Simple Summary
Sphingolipidoses are a subgroup of rare inherited disorders of lipid metabolism, most often due to a lysosomal enzymatic defect affecting sphingolipid catabolism. They are characterized by the accumulation of sphingolipids and their deacylated derivatives, called lysosphingolipids. An increased occurrence of cancer is suspected in some of these disorders. Whether lysosphingolipids are involved is unknown, and there is little data available on this topic. Here, we review the literature on lysosphingolipids and their potential effects on cellular properties, which could contribute to cancer development. Finally, we present data showing that one of them (namely, glucosylsphingosine) induces modifications of melanoma cells, which may favor tumor progression. Our review highlights that a better knowledge of lysosphingolipids, the biomarkers of rare diseases, could contribute to a better understanding of the pathophysiology of cancer.
Abstract
Sphingolipids play a key structural role in cellular membranes and/or act as signaling molecules. Inherited defects of their catabolism lead to lysosomal storage diseases called sphingolipidoses. Although progress has been made toward a better understanding of their pathophysiology, several issues still remain unsolved. In particular, whether lysosphingolipids, the deacylated form of sphingolipids, both of which accumulate in these diseases, are simple biomarkers or play an instrumental role is unclear. In the meanwhile, evidence has been provided for a high risk of developing malignancies in patients affected with Gaucher disease, the most common sphingolipidosis. This article aims at analyzing the potential involvement of lysosphingolipids in cancer. Knowledge about lysosphingolipids in the context of lysosomal storage diseases is summarized. Available data on the nature and prevalence of cancers in patients affected with sphingolipidoses are also reviewed. Then, studies investigating the biological effects of lysosphingolipids toward pro or antitumor pathways are discussed. Finally, original findings exploring the role of glucosylsphingosine in the development of melanoma are presented. While this lysosphingolipid may behave like a protumorigenic agent, further investigations in appropriate models are needed to elucidate the role of these peculiar lipids, not only in sphingolipidoses but also in malignant diseases in general.
1. Introduction
Sphingolipids (SLs) comprise a very large number of amphiphilic lipid molecules, having in common a long chain aminoalcohol referred to as a sphingoid base. They are present in plants and animals, particularly in mammals. Owing to their chemical structure, most of them are constituents of cell membranes and preferentially locate in the outer leaflet of the plasma membrane. Similar to diacylglycerolipids, some of the major SLs are also components of circulating lipoproteins. Of note, sphingosine 1-phosphate (S1P) is typically found in the extracellular compartment, being relatively abundant in plasma and lymph. Membrane SLs, which are, by far, the predominant SL species, contain one molecule of fatty acid. In accordance with previous classifications of lipids, where the term “lyso” denotes a glycero(phospho)lipid lacking a radyl group [1], lysosphingolipids (lysoSLs) are defined as SLs that lack the fatty acyl moiety.
SLs are synthesized by all mammalian cells. Their biosynthesis starts in the endoplasmic reticulum (ER) by the condensation of an acyl-CoA, mainly palmitoyl-CoA, and L-serine to form the backbone of the sphingoid base. Reduction of this initial product leads to sphinganine, which is N-acylated, i.e., linked to a fatty acyl moiety through an amide bond by a ceramide synthase. After desaturation, the resulting ceramide molecule can be further transformed into complex SLs, such as sphingomyelin or glycosphingolipids. Whereas sphingomyelin and β-glucosylceramide-based glycolipids are synthesized in the Golgi apparatus, β-galactosylceramide is formed in the ER. They all are transported to the plasma membrane. The degradation of diet-derived SLs is mediated by secreted intestinal enzymes. As to cellular SLs, their physiological catabolism mostly occurs in the lysosomes through a conserved sequence of hydrolytic steps (see Figure 1). In this pathway, the breakdown of complex SLs gradually releases the residues of the hydrophilic headgroup attached to the ceramide backbone. The last step of lysosomal degradation is catalyzed by acid ceramidase, which cleaves the amide bond and, thus, liberates sphingosine and fatty acids.
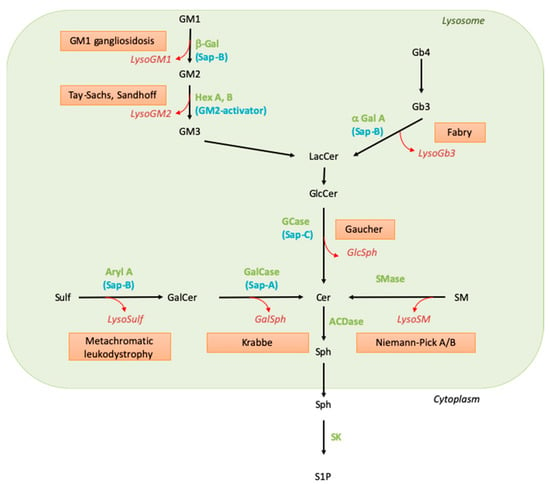
Figure 1.
Sphingolipid catabolism and associated diseases. Green names correspond to the enzyme names, blue names to their activators, the red boxed texts contain the disease name, and the red and italic names indicate the corresponding lysoSL. Abbreviations: α-Gal: alpha-galactosidase; ACDase, acid ceramidase; Aryl A, arylsulfatase A; β-Gal, beta-galactosidase; Cer, ceramide; GalCase, galactosylceramidase; GalSph, galactosylsphingosine; GCase, glucosylceramidase; GlcCer, glucosylceramide; GlcSph, glucosylsphingosine; Hex, hexosaminidase; LacCer, lactosylceramide; LysoSulf, lysosulfatide; Sap, saposin; SK, sphingosine kinase; SM, sphingomyelin; SMase, sphingomyelinase; Sph, sphingosine; Sulf, sulfatide; S1P, sphingosine 1-phosphate.
Knowledge of SLs and SL metabolism has been strongly stimulated by the existence in humans of genetic conditions characterized by the accumulation of selective undegraded SL molecules. Extensive biochemical and genetic studies on these diseases, named sphingolipid storage disorders (or sphingolipidoses), led to the identification of their underlying defects more than 50 years ago. These disorders result from the disruption of the lysosomal catabolic pathway due to the deficient function of one of the hydrolases, either because this enzyme or its so-called activator protein (sphingolipid activator protein) is mutated, leading to profoundly decreased catalytic activity [2,3]. The catabolic pathway implicating these enzymatic and activator proteins is depicted in Figure 1, and the lipid molecules that accumulate in the corresponding sphingolipid storage disorders are listed in Table 1. As the entry of SLs into the endolysosomal compartment is permanent, although variable, depending on cell type and external conditions, the enzymatic defect translates into substrate accumulation in the lysosomes (see Table 1). Abnormally elevated concentrations of the undegraded SLs can be observed in organs as well as in biological fluids such as blood and urine; the presence of the accumulated SLs in the extracellular milieu may be explained by cell damage or lysosomal exocytosis.

Table 1.
Primary accumulated SLs and lysoSLs in sphingolipid storage diseases. Of note, genetic conditions in which the accumulation of some SLs occurs as a secondary phenomenon are not listed here. The plasma concentrations of lysosphingolipids are indicated in brackets (control values).
The clinical presentation of patients affected with sphingolipid storage disorders is quite diverse, ranging from isolated visceral symptomatology to severe and fatal neuronopathic forms. A factor that determines organ involvement is the tissue distribution of the accumulated SLs. For instance, a neurological disease develops when the metabolism of GM1 and GM2 gangliosides or sulfatides and galactosylceramide, which are key components of neurons and myelin, respectively, are not properly degraded. On the other hand, the defective turnover of glucosylceramide (GlcCer) or sphingomyelin (SM), which are widely distributed, affects cells such as professional phagocytes, i.e., monocytes-macrophages. Of importance for the discussion below, the age of disease onset can vary widely, ranging from the antenatal period up to late adulthood. This variability is explained, at least partially, by the residual activity of the affected enzyme: the lower the activity is, the more severe the lipid storage and the symptomatology are [4].
As already mentioned, the deficient activity of a lysosomal hydrolase results in the accumulation of its primary substrate. However, biochemical studies performed as early as in the mid-seventies have also documented the presence and storage of deacylated SLs, e.g., galactosylsphingosine (GalSph), also called psychosine, and glucosylsphingosine (GlcSph), in organs of patients affected with Krabbe and Gaucher diseases, respectively [5,6]. The discovery of these two lysoSLs was soon followed by the observation that other similarly N-deacylated SLs accumulate in distinct sphingolipidoses (see Table 1). Abnormally high levels of lysoSLs are also found in patients’ biological fluids such as plasma, urine, and cerebrospinal fluid. The metabolic source of lysoSLs has long been debated. Initially, it was postulated that the synthesis of a lysoSL follows the same biosynthetic route as the conventional lipid but uses a sphingoid base rather than ceramide. Recent evidence has shown that instead, GalSph, GlcSph and lysoGb3 are generated by the action of acid ceramidase on their corresponding SL in the lysosomal compartment, i.e., where the parental lipid is stored [7,8]. In fact, the elimination of GalSph production by ablating acid ceramidase in a mouse model of Krabbe suppressed the behavioral and histopathological features of leukodystrophy [9]. Whether other lysoSLs are produced by acid ceramidase still requires further investigation. The fatty acid amide hydrolase (FAAH) enzyme has been reported to partially account for the production of lysosulfatide [10].
Finally, for the purpose of the present paper, one should recall that sphingosine 1-phosphate (S1P) is also a lysoSL. This lysophospholipid is mainly formed by the sphingosine-kinase-mediated phosphorylation of sphingosine and by the autotaxin-mediated breakdown of lysoSM [11]. It is still unknown whether a ceramidase can generate S1P from ceramide 1-phosphate. So far, with the possible exception of Gaucher disease, neither accumulation of S1P nor ceramide 1-phosphate has been reported in sphingolipid storage disorders.
As some sphingolipid storage diseases are associated with the occurrence of malignancies and because the lysolipid S1P is well known to behave as a second messenger, mediating survival and pro-angiogenic pathways and being involved in tumorigenesis, one can ask the question of the potential role of lysoSLs in cancer. The following chapters will discuss the biological properties of lysoSLs related to cancer and their potential contribution to the development of malignancies that are associated with some sphingolipid storage diseases.
2. Cancer Prevalence in Sphingolipid Storage Disorders
Gaucher disease (GD) is the most frequent sphingolipid storage disease, of which the deficiency of lysosomal glucosylceramidase (GCase), encoded by the GBA gene, results in an accumulation of GlcCer and GlcSph (Table 1). Three disease forms are described: type 1 is the most frequent, with hepatosplenomegaly, anemia, thrombocytopenia, bone abnormalities, and lung complications without neurological involvement, the latter being only present in types 2 and 3 [28] (Table 2). Numerous case reports, case series, and cohort studies have described the occurrence of malignancies in Gaucher patients and have suggested that the risk of developing cancer is increased in Gaucher patients with a relative risk evaluated at 1.7 (95% confidence interval (95% CI) 1.3–2.3) [29]. In the French Gaucher Disease Registry (FGDR) (n = 657 patients), we report that 27 patients presented malignancies (4.1%) [30]. Compared to data from the French population (obtained from the International Agency for Research on Cancer (https://gco.iarc.fr/today/home) accessed on 31 March 2021), our observations suggest a marked increase in the prevalence of malignancies at an odds ratio (OR) of 1.8 (95% CI 1.03–2.81) (Table 3). The risk of multiple myeloma seems to be particularly marked, with an OR of 23.8 (95% CI 4.9–70.2) (see Table 2 and Table 3), which is very consistent with the literature [29,31,32,33]. Nevertheless, these results should be interpreted with caution because of limits relative to study design. In addition, an association with monoclonal gammopathy of undetermined significance (MGUS), a pre-malignant condition for multiple myeloma, is also suspected [32]. In the FGDR, MGUS has been found in 59 patients (25%) [34]. Besides the risk of hematological malignancies, the prevalence of digestive cancer and, especially, hepatocellular carcinoma in Gaucher patients also seems to be increased [35]. However, in the FGDR, no hepatocellular carcinoma has been observed. Interestingly, in the FGDR, five Gaucher patients presented two cancers, a finding that has been previously described [31,33,36] (see Table 3).

Table 2.
Overview of malignancies described in patients affected with Gaucher disease, Fabry disease, Niemann–Pick B disease, or metachromatic leukodystrophy.

Table 3.
Cancer prevalence in the French Gaucher Disease Registry and French population.
All these observations would suggest that GD could be a predisposing condition for the development of cancers.
The risk of cancer could also be increased in patients suffering from other sphingolipidoses. Indeed, some case reports [37,38,39,40,41,42,43] and cohort studies [44,45] have also described the development of cancer in Fabry patients. Fabry disease (FD), the second most frequent sphingolipid storage disease, is an X-linked disorder resulting from the deficient activity of lysosomal alpha-galactosidase A, encoded by the GLA gene, leading to an accumulation of Gb3 and lysoGb3 (Table 1). FD is classically characterized by angiokeratoma, cornea verticillata, neuropathy (acroparesthesia), progression toward chronic kidney disease, cerebrovascular accidents, and hypertrophic cardiomyopathy (Table 2). In British (n = 261) [44] and Italian (n = 53) [46] cohorts of Fabry patients, an increased incidence was observed for urological and kidney cancers, as well as melanoma, compared to the general population [44]. An increase in the occurrence of meningioma, a benign tumor, has also been observed (see Table 2) [44,45].
The occurrence of cancer in Niemann–Pick disease types A and B (NPD-A and B) could also be non-negligible. NPD-A and -B are very rare diseases that result from the deficient activity of acid sphingomyelinase (ASM), encoded by the SMPD1 gene, leading to an accumulation of SM and lysoSM (Table 1). Clinical phenotypes range from a very severe phenotype (NPD-A), with neurovisceral involvement and an early death, to a mild phenotype (NPD-B), with hepatosplenomegaly, cytopenia, and lung involvement. Very recently, an increase in the prevalence of cancer has been shown in a French cohort of adults (n = 31) suffering from NPD-A and -B, in which five patients presented with cancer, two of whom had lung cancer, and two patients presented MGUS (Table 2) [47]. In addition, cancer has been reported as the cause of death in 9% of patients with NPD-B [48].
