Efficacy of COVID-19 Booster Vaccines in Patients with Hematologic Malignancies: Experiences in a Real-World Scenario
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and COVID-19 Vaccination
2.2. Assessment of Humoral Response (Seroconversion) after Booster Vaccination
2.3. Definitions
2.4. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
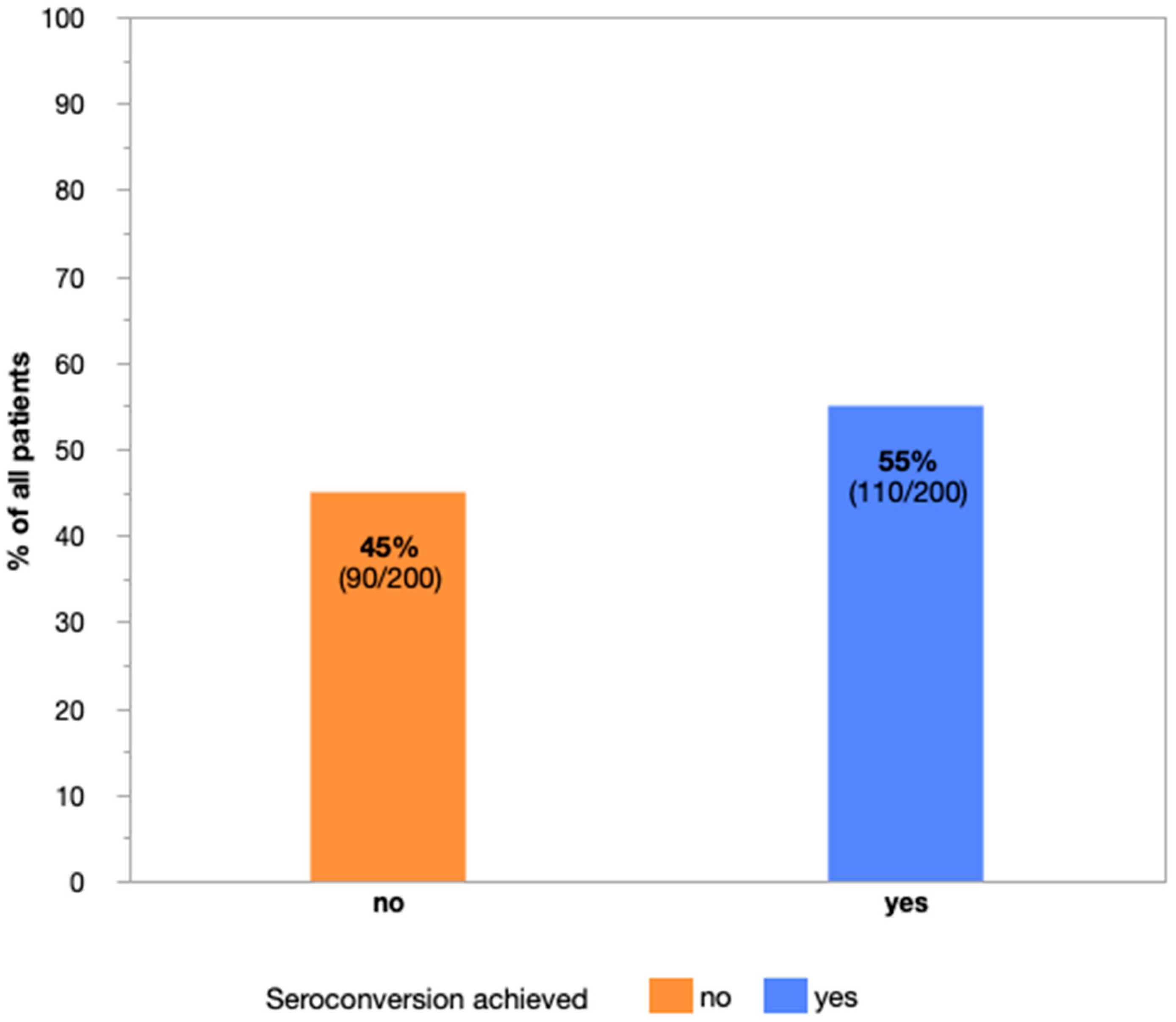
3.2. Serologic Response to COVID-19 Booster Vaccines in Study Patients
3.3. Impact of Time Interval between Last Cancer Treatment and Booster Vaccination
3.4. Age, Prior Anti-CD20 Therapy, Ongoing Cancer Treatment and Lymphocytopenia at the Time-Point of Booster Vaccination Impede Seroconversion in Patients with Hematologic Malignancies
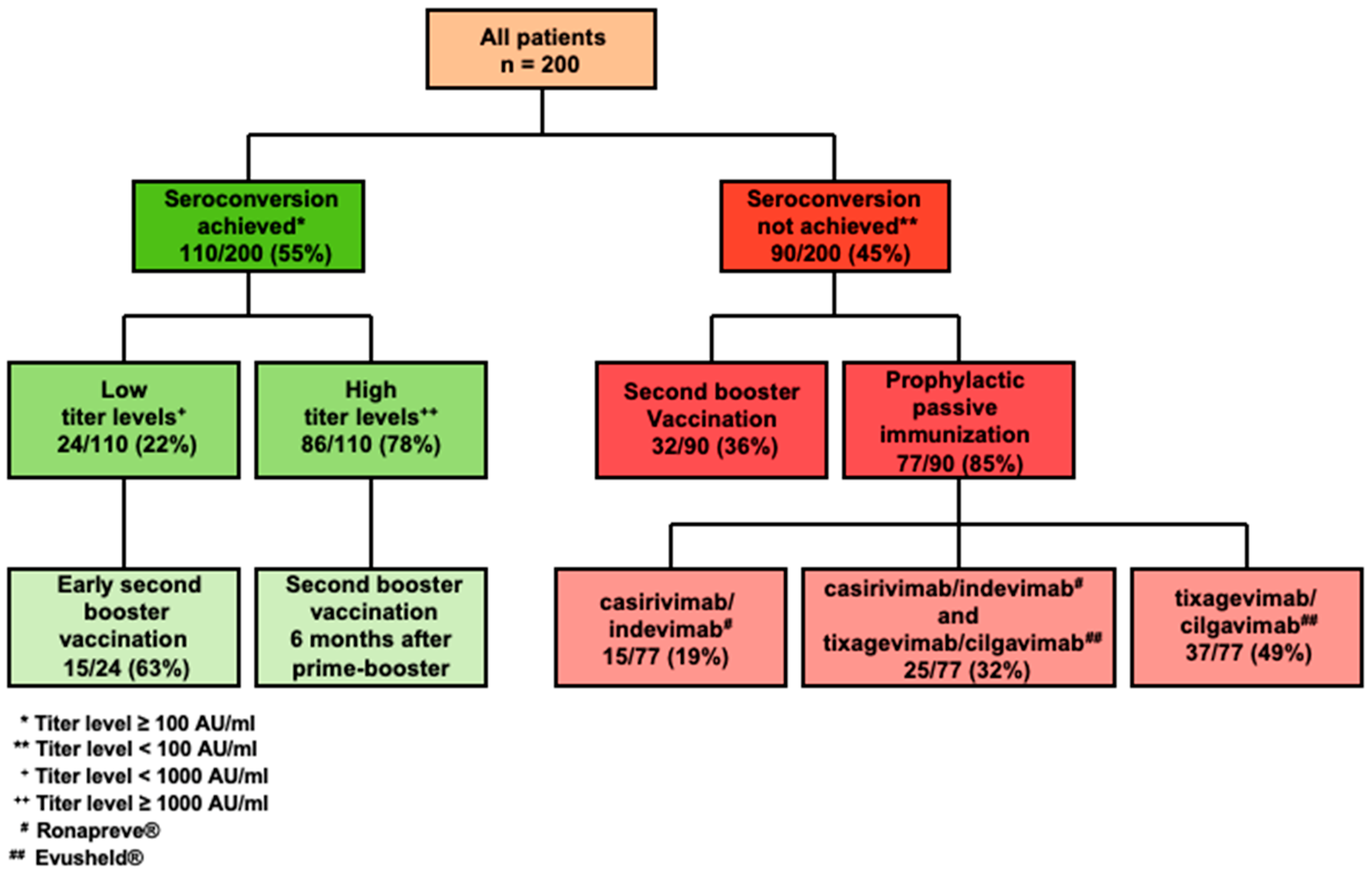
3.5. Comprehensive Management of HMs Patients According to Serologic Response after Prime-Boost Vaccination
3.6. Risk-Adjusted Pre-Emptive Prophylaxis of SARS-CoV-2 Infection in Vaccination Non-Responders with Hematologic Malignancies
3.7. Disease Courses of COVID-19 Breakthrough Infections in Patients with Hematologic Malignancies after Booster Vaccination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liebers, N.; Speer, C.; Benning, L.; Bruch, P.-M.; Kraemer, I.; Meissner, J.; Schnitzler, P.; Kräusslich, H.-G.; Dreger, P.; Mueller-Tidow, C.; et al. Humoral and Cellular Responses after COVID-19 Vaccination in Anti-CD20-Treated Lymphoma Patients. Blood 2022, 139, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Levy, I.; Lavi, A.; Zimran, E.; Grisariu, S.; Aumann, S.; Itchaki, G.; Berger, T.; Raanani, P.; Harel, R.; Aviv, A.; et al. COVID-19 among Patients with Hematological Malignancies: A National Israeli Retrospective Analysis with Special Emphasis on Treatment and Outcome. Leuk. Lymphoma 2021, 62, 3384–3393. [Google Scholar] [CrossRef] [PubMed]
- Boeckel, G.R.; Hölscher, S.D.; Bürger, C.; Jacob, T.; Krekeler, C.; Shumilov, E.; Reicherts, C.; Bleckmann, A.; Lenz, G.; Vollenberg, R.; et al. Comprehensive Treatment of Hematological Patients with SARS-CoV-2 Infection Including Anti-SARS-CoV-2 Monoclonal Antibodies: A Single-Center Experience Case Series. Curr. Oncol. 2022, 29, 2312–2325. [Google Scholar] [CrossRef]
- Passamonti, F.; Cattaneo, C.; Arcaini, L.; Bruna, R.; Cavo, M.; Merli, F.; Angelucci, E.; Krampera, M.; Cairoli, R.; Della Porta, M.G.; et al. Clinical Characteristics and Risk Factors Associated with COVID-19 Severity in Patients with Haematological Malignancies in Italy: A Retrospective, Multicentre, Cohort Study. Lancet Haematol. 2020, 7, e737–e745. [Google Scholar] [CrossRef]
- Pagano, L.; Salmanton-García, J.; Marchesi, F.; Busca, A.; Corradini, P.; Hoenigl, M.; Klimko, N.; Koehler, P.; Pagliuca, A.; Passamonti, F.; et al. COVID-19 Infection in Adult Patients with Hematological Malignancies: A European Hematology Association Survey (EPICOVIDEHA). J. Hematol. Oncol. J. Hematol. Oncol. 2021, 14, 168. [Google Scholar] [CrossRef]
- Vijenthira, A.; Gong, I.; Betschel, S.D.; Cheung, M.; Hicks, L.K. Vaccine Response Following Anti-CD20 Therapy: A Systematic Review and Meta-Analysis of 905 Patients. Blood Adv. 2021, 5, 2624–2643. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- El Sahly, H.M.; Baden, L.R.; Essink, B.; Doblecki-Lewis, S.; Martin, J.M.; Anderson, E.J.; Campbell, T.B.; Clark, J.; Jackson, L.A.; Fichtenbaum, C.J.; et al. Efficacy of the MRNA-1273 SARS-CoV-2 Vaccine at Completion of Blinded Phase. N. Engl. J. Med. 2021, 385, 1774–1785. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the MRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Sadoff, J.; Gray, G.; Vandebosch, A.; Cárdenas, V.; Shukarev, G.; Grinsztejn, B.; Goepfert, P.A.; Truyers, C.; Fennema, H.; Spiessens, B.; et al. Safety and Efficacy of Single-Dose Ad26.COV2.S Vaccine against Covid-19. N. Engl. J. Med. 2021, 384, 2187–2201. [Google Scholar] [CrossRef]
