Regression of Lung Cancer in Mice by Intranasal Administration of SARS-CoV-2 Spike S1
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents
- Wild type (wt) AIDS: TNGVGY
- Mutated (m) AIDS: TGGVGD)
2.2. Cell Culture
- H1299 (human NSCLC, p53 negative; Catalog# CRL-5803)
- H358 (human NSCLC, KRAS mutant; Catalog# CRL-5807)
2.3. Assessment of Viability in Cell Lines
2.3.1. MTT Assay
2.3.2. Lactate Dehydrogenase Measurement
2.4. Fragment end Labeling DNA
2.5. Immunostaining
2.6. Annexin V and PI Flow Cytometry
2.7. Immunoblotting
- Caspase-3 (Vendor: Santa-Cruz, Dallas, TX; Dilution: 1:200)
- Cleaved caspase-3 (Vendor: Cell Signaling, Danvers, MA; Dilution: 1:1000)
- p53 (Vendor: Santa-Cruz, Dallas, TX; Dilution: 1:200)
- Bcl2 (Vendor: Santa-Cruz, Dallas, TX; Dilution: 1:200)
- Bad (Vendor: Santa-Cruz, Dallas, TX; Dilution: 1:200)
- β-actin (Vendor: Abcam, Dallas, TX; Dilution: 1:10,000)
2.8. Animals and Experimental Design: Intoxication of A/J Mice with NNK
2.8.1. Treatment of NNK-Intoxicated Mice with Recombinant SARS-CoV-2 Spike S1 Protein
2.8.2. Tumor Histology
2.9. Statistical Analysis
3. Results
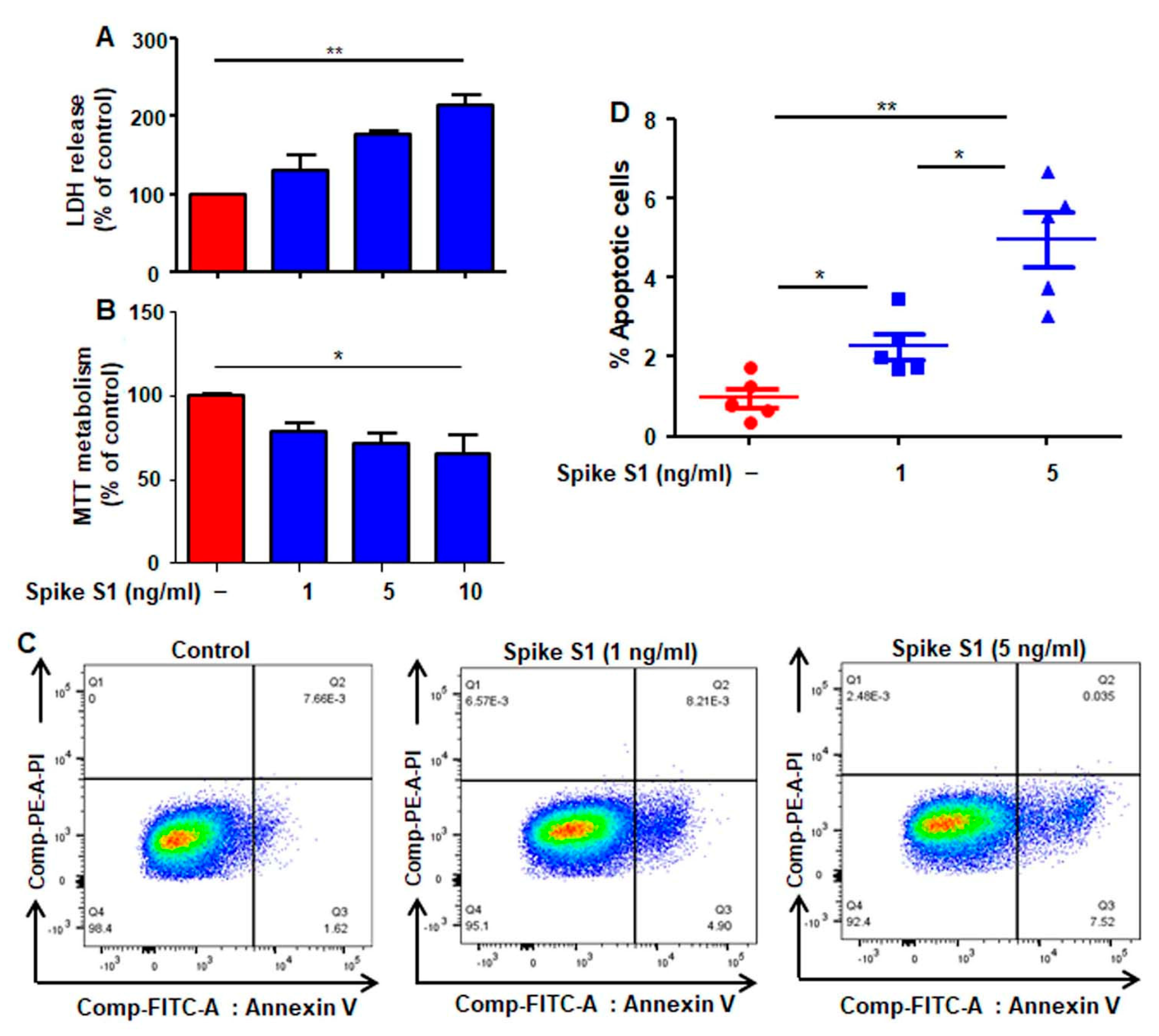
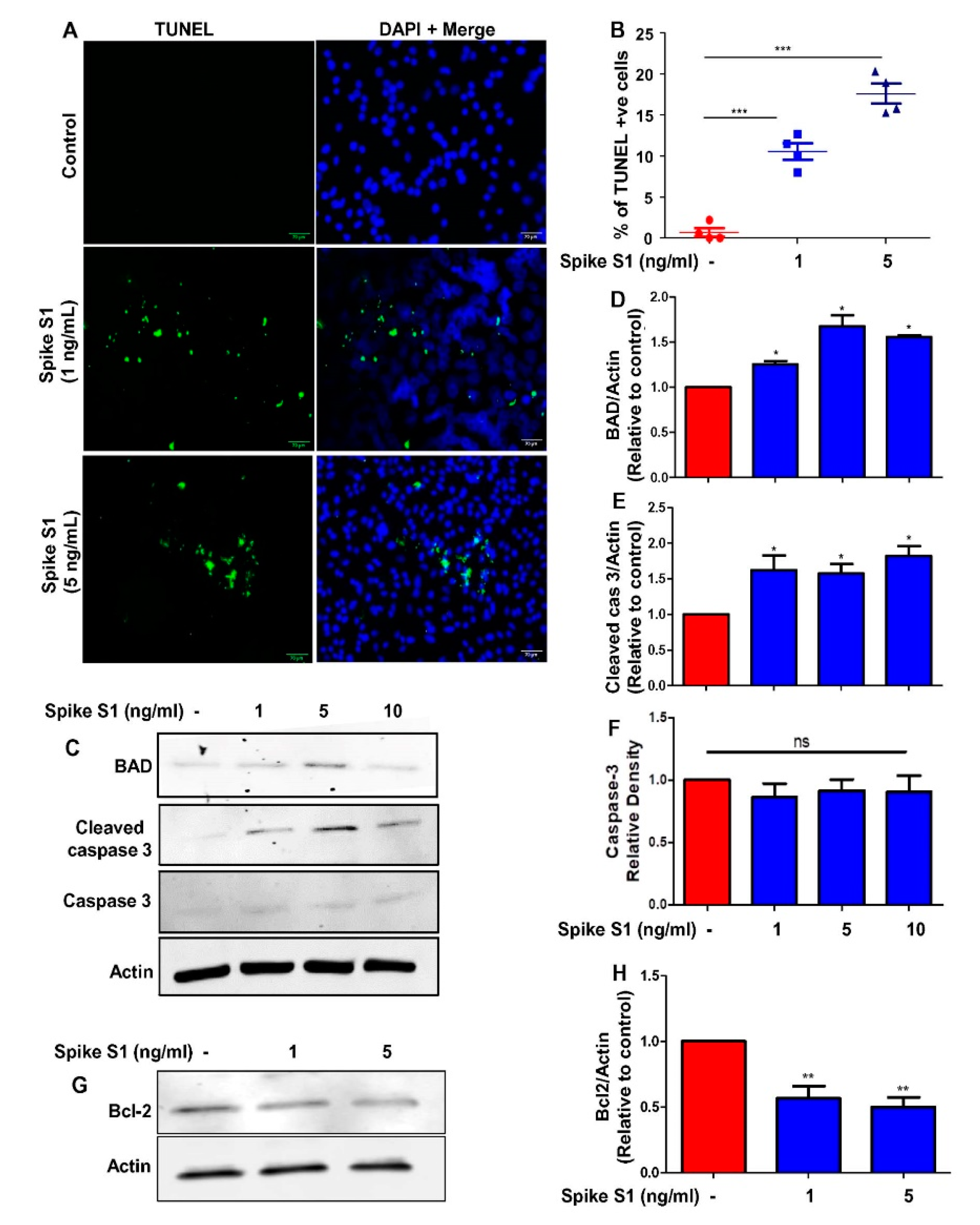
3.1. Recombinant SARS-CoV-2 Spike S1 Treatment Induces Apoptosis and Death in Human A549 Lung Cancer Cells
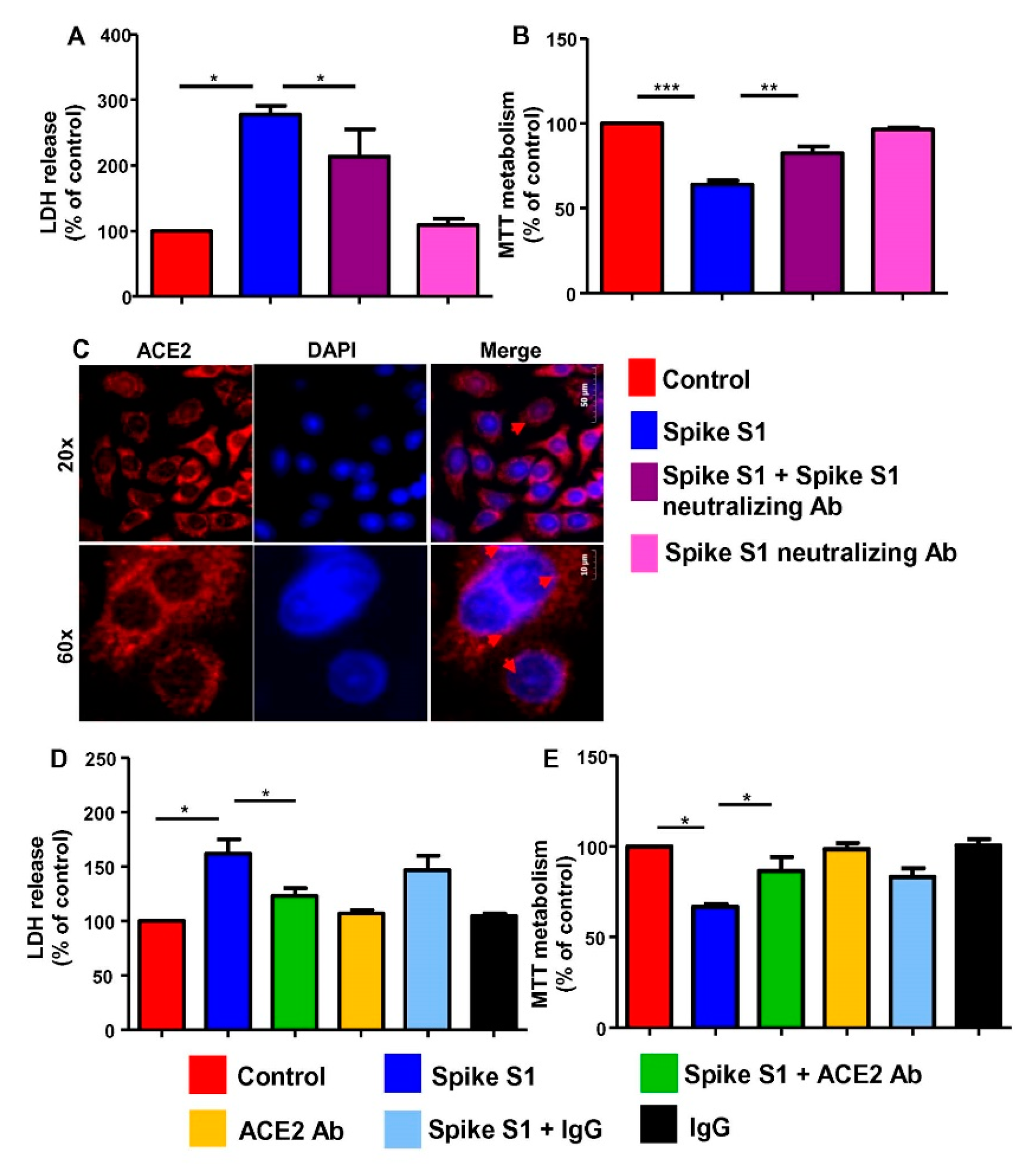
3.2. Recombinant SARS-CoV-2 Spike S1 Induces Death of Human A549 Lung Cancer Cells via Its Interaction with ACE2 Receptor
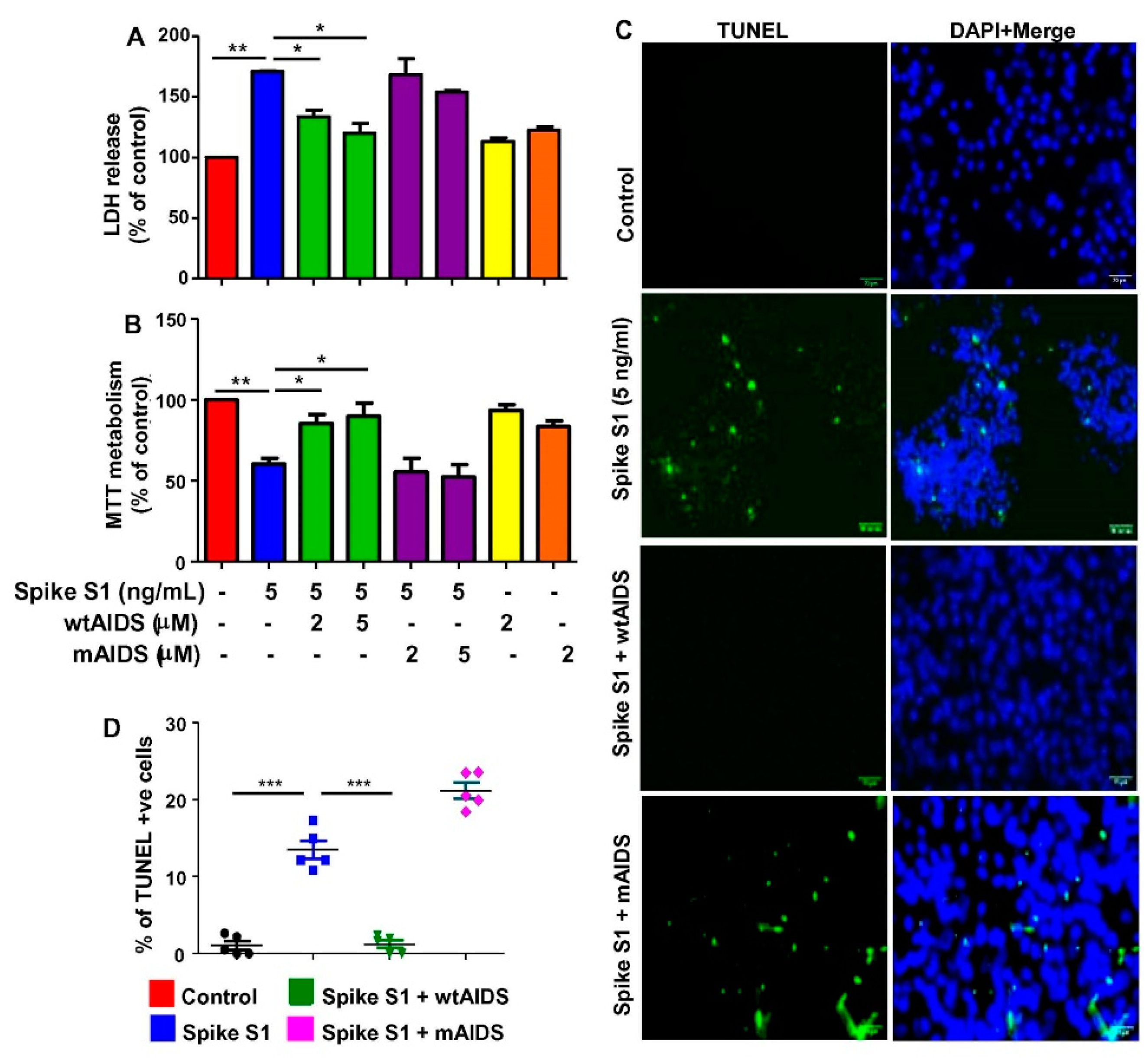
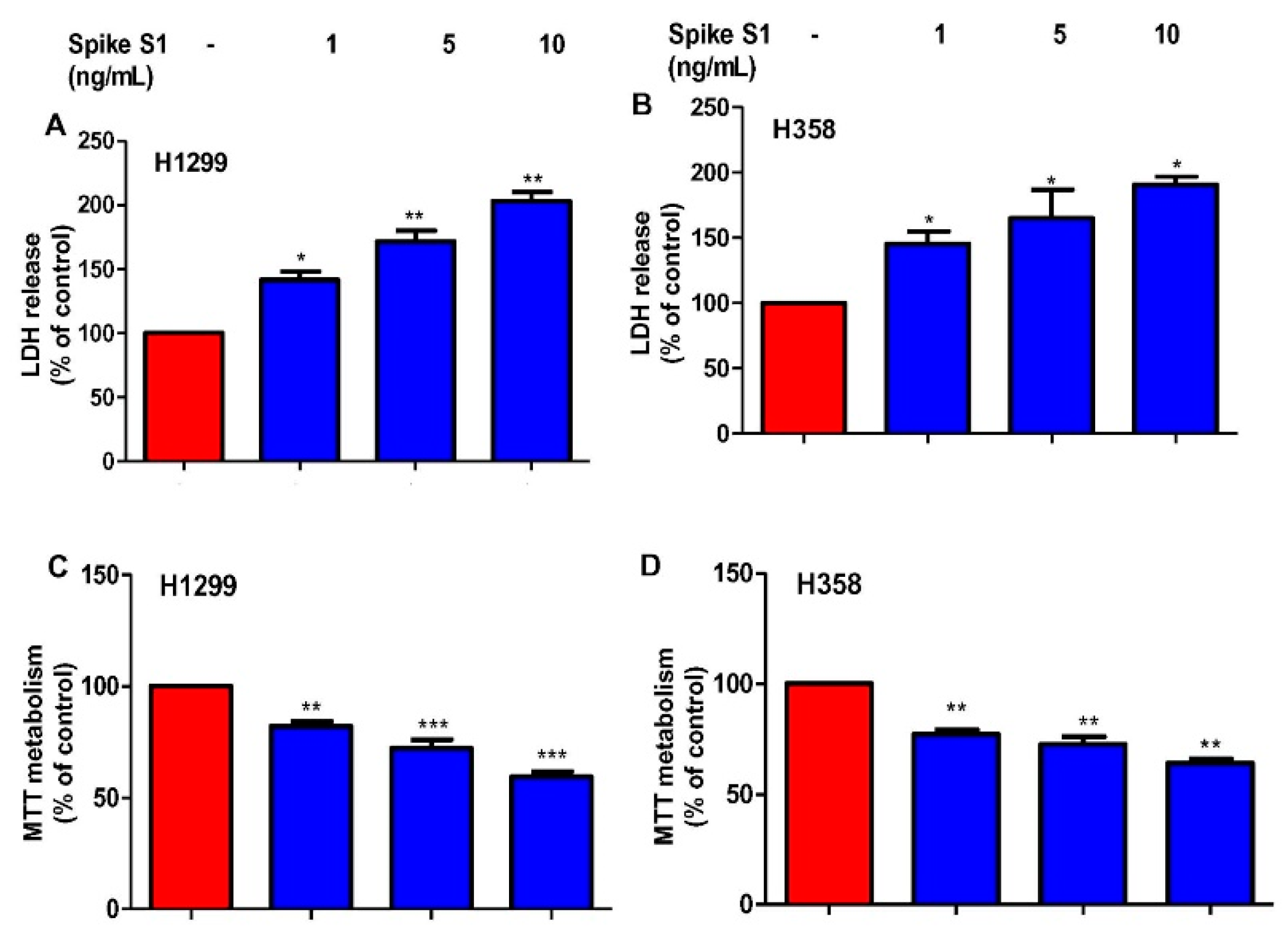
3.3. Recombinant SARS-CoV-2 Spike S1 Treatment Leads to Death of Human H1299 and H358 Lung Cancer Cells
3.4. Treatment with Recombinant SARS-CoV-2 Spike S1 Protein Causes Tumor Regression in NNK-Induced A/J Mice
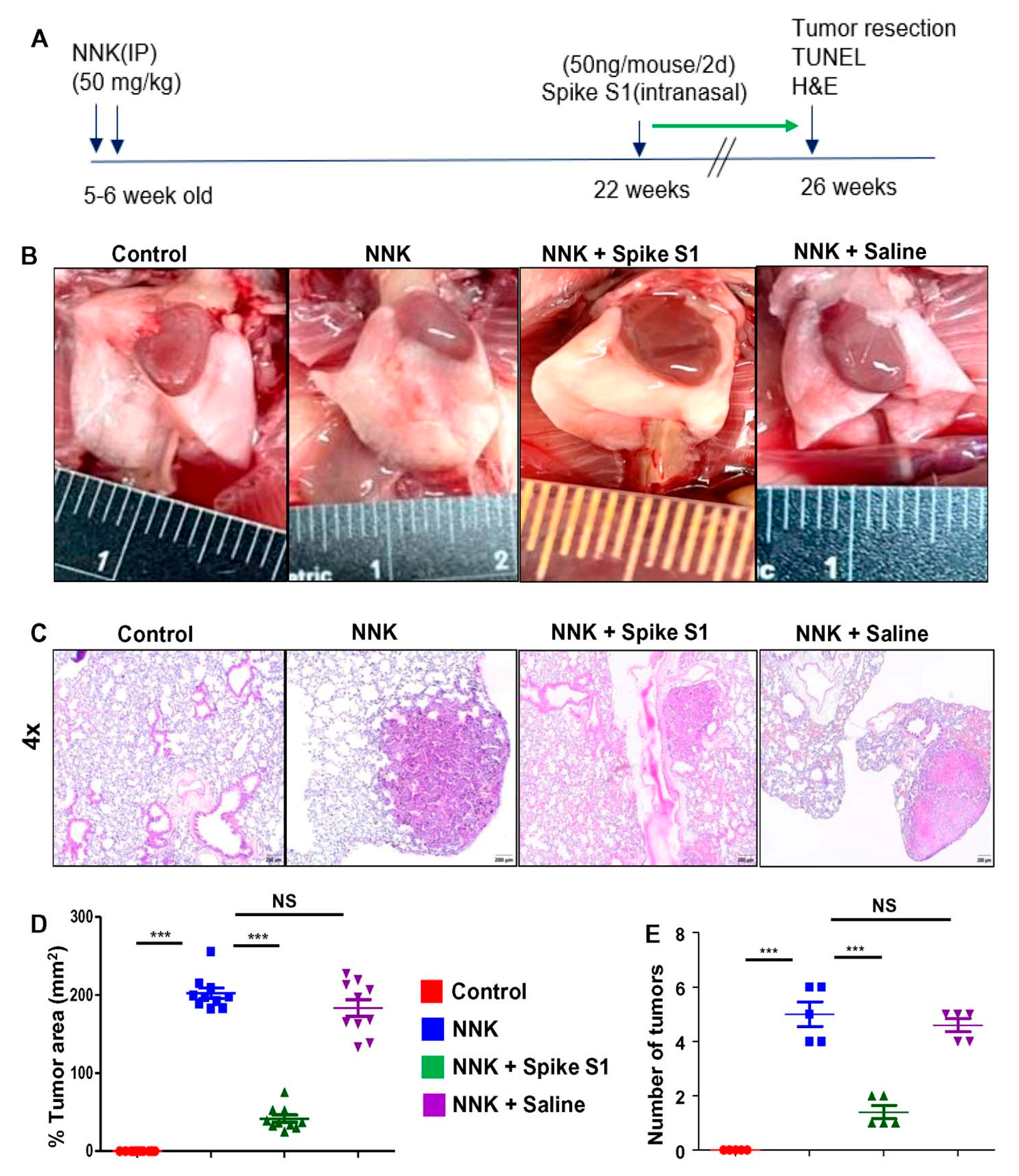