To a lesser extent, metachromatic leukodystrophy (MLD) could be associated with gallbladder carcinoma. MLD is caused by the deficient activity of arylsulfatase A, encoded by the ARSA gene, which results in the accumulation of sulfatide and lysosulfatide (Table 1). Three clinical subtypes are described: the late-infantile (0–2.5 years), juvenile (2.5–16 years), and adult (>16 years) forms [49]. Patients with this disease present a progressive neurological involvement with leukodystrophy at MRI; gallbladder complications such as hemobilia and cholecystitis are also described [50] (Table 2). Interestingly, in a cohort of 34 patients, an increase in the prevalence of gallbladder polyposis, a precancerous condition for gallbladder carcinoma, has been observed [51]. In addition, cases of gallbladder carcinoma with liver metastases have been reported in two patients with an adult form of MLD [51,52] and a case without metastases in one patient with a juvenile form [53]. It should be noted that in these patients, the carcinoma occurred earlier than in the general population (56–63 years).
Taken together, these observations suggest a potential link between the occurrence of cancer and the above four sphingolipid storage diseases. In some cases, a common location was observed between typically affected organs and associated cancer, e.g., cytopenia and blood cancers in GD or chronic kidney disease and kidney cancer in FD (Table 2). It seems that there is no correlation between the plasma concentration of lysoSLs and the risk of developing malignancies. The development of cancer seems to be associated with mild or late-onset forms of sphingolipid storage diseases. For instance, the majority of Gaucher patients having cancer present the classical mild form type 1. Indeed, a very slight augmentation of plasma GlcSph levels is associated with the occurrence of GlcSph-reactive IgGs [62]. Such IgGs have already been described in some GD patients with gammopathy and could be causally involved (see Section 3.5). Moreover, in the studied cohorts of Fabry patients with cancer, there are fewer males than females [44,45]. Females usually have lower lysoGb3 levels, present a milder, late-onset form of the disease, and very rarely develop kidney complications compared to males. No patient who is affected by a severe form of NPD and suffers from cancer has been reported [47,48]. These observations could be explained by life expectancy, which is longer in the milder forms, thus allowing cancer development. Moreover, the above findings were based on retrospective or cross-sectional studies, which limits the scientific evidence level. This would require further randomized studies in order to confirm the association between sphingolipid storage diseases and cancer and, if necessary, to determine risk factors such as splenectomy, treatment, SLs, and lysoSL levels.
Although the underlying mechanisms remain unknown, the accumulation of sphingolipids and their corresponding lysoSLs could be implicated in the increased risk of cancer. In GD, the therapeutic splenectomy may lead to the release of undegraded lipids and could be associated with the occurrence of multiple cancers in the same patient [36]. In the FGDR, three out of five patients with two distinct cancers were splenectomized (data were unavailable for the remaining two). A common treatment for Gaucher and Fabry patients is enzyme replacement therapy (ERT), which is based on the administration of exogenous recombinant enzymes. Considering that these treatments improve clinical symptoms and reduce circulating lysoSL levels, they would be expected to be protective against cancer development, which has already been reported [63]. However, reports in the literature are inconsistent in this regard [64], which may suggest that the build-up of these lipids could result in early irreversible protumor events.
In the following chapter, the potential protumor effects of lysoSLs are discussed. The possible role of their parental lipids (GlcCer, Gb3, and SM) in cancer has already been discussed elsewhere [30,65,66,67].
3. Can Lysosphingolipids Be Related to Cancer Features?
Here, we attempt to review the potential protumor roles of lysoSLs according to the hallmarks of cancer published by Hanahan and Weinberg in 2000 and a recently completed study [68]. LysoSLs could activate several signaling pathways in tumor cells and/or tumor stromal cells, allowing cancer cells to proliferate, survive, and invade other tissues.
3.1. Lysosphingolipids and ‘Sustained Proliferation and/or Resistance to Cell Death’
The first report on the mitogenic properties of a lysoSL described the ability of lysoSMs (i.e., sphingosylphosphocholine or sphingosylphosphorylcholine) to stimulate the DNA synthesis and cell division of several untransformed and transformed cells [69]. Since then, numerous studies have shown that lysoSM controls cell proliferation, either positively or negatively, depending on cell type. However, whereas lysoSM treatment stimulates the proliferation of several normal cells, it would rather have an antiproliferative effect on cancer cells [70,71]. This latter phenomenon is associated with rapid increases in cytosolic free Ca2+ and the phosphorylation of the focal adhesion kinase p125FAK in ovarian cancer cell lines [72]. It is mediated by inhibition of both the PI3K-Akt and the mitogen-activated protein kinase (MAPK) signaling pathways in thyroid FRO cancer cells [73] or the inhibition of the G1/S transition of the cell cycle in numerous human pancreatic cancer cells [74]. Moreover, lysoSM strongly inhibits the proliferation of MDA-MB-435S breast cancer cells by regulating the Hippo-signaling pathway, causing an up-regulation of the tumor suppressive kinase Lats2 via S1P receptor 2 (S1P2) and Akt inhibition [75]. Besides its antiproliferative effects, lysoSM is able to trigger both autophagy and apoptosis in triple-negative breast cancer MDA-MB-231 cells [76]. Autophagy and apoptosis are catabolic pathways interconnected by several molecular nodes of crosstalk. Autophagy acts as a double-edged sword in cancer, preventing cancer development through the degradation of oncogenic molecules or by inducing the survival of tumor cells in hypoxic or low-nutrition environments. Moreover, autophagy plays a pivotal role in some cancer hallmarks, including the epithelial–mesenchymal transition (EMT) process and cancer stem cell promotion. Quite surprisingly, lysoSM-induced autophagy, which is mediated by Akt/p38 MAPK signaling, was found to antagonize apoptosis through the inhibition of JNK signaling [76]. Similar results have been reported in non-small-cell lung cancer A549 and H157 cells, in which lysoSM treatment stimulates autophagy through Akt/mTOR and p53 signaling pathways and inhibits apoptosis at the same concentrations [77]. Moreover, the evasion of apoptosis encourages tumor progression, in part through the emergence of resistant variants with great metastatic potential [78].
Lysoglycosphingolipids (lysoGSLs), in particular, GlcSph and GalSph, have also been reported to affect cell growth. Of note, most studies that have examined the effects of these lipids were conducted on cultured non-cancer cells, using cell types known to be affected in sphingolipid storage disorders. For instance, GlcSph was shown to reduce the cell proliferation of human bone cells (osteoblasts, mesenchymal stem cells, and myeloma plasma cells) and the differentiation of peripheral blood mononuclear cells (PBMCs) into osteoclasts [79,80]. In neuronal cells, GlcSph reduces cell growth, promotes apoptosis, and activates mTORC1, a potent inhibitor of autophagy [81]. This autophagy defect could contribute to cell death, as observed in GD [82]. Likewise, GalSph decreases the cell growth of human and murine oligodendroglial cell lines (MO3.1 and OLP-II) and astrocytes [83,84,85,86]. Several pathogenic signaling pathways [83,84] involving either S1P receptors (S1PRs) [87] or cPLA2 [88] have been described. Finally, lysoGM1a and lysoGM2 can induce the apoptosis of murine neuroblastoma Neuro2a cells [89].
Hence, whereas lysoSLs generally elicit antiproliferative effects on many cell types, including tumor cells in vitro, they can differentially affect autophagy, leading to the inhibition or activation of apoptosis and cell death, depending on the lysoSL implicated.
3.2. Lysosphingolipids and “Activating Invasion and Metastasis”
Metastasis is the most life-threatening event in patients with cancer. During the metastatic cascade, loss of cell–cell adhesion capacity and modifications in cell–matrix interaction allow cancer cells to invade local tissue. These events are based on changes in the expression and function of proteins involved in the control of motility and the secretion of molecules to degrade the extracellular matrix (ECM).
LysoSM favors the migration or invasion of many cancer cells, including pancreatic, breast, and lung cancer cells [71]. LysoSM-induced cell migration is associated with increased elastic properties in PANC-1 pancreatic cancer cells [90] and the perinuclear reorganization of keratin-8 intermediate filaments in PANC-1 pancreatic cancer cells and A549 lung cancer cells [91]. Depending on cell type, lysoSM-induced keratin-8 phosphorylation and reorganization were shown to be mediated by the G protein-coupled orphan receptor GPR12 [92], the small GTPase RhebL1 [91], or transglutaminase-2, a Ca2+-dependent enzyme [93]. Exogenous lysoSM can also induce cell invasion by stimulating the expression and secretion of the ECM-degrading enzyme MMP3 in an ERK-dependent manner in several breast cancer cells [94]. Moreover, lysoSM can induce EMT in lung [95] and breast [96] cancer cells by reducing E-cadherin expression and, inversely, enhancing the expression of N-cadherin and vimentin. LysoSM also triggers TGF-β1 expression/secretion and the Wnt-signaling pathway; all these events mediate cancer cell migration and invasion in vitro as well as metastasis in a mouse model of lung metastasis [95]. Interestingly, lysoSM can stimulate the release of connective tissue growth factor (CTGF) [97], which is known to induce tumor cell EMT and facilitate tumor growth and metastasis by promoting the deposition and orientation of collagen I fibers at the primary tumor stroma [98].
Although the promigratory effects of lysoSM have been well documented, anti-migratory effects have also been reported. LysoSM shares a similar structure to S1P, and several cellular effects of lysoSM can be explained by low-affinity binding to and activation of S1PRs [99]. The dual effect of lysoSM on migration may depend on the expression pattern of S1PR subtypes. For instance, lysoSM and S1P inhibit the migration and invasion of B16 murine melanoma cells via S1P2 [100]. It is tempting to speculate that lysoSM promotes the migration/invasion of cancer cells through binding to S1P1 or S1P3, both of which exert promigratory effects; however, this hypothesis remains to be demonstrated [100]. Of interest is the finding that lysoSM concentration is markedly elevated in ascites samples from ovarian cancer patients compared to patients with non-malignant diseases, suggesting a potential role as an extracellular signaling molecule in tumor progression [101]. It was proposed that lysoSM could exert biological actions not shared with S1P; however, no high-affinity lysoSM-specific membrane receptor has yet been conclusively identified. Indeed, after the characterization of an orphan receptor named ovarian cancer G-protein-coupled receptor 1 (ORG1) and other receptors with sequence homology, such as high-affinity lysoSM receptors, subsequent studies have failed to reproduce important features of the original reports, and those were finally retracted.
Contrary to lysoSM, lysoGSLs would hamper cell migration. Indeed, GlcSph slows human umbilical vein endothelial cells (HUVEC) wound healing closure [102], and lysosulfatide inhibits the migration and adhesion of B35 neuroblastoma cells through calcium release, leading to cell retraction and rounding [103].
3.3. Lysosphingolipids and “Unlocking Phenotypic Plasticity”
Unlocking phenotypic plasticity, which confers to cancer cells the ability to escape from the state of terminal differentiation, is a critical component of tumor aggressiveness in multiple cancer types [68]. This plasticity is related to the disruption of cellular differentiation (e.g., dedifferentiation from mature to progenitor states), blocked differentiation from progenitor cell states, and transdifferentiation into different cell lineages. In melanoma, loss of microphthalmia-associated transcription factor (MITF), the master regulator of melanocyte differentiation, is associated with the reactivation of neural crest progenitor genes and leads to invasive tumors. Interestingly, lysoSM is able to reduce the expression of MITF and its downstream target tyrosinase and, therefore, to induce hypopigmentation in human melanocytes via the activation of ERK [104]. However, whether the lysoSM-induced loss of MITF is associated with the reactivation of neural crest progenitor genes and melanoma progression is unknown. In contrast, there is some evidence that lysoSM stimulates the differentiation of promyelocytic leukemia cells. As a matter of fact, treatment of NB4 cells with lysoSM results in a marked increase in cell differentiation compared to the untreated controls, as demonstrated by the increased expression of the β2 integrin CD11c/CD18. This effect is also mediated by the ERK cascade but is independent of S1P1 because NB4 cells do not express this receptor [105].
So far, there is no report on lysoGSLs and phenotypic plasticity.
3.4. Lysosphingolipids and “Inducing or Accessing Vasculature”
Angiogenesis is a key feature of tumor progression and metastasis as the formation of new blood vessels from pre-existing vessels provides the principal route by which tumor cells enter the circulation. Although the following effects have never been described in a tumor context, lysoSM appears to be a critical regulator of angiogenesis by inducing capillary-like tube formation via vascular endothelial growth factor (VEGF) receptor 2 transactivation and the activation of both PI3K and Akt [106]. LysoSM also induces the chemotactic migration of human and bovine endothelial cells in a manner similar to that exerted by VEGF [107]. The molecular mechanisms of lysoSM-induced angiogenesis involve an increased expression of the urokinase-type plasminogen activator (uPA), which is known to promote pro-angiogenic signaling through the proteolytic degradation of ECM and upon binding to uPAR/CD87 receptors [108]. Moreover, lysoSM dose-dependently increases the activity of ecto-5′-nucleotidase (CD73) in HUVEC [109]. This effect could lead to adenosine production, an immunosuppressive metabolite that also exerts mitogenic effects on vascular cells and may contribute to angiogenesis [110].
So far, there have been no reports on lysoGSLs and angiogenesis.
