Accurate Diagnosis and Survival Prediction of Bladder Cancer Using Deep Learning on Histological Slides
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Cohorts
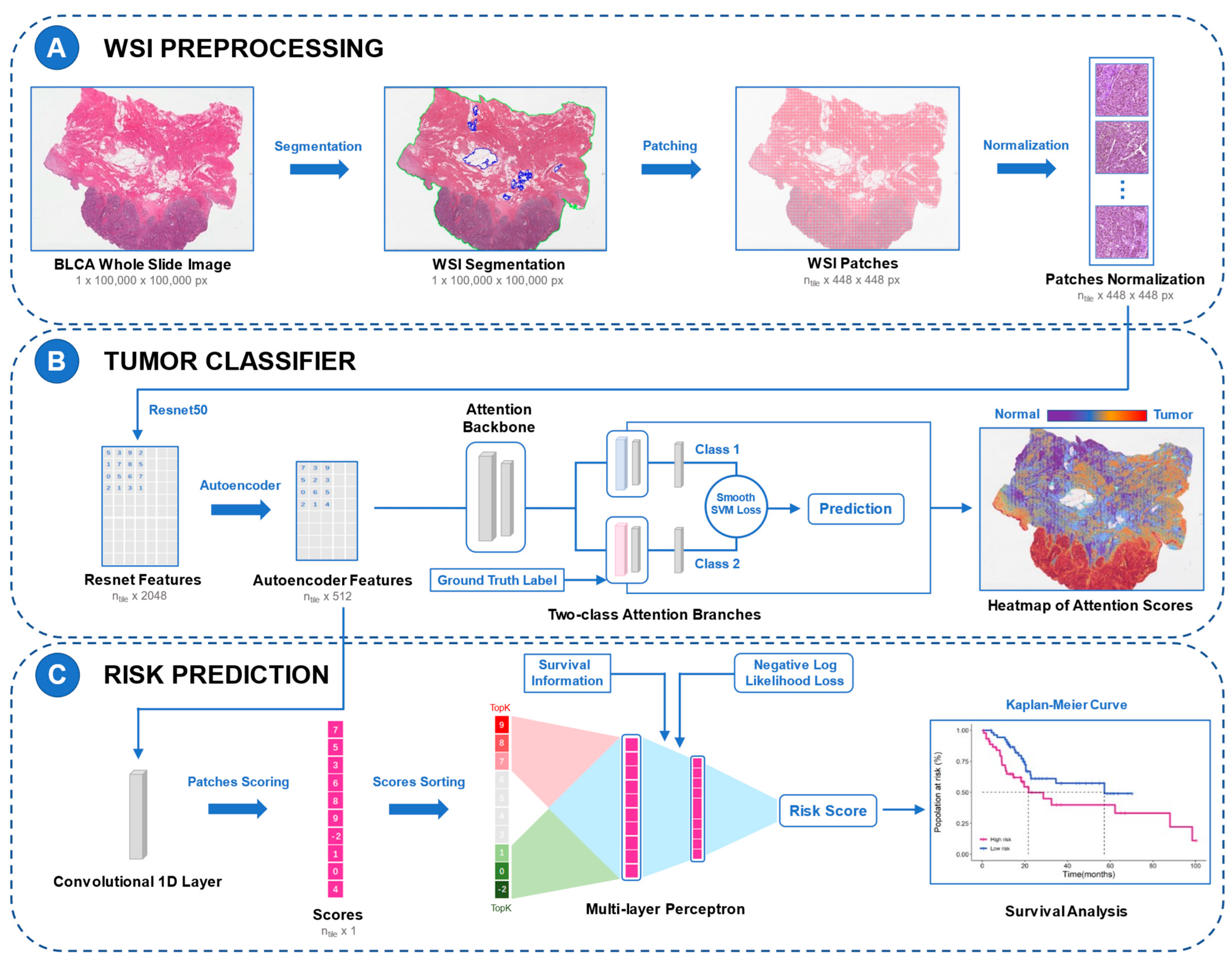
2.2. WSI Preprocessing
2.3. Feature Extraction and Reduction
2.4. Development of Diagnostic Model
2.5. Development of Prognostic Model
2.6. Model Interpretability and Visualization
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Performance of the Diagnostic Model
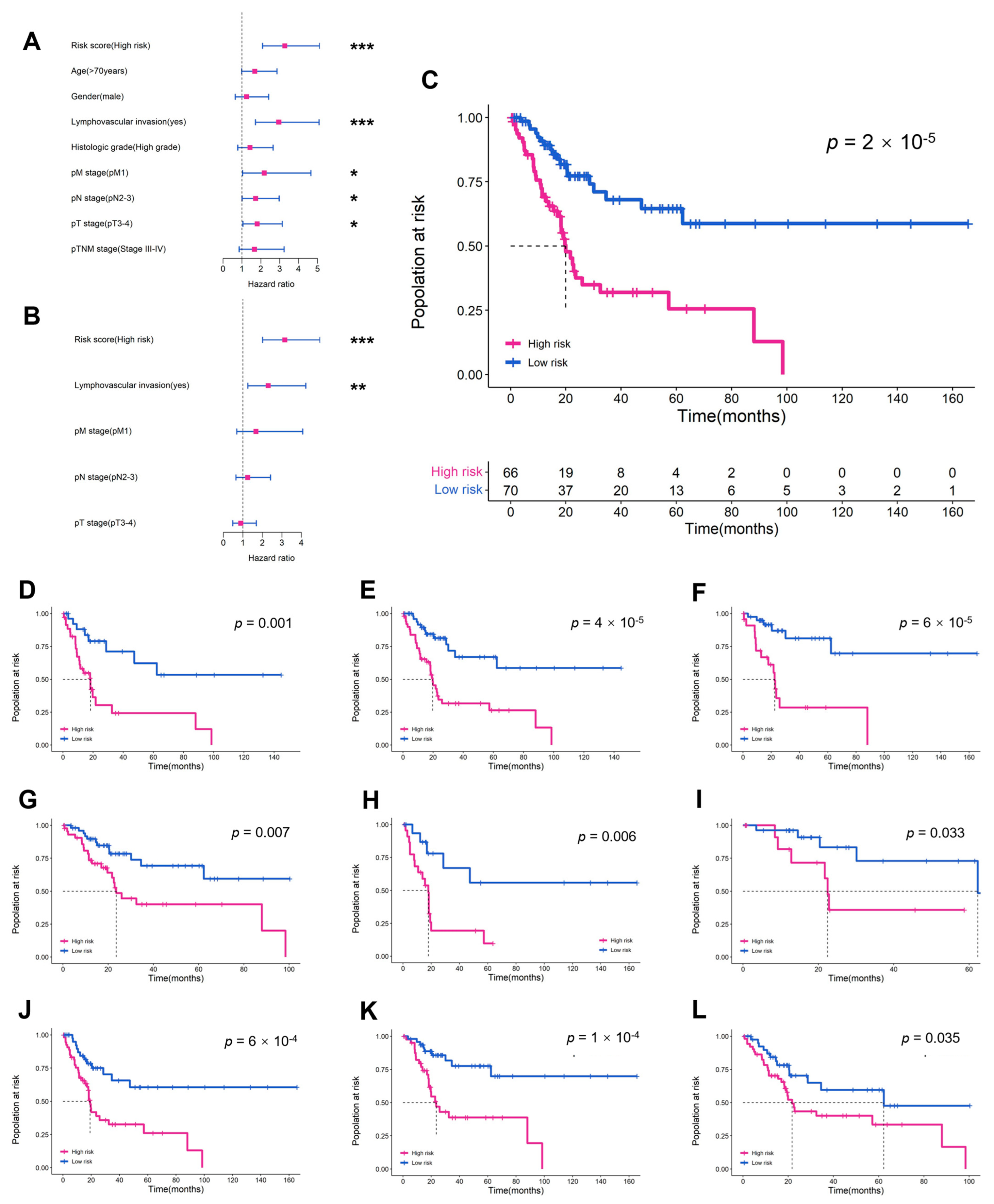
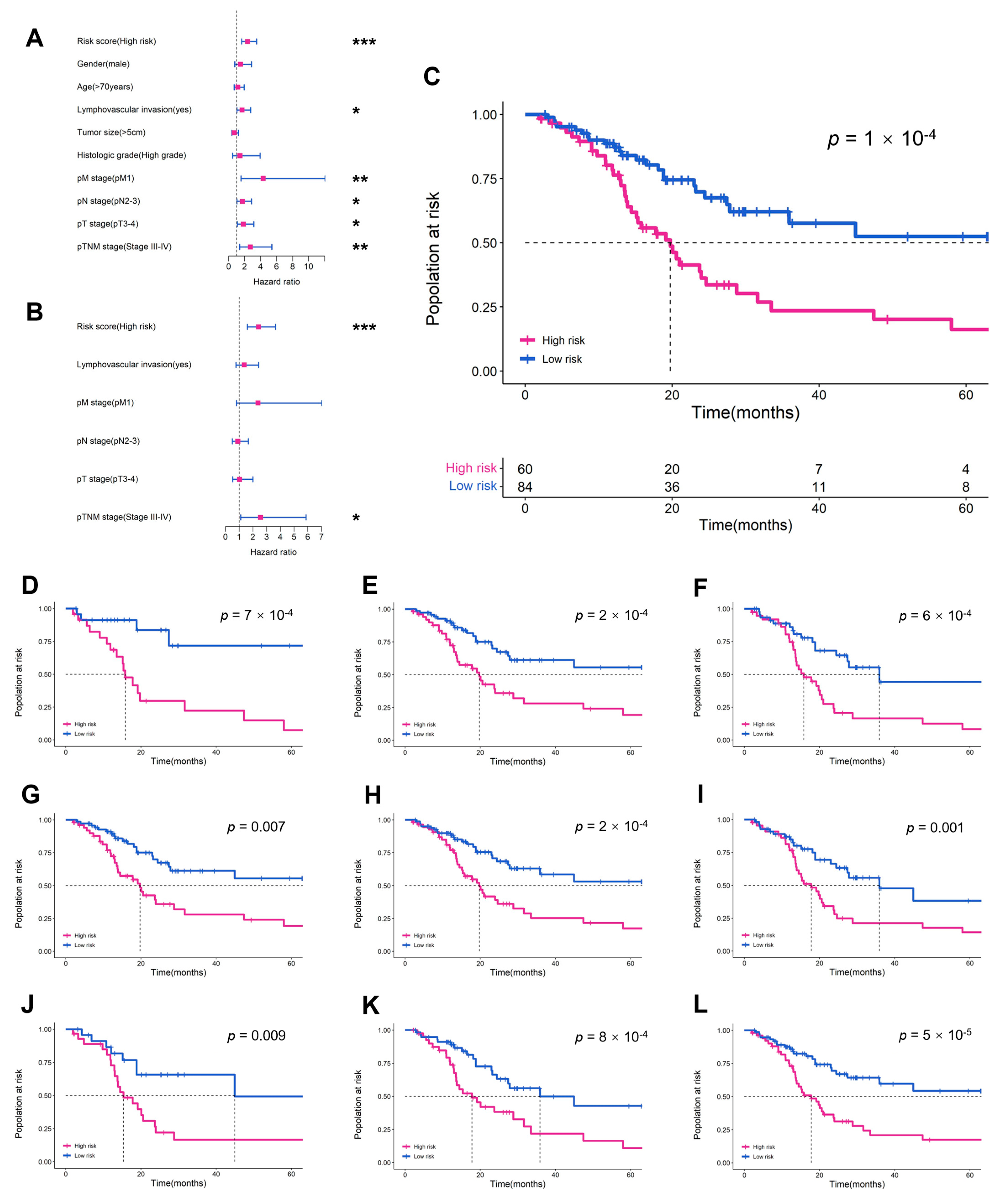
3.3. Performance of the Prognostic Model
3.4. Visualization of DL Models
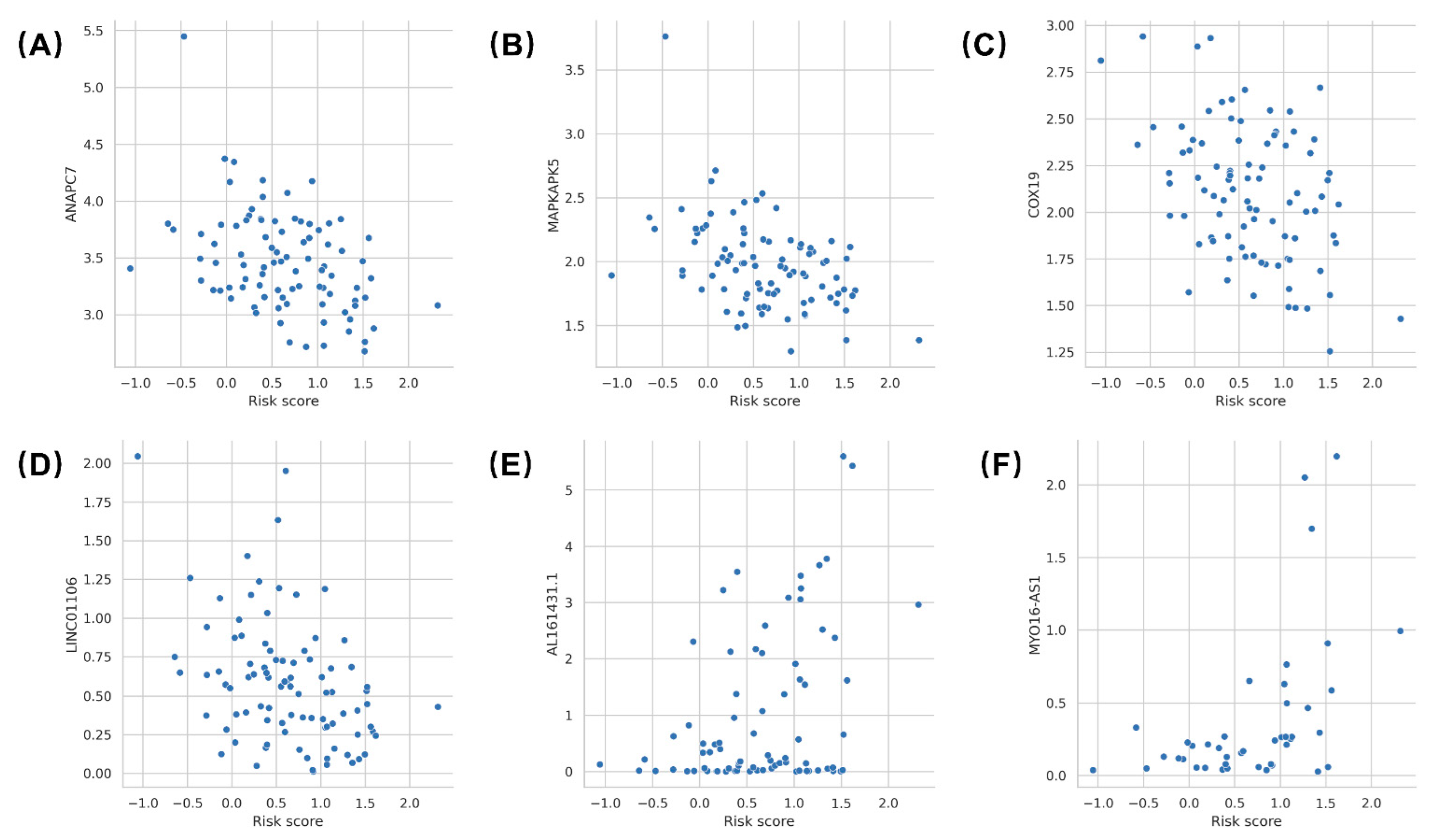
3.5. Gene Expression Correlation with Risk Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Khadhouri, S.; Gallagher, K.M.; Mackenzie, K.R.; Shah, T.T.; Gao, C.; Moore, S.; Zimmermann, E.F.; Edison, E.; Jefferies, M.; Nambiar, A.; et al. The IDENTIFY study: The investigation and detection of urological neoplasia in patients referred with suspected urinary tract cancer-a multicentre observational study. BJU Int. 2021, 128, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.G.; Oh, W.K.; Galsky, M.D. Treatment of muscle-invasive and advanced bladder cancer in 2020. CA Cancer J. Clin. 2020, 70, 404–423. [Google Scholar] [CrossRef] [PubMed]
- Khadhouri, S.; Gallagher, K.M.; Mackenzie, K.R.; Shah, T.T.; Gao, C.; Moore, S.; Zimmermann, E.F.; Edison, E.; Jefferies, M.; Nambiar, A.; et al. Developing a diagnostic multivariable prediction model for urinary tract cancer in patients referred with haematuria: Results from the IDENTIFY collaborative study. Eur. Urol. Focus 2022. [Google Scholar] [CrossRef] [PubMed]
- Zehnder, P.; Studer, U.E.; Skinner, E.C.; Thalmann, G.N.; Miranda, G.; Roth, B.; Cai, J.; Birkhäuser, F.D.; Mitra, A.P.; Burkhard, F.C.; et al. Unaltered oncological outcomes of radical cystectomy with extended lymphadenectomy over three decades. BJU Int. 2013, 112, E51–E58. [Google Scholar] [CrossRef]
- Metter, D.M.; Colgan, T.J.; Leung, S.T.; Timmons, C.F.; Park, J.Y. Trends in the US and Canadian Pathologist Workforces From 2007 to 2017. JAMA Netw. Open 2019, 2, e194337. [Google Scholar] [CrossRef]
- Witjes, J.A.; Bruins, H.M.; Cathomas, R.; Compérat, E.M.; Cowan, N.C.; Gakis, G.; Hernández, V.; Linares, E.E.; Lorch, A.; Neuzillet, Y.; et al. European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur. Urol. 2021, 79, 82–104. [Google Scholar] [CrossRef]
- Rosai, J. Rosai and Ackerman′s Surgical Pathology e-Book; Elsevier Health Sciences: USA, 2011. [Google Scholar]
- Rouprêt, M.; Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Cowan, N.C.; Dominguez-Escrig, J.L.; Gontero, P.; Hugh, M.A.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur. Urol. 2021, 79, 62–79. [Google Scholar] [CrossRef]
