Sanz, P.; Gago Sánchez, A.I.; Rodríguez Gómez, P.; Jurado García, J.M.; Artime Rodríguez-Hermida, F.; et al. A multicentre observational study of the effectiveness, safety and economic impact of nivolumab on non-small-cell lung cancer in real clinical practice. Int. J. Clin. Pharm. 2019, 41, 272–279. [Google Scholar] [CrossRef]
- Schouten, R.D.; Muller, M.; de Gooijer, C.J.; Baas, P.; van den Heuvel, M. Real life experience with nivolumab for the treatment of non-small cell lung carcinoma: Data from the expanded access program and routine clinical care in a tertiary cancer centre-The Netherlands Cancer Institute. Lung Cancer 2018, 126, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Spigel, D.R.; McCleod, M.; Jotte, R.M.; Einhorn, L.; Horn, L.; Waterhouse, D.M.; Creelan, B.; Babu, S.; Leighl, N.B.; Chandler, J.C.; et al. Safety, Efficacy, and Patient-Reported Health-Related Quality of Life and Symptom Burden with Nivolumab in Patients with Advanced Non-Small Cell Lung Cancer, Including Patients Aged 70 Years or Older or with Poor Performance Status (CheckMate 153). J. Thorac. Oncol. 2019, 14, 1628–1639. [Google Scholar] [CrossRef]
- Stenehjem, D.D.; Lubinga, S.J.; Gupte-Singh, K.; Zhang, Y.; Le, T.K.; Penrod, J.R.; Smith, C.B. Real-World Effectiveness of Nivolumab Monotherapy After Prior Systemic Therapy in Advanced Non-Small-Cell Lung Cancer in the United States. Clin. Lung Cancer 2021, 22, e35–e47. [Google Scholar] [CrossRef]
- Tournoy, K.G.; Thomeer, M.; Germonpré, P.; Derijcke, S.; De Pauw, R.; Galdermans, D.; Govaert, K.; Govaerts, E.; Schildermans, R.; Declercq, I.; et al. Does nivolumab for progressed metastatic lung cancer fulfill its promises? An efficacy and safety analysis in 20 general hospitals. Lung Cancer 2018, 115, 49–55. [Google Scholar] [CrossRef]
- Gebbia, V.; Galetta, D.; De Marinis, F. Non small cell lung cancer patients with ECOG PS2: Unsolved questions and lessons from clinical trials. Ann. Oncol. 2005, 16 (Suppl. S4), iv123–iv131. [Google Scholar] [CrossRef] [PubMed]
- Gridelli, C.; Ardizzoni, A.; Le Chevalier, T.; Manegold, C.; Perrone, F.; Thatcher, N.; van Zandwijk, N.; Di Maio, M.; Martelli, O.; De Marinis, F. Treatment of advanced non-small-cell lung cancer patients with ECOG performance status 2: Results of an European Experts Panel. Ann. Oncol. 2004, 15, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Geier, M.; Descourt, R.; Corre, R.; Léveiller, G.; Lamy, R.; Goarant, É.; Bizec, J.; Bernier, C.; Quéré, G.; Gaye, É.; et al. Real life second-line nivolumab in advanced non-small cell lung cancer: A French observational multicenter study of 259 patients (ABCTIMMUNOBZH). Cancer Rep. Rev. 2018, 2, 1–6. [Google Scholar] [CrossRef]
