Landscape of Savolitinib Development for the Treatment of Non-Small Cell Lung Cancer with MET Alteration—A Narrative Review
Abstract
Simple Summary
Abstract
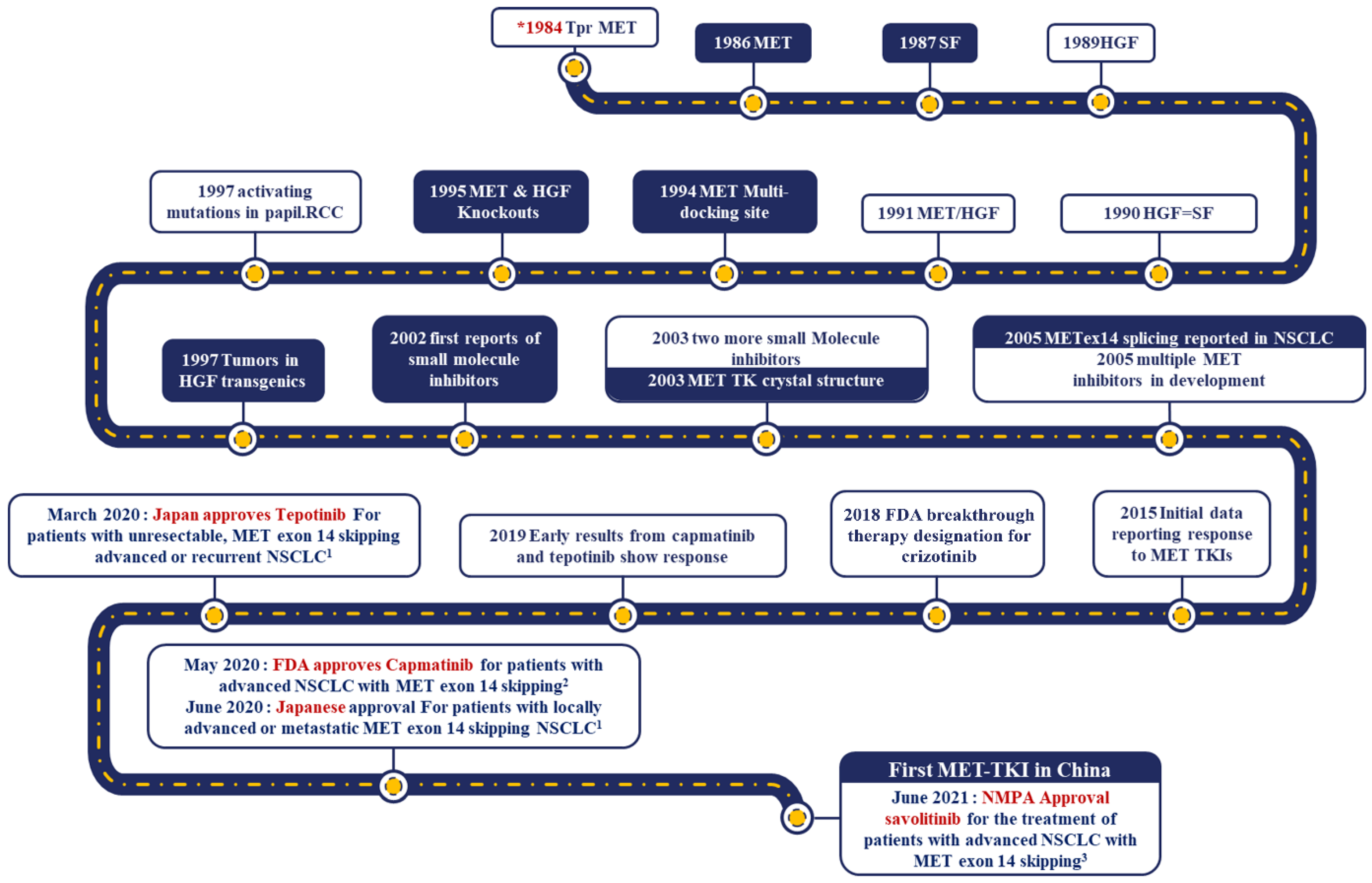
1. Introduction
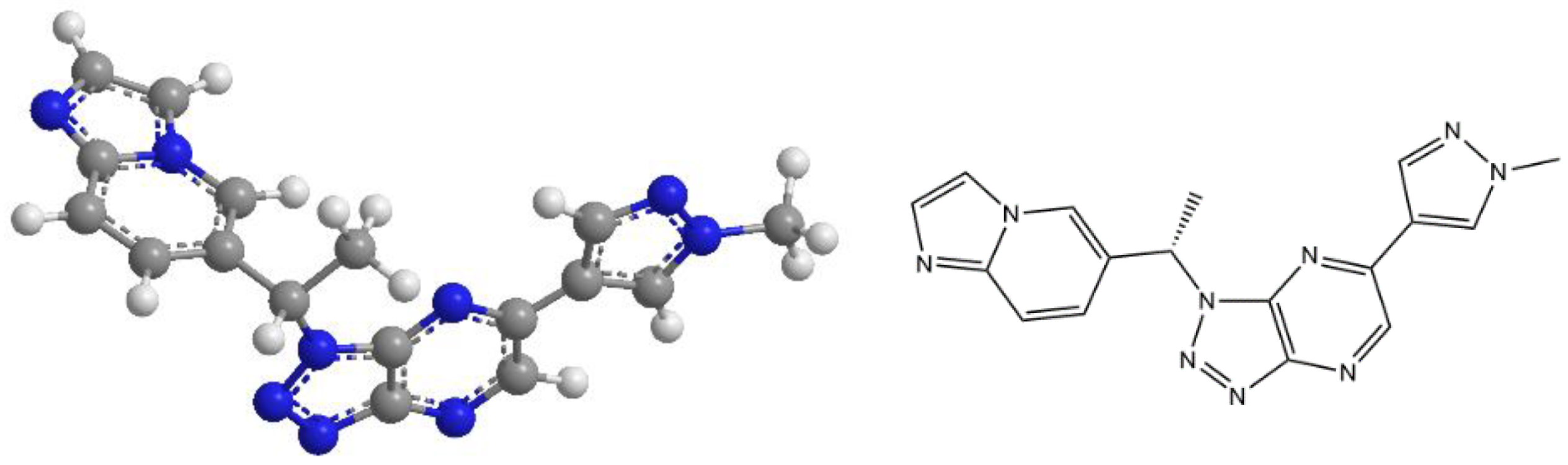
2. Savolitinib, in Brief
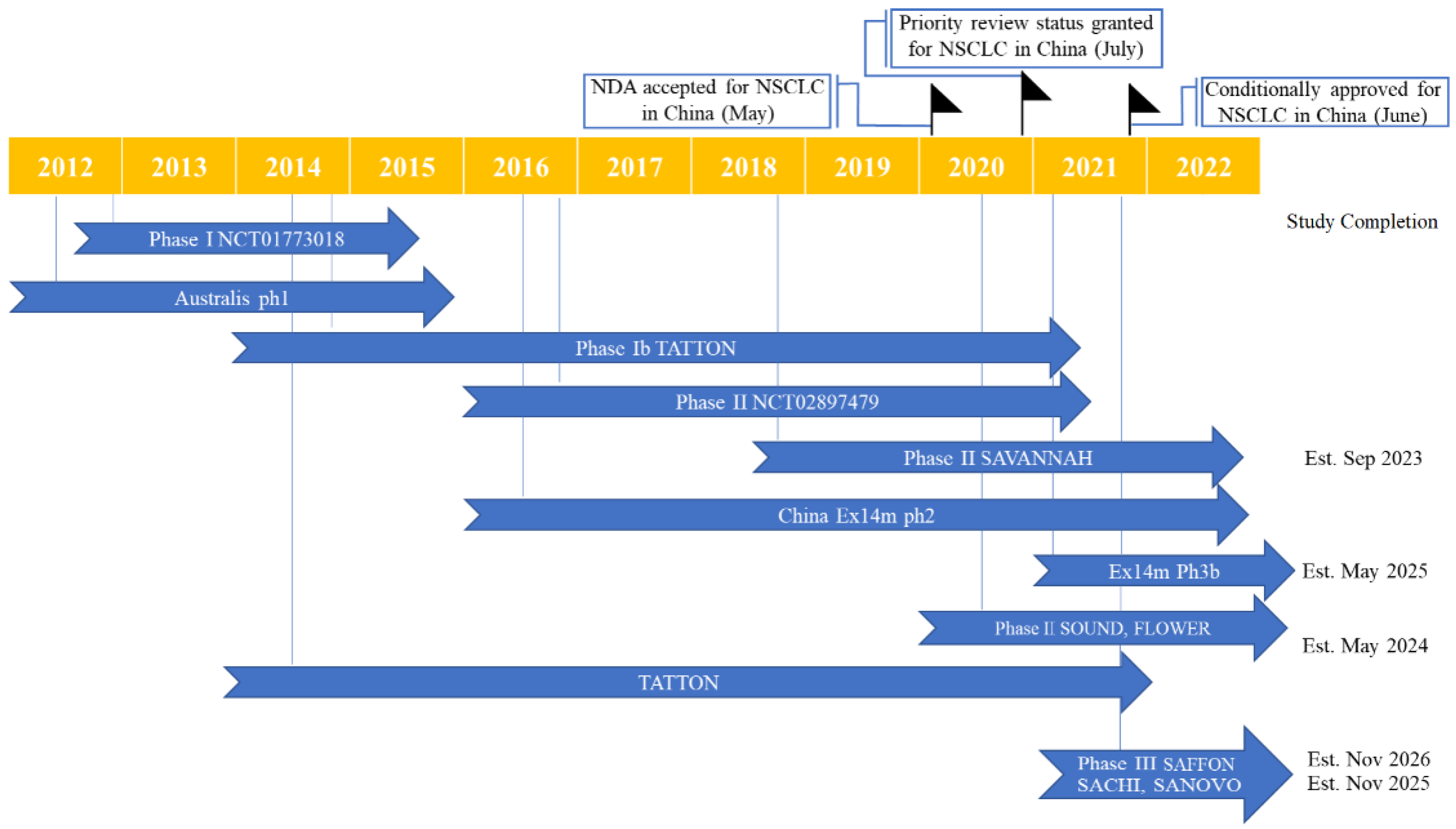
3. First Steps towards the Development of Savolitinib as Mono and Combination Therapies
4. Clinical Development of Savolitinib: Phase I Trials
5. Clinical Development of Savolitinib: Phase II Trials
5.1. Efficacy Evidence
5.2. Safety Evidence
5.3. Brief Introduction of Other Phase II Trials
6. Ongoing Phase III Trials
7. Discussion
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Cancer.Net. Lung Cancer—Non-Small Cell: Statistics. Available online: https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/statistics (accessed on 12 June 2022).
- Yuan, M.; Huang, L.L.; Chen, J.H.; Wu, J.; Xu, Q. The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal. Transduct. Target Ther. 2019, 4, 61. [Google Scholar] [CrossRef] [PubMed]
- Liam, C.K.; Stone, E.; Andarini, S.; Liam, Y.S.; Lam, D.C.L.; Lee, P. Molecular testing of metastatic non-small cell lung cancer in the Asia-Pacific region. Respirology 2020, 25, 685–687. [Google Scholar] [CrossRef] [PubMed]
- Drilon, A.; Cappuzzo, F.; Ou, S.H.I.; Camidge, D.R. Targeting MET in Lung Cancer: Will Expectations Finally Be MET? J. Thorac. Oncol. 2017, 12, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Santarpia, M.; Massafra, M.; Gebbia, V.; D’Aquino, A.; Garipoli, C.; Altavilla, G.; Rosell, R. A narrative review of MET inhibitors in non-small cell lung cancer with MET exon 14 skipping mutations. Transl. Lung Cancer Res. 2021, 10, 1536–1556. [Google Scholar] [CrossRef] [PubMed]
- Davies, K.D.; Ritterhouse, L.L.; Snow, A.N.; Sidiropoulos, N. MET Exon 14 Skipping Mutations: Essential Considerations for Current Management of Non-Small Cell Lung Cancer. J. Mol. Diagn. 2022, 24, 841–843. [Google Scholar] [CrossRef]
- Stoker, M.; Gherardi, E.; Perryman, M.; Gray, J. Scatter factor is a fibroblast-derived modulator of epithelial cell mobility. Nature 1987, 327, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Weidner, K.M.; Behrens, J.; Vandekerckhove, J.; Birchmeier, W. Scatter factor: Molecular characteristics and effect on the invasiveness of epithelial cells. J. Cell Biol. 1990, 111, 2097–2108. [Google Scholar] [CrossRef]
- Kaposi-Novak, P.; Lee, J.S.; Gòmez-Quiroz, L.; Coulouarn, C.; Factor, V.M.; Thorgeirsson, S.S. Met-regulated expression signature defines a subset of human hepatocellular carcinomas with poor prognosis and aggressive phenotype. J. Clin. Investig. 2006, 116, 1582–1595. [Google Scholar] [CrossRef]
- Baldanzi, G.; Graziani, A. Physiological Signaling and Structure of the HGF Receptor MET. Biomedicines 2014, 3, 1–31. [Google Scholar] [CrossRef]
- Raghav, K.; Bailey, A.M.; Loree, J.M.; Kopetz, S.; Holla, V.; Yap, T.A.; Wang, F.; Chen, K.; Salgia, R.; Hong, D. Untying the gordion knot of targeting MET in cancer. Cancer Treat. Rev. 2018, 66, 95–103. [Google Scholar] [CrossRef]
- Jo, M.; Stolz, D.B.; Esplen, J.E.; Dorko, K.; Michalopoulos, G.K.; Strom, S.C. Cross-talk between epidermal growth factor receptor and c-Met signal pathways in transformed cells. J. Biol. Chem. 2000, 275, 8806–8811. [Google Scholar] [CrossRef] [PubMed]
- Soman, N.R.; Correa, P.; Ruiz, B.A.; Wogan, G.N. The TPR-MET oncogenic rearrangement is present and expressed in human gastric carcinoma and precursor lesions. Proc. Natl. Acad. Sci. USA 1991, 88, 4892–4896. [Google Scholar] [CrossRef] [PubMed]
- Socinski, M.A.; Pennell, N.A.; Davies, K.D. MET Exon 14 Skipping Mutations in Non-Small-Cell Lung Cancer: An Overview of Biology, Clinical Outcomes, and Testing Considerations. JCO Precis. Oncol. 2021, 5, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Mo, H.N.; Liu, P. Targeting MET in cancer therapy. Chronic Dis. Transl. Med. 2017, 3, 148–153. [Google Scholar] [CrossRef]
- Tong, J.H.; Yeung, S.F.; Chan, A.W.H.; Chung, L.Y.; Chau, S.L.; Lung, R.W.M.; Tong, C.Y.; Chow, C.; Tin, E.K.Y.; Yu, Y.H.; et al. MET Amplification and Exon 14 Splice Site Mutation Define Unique Molecular Subgroups of Non-Small Cell Lung Carcinoma with Poor Prognosis. Clin. Cancer Res. 2016, 22, 3048–3056. [Google Scholar] [CrossRef]
- Guo, R.; Luo, J.; Chang, J.; Rekhtman, N.; Arcila, M.; Drilon, A. MET-dependent solid tumours—Molecular diagnosis and targeted therapy. Nat. Rev. Clin. Oncol. 2020, 17, 569–587. [Google Scholar] [CrossRef]
- Recondo, G.; Che, J.; Jänne, P.A.; Awad, M.M. Targeting MET Dysregulation in Cancer. Cancer Discov. 2020, 10, 922–934. [Google Scholar] [CrossRef]