3.5. Lysosphingolipids and “Tumor Promoting Inflammation/Avoiding Immune Destruction”
Smoldering inflammation favors cancer progression as it contributes to the proliferation and survival of tumor cells, angiogenesis, metastasis, and the subversion of adaptive immunity. LysoSM could exert a pro-inflammatory role, thanks to its capacity to recruit immune cells such as natural-killer-cell-producing cytokines [111] and to trigger the release of lipid mediators and cytokines, including leukotriene B4 [112], interleukin-6 (IL-6) [113,114], and tumor necrosis factor-α (TNF-α) [115] in normal cells. TNF-α production was also reported upon repeated exposure of astrocytes to lysoSM, mimicking the pathological conditions observed in NPD-A [116]. Mechanistically, as reported in cerebral artery vascular smooth muscle cells, lysoSM can stimulate pro-inflammatory transcription factors, nuclear factor-κB (NF-κB), and CCAAT-enhancer-binding protein in a p38MAPK-dependent manner [117], leading to the release of cytokines and monocyte chemoattractant protein-1 (MCP-1) [117]. Similarly, lysoSM also activated NF-κB and AP-1 via p38MAPK and Jak/STAT3 to produce MCP-1 in HUVEC [118].
Interestingly, lysoSM induces IL-8 expression and secretion in ovarian cancer cells [119], probably creating a tumor microenvironment that could be conducive to the recruitment of neutrophil populations. Tumor-associated neutrophils have immunosuppressive functions, stimulate angiogenesis, and favor tumor progression [120]. However, the immunosuppressive properties of lysoSM may be counterbalanced by its ability to reduce IL-1β-stimulated prostaglandin E2 (PGE2) formation [121], PGE2 being an important player in tumor immune evasion. Moreover, the accumulation of lysoSM in peripheral tissues may favor a T helper type 1-mediated immune response through the release of IL-12 and IL18 from dendritic cells [122]. However, the relevance of these in vitro data, obtained with a high concentration (40 µM) of lysoSM, remains questionable in the context of NPD.
Increasing evidence also implicates lysoGb3 as a mediator of inflammation. Indeed, lysoGb3 triggers Notch1 signaling and the subsequent activation of the NF-κB pathway, resulting in the production of pro-inflammatory cytokines in human podocytes [123]. Accordingly, systemic injection of lysoGb3 into mice resulted in the whole kidney up-regulation of Notch ligand Jagged1 and chemokine (MCP1, RANTES) expression, leading to increased numbers of macrophages in glomeruli. The shear stress induced by the lysoGb3-mediated remodeling of the arterial wall may increase the inflammatory potential of endothelial cells [124]. Interestingly, it was also reported that cultured peripheral blood mononuclear cells from Fabry patients exhibit a higher pro-inflammatory cytokine expression profile than that of healthy individuals [125]. Moreover, reduced proportions of blood monocytes, CD8+ T-cells, and dendritic cells have been reported in Fabry patients, together with increased percentages of total lymphocytes and B-cells [126]. Whether these changes are solely due to lysoGb3 remains to be established.
GlcSph is another lysoSL that affects innate and adaptive immune responses. The first evidence of GlcSph is a marked elevation of chitotriosidase, a macrophage activation marker, as well as an increased concentration of pro-inflammatory cytokines such as IL-6 and TNFα in the plasma of Gaucher patients [36,127,128,129,130,131]. In addition, the long-term subcutaneous administration of high doses of GlcSph in C57BL/6JRj mice replicated the visceral inflammatory response observed in patients [132,133,134]. Moreover, the activation of B-cell proliferation could result from the production of IL-6 [127] but also from the activation of type II Natural Killer (NK) T-cells against GlcCer or GlcSph [135]. These results highlight the potential role of GlcSph in B-cell lymphoma development. Although the specific implication of GlcSph was not demonstrated, sporadic B lymphoma was seen in aged mice affected with GD [136].
The monoclonal immunoglobulin (IgG) found in Gaucher patients and in a conditional Gaucher mouse model reacts against GlcSph [137]. The IgG level decreased following pharmacological inhibition of GlcCer synthase, an intervention that reduces the production of both GlcCer and GlcSph. Quite surprisingly, GlcSph-reactive IgGs were also detected in patients suffering from sporadic monoclonal gammopathy [137] and myeloproliferative neoplasms [62]. These results indicate that GlcSph could have an immunogenic role, linking auto-immunity and inflammation [138].
To elucidate the specific role of GlcSph in inflammation (and neuroinflammation in particular), experiments were conducted using a Gaucher zebrafish model where the expression of acid ceramidase, the enzyme responsible for GlcSph production, was ablated. This manipulation caused no reduction in the expression of inflammatory cytokines such as IL-1β and TNFβ in the brain [139], suggesting the minor contribution of GlcSph to the neuroinflammation in this model.
Similar to GlcSph, lysosulfatide has been recognized as a potent ligand for murine type II CD1d-restricted NKT cells [140], indicating a potential involvement in tumor immunity.
In sum, the data reviewed in this section suggest that lysoSM behaves as a pro-tumorigenic metabolite. This effect could be linked to its structure, which is similar to that of S1P, a well-known lysolipid that has potent protumorigenic activities. The effects of lysoSM vary according to cell type and extracellular concentration. They may also depend on the nature of the S1PR that mediates these effects, the potential competition with S1P, or the autotaxin-mediated transformation of lysoSM into S1P. These effects will ultimately depend on other microenvironmental stimuli.
Moreover, a number of the aforementioned results should be taken with caution because most of the in vitro experiments were conducted on different cell types. Indeed, one could conclude that lysoGSLs have anti-tumorigenic properties, but these observations were made on non-cancer cells. Moreover, the choice of concentrations (up to 10 µM) of the tested lysoSLs is often questionable. Physiological levels of these lipids in plasma approximate the nanomolar range; in a pathological context such as sphingolipid storage disorders, their plasma concentrations can rise by one or two orders of magnitude [13,27]. Although very little information on their concentrations in organs is available, it is likely that the concentrations can reach the submicromolar range.
In the first two chapters, a likely association between sphingolipidoses and cancer occurrence has been emphasized. Thus, it is tempting to speculate that the accumulation of these lysoSLs in patients could facilitate tumor formation and/or progression. Faced with a lack of knowledge about lysoGSLs in cancer, we undertook a study to examine the role of one lysoGSL, namely, GlcSph, in cancer.
4. What Is the Role of Lysosphingolipids in Sphingolipid-Storage-Disorder-Associated Cancers? The Example of Glucosylsphingosine in Melanoma
Evidence has accumulated for a dysregulation of sphingolipid metabolism in numerous cancers, including cutaneous melanoma [141]. Moreover, melanoma has been reported in Gaucher patients (see Table 2). In this last part, we investigate the role of the lysoSL GlcSph in melanoma progression.
4.1. Melanoma Growth Is Promoted in a Mouse Model of Gaucher Disease
First, we studied melanoma growth in a well-established, type 1 GD mouse model carrying the homozygous point mutation p.D409V (Gba1D409V/D409V) [142,143]. Murine melanoma cells (B16F10) were injected subcutaneously in these mutant mice and in their control, age-matched heterozygous littermates (Gba1D409V/wt). Tumor growth (Figure 2A) and tumor weight (Figure 2B) were significantly increased in Gaucher mice compared with their control counterparts. As expected, the enzyme activity of GCase in the liver and spleen was significantly decreased in Gaucher mice (Figure 2C). In addition, the concentrations of GlcCer and GlcSph in these two organs were significantly higher in GD mice than in control ones (Figure 2D,E). The quantification of ceramide, SM, dihydroceramide, GM3, and lactosylceramide levels did not show any significant differences between the groups [144]. These results on tumor growth are consistent with those found in a similar GD mouse model D409V/null [30]. Thus, melanoma growth seems to be facilitated in GD mice, which suggests that the Gaucher microenvironment, encompassing the lipids GlcCer and GlcSph, could promote tumor development. This finding is in line with previous observations showing that, similar to Gaucher patients, who are prone to hematological malignancies, a conditional mouse model of GD developed significantly more B-cell lymphomas than control animals [136]. Of note, the early administration of an inhibitor of UDP-GlcCer transferase resulted in a reduction of plasma GlcSph levels and protected against lymphoma and myeloma development [145], possibly suggesting that GlcSph was implicated in the higher susceptibility of Gaucher animals. To test this hypothesis, we investigated the potential role of GlcSph in melanoma progression.
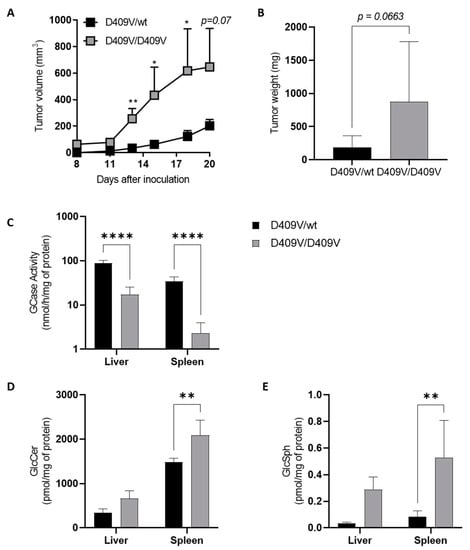
Figure 2.
Melanoma tumor growth is increased in a Gba1D409V/D409V Gaucher mouse model. Murine B16F10 melanoma cells (3 × 105) were injected subcutaneously into Gba1D409V/D409V (D409V/D409V) female mice and heterozygous (D409V/wt) littermates having the same mixed genetic background (19–22 weeks of age). (A) Tumor volumes were measured every 3 days. (B) Tumor weights were measured 25 days after tumor inoculation. Data are expressed as means +/− SEM of at least two independent experiments (n = 7–21 mice). (C) GCase enzyme activity was determined in lysates of liver and spleen isolated from D409V/D409V or heterozygous D409V/wt mice. Assays were performed in duplicate on samples of three to six animals. GlcCer (D) and GlcSph (E) were extracted by the Bligh and Dyer method [146] from the liver and spleen and analyzed by LC-MS (liquid chromatography coupled by mass spectrometry); assays were performed in duplicate on samples taken at day 20 of three to six animals (18–22 weeks of age). Statistical significance was determined by a Mann–Whitney test. *, p < 0.05; **, p < 0.01; ****, p < 0.0001.
4.2. GlcSph Dose-Dependently Decreases Human Melanoma Cell Growth In Vitro
To examine the role of GlcSph, A375 cells, a human metastatic melanoma cell line, were treated with various concentrations of GlcSph (up to 5 µM) or ethanol (vehicle) for 4 days. Cell growth was evaluated using the IncuCyte S3 time-lapse microscopy system, a live cell-imaging incubator, through the determination of cellular confluence. Figure 3A depicts a concentration-dependent reduction in cellular confluence during the first 24 h. These results were also observed in GlcSph-treated WM35 cells, a primary human melanoma cell line (Figure 3B). To further assess the role of GCase inhibition in cell growth, A375 cells were incubated with conduritol B epoxide (CBE), a GCase irreversible and specific inhibitor [147], resulting in a significant decrease in enzyme activity (Figure 3C). However, only a trend of decreased cell growth in CBE-treated cells compared to vehicle-treated cells was observed (Figure 3D). To go further, we analyzed SL levels in cells treated with CBE for 48 h or GlcSph for 24 h. No significant increase in the GlcSph level was observed after CBE treatment, whereas its concentration was very high in GlcSph-treated cells (Figure 3E). These changes in GlcSph concentrations could explain the above difference in cell growth.
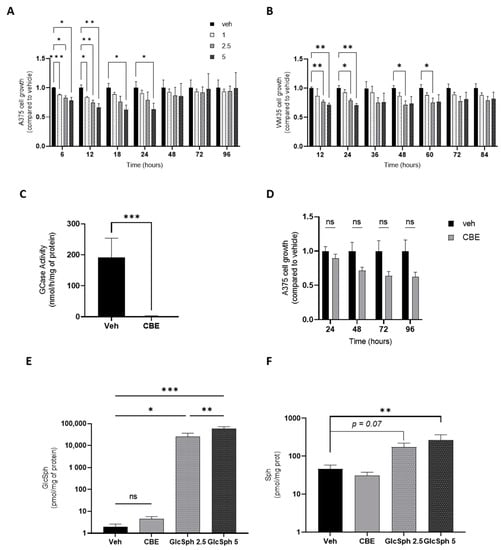
Figure 3.
GlcSph decreases the growth of cultured human melanoma cells in a dose-dependent manner. (A,B) A375 and WM35 human melanoma cells were seeded into a 96-well plate (10,000 cells/well) and, 24 h later, treated either with different concentrations of GlcSph (1, 2.5, or 5 µM) or with ethanol (veh). Cell growth was assessed by measuring the cellular confluence using an IncuCyte S3 time-lapse microscopy system. For each sample, the cellular confluence was measured in duplicate at different incubation times for 4 days. (C) GCase enzyme activity in A375 cells treated with CBE (30 µM) or DMSO (veh) for 48 h. (D) A375 cells were seeded into a 96-well plate and, after 24 h, treated either with CBE (30 µM) or DMSO (veh). Cell growth was evaluated as described in (A,B). GlcSph (E) and Sph (F) were extracted as described in [13], and concentrations were determined by liquid chromatography-tandem mass spectrometry in CBE- or GlcSph-treated cells compared to controls. For all experiments, data are expressed as means +/− SEM of three independent experiments. Statistical significance was determined by a two-way mixed ANOVA with Geisser–Greenhouse correction (A,B,D) or a Mann–Whitney test (C,E,F). *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, not significant compared to vehicle-treated cells.