- Jiang, Y.; Yang, M.; Wang, S.; Li, X.; Sun, Y. Emerging role of deep learning-based artificial intelligence in tumor pathology. Cancer Commun. 2020, 40, 154–166. [Google Scholar] [CrossRef]
- Wu, S.; Chen, X.; Pan, J.; Dong, W.; Diao, X.; Zhang, R.; Zhang, Y.; Zhang, Y.; Qian, G.; Chen, H.; et al. An artificial intelligence system for the detection of bladder cancer via cystoscopy: A multicenter diagnostic study. J. Natl. Cancer Inst. 2022, 114, 220–227. [Google Scholar] [CrossRef]
- Zou, Y.; Cai, L.; Chen, C.; Shao, Q.; Fu, X.; Yu, J.; Wang, L.; Chen, Z.; Yang, X.; Yuan, B.; et al. Multi-task deep learning based on T2-Weighted Images for predicting Muscular-Invasive Bladder Cancer. Comput. Biol. Med. 2022, 151, 106219. [Google Scholar] [CrossRef]
- Freitas, N.R.; Vieira, P.M.; Cordeiro, A.; Tinoco, C.; Morais, N.; Torres, J.; Anacleto, S.; Laguna, M.P.; Lima, E.; Lima, C.S. Detection of bladder cancer with feature fusion, transfer learning and CapsNets. Artif. Intell. Med. 2022, 126, 102275. [Google Scholar] [CrossRef] [PubMed]
- Shkolyar, E.; Jia, X.; Chang, T.C.; Trivedi, D.; Mach, K.E.; Meng, M.Q.; Xing, L.; Liao, J.C. Augmented bladder tumor detection using deep learning. Eur. Urol. 2019, 76, 714–718. [Google Scholar] [CrossRef]
- Woerl, A.C.; Eckstein, M.; Geiger, J.; Wagner, D.C.; Daher, T.; Stenzel, P.; Fernandez, A.; Hartmann, A.; Wand, M.; Roth, W.; et al. Deep learning predicts molecular subtype of muscle-invasive bladder cancer from conventional histopathological slides. Eur. Urol. 2020, 78, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.Y.; Wang, X.; Ding, G.Y.; Dong, Z.; Han, J.; Guan, Z.; Ma, L.J.; Zheng, Y.; Zhang, L.; Yu, G.Z.; et al. Exploring prognostic indicators in the pathological images of hepatocellular carcinoma based on deep learning. Gut 2021, 70, 951–961. [Google Scholar] [CrossRef]
- Huang, B.; Tian, S.; Zhan, N.; Ma, J.; Huang, Z.; Zhang, C.; Zhang, H.; Ming, F.; Liao, F.; Ji, M.; et al. Accurate diagnosis and prognosis prediction of gastric cancer using deep learning on digital pathological images: A retrospective multicentre study. EBioMedicine 2021, 73, 103631. [Google Scholar] [CrossRef]
- Jiao, Y.; Li, J.; Qian, C.; Fei, S. Deep learning-based tumor microenvironment analysis in colon adenocarcinoma histopathological whole-slide images. Comput. Methods Programs Biomed. 2021, 204, 106047. [Google Scholar] [CrossRef]
- Skrede, O.J.; de Raedt, S.; Kleppe, A.; Hveem, T.S.; Liestøl, K.; Maddison, J.; Askautrud, H.A.; Pradhan, M.; Nesheim, J.A.; Albregtsen, F.; et al. Deep learning for prediction of colorectal cancer outcome: A discovery and validation study. Lancet 2020, 395, 350–360. [Google Scholar] [CrossRef]
- Courtiol, P.; Maussion, C.; Moarii, M.; Pronier, E.; Pilcer, S.; Sefta, M.; Manceron, P.; Toldo, S.; Zaslavskiy, M.; Le Stang, N.; et al. Deep learning-based classification of mesothelioma improves prediction of patient outcome. Nat. Med. 2019, 25, 1519–1525. [Google Scholar] [CrossRef]