- Kaderbhai, C.G.; Richard, C.; Fumet, J.D.; Aarnink, A.; Ortiz-Cuaran, S.; Pérol, M.; Foucher, P.; Coudert, B.; Favier, L.; Lagrange, A.; et al. Response to first line chemotherapy regimen is associated with efficacy of nivolumab in non-small-cell lung cancer. Oncoimmunology 2017, 6, e1339856. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Omori, S.; Nakashima, K.; Wakuda, K.; Ono, A.; Kenmotsu, H.; Naito, T.; Murakami, H.; Endo, M.; Takahashi, T. Response to the treatment immediately before nivolumab monotherapy may predict clinical response to nivolumab in patients with non-small cell lung cancer. Int. J. Clin. Oncol. 2017, 22, 690–697. [Google Scholar] [CrossRef]
- Grossi, F.; Crinò, L.; Logroscino, A.; Canova, S.; Delmonte, A.; Melotti, B.; Proto, C.; Gelibter, A.; Cappuzzo, F.; Turci, D.; et al. Use of nivolumab in elderly patients with advanced squamous non-small-cell lung cancer: Results from the Italian cohort of an expanded access programme. Eur. J. Cancer 2018, 100, 126–134. [Google Scholar] [CrossRef]
| ESME-AMLC | CRISP | ||||||
|---|---|---|---|---|---|---|---|
| Overall | SQ | NSQ/ Others | Overall | SQ | NSQ/ Others | ||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Cohort Size | N | 2262 | 567 | 1695 | 522 | 133 | 389 |
| Year of nivolumab start | 2015 | 186 (8.2) | 63 (11.1) | 123 (7.3) | - | - | - |
| 2016 | 695 (30.7) | 184 (32.5) | 511 (30.1) | 42 (8.0) | 14 (10.5) | 28 (7.2) | |
| 2017 | 856 (37.8) | 213 (37.6) | 643 (37.9) | 167 (32.0) | 40 (30.1) | 127 (32.6) | |
| 2018 | 460 (20.3) | 95 (16.8) | 365 (21.5) | 214 (41.0) | 48 (36.1) | 166 (42.7) | |
| 2019/2020 * | 65 (2.9) | 12 (2.1) | 53 (3.1) | 99 (19.0) | 31 (23.3) | 68 (17.5) | |
| Age (years) at nivolumab start | Median | 64 | 66 | 63 | 66 | 69 | 64 |
| Q1–Q3 | 56.9–69.8 | 59.9–72.8 | 55.8–68.8 | 60.0–73.0 | 64.0–76.0 | 59.0–72.0 | |
| ≥75 | 262 (11.6) | 106 (18.7) | 156 (9.2) | 126 (24.1) | 46 (34.6) | 80 (20.6) | |
| Sex | Male | 1560 (69.0) | 465 (82.0) | 1095 (64.6) | 327 (62.6) | 94 (70.7) | 233 (59.9) |
| Stage at initial diagnosis | I–II | 176 (7.8) | 64 (11.3) | 112 (6.6) | 18 (3.4) | 5 (3.8) | 13 (3.3) |