- Cavaleri, M.; Enzmann, H.; Straus, S.; Cooke, E. The European Medicines Agency’s EU Conditional Marketing Authorisations for COVID-19 Vaccines. Lancet 2021, 397, 355–357. [Google Scholar] [CrossRef]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Benda, M.; Mutschlechner, B.; Ulmer, H.; Grabher, C.; Severgnini, L.; Volgger, A.; Reimann, P.; Lang, T.; Atzl, M.; Huynh, M.; et al. Serological SARS-CoV-2 Antibody Response, Potential Predictive Markers and Safety of BNT162b2 MRNA COVID-19 Vaccine in Haematological and Oncological Patients. Br. J. Haematol. 2021, 195, 523–531. [Google Scholar] [CrossRef]
- Massarweh, A.; Eliakim-Raz, N.; Stemmer, A.; Levy-Barda, A.; Yust-Katz, S.; Zer, A.; Benouaich-Amiel, A.; Ben-Zvi, H.; Moskovits, N.; Brenner, B.; et al. Evaluation of Seropositivity Following BNT162b2 Messenger RNA Vaccination for SARS-CoV-2 in Patients Undergoing Treatment for Cancer. JAMA Oncol. 2021, 7, 1133. [Google Scholar] [CrossRef]
- Cavanna, L.; Citterio, C.; Toscani, I. COVID-19 Vaccines in Cancer Patients. Seropositivity and Safety. Systematic Review and Meta-Analysis. Vaccines 2021, 9, 1048. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.; Tessier, E.; Stowe, J.; Gower, C.; Kirsebom, F.; Simmons, R.; Gallagher, E.; Thelwall, S.; Groves, N.; Dabrera, G.; et al. Duration of Protection against Mild and Severe Disease by Covid-19 Vaccines. N. Engl. J. Med. 2022, 386, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Peeters, M.; Verbruggen, L.; Teuwen, L.; Vanhoutte, G.; Vande Kerckhove, S.; Peeters, B.; Raats, S.; Van der Massen, I.; De Keersmaecker, S.; Debie, Y.; et al. Reduced Humoral Immune Response after BNT162b2 Coronavirus Disease 2019 Messenger RNA Vaccination in Cancer Patients under Antineoplastic Treatment. ESMO Open 2021, 6, 100274. [Google Scholar] [CrossRef]
- Gavriatopoulou, M.; Terpos, E.; Ntanasis-Stathopoulos, I.; Briasoulis, A.; Gumeni, S.; Malandrakis, P.; Fotiou, D.; Migkou, M.; Theodorakakou, F.; Eleutherakis-Papaiakovou, E.; et al. Poor Neutralizing Antibody Responses in 106 Patients with WM after Vaccination against SARS-CoV-2: A Prospective Study. Blood Adv. 2021, 5, 4398–4405. [Google Scholar] [CrossRef]
- Herishanu, Y.; Avivi, I.; Aharon, A.; Shefer, G.; Levi, S.; Bronstein, Y.; Morales, M.; Ziv, T.; Shorer Arbel, Y.; Scarfò, L.; et al. Efficacy of the BNT162b2 MRNA COVID-19 Vaccine in Patients with Chronic Lymphocytic Leukemia. Blood 2021, 137, 3165–3173. [Google Scholar] [CrossRef]
- Roeker, L.E.; Knorr, D.A.; Thompson, M.C.; Nivar, M.; Lebowitz, S.; Peters, N.; Deonarine, I.; Momotaj, S.; Sharan, S.; Chanlatte, V.; et al. COVID-19 Vaccine Efficacy in Patients with Chronic Lymphocytic Leukemia. Leukemia 2021, 35, 2703–2705. [Google Scholar] [CrossRef]
- Pimpinelli, F.; Marchesi, F.; Piaggio, G.; Giannarelli, D.; Papa, E.; Falcucci, P.; Pontone, M.; Di Martino, S.; Laquintana, V.; La Malfa, A.; et al. Fifth-Week Immunogenicity and Safety of Anti-SARS-CoV-2 BNT162b2 Vaccine in Patients with Multiple Myeloma and Myeloproliferative Malignancies on Active Treatment: Preliminary Data from a Single Institution. J. Hematol. Oncol.J. Hematol. Oncol. 2021, 14, 81. [Google Scholar] [CrossRef] [PubMed]
- Malard, F.; Gaugler, B.; Gozlan, J.; Bouquet, L.; Fofana, D.; Siblany, L.; Eshagh, D.; Adotevi, O.; Laheurte, C.; Ricard, L.; et al. Weak Immunogenicity of SARS-CoV-2 Vaccine in Patients with Hematologic Malignancies. Blood Cancer J. 2021, 11, 142. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, E.A.; Segal, B.H. Immune Responses to COVID-19 Vaccines in Patients with Cancer: Promising Results and a Note of Caution. Cancer Cell 2021, 39, 1045–1047. [Google Scholar] [CrossRef] [PubMed]
- Greenberger, L.M.; Saltzman, L.A.; Senefeld, J.W.; Johnson, P.W.; DeGennaro, L.J.; Nichols, G.L. Antibody Response to SARS-CoV-2 Vaccines in Patients with Hematologic Malignancies. Cancer Cell 2021, 39, 1031–1033. [Google Scholar] [CrossRef] [PubMed]
- Schönlein, M.; Wrage, V.; Ghandili, S.; Mellinghoff, S.C.; Brehm, T.T.; Leypoldt, L.B.; Utz, N.; Schrader, R.M.; Alsdorf, W.; Börschel, N.; et al. Risk Factors for Poor Humoral Response to Primary and Booster SARS-CoV-2 Vaccination in Hematologic and Oncological Outpatients—COVIDOUT Study. Cancer Cell 2022, 40, 581–583. [Google Scholar] [CrossRef]