Thus, exogenously added GlcSph and, possibly, the intracellular GlcSph produced upon the pharmacological inhibition of GCase decrease the proliferation of human melanoma cells in a concentration-dependent manner. A cytotoxic effect of GlcSph has already been reported in other cell types in a micromolar concentration range of GlcSph [80,148]. The concentrations we used are consistent with the GlcSph plasma concentration found in Gaucher patients [13,149]. The intraepidermal GlcSph concentrations in Gaucher patients are unknown, but in Gaucher mouse models (D409V; C* and N409S-/-), they are elevated [150]. This suggests that melanocytes could be surrounded by a local accumulation of GlcSph. Moreover, a significant increase in sphingosine (Sph) (Figure 3F) and a slight increase (p = 0.05) in sphingosine 1-phosphate (S1P) levels were observed only in GlcSph-treated cells, while the quantification of ceramide, sphinganine, GlcCer, SM, dihydroceramide, and GM3 levels did not show any differences between groups [144]. These results are consistent with the reported elevation of sphingosine and S1P levels in the plasma of Gaucher patients [149]. Pro-apoptotic effects of sphingosine have already been described in different cell types but not in melanoma cells [151]. Although S1P is considered an anti-apoptotic metabolite [152], it may lead to cell death by apoptosis, as shown in prostate cancer cells, possibly via its dephosphorylation to sphingosine [153]. Sphingosine comes from the N-deacylation of ceramide by ceramidases and can be phosphorylated by the sphingosine kinase to produce S1P (Figure 1). Here, the observed increase of sphingosine and S1P in GlcSph-treated cells could originate from GlcSph catabolism. The enzyme involved in this catabolism could be the lysosomal GCase or GBA2, a glucosylceramidase located in the ER. Indeed, the double gba1:gba2 knockout in zebrafish larvae led to a higher level of GlcSph than in single gba1 knockout larvae [154]. Lastly, GlcSph has also been reported to be able to alter the lipid composition of plasma membranes, as shown with GalSph, which shares a similar chemical structure and build-up to the neurodegenerative Krabbe disease. Indeed, enrichment of GalSph in the inner layer of the plasma membrane promotes neuronal death [155].
4.3. GlcSph Promotes Necrosis and Produces Multinucleated Melanoma Cells
To further characterize the reduction of cell growth upon GlcSph administration, cellular death was explored. A375 cells, treated or not with GlcSph for 24 h, were stained with Annexin V-FITC and 7-AAD and analyzed by flow cytometry. The percentage of necrotic cells was significantly higher in GlcSph-treated cells than in control cells, while no difference was observed in the proportion of apoptotic cells (Figure 4A). These findings indicate that GlcSph decreases melanoma cell growth in vitro by promoting necrosis. Whereas the underlying mechanisms remain unknown, it is interesting that the development of neurodegeneration in the neuronopathic forms of GD (i.e., types 2 and 3) would result from necroptosis, a programmed form of necrosis, which could be induced by GlcSph [156,157]. Moreover, the involvement of Sph and S1P has been observed in nutrient-deprivation-induced necroptosis in murine embryonic fibroblasts [158]. Interestingly, necroptosis has also been reported as a mechanism participating in tumor growth in pancreatic cancer through the release of immunosuppressive factors [159]. Although necroptosis of GlcSph was not documented in our model, it could explain how melanoma growth was exacerbated in GD mice (Figure 2), whereas the in vitro cell growth was reduced under GlcSph (Figure 3).
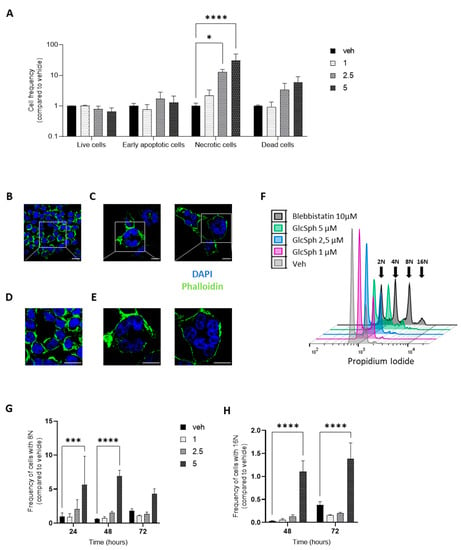
Figure 4.
GlcSph induces necrosis and produces multinucleated cells in A375 human melanoma cells. (A) A375 cells were treated for 24 h with either different concentrations of GlcSph (1, 2.5, and 5 µM) or with ethanol (veh), stained with Annexin V-FITC and 7-AAD, and analyzed by flow cytometry; 20,000 events were recorded and sorted as follows: live cells (Annexin V-negative/7-AAD-negative), dead cells (Annexin V-positive/7-AAD-positive), early apoptosis (Annexin V-positive/7-AAD-negative), and necrosis (Annexin V-negative/7-AAD-positive). Histograms represent the cell frequency of GlcSph-treated cells compared to vehicle-treated cells. (B–E) A375 cells were treated for 48 h with ethanol (B,D) or GlcSph 5 µM (C and E), fixed and stained with phalloidin (for F-actin, green), and nuclei were counterstained with DAPI (for DNA, blue). Then, they were imaged by confocal microscopy (Zeiss) at 63× (B,C), with an additional upper zoom (×2) of the selected regions (white square) (D,E). Scale bar = 20 µm. (F–H) A375 cells were incubated either with different concentrations of GlcSph (1, 2.5, or 5 µM) or with ethanol (veh) for 24, 48, and 72 h. Then, cells were stained with propidium iodide (PI) and analyzed by flow cytometry. Figure (F) is a representative plot of cell cycle analysis of GlcSph- and vehicle-treated A375 cells for 48 h. To identify the peaks corresponding to abnormal ploidies, A375 cells were treated with blebbistatin (10 µM), a myosin II inhibitor (see arrows). The proportion of cells with 8N (G) and 16N (H) in GlcSph-treated cells compared to controls was quantified. For experiments in A, G, and H, data are expressed as means +/− SEM of three independent experiments. Statistical significance was determined by a two-way mixed ANOVA. *, p < 0.05; ***, p < 0.001; ****, p < 0.0001 compared to vehicle-treated cells.
Concurrently, morphological analysis of A375 cells after exposure to GlcSph (5 µM) for 48 h showed larger and multinucleated cells, as illustrated in Figure 4B–E. To quantify the presence of multinucleated cells, the cell cycle was analyzed and DNA content measured. As depicted in Figure 4F–H, the percentage of cells with 8N and 16N DNA content, relative to total cell count, was augmented after GlcSph (5 µM) treatment. The percentage of polyploidy reached a maximum of 7% of cells with 8N after 48 h incubation (Figure 4G), demonstrating that GlcSph induced the formation of multinucleated cells in a human melanoma cell line. Of note, giant multinucleated cells have been described in histopathologic analyses of melanoma [160,161], but their presence does not seem to be associated with poor prognosis [162]. Usually, aneuploidy confers pro-tumoral properties to cancer cells [163]. Because of their genetic instability, multinucleated cells are usually programmed for cell death. However, the genetic rearrangement could confer to cancer cells selective advantages that favor tumor growth, migration, and resistance to treatment [163]. Our observations might suggest that the multinucleated cells represent a fraction of cells resistant to GlcSph-induced death.
The appearance of multinucleated cells elicited by GlcSph has already been observed in non-melanoma cell lines, including the human myelomonocytic U937 cell line [102,164] and with GalCer. GalSph was proposed to inhibit cytokinesis by impacting actin reorganization [164] or by disrupting SM clusters at the plasma membrane and suppressing the formation of phosphatidylinositol 4,5-bisphosphate at the cleavage furrow [152]. Whether GlcSph and GalSph induce polyploidy through the same molecular mechanisms remains to be determined.
5. Conclusions
This review aims to provide an overview of lysoSLs and their potential role in cancer. Although they represent a very small fraction of total lipids, they are considered bioactive lipids. Their biological effects likely depend on their lysoSL nature (with a distinction between lysoSMs and lysoGSLs) and on cell type. Current evidence indicates that these lipids come from the deacylation of their parental SL by aCDase. Their mechanisms of action are not fully understood. LysoSM can act on G-protein-coupled receptors (S1PRs) [92,99]. On the other hand, GalSph may alter the lipid composition of plasma membranes and, as a consequence, affect signaling pathways that depend on lipid rafts [165] and/or tyrosine kinase receptors [155].
As discussed, there are very little data on the effects of lysoGSLs in the context of cancer. However, these lysoSLs, nowadays considered useful biomarkers of sphingolipid storage diseases, could be involved in the occurrence of malignancies in patients suffering from these inherited metabolic disorders. LysoSLs may act directly on cancer cells to promote their growth and/or resistance to anticancer regimes or indirectly on the cellular tumor microenvironment by triggering protumorigenic (e.g., pro-inflammatory and immunosuppressive) responses. For example, GlcSph could be a good candidate in the genesis of lymphoma and myeloma in patients with GD. Regarding cutaneous melanoma, we have shown that the treatment of melanoma cells results in cell necrosis and the build-up of multinucleated melanoma cells. Such modifications in cell cycle and death programs could play a significant role in the progression of skin melanoma. Indeed, as previously mentioned, necroptosis could induce immunosuppression, and the multinucleated cells may represent a way to resist cell death, thereby leading to tumor growth.
Another hypothesis linking sphingolipids, GD, and cancer implicates α-synuclein. As a matter of fact, it is now established that carrying a GBA pathogenic variant gene represents the greatest risk factor for developing Parkinson’s disease (PD) [166]. PD is a neurodegenerative disease in which α-synuclein aggregates are part of the pathophysiological process [167,168]. The accumulation of GlcCer and GlcSph that accompanies GCase deficiency could be implicated in this protein aggregation [169,170]. Interestingly, patients affected with PD have a high risk of developing cutaneous melanoma [171,172]. Whereas α-synuclein aggregation induces neuronal cell death, some observations account for its capacity to promote some cancers, such as melanoma. For example, α-synuclein has been reported to favor cell survival both in in vitro and in vivo melanoma models [173,174], raising the possibility of a link between GlcCer/GlcSph, α-synuclein aggregation, and melanoma.
Taken together, current knowledge points to the potential role of lysoSLs in the occurrence of cancer. Further investigation of these metabolites in relation to cancer should be supported. This certainly includes systematic studies on their biological effects and their modes of action. Also needed are accurate measurements by mass spectrometry of their concentrations in tumor samples and plasma at the time of diagnosis and during the follow-up of patients with cancer. LysoSLs are usually quantified in the plasma of patients suspected of suffering from sphingolipidoses, but plasma may not be the appropriate milieu to reveal their possible role in cancer development. Indeed, malignancies seem to occur in patients affected with mild forms of sphingolipid storage diseases, i.e., under conditions where the plasma levels of lysoSLs are lower than in patients with infantile severe forms, and a long-term cumulative effect operates. Finally, future work should determine whether the incidence of cancer can be reduced in patients who receive long-term enzyme replacement (ERT) or substrate reduction (SRT) therapy, as these treatments lead to a considerably reduced production of lysoSLs.
Author Contributions
Conceptualization, P.D., T.L., N.A.-A. and F.S.; methodology, P.D., T.L., N.A.-A. and F.S.; software, not applicable; validation, P.D., T.L., N.A.-A. and F.S.; formal analysis, P.D. and N.A.-A.; investigation, P.D., L.A., N.T., L.C., M.P., D.C. and J.S.; resources, T.L. and N.A.-A.; data curation, not applicable; writing—original draft preparation, P.D., T.L., N.A.-A. and F.S.; writing—review and editing, P.D., L.A., N.T, L.C., M.P., D.C., J.S., T.L., N.A.-A. and F.S.; visualization, P.D., T.L., N.A.-A. and F.S.; supervision, N.A.-A. and F.S.; project administration, N.A.-A. and F.S.; funding acquisition, T.L. and N.A.-A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by INSERM and Université Paul Sabatier (U1037SE20BA).
Institutional Review Board Statement
Animal experiments were conducted in accordance with national and international policies, and our protocol was approved by the Regional Ethics Committee of Midi-Pyrénées.