| IIIA | 181 (8.0) | 60 (10.6) | 121 (7.1) | 9 (1.7) | 4 (3.0) | 5 (1.3) | |
| IIIB–IIIC | 326 (14.4) | 132 (23.3) | 194 (11.4) | 44 (8.4) | 18 (13.5) | 26 (6.7) | |
| IV | 1550 (68.5) | 305 (53.8) | 1245 (73.5) | 428 (82) | 100 (75.2) | 328 (84.3) | |
| ECOG performance status at nivolumab start | 0–1 | 1014 (44.8) | 260 (45.9) | 754 (44.5) | 293 (56.1) | 78 (58.6) | 215 (55.3) |
| 2 | 247 (10.9) | 61 (10.8) | 186 (11.0) | 92 (17.6) | 23 (17.3) | 69 (17.7) | |
| 3–4 | 81 (3.6) | 15 (2.6) | 66 (3.9) | 10 (1.9) | 2 (1.5) | 8 (2.1) | |
| Missing | 920 (40.7) | 231 (40.7) | 689 (40.6) | 127 (24.3) | 30 (22.6) | 97 (24.9) | |
| Smoking status at diagnosis † | Never smoked | 138 (6.1) | 11 (1.9) | 127 (7.5) | 46 (8.8) | 7 (5.3) | 39 (10.0) |
| Light former smoker | 93 (4.1) | 20 (3.5) | 73 (4.3) | 44 (8.4) | 11 (8.3) | 33 (8.5) | |
| Heavy former smoker | 1139 (50.4) | 317 (55.9) | 822 (48.5) | 200 (38.3) | 56 (42.1) | 144 (37.0) | |
| Former smoker of unknown intensity | 27 (1.2) | 5 (0.9) | 22 (1.3) | 17 (3.3) | 8 (6.0) | 9 (2.3) | |
| Smoker | 804 (35.5) | 200 (35.3) | 604 (35.6) | 160 (30.7) | 38 (28.6) | 122 (31.4) | |
| Missing | 61 (2.7) | 14 (2.5) | 47 (2.8) | 55 (10.5) | 13 (9.8) | 42 (10.8) | |
| At least one metastasis at time of nivolumab start | Any location | 2052 (90.7) | 444 (78.3) | 1608 (94.9) | 507 (97.1) | 129 (97.0) | 378 (97.2) |
| Bone | 992 (43.9) | 170 (30.0) | 822 (48.5) | 237 (45.4) | 50 (37.6) | 187 (48.1) | |
| Brain | 785 (34.7) | 111 (19.6) | 674 (39.8) | 128 (24.5) | 16 (12.0) | 112 (28.8) | |
| Symptomatic | 192 (8.5) | 26 (4.6) | 166 (9.8) | NR | NR | NR | |
| Asymptomatic | 593 (26.2) | 85 (15.0) | 508 (30.0) | NR | NR | NR | |
| Liver | 515 (22.8) | 117 (20.6) | 398 (23.5) | 128 (24.5) | 29 (21.8) | 99 (25.4) | |
| PD-L1 testing at nivolumab start ‡ | Testing done | 678 (30.0) | 114 (20.1) | 564 (33.3) | 310 (59.4) | 76 (57.1) | 234 (60.2) |
| Positive | 276 (12.2) | 49 (8.6) | 277 (16.3) | 136 (26.1) | 29 (21.8) | 107 (27.5) | |
| ≥50% | 115 (5.1) | 15 (2.6) | 100 (5.9) | 29 (5.6) | 7 (5.3) | 22 (5.7) | |
| 1–49% | 154 (6.8) | 25 (4.4) | 129 (7.6) | 92 (17.6) | 20 (15.0) | 72 (18.5) | |
| Unknown | 57 (2.5) | 9 (1.6) | 48 (2.8) | 15 (2.9) | 2 (1.5) | 13 (3.3) | |
| Negative | 352 (15.6) | 65 (11.5) | 287 (16.9) | 170 (32.6) | 47 (35.3) | 123 (31.6) | |
| Not contributive | - | - | - | 4 (0.8) | 0 (0.0) | 4 (1.0) | |