- Engelman, J.A.; Zejnullahu, K.; Mitsudomi, T.; Song, Y.; Hyland, C.; Park, J.O.; Lindeman, N.; Gale, C.M.; Zhao, X.; Christensen, J.; et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 2007, 316, 1039–1043. [Google Scholar] [CrossRef]
- Zhang, Z.; Yang, S.; Wang, Q. Impact of MET alterations on targeted therapy with EGFR-tyrosine kinase inhibitors for EGFR-mutant lung cancer. Biomark. Res. 2019, 7, 27. [Google Scholar] [CrossRef]
- Bean, J.; Brennan, C.; Shih, J.Y.; Riely, G.; Viale, A.; Wang, L.; Chitale, D.; Motoi, N.; Szoke, J.; Broderick, S.; et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc. Natl. Acad. Sci. USA 2007, 104, 20932–20937. [Google Scholar] [CrossRef]
- Wang, Y.; Li, L.; Han, R.; Jiao, L.; Zheng, J.; He, Y. Clinical analysis by next-generation sequencing for NSCLC patients with MET amplification resistant to osimertinib. Lung Cancer 2018, 118, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Li, X.M.; Li, W.F.; Lin, J.T.; Yan, H.H.; Tu, H.Y.; Chen, H.J.; Wang, B.C.; Wang, Z.; Zhou, Q.; Zhang, X.C.; et al. Predictive and Prognostic Potential of TP53 in Patients with Advanced Non-Small-Cell Lung Cancer Treated With EGFR-TKI: Analysis of a Phase III Randomized Clinical Trial (CTONG 0901. Clin. Lung Cancer 2021, 22, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Lai, G.G.Y.; Lim, T.H.; Lim, J.; Liew, P.J.R.; Kwang, X.L.; Nahar, R.; Aung, Z.W.; Takano, A.; Lee, Y.Y.; Lau, D.P.X.; et al. Clonal MET Amplification as a Determinant of Tyrosine Kinase Inhibitor Resistance in Epidermal Growth Factor Receptor-Mutant Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2019, 37, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Camidge, D.R.; Barlesi, F.; Goldman, J.W.; Morgensztern, D.; Heist, R.; Vokes, E.; Angevin, E.; Hong, D.S.; Rybkin, I.I.; Barve, M.; et al. A Phase Ib Study of 25 in Combination with Nivolumab in Patients With NSCLC. JTO Clin. Res. Rep. 2022, 3, 100262. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, L.N.; Larkins, E.; Akinboro, O.; Roy, P.; Amatya, A.K.; Fiero, M.H.; Mishra-Kalyani, P.S.; Helms, W.S.; Myers, C.E.; Skinner, A.M.; et al. FDA Approval Summary: Capmatinib and Tepotinib for the Treatment of Metastatic NSCLC Harboring MET Exon 14 Skipping Mutations or Alterations. Clin. Cancer Res. 2022, 28, 249–254. [Google Scholar] [CrossRef]
- Pfizer. Pfizer’s XALKORI® (Crizotinib) Receives FDA Breakthrough Therapy Designation in Two New Indications. Available online: https://www.pfizer.com/news/press-release/press-release-detail/pfizer_s_xalkori_crizotinib_receives_fda_breakthrough_therapy_designation_in_two_new_indications-0 (accessed on 12 June 2022).
- AstraZeneca. Orpathys Approved in China for Patients with Lung Cancer and MET Gene Alterations. Available online: https://www.astrazeneca.com/media-centre/press-releases/2021/orpathys-approved-in-china-for-patients-with-lung-cancer-and-met-gene-alterations.html (accessed on 12 June 2022).
- Sequist, L.V.; Han, J.Y.; Ahn, M.J.; Cho, B.C.; Yu, H.; Kim, S.W.; Yang, J.C.; Lee, J.S.; Su, W.C.; Kowalski, D.; et al. Osimertinib plus savolitinib in patients with EGFR mutation-positive, MET-amplified, non-small-cell lung cancer after progression on EGFR tyrosine kinase inhibitors: Interim results from a multicentre, open-label, phase Ib study. Lancet Oncol. 2020, 21, 373–386. [Google Scholar] [CrossRef]
- Yang, J.J.; Fang, J.; Shu, Y.Q.; Chang, J.H.; Chen, G.Y.; He, J.X.; Li, W.; Liu, X.Q.; Yang, N.; Zhou, C.; et al. A phase Ib study of the highly selective MET-TKI savolitinib plus gefitinib in patients with EGFR-mutated, MET-amplified advanced non-small-cell lung cancer. Investig. New Drugs. 2021, 39, 477–487. [Google Scholar] [CrossRef]
- Markham, A. Savolitinib: First Approval. Drugs 2021, 81, 1665–1670. [Google Scholar] [CrossRef]
- Hong, L.; Zhang, J.; Heymach, J.V.; Le, X. Current and future treatment options for MET exon 14 skipping alterations in non-small cell lung cancer. Ther. Adv. Med. Oncol. 2021, 13, 1758835921992976. [Google Scholar] [CrossRef]
- Schuller, A.G.; Barry, E.R.; Jones, R.D.O.; Henry, R.E.; Frigault, M.M.; Beran, G.; Linsenmayer, D.; Hattersley, M.; Smith, A.; Wilson, J.; et al. The MET Inhibitor AZD6094 (Savolitinib, HMPL-504) Induces Regression in Papillary Renal Cell Carcinoma Patient-Derived Xenograft Models. Clin. Cancer Res. 2015, 21, 2811–2819. [Google Scholar] [CrossRef]