- Saillard, C.; Schmauch, B.; Laifa, O.; Moarii, M.; Toldo, S.; Zaslavskiy, M.; Pronier, E.; Laurent, A.; Amaddeo, G.; Regnault, H.; et al. Predicting survival after hepatocellular carcinoma resection using deep learning on histological slides. Hepatology 2020, 72, 2000–2013. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.Y.; Williamson, D.; Chen, T.Y.; Chen, R.J.; Barbieri, M.; Mahmood, F. Data-efficient and weakly supervised computational pathology on whole-slide images. Nat. Biomed. Eng. 2021, 5, 555–570. [Google Scholar] [CrossRef]
- Shamai, G.; Livne, A.; Polónia, A.; Sabo, E.; Cretu, A.; Bar-Sela, G.; Kimmel, R. Deep learning-based image analysis predicts PD-L1 status from H&E-stained histopathology images in breast cancer. Nat. Commun. 2022, 13, 6753. [Google Scholar]
- Loeffler, C.; Ortiz, B.N.; Jung, M.; Seillier, L.; Rose, M.; Laleh, N.G.; Knuechel, R.; Brinker, T.J.; Trautwein, C.; Gaisa, N.T.; et al. Artificial intelligence-based detection of FGFR3 mutational status directly from routine histology in bladder cancer: A possible preselection for molecular testing? Eur. Urol. Focus 2022, 8, 472–479. [Google Scholar] [CrossRef]
- Velmahos, C.S.; Badgeley, M.; Lo, Y.C. Using deep learning to identify bladder cancers with FGFR-activating mutations from histology images. Cancer Med. 2021, 10, 4805–4813. [Google Scholar] [CrossRef]
- Paner, G.P.; Stadler, W.M.; Hansel, D.E.; Montironi, R.; Lin, D.W.; Amin, M.B. Updates in the eighth edition of the Tumor-Node-Metastasis staging classification for urologic cancers. Eur. Urol. 2018, 73, 560–569. [Google Scholar] [CrossRef]
- Vahadane, A.; Peng, T.Y.; Albarqouni, S.; Baust, M.; Steiger, K.; Schlitter, A.M.; Sethi, A.; Esposito, I.; Navab, N. Structure-preserved color normalization for histological images. In Proceedings of the IEEE 12th International Symposium on Biomedical Imaging (ISBI), Brooklyn, NY, USA, 16–19 April 2015; pp. 1012–1015. [Google Scholar]
- Anand, D.; Ramakrishnan, G.; Sethi, A. Fast GPU-Enabled color normalization for digital pathology. In Proceedings of the International Conference on Systems, Signals and Image Processing (IWSSIP), Osijek, Croatia, 5–7 June 2019; pp. 219–224. [Google Scholar]
- He, K.M.; Zhang, X.Y.; Ren, S.Q.; Sun, J. Deep Residual Learning for Image Recognition. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778. [Google Scholar]
- Mertens, L.S.; Claps, F.; Mayr, R.; Bostrom, P.J.; Shariat, S.F.; Zwarthoff, E.C.; Boormans, J.L.; Abas, C.; van Leenders, G.; Götz, S.; et al. Prognostic markers in invasive bladder cancer: FGFR3 mutation status versus P53 and KI-67 expression: A multi-center, multi-laboratory analysis in 1058 radical cystectomy patients. Urol. Oncol. 2022, 40, 110–111. [Google Scholar] [CrossRef]