3.5. Intranasal Administration of Recombinant SARS-CoV-2 Spike S1 Protein Induces Apoptosis in Lung Tumor of NNK-Intoxicated A/J Mice
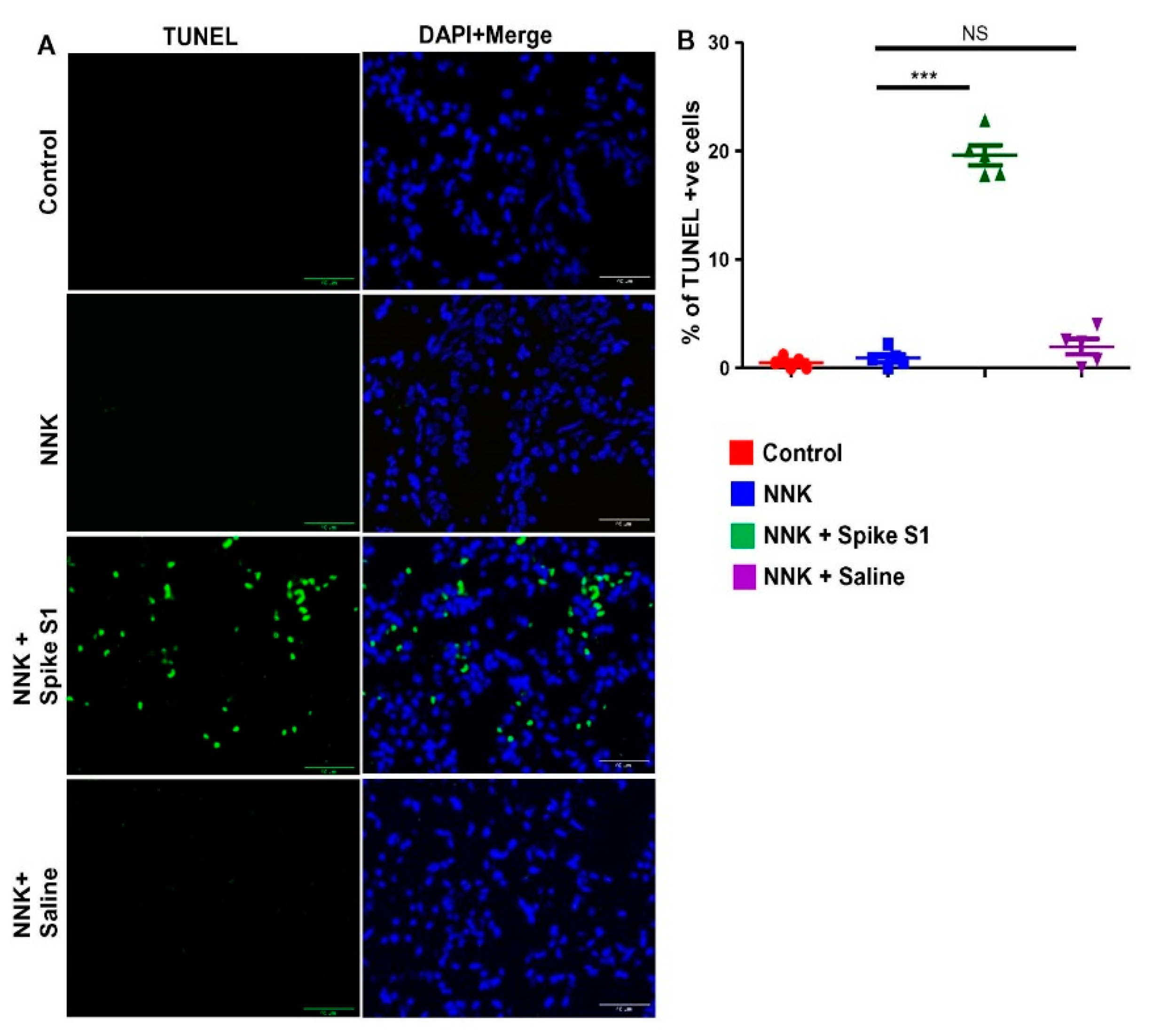
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control. Chronic disease reports: Deaths from lung cancer--United States, 1986. JAMA 1989, 262, 1170–1172. [Google Scholar]
- Dela Cruz, C.S.; Tanoue, L.T.; Matthay, R.A. Lung Cancer: Epidemiology, Etiology, and Prevention. Clin. Chest Med. 2011, 32, 605–644. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA A Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Rachow, T.; Schiffl, H.; Lang, S.M. Risk of lung cancer and renin–angiotensin blockade: A concise review. J. Cancer Res. Clin. Oncol. 2020, 147, 195–204. [Google Scholar] [CrossRef]
- Alexander, M.; Kim, S.Y.; Cheng, H. Update 2020: Management of Non-Small Cell Lung Cancer. Lung 2020, 198, 897–907. [Google Scholar] [CrossRef]
- Osmani, L.; Askin, F.; Gabrielson, E.; Li, Q.K. Current WHO guidelines and the critical role of immunohistochemical markers in the subclassification of non-small cell lung carcinoma (NSCLC): Moving from targeted therapy to immunotherapy. Semin. Cancer Biol. 2018, 52, 103–109. [Google Scholar] [CrossRef]
- Cheng, Q.; Zhou, L.; Zhou, J.; Wan, H.; Li, Q.; Feng, Y. ACE2 overexpression inhibits acquired platinum resistance-induced tumor angiogenesis in NSCLC. Oncol. Rep. 2016, 36, 1403–1410. [Google Scholar] [CrossRef]
- Wan, H.; Feng, Y.; Ni, L.; Fan, L.; Fei, X.; Ma, Q.; Gao, B.; Xiang, Y.; Che, J.; Li, Q. Overexpression of ACE2 produces antitumor effects via inhibition of angiogenesis and tumor cell invasion in vivo and in vitro. Oncol. Rep. 2011, 26, 1157–1164. [Google Scholar] [CrossRef]