- Gavine, P.R.; Ren, Y.; Han, L.; Lv, J.; Fan, S.; Zhang, W.; Xu, W.; Liu, Y.J.; Zhang, T.; Fu, H.; et al. Volitinib, a potent and highly selective c-Met inhibitor, effectively blocks c-Met signaling and growth in c-MET amplified gastric cancer patient-derived tumor xenograft models. Mol. Oncol. 2015, 9, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; Sai, Y.; Wang, J.; Yu, M.; Wang, G.; Zhang, L.; Ren, H.; Fan, S.; Ren, Y.; Qing, W.; et al. Preclinical pharmacokinetics, disposition, and translational pharmacokinetic/pharmacodynamic modeling of savolitinib, a novel selective cMet inhibitor. Eur. J. Pharm. Sci. 2019, 136, 104938. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.D.O.; Grondine, M.; Borodovsky, A.; San Martin, M.; DuPont, M.; D’Cruz, C.; Schuller, A.; Henry, R.; Barry, E.; Castriotta, L.; et al. A pharmacokinetic-pharmacodynamic model for the MET tyrosine kinase inhibitor, savolitinib, to explore target inhibition requirements for anti-tumour activity. Br. J. Pharmacol. 2021, 178, 600–613. [Google Scholar] [CrossRef] [PubMed]
- Ding, Q.; Ou, M.; Zhu, H.; Wang, Y.; Jia, J.; Sai, Y.; Chen, Q.; Wang, J. Effect of food on the single-dose pharmacokinetics and tolerability of savolitinib in Chinese healthy volunteers. Fundam. Clin. Pharmacol. 2022, 36, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Fang, J.; Li, X.; Cao, L.; Zhou, J.; Guo, Q.; Liang, Z.; Cheng, Y.; Jiang, L.; Yang, N.; et al. Once-daily savolitinib in Chinese patients with pulmonary sarcomatoid carcinomas and other non-small-cell lung cancers harbouring MET exon 14 skipping alterations: A multicentre, single-arm, open-label, phase 2 study. Lancet Respir. Med. 2021, 9, 1154–1164. [Google Scholar] [CrossRef]
- Henry, R.E.; Barry, E.R.; Castriotta, L.; Ladd, B.; Markovets, A.; Beran, G.; Ren, Y.; Zhou, F.; Adam, A.; Zinda, M.; et al. Acquired savolitinib resistance in non-small cell lung cancer arises via multiple mechanisms that converge on MET-independent mTOR and MYC activation. Oncotarget 2016, 7, 57651–57670. [Google Scholar] [CrossRef]
- Dua, R.; Zhang, J.; Parry, G.; Penuel, E. Detection of hepatocyte growth factor (HGF) ligand-c-MET receptor activation in formalin-fixed paraffin embedded specimens by a novel proximity assay. PLoS ONE 2011, 6, e15932. [Google Scholar] [CrossRef]
- Li, Y.; Dong, S.; Tamaskar, A.; Wang, H.; Zhao, J.; Ma, H.; Zhao, Y. Proteasome Inhibitors Diminish c-Met Expression and Induce Cell Death in Non-Small Cell Lung Cancer Cells. Oncol. Res. 2020, 28, 497–507. [Google Scholar] [CrossRef]
- Gan, H.K.; Millward, M.; Hua, Y.; Qi, C.; Sai, Y.; Su, W.; Wang, J.; Zhang, L.; Frigault, M.M.; Morgan, S.; et al. First-in-Human Phase I Study of the Selective MET Inhibitor, Savolitinib, in Patients with Advanced Solid Tumors: Safety, Pharmacokinetics, and Antitumor Activity. Clin. Cancer Res. 2019, 25, 4924–4932. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, T.; Chen, G.; Gong, J.; Bai, Y.; Zhang, T.; Xu, N.; Liu, L.; Xu, J.; He, J.; et al. Phase Ia/Ib Study of the Selective MET Inhibitor, Savolitinib, in Patients with Advanced Solid Tumors: Safety, Efficacy, and Biomarkers. Oncologist 2022, 27, e342–e383. [Google Scholar] [CrossRef]
- Oxnard, G.R.; Yang, J.C.H.; Yu, H.; Kim, S.W.; Saka, H.; Horn, L.; Goto, K.; Ohe, Y.; Mann, H.; Thress, K.S.; et al. TATTON: A multi-arm, phase Ib trial of osimertinib combined with selumetinib, savolitinib, or durvalumab in EGFR-mutant lung cancer. Ann. Oncol. 2020, 31, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Hartmaier, R.J.; Markovets, A.A.; Ahn, M.J.; Sequist, L.V.; Han, J.Y.; Cho, B.C.; Yu, H.A.; Kim, S.W.; Yang, J.C.; Lee, J.S.; et al. Osimertinib+Savolitinib to Overcome Acquired MET-Mediated Resistance in Epidermal Growth Factor Receptor Mutated MET-Amplified Non-Small Cell Lung Cancer: TATTON. Cancer Discov. 2022, 20, CD-22-0586. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Fang, J.; Li, X.; Cao, L.; Zhou, J.; Guo, Q.; Liang, Z.; Cheng, Y.; Jiang, L.; Yang, N.; et al. Final OS results and subgroup analysis of savolitinib in patients with MET exon 14 skipping mutations (METex14+) NSCLC. In Proceedings of the ELCC 2022 Virtual Meeting, Virtual, 30 March–2 April 2022. [Google Scholar]
- Lu, S.; Fang, J.; Cao, L.; Li, X.; Guo, Q.; Zhou, J.; Cheng, Y.; Jiang, L.; Chen, Y.; Zhang, H.; et al. Abstract CT031: Preliminary efficacy and safety results of savolitinib treating patients with pulmonary sarcomatoid carcinoma (PSC) and other types of non-small cell lung cancer (NSCLC) harboring MET exon 14 skipping mutations. In Proceedings of the AACR Annual Meeting 2019, Atlanta, GA, USA, 29 March–3 April 2019. [Google Scholar]