- Claps, F.; Mir, M.C.; van Rhijn, B.; Mazzon, G.; Soria, F.; D′Andrea, D.; Marra, G.; Boltri, M.; Traunero, F.; Massanova, M.; et al. Impact of the controlling nutritional status (CONUT) score on perioperative morbidity and oncological outcomes in patients with bladder cancer treated with radical cystectomy. Urol. Oncol. 2022. [Google Scholar] [CrossRef]
- Mori, K.; Miura, N.; Mostafaei, H.; Quhal, F.; Motlagh, R.S.; Lysenko, I.; Kimura, S.; Egawa, S.; Karakiewicz, P.I.; Shariat, S.F. Prognostic value of preoperative hematologic biomarkers in urothelial carcinoma of the bladder treated with radical cystectomy: A systematic review and meta-analysis. Int. J. Clin. Oncol. 2020, 25, 1459–1474. [Google Scholar] [CrossRef]
- Schuettfort, V.M.; David, D.; Quhal, F.; Mostafaei, H.; Laukhtina, E.; Mori, K.; Sari, M.R.; Rink, M.; Abufaraj, M.; Karakiewicz, P.I.; et al. Impact of preoperative serum albumin-globulin ratio on disease outcome after radical cystectomy for urothelial carcinoma of the bladder. Urol. Oncol. 2021, 39, 235. [Google Scholar] [CrossRef]
- Claps, F.; Rai, S.; Mir, M.C.; van Rhijn, B.; Mazzon, G.; Davis, L.E.; Valadon, C.L.; Silvestri, T.; Rizzo, M.; Ankem, M.; et al. Prognostic value of preoperative albumin-to-fibrinogen ratio (AFR) in patients with bladder cancer treated with radical cystectomy. Urol. Oncol. 2021, 39, 835–839. [Google Scholar] [CrossRef]
- Claps, F.; van de Kamp, M.W.; Mayr, R.; Bostrom, P.J.; Boormans, J.L.; Eckstein, M.; Mertens, L.S.; Boevé, E.R.; Neuzillet, Y.; Burger, M.; et al. Risk factors associated with positive surgical margins′ location at radical cystectomy and their impact on bladder cancer survival. World J. Urol. 2021, 39, 4363–4371. [Google Scholar] [CrossRef] [PubMed]
- Mir, M.C.; Campi, R.; Loriot, Y.; Puente, J.; Giannarini, G.; Necchi, A.; Rouprêt, M. Adjuvant systemic therapy for high-risk muscle-invasive bladder cancer after radical cystectomy: Current options and future opportunities. Eur. Urol. Oncol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Afferi, L.; Lonati, C.; Montorsi, F.; Briganti, A.; Necchi, A.; Mari, A.; Minervini, A.; Tellini, R.; Campi, R.; Schulz, G.B.; et al. Selecting the best candidates for cisplatin-based adjuvant chemotherapy after radical cystectomy among patients with pN+ bladder cancer. Eur. Urol. Oncol 2022. [Google Scholar] [CrossRef] [PubMed]
- Beşler, M.S.; Koç, U. A new approach to predict the histological variants of bladder urothelial carcinoma: Machine Learning-Based radiomics analysis. Acad. Radiol. 2022. [Google Scholar] [CrossRef]
- Cuocolo, R.; Stanzione, A.; Faletti, R.; Gatti, M.; Calleris, G.; Fornari, A.; Gentile, F.; Motta, A.; Dell′Aversana, S.; Creta, M.; et al. MRI index lesion radiomics and machine learning for detection of extraprostatic extension of disease: A multicenter study. Eur. Radiol. 2021, 31, 7575–7583. [Google Scholar] [CrossRef]