- Jiménez, M.; Roldán, E.; Fernández-Naval, C.; Villacampa, G.; Martinez-Gallo, M.; Medina-Gil, D.; Peralta-Garzón, S.; Pujadas, G.; Hernández, C.; Pagès, C.; et al. Cellular and Humoral Immunogenicity of the MRNA-1273 SARS-CoV-2 Vaccine in Patients with Hematologic Malignancies. Blood Adv. 2022, 6, 774–784. [Google Scholar] [CrossRef]
- Shroff, R.T.; Chalasani, P.; Wei, R.; Pennington, D.; Quirk, G.; Schoenle, M.V.; Peyton, K.L.; Uhrlaub, J.L.; Ripperger, T.J.; Jergović, M.; et al. Immune Responses to Two and Three Doses of the BNT162b2 MRNA Vaccine in Adults with Solid Tumors. Nat. Med. 2021, 27, 2002–2011. [Google Scholar] [CrossRef]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Sachdeva, R.; Gower, C.; Ramsay, M.; Lopez Bernal, J. Effectiveness of COVID-19 Booster Vaccines against COVID-19-Related Symptoms, Hospitalization and Death in England. Nat. Med. 2022, 28, 831–837. [Google Scholar] [CrossRef]
- Fendler, A.; Shepherd, S.T.C.; Au, L.; Wilkinson, K.A.; Wu, M.; Schmitt, A.M.; Tippu, Z.; Farag, S.; Rogiers, A.; Harvey, R.; et al. Immune Responses Following Third COVID-19 Vaccination Are Reduced in Patients with Hematological Malignancies Compared to Patients with Solid Cancer. Cancer Cell 2022, 40, 114–116. [Google Scholar] [CrossRef]
- Fendler, A.; Shepherd, S.T.C.; Au, L.; Wu, M.; Harvey, R.; Schmitt, A.M.; Tippu, Z.; Shum, B.; Farag, S.; Rogiers, A.; et al. Omicron Neutralising Antibodies after Third COVID-19 Vaccine Dose in Patients with Cancer. Lancet 2022, 399, 905–907. [Google Scholar] [CrossRef]
- Shapiro, L.C.; Thakkar, A.; Campbell, S.T.; Forest, S.K.; Pradhan, K.; Gonzalez-Lugo, J.D.; Quinn, R.; Bhagat, T.D.; Choudhary, G.S.; McCort, M.; et al. Efficacy of Booster Doses in Augmenting Waning Immune Responses to COVID-19 Vaccine in Patients with Cancer. Cancer Cell 2022, 40, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Alejo, J.L.; Mitchell, J.; Chiang, T.P.-Y.; Abedon, A.T.; Boyarsky, B.J.; Avery, R.K.; Tobian, A.A.R.; Levan, M.L.; Massie, A.B.; Garonzik-Wang, J.M.; et al. Antibody Response to a Fourth Dose of a SARS-CoV-2 Vaccine in Solid Organ Transplant Recipients: A Case Series. Transplantation 2021, 105, e280–e281. [Google Scholar] [CrossRef] [PubMed]
- Levin, M.J.; Ustianowski, A.; De Wit, S.; Launay, O.; Avila, M.; Templeton, A.; Yuan, Y.; Seegobin, S.; Ellery, A.; Levinson, D.J.; et al. Intramuscular AZD7442 (Tixagevimab–Cilgavimab) for Prevention of COVID-19. N. Engl. J. Med. 2022, 386, 2188–2200. [Google Scholar] [CrossRef]
- Shumilov, E.; Aperdannier, L.; Schmidt, N.; Szuszies, C.; Neesse, A.; Hoffknecht, P.; Khandanpour, C.; Mikesch, J.-H.; Stelljes, M.; Boeckel, G.R.; et al. Clinical Post-SARS-CoV-2 Infection Scenarios in Vaccinated and Non-Vaccinated Cancer Patients in Three German Cancer Centers: A Retrospective Analysis. Cancers 2022, 14, 3746. [Google Scholar] [CrossRef]
- Notarte, K.I.; Guerrero-Arguero, I.; Velasco, J.V.; Ver, A.T.; Santos de Oliveira, M.H.; Catahay, J.A.; Khan, M.S.R.; Pastrana, A.; Juszczyk, G.; Torrelles, J.B.; et al. Characterization of the Significant Decline in Humoral Immune Response Six Months Post-SARS-CoV-2 MRNA Vaccination: A Systematic Review. J. Med. Virol. 2022, 94, 2939–2961. [Google Scholar] [CrossRef]
- Pérez-Alós, L.; Armenteros, J.J.A.; Madsen, J.R.; Hansen, C.B.; Jarlhelt, I.; Hamm, S.R.; Heftdal, L.D.; Pries-Heje, M.M.; Møller, D.L.; Fogh, K.; et al. Modeling of Waning Immunity after SARS-CoV-2 Vaccination and Influencing Factors. Nat. Commun. 2022, 13, 1614. [Google Scholar] [CrossRef]
- Eliakim-Raz, N.; Stemmer, A.; Ghantous, N.; Ness, A.; Awwad, M.; Leibovici-Weisman, Y.; Stemmer, S.M. Antibody Titers After a Third and Fourth SARS-CoV-2 BNT162b2 Vaccine Dose in Older Adults. JAMA Netw. Open 2022, 5, e2223090. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239. [Google Scholar] [CrossRef]