- Lu, S.; Fang, J.; Li, X.; Cao, L.; Zhou, J.; Guo, Q.; Liang, Z.; Cheng, Y.; Jiang, L.; Yang, N.; et al. Long-Term Efficacy, Safety and Subgroup Analysis of Savolitinib in Chinese Patients with Non-Small Cell Lung Cancers Harboring MET Exon 14 Skipping Alterations. JTO Clin. Res. Rep. 2022, 3, 100407. [Google Scholar] [CrossRef] [PubMed]
- Gow, C.H.; Hsieh, M.S.; Wu, S.G.; Shih, J.Y. A comprehensive analysis of clinical outcomes in lung cancer patients harboring a MET exon 14 skipping mutation compared to other driver mutations in an East Asian population. Lung Cancer 2017, 103, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Manochakian, R.; James, L.; Azzouqa, A.G.; Shi, H.; Zhang, Y.; Zhao, Y.; Zhou, K.; Lou, Y. Emerging therapeutic agents for advanced non-small cell lung cancer. J. Hematol. Oncol. 2020, 13, 58. [Google Scholar] [CrossRef]
- Bae, H.M.; Min, H.S.; Lee, S.H.; Kim, D.W.; Chung, D.H.; Lee, J.S.; Kim, Y.W.; Heo, D.S. Palliative chemotherapy for pulmonary pleomorphic carcinoma. Lung Cancer 2007, 58, 112–115. [Google Scholar] [CrossRef]
- Ung, M.; Rouquette, I.; Filleron, T.; Taillandy, K.; Brouchet, L.; Bennouna, J.; Delord, J.P.; Milia, J.; Mazières, J. Characteristics and Clinical Outcomes of Sarcomatoid Carcinoma of the Lung. Clin. Lung Cancer. 2016, 17, 391–397. [Google Scholar] [CrossRef]
- Vieira, T.; Girard, N.; Ung, M.; Monnet, I.; Cazes, A.; Bonnette, P.; Duruisseaux, M.; Mazieres, J.; Antoine, M.; Cadranel, J.; et al. Efficacy of first-line chemotherapy in patients with advanced lung sarcomatoid carcinoma. J. Thorac. Oncol. 2013, 8, 1574–1577. [Google Scholar] [CrossRef]
- Hong, J.Y.; Choi, M.K.; Uhm, J.E.; Park, M.J.; Lee, J.; Park, Y.H.; Ahn, J.S.; Park, K.; Han, J.H.; Ahn, M.J. The role of palliative chemotherapy for advanced pulmonary pleomorphic carcinoma. Med. Oncol. 2009, 26, 287–291. [Google Scholar] [CrossRef]
- Cheng, H.; Perez-Soler, R. Leptomeningeal metastases in non-small-cell lung cancer. Lancet Oncol. 2018, 19, e43–e55. [Google Scholar] [CrossRef]
- Deeken, J.F.; Löscher, W. The blood-brain barrier and cancer: Transporters, treatment, and Trojan horses. Clin. Cancer Res. 2007, 13, 1663–1674. [Google Scholar] [CrossRef] [PubMed]
- Choueiri, T.K.; Heng, D.Y.C.; Lee, J.L.; Cancel, M.; Verheijen, R.B.; Mellemgaard, A.; Ottesen, L.H.; Frigault, M.M.; L’Hernault, A.; Szijgyarto, Z.; et al. Efficacy of Savolitinib vs Sunitinib in Patients With MET-Driven Papillary Renal Cell Carcinoma: The SAVOIR Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- Cortot, A.; Le, X.; Smit, E.; Viteri, S.; Kato, T.; Sakai, H.; Park, K.; Camidge, D.R.; Berghoff, K.; Vlassak, S.; et al. Safety of MET Tyrosine Kinase Inhibitors in Patients with MET Exon 14 Skipping Non-small Cell Lung Cancer: A Clinical Review. Clin. Lung Cancer 2022, 3, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Paik, P.K.; Felip, E.; Veillon, R.; Sakai, H.; Cortot, A.B.; Garassino, M.C.; Mazieres, J.; Viteri, S.; Senellart, H.; Meerbeeck, J.V.; et al. Tepotinib in Non-Small-Cell Lung Cancer with MET Exon 14 Skipping Mutations. N. Engl. J. Med. 2020, 383, 931–943. [Google Scholar] [CrossRef]
- Ahn, M.J.; De Marinis, F.; Bonanno, L.; Cho, B.C.; Kim, T.M.; Cheng, S.; Novello, S.; Proto, C.; Kim, S.W.; Lee, J.S.; et al. MET Biomarker-based Preliminary Efficacy Analysis in SAVANNAH: Savolitinib+osimertinib in EGFRm NSCLC Post-Osimertinib. In Proceedings of the WCLC 2022, Vienna, Austria, 6–9 August 2022. [Google Scholar]
- Li, A.; Chen, H.J.; Yang, J.J. Design and Rationale for a Phase II, Randomized, Open-Label, Two-Cohort Multicenter Interventional Study of Osimertinib with or Without Savolitinib in De Novo MET Aberrant, EGFR-Mutant Patients with Advanced Non-Small-Cell Lung Cancer: The FLOWERS Trial. Clin. Lung Cancer 2022, 22, 00205-4. [Google Scholar] [CrossRef]
- Wolf, J.; Garon, E.B.; Groen, H.J.M.; Tan, D.S.W.; Robeva, A.; Le Mouhaer, S.; Carbini, M.; Chassot-Agostinho, A.; Heist, R.S. Capmatinib in MET exon 14-mutated, advanced NSCLC: Updated results from the GEOMETRY mono-1 study. In Proceedings of the 2021 ASCO Annual Meeting I, Virtual, 4–8 June 2021. [Google Scholar]
- Thomas, M.; Garassino, M.; Felip, E.; Sakai, H.; Le, X.; Veillon, R.; Smit, E.; Mazieres, J.; Cortot, A.; Raskin, J.; et al. Tepotinib in Patients with MET Exon 14 (METex14) Skipping NSCLC: Primary Analysis of the Confirmatory VISION Cohort C. In Proceedings of the WCLC 2022, Vienna, Austria, 6–9 August 2022. [Google Scholar]
- Krebs, M.; Spira, A.I.; Cho, B.C.; Besee, B.; Goldman, J.W.; Janne, P.A.; Ma, Z.; Mansfield, A.S.; Minchom, A.R.; Ou, S.H.I.; et al. Amivantamab in patients with NSCLC with MET exon 14 skipping mutation: Updated results from the CHRYSALIS study. In Proceedings of the 2022 ASCO Annual Meeting, Chicago, IL, USA, 3–7 June 2022. [Google Scholar]