- Yang, G.; Nie, P.; Yan, L.; Zhang, M.; Wang, Y.; Zhao, L.; Li, M.; Xie, F.; Xie, H.; Li, X.; et al. The radiomics-based tumor heterogeneity adds incremental value to the existing prognostic models for predicting outcome in localized clear cell renal cell carcinoma: A multicenter study. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2949–2959. [Google Scholar] [CrossRef]
- Yang, R.; Du, Y.; Weng, X.; Chen, Z.; Wang, S.; Liu, X. Automatic recognition of bladder tumours using deep learning technology and its clinical application. Int. J. Med. Robot 2021, 17, e2194. [Google Scholar] [CrossRef]
- Foersch, S.; Eckstein, M.; Wagner, D.C.; Gach, F.; Woerl, A.C.; Geiger, J.; Glasner, C.; Schelbert, S.; Schulz, S.; Porubsky, S.; et al. Deep learning for diagnosis and survival prediction in soft tissue sarcoma. Ann. Oncol. 2021, 32, 1178–1187. [Google Scholar] [CrossRef]
- Jin, L.; Shi, F.; Chun, Q.; Chen, H.; Ma, Y.; Wu, S.; Hameed, N.; Mei, C.; Lu, J.; Zhang, J.; et al. Artificial intelligence neuropathologist for glioma classification using deep learning on hematoxylin and eosin stained slide images and molecular markers. Neuro Oncol. 2021, 23, 44–52. [Google Scholar] [CrossRef]
- Wetteland, R.; Kvikstad, V.; Eftestøl, T.; Tøssebro, E.; Lillesand, M.; Janssen, E.A.; Engan, K. Automatic diagnostic tool for predicting cancer grade in bladder cancer patients using deep learning. IEEE Access 2021, 9, 115813–115825. [Google Scholar] [CrossRef]
- Fuster, S.; Khoraminia, F.; Kiraz, U.; Kanwal, N.; Kvikstad, V.; Eftestøl, T.; Zuiverloon, T.C.; Janssen, E.A.; Engan, K. Invasive cancerous area detection in Non-Muscle invasive bladder cancer whole slide images. In Proceedings of the 2022 IEEE 14th Image, Video, and Multidimensional Signal Processing Workshop (IVMSP), Nafplio, Greece, 26–29 June 2022; pp. 1–5. [Google Scholar]
- Lucas, M.; Jansen, I.; van Leeuwen, T.G.; Oddens, J.R.; de Bruin, D.M.; Marquering, H.A. Deep learning-based recurrence prediction in patients with non-muscle-invasive bladder cancer. Eur. Urol. Focus 2022, 8, 165–172. [Google Scholar] [CrossRef]
- Chen, F.; Wang, Q.; Zhou, Y. The construction and validation of an RNA binding protein-related prognostic model for bladder cancer. BMC Cancer 2021, 21, 244. [Google Scholar] [CrossRef]
- Lin, J.T.; Tsai, K.W. Circulating miRNAs act as diagnostic biomarkers for bladder cancer in urine. Int. J. Mol. Sci. 2021, 22, 4278. [Google Scholar] [CrossRef]
- Wang, Z.; Tu, L.; Chen, M.; Tong, S. Identification of a tumor microenvironment-related seven-gene signature for predicting prognosis in bladder cancer. BMC Cancer 2021, 21, 692. [Google Scholar] [CrossRef]
