Simple Summary
Cancer is a condition that affects millions of people worldwide each year. Treatments include pharmacologic and surgical interventions that can pose great risks to the physical and mental health of patients. The objective of this systematic review is to consolidate the literature surrounding the use of music therapy as a low-risk and effective pain management adjunct to traditional cancer therapy. This analysis reveals that the use of music therapy thus far has provided a nearly unanimous positive effect on cancer patients, with the potential to provide both physical and psychosocial benefits. The apparent adverse effects appear to be negligible, and music therapy should be considered when creating a cancer care plan.
Abstract
Aims and Objectives: To consolidate and summarize the current literature surrounding the use of music therapy as an effective noninvasive adjunct to conventional cancer therapy, especially as a low-risk alternative for pain management and anesthetic use in cancer patients. Background: Current studies have proposed that music therapy may be effective as a noninvasive adjunct to conventional cancer therapy in managing numerous outcomes in cancer patients. However, the findings of these investigations have not been consolidated and analyzed on a large scale. Therefore, focusing a systematic review on the effects of music therapy as an adjunct to conventional cancer therapy would give a better understanding of which intervention approaches are associated with better clinical outcomes for cancer patients. Design: A systematic review. Methods: A review of randomized controlled trials to evaluate the effectiveness of music therapy in physical, cognitive, and psychosocial outcomes for cancer patients alone or in conjunction with standard therapy was implemented. We conducted searches using the PubMed/MEDLINE, CINAHL, and Cochrane Library databases for all articles meeting the search criteria up until the time of article extraction in May, 2022. Only studies published in English were included. Two reviewers independently extracted data on participant and intervention characteristics. The main outcome variables included pain, anxiety, quality of life, mood, sleep disorders, fatigue, heart rate, blood pressure, respiratory rate, and oxygen saturation. Results: Of the 202 initially identified articles, 25 randomized controlled trials met the inclusion criteria for evaluation. Of the 25 studies, 23 (92.0%) reported statistically and clinically significant improvements across the outcome variables. Two of the studies (8.00%) found no significant positive effect from music therapy in any of the aforementioned outcomes variables. Conclusion: Music therapy, both as a standalone treatment and when used in conjunction with other pharmacologic and nonpharmacologic modalities, has a generally beneficial effect across several physiologic and psychosocial aspects of cancer.
1. Introduction
A new cancer diagnosis is a dreaded reality that many must face in their lifetime, with the prospect of chemotherapy, radiation, surgery, and even possible mortality in mind. In 2021, within the United States (U.S.) alone, an estimated 1.9 million people began to face this reality, and approximately 39.2% of men and women in the country will be diagnosed with cancer at some point in their lifetime [1]. While the general cancer 5-year survival rate has increased to 67.7%, the estimated number of cancer deaths in 2021 still reached slightly over 600,000, or roughly 1650 deaths per day [1,2].
While these metrics may be ominous, cancer mortality rates over the last 3 decades have dropped roughly 30% [1]. This is largely attributable to nationwide campaigns promoting smoking awareness and subsequent smoking cessation; however, expanded pre-screenings, genetic testing, and advanced medical technology have also played a role [1,3]. As a result, the rate of new cancer diagnoses has been increasing at a proportional rate. The American Cancer Society estimates the top five most common new cancer diagnoses in men to be prostate, lung, colorectal, bladder, and melanoma. These cancers make up nearly 60% of all new cancer diagnoses (roughly 600,000 cases) for men in the U.S. For women, the top 5 most common new cancer diagnoses include breast, lung, colorectal, uterine, and melanoma, also accounting for roughly 60% (550,000 cases) of new diagnoses [1].
The prevalence of each of these cancers varies widely, as both genetic predisposition and epigenetic factors influence rates. While familial history and genetic alterations are consistently implicated in cancer incidence, environmental risks and lifestyle behaviors such as poor diet, drinking alcohol, and obesity have become more prominent causative factors [4,5,6]. Other predisposing conditions can include viral infections such as Epstein–Barr Virus (EBV), ultraviolet (UV) radiation exposure, medications, occupational exposures, and chromosomal abnormalities [4,7,8]. These listed risks reflect only a small sample of the overarching complexity in cancer development, as each form of cancer is associated with both common and unique environmental and genetic considerations.