- Yu, Y.; Ren, Y.; Fang, J.; Cao, L.; Liang, Z.; Guo, Q.; Han, S.; Ji, Z.; Wang, Y.; Sun, Y.; et al. Circulating tumour DNA biomarkers in savolitinib-treated patients with non-small cell lung cancer harbouring MET exon 14 skipping alterations: A post hoc analysis of a pivotal phase 2 study. Ther. Adv. Med. Oncol. 2022, 14, 17588359221133546. [Google Scholar] [CrossRef]
- Le, X.; Sakai, H.; Felip, E.; Veillon, R.; Garassino, M.C.; Raskin, J.; Cortot, A.B.; Viteri, S.; Mazieres, J.; Smit, E.F.; et al. Tepotinib Efficacy and Safety in Patients with MET Exon 14 Skipping NSCLC: Outcomes in Patient Subgroups from the VISION Study with Relevance for Clinical Practice. Clin. Cancer Res. 2022, 28, 1117–1126. [Google Scholar] [CrossRef]
- Wolf, J.; Seto, T.; Han, J.Y.; Reguart, N.; Garon, E.B.; Groen, H.J.M.; Tan, D.S.W.; Hida, T.; de Jonge, M.; Orlov, S.V.; et al. Capmatinib in MET Exon 14-Mutated or MET-Amplified Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2020, 383, 944–957. [Google Scholar] [CrossRef]
- Paik, P.K.; Sakai, H.; Felip, E.; Veillon, R.; Garassino, M.C.; Raskin, J.; Viteri, S.; Mazieres, J.; Cortot, A.; Smit, E.; et al. Tepotinib in patients with MET exon 14 (METex14) skipping advanced NSCLC: Updated efficacy from VISION Cohort A. In Proceedings of the WCLC 2020, Virtual, 28–31 January 2021. [Google Scholar]
- Spira, A.; Krebs, M.; Cho, B.C.; Besse, B.; Goldman, J.; Janne, P.; Lee, C.K.; Ma, Z.; Mansfield, A.; Minchom, A.; et al. Amivantamab in non-small cell lung cancer with MET exon 14 skipping muta- tion: Initial results from CHRYSALIS. In Proceedings of the WCLC 2021, Virtual, 8–14 September 2021. [Google Scholar]
- Fujino, T.; Kobayashi, Y.; Suda, K.; Koga, T.; Nishino, M.; Ohara, S.; Chiba, M.; Shimoji, M.; Tomizawa, K.; Takemoto, T.; et al. Sensitivity and Resistance of MET Exon 14 Mutations in Lung Cancer to Eight MET Tyrosine Kinase Inhibitors In Vitro. J. Thorac. Oncol. 2019, 14, 1753–1765. [Google Scholar] [CrossRef]
- Wolf, J.; Garon, E.B.; Groen, H.J.M.; Tan, D.S.W.; Robeva, A.; Le Mouhaer, S.; Carbini, M.; Yovine, A.; Heist, R. Capmatinib in treatment (Tx)-naive MET exon 14-mutated (METex14) advanced non-small cell lung cancer (aNSCLC): Updated results from GEOMETRY mono-1. In Proceedings of the ELCC 2022 Virtual Meeting, Virtual, 30 March–2 April 2022. [Google Scholar]
- Moro-Sibilot, D.; Cozic, N.; Pérol, M.; Mazières, J.; Otto, J.; Souquet, P.J.; Bahleda, R.; Wislez, M.; Zalcman, G.; Guibert, S.D.; et al. Crizotinib in c-MET- or ROS1-positive NSCLC: Results of the AcSé phase II trial. Ann. Oncol. 2019, 30, 1985–1991. [Google Scholar] [CrossRef]
- Drilon, A.; Clark, J.W.; Weiss, J.; Ou, S.I.; Camidge, D.R.; Solomon, B.J.; Otterson, G.A.; Villaruz, L.C.; Riely, G.J.; Heist, R.S.; et al. Antitumor activity of crizotinib in lung cancers harboring a MET exon 14 alteration. Nat. Med. 2020, 26, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Reis, H.; Metzenmacher, M.; Goetz, M.; Savvidou, N.; Darwiche, K.; Aigner, C.; Herold, T.; Eberhardt, W.E.; Skiba, C.; Hense, J.; et al. MET Expression in Advanced Non-Small-Cell Lung Cancer: Effect on Clinical Outcomes of Chemotherapy, Targeted Therapy, and Immunotherapy. Clin. Lung Cancer 2018, 19, e441–e463. [Google Scholar] [CrossRef] [PubMed]
- Wood, G.E.; Hockings, H.; Hilton, D.M.; Kermorgant, S. The role of MET in chemotherapy resistance. Oncogene 2021, 40, 1927–1941. [Google Scholar] [CrossRef] [PubMed]
- Bauml, J.; Cho, B.C.; Park, K.; Lee, K.H.; Cho, E.K.; Kim, D.W.; Kim, S.W.; Haura, E.B.; Sabari, J.K.; Sanborn, R.E.; et al. Amivantamab in combination with lazertinib for the treatment of osimertinib-relapsed, chemotherapy-naïve EGFR mutant (EGFRm) non-small cell lung cancer (NSCLC) and potential biomarkers for response. In Proceedings of the 2021 ASCO Annual Meeting I, Virtual, 4–8 June 2021. [Google Scholar]
- Park, K.; Zhou, J.; Kim, D.; Ahmad, A.R.; Soo, R.A.; Bruns, R.; Straub, J.; Johne, A.; Scheele, J.; Yang, J.C.; et al. Tepotinib plus gefitinib in patients with MET-amplified EGFR-mutant NSCLC: Long-term outcomes of the INSIGHT study. In Proceedings of the ESMO Asia Congress 2019, Singapore, 22–24 November 2019. [Google Scholar]