- Hicks, B.M.; Filion, K.B.; Yin, H.; Sakr, L.; A Udell, J.; Azoulay, L. Angiotensin converting enzyme inhibitors and risk of lung cancer: Population based cohort study. BMJ 2018, 363, k4209. [Google Scholar] [CrossRef]
- Machhi, J.; Herskovitz, J.; Senan, A.M.; Dutta, D.; Nath, B.; Oleynikov, M.D.; Blomberg, W.R.; Meigs, D.D.; Hasan, M.; Patel, M.; et al. The Natural History, Pathobiology, and Clinical Manifestations of SARS-CoV-2 Infections. J. Neuroimmune Pharmacol. 2020, 15, 359–386. [Google Scholar] [CrossRef]
- Pahan, P.; Pahan, K. Smooth or Risky Revisit of an Old Malaria Drug for COVID-19? J. Neuroimmune Pharmacol. 2020, 15, 174–180. [Google Scholar] [CrossRef]
- Paidi, R.K.; Jana, M.; Mishra, R.K.; Dutta, D.; Pahan, K. Selective Inhibition of the Interaction between SARS-CoV-2 Spike S1 and ACE2 by SPIDAR Peptide Induces Anti-Inflammatory Therapeutic Responses. J. Immunol. 2021, 207, 2521–2533. [Google Scholar] [CrossRef]
- Paidi, R.K.; Jana, M.; Mishra, R.K.; Dutta, D.; Raha, S.; Pahan, K. ACE-2-interacting Domain of SARS-CoV-2 (AIDS) Peptide Suppresses Inflammation to Reduce Fever and Protect Lungs and Heart in Mice: Implications for COVID-19 Therapy. J. Neuroimmune Pharmacol. 2021, 16, 59–70. [Google Scholar] [CrossRef]
- Mukherjee, S.; Pahan, K. Is COVID-19 Gender-sensitive? J. Neuroimmune Pharmacol. 2021, 16, 38–47. [Google Scholar] [CrossRef]
- Ito, T.; Saeki, H.; Guo, X.; Sysa-Shah, P.; Coulter, J.; Tamashiro, K.L.K.; Lee, R.; Orita, H.; Sato, K.; Ishiyama, S.; et al. Prenatal stress enhances NNK-induced lung tumors in A/J mice. Carcinogenesis 2020, 41, 1713–1723. [Google Scholar] [CrossRef]
- Kundu, M.; Roy, A.; Pahan, K. Selective neutralization of IL-12 p40 monomer induces death in prostate cancer cells via IL-12–IFN-γ. Proc. Natl. Acad. Sci. USA 2017, 114, 11482–11487. [Google Scholar] [CrossRef]