With both the increasing number of cancers and the evolution of cancer understanding, diagnostics have also progressed. Colonoscopies have become commonplace in American healthcare, aiding in the early detection and diagnosis of colorectal cancer [9,10]. Tumors of virtually any location can be noninvasively analyzed for malignancy with positron emission tomography (PET) scans, which show the rate of glucose uptake within a potentially cancerous neoplasm [11]. Some nations even offer this form of screening as a full-body scan for every individual over a certain age to obtain a baseline [12,13]. Varying methods of obtaining biopsies are now available as well, allowing for diagnosis of various growths in a relatively noninvasive manner [14].
Following a formal diagnosis, a range of treatment options are discussed. Often, some form of combination therapy is prescribed. The type, staging, and location of the cancer are all key components that play a role in the subsequent course of action with regard to the level of urgency and risk involved [15]. Some management modalities include surgical resection and excision, transplant surgery, radiation, chemotherapy, and immunotherapy [1,16].
Cancer patients can develop significant psychological distress, including anxiety, depression, post-traumatic stress symptoms, fear of cancer recurrence, pain, fatigue, and sleep disturbances [17]. This symptomology extends beyond the physical impact of a cancer diagnosis and must be addressed and treated accordingly [18]. The aforementioned methods are often the first thought of when a cancer diagnosis has been delivered; however, there is literature on further nontraditional methods such as music therapy (MT) for both the physical and mental rigors of such an illness.
MT can be utilized in numerous forms—a patient may listen to selected recordings or a live performance by a musical therapist. In addition to passive listening, patients may also actively participate within this setting and join in creating music. This form of outlet has been shown through numerous studies to aid in both the emotional and physical strains experienced by cancer patients [19,20,21,22]. MT has been used previously as an adjunctive therapy in the treatment diseases other than cancer [22,23]. These include, but are not limited to, the fields of psychiatry, general medicine, neurology, learning disabilities, and cardiovascular disease [22,23].
Studies have shown a significant reduction in pain, pharmacologic intervention, and emotional suffering as a result of MT [19,20,21,22,23]. The rationale stems from the ability to generate emotional and subsequent physical relaxation in response to the listening or creation of music, a concept that transcends medicine and is evident both currently and historically [23]. This form of intervention, whether a solitary treatment or as an adjunct, can present an option to reduce suffering in cancer patients while allowing for maintenance of baseline physiological and mental function [19,20,21,22,23].
The purpose of this review is to consolidate and summarize the current literature surrounding the use of music as an adjunct noninvasive cancer therapy. Our primary objective was to highlight MT as an effective noninvasive component to traditional combination treatment, especially as a low-risk alternative for pain management and anesthetic use in cancer patients [11,13].
2. Materials and Methods
For the purposes of this review, we sourced studies regarding MT as an adjunct treatment for cancer as it relates to both physical and emotional pain. This search was performed by two investigators in the following databases: PubMed/MEDLINE, CINAHL, and the Cochrane Library.
The search terms used in this literature review were as follows: “cancer” or “cancer patients” or “leukemia” or “neoplasm” or “tumor” AND “pain control” or “palliative care” AND “singing” or “choir” or “drumming” or “music” or “music therapy.”
The search sequence used in this review utilized the PICOS format of Patient, Interventions, Comparative Interventions, Outcomes, and Studies:
- P—Patients with cancer
- I—Received music therapy in addition to traditional cancer treatment
- C—Received traditional cancer treatment
- O—Pain, anxiety, quality of life, mood, sleep disorders, fatigue, heart rate (HR), blood pressure (BP), respiratory rate (RR), and oxygen saturation.
- S—Randomized controlled trials (RCTs)
This literature search was performed in May 2022. Only studies published or available in English were considered in this review. Inclusion criteria limited these articles to both observational studies and randomized controlled studies that focused on the use of MT for cancer pain management. Studies were not limited by a timeframe of publication, patient age, cancer type, or solitary MT. We included all studies where MT was utilized as a part of the cancer care plan, both as a standalone treatment and when used in conjunction with other noninvasive or invasive forms of therapy.