- La Torre, G. Influenza and Pneumococcal Vaccination in Hematological Malignancies: A Systematic Review of Efficacy, Effectiveness and Safety. Mediterr. J. Hematol. Infect. Dis. 2016, 8, e2016044. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rieger, C.T.; Liss, B.; Mellinghoff, S.; Buchheidt, D.; Cornely, O.A.; Egerer, G.; Heinz, W.J.; Hentrich, M.; Maschmeyer, G.; Mayer, K.; et al. Anti-Infective Vaccination Strategies in Patients with Hematologic Malignancies or Solid Tumors—Guideline of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Medical Oncology (DGHO). Ann. Oncol. 2018, 29, 1354–1365. [Google Scholar] [CrossRef]
- Özkurt, Z.N.; Suyanı, E.; Haznedar, R.; Yağcı, M. A Randomized Study Comparing the Efficacy of Three Hepatitis B Vaccine Induction Regimens in Adult Patients with Hematological Malignancies. Turk. J. Hematol. 2016, 33, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Riccardi, N.; Falcone, M.; Yahav, D. Vaccination for SARS-CoV-2 in Hematological Patients. Acta Haematol. 2022, 145, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Teh, J.S.K.; Coussement, J.; Neoh, Z.C.F.; Spelman, T.; Lazarakis, S.; Slavin, M.A.; Teh, B.W. Immunogenicity of COVID-19 Vaccines in Patients with Hematologic Malignancies: A Systematic Review and Meta-Analysis. Blood Adv. 2022, 6, 2014–2034. [Google Scholar] [CrossRef]
- Reimann, P.; Ulmer, H.; Mutschlechner, B.; Benda, M.; Severgnini, L.; Volgger, A.; Lang, T.; Atzl, M.; Huynh, M.; Gasser, K.; et al. Efficacy and Safety of Heterologous Booster Vaccination with Ad26.COV2.S after BNT162b2 MRNA COVID-19 Vaccine in Haemato-oncological Patients with No Antibody Response. Br. J. Haematol. 2022, 196, 577–584. [Google Scholar] [CrossRef]
- Petzer, V.; Steiner, N.; Angelova-Unterberger, O.; Hetzenauer, G.; Philipp-Abbrederis, K.; Willenbacher, E.; Feistritzer, C.; Willenbacher, W.; Rudzki, J.; Stauder, R.; et al. Serologic Responses to COVID-19 Vaccines in Hematological Patients Are Predominantly Impaired in Lymphoid but Not in Myeloid Malignancies. HemaSphere 2022, 6, e686. [Google Scholar] [CrossRef]
- Mittelman, M. Is COVID Vaccine Effective in Patients with Myeloid Malignancy? Br. J. Haematol. 2022, 197, 656–658. [Google Scholar] [CrossRef] [PubMed]
- Nelli, F.; Fabbri, A.; Panichi, V.; Giannarelli, D.; Topini, G.; Giron Berrios, J.R.; Virtuoso, A.; Marrucci, E.; Mazzotta, M.; Schirripa, M.; et al. Peripheral Lymphocyte Subset Counts Predict Antibody Response after SARS-CoV-2 MRNA-BNT162b2 Vaccine in Cancer Patients: Results from the Vax-On-Profile Study. Int. Immunopharmacol. 2022, 108, 108774. [Google Scholar] [CrossRef]
- Ghandili, S.; Schönlein, M.; Wiessner, C.; Becher, H.; Lütgehetmann, M.; Brehm, T.T.; Schulze zur Wiesch, J.; Bokemeyer, C.; Sinn, M.; Weisel, K.C.; et al. Lymphocytopenia and Anti-CD38 Directed Treatment Impact the Serological SARS-CoV-2 Response after Prime Boost Vaccination in Patients with Multiple Myeloma. J. Clin. Med. 2021, 10, 5499. [Google Scholar] [CrossRef]
- Jullien, M.; Le Bourgeois, A.; Coste-Burel, M.; Peterlin, P.; Garnier, A.; Audrain, M.; Rimbert, M.; Imbert, B.M.; Drumel, T.; Le Gouill, S.; et al. Profound B-Cell Lymphopenia Is a Major Factor Predicting Poor Humoral Response after BNT162b2 MRNA Sars-Cov-2 Vaccines in Recipients of Allogeneic Hematopoietic Stem Cell Transplantation. Blood 2021, 138, 3911. [Google Scholar] [CrossRef]
- Bagacean, C.; Letestu, R.; Al-Nawakil, C.; Brichler, S.; Lévy, V.; Sritharan, N.; Delmer, A.; Dartigeas, C.; Leblond, V.; Roos-Weil, D.; et al. Humoral Response to MRNA Anti–COVID-19 Vaccines BNT162b2 and MRNA-1273 in Patients with Chronic Lymphocytic Leukemia. Blood Adv. 2022, 6, 207–211. [Google Scholar] [CrossRef]
- Pleyer, C.; Laing, K.J.; Ali, M.A.; McClurkan, C.L.; Soto, S.; Ahn, I.E.; Nierman, P.; Maddux, E.; Lotter, J.; Superata, J.; et al. BTK Inhibitors Impair Humoral and Cellular Responses to Recombinant Zoster Vaccine in CLL. Blood Adv. 2022, 6, 1732–1740. [Google Scholar] [CrossRef] [PubMed]
- Henriquez, S.; Zerbit, J.; Bruel, T.; Ouedrani, A.; Planas, D.; Deschamps, P.; Staropoli, I.; Hadjadj, J.; Varet, B.; Suarez, F.; et al. Anti-CD38 Therapy Impairs SARS-CoV-2 Vaccine Response in Multiple Myeloma Patients; Infectious Diseases (except HIV/AIDS): Brookline, MA, USA, 2021. [Google Scholar]