- Kundu, M.; Raha, S.; Roy, A.; Pahan, K. Regression of Triple-Negative Breast Cancer in a Patient-Derived Xenograft Mouse Model by Monoclonal Antibodies against IL-12 p40 Monomer. Cells 2022, 11, 259. [Google Scholar] [CrossRef]
- Jana, M.; Jana, A.; Pal, U.; Pahan, K. A Simplified Method for Isolating Highly Purified Neurons, Oligodendrocytes, Astrocytes, and Microglia from the Same Human Fetal Brain Tissue. Neurochem. Res. 2007, 32, 2015–2022. [Google Scholar] [CrossRef]
- Dutta, D.; Jana, M.; Majumder, M.; Mondal, S.; Roy, A.; Pahan, K. Selective targeting of the TLR2/MyD88/NF-κB pathway reduces α-synuclein spreading in vitro and in vivo. Nat. Commun. 2021, 12, 1–19. [Google Scholar] [CrossRef]
- Patel, D.; Roy, A.; Raha, S.; Kundu, M.; Gonzalez, F.J.; Pahan, K. Upregulation of BDNF and hippocampal functions by a hippocampal ligand of PPARα. JCI Insight 2020, 5, 136654. [Google Scholar] [CrossRef]
- Chandra, S.; Jana, M.; Pahan, K. Aspirin Induces Lysosomal Biogenesis and Attenuates Amyloid Plaque Pathology in a Mouse Model of Alzheimer’s Disease via PPARα. J. Neurosci. 2018, 38, 6682–6699. [Google Scholar] [CrossRef]
- Mondal, S.; Kundu, M.; Jana, M.; Roy, A.; Rangasamy, S.B.; Modi, K.K.; Wallace, J.; Albalawi, Y.A.; Balabanov, R.; Pahan, K. IL-12 p40 monomer is different from other IL-12 family members to selectively inhibit IL-12Rβ1 internalization and suppress EAE. Proc. Natl. Acad. Sci. USA 2020, 117, 21557–21567. [Google Scholar]
- Chakrabarti, S.; Prorok, T.; Roy, A.; Patel, D.; Dasarathi, S.; Pahan, K. Upregulation of IL-1 Receptor Antagonist by Aspirin in Glial Cells via Peroxisome Proliferator-Activated Receptor-Alpha. J. Alzheimers Dis. Rep. 2021, 5, 647–661. [Google Scholar] [CrossRef]