| Testing not done | 1584 (70.0) | 453 (79.9) | 1131 (66.7) | 212 (40.6) | 57 (42.9) | 155 (39.8) | |
| EGFR | Positive | 79 (3.5) | 2 (0.4) | 77 (4.5) | 24 (4.6) | 2 (1.5) | 22 (5.7) |
| ALK | Positive | 19 (0.8) | 3 (0.5) | 16 (0.9) | 10 (1.9) | 1 (0.8) | 9 (2.3) |
| ROS | Positive | 14 (0.6) | 1 (0.2) | 13 (0.8) | 8 (1.5) | 1 (0.8) | 7 (1.8) |
| Time from initial diagnosis (months) | Median | 9.6 | 8.8 | 9.9 | 7.8 | 7.7 | 7.9 |
| Q1–Q3 | 6.2–15.9 | 5.9–15.1 | 6.3–16.2 | 5.2–11.8 | 5.3–11.1 | 5.2–12.2 | |
| Line of nivolumab treatment | 2L | 1516 (67.0) | 429 (75.7) | 1087 (64.1) | 433 (83.0) | 122 (91.7) | 311 (79.9) |
| 3L | 554 (24.5) | 121 (21.3) | 433 (25.5) | 75 (14.4) | 8 (6.0) | 67 (17.2) | |
| 4L | 141 (6.2) | 16 (2.8) | 125 (7.4) | 11 (2.1) | 3 (2.3) | 8 (2.1) | |
| 5L+ | 51 (2.3) | 1 (0.2) | 50 (2.9) | 3 (0.6) | 0 (0.0) | 3 (0.8) | |
| Previous regimens received (all) | PT-based CT | 2052 (90.7) | 507 (89.4) | 1545 (91.2) | 492 (94.3) | 119 (89.5) | 373 (95.9) |
| Non-PT-based CT | 506 (22.4) | 105 (18.5) | 401 (23.7) | 43 (8.2) | 9 (6.8) | 34 (8.7) | |
| Targeted therapy | 120 (5.3) | 10 (1.8) | 110 (6.5) | 14 (2.7) | 0 (0.0) | 14 (3.6) | |
| Immunotherapy | 5 (0.2) | 0 (0.0) | 5 (0.3) | 13 (2.5) | 6 (4.5) | 7 (1.8) | |
| Investigational agents | 171 (7.6) | 34 (6.0) | 137 (8.1) | 5 (1.0) | 1 (0.8) | 4 (1.0) | |
| Other combinations | 20 (0.9) | 0 (0.0) | 20 (1.2) | 30 (5.7) | 6 (4.5) | 24 (6.2) | |
| Last LoT regimen received prior to nivolumab | PT-based CT | 1590 (70.3) | 430 (75.8) | 1160 (68.4) | 439 (84.1) | 115 (86.5) | 324 (83.3) |
| Non-PT-based CT | 461 (20.4) | 98 (17.3) | 363 (21.4) | 38 (7.3) | 8 (6.0) | 30 (7.7) | |
| Targeted therapy | 66 (2.9) | 10 (1.8) | 56 (3.3) | 4 (0.8) | 0 (0.0) | 4 (1.0) | |
| Immunotherapy | 2 (0.1) | 0 (0.0) | 2 (0.1) | 7 (1.3) | 4 (3.0) | 3 (0.8) | |
| Investigational agents | 130 (5.7) | 29 (5.1) | 101 (6.0) | 5 (1.0) | 1 (0.8) | 4 (1.0) | |
| Other combinations | 13 (0.6) | 0 (0.0) | 13 (0.8) | 29 (5.6) | 5 (3.8) | 24 (6.2) | |
| Time from start of previous LoT until start of nivolumab (months) | Median | 5.5 | 5.5 | 5.5 | 5.4 | 5.4 | 5.6 |
| Q1–Q3 | 2.9–8.6 | 3.0–8.0 | 2.9–8.9 | 3.2–8.1 | 3.4–7.8 | 3.0–8.2 | |
| <3 | 606 (26.8) | 146 (25.7) | 460 (27.1) | 121 (23.2) | 26 (19.5) | 95 (24.4) | |
| ≥3–< 6 | 649 (28.7) | 173 (30.5) | 476 (28.1) | 173 (33.1) | 53 (39.8) | 120 (30.8) | |