- Maneikis, K.; Šablauskas, K.; Ringelevičiūtė, U.; Vaitekėnaitė, V.; Čekauskienė, R.; Kryžauskaitė, L.; Naumovas, D.; Banys, V.; Pečeliūnas, V.; Beinortas, T.; et al. Immunogenicity of the BNT162b2 COVID-19 MRNA Vaccine and Early Clinical Outcomes in Patients with Haematological Malignancies in Lithuania: A National Prospective Cohort Study. Lancet Haematol. 2021, 8, e583–e592. [Google Scholar] [CrossRef]
- Ghione, P.; Gu, J.J.; Attwood, K.; Torka, P.; Goel, S.; Sundaram, S.; Mavis, C.; Johnson, M.; Thomas, R.; McWhite, K.; et al. Impaired Humoral Responses to COVID-19 Vaccination in Patients with Lymphoma Receiving B-Cell–Directed Therapies. Blood 2021, 138, 811–814. [Google Scholar] [CrossRef]
- Crombie, J.L.; Sherman, A.C.; Cheng, C.-A.; Ryan, C.E.; Zon, R.; Desjardins, M.; Baker, P.; McDonough, M.; Izaguirre, N.; Bausk, B.; et al. Activity of MRNA COVID-19 Vaccines in Patients with Lymphoid Malignancies. Blood Adv. 2021, 5, 3062–3065. [Google Scholar] [CrossRef] [PubMed]
- Benjamini, O.; Rokach, L.; Itchaki, G.; Braester, A.; Shvidel, L.; Goldschmidt, N.; Shapira, S.; Dally, N.; Avigdor, A.; Rahav, G.; et al. Safety and Efficacy of BNT162b MRNA Covid19 Vaccine in Patients with Chronic Lymphocytic Leukemia. Haematologica 2021, 107, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Perry, C.; Luttwak, E.; Balaban, R.; Shefer, G.; Morales, M.M.; Aharon, A.; Tabib, Y.; Cohen, Y.C.; Benyamini, N.; Beyar-Katz, O.; et al. Efficacy of the BNT162b2 MRNA COVID-19 Vaccine in Patients with B-Cell Non-Hodgkin Lymphoma. Blood Adv. 2021, 5, 3053–3061. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Honda, A.; Kurokawa, M. COVID-19 MRNA Vaccine in Patients With Lymphoid Malignancy or Anti-CD20 Antibody Therapy: A Systematic Review and Meta-Analysis. Clin. Lymphoma Myeloma Leuk. 2022, 22, e691–e707. [Google Scholar] [CrossRef]
- Shree, T.; Shankar, V.; Lohmeyer, J.J.K.; Czerwinski, D.K.; Schroers-Martin, J.G.; Rodriguez, G.M.; Beygi, S.; Kanegai, A.M.; Corbelli, K.S.; Gabriel, E.; et al. CD20-Targeted Therapy Ablates De Novo Antibody Response to Vaccination but Spares Preestablished Immunity. Blood Cancer Discov. 2022, 3, 95–102. [Google Scholar] [CrossRef]
- Shumilov, E.; Hoffknecht, P.; Koch, R.; Peceny, R.; Voigt, S.; Schmidt, N.; Peeck, M.; Bacher, U.; Scheithauer, S.; Trümper, L.; et al. Diagnostic, Clinical and Post-SARS-CoV-2 Scenarios in Cancer Patients with SARS-CoV-2: Retrospective Analysis in Three German Cancer Centers. Cancers 2021, 13, 2917. [Google Scholar] [CrossRef]
- Magen, O.; Waxman, J.G.; Makov-Assif, M.; Vered, R.; Dicker, D.; Hernán, M.A.; Lipsitch, M.; Reis, B.Y.; Balicer, R.D.; Dagan, N. Fourth Dose of BNT162b2 MRNA Covid-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2022, 386, 1603–1614. [Google Scholar] [CrossRef]
- Bar-On, Y.M.; Goldberg, Y.; Mandel, M.; Bodenheimer, O.; Amir, O.; Freedman, L.; Alroy-Preis, S.; Ash, N.; Huppert, A.; Milo, R. Protection by a Fourth Dose of BNT162b2 against Omicron in Israel. N. Engl. J. Med. 2022, 386, 1712–1720. [Google Scholar] [CrossRef] [PubMed]
- Dimeglio, C.; Del Bello, A.; Chapuy-Regaud, S.; Esposito, L.; Danet, C.; Couat, C.; Izopet, J.; Kamar, N. Casirivimab–Imdevimab to Prevent SARS-CoV-2 Infections in Solid Organ Transplant Recipients. Transplantation 2022, 106, e275–e276. [Google Scholar] [CrossRef]
- Al Jurdi, A.; Morena, L.; Cote, M.; Bethea, E.; Azzi, J.; Riella, L.V. Tixagevimab/Cilgavimab Pre-exposure Prophylaxis Is Associated with Lower Breakthrough Infection Risk in Vaccinated Solid Organ Transplant Recipients during the Omicron Wave. Am. J. Transplant. 2022, ajt.17128. [Google Scholar] [CrossRef] [PubMed]
- Young-Xu, Y.; Epstein, L.; Marconi, V.C.; Davey, V.; Zwain, G.; Smith, J.; Korves, C.; Cunningham, F.; Bonomo, R.; Ginde, A.A. Tixagevimab/Cilgavimab for Prevention of COVID-19 during the Omicron Surge: Retrospective Analysis of National VA Electronic Data; Infectious Diseases (Except HIV/AIDS): Brookline, MA, USA, 2022. [Google Scholar]
- Food and Drug Administration Emergency Use Authorization (EUA) for Evusheld 2022. Available online: https://www.fda.gov/media/154701/download (accessed on 3 November 2022).