- Haratani, K.; Hayashi, H.; Tanaka, T.; Kaneda, H.; Togashi, Y.; Sakai, K.; Hayashi, K.; Tomida, S.; Yonesaka, K.; Nonagase, Y.; et al. Tumor immune microenvironment and nivolumab efficacy in EGFR mutation-positive non-small-cell lung cancer based on T790M status after disease progression during EGFR-TKI treatment. Ann. Oncol. 2017, 28, 1532–1539. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, H.; Sugawara, S.; Fukuda, Y.; Fujimoto, D.; Miura, S.; Ota, K.; Ozawa, Y.; Hara, S.; Tanizaki, J.; Azuma, K.; et al. A Randomized Phase II Study Comparing Nivolumab with Carboplatin-Pemetrexed for EGFR-Mutated NSCLC with Resistance to EGFR Tyrosine Kinase Inhibitors (WJOG8515L. Clin. Cancer Res. 2022, 28, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Mok, T.; Socinski, M.A.; Jotte, R.M.; Lim, D.W.; Cappuzzo, F.; Orlandi, F.J.; Stroyakovskiy, D.; Nogami, N.; Rodriguez-Abreu, D.; et al. IMpower150: Updated efficacy analysis in patients with EGFR mutations. In Proceedings of the ESMO Virtual Congress 2020, Virtual, 19–21 September 2020. [Google Scholar]
- Lu, S.; Wu, L.; Jian, H.; Chen, Y.; Wang, Q.; Fang, J.; Wang, Z.; Hu, Y.; Sun, M.; Han, L.; et al. Sintilimab plus bevacizumab biosimilar IBI305 and chemotherapy for patients with EGFR-mutated non-squamous non-small-cell lung cancer who progressed on EGFR tyrosine-kinase inhibitor therapy (ORIENT-31): First interim results from a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2022, 23, 1167–1179. [Google Scholar] [CrossRef] [PubMed]
- Baldacci, S.; Mazieres, J.; Tomasini, P.; Girard, N.; Guisier, F.; Audigier-Valette, C.; Monnet, I.; Wislez, M.; Pérol, M.; Dô, P.; et al. Outcome of EGFR-mutated NSCLC patients with MET-driven resistance to EGFR tyrosine kinase inhibitors. Oncotarget 2017, 8, 105103–105114. [Google Scholar] [CrossRef]
- Baldacci, S.; Kherrouche, Z.; Cockenpot, V.; Stoven, L.; Copin, M.C.; Werkmeister, E.; Marchand, N.; Kyheng, M.; Tulasne, D.; Cortot, A.B. MET amplification increases the metastatic spread of EGFR-mutated NSCLC. Lung Cancer 2018, 125, 57–67. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, S.; Wang, K.; Sun, S.Y. MET inhibitors for targeted therapy of EGFR TKI-resistant lung cancer. J. Hematol. Oncol. 2019, 12, 63. [Google Scholar] [CrossRef]
- Yu, H.A.; Ambrose, H.; Baik, C.; Cho, B.C.; Cocco, E.; Goldberg, S.B.; Goldman, J.W.; Kraljevic, S.; de Langen, A.J.; Okamoto, I.; et al. ORCHARD osimertinib + savolitinib interim analysis: A biomarker-directed phase II platform study in patients (pts) with advanced non-small cell lung cancer (NSCLC) whose disease has progressed on first-line (1L) osimertinib. In Proceedings of the ESMO Congress 2021, Paris, France, 16–21 September 2021. [Google Scholar]
- Wu, Y.L.; Zhang, L.; Kim, D.W.; Liu, X.; Lee, D.H.; Yang, J.C.H.; Ahn, M.J.; Vansteenkiste, J.F.; Su, W.C.; Felip, E.; et al. Phase Ib/II Study of Capmatinib (INC280) Plus Gefitinib After Failure of Epidermal Growth Factor Receptor (EGFR) Inhibitor Therapy in Patients With EGFR-Mutated, MET Factor-Dysregulated Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2018, 36, 3101–3109. [Google Scholar] [CrossRef]
- Wu, Y.L.; Cheng, Y.; Zhou, J.; Lu, S.; Zhang, Y.; Zhao, J.; Kim, D.W.; Soo, R.A.; Kim, S.W.; Pan, H.; et al. Tepotinib plus gefitinib in patients with EGFR-mutant non-small-cell lung cancer with MET overexpression or MET amplification and acquired resistance to previous EGFR inhibitor (INSIGHT study): An open-label, phase Ib/2, multicentre, randomised trial. Lancet Respir Med. 2020, 8, 1132–1143. [Google Scholar] [CrossRef] [PubMed]
- Liam, C.K.; Ahmad, A.R.; Hsia, T.C.; Zhou, J.; Kim, D.W.; Soo, R.A.; Cheng, Y.; Lu, S.; Shin, S.W.; Yang, J.C.H.; et al. Tepotinib + gefitinib in patients with EGFR-mutant NSCLC with MET amplification: Final analysis of INSIGHT. In Proceedings of the 2022 AACR Annual Meeting, New Orleans, LA, USA, 8–13 April 2022. [Google Scholar]
- Goldman, J.W.; Horinouchi, H.; Cho, B.C.; Tomasini, P.; Dunbar, M.; Hoffman, D.; Parikh, A.; Blot, V.; Camidge, D.R. Phase 1/1b study of telisotuzumab vedotin (Teliso-V) + osimertinib (Osi), after failure on prior Osi, in patients with advanced, c-Met overexpressing, EGFR-mutated non-small cell lung cancer (NSCLC. In Proceedings of the 2022 ASCO Annual Meeting, Chicago, IL, USA, 3–7 June 2022. [Google Scholar]
- Yin, W.; Cheng, J.; Tang, Z.; Toruner, G.; Hu, S.; Guo, M.; Robinson, M.; Medeiros, L.J.; Tang, G. MET Amplification (MET/CEP7 Ratio ≥ 1.8) Is an Independent Poor Prognostic Marker in Patients with Treatment-naive Non-Small-cell Lung Cancer. Clin. Lung Cancer 2021, 22, e512–e518. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Chen, H.; Tang, Z.; Kalhor, N.; Liu, C.H.; Yao, H.; Hu, S.; Lin, P.; Zhao, J.; Luthra, R.; et al. MET amplification assessed using optimized FISH reporting criteria predicts early distant metastasis in patients with non-small cell lung cancer. Oncotarget 2018, 9, 12959–12970. [Google Scholar] [CrossRef] [PubMed][Green Version]
| MET Alterations | Proportion, % | Publication [Reference] | |