| ≥6–<12 | 730 (32.3) | 198 (34.9) | 532 (31.4) | 183 (35.1) | 47 (35.3) | 136 (35.0) | |
| ≥12 | 277 (12.2) | 50 (8.8) | 227 (13.4) | 44 (8.4) | 7 (5.3) | 37 (9.5) | |
| Histology | PD-L1 Status at Nivolumab Start | ||||||
|---|---|---|---|---|---|---|---|
| Overall | SQ | NSQ/Others | Not Tested | Positive | Negative | ||
| Cohort Size | N | 522 | 133 | 389 | 212 | 136 | 170 |
| Best treatment response | Complete/partial response | 58 (11.1%) | 12 (9.0%) | 46 (11.8%) | 23 (10.8%) | 25 (18.4%) | 10 (5.9%) |
| Stable disease | 107 (20.5%) | 27 (20.3%) | 80 (20.6%) | 48 (22.6%) | 21 (15.4%) | 37 (21.8%) | |
| Progressive disease | 164 (31.4%) | 41 (30.8%) | 123 (31.6%) | 58 (27.4%) | 52 (38.2%) | 53 (31.2%) | |
| Unknown | 193 (37.0%) | 53 (39.8%) | 140 (36.0%) | 83 (39.2%) | 38 (27.9%) | 70 (41.2%) | |
| ESME-AMLC | CRISP | |||||
|---|---|---|---|---|---|---|
| Overall | SQ | NSQ/Others | Overall | SQ | NSQ/Others | |
| Reason for Discontinuation * | 1861 | 483 | 1378 | 522 | 133 | 389 |
| Progression | 1073 (57.7) | 285 (59.0) | 788 (57.2) | 271 (51.9) | 66 (49.6) | 205 (52.7) |
| Toxicity | 152 (8.2) | 42 (8.7) | 110 (8.0) | 28 (5.4) | 7 (5.3) | 21 (5.4) |
| Gastrointestinal | 19 (1.0) | 4 (0.8) | 15 (1.1) | NR | NR | NR |
| Hepatic | 16 (0.9) | 3 (0.6) | 13 (0.9) | NR | NR | NR |
| Cutaneous | 8 (0.4) | 5 (1.0) | 3 (0.2) | NR | NR | NR |
| Hematological | 10 (0.5) | 4 (0.8) | 6 (0.4) | NR | NR | NR |
| Autoimmune | 12 (0.6) | 3 (0.6) | 9 (0.7) | NR | NR | NR |
| Other toxicities | 74 (4.0) | 17 (3.5) | 57 (4.1) | NR | NR | NR |
| Doctor’s choice/protocol driven | 263 (14.1) | 66 (13.7) | 197 (14.3) | 14 (2.7) | 5 (3.8) | 9 (2.3) |
| Patient’s death | 296 (15.9) | 78 (16.1) | 218 (15.8) | NR | NR | NR |
| Patient’s choice | 22 (1.2) | 1 (0.2) | 21 (1.5) | NR | NR | NR |
| Others | 138 (7.4) | 28 (5.8) | 110 (8.0) | 164 (31.4) | 48 (36.1) | 116 (29.8) |
| Missing | 8 (0.4) | 2 (0.4) | 6 (0.4) | 45 (8.6) | 7 (5.3) | 38 (9.8) |
| ESME-AMLC | CRISP | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable * | Cohort Size | Median | 95% CI | HR (95% CI) | p-Value | Cohort Size | Median | 95% CI | HR (95% CI) | p-Value | |
| Age (years) | <70 | 1709 | 2.6 | 2.3–2.8 | Reference | 0.67 | 328 | 2.2 | 1.8–2.5 | Reference | 0.67 |
| 70–74 | 291 | 2.9 | 2.4–3.4 | 1.06 (0.92–1.21) | 68 | 2.8 | 2.1–3.7 | 0.89 (0.67–1.17) | |||
| ≥75 | 262 | 2.4 | 2.1–3.1 | 0.98 (0.84–1.14) | 126 | 2.6 | 2.0–3.2 | 1.01 (0.81–1.27) | |||