The results obtained from the original database search were subsequently screened manually by the two investigators for the aforementioned inclusion criteria. Those studies that met the criteria but lacked substantial pertinent data were also excluded. After initial exclusion by two independent investigators, full texts of the studies were read and evaluated. Pertinent data were extracted from the selected studies if they continued to meet inclusion criteria upon further review. Both of the authors assessed the methodological study quality independently, and a consensus was reached on the articles to be included in this analysis. All the reviews were performed blind, and any discrepancies on inclusion were later discussed and agreed upon. The Cochrane risk-of-bias tool for randomized trials was used to score all the articles prior to including them in this study. This decision was made because all the studies included in our systematic review were randomized controlled trials (RCTs). The authors determined that only studies with a perceived “low risk of bias” would be included in this study.
The articles screened were recorded in Table 1 with the following categories: study, first author, year of publication, country, type of study design, patients, MT type and treatment methods, clinical outcome evaluated, and main results. “Type of therapy” was designated as music and/or mixed, with music being solitary MT and mixed being MT in conjunction with other modes of treatment such as aroma therapy. “Treatment methods” expands on this section and demonstrates the way in which the MT was applied. This unbiased screening further limited the resultant publications, and only those that were deemed eligible by concurrent agreement were recorded in Table 1 and utilized in the subsequent analysis. The primary outcome variables used for analysis of MT were pain, anxiety, quality of life, mood, sleep disorders, fatigue, heart rate (HR), blood pressure (BP), respiratory rate (RR), and oxygen saturation.
3. Results
As seen in Figure 1, a total of 202 articles were originally identified in the primary search. After a review and exclusions were made, the results were limited to 25 publications eligible for the following qualitative analyses. Table 1 depicts the data derived from each qualifying paper, with information regarding authorship and publication, country of origin, clinical setting, patient data, type of therapy, treatment methods, study design, and main findings.
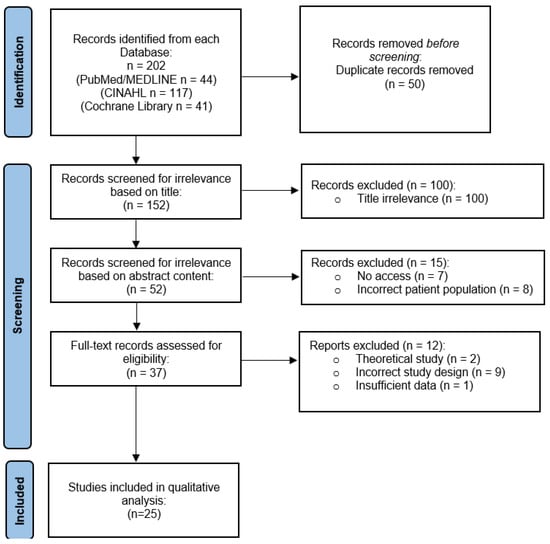
Figure 1.
Prisma flow chart—identification of studies via databases.

Table 1.
Summary of data extracted from relevant studies.
Table 1.
Summary of data extracted from relevant studies.
| Study | Year | Country | Study Design | Patients | MT Type and Treatment Methods | Clinical Outcomes Evaluated | Main Results |
|---|---|---|---|---|---|---|---|
| Xiao et al. [24] | 2018 | China | RCT | N = 100 Tx. for breast CA, inpatient | MT and mixed therapy. Record 30 min prior to symptoms, 30 min after symptoms, 4 hours after symptoms | Stress and pain scores. | MT ↓ stress and pain in both tx. groups. |
| Liu et al. [25] | 2019 | China | RCT | N = 91 Tx. for osteo-sarcoma, in-patient | Mixed therapy. 30 min MT, followed by mindfulness-based stress reduction (MSBR), followed by 30 min of listening to any music | Pain, anxiety, and sleep dysfunction. | MT + MBSR ↓ pain, anxiety, and sleep disorders. |
| Nguyen et al. [26] | 2010 | Vietnam | RCT | N = 40 Tx. for leukemia, inpa-tient | MT. Received MT before, during, and after lumbar puncture (LP). | Anxiety, pain, RR, and HR. | MT ↓ anxiety and pain, RR, and HR. |