Acknowledgments
The authors wish to thank Gregory A. Grabowski (Division of Human Genetics, Cincinnati, OH) for providing the Gaucher mouse models, Justine Bertrand-Michel (Lipidomics facility, INSERM, Toulouse, France), and the technical team of the Bron Biochemistry Laboratory for sphingolipid analyses and the technical facilities of the CRCT, and James McDonagh for proofreading.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Fahy, E.; Subramaniam, S.; Brown, H.A.; Glass, C.K.; Merrill, A.H., Jr.; Murphy, R.C.; Raetz, C.R.; Russell, D.W.; Seyama, Y.; Shaw, W.; et al. A comprehensive classification system for lipids. J. Lipid Res. 2005, 46, 839–861. [Google Scholar] [CrossRef] [PubMed]
- Kolter, T.; Sandhoff, K. Sphingolipid metabolism diseases. Biochim. Biophys. Acta 2006, 1758, 2057–2079. [Google Scholar] [CrossRef]
- Breiden, B.; Sandhoff, K. Lysosomal Glycosphingolipid Storage Diseases. Annu. Rev. Biochem. 2019, 88, 461–485. [Google Scholar] [CrossRef]
- Leinekugel, P.; Michel, S.; Conzelmann, E.; Sandhoff, K. Quantitative correlation between the residual activity of beta-hexosaminidase A and arylsulfatase A and the severity of the resulting lysosomal storage disease. Hum. Genet. 1992, 88, 513–523. [Google Scholar] [CrossRef]
- Vanier, M.; Svennerholm, L. Chemical pathology of Krabbe disease: The occurrence of psychosine and other neutral sphingoglycolipids. Adv. Exp. Med. Biol. 1976, 68, 115–126. [Google Scholar] [PubMed]
- Raghavan, S.S.; Mumford, R.A.; Kanfer, J.N. Isolation and characterization of glucosylsphingosine from Gaucher’s spleen. J. Lipid Res. 1974, 15, 484–490. [Google Scholar] [CrossRef]
- Yamaguchi, Y.; Sasagasako, N.; Goto, I.; Kobayashi, T. The synthetic pathway for glucosylsphingosine in cultured fibroblasts. J. Biochem. 1994, 116, 704–710. [Google Scholar] [CrossRef]
- Ferraz, M.J.; Marques, A.R.; Appelman, M.D.; Verhoek, M.; Strijland, A.; Mirzaian, M.; Scheij, S.; Ouairy, C.M.; Lahav, D.; Wisse, P.; et al. Lysosomal glycosphingolipid catabolism by acid ceramidase: Formation of glycosphingoid bases during deficiency of glycosidases. FEBS Lett. 2016, 590, 716–725. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, Y.; Benitez, B.A.; Nagree, M.S.; Dearborn, J.T.; Jiang, X.; Guzman, M.A.; Woloszynek, J.C.; Giaramita, A.; Yip, B.K.; et al. Genetic ablation of acid ceramidase in Krabbe disease confirms the psychosine hypothesis and identifies a new therapeutic target. Proc. Natl. Acad. Sci. USA 2019, 116, 20097–20103. [Google Scholar] [CrossRef] [PubMed]
- Yaghootfam, C.; Gehrig, B.; Sylvester, M.; Gieselmann, V.; Matzner, U. Deletion of fatty acid amide hydrolase reduces lyso-sulfatide levels but exacerbates metachromatic leukodystrophy in mice. J. Biol. Chem. 2021, 297, 101064. [Google Scholar] [CrossRef]
- Clair, T.; Aoki, J.; Koh, E.; Bandle, R.W.; Nam, S.W.; Ptaszynska, M.M.; Mills, G.B.; Schiffmann, E.; Liotta, L.A.; Stracke, M.L. Autotaxin hydrolyzes sphingosylphosphorylcholine to produce the regulator of migration, sphingosine-1-phosphate. Cancer Res. 2003, 63, 5446–5453. [Google Scholar]
- Kobayashi, T.; Goto, I.; Okada, S.; Orii, T.; Ohno, K.; Nakano, T. Accumulation of lysosphingolipids in tissues from patients with GM1 and GM2 gangliosidoses. J. Neurochem. 1992, 59, 1452–1458. [Google Scholar] [CrossRef]
- Pettazzoni, M.; Froissart, R.; Pagan, C.; Vanier, M.T.; Ruet, S.; Latour, P.; Guffon, N.; Fouilhoux, A.; Germain, D.P.; Levade, T.; et al. LC-MS/MS multiplex analysis of lysosphingolipids in plasma and amniotic fluid: A novel tool for the screening of sphingolipidoses and Niemann-Pick type C disease. PLoS ONE 2017, 12, e0181700. [Google Scholar] [CrossRef]
- Neuenhofer, S.; Conzelmann, E.; Schwarzmann, G.; Egge, H.; Sandhoff, K. Occurrence of lysoganglioside lyso-GM2 (II3-Neu5Ac-gangliotriaosylsphingosine) in GM2 gangliosidosis brain. Biol. Chem. Hoppe Seyler 1986, 367, 241–244. [Google Scholar] [CrossRef]
- Kodama, T.; Togawa, T.; Tsukimura, T.; Kawashima, I.; Matsuoka, K.; Kitakaze, K.; Tsuji, D.; Itoh, K.; Ishida, Y.; Suzuki, M.; et al. Lyso-GM2 ganglioside: A possible biomarker of Tay-Sachs disease and Sandhoff disease. PLoS ONE 2011, 6, e29074. [Google Scholar] [CrossRef]
- Nilsson, O.; Mansson, J.-E.; Hakansson, G.; Svennerholm, L. The occurrence of psychosine and other glycolipids in spleen and liver from the three major types of Gaucher’s disease. Biochim. Biophys. Acta Lipids Lipid Metab. 1982, 712, 453–463. [Google Scholar] [CrossRef]
- Kang, L.; Zhan, X.; Ye, J.; Han, L.; Qiu, W.; Gu, X.; Zhang, H. A rare form of Gaucher disease resulting from saposin C deficiency. Blood Cells Mol. Dis. 2018, 68, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Aerts, J.M.; Groener, J.E.; Kuiper, S.; Donker-Koopman, W.E.; Strijland, A.; Ottenhoff, R.; van Roomen, C.; Mirzaian, M.; Wijburg, F.A.; Linthorst, G.E.; et al. Elevated globotriaosylsphingosine is a hallmark of Fabry disease. Proc. Natl. Acad. Sci. USA 2008, 105, 2812–2817. [Google Scholar] [CrossRef]
- Toda, K.; Kobayashi, T.; Goto, I.; Kurokawa, T.; Ogomori, K. Accumulation of lysosulfatide (sulfogalactosylsphingosine) in tissues of a boy with metachromatic leukodystrophy. Biochem. Biophys. Res. Commun. 1989, 159, 605–611. [Google Scholar] [CrossRef]
- Rosengren, B.; Fredman, P.; Månsson, J.E.; Svennerholm, L. Lysosulfatide (galactosylsphingosine-3-O-sulfate) from metachromatic leukodystrophy and normal human brain. J. Neurochem. 1989, 52, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Saville, J.T.; Smith, N.J.; Fletcher, J.M.; Fuller, M. Quantification of plasma sulfatides by mass spectrometry: Utility for metachromatic leukodystrophy. Anal. Chim. Acta 2017, 955, 79–85. [Google Scholar] [CrossRef]
- Deconinck, N.; Messaaoui, A.; Ziereisen, F.; Kadhim, H.; Sznajer, Y.; Pelc, K.; Nassogne, M.C.; Vanier, M.T.; Dan, B. Metachromatic leukodystrophy without arylsulfatase A deficiency: A new case of saposin-B deficiency. Eur. J. Paediatr. Neurol. 2008, 12, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; De Jesus, O. Krabbe Disease. In StatPearls; StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.: Treasure Island, FL, USA, 2022. [Google Scholar]
- Zhao, S.; Zhan, X.; Wang, Y.; Ye, J.; Han, L.; Qiu, W.; Gao, X.; Gu, X.; Zhang, H. Large-scale study of clinical and biochemical characteristics of Chinese patients diagnosed with Krabbe disease. Clin. Genet. 2018, 93, 248–254. [Google Scholar] [CrossRef]
- Calderwood, L.; Wenger, D.A.; Matern, D.; Dahmoush, H.; Watiker, V.; Lee, C. Rare Saposin A deficiency: Novel variant and psychosine analysis. Mol. Genet. Metab. 2020, 129, 161–164. [Google Scholar] [CrossRef] [PubMed]
- Motta, M.; Tatti, M.; Furlan, F.; Celato, A.; Di Fruscio, G.; Polo, G.; Manara, R.; Nigro, V.; Tartaglia, M.; Burlina, A.; et al. Clinical, biochemical and molecular characterization of prosaposin deficiency. Clin. Genet. 2016, 90, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Kuchar, L.; Sikora, J.; Gulinello, M.E.; Poupetova, H.; Lugowska, A.; Malinova, V.; Jahnova, H.; Asfaw, B.; Ledvinova, J. Quantitation of plasmatic lysosphingomyelin and lysosphingomyelin-509 for differential screening of Niemann-Pick A/B and C diseases. Anal. Biochem. 2017, 525, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Stirnemann, J.; Belmatoug, N.; Camou, F.; Serratrice, C.; Froissart, R.; Caillaud, C.; Levade, T.; Astudillo, L.; Serratrice, J.; Brassier, A.; et al. A Review of Gaucher Disease Pathophysiology, Clinical Presentation and Treatments. Int. J. Mol. Sci. 2017, 18, 441. [Google Scholar] [CrossRef] [PubMed]
- Arends, M.; van Dussen, L.; Biegstraaten, M.; Hollak, C.E.M. Malignancies and monoclonal gammopathy in Gaucher disease; a systematic review of the literature. Br. J. Haematol. 2013, 161, 832–842. [Google Scholar] [CrossRef] [PubMed]
- Dubot, P.; Astudillo, L.; Therville, N.; Sabourdy, F.; Stirnemann, J.; Levade, T.; Andrieu-Abadie, N. Are Glucosylceramide-Related Sphingolipids Involved in the Increased Risk for Cancer in Gaucher Disease Patients? Review and Hypotheses. Cancers 2020, 12, 475. [Google Scholar] [CrossRef]
- Taddei, T.H.; Kacena, K.A.; Yang, M.; Yang, R.; Malhotra, A.; Boxer, M.; Aleck, K.A.; Rennert, G.; Pastores, G.M.; Mistry, P.K. The underrecognized progressive nature of N370S Gaucher disease and assessment of cancer risk in 403 patients. Am. J. Hematol. 2009, 84, 208–214. [Google Scholar] [CrossRef]
- de Fost, M.; Vom Dahl, S.; Weverling, G.J.; Brill, N.; Brett, S.; Häussinger, D.; Hollak, C.E.M. Increased incidence of cancer in adult Gaucher disease in Western Europe. Blood Cells Mol. Dis. 2006, 36, 53–58. [Google Scholar] [CrossRef]
- Landgren, O.; Turesson, I.; Gridley, G.; Caporaso, N.E. Risk of malignant disease among 1525 adult male US Veterans with Gaucher disease. Arch. Intern. Med. 2007, 167, 1189–1194. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Y.; Stirnemann, J.; Lautredoux, F.; Cador, B.; Bengherbia, M.; Yousfi, K.; Hamroun, D.; Astudillo, L.; Billette de Villemeur, T.; Brassier, A.; et al. Immunoglobulin Abnormalities in Gaucher Disease: An Analysis of 278 Patients Included in the French Gaucher Disease Registry. Int. J. Mol. Sci. 2020, 21, 1247. [Google Scholar] [CrossRef] [PubMed]
- Regenboog, M.; van Dussen, L.; Verheij, J.; Weinreb, N.J.; Santosa, D.; Vom Dahl, S.; Häussinger, D.; Müller, M.N.; Canbay, A.; Rigoldi, M.; et al. Hepatocellular carcinoma in Gaucher disease: An international case series. J. Inherit. Metab. Dis. 2018, 41, 819–827. [Google Scholar] [CrossRef]
- Lo, S.M.; Stein, P.; Mullaly, S.; Bar, M.; Jain, D.; Pastores, G.M.; Mistry, P.K. Expanding spectrum of the association between Type 1 Gaucher disease and cancers: A series of patients with up to 3 sequential cancers of multiple types--correlation with genotype and phenotype. Am. J. Hematol. 2010, 85, 340–345. [Google Scholar] [CrossRef]
- Pagni, F.; Pieruzzi, F.; Zannella, S.; Di Giacomo, A.; Bovo, G.; Ferrario, F.; Torti, G.; Rivera, R.; Assi, E.; Viglione, F.; et al. Possible pathogenetic relationship between Fabry disease and renal cell carcinoma. Am. J. Nephrol. 2012, 36, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Tisi, M.C.; Zampetti, A.; Feliciani, C.; Fianchi, L.; Valentini, C.G.; Hohaus, S.; Larocca, L.M.; Leone, G.; Voso, M.T. Small lymphocytic lymphoma in a patient with Fabry disease. Leuk Lymphoma 2013, 54, 184–185. [Google Scholar] [CrossRef]
- Blanco, J.; Herrero, J.; Arias, L.F.; Garcia-Miralles, N.; Gamez, C.; Barrientos, A. Renal variant of Anderson-Fabry disease and bilateral renal cell carcinoma. Pathol. Res. Pract. 2005, 200, 857–860. [Google Scholar] [CrossRef]
- Cassiman, D.; Claes, K.; Lerut, E.; Oyen, R.; Joniau, S.; Van Damme, B.; Jaeken, J. Bilateral renal cell carcinoma development in long-term Fabry disease. J. Inherit. Metab. Dis. 2007, 30, 830–831. [Google Scholar] [CrossRef]
- Thurberg, B.L.; Germain, D.P.; Perretta, F.; Jurca-Simina, I.E.; Politei, J.M. Fabry disease: Four case reports of meningioma and a review of the literature on other malignancies. Mol. Genet. Metab. Rep. 2017, 11, 75–80. [Google Scholar] [CrossRef]