- Ollila, T.A.; Masel, R.H.; Reagan, J.L.; Lu, S.; Rogers, R.D.; Paiva, K.J.; Taher, R.; Burguera-Couce, E.; Zayac, A.S.; Yakirevich, I.; et al. Seroconversion and Outcomes after Initial and Booster COVID-19 Vaccination in Adults with Hematologic Malignancies. Cancer 2022, 128, 3319–3329. [Google Scholar] [CrossRef] [PubMed]
- Pagano, L.; Salmanton-García, J.; Marchesi, F.; López-García, A.; Lamure, S.; Itri, F.; Gomes-Silva, M.; Dragonetti, G.; Falces-Romero, I.; van Doesum, J.; et al. COVID-19 in Vaccinated Adult Patients with Hematological Malignancies: Preliminary Results from EPICOVIDEHA. Blood 2022, 139, 1588–1592. [Google Scholar] [CrossRef] [PubMed]
- Langerbeins, P.; Hallek, M. COVID-19 in Patients with Hematologic Malignancy. Blood 2022, 140, 236–252. [Google Scholar] [CrossRef]
- Gupta, A.; Gonzalez-Rojas, Y.; Juarez, E.; Crespo Casal, M.; Moya, J.; Falci, D.R.; Sarkis, E.; Solis, J.; Zheng, H.; Scott, N.; et al. Early Treatment for Covid-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab. N. Engl. J. Med. 2021, 385, 1941–1950. [Google Scholar] [CrossRef]
- Gupta, A.; Gonzalez-Rojas, Y.; Juarez, E.; Crespo Casal, M.; Moya, J.; Rodrigues Falci, D.; Sarkis, E.; Solis, J.; Zheng, H.; Scott, N.; et al. Effect of Sotrovimab on Hospitalization or Death Among High-Risk Patients With Mild to Moderate COVID-19: A Randomized Clinical Trial. JAMA 2022, 327, 1236. [Google Scholar] [CrossRef]
- Najjar-Debbiny, R.; Gronich, N.; Weber, G.; Khoury, J.; Amar, M.; Stein, N.; Goldstein, L.H.; Saliba, W. Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients. Clin. Infect. Dis. 2022, ciac443. [Google Scholar] [CrossRef]
- European Medicines Agency Adapted Vaccine Targeting BA.4 and BA.5 Omicron Variants and Original SARS-CoV-2 Recommended for Approval. Available online: https://www.ema.europa.eu/en/news/adapted-vaccine-targeting-ba4-ba5-omicron-variants-original-sars-cov-2-recommended-approval (accessed on 3 November 2022).
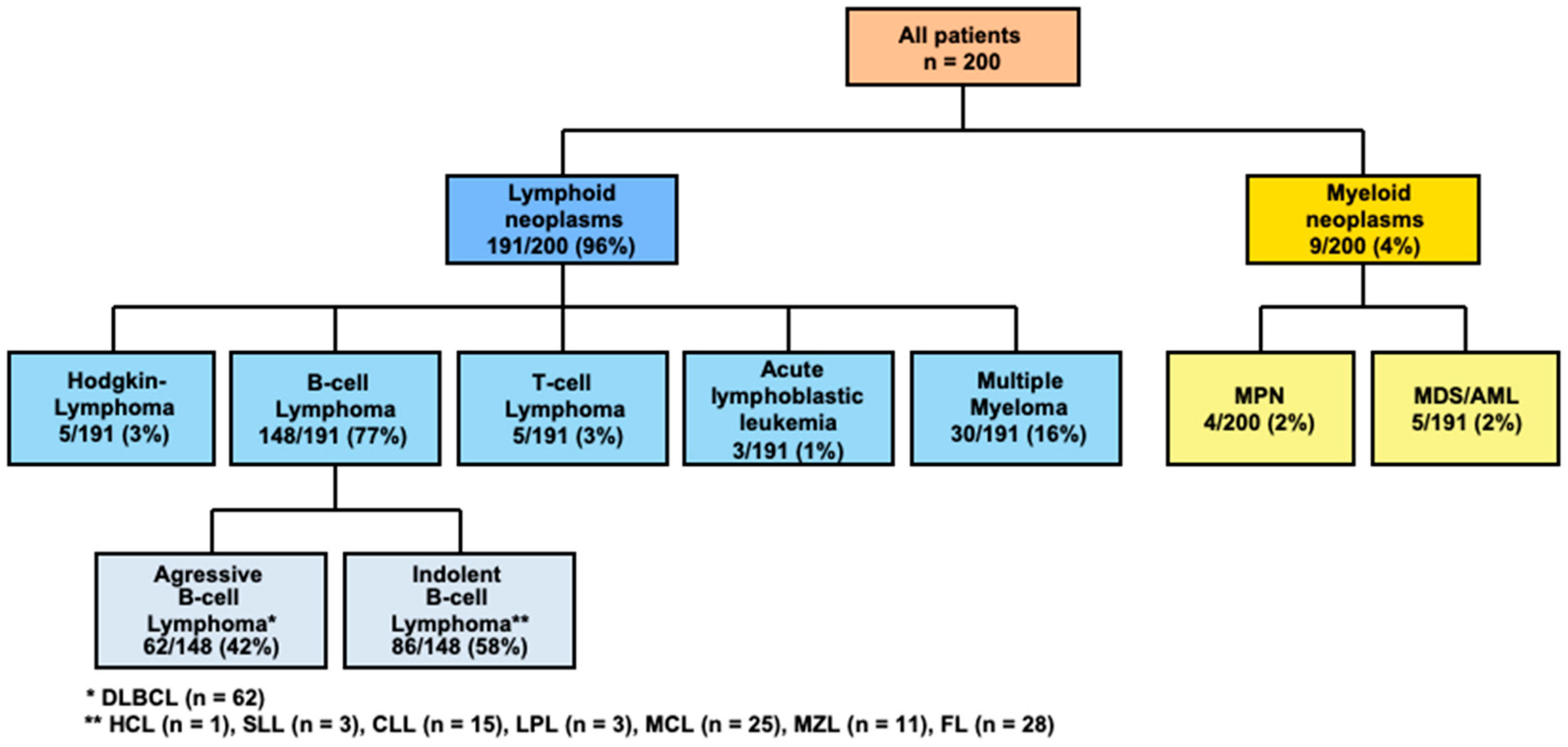

| Parameter | Patients, n = 200 | |
|---|---|---|
| Sex (M/F), n (%) | 136/64 | 68%/32% |
| Median age, years (range) | 65 | 20–91 |
| Hematologic neoplasms, n (%) | n = 200 | 100% |
| Lymphoma | 158 | 79% |
| - B-cell lymphoma | 148 | 94% |
| - T-cell lymphoma | 5 | 3% |
| - Hodgkin lymphoma | 5 | 3% |
| Multiple myeloma | 30 | 15% |
| Acute leukemia | 7 | 3% |
| - ALL | 3 | 43% |
| - AML | 4 | 57% |
| MPN | 4 | 2% |
| MDS | 1 | 1% |
| Cancer treatment preceding prime-boost vaccination, n (%) | ||
| Cytostatic (conventional) chemotherapy | 165 | 82% |
| - cytostatic agents only | 5 | 3% |
| - combined with immunotherapy | 95 | 57% |
| - combined with immunotherapy and targeted therapy | 25 | 15% |
| - combined with immunotherapy and radiotherapy | 12 | 7% |
| - combined with targeted therapy | 27 | 17% |
| - combined with radiotherapy | 1 | 1% |
| Immunotherapy | 15 | 8% |
| - immunotherapy monoregimen | 7 | 47% |
| - combined with radiotherapy | 8 | 53% |
| Targeted therapy | 12 | 6% |
| - targeted therapy only | 11 | 92% |
| - combined with radiotherapy | 1 | 8% |
| No therapy yet due to first diagnosis or “watch and wait” strategy | 8 | 4% |
| Active treatment at time-point of prime-boost vaccination | 94/200 | 47% |
| Anti-CD20 B cell-depleting therapy prior to prime-boost vaccination | 140/200 | 70% |
| - rituximab only | 111 | 79% |
| - obinutuzumab only | 22 | 16% |
| - more than one CD20-depleting agent | 7 | 5% |
| Therapy with an anti-CD38 directed antibody prior toprime-boost vaccination | 14/200 | 7% |
| Therapy with BTK inhibitor prior to prime-boost vaccination | 23/200 | 12% |
| - ibrutinib | 20 | 87% |
| - acalabrutinib | 3 | 13% |
| Lymphocytopenia at time-point of prime-boost vaccination | 42/200 | 21% |