| Tang et al. [27] | 2021 | China | RCT | N = 100 Tx. for SCLC, inpatient | MT. 6 steps of MT before, during, and after chemotherapy. | Pain, anxiety, and sleep quality. | MT ↓ pain and anxiety, and ↑ sleep quality. |
| Reimnitz et al. [28] | 2020 | USA | RCT | N = 35 Tx. for blood and bone marrow CA, inpatient. | MT. Patient Preferred Live Music (PPLM). | Pain and fatigue. | PPLM MT ↓ pain and fa-tigue. |
| Warth et al. [29] | 2016 | Germany | RCT | N = 84 Tx. for un-known CA, inpatient. | MT. Live MT with pre and post therapy discussion, 30 min total. | Vascular sympathetic tone via stress and pain. | MT ↓ vascular sympathetic tone, stress, and pain |
| Tuinmann et al. [30] | 2016 | Germany | RCT | N = 66 Tx. for un-known CA, inpatient. | MT. Standard adjunct MT. | Pain, toxicity levels, and amount of antiemetics prescribed. | MT ↓ pain, tox-icities, and antiemetic use. |
| Kwekkeboom [31] | 2007 | USA | RCT | N = 60 Tx. for un-known CA, inpatient | MT. MT before and during procedure | Pain and anxiety scores. | MT showed no significant difference |
| Huang et al. [32] | 2010 | Taiwan | RCT | N = 126 Tx. for multiple CA types, inpatient | MT. Patients listened to a chosen recording out of four 60-80 bpm melodic tracks for 30 min. | Pain management compared to analgesic usage. | MT ↑ pain relief. |
| Shabanloei et al. [33] | 2010 | Iran | RCT | N = 100 Tx. for un-known CA, inpatient. | MT. MT during a bone marrow biop-sy/aspiration. | Pain and anxiety scores. | MT ↓ pain and anxiety. |
| Li et al. [34] | 2011 | China | RCT | N = 120 Tx. for breast CA, inpatient | MT. Patient preferred mu-sic via headphones 2x a day. | Short and long-term postoperative pain. | MT ↓ pain following mastec-tomy. |
| Deng et al. [35] | 2021 | China | RCT | N = 160 Tx. for breast CA, inpatient | MT and mixed therapy. MT +/- aroma therapy | Pain, anxiety scores, IL-6, and HMGB-1 levels. | MT +/– aroma therapy improved all out-comes. |
| Bieligmeyer et al. [36] | 2019 | Germany | RCT | N = 48 Tx. for multiple CA types, inpatient | MT. MT via vibroacoustic sound bed. | Emotional and physical well-being. | ↑ Subjective emo-tional experiences and well-being. |
| Bradt et al. [37] | 2015 | USA | RCT | N = 31 Tx. for un-known CA, inpatient | MT and MM. 2 sessions of live music + 2 sessions of recorded music. | Pain and anxiety. | MT and MM ↓ pain and anxiety |
| Hsieh et al. [38] | 2019 | Taiwan | RCT | N = 60 Tx. for breast CA, at home | MT. Five 30 min sessions of HBMI for 24 weeks. | Mental fatigue, and pain intensity. | HBMI ↓ mental fatigue and pain intensity |
| Alam et al. [39] | 2015 | USA | RCT | N = 155 Tx. for skin CA, inpatient | MT. MT 4 days before and during surgery. | Intraoperative pain and anxiety. | MT showed no effect on intraoperative pain or anxiety |
| Hilliard [40] | 2003 | USA | RCT | N = 80 Tx. for multiple CA types, hospice | MT. Regular MT sessions. | Quality of life measures and lifespan. | Quality of life ↑. Lifespan had no change. |
| Bates et al. [41] | 2015 | USA | RCT | N = 108 Tx. for unknown CA, inpatient | MT. Two 30 min sessions 1 day prior and within 5 days of transplant. | Pain scores and amount of morphine required | MT ↓ pain and morphine use. |
| Wang et al. [42] | 2015 | China | RCT | N = 60 Tx. for lung CA, inpatient | MT. IV analgesia +/− MT pre- and post-op | VAS, SAS, BP, HR, analgesia frequency, and analgesic dosage | MT ↓ VAS, SAS, BP, HR, analgesia frequency, and dose |
| Burrai et al. [43] | 2014 | Italy | RCT | N = 52 Tx. for un-known CA, inpatient | MT. 30 minutes of live saxophone MT prior to treatment | Oxygen saturation and patient mood | MT ↑ oxygen saturation and mood |
| Clark et al. [44] | 2006 | USA | RCT | N = 63 Tx. for un-known CA, outpatient | MT. MT with preselected or self-selected music | Stress and anxiety | MT ↓ stress and anxiety |