- Rangasamy, S.B.; Dasarathi, S.; Pahan, P.; Jana, M.; Pahan, K. Low-Dose Aspirin Upregulates Tyrosine Hydroxylase and Increases Dopamine Production in Dopaminergic Neurons: Implications for Parkinson’s Disease. J. Neuroimmune Pharmacol. 2018, 14, 173–187. [Google Scholar] [CrossRef]
- Yao, Y.; Wu, J.; Zhou, H.; Firrman, J.; Xiao, W.; Sun, Z.; Li, D. A deficiency in cathelicidin reduces lung tumor growth in NNK/NTHi-induced A/J mice. Am. J. Cancer Res. 2018, 8, 1190–1199. [Google Scholar]
- Brahmachari, S.; Pahan, K. Sodium Benzoate, a Food Additive and a Metabolite of Cinnamon, Modifies T Cells at Multiple Steps and Inhibits Adoptive Transfer of Experimental Allergic Encephalomyelitis. J. Immunol. 2007, 179, 275–283. [Google Scholar] [CrossRef]
- Dasgupta, S.; Zhou, Y.; Jana, M.; Banik, N.L.; Pahan, K. Sodium Phenylacetate Inhibits Adoptive Transfer of Experimental Allergic Encephalomyelitis in SJL/J Mice at Multiple Steps. J. Immunol. 2003, 170, 3874–3882. [Google Scholar] [CrossRef]
- Modi, K.K.; Roy, A.; Brahmachari, S.; Rangasamy, S.B.; Pahan, K. Cinnamon and Its Metabolite Sodium Benzoate Attenuate the Activation of p21rac and Protect Memory and Learning in an Animal Model of Alzheimer’s Disease. PLoS ONE 2015, 10, e0130398. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. The Hallmarks of Cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef]
- Pore, M.M.; Hiltermann, T.J.N.; Kruyt, F.A. Targeting apoptosis pathways in lung cancer. Cancer Lett. 2013, 332, 359–368. [Google Scholar] [CrossRef]
- Tan, Y.; Demeter, M.R.; Ruan, H.; Comb, M.J. BAD Ser-155 Phosphorylation Regulates BAD/Bcl-XL Interaction and Cell Survival. J. Biol. Chem. 2000, 275, 25865–25869. [Google Scholar] [CrossRef]
- Zaman, M.A.; Oparil, S.; Calhoun, D.A. Drugs targeting the renin–angiotensin–aldosterone system. Nat. Rev. Drug Discov. 2002, 1, 621–636. [Google Scholar] [CrossRef]