- Kusama, M.; Kimura, K.; Koyanagi, Y.; Tsuchida, A.; Yoshimatsu, A.; Ebinara, Y. A case report of atypical Fabry’s disease with colon cancer. Nihon Geka Gakkai Zasshi 1993, 94, 755–757. [Google Scholar]
- Cybulla, M.; Kleber, M.; Walter, K.N.; Kroeber, S.M.; Neumann, H.P.; Engelhardt, M. Is Fabry disease associated with leukaemia? Br. J. Haematol. 2006, 135, 264–265. [Google Scholar] [CrossRef]
- Bird, S.; Hadjimichael, E.; Mehta, A.; Ramaswami, U.; Hughes, D. Fabry disease and incidence of cancer. Orphanet J. Rare Dis. 2017, 12, 150. [Google Scholar] [CrossRef]
- Rossi, F.; Auricchio, S.; Binaggia, A.; L’imperio, V.; Pagni, F.; Pieruzzi, F. Tumour incidence in Fabry disease: A cross-sectional study. J. Onco-nephrol. 2019, 3, 80–87. [Google Scholar] [CrossRef]
- Alexandrov, L.B.; Nik-Zainal, S.; Wedge, D.C.; Aparicio, S.A.; Behjati, S.; Biankin, A.V.; Bignell, G.R.; Bolli, N.; Borg, A.; Børresen-Dale, A.L.; et al. Signatures of mutational processes in human cancer. Nature 2013, 500, 415–421. [Google Scholar] [CrossRef]
- Mauhin, W.; Levade, T.; Vanier, M.T.; Froissart, R.; Lidove, O. Prevalence of Cancer in Acid Sphingomyelinase Deficiency. J. Clin. Med. 2021, 10, 5029. [Google Scholar] [CrossRef]
- Cassiman, D.; Packman, S.; Bembi, B.; Turkia, H.B.; Al-Sayed, M.; Schiff, M.; Imrie, J.; Mabe, P.; Takahashi, T.; Mengel, K.E.; et al. Cause of death in patients with chronic visceral and chronic neurovisceral acid sphingomyelinase deficiency (Niemann-Pick disease type B and B variant): Literature review and report of new cases. Mol. Genet. Metab. 2016, 118, 206–213. [Google Scholar] [CrossRef]
- van Rappard, D.F.; Boelens, J.J.; Wolf, N.I. Metachromatic leukodystrophy: Disease spectrum and approaches for treatment. Best Pract. Res. Clin. Endocrinol. Metab. 2015, 29, 261–273. [Google Scholar] [CrossRef]
- Agarwal, A.; Shipman, P.J. Gallbladder polyposis in metachromatic leukodystrophy. Pediatr. Radiol. 2013, 43, 631–633. [Google Scholar] [CrossRef]
- van Rappard, D.F.; Bugiani, M.; Boelens, J.J.; van der Steeg, A.F.; Daams, F.; de Meij, T.G.; van Doorn, M.M.; van Hasselt, P.M.; Gouma, D.J.; Verbeke, J.I.; et al. Gallbladder and the risk of polyps and carcinoma in metachromatic leukodystrophy. Neurology 2016, 87, 103–111. [Google Scholar] [CrossRef]
- Simanovsky, N.; Ackerman, Z.; Kiderman, A.; Fields, S. Unusual gallbladder findings in two brothers with metachromatic leukodystrophy. Pediatr. Radiol. 1998, 28, 706–708. [Google Scholar] [CrossRef]
- Koshu, K.; Ikeda, T.; Tamura, D.; Muramatsu, K.; Osaka, H.; Ono, S.; Adachi, K.; Nanba, E.; Nakajima, T.; Yamagata, T. Gallbladder cancer with ascites in a child with metachromatic leukodystrophy. Brain Dev. 2021, 43, 140–143. [Google Scholar] [CrossRef]
- Stirnemann, J.; Vigan, M.; Hamroun, D.; Heraoui, D.; Rossi-Semerano, L.; Berger, M.G.; Rose, C.; Camou, F.; de Roux-Serratrice, C.; Grosbois, B.; et al. The French Gaucher’s disease registry: Clinical characteristics, complications and treatment of 562 patients. Orphanet J. Rare Dis. 2012, 7, 77. [Google Scholar] [CrossRef]
- Jurecka, A.; Gregorek, H.; Kleinotiene, G.; Czartoryska, B.; Tylki-Szymanska, A. Gaucher disease and dysgammaglobulinemia: a report of 61 patients, including 18 with GD type III. Blood Cells Mol. Dis. 2011, 46, 85–87. [Google Scholar] [CrossRef]
- Lee, R.E. The pathology of Gaucher disease. Prog. Clin. Biol. Res. 1982, 95, 177–217. [Google Scholar]
- Zimran, A.; Liphshitz, I.; Barchana, M.; Abrahamov, A.; Elstein, D. Incidence of malignancies among patients with type I Gaucher disease from a single referral clinic. Blood Cells Mol. Dis. 2005, 34, 197–200. [Google Scholar] [CrossRef]
- Leone, J.P.; Dudek, A.Z. Enzyme replacement therapy for Gaucher’s disease in patient treated for non-small cell lung cancer. Anticancer Res. 2008, 28, 3937–3939. [Google Scholar]
- Shuai, W.; Wagner, C.E.; Sukswai, N.; Medeiros, L.J.; Bueso-Ramos, C.; Oo, T.H. Gaucher disease type 1 first recognized in an elderly patient with thrombocytopenia and lung adenocarcinoma. Clin. Case Rep. 2019, 7, 1804–1805. [Google Scholar] [CrossRef]
- Germain, D.P. Fabry disease. Orphanet J Rare Dis 2010, 5, 30. [Google Scholar] [CrossRef]
- Portier, E.; Talbot, A.; Nguyen, Y.; Royer, B.; Pettazzoni, M.; Ben Salah, I.; Trichet, C.; Vercellino, L.; Arnulf, B.; Belmatoug, N. Multiple myeloma occurring in a case of Niemann-Pick disease Type B: A pathophysiological link? Br. J. Haematol. 2022, 197, e53–e55. [Google Scholar] [CrossRef]
- Allain-Maillet, S.; Bosseboeuf, A.; Mennesson, N.; Bostoën, M.; Dufeu, L.; Choi, E.H.; Cleyrat, C.; Mansier, O.; Lippert, E.; Le Bris, Y.; et al. Anti-Glucosylsphingosine Autoimmunity, JAK2V617F-Dependent Interleukin-1β and JAK2V617F-Independent Cytokines in Myeloproliferative Neoplasms. Cancers 2020, 12, 2446. [Google Scholar] [CrossRef] [PubMed]
- Harel, R.; Gavish, I.; Aviv, A.; Greenman Maravi, N.; Trougouboff, P.; Zimran, A.; Revel-Vilk, S. Enzyme replacement therapy leading to improvement in myeloma indices in a patient with concomitant Gaucher disease. Intern. Med. J. 2022, 52, 872–875. [Google Scholar] [CrossRef]
- Jaffe, D.H.; Flaks-Manov, N.; Benis, A.; Gabay, H.; DiBonaventura, M.; Rosenbaum, H.; Joseph, A.; Bachrach, A.; Leventer-Roberts, M. Population-based cohort of 500 patients with Gaucher disease in Israel. BMJ Open 2019, 9, e024251. [Google Scholar] [CrossRef] [PubMed]
- Tallima, H.; Azzazy, H.M.E.; El Ridi, R. Cell surface sphingomyelin: Key role in cancer initiation, progression, and immune evasion. Lipids Health Dis 2021, 20, 150. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Suzuki, T. Role of sulfatide in normal and pathological cells and tissues. J. Lipid Res. 2012, 53, 1437–1450. [Google Scholar] [CrossRef]
- Reza, S.; Ugorski, M.; Suchański, J. Glucosylceramide and galactosylceramide, small glycosphingolipids with significant impact on health and disease. Glycobiology 2021, 31, 1416–1434. [Google Scholar] [CrossRef]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef]
- Desai, N.N.; Spiegel, S. Sphingosylphosphorylcholine is a remarkably potent mitogen for a variety of cell lines. Biochem. Biophys. Res. Commun. 1991, 181, 361–366. [Google Scholar] [CrossRef]
- Nixon, G.F.; Mathieson, F.A.; Hunter, I. The multi-functional role of sphingosylphosphorylcholine. Prog. Lipid Res. 2008, 47, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Park, M.K.; Lee, C.H. Role of Sphingosylphosphorylcholine in Tumor and Tumor Microenvironment. Cancers 2019, 11, 1696. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Fang, X.J.; Casey, G.; Mills, G.B. Lysophospholipids activate ovarian and breast cancer cells. Biochem. J. 1995, 309 Pt 3, 933–940. [Google Scholar] [CrossRef]
- Afrasiabi, E.; Blom, T.; Balthasar, S.; Törnquist, K. Antiproliferative effect of sphingosylphosphorylcholine in thyroid FRO cancer cells mediated by cell cycle arrest in the G2/M phase. Mol. Cell Endocrinol. 2007, 274, 43–52. [Google Scholar] [CrossRef]
- Yamada, T.; Okajima, F.; Ohwada, S.; Kondo, Y. Growth inhibition of human pancreatic cancer cells by sphingosylphosphorylcholine and influence of culture conditions. Cell Mol. Life Sci. 1997, 53, 435–441. [Google Scholar] [CrossRef]
- Kemppainen, K.; Wentus, N.; Lassila, T.; Laiho, A.; Törnquist, K. Sphingosylphosphorylcholine regulates the Hippo signaling pathway in a dual manner. Cell Signal. 2016, 28, 1894–1903. [Google Scholar] [CrossRef]
- Ge, D.; Gao, J.; Han, L.; Li, Y.; Liu, H.H.; Yang, W.C.; Chang, F.; Liu, J.; Yu, M.; Zhao, J. Novel effects of sphingosylphosphorylcholine on the apoptosis of breast cancer via autophagy/AKT/p38 and JNK signaling. J. Cell. Physiol. 2019, 234, 11451–11462. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Li, W.; Liu, P.; Gao, J.; Miao, J.; Zhao, J. Inhibition of autophagy promoted sphingosylphosphorylcholine induced cell death in non-small cell lung cancer cells. Biochem. Biophys. Res. Commun. 2014, 453, 502–507. [Google Scholar] [CrossRef]
- Su, Z.; Yang, Z.; Xu, Y.; Chen, Y.; Yu, Q. Apoptosis, autophagy, necroptosis, and cancer metastasis. Mol. Cancer 2015, 14, 48. [Google Scholar] [CrossRef]
- Mistry, P.K.; Liu, J.; Yang, M.; Nottoli, T.; McGrath, J.; Jain, D.; Zhang, K.; Keutzer, J.; Chuang, W.-L.; Mehal, W.Z.; et al. Glucocerebrosidase gene-deficient mouse recapitulates Gaucher disease displaying cellular and molecular dysregulation beyond the macrophage. Proc. Natl. Acad. Sci. USA 2010, 107, 19473–19478. [Google Scholar] [CrossRef]
- Reed, M.C.; Schiffer, C.; Heales, S.; Mehta, A.B.; Hughes, D.A. Impact of sphingolipids on osteoblast and osteoclast activity in Gaucher disease. Mol. Genet. Metab. 2018, 124, 278–286. [Google Scholar] [CrossRef]
- Srikanth, M.P.; Jones, J.W.; Kane, M.; Awad, O.; Park, T.S.; Zambidis, E.T.; Feldman, R.A. Elevated glucosylsphingosine in Gaucher disease induced pluripotent stem cell neurons deregulates lysosomal compartment through mammalian target of rapamycin complex 1. Stem Cells Transl. Med. 2021, 10, 1081–1094. [Google Scholar] [CrossRef]
- Kinghorn, K.J.; Grönke, S.; Castillo-Quan, J.I.; Woodling, N.S.; Li, L.; Sirka, E.; Gegg, M.; Mills, K.; Hardy, J.; Bjedov, I.; et al. A Drosophila Model of Neuronopathic Gaucher Disease Demonstrates Lysosomal-Autophagic Defects and Altered mTOR Signalling and Is Functionally Rescued by Rapamycin. J. Neurosci. 2016, 36, 11654–11670. [Google Scholar] [CrossRef] [PubMed]
- Haq, E.; Giri, S.; Singh, I.; Singh, A.K. Molecular mechanism of psychosine-induced cell death in human oligodendrocyte cell line. J. Neurochem. 2003, 86, 1428–1440. [Google Scholar] [CrossRef]
- Giri, S.; Khan, M.; Rattan, R.; Singh, I.; Singh, A.K. Krabbe disease: Psychosine-mediated activation of phospholipase A2 in oligodendrocyte cell death. J. Lipid Res. 2006, 47, 1478–1492. [Google Scholar] [CrossRef]
- Zaka, M.; Wenger, D.A. Psychosine-induced apoptosis in a mouse oligodendrocyte progenitor cell line is mediated by caspase activation. Neurosci. Lett. 2004, 358, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Zaka, M.; Rafi, M.A.; Rao, H.Z.; Luzi, P.; Wenger, D.A. Insulin-like growth factor-1 provides protection against psychosine-induced apoptosis in cultured mouse oligodendrocyte progenitor cells using primarily the PI3K/Akt pathway. Mol. Cell Neurosci. 2005, 30, 398–407. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, C.; Dev, K.K. Galactosylsphingosine (psychosine)-induced demyelination is attenuated by sphingosine 1-phosphate signalling. J. Cell Sci. 2015, 128, 3878–3887. [Google Scholar] [CrossRef]
- Misslin, C.; Velasco-Estevez, M.; Albert, M.; O’Sullivan, S.A.; Dev, K.K. Phospholipase A2 is involved in galactosylsphingosine-induced astrocyte toxicity, neuronal damage and demyelination. PLoS ONE 2017, 12, e0187217. [Google Scholar] [CrossRef] [PubMed]
- Sueyoshi, N.; Maehara, T.; Ito, M. Apoptosis of Neuro2a cells induced by lysosphingolipids with naturally occurring stereochemical configurations. J. Lipid Res. 2001, 42, 1197–1202. [Google Scholar] [CrossRef]