| Sex | Female | 702 | 2.5 | 2.3–2.8 | Reference | 0.55 | 195 | 2.3 | 1.8–2.8 | Reference | 0.29 |
| Male | 1560 | 2.7 | 2.4–2.9 | 1.03 (0.93–1.14) | 327 | 2.3 | 1.9–2.8 | 0.90 (0.74–1.09) | |||
| ECOG PS | 0 | 228 | 3.7 | 2.8–4.7 | Reference | <0.01 | 68 | 2.8 | 2.1–3.4 | Reference | 0.03 |
| 1 | 786 | 2.6 | 2.3–2.9 | 1.18 (1.00–1.39) | 225 | 2.3 | 2.0–2.8 | 1.02 (0.76–1.36) | |||
| 2+ | 328 | 1.4 | 1.3–1.8 | 1.87 (1.55–2.25) | 102 | 1.4 | 1.0–2.3 | 1.29 (0.93–1.79) | |||
| Missing | 920 | 3.0 | 2.8–3.3 | 1.12 (0.95–1.31) | 127 | 2.5 | 1.7–3.6 | 0.82 (0.59–1.13) | |||
| Smoking status | Non-smokers | 138 | 2.0 | 1.6–2.4 | Reference | 0.16 | NA | ||||
| Former smokers | 1259 | 2.6 | 2.3–2.8 | 0.98 (0.80–1.20) | |||||||
| Smokers | 804 | 2.8 | 2.5–3.2 | 0.88 (0.71–1.09) | |||||||
| Missing | 61 | 2.6 | 1.9–4.0 | 0.84 (0.60–1.19) | |||||||
| Metastases | Brain | 785 | 2.5 | 2.3–2.9 | Reference | 0.03 | 128 | 2.1 | 1.4–2.6 | NP | NP |
| Other only | 1267 | 2.5 | 2.3–2.8 | 1.07 (0.96–1.18) | 379 | 2.3 | 2.0–2.8 | NP | |||
| No metastases | 210 | 3.5 | 3.0–4.7 | 0.87 (0.73–1.03) | 15 | 3.3 | 1.4–7.0 | NP | |||
| Time from start of previous LoT until start of nivolumab (months) | <3 | 606 | 1.9 | 1.8–2.3 | Reference | <0.01 | 121 | 1.4 | 1.1–2.1 | Reference | <0.01 |
| 3–6 | 649 | 2.3 | 1.9–2.4 | 0.99 (0.87–1.11) | 173 | 2.1 | 1.4–2.4 | 0.78 (0.61–1.01) | |||
| 6–12 | 730 | 3.1 | 2.8–3.5 | 0.80 (0.71–0.91) | 183 | 2.8 | 2.3–3.5 | 0.65 (0.50–0.84) | |||
| ≥12 | 277 | 4.4 | 3.5–5.5 | 0.63 (0.53–0.75) | 44 | 4.6 | 3.2–7.9 | 0.55 (0.37–0.82) | |||
| PD-L1 expression | Positive | 276 | 2.8 | 2.3–3.4 | Reference | 0.03 | 136 | 1.9 | 1.5–2.8 | Reference | 0.06 |
| Negative | 352 | 2.3 | 1.8–2.7 | 1.24 (1.03–1.48) | 170 | 2.3 | 1.7–2.8 | 1.31 (1.01–1.68) | |||
| Unknown | 1634 | 2.8 | 2.5–2.9 | 1.04 (0.90–1.20) | 216 | 2.4 | 2.2–3.2 | 1.29 (1.02–1.64) | |||
| EGFR, ALK or ROS mutations | No | 2154 | 2.7 | 2.5–2.9 | Reference | <0.01 | NA | ||||
| Yes | 108 | 2.0 | 1.5–2.3 | 1.50 (1.20–1.87) | |||||||
| Year of nivolumab start | 2015 | 186 | 2.2 | 1.9–2.8 | Reference | 0.17 | |||||
| 2016 | 695 | 2.6 | 2.3–3.0 | 0.99 (0.83–1.17) | 42 | 2.3 | 1.0–5.2 | Reference | 0.08 | ||
| 2017 | 856 | 2.5 | 2.3–2.8 | 1.00 (0.84–1.18) | 167 | 2.6 | 1.9–3.5 | 1.11 (0.77–1.59) | |||
| 2018 | 460 | 3.1 | 2.4–3.5 | 0.91 (0.75–1.11) | 214 | 1.9 | 1.4–2.3 | 1.42 (1.00–2.04) | |||