| - prior anti-CD20 B-cell depletion | 28/42 | 67% |
| - prior BTKi therapy | 6/42 | 14% |
| - prior therapy with anti-CD38 antibody | 4/42 | 9% |
| Hematopoietic stem cell transplantation prior to prime-boost vaccination | 61/200 | 31% |
| Autologous stem cell transplantation | 60 | 98% |
| Allogeneic stem cell transplantation | 1 | 2% |
| Number of therapy lines prior to prime-boost vaccination, n (%) | ||
| No therapy yet | 7 | 4% |
| One therapy line | 131 | 65% |
| Two therapy lines | 31 | 16% |
| Three therapy lines | 12 | 6% |
| ≥ Four therapy lines | 19 | 9% |
| Remission status of HM at SARS-CoV-2 antibody testing, n (%) | ||
| Complete remission | 123 | 61% |
| Partial remission | 58 | 29% |
| Stable disease | 5 | 3% |
| Relapsed/progressive disease | 10 | 5% |
| Not yet assessed | 4 | 2% |
| Parameter | Seroconversion Achieved n = 110/200 (55%) | Seroconversion Not Achieved N = 90/200 (45%) | p-Value |
|---|---|---|---|
| Sex (M/F, in %) | 66%/34% | 71%/29% | 0.45 |
| Mean age, years (range) | 62 | 67 | 0.08 |
| Therapy prior to prime-boost vaccination (%) | |||
| - Cytotoxic therapy | 92% | 99% | 0.045 |
| - anti-CD20 B-cell depletion | 52% | 91% | <0.001 |
| - BTKi | 9% | 14% | 0.27 |
| - anti-CD38 therapy | 9% | 4% | 0.27 |
| - autologous transplantation | 35% | 27% | 0.21 |
| Ongoing systemic cancer treatment at time-point of prime-boost vaccination (% of all patients. in subgroup) | 39% | 57% | 0.045 |
| Lymphocytopenia at time-point of prime-boost vaccination (% of patients. in subgroup) | 16% | 34% | 0.03 |
| Heterologous vaccination (%) | 9% | 12% | 0.49 |
| Mean therapy line (range) | 1.5 (1–6) | 2.0 (1–15) | 0.01 |
| Remission status prior to prime-boost vaccination | |||
| - Complete Remission | 62% | 61% | |
| - Partial Remission | 29% | 29% | |
| - Stable Disease | 4% | 1% | } 0.52 |
| - Progressive Disease | 2% | 1% | |
| - not yet assessed | 3% |
| Parameter | Coefficient (B) | EXP(B) | 95% Confidence Interval of EXP(B) | p-Value |
|---|---|---|---|---|
| Constant | 7.183 | 1316.57 | <0.001 | |
| Age | −0.034 | 0.966 | [0.935; 0.998] | 0.039 |
| Sex | −0.055 | 0.946 | [0.446; 2.007] | 0.885 |
| Prior anti-CD20 B-cell depleting-therapy | −3.953 | 0.019 | [0.004; 0.083] | <0.001 |
| Prior cytotoxic treatment | −0.203 | 0.816 | [0.06; 11.084] | 0.879 |
| Prior treatment with BTKi | −0.256 | 1.292 | [0.409; 4.077] | 0.662 |
| Prior anti-CD38 containing therapy | −0.397 | 0.673 | [0.902; 4.937] | 0.672 |
| Ongoing cancer treatment | −1.807 | 0.164 | [0.069; 0.391] | <0.001 |
| Heterologous vaccination | −0.336 | 0.715 | [0.24; 2.125] | 0.546 |
| Prior autologous transplantation | −0.344 | 0.709 | [0.301; 1.670] | 0.432 |
| Therapy line | −0.281 | 0.755 | [0.546; 1.045] | 0.091 |
| Remission state at time point of booster vaccination | −0.008 | 0.992 | [0.601; 1.638] | 0.975 |
| Lymphocytopenia at time point of booster vaccination | −0.791 | 0.453 | [0.221; 0.928] | 0.03 |
| Parameter | Patients, n = 200 | |
|---|---|---|
| COVID-19 breakthrough infection after booster vaccination n = 29/200 (15%) | ||
| Sex (M/F; %) | 20/9 | 69%/31% |
| Median age, years (range) | 66 | 45–82 |
| B-cell lymphoma | 27 | 93% |
| MPN | 2 | 7% |
| Cancer treatment preceding COVID-19, n (%) | ||
| Conventional chemotherapy | 25 | 86% |
| - combined with immunotherapy | 11 | 44% |
| - combined with immunotherapy and targeted therapy | 5 | 20% |
| - combined with immunotherapy and radiotherapy | 1 | 4% |
| - combined with targeted therapy | 8 | 32% |
| Targeted therapy | 4 | 14% |
| Anti-CD20 B cell-depleting therapy prior to COVID-19 | 16/29 | 55% |
| Median time from last cancer treatment to COVID-19, months (range) | 0.6 | 0–64 |
| <3 months | 15 | 52% |
| 3–12 months | 5 | 17% |
| >12 months | 9 | 31% |