- Zhang, P.; Liu, Z.; Wang, D.; Li, Y.; Xing, Y.; Xiao, Y. Scoring system based on RNA modification Writer-Related genes to predict overall survival and therapeutic response in bladder cancer. Front. Immunol. 2021, 12, 724541. [Google Scholar] [CrossRef]
- Claps, F.; Mir, M.C.; Zargar, H. Molecular markers of systemic therapy response in urothelial carcinoma. Asian J. Urol. 2021, 8, 376–390. [Google Scholar] [CrossRef]
- Lindskrog, S.V.; Prip, F.; Lamy, P.; Taber, A.; Groeneveld, C.S.; Birkenkamp-Demtröder, K.; Jensen, J.B.; Strandgaard, T.; Nordentoft, I.; Christensen, E.; et al. An integrated multi-omics analysis identifies prognostic molecular subtypes of non-muscle-invasive bladder cancer. Nat. Commun. 2021, 12, 2301. [Google Scholar] [CrossRef]
- Yang, G.; Ye, Q.; Xia, J. Unbox the black-box for the medical explainable AI via multi-modal and multi-centre data fusion: A mini-review, two showcases and beyond. Inf. Fusion 2022, 77, 29–52. [Google Scholar] [CrossRef]
- Muppa, P.; Gupta, S.; Frank, I.; Boorjian, S.A.; Karnes, R.J.; Thompson, R.H.; Thapa, P.; Tarrell, R.F.; Herrera, H.L.; Jimenez, R.E.; et al. Prognostic significance of lymphatic, vascular and perineural invasion for bladder cancer patients treated by radical cystectomy. Pathology 2017, 49, 259–266. [Google Scholar] [CrossRef]
- Acs, B.; Ahmed, F.S.; Gupta, S.; Wong, P.F.; Gartrell, R.D.; Sarin, P.J.; Rizk, E.M.; Gould, R.B.; Saenger, Y.M.; Rimm, D.L. An open source automated tumor infiltrating lymphocyte algorithm for prognosis in melanoma. Nat. Commun. 2019, 10, 5440. [Google Scholar] [CrossRef]
- He, Y.; Jiang, Z.; Chen, C.; Wang, X. Classification of triple-negative breast cancers based on Immunogenomic profiling. J. Exp. Clin. Cancer Res. 2018, 37, 327. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Ma, T.; Xi, Y. Characterization of the immune cell infiltration landscape in bladder cancer to aid immunotherapy. Arch. Biochem. Biophys. 2021, 708, 108950. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Yang, J.; Liu, M.; Zhang, Y.; Zhou, Z.; Luo, W.; Fung, K.M.; Xu, C.; Bronze, M.S.; Houchen, C.W.; et al. Circular RNA ANAPC7 inhibits tumor growth and muscle wasting via PHLPP2-AKT-TGF-β signaling axis in pancreatic cancer. Gastroenterology 2022, 162, 2004–2017. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.; Kim, M.H.; Hong, H.; Cho, H.; Park, S.; Kim, S.K.; Kim, J. MK5 regulates YAP stability and is a molecular target in YAP-Driven cancers. Cancer Res. 2019, 79, 6139–6152. [Google Scholar] [CrossRef]
- Leary, S.C.; Cobine, P.A.; Nishimura, T.; Verdijk, R.M.; de Krijger, R.; de Coo, R.; Tarnopolsky, M.A.; Winge, D.R.; Shoubridge, E.A. COX19 mediates the transduction of a mitochondrial redox signal from SCO1 that regulates ATP7A-mediated cellular copper efflux. Mol. Biol. Cell 2013, 24, 683–691. [Google Scholar] [CrossRef]