| 2019/2020 | 65 | 6.2 | 2.3–NE | 0.60 (0.38–0.94) | 99 | 3.1 | 2.4–3.7 | 1.30 (0.86–1.98) | |||
 | |||||||||||
| ESME-AMLC | CRISP | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable * | Cohort Size | Median | 95% CI | HR (95% CI) | p-Value | Cohort Size | Median | 95% CI | HR (95% CI) | p-Value | |
| Age (years) | <70 | 1709 | 12.2 | 10.7–13.9 | Reference | 0.39 | 328 | 7.3 | 5.4–8.5 | Reference | 0.08 |
| 70–74 | 291 | 12.6 | 9.2–14.8 | 1.08 (0.90–1.29) | 68 | 8.0 | 5.3–18.9 | 0.71 (0.51–1.01) | |||
| ≥75 | 262 | 9.7 | 7.5–12.6 | 1.12 (0.93–1.34) | 126 | 7.8 | 6.1–11.4 | 1.11 (0.86–1.44) | |||
| Sex | Female | 702 | 13.9 | 11.0–16.0 | Reference | 0.04 | 195 | 8.0 | 5.8–9.9 | Reference | 0.58 |
| Male | 1560 | 11.2 | 10.0–12.8 | 1.15 (1.01–1.31) | 327 | 7.4 | 5.8–8.9 | 0.94 (0.75–1.17) | |||
| ECOG PS | 0 | 228 | 19.8 | 17.0–27.1 | Reference | <0.01 | 68 | 11.8 | 7.9–15.3 | Reference | <0.01 |
| 1 | 786 | 10.7 | 9.4–12.5 | 1.73 (1.38–2.15) | 225 | 7.8 | 6.2–9.3 | 1.22 (0.86–1.73) | |||
| 2+ | 328 | 3.7 | 2.9–4.3 | 3.24 (2.55–4.12) | 102 | 3.9 | 2.5–5.5 | 2.00 (1.36–2.94) | |||
| Missing | 920 | 15.4 | 13.2–18.0 | 1.42 (1.13–1.77) | 127 | 7.6 | 5.3–13.2 | 1.07 (0.73–1.57) | |||
| Smoking status | Non-smoker | 138 | 10.7 | 8.0–17.3 | Reference | 0.07 | 46 | 6.8 | 3.9–17.0 | NP | NA |
| Former | 1259 | 10.7 | 9.9–12.4 | 0.96 (0.76–1.22) | 261 | 8.1 | 5.8–11.3 | NP | |||
| Current | 804 | 14.7 | 11.6–16.6 | 0.82 (0.64–1.06) | 160 | 7.2 | 5.0–8.1 | NP | |||
| Missing | 61 | 14.6 | 7.6–23.8 | 0.75 (0.48–1.15) | 55 | 8.9 | 5.2–12.7 | NP | |||
| Metastases | Brain | 785 | 13.0 | 11.0–15.1 | Reference | 0.05 | 128 | 7.1 | 4.1–8.5 | Reference | 0.17 |
| Other | 1267 | 10.5 | 9.2–12.5 | 1.07 (0.94–1.22) | 379 | 7.6 | 6.2–9.6 | 0.90 (0.70–1.17) | |||
| No metastases | 210 | 14.5 | 12.0–17.3 | 0.84 (0.67–1.04) | 15 | 23.7 | 5.3–NA | 0.44 (0.19–1.05) | |||
| Time from start of previous lot until start of nivolumab (months) | <3 | 606 | 7.0 | 6.0–8.3 | Reference | <0.01 | 121 | 4.0 | 2.8–6.1 | Reference | <0.01 |
| 3–6 | 649 | 9.8 | 8.4–11.6 | 0.86 (0.75–1.00) | 173 | 6.7 | 5.0–7.9 | 0.75 (0.57–1.00) | |||
| 6–12 | 730 | 15.4 | 14.0–18.5 | 0.61 (0.53–0.71) | 183 | 10.9 | 7.7–13.4 | 0.57 (0.43–0.75) | |||
| ≥12 | 277 | 23.8 | 18.0–28.0 | 0.44 (0.35–0.55) | 44 | 12.8 | 6.2–19.7 | 0.48 (0.30–0.77) | |||
| PD-L1 expression | Positive | 276 | 13.0 | 9.4–18.4 | NP | NA | 136 | 10.8 | 5.8–13.3 | Reference | <0.01 |