| Walworth et al. [45] | 2008 | USA | RCT | N = 27 Tx. for brain CA, inpatient | MT. MT preoperatively and each day until discharge | Anxiety, relaxation, stress, and pre-procedure perception | MT ↑ quality of life measures. Length of stay was not affected |
| Bufalini [46] | 2009 | Italy | RCT | N = 39 Tx. for unknown CA, inpatient | MT. MT +/− conscious sedation | Conscious sedation, anxiety, and compliance | MT ↓ anxiety and ↑ compliance |
| Wint et al. [47] | 2002 | USA | RCT | N = 30 Tx. for unknown CA, inpatient | Mixed therapy. Patients undergoing LP were provided virtual reality (VR) glasses that incorporated visuals and music in a distraction therapy | Pain levels | VR glasses (with MT) ↓ pain |
| Ramirez et al. [48] | 2018 | Spain | RCT | N = 40 Tx. for un-known CA, inpatient | MT. One session of MT or company of the music therapist with no MT. EEG was performed for both groups | Emotional state, fatigue, anxiety, perceived ability to breathe, and relaxation | MT ↑ breathing ease and emotional state and ↓ fatigue and anxiety |
Abbreviations: Blood Pressure BP, Cancer CA, Heart Rate HR, Home Based Music Intervention HBMI, Music Medicine MM, Music Therapy MT, Randomized Controlled Trial RCT, Respiratory Rate RR, Sedation Agitation Scale SAS, Treatment Tx, Visual Analog Scale VAS.
As part of the inclusion criteria, the 25 studies were all published or available in English and were performed in the following seven countries: USA (n = 9; 36.0%), China (n = 6; 24.0%), Germany (n = 3; 12.0%), Taiwan (n = 2; 8.00%), Italy (n = 2; 8.00%), Iran (n = 1; 4.00%), Spain (n = 1, 4.00%), and Vietnam (n = 1; 4.00%) [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. The clinical setting for the administration of the MT was also recorded, with 22 (88.0%) studies occurring in inpatient hospitals [24,25,26,27,28,29,30,31,32,33,34,35,36,37,39,41,42,43,45,46,47,48], 1 (4.00%) in an outpatient facility [44], 1 (4.00%) in hospice care [40], and 1 (4.00%) as part of home healthcare [38].
In the 25 eligible records, 100% (n = 25) were randomized controlled trials (RCT), with a total of 1,875 cancer patients included. The number of participants included in each RCT ranged from 27 to 160, with the mean being 75.0 patients [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. Demographic data such as patient age, sex, gender, and race were not reported in each eligible publication and thus were not included.
The criteria for this search allowed all types of cancer to be included. Eleven studies (44.0%) did not designate a specific form(s) of cancer being treated with MT and thus are listed as “Unknown” in Table 1 [26,29,30,31,33,37,39,41,43,44,46,47,48]. Three RCTs (12.0%) stated that MT was utilized for cancer patients, listing several types; these cases are represented in Table 1 with the “Multiple” designation [32,36,40]. The remaining studies each identified a single cancer type: breast (n = 4; 16.0%) [24,34,35,38], lung (n = 2; 8.00%) [27,42], osteosarcoma (n = 1; 4.00%) [25], leukemia (n = 1; 4.00%) [26], blood and marrow (n = 1; 4.00%) [28], skin (n = 1; 4.00%) [39], and brain (n = 1; 4.00%) [45].
Any form of music included within the care plan was considered for this literature search, regardless of whether it was a solitary treatment or part of a combination therapy. Of the 25 papers included in this qualitative analysis, 20 (80.0%) utilized MT alone as a single variable intervention [26,27,28,29,30,31,32,33,34,36,38,39,40,41,42,43,44,45,46,48]; two (8.00%) utilized mixed therapy [25,47], which in this case was a conjoined music-and-aroma treatment [24,35]; and two (8.00%) tested both music as a standalone and as part of an integrated therapy