- Guo, Q.; Zhang, H.; Zhang, L.; He, Y.; Weng, S.; Dong, Z.; Wang, J.; Zhang, P.; Nao, R. MicroRNA-21 regulates non-small cell lung cancer cell proliferation by affecting cell apoptosis via COX-19. Int. J. Clin. Exp. Med. 2015, 8, 8835–8841. [Google Scholar]
- Meng, L.; Xing, Z.; Guo, Z.; Liu, Z. LINC01106 post-transcriptionally regulates ELK3 and HOXD8 to promote bladder cancer progression. Cell Death Dis. 2020, 11, 1063. [Google Scholar] [CrossRef]
- Jiang, H.; Xu, A.; Li, M.; Han, R.; Wang, E.; Wu, D.; Fei, G.; Zhou, S.; Wang, R. Seven autophagy-related lncRNAs are associated with the tumor immune microenvironment in predicting survival risk of nonsmall cell lung cancer. Brief. Funct. Genomics 2021, 21, 177–187. [Google Scholar] [CrossRef]
- Shao, J.; Zhang, B.; Kuai, L.; Li, Q. Integrated analysis of hypoxia-associated lncRNA signature to predict prognosis and immune microenvironment of lung adenocarcinoma patients. Bioengineered 2021, 12, 6186–6200. [Google Scholar] [CrossRef]
- Ma, G.; Li, G.; Fan, W.; Xu, Y.; Song, S.; Guo, K.; Liu, Z. The role of long noncoding RNA AL161431.1 in the development and progression of pancreatic cancer. Front. Oncol. 2021, 11, 666313. [Google Scholar] [CrossRef]
- Gu, Z.R.; Liu, W. The LncRNA AL161431.1 targets miR-1252-5p and facilitates cellular proliferation and migration via MAPK signaling in endometrial carcinoma. Eur Rev Med Pharmacol Sci 2020, 24, 2294–2302. [Google Scholar]
- Ju, Q.; Zhao, Y.J.; Ma, S.; Li, X.M.; Zhang, H.; Zhang, S.Q.; Yang, Y.M.; Yan, S.X. Genome-wide analysis of prognostic-related lncRNAs, miRNAs and mRNAs forming a competing endogenous RNA network in lung squamous cell carcinoma. J. Cancer Res. Clin. Oncol. 2020, 146, 1711–1723. [Google Scholar] [CrossRef]
- Shen, D.; Zhang, Y.; Zheng, Q.; Yu, S.; Xia, L.; Cheng, S.; Li, G. A competing endogenous RNA network and an 8-lncRNA prognostic signature identify MYO16-AS1 as an oncogenic lncRNA in bladder cancer. DNA Cell Biol. 2021, 40, 26–35. [Google Scholar] [CrossRef]
- Cruz, R.S.; Liu, X.; Chan, A.W.; Denniston, A.K.; Calvert, M.J. Guidelines for clinical trial protocols for interventions involving artificial intelligence: The SPIRIT-AI extension. Nat. Med. 2020, 26, 1351–1363. [Google Scholar] [CrossRef]


| TCGA (N = 326) | RHWU (N = 144) | |
|---|---|---|
| Age (years) | 68 (57, 79) | 66 (26, 87) |
| Sex | ||
| female | 87 (26.69%) | 21 (14.58%) |
| male | 239 (73.31%) | 123 (85.42%) |
| pT stage | ||
| pT2 | 99 (30.37%) | 58 (40.28%) |
| pT3 | 158 (48.47%) | 67 (46.53%) |
| pT4 | 42 (12.88%) | 19 (13.19%) |
| pTx | 27 (8.28%) | 0 (0%) |
| pN stage | ||
| pN0 | 179 (54.91%) | 71 (49.31%) |
| pN1 | 38 (11.66%) | 37 (25.69%) |
| pN2 | 67 (20.55%) | 20 (13.89%) |
| pN3 | 6 (1.84%) | 16 (11.11%) |
| pNx | 36 (11.04%) | 0 (0%) |
| pM stage | ||
| pM0 | 138 (42.33%) | 140 (97.22%) |
| pM1 | 8 (2.45%) | 4 (2.78%) |
| pMx | 180 (55.22%) | 0 (0%) |
| pTNM stage | ||
| Stage II | 106 (32.52%) | 41 (28.47%) |