|---|---|---|---|
| METex14 | NSCLC 1 | 0.9–4 | Davies KD et al. [6] |
| PSC subtype | 20–31.8 | Mo HN et al. [15] Tong JH et al. [16] | |
| MET Fusion 1 | 0.5 | Recondo G et al. [18] | |
| MET Overexpression 1 | 13.7–63.7 | Guo R et al. [17] | |
| MET Amplification 2 | 1–5 | Guo R et al. [17] | |
| Secondary MET Amplification | 1/2G EGFR–TKI resistance | 5–22 | Recondo G et al. [18] Bean J et al. [21] |
| 3G EGFR–TKI resistance | 5–50 | Wang Y et al. [22] | |
| MET Amplification Co-occurrence with EGFR Mutation 3 | 2–11 | Li XM et al. [23] Lai GGY et al. [24] | |
| Age | Sex | Smoking History | ECOG Performance Status | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median Age, Years | <75 Years | ≥75 Years | Female | Male | Non-Smokers | Smokers | 0 | 1 | 3 | ||
| Full Analysis Set (n = 70) | 68.7 (51.7–85.0) | 54 (77%) | 16 (23%) | 29 (41%) | 41 (59%) | 42 (60%) | 28 (40%) | 12 (17%) | 57 (81%) | 1 (1%) | |
| Type of Primary Tumor | PSC (n = 25) | 69.3 (54.1–84.8) | 19 (76%) | 6 (24%) | 8 (32%) | 17 (68%) | 13 (52%) | 12 (48%) | 3 (12%) | 22 (88%) | 0 |
| Other NSCLC (n = 45) | 68.1 (51.7–85.0) | 35 (78%) | 10 (22%) | 21 (47%) | 24 (53%) | 29 (64%) | 16 (36%) | 9 (20%) | 35 (78%) | 1 (2%) | |
| Prior Anti-tumor Treatment | Pre-treated (n = 42) | 67.7 (51.7–84.8) | 38 (90%) | 4 (10%) | 17 (40%) | 25 (60%) | 28 (67%) | 14 (33%) | 8 (19%) | 34 (81%) | 0 |
| Treatment-naïve (n = 28) | 74.5 (56.0–85.0) | 16 (57%) | 12 (43%) | 17 (40%) | 16 (57%) | 14 (50%) | 14 (50%) | 4 (14%) | 23 (82%) | 1 (4%) | |
| Brain Metastases Status | Brain metastases (n = 15) | 68.6 (51.7–84.8) | 11 (73%) | 4 (27%) | 7 (47%) | 8 (53%) | 11 (73%) | 4 (27%) | 3 (20%) | 12 (80%) | 0 |
| Non-brain metastases (n = 55) | 68.7 (51.9–85.0) | 43 (78%) | 12 (22%) | 22 (40%) | 33 (60%) | 31 (56%) | 24 (44%) | 9 (16%) | 45 (82%) | 1 (2%) | |
| Histology | Prior Anti-tumor Treatment | Brain Involvement at Baseline | |||||||||
| Pulmonary sarcomatoid carcinoma | Other NSCLC subtypes | Yes | No | ||||||||
| Adenocarcinoma | Squamous cell carcinoma | Adenosquamous carcinoma | NSCLC, not otherwise specified | ||||||||
| Full Analysis Set (n = 70) | 25 (36%) | 40 (57%) | 3 (3%) | 1 (1%) | 1 (1%) | 42 (60%) | 28 (40%) | 15 (21%) | |||
| Type of Primary Tumor | PSC (n = 25) | 25 (100%) | - | 12 (48%) | 13 (52%) | 2 (8%) | |||||
| Other NSCLC (n = 45) | - | 40 (89%) | 3 (7%) | 1 (2%) | 1 (2%) | 30 (67%) | 15 (33%) | 13 (29%) | |||
| Prior Anti-tumor Treatment | Pre-treated (n = 42) | 12 (29%) | 27 (64%) | 2 (5%) | 1 (2%) | 0 | 42 (100%) | - | 11 (26%) | ||
| Treatment-naïve (n = 28) | 13 (46%) | 13 (46%) | 1 (4%) | 0 | 1 (4%) | - | 28 (100%) | 4 (14%) | |||
| Brain Metastases Status | Brain metastases (n = 15) | 2 (13%) | 13 (87%) | 0 | 0 | 0 | 11 (73%) | 4 (27%) | 15 (100%) | ||
| Non-brain metastases (n = 55) | 23 (42%) | 27 (49%) | 3 (5%) | 1 (2%) | 1 (2%) | 33 (60%) | 22 (40%) | - | |||
| ORR, n (%) | DCR, n (%) | Median DOR, Months 1 | Median TTR, Months 1 | ||
|---|---|---|---|---|---|
| Tumor-Response-Evaluable Set (n = 62) | Total (n = 62) | 33 (53.2%) | 57 (91.9%) | 6.9 | 1.4 |
| PSC (n = 20) | 10 (50.0%) | 18 (90.0%) | 12.4 | 1.4 | |
| Other NSCLC subtypes (n = 42) | 23 (54.8%) | 39 (92.9%) | 5.6 | 1.4 | |
| Pretreated (n = 38) | 20 (52.6%) | 34 (89.5%) | 10.9 | 1.4 | |
| Treatment-naive (n = 24) | 13 (54.2%) | 23 (95.8%) | 5.6 | 1.4 | |
| Brain metastases (n = 14) | 9 (64.3%) | 14 (100.0%) | 4.9 | 1.5 | |
| Non-brain metastases (n = 48) | 24 (50.0%) | 43 (89.6%) | 7.0 | 1.4 | |
| Full Analysis Set (n = 70) | Total (n = 70) | 33 (47.1%) | 57 (81.4%) | n/A | n/A |
| PSC (n = 25) | 10 (40.0%) | 18 (72.0%) | n/A | n/A | |
| Other NSCLC subtypes (n = 45) | 23 (51.1%) | 39 (86.7%) | n/A | n/A | |
| Pretreated (n = 42) | 20 (47.6%) | 34 (81.0%) | n/A | n/A | |
| Treatment-naive (n = 28) | 13 (46.4%) | 23 (82.1%) | n/A | n/A | |
| Brain metastases (n = 15) | 9 (60.0%) | 14 (93.3%) | n/A | n/A | |
| Non-brain metastases (n = 55) | 24 (43.6%) | 43 (78.2%) | n/A | n/A |
| Any Grade | ≥Grade 3 | ||
|---|---|---|---|
| All-cause adverse events | Any event | 70 (100.0%) | 46 (65.7%) |
| Peripheral edema | 40 (57.1%) | 6 (8.6%) | |
| Nausea | 37 (52.9%) | 0 | |
| Hypoalbuminemia | 29 (41.4%) | 1 (1.4%) | |
| Elevated alanine aminotransferase | 27 (38.6%) | 7 (10.0%) | |
| Elevated aspartate aminotransferase | 27 (38.6%) | 9 (12.9%) | |
| Decreased appetite | 24 (34.3%) | 0 | |
| Vomiting | 23 (32.9%) | 0 | |
| Pyrexia | 21 (30.0%) | 1 (1.4%) | |
| Treatment-related adverse events | Any event | 70 (100.0%) | 32 (45.7%) |
| Peripheral edema | 39 (55.7) | 6 (8.6) | |