- Du, L.; He, Y.; Zhou, Y.; Liu, S.; Zheng, B.-J.; Jiang, S. The spike protein of SARS-CoV—A target for vaccine and therapeutic development. Nat. Rev. Microbiol. 2009, 7, 226–236. [Google Scholar] [CrossRef]
- Takeda, M. Proteolytic activation of SARS-CoV-2 spike protein. Microbiol. Immunol. 2021, 66, 15–23. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Taniyama, Y.; Oze, I.; Koyanagi, Y.N.; Kawakatsu, Y.; Ito, Y.; Matsuda, T.; Matsuo, K.; Mitsudomi, T.; Ito, H. Changes in survival of patients with non-small cell lung cancer in Japan: An interrupted time series study. Cancer Sci. 2022. [Google Scholar] [CrossRef]
- Yang, Z.; Hackshaw, A.; Feng, Q.; Fu, X.; Zhang, Y.; Mao, C.; Tang, J. Comparison of gefitinib, erlotinib and afatinib in non-small cell lung cancer: A meta-analysis. Int. J. Cancer 2017, 140, 2805–2819. [Google Scholar] [CrossRef]
- Thomas, A.; Liu, S.V.; Subramaniam, D.S.; Giaccone, G. Refining the treatment of NSCLC according to histological and molecular subtypes. Nat. Rev. Clin. Oncol. 2015, 12, 511–526. [Google Scholar] [CrossRef]
- Solomon, B.J.; Mok, T.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Mekhail, T.; Felip, E.; Cappuzzo, F.; Paolini, J.; Usari, T.; et al. First-Line Crizotinib versus Chemotherapy in ALK-Positive Lung Cancer. N. Engl. J. Med. 2014, 371, 2167–2177. [Google Scholar] [CrossRef]
- Zhou, C.; Wu, Y.-L.; Chen, G.; Feng, J.; Liu, X.-Q.; Wang, C.; Zhang, S.; Wang, J.; Zhou, S.; Ren, S.; et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): A multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011, 12, 735–742. [Google Scholar] [CrossRef]
- Rosell, R.; Carcereny, E.; Gervais, R.; Vergnenegre, A.; Massuti, B.; Felip, E.; Palmero, R.; Garcia-Gomez, R.; Pallares, C.; Sanchez, J.M.; et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012, 13, 239–246. [Google Scholar] [CrossRef]