| Stage III | 104 (31.90%) | 81 (56.25%) |
| Stage IV | 115 (35.28%) | 22 (15.28%) |
| Missing | 1 (0.31%) | 0 (0%) |
| Lymphovascular invasion | ||
| No | 100 (30.67%) | 91 (63.19%) |
| Yes | 121 (37.12%) | 53 (36.81%) |
| Missing | 105 (32.21%) | 0 (0%) |
| Survival status | ||
| Alive | 180 (55.21%) | 79 (54.86%) |
| Dead | 146 (44.79%) | 65 (45.14%) |
| OS time (months) | 18.1 (0, 165.6) | 16.0 (1.9, 66.0) |
| a. Accuracy, Sensitivity, and Specificity in the Diagnostic Model (BlcaMIL) | |||||
| Accuracy (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | AUC (95% CI) | ||
| Training set | 0.998 (0.996, 0.999) | 0.999 (0.998, 1.000) | 0.998 (0.996, 0.999) | 1.000 (1.000, 1.000) | |
| Internal validation set | 0.998 (0.996, 1.000) | 1.000 (1.000, 1.000) | 0.996 (0.992, 1.000) | 1.000 (1.000, 1.000) | |
| External validation set | 0.987 (0.981, 0.994) | 0.984 (0.971, 0.998) | 0.986 (0.979, 0.993) | 0.993 (0.990, 0.997) | |
| b. Comparison of the BlcaMIL model and human pathologists in the external validation set | |||||
| Accuracy (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | p-Value * | Kappa # | |
| BlcaMIL Model | 0.987 (0.981, 0.994) | 0.984 (0.971, 0.998) | 0.986 (0.979, 0.993) | - | - |
| Expert Uropathologist A | 0.991 (0.987, 0.995) | 0.988 (0.981, 0.995) | 0.996 (0.989, 1.000) | 1.000 | 0.909 |
| Expert Uropathologist B | 0.993 (0.991, 0.995) | 0.991 (0.987, 0.995) | 0.996 (0.989, 1.000) | 1.000 | 0.925 |
| Junior Pathologist C | 0.876 (0.852, 0.900) | 0.834 (0.811, 0.858) | 0.940 (0.904, 0.976) | <0.0001 | 0.711 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, Q.; Yang, R.; Ni, X.; Yang, S.; Xiong, L.; Yan, D.; Xia, L.; Yuan, J.; Wang, J.; Jiao, P.; et al. Accurate Diagnosis and Survival Prediction of Bladder Cancer Using Deep Learning on Histological Slides. Cancers 2022, 14, 5807. https://doi.org/10.3390/cancers14235807
Zheng Q, Yang R, Ni X, Yang S, Xiong L, Yan D, Xia L, Yuan J, Wang J, Jiao P, et al. Accurate Diagnosis and Survival Prediction of Bladder Cancer Using Deep Learning on Histological Slides. Cancers. 2022; 14(23):5807. https://doi.org/10.3390/cancers14235807
Chicago/Turabian StyleZheng, Qingyuan, Rui Yang, Xinmiao Ni, Song Yang, Lin Xiong, Dandan Yan, Lingli Xia, Jingping Yuan, Jingsong Wang, Panpan Jiao, and et al. 2022. "Accurate Diagnosis and Survival Prediction of Bladder Cancer Using Deep Learning on Histological Slides" Cancers 14, no. 23: 5807. https://doi.org/10.3390/cancers14235807
APA StyleZheng, Q., Yang, R., Ni, X., Yang, S., Xiong, L., Yan, D., Xia, L., Yuan, J., Wang, J., Jiao, P., Wu, J., Hao, Y., Wang, J., Guo, L., Jiang, Z., Wang, L., Chen, Z., & Liu, X. (2022). Accurate Diagnosis and Survival Prediction of Bladder Cancer Using Deep Learning on Histological Slides. Cancers, 14(23), 5807. https://doi.org/10.3390/cancers14235807