- Beil, M.; Micoulet, A.; von Wichert, G.; Paschke, S.; Walther, P.; Omary, M.B.; Van Veldhoven, P.P.; Gern, U.; Wolff-Hieber, E.; Eggermann, J.; et al. Sphingosylphosphorylcholine regulates keratin network architecture and visco-elastic properties of human cancer cells. Nat. Cell Biol. 2003, 5, 803–811. [Google Scholar] [CrossRef]
- Kim, H.J.; Byun, H.J.; Park, M.K.; Kim, E.J.; Kang, G.J.; Lee, C.H. Novel involvement of RhebL1 in sphingosylphosphorylcholine-induced keratin phosphorylation and reorganization: Binding to and activation of AKT1. Oncotarget 2017, 8, 20851–20864. [Google Scholar] [CrossRef][Green Version]
- Park, M.K.; Park, S.; Kim, H.J.; Kim, E.J.; Kim, S.Y.; Kang, G.J.; Byun, H.J.; Kim, S.H.; Lee, H.; Lee, C.H. Novel effects of FTY720 on perinuclear reorganization of keratin network induced by sphingosylphosphorylcholine: Involvement of protein phosphatase 2A and G-protein-coupled receptor-12. Eur. J. Pharmacol. 2016, 775, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Park, M.K.; Lee, H.J.; Shin, J.; Noh, M.; Kim, S.Y.; Lee, C.H. Novel participation of transglutaminase-2 through c-Jun N-terminal kinase activation in sphingosylphosphorylcholine-induced keratin reorganization of PANC-1 cells. Biochim. Biophys. Acta 2011, 1811, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Kang, G.J.; Kim, E.J.; Park, M.K.; Byun, H.J.; Nam, S.; Lee, H.; Lee, C.H. Novel effects of sphingosylphosphorylcholine on invasion of breast cancer: Involvement of matrix metalloproteinase-3 secretion leading to WNT activation. Biochim. Biophys. Acta 2016, 1862, 1533–1543. [Google Scholar] [CrossRef]
- Yu, L.; Kim, H.J.; Park, M.K.; Byun, H.J.; Kim, E.J.; Kim, B.; Nguyen, M.T.; Kim, J.H.; Kang, G.J.; Lee, H.; et al. Ethacrynic acid, a loop diuretic, suppresses epithelial-mesenchymal transition of A549 lung cancer cells via blocking of NDP-induced WNT signaling. Biochem. Pharmacol. 2021, 183, 114339. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Kim, H.J.; Park, M.K.; Lee, C.H. Sphingosylphosphorylcholine Induces Thrombospondin-1 Secretion in MCF10A Cells via ERK2. Biomol. Ther. 2017, 25, 625–633. [Google Scholar] [CrossRef]
- Zhu, M.J.; Kim, C.D.; Kwon, Y.B.; Kye, K.C.; Chen, Y.Y.; Lee, W.H.; Lee, S.; Lim, J.S.; Seo, Y.J.; Suhr, K.B.; et al. Induction of connective tissue growth factor expression by sphingosylphosphorylcholine in cultured human skin fibroblasts. Exp. Dermatol. 2005, 14, 509–514. [Google Scholar] [CrossRef]
- Zhu, X.; Zhong, J.; Zhao, Z.; Sheng, J.; Wang, J.; Liu, J.; Cui, K.; Chang, J.; Zhao, H.; Wong, S. Epithelial derived CTGF promotes breast tumor progression via inducing EMT and collagen I fibers deposition. Oncotarget 2015, 6, 25320–25338. [Google Scholar] [CrossRef]
- Meyer zu Heringdorf, D.; Jakobs, K.H. Lysophospholipid receptors: Signalling, pharmacology and regulation by lysophospholipid metabolism. Biochim. Biophys. Acta 2007, 1768, 923–940. [Google Scholar] [CrossRef]
- Arikawa, K.; Takuwa, N.; Yamaguchi, H.; Sugimoto, N.; Kitayama, J.; Nagawa, H.; Takehara, K.; Takuwa, Y. Ligand-dependent inhibition of B16 melanoma cell migration and invasion via endogenous S1P2 G protein-coupled receptor. Requirement of inhibition of cellular RAC activity. J. Biol. Chem. 2003, 278, 32841–32851. [Google Scholar] [CrossRef]
- Xiao, Y.J.; Schwartz, B.; Washington, M.; Kennedy, A.; Webster, K.; Belinson, J.; Xu, Y. Electrospray ionization mass spectrometry analysis of lysophospholipids in human ascitic fluids: Comparison of the lysophospholipid contents in malignant vs nonmalignant ascitic fluids. Anal. Biochem. 2001, 290, 302–313. [Google Scholar] [CrossRef]
- Smith, N.J.C.; Fuller, M.; Saville, J.T.; Cox, T.M. Reduced cerebral vascularization in experimental neuronopathic Gaucher disease. J. Pathol. 2018, 244, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Hans, M.; Pusch, A.; Dai, L.; Racké, K.; Swandulla, D.; Gieselmann, V.; Kappler, J. Lysosulfatide regulates the motility of a neural precursor cell line via calcium-mediated process collapse. Neurochem. Res. 2009, 34, 508–517. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Park, S.H.; Kwon, S.B.; Park, E.S.; Huh, C.H.; Youn, S.W.; Park, K.C. Sphingosylphosphorylcholine-induced ERK activation inhibits melanin synthesis in human melanocytes. Pigment Cell Res. 2006, 19, 146–153. [Google Scholar] [CrossRef]
- Kleger, A.; Busch, T.; Liebau, S.; Prelle, K.; Paschke, S.; Beil, M.; Rolletschek, A.; Wobus, A.; Wolf, E.; Adler, G.; et al. The bioactive lipid sphingosylphosphorylcholine induces differentiation of mouse embryonic stem cells and human promyelocytic leukaemia cells. Cell Signal. 2007, 19, 367–377. [Google Scholar] [CrossRef]
- Kim, K.S.; Ren, J.; Jiang, Y.; Ebrahem, Q.; Tipps, R.; Cristina, K.; Xiao, Y.J.; Qiao, J.; Taylor, K.L.; Lum, H.; et al. GPR4 plays a critical role in endothelial cell function and mediates the effects of sphingosylphosphorylcholine. FASEB J. 2005, 19, 819–821. [Google Scholar] [CrossRef]
- Boguslawski, G.; Lyons, D.; Harvey, K.A.; Kovala, A.T.; English, D. Sphingosylphosphorylcholine induces endothelial cell migration and morphogenesis. Biochem. Biophys. Res. Commun. 2000, 272, 603–609. [Google Scholar] [CrossRef]
- Piao, Y.J.; Lee, C.H.; Zhu, M.J.; Kye, K.C.; Kim, J.M.; Seo, Y.J.; Suhr, K.B.; Park, J.K.; Kim, C.D.; Lee, J.H. Involvement of urokinase-type plasminogen activator in sphingosylphosphorylcholine-induced angiogenesis. Exp. Dermatol. 2005, 14, 356–362. [Google Scholar] [CrossRef]
- Pexa, A.; Deussen, A. Modulation of ecto-5’-nucleotidase by phospholipids in human umbilical vein endothelial cells (HUVEC). Naunyn Schmiedebergs Arch. Pharmacol. 2005, 372, 131–138. [Google Scholar] [CrossRef]
- Auchampach, J.A. Adenosine receptors and angiogenesis. Circ. Res. 2007, 101, 1075–1077. [Google Scholar] [CrossRef]
- Jin, Y.; Damaj, B.B.; Maghazachi, A.A. Human resting CD16-, CD16+ and IL-2-, IL-12-, IL-15- or IFN-alpha-activated natural killer cells differentially respond to sphingosylphosphorylcholine, lysophosphatidylcholine and platelet-activating factor. Eur J. Immunol. 2005, 35, 2699–2708. [Google Scholar] [CrossRef]
- Andoh, T.; Saito, A.; Kuraishi, Y. Leukotriene B(4) mediates sphingosylphosphorylcholine-induced itch-associated responses in mouse skin. J. Investig. Dermatol. 2009, 129, 2854–2860. [Google Scholar] [CrossRef]
- Suhr, K.B.; Tsuboi, R.; Seo, E.Y.; Piao, Y.J.; Lee, J.H.; Park, J.K.; Ogawa, H. Sphingosylphosphorylcholine stimulates cellular fibronectin expression through upregulation of IL-6 in cultured human dermal fibroblasts. Arch. Dermatol. Res. 2003, 294, 433–437. [Google Scholar] [CrossRef]
- Kwon, Y.B.; Lee, Y.S.; Sohn, K.C.; Piao, Y.J.; Back, S.J.; Seo, Y.J.; Suhr, K.B.; Park, J.K.; Kim, C.D.; Lee, J.H. Sphingosylphosphorylcholine-induced interleukin-6 production is mediated by protein kinase C and p42/44 extracellular signal-regulated kinase in human dermal fibroblasts. J. Dermatol. Sci. 2007, 46, 91–99. [Google Scholar] [CrossRef]
- Imokawa, G.; Takagi, Y.; Higuchi, K.; Kondo, H.; Yada, Y. Sphingosylphosphorylcholine is a potent inducer of intercellular adhesion molecule-1 expression in human keratinocytes. J. Investig. Dermatol. 1999, 112, 91–96. [Google Scholar] [CrossRef]
- Chiulli, N.; Codazzi, F.; Di Cesare, A.; Gravaghi, C.; Zacchetti, D.; Grohovaz, F. Sphingosylphosphocholine effects on cultured astrocytes reveal mechanisms potentially involved in neurotoxicity in Niemann-Pick type A disease. Eur. J. Neurosci. 2007, 26, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Wirrig, C.; Hunter, I.; Mathieson, F.A.; Nixon, G.F. Sphingosylphosphorylcholine is a proinflammatory mediator in cerebral arteries. J. Cereb. Blood Flow Metab. 2011, 31, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Lee, S.Y.; Kim, S.D.; Shim, J.W.; Kim, H.J.; Jung, Y.S.; Kwon, J.Y.; Baek, S.H.; Chung, J.; Bae, Y.S. Sphingosylphosphorylcholine stimulates CCL2 production from human umbilical vein endothelial cells. J. Immunol. 2011, 186, 4347–4353. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, B.M.; Hong, G.; Morrison, B.H.; Wu, W.; Baudhuin, L.M.; Xiao, Y.J.; Mok, S.C.; Xu, Y. Lysophospholipids increase interleukin-8 expression in ovarian cancer cells. Gynecol. Oncol. 2001, 81, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Bui, T.M.; Yalom, L.K.; Sumagin, R. Tumor-associated neutrophils: Orchestrating cancer pathobiology and therapeutic resistance. Expert Opin. Ther. Targets 2021, 25, 573–583. [Google Scholar] [CrossRef]
- Xin, C.; Ren, S.; Eberhardt, W.; Pfeilschifter, J.; Huwiler, A. Sphingosylphosphorylcholine acts in an anti-inflammatory manner in renal mesangial cells by reducing interleukin-1beta-induced prostaglandin E2 formation. J. Lipid Res. 2007, 48, 1985–1996. [Google Scholar] [CrossRef] [PubMed]
- Ceballos, A.; Sabatté, J.; Nahmod, K.; Martínez, D.; Salamone, G.; Vermeulen, M.; Maggini, J.; Salomón, H.; Geffner, J. Sphingosylphosphorylcholine activates dendritic cells, stimulating the production of interleukin-12. Immunology 2007, 121, 328–336. [Google Scholar] [CrossRef]
- Sanchez-Niño, M.D.; Carpio, D.; Sanz, A.B.; Ruiz-Ortega, M.; Mezzano, S.; Ortiz, A. Lyso-Gb3 activates Notch1 in human podocytes. Hum. Mol. Genet. 2015, 24, 5720–5732. [Google Scholar] [CrossRef]
- Rombach, S.M.; Twickler, T.B.; Aerts, J.M.; Linthorst, G.E.; Wijburg, F.A.; Hollak, C.E. Vasculopathy in patients with Fabry disease: Current controversies and research directions. Mol. Genet. Metab. 2010, 99, 99–108. [Google Scholar] [CrossRef]
- De Francesco, P.N.; Mucci, J.M.; Ceci, R.; Fossati, C.A.; Rozenfeld, P.A. Fabry disease peripheral blood immune cells release inflammatory cytokines: Role of globotriaosylceramide. Mol. Genet. Metab. 2013, 109, 93–99. [Google Scholar] [CrossRef]
- Rozenfeld, P.; Agriello, E.; De Francesco, N.; Martinez, P.; Fossati, C. Leukocyte perturbation associated with Fabry disease. J. Inherit. Metab. Dis. 2009, 32 Suppl 1, S67–S77. [Google Scholar] [CrossRef]
- Allen, M.J.; Myer, B.J.; Khokher, A.M.; Rushton, N.; Cox, T.M. Pro-inflammatory cytokines and the pathogenesis of Gaucher’s disease: Increased release of interleukin-6 and interleukin-10. QJM 1997, 90, 19–25. [Google Scholar] [CrossRef]
- Boven, L.A.; van Meurs, M.; Boot, R.G.; Mehta, A.; Boon, L.; Aerts, J.M.; Laman, J.D. Gaucher cells demonstrate a distinct macrophage phenotype and resemble alternatively activated macrophages. Am. J. Clin. Pathol. 2004, 122, 359–369. [Google Scholar] [CrossRef]
- Jmoudiak, M.; Futerman, A.H. Gaucher disease: Pathological mechanisms and modern management. Br. J. Haematol. 2005, 129, 178–188. [Google Scholar] [CrossRef]
- Michelakakis, H.; Spanou, C.; Kondyli, A.; Dimitriou, E.; Van Weely, S.; Hollak, C.E.; Van Oers, M.H.; Aerts, J.M. Plasma tumor necrosis factor-a (TNF-a) levels in Gaucher disease. Biochim. Biophys. Acta 1996, 1317, 219–222. [Google Scholar] [CrossRef]
- Hollak, C.E.; van Weely, S.; van Oers, M.H.; Aerts, J.M. Marked elevation of plasma chitotriosidase activity. A novel hallmark of Gaucher disease. J. Clin. Investig. 1994, 93, 1288–1292. [Google Scholar] [CrossRef]