| Negative | 352 | 10.8 | 8.4–15.8 | NP | 170 | 6.1 | 4.6–7.7 | 1.66 (1.24–2.23) | |||
| Unknown | 1634 | 12.0 | 10.6–13.3 | NP | 216 | 7.8 | 6.1–8.9 | 1.39 (1.06–1.82) | |||
| Stage at diagnosis | I–II | 176 | 10.9 | 8.7–15.2 | NP | NA | 18 | 27.3 | 6.9–NA | Reference | 0.14 |
| III | 507 | 13.4 | 11.2–16.0 | NP | 53 | 12.1 | 6.2–18.0 | 2.02 (0.88–4.62) | |||
| IV | 1550 | 11.1 | 10.0–13.0 | NP | 428 | 7.2 | 5.5–8.0 | 2.38 (1.12–5.07) | |||
| Missing | 0 | NA | NA | NA | 23 | 7.2 | 4.8–11.4 | 2.19 (0.88–5.48) | |||
 | |||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chouaid, C.; Thomas, M.; Debieuvre, D.; Durand-Zaleski, I.; Zacharias, S.; Bosquet, L.; Groth, A.; Fleitz, A.; Calleja, A.; Patel, S.; et al. Effectiveness of Nivolumab in Second-Line and Later in Patients with Advanced Non-Small Cell Lung Cancer in Real-Life Practice in France and Germany: Analysis of the ESME-AMLC and CRISP Cohorts. Cancers 2022, 14, 6148. https://doi.org/10.3390/cancers14246148
Chouaid C, Thomas M, Debieuvre D, Durand-Zaleski I, Zacharias S, Bosquet L, Groth A, Fleitz A, Calleja A, Patel S, et al. Effectiveness of Nivolumab in Second-Line and Later in Patients with Advanced Non-Small Cell Lung Cancer in Real-Life Practice in France and Germany: Analysis of the ESME-AMLC and CRISP Cohorts. Cancers. 2022; 14(24):6148. https://doi.org/10.3390/cancers14246148
Chicago/Turabian StyleChouaid, Christos, Michael Thomas, Didier Debieuvre, Isabelle Durand-Zaleski, Stefan Zacharias, Lise Bosquet, Annika Groth, Annette Fleitz, Alan Calleja, Sonya Patel, and et al. 2022. "Effectiveness of Nivolumab in Second-Line and Later in Patients with Advanced Non-Small Cell Lung Cancer in Real-Life Practice in France and Germany: Analysis of the ESME-AMLC and CRISP Cohorts" Cancers 14, no. 24: 6148. https://doi.org/10.3390/cancers14246148
APA StyleChouaid, C., Thomas, M., Debieuvre, D., Durand-Zaleski, I., Zacharias, S., Bosquet, L., Groth, A., Fleitz, A., Calleja, A., Patel, S., Lacoin, L., Daumont, M. J., Penrod, J. R., Carroll, R., Waldenberger, D., Cotté, F.-E., Audigier-Valette, C., & Griesinger, F. (2022). Effectiveness of Nivolumab in Second-Line and Later in Patients with Advanced Non-Small Cell Lung Cancer in Real-Life Practice in France and Germany: Analysis of the ESME-AMLC and CRISP Cohorts. Cancers, 14(24), 6148. https://doi.org/10.3390/cancers14246148