| Nausea | 32 (45.7) | 0 | |
| Hypoalbuminemia | 16 (22.9) | 0 | |
| Elevated alanine aminotransferase | 27 (38.6) | 7 (10.0%) | |
| Elevated aspartate aminotransferase | 26 (37.1) | 9 (12.9%) | |
| Decreased appetite | 14 (20.0%) | 0 | |
| Vomiting | 18 (25.7%) | 0 | |
| Pyrexia | 11 (15.7%) | 1 (1.4%) |
| Savolitinib 1 | Capmatinib 2 | Tepotinib 3 | Crizotinib 4 | Amivantamab 5 | |
|---|---|---|---|---|---|
| Approval | China approved in June 2021 | Approved in the US in 2020 | Approved in Japan in 2020 | FDA breakthrough therapy designation | Approved in the US in May 2021 |
| Mechanism | METi Ib | METi Ib | METi Ib | ALK/ROS1/METi Ia | Anti-MET and EGFR antibody |
| n | 45 | 160 | 313 | 25/69 | 46 |
| Population | 100% Chinese patients | 20.2% Asian patients | 33.9% Asian patients | Unknown/15.9% Asian patients | 50.9% Asian patients |
| Proportion of brain metastases | 28.9% | 16.9% | 18.2% | Unknown | 18.2% |
| Dose | 600 mg (BW ≥ 50 kg), or 400 mg (BW < 50 kg) OD | 400 mg BID | 500 mg OD | 250 mg BID | 1050 mg (<80 kg), or 1400 mg (≥80 kg) |
| ORR | 54.8% | 52.5% | 50.8% | 12.0%/32.3% | 32.6% |
| DCR | 92.9% | 88.1% | 75.4% | 44.0%/unknown | 76.1% |
| Median PFS, Months | 6.9 | 12.4/12.5/5.4/6.9 | 11.2 | 3.6/7.3 | 6.7 |
| Common Grade 3/4 AEs | Elevated AST Elevated ALT Peripheral edema (No interstitial lung disease occurred in registry studies) | Peripheral edema Difficulty breathing Fatigue Elevated ALT Weak Pneumonia | Peripheral edema Generalized edema Vomit Nausea Interstitial lung disease | Elevated transaminases Difficulty breathing Hypophosphatemia Lymphopenia Pulmonary embolism Interstitial lung disease | Rash Hypoalbuminemia Difficulty breathing |
| Combination | Publication [Reference] | n | Patient Population | MET Status | ORR | Median PFS, Months |
|---|---|---|---|---|---|---|
| - | Sequist LV et al. [29] Hartmaier RJ et al. [45] 1 | 93 | 1/2G EGFR–TKI resistance, T790M- | FISH: MET GCN ≥ 5 or MET/CEP7 ≥ 2; IHC: 3+ in ≥50% tumor cell; NGS: ≥ 20% tumor cell, ≥200X seq, GCN ≥ 5 | Part B2: 64.7% | Part B2: 9.1 |
| Part D: 61.9% | Part D: 9.0 | |||||
| Hartmaier RJ et al. [45] 2 | 69 | 3G EGFR–TKI (osimertinib) resistance | FISH: MET GCN ≥ 5 or MET/CEP7 ≥ 2; IHC: 3+ in ≥50% tumor cell; NGS: ≥ 20% tumor cell, ≥200X seq, GCN ≥ 5 | 33.3% | 5.5 | |
| Yu HA et al. [85] | 17 | 3G EGFR–TKI (osimertinib) resistance | NGS: GCN range from 7 to 68 | 41.2% | Unknown | |
| Ahn MJ et al. [60] | 193 | 3G EGFR–TKI (osimertinib) resistance | FISH: MET GCN ≥ 5 or MET/CEP7 ≥ 2; IHC: 3+ in ≥50% tumor cell | Overall: 32% | Overall: 5.3 | |
| FISH10+ or IHC90+: 49.1% 3 | FISH10+ or IHC90+: 7.1 | |||||
| Capmatinib + Gefitinib | Wu YL et al. [86] | 100 | 1/2G EGFR–TKI resistance, T790M- | FISH: GCN ≥ 4 | 4 ≤ GCN < 6: 22.2% | 4 ≤ GCN < 6: 5.4 |
| GCN ≥ 6: 47.2% | GCN ≥ 6: 5.5 | |||||
| IHC: 3+ in ≥50% tumor cell | IHC3+: 32.1% | IHC3+: 5.5 | ||||
| Tepotinib + Gefitinib | Wu YL et al. [87] Liam CK et al. [88] | 31 | 1/2G EGFR–TKI resistance, T790M- | FISH: GCN ≥ 5 or MET/CEP7 ≥ 2 | Overall: 45.2% | Overall: 4.9 |
| MET amp: 66.7% | MET amp: 16.6 | |||||
| IHC: 2+ or 3+ | IHC3+: 68.4% | IHC3+: 8.3 | ||||
| Amivantamab + Lazertinib | Bauml J et al. [76] | 45 | 3G EGFR–TKI (osimertinib) resistance, without previous chemotherapy | No MET selection | Overall: 35.6% | Overall: 4.9 |
| EGFR/MET dependent: 47.1% 4 | EGFR/MET dependent: 6.7 | |||||
| Unknown/non-EGFR/MET: 28.6% | Unknown/non-EGFR/MET: 4.1 | |||||
| EGFR/MET IHC+: 90.0% | EGFR/MET IHC+: 12.5 | |||||
| Telisotuzumab vedotin + Osimertinib | Goldman JW et al. [89] | 19 | 3G EGFR–TKI (osimertinib) resistance | IHC: 3+ in ≥25% tumor cell | 57.9% | Unknown |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, X.; Lu, Y.; Lu, S. Landscape of Savolitinib Development for the Treatment of Non-Small Cell Lung Cancer with MET Alteration—A Narrative Review. Cancers 2022, 14, 6122. https://doi.org/10.3390/cancers14246122
Zhu X, Lu Y, Lu S. Landscape of Savolitinib Development for the Treatment of Non-Small Cell Lung Cancer with MET Alteration—A Narrative Review. Cancers. 2022; 14(24):6122. https://doi.org/10.3390/cancers14246122
Chicago/Turabian StyleZhu, Xiaokuan, Yao Lu, and Shun Lu. 2022. "Landscape of Savolitinib Development for the Treatment of Non-Small Cell Lung Cancer with MET Alteration—A Narrative Review" Cancers 14, no. 24: 6122. https://doi.org/10.3390/cancers14246122
APA StyleZhu, X., Lu, Y., & Lu, S. (2022). Landscape of Savolitinib Development for the Treatment of Non-Small Cell Lung Cancer with MET Alteration—A Narrative Review. Cancers, 14(24), 6122. https://doi.org/10.3390/cancers14246122