- Mithoowani, H.; Febbraro, M. Non-Small-Cell Lung Cancer in 2022: A Review for General Practitioners in Oncology. Curr. Oncol. 2022, 29, 1828–1839. [Google Scholar] [CrossRef]
- Steven, A.; Fisher, S.A.; Robinson, B.W.; Fong, K.M.; Van Zandwijk, N. Immunotherapy for lung cancer. Respirology 2016, 21, 821–833. [Google Scholar] [CrossRef]
- Zhang, R.; Meng, Z.; Wu, X.; Zhang, M.; Piao, Z.; Jin, T. PD-L1/p-STAT3 promotes the progression of NSCLC cells by regulating TAM polarization. J. Cell. Mol. Med. 2022. [Google Scholar] [CrossRef]
- Qiao, T.; Zhao, J.; Xin, X.; Xiong, Y.; Guo, W.; Meng, F.; Li, H.; Feng, Y.; Xu, H.; Shi, C.; et al. Combined pembrolizumab and bevacizumab therapy effectively inhibits non-small-cell lung cancer growth and prevents postoperative recurrence and metastasis in humanized mouse model. Cancer Immunol. Immunother. 2022. [Google Scholar] [CrossRef]
- Zheng, H.-C.; Takano, Y. NNK-Induced Lung Tumors: A Review of Animal Model. J. Oncol. 2011, 2011, 635379. [Google Scholar] [CrossRef]
- Patlolla, J.M.; Kopelovich, L.; Qian, L.; Zhang, Y.; Kumar, G.; Madka, V.; Mohammed, A.; Biddick, L.; Sadeghi, M.; Lightfoot, S.; et al. Early and delayed intervention with Rapamycin prevents NNK-induced lung adenocarcinoma in A/J mice. Oncol. Rep. 2015, 34, 2925–2934. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J.; on behalf of theHLH Across Speciality Collaboration, UK. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Jana, M.; Jana, A.; Liu, X.; Ghosh, S.; Pahan, K. Involvement of Phosphatidylinositol 3-Kinase-Mediated Up-Regulation of IκBα in Anti-Inflammatory Effect of Gemfibrozil in Microglia. J. Immunol. 2007, 179, 4142–4152. [Google Scholar] [CrossRef]