| Remission status assessed prior to COVID-19 breakthrough infection | 29 | 100% |
| - Complete Remission | 14 | 49% |
| - Partial Remission | 11 | 38% |
| - Stable Disease | 1 | 3% |
| - Progressive Disease | 2 | 7% |
| - not yet assessed | 1 | 3% |
| Non-responders to booster vaccination as indicated by lack of antibody titer levels prior to COVID-19 | 12/29 | 41% |
| Documented seroconversion after booster vaccination prior to COVID-19 | 17/29 | 59% |
| - median (mean) antibody titer level (range) in AU/mL | 302 (6 298) | 0–40,000 AU/ml |
| 4th vaccination prior to COVID-19 | 6/29 | 21% |
| Prior passive immunization | 4/29 | 14% |
| Clinical courses of COVID-19 breakthrough infection | ||
| - asymptomatic/mild COVID-19 | 27 | 93% |
| - patients with lack of seroconversion (of them with prior passive immunization) | 10 (4) | 37% (40%) |
| - patients with seroconversion | 17 | 63% |
| - severe COVID-19 | 2 | 7% |
| - patients with lack of seroconversion (of them with prior passive immunization) | 2 (0) | 100% (0%) |
| - critical COVID-19 | 0 | 0 |
| COVID-19 treatment | 15 | 52% |
| - sotrovimab | 10 | 67% |
| - cilgavimab/indevimab | 1 | 6% |
| - nirmatrelvir/ritonavir | 4 | 27% |
| Parameter | Coefficient (B) | EXP(B) | 95% Confidence Interval of EXP(B) | p-Value |
| Constant | 0.512 | 1.668 | 0.028 | |
| Age | 0.002 | 1.002 | [0.962; 1.004] | 0.912 |
| Sex | −0.256 | 1.292 | [0.446; 2.007] | 0.885 |
| seroconversion | −1.927 | 0.146 | [0.030; 0.707] | 0.017 |
| casirivimab/indevimab | −1.718 | 0.179 | [0.032; 0.993] | 0.049 |
| tixagevimab/cilgavimab | −4.229 | 0.015 | [0.001; 0.159] | <0.001 |
| active treatment at booster vaccination | 0.387 | 1.473 | [0.452; 4.803] | 0.521 |
| second booster (fourth) vaccination | −0.710 | 0.492 | [0.155; 1.557] | 0.227 |
| Therapy line | 0.268 | 7.37 | [0.909; 1.879] | 0.148 |
| Remission state | −0.305 | 0.453 | [0336; 0.737] | 0.505 |
| Entity | −0.190 | 0.827 | [0.615; 1.112] | 0.209 |
| Cytotoxic therapy prior to treatment | 0.215 | 1.24 | [0.1; 15.43] | 0.867 |
| CD20 depletion prior to vaccination | −1.017 | 0.362 | [0.101; 1.29] | 0.117 |
| Ab titer level | 0.03 | 1 | [0.972; 1.032] | 0.505 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krekeler, C.; Reitnauer, L.; Bacher, U.; Khandanpour, C.; Steger, L.; Boeckel, G.R.; Klosner, J.; Tepasse, P.-R.; Kemper, M.; Hennies, M.T.; et al. Efficacy of COVID-19 Booster Vaccines in Patients with Hematologic Malignancies: Experiences in a Real-World Scenario. Cancers 2022, 14, 5512. https://doi.org/10.3390/cancers14225512
Krekeler C, Reitnauer L, Bacher U, Khandanpour C, Steger L, Boeckel GR, Klosner J, Tepasse P-R, Kemper M, Hennies MT, et al. Efficacy of COVID-19 Booster Vaccines in Patients with Hematologic Malignancies: Experiences in a Real-World Scenario. Cancers. 2022; 14(22):5512. https://doi.org/10.3390/cancers14225512
Chicago/Turabian StyleKrekeler, Carolin, Lea Reitnauer, Ulrike Bacher, Cyrus Khandanpour, Leander Steger, Göran Ramin Boeckel, Justine Klosner, Phil-Robin Tepasse, Marcel Kemper, Marc Tim Hennies, and et al. 2022. "Efficacy of COVID-19 Booster Vaccines in Patients with Hematologic Malignancies: Experiences in a Real-World Scenario" Cancers 14, no. 22: 5512. https://doi.org/10.3390/cancers14225512
APA StyleKrekeler, C., Reitnauer, L., Bacher, U., Khandanpour, C., Steger, L., Boeckel, G. R., Klosner, J., Tepasse, P.-R., Kemper, M., Hennies, M. T., Mesters, R., Stelljes, M., Schmitz, N., Kerkhoff, A., Schliemann, C., Mikesch, J.-H., Schmidt, N., Lenz, G., Bleckmann, A., & Shumilov, E. (2022). Efficacy of COVID-19 Booster Vaccines in Patients with Hematologic Malignancies: Experiences in a Real-World Scenario. Cancers, 14(22), 5512. https://doi.org/10.3390/cancers14225512