- Lukas, J.; Cozma, C.; Yang, F.; Kramp, G.; Meyer, A.; Neßlauer, A.-M.; Eichler, S.; Böttcher, T.; Witt, M.; Bräuer, A.; et al. Glucosylsphingosine Causes Hematological and Visceral Changes in Mice—Evidence for a Pathophysiological Role in Gaucher Disease. Int. J. Mol. Sci. 2017, 18, 2192. [Google Scholar] [CrossRef]
- Carubbi, F.; Cappellini, M.D.; Fargion, S.; Fracanzani, A.L.; Nascimbeni, F. Liver involvement in Gaucher disease: A practical review for the hepatologist and the gastroenterologist. Dig Liver Dis. 2020, 52, 368–373. [Google Scholar] [CrossRef]
- James, S.P.; Stromeyer, F.W.; Chang, C.; Barranger, J.A. LIver abnormalities in patients with Gaucher’s disease. Gastroenterology 1981, 80, 126–133. [Google Scholar] [CrossRef]
- Nair, S.; Boddupalli, C.S.; Verma, R.; Liu, J.; Yang, R.; Pastores, G.M.; Mistry, P.K.; Dhodapkar, M.V. Type II NKT-TFH cells against Gaucher lipids regulate B-cell immunity and inflammation. Blood 2015, 125, 1256–1271. [Google Scholar] [CrossRef] [PubMed]
- Pavlova, E.V.; Wang, S.Z.; Archer, J.; Dekker, N.; Aerts, J.M.F.G.; Karlsson, S.; Cox, T.M. B cell lymphoma and myeloma in murine Gaucher’s disease. J. Pathol. 2013, 231, 88–97. [Google Scholar] [CrossRef]
- Nair, S.; Branagan, A.R.; Liu, J.; Boddupalli, C.S.; Mistry, P.K.; Dhodapkar, M.V. Clonal Immunoglobulin against Lysolipids in the Origin of Myeloma. N. Engl. J. Med. 2016, 374, 555–561. [Google Scholar] [CrossRef] [PubMed]
- van Eijk, M.; Ferraz, M.J.; Boot, R.G.; Aerts, J. Lyso-glycosphingolipids: Presence and consequences. Essays Biochem. 2020, 64, 565–578. [Google Scholar] [PubMed]
- Lelieveld, L.T.; Gerhardt, S.; Maas, S.; Zwiers, K.C.; de Wit, C.; Beijk, E.H.; Ferraz, M.J.; Artola, M.; Meijer, A.H.; Tudorache, C.; et al. Consequences of excessive glucosylsphingosine in glucocerebrosidase-deficient zebrafish. J. Lipid Res. 2022, 63, 100199. [Google Scholar] [CrossRef]
- Blomqvist, M.; Rhost, S.; Teneberg, S.; Löfbom, L.; Osterbye, T.; Brigl, M.; Månsson, J.E.; Cardell, S.L. Multiple tissue-specific isoforms of sulfatide activate CD1d-restricted type II NKT cells. Eur. J. Immunol. 2009, 39, 1726–1735. [Google Scholar] [CrossRef]
- Carrié, L.; Virazels, M.; Dufau, C.; Montfort, A.; Levade, T.; Ségui, B.; Andrieu-Abadie, N. New Insights into the Role of Sphingolipid Metabolism in Melanoma. Cells 2020, 9, 1967. [Google Scholar] [CrossRef]
- Xu, Y.-H.; Quinn, B.; Witte, D.; Grabowski, G.A. Viable mouse models of acid beta-glucosidase deficiency: The defect in Gaucher disease. Am. J. Pathol. 2003, 163, 2093–2101. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, W.; Xu, Y.-H.; Quinn, B.; Dasgupta, N.; Liou, B.; Setchell, K.D.R.; Grabowski, G.A. Substrate compositional variation with tissue/region and Gba1 mutations in mouse models--implications for Gaucher disease. PLoS ONE 2013, 8, e57560. [Google Scholar] [CrossRef]
- Dubot, P.; Pettazzoni, M.; Carrié, L.; Cheillan, D.; Levade, T.; Andrieu-Abadie, N.; Sabourdy, F. Université de Toulouse, Inserm, CNRS, Université Toulouse III-Paul Sabatier, Centre de Recherches en Cancérologie de Toulouse, Equipe Labellisée Fondation ARC, 2 Avenue Hubert Curien, CS 53717, CEDEX 1, 31037 Toulouse, Laboratoire de Biochimie Métabolique, CHU Toulouse, 31059 Toulouse, France. 2022; (manuscript in preparation). [Google Scholar]
- Pavlova, E.V.; Archer, J.; Wang, S.; Dekker, N.; Aerts, J.M.; Karlsson, S.; Cox, T.M. Inhibition of UDP-glucosylceramide synthase in mice prevents Gaucher disease-associated B-cell malignancy. J. Pathol. 2015, 235, 113–124. [Google Scholar] [CrossRef]
- Bligh, E.G.; Dyer, W.J. A rapid method of total lipid extraction and purification. Can. J. Biochem. Physiol. 1959, 37, 911–917. [Google Scholar] [CrossRef]
- Kuo, C.L.; Kallemeijn, W.W.; Lelieveld, L.T.; Mirzaian, M.; Zoutendijk, I.; Vardi, A.; Futerman, A.H.; Meijer, A.H.; Spaink, H.P.; Overkleeft, H.S.; et al. In vivo inactivation of glycosidases by conduritol B epoxide and cyclophellitol as revealed by activity-based protein profiling. FEBS J. 2019, 286, 584–600. [Google Scholar] [CrossRef]
- Schueler, U.H.; Kolter, T.; Kaneski, C.R.; Blusztajn, J.K.; Herkenham, M.; Sandhoff, K.; Brady, R.O. Toxicity of glucosylsphingosine (glucopsychosine) to cultured neuronal cells: a model system for assessing neuronal damage in Gaucher disease type 2 and 3. Neurobiol. Dis. 2003, 14, 595–601. [Google Scholar] [CrossRef]
- Chipeaux, C.; de Person, M.; Burguet, N.; Billette de Villemeur, T.; Rose, C.; Belmatoug, N.; Héron, S.; Le Van Kim, C.; Franco, M.; Moussa, F. Optimization of ultra-high pressure liquid chromatography - tandem mass spectrometry determination in plasma and red blood cells of four sphingolipids and their evaluation as biomarker candidates of Gaucher’s disease. J. Chromatogr. A 2017, 1525, 116–125. [Google Scholar] [CrossRef]
- Liou, B.; Zhang, W.; Fannin, V.; Quinn, B.; Ran, H.; Xu, K.; Setchell, K.D.R.; Witte, D.; Grabowski, G.A.; Sun, Y. Combination of acid β-glucosidase mutation and Saposin C deficiency in mice reveals Gba1 mutation dependent and tissue-specific disease phenotype. Sci. Rep. 2019, 9, 5571. [Google Scholar] [CrossRef]
- Cuvillier, O. Sphingosine in apoptosis signaling. Biochim. Biophys. Acta 2002, 1585, 153–162. [Google Scholar] [CrossRef]
- Maceyka, M.; Payne, S.G.; Milstien, S.; Spiegel, S. Sphingosine kinase, sphingosine-1-phosphate, and apoptosis. Biochim. Biophys. Acta 2002, 1585, 193–201. [Google Scholar] [CrossRef]
- Mulders, A.C.; Nau, S.; Li, Y.; Michel, M.C. Effects of sphingosine-1-phosphate and sphingosylphosphorylcholine on intracellular Ca2+ and cell death in prostate cancer cell lines. Auton Autacoid Pharmacol. 2007, 27, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Lelieveld, L.T.; Mirzaian, M.; Kuo, C.L.; Artola, M.; Ferraz, M.J.; Peter, R.E.A.; Akiyama, H.; Greimel, P.; van den Berg, R.; Overkleeft, H.S.; et al. Role of β-glucosidase 2 in aberrant glycosphingolipid metabolism: Model of glucocerebrosidase deficiency in zebrafish. J. Lipid Res. 2019, 60, 1851–1867. [Google Scholar] [CrossRef] [PubMed]
- Sural-Fehr, T.; Singh, H.; Cantuti-Catelvetri, L.; Zhu, H.; Marshall, M.S.; Rebiai, R.; Jastrzebski, M.J.; Givogri, M.I.; Rasenick, M.M.; Bongarzone, E.R. Inhibition of the IGF-1–PI3K–Akt–mTORC2 pathway in lipid rafts increases neuronal vulnerability in a genetic lysosomal glycosphingolipidosis. Dis. Model. Mech. 2019, 12, dmm036590. [Google Scholar] [CrossRef]
- Vitner, E.B.; Salomon, R.; Farfel-Becker, T.; Meshcheriakova, A.; Ali, M.; Klein, A.D.; Platt, F.M.; Cox, T.M.; Futerman, A.H. RIPK3 as a potential therapeutic target for Gaucher’s disease. Nat. Med. 2014, 20, 204–208. [Google Scholar] [CrossRef]
- Yañez, M.J.; Campos, F.; Marín, T.; Klein, A.D.; Futerman, A.H.; Alvarez, A.R.; Zanlungo, S. c-Abl activates RIPK3 signaling in Gaucher disease. Biochim. Biophys. Acta Mol. Basis Dis. 2021, 1867, 166089. [Google Scholar] [CrossRef]
- Sundaram, K.; Mather, A.R.; Marimuthu, S.; Shah, P.P.; Snider, A.J.; Obeid, L.M.; Hannun, Y.A.; Beverly, L.J.; Siskind, L.J. Loss of neutral ceramidase protects cells from nutrient- and energy -deprivation-induced cell death. Biochem. J. 2016, 473, 743–755. [Google Scholar] [CrossRef]
- Seifert, L.; Werba, G.; Tiwari, S.; Giao Ly, N.N.; Alothman, S.; Alqunaibit, D.; Avanzi, A.; Barilla, R.; Daley, D.; Greco, S.H.; et al. The necrosome promotes pancreatic oncogenesis via CXCL1 and Mincle-induced immune suppression. Nature 2016, 532, 245–249. [Google Scholar] [CrossRef]
- Boyd, A.S.; Wu, H.; Shyr, Y. Monster cells in malignant melanoma. Am. J. Dermatopathol. 2005, 27, 208–210. [Google Scholar] [CrossRef]
- Pouryazdanparast, P.; Newman, M.; Mafee, M.; Guitart, J.; Gerami, P. Malignant melanoma with monster cells showing massive cyclin D1 amplification. Am. J. Dermatopathol. 2009, 31, 402–403. [Google Scholar] [CrossRef]
- Srisuttiyakorn, C.; Bulloch, K.; Rodic, N.; Bosenberg, M.; Ariyan, S.; Narayan, D.; Gould Rothberg, B.E.; Galan, A. Intratumoral multinucleated giant cells are not a prognostic pathologic feature in cutaneous melanoma. J. Cutan Pathol. 2016, 43, 821–829. [Google Scholar] [CrossRef]
- Ben-David, U.; Amon, A. Context is everything: Aneuploidy in cancer. Nat. Rev. Genet. 2020, 21, 44–62. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, T.; Nakamura, S.; Momoi, M.; Yamaji, T.; Takematsu, H.; Yano, H.; Sabe, H.; Yamamoto, A.; Kawasaki, T.; Kozutsumi, Y. Inhibition of cytokinesis by a lipid metabolite, psychosine. J. Cell Biol. 2000, 149, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Okahara, K.; Naito-Matsui, Y.; Abe, M.; Go, S.; Inokuchi, J.; Okazaki, T.; Kobayashi, T.; Kozutsumi, Y.; Oka, S.; et al. Psychosine-triggered endomitosis is modulated by membrane sphingolipids through regulation of phosphoinositide 4,5-bisphosphate production at the cleavage furrow. Mol. Biol. Cell 2016, 27, 2037–2050. [Google Scholar] [CrossRef] [PubMed]
- Kalia, L.V.; Lang, A.E. Parkinson’s disease. Lancet 2015, 386, 896–912. [Google Scholar] [CrossRef]
- Butler, B.; Sambo, D.; Khoshbouei, H. Alpha-synuclein modulates dopamine neurotransmission. J. Chem. Neuroanat 2017, 83-84, 41–49. [Google Scholar] [CrossRef]
- Burre, J.; Sharma, M.; Sudhof, T.C. Cell Biology and Pathophysiology of alpha-Synuclein. Cold Spring Harb Perspect. Med. 2018, 8, 024091. [Google Scholar] [CrossRef]
- Mazzulli, J.R.; Xu, Y.-H.; Sun, Y.; Knight, A.L.; McLean, P.J.; Caldwell, G.A.; Sidransky, E.; Grabowski, G.A.; Krainc, D. Gaucher disease glucocerebrosidase and α-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell 2011, 146, 37–52. [Google Scholar] [CrossRef]
- Glajch, K.E.; Moors, T.E.; Chen, Y.; Bechade, P.A.; Nam, A.Y.; Rajsombath, M.M.; McCaffery, T.D.; Dettmer, U.; Weihofen, A.; Hirst, W.D.; et al. Wild-type GBA1 increases the α-synuclein tetramer-monomer ratio, reduces lipid-rich aggregates, and attenuates motor and cognitive deficits in mice. Proc. Natl. Acad. Sci. USA 2021, 118, e2103425118. [Google Scholar] [CrossRef]
- Ejma, M.; Madetko, N.; Brzecka, A.; Guranski, K.; Alster, P.; Misiuk-Hojło, M.; Somasundaram, S.G.; Kirkland, C.E.; Aliev, G. The Links between Parkinson’s Disease and Cancer. Biomedicines 2020, 8, 416. [Google Scholar] [CrossRef]
- Bertoni, J.M.; Arlette, J.P.; Fernandez, H.H.; Fitzer-Attas, C.; Frei, K.; Hassan, M.N.; Isaacson, S.H.; Lew, M.F.; Molho, E.; Ondo, W.G.; et al. Increased melanoma risk in Parkinson disease: A prospective clinicopathological study. Arch. Neurol. 2010, 67, 347–352. [Google Scholar] [CrossRef]
- Israeli, E.; Yakunin, E.; Zarbiv, Y.; Hacohen-Solovich, A.; Kisos, H.; Loeb, V.; Lichtenstein, M.; Ben-Gedalya, T.; Sabag, O.; Pikarsky, E.; et al. α-Synuclein Expression Selectively Affects Tumorigenesis in Mice Modeling Parkinson’s Disease. PLoS ONE 2011, 6, e19622. [Google Scholar] [CrossRef] [PubMed]
- Turriani, E.; Lázaro, D.F.; Ryazanov, S.; Leonov, A.; Giese, A.; Schön, M.; Schön, M.P.; Griesinger, C.; Outeiro, T.F.; Arndt-Jovin, D.J.; et al. Treatment with diphenyl–pyrazole compound anle138b/c reveals that α-synuclein protects melanoma cells from autophagic cell death. Proc. Natl. Acad. Sci. USA 2017, 114, E4971–E4977. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).