- Pahan, K.; Sheikh, F.G.; Namboodiri, A.M.; Singh, I. Inhibitors of Protein Phosphatase 1 and 2A Differentially Regulate the Expression of Inducible Nitric-oxide Synthase in Rat Astrocytes and Macrophages. J. Biol. Chem. 1998, 273, 12219–12226. [Google Scholar] [CrossRef]
- Paidi, R.K.; Jana, M.; Raha, S.; McKay, M.; Sheinin, M.; Mishra, R.K.; Pahan, K. Eugenol, a Component of Holy Basil (Tulsi) and Common Spice Clove, Inhibits the Interaction Between SARS-CoV-2 Spike S1 and ACE2 to Induce Therapeutic Responses. J. Neuroimmune Pharmacol. 2021, 16, 743–755. [Google Scholar] [CrossRef]
- Verbik, D.; Joshi, S. Immune Cells and Cytokines-Their Role in Cancer-Immunotherapy (Review). Int. J. Oncol. 1995, 7, 205–223. [Google Scholar] [CrossRef]
- Showalter, A.; Limaye, A.; Oyer, J.L.; Igarashi, R.; Kittipatarin, C.; Copik, A.J.; Khaled, A.R. Cytokines in immunogenic cell death: Applications for cancer immunotherapy. Cytokine 2017, 97, 123–132. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheinin, M.; Jeong, B.; Paidi, R.K.; Pahan, K. Regression of Lung Cancer in Mice by Intranasal Administration of SARS-CoV-2 Spike S1. Cancers 2022, 14, 5648. https://doi.org/10.3390/cancers14225648
Sheinin M, Jeong B, Paidi RK, Pahan K. Regression of Lung Cancer in Mice by Intranasal Administration of SARS-CoV-2 Spike S1. Cancers. 2022; 14(22):5648. https://doi.org/10.3390/cancers14225648
Chicago/Turabian StyleSheinin, Monica, Brian Jeong, Ramesh K. Paidi, and Kalipada Pahan. 2022. "Regression of Lung Cancer in Mice by Intranasal Administration of SARS-CoV-2 Spike S1" Cancers 14, no. 22: 5648. https://doi.org/10.3390/cancers14225648
APA StyleSheinin, M., Jeong, B., Paidi, R. K., & Pahan, K. (2022). Regression of Lung Cancer in Mice by Intranasal Administration of SARS-CoV-2 Spike S1. Cancers, 14(22), 5648. https://doi.org/10.3390/cancers14225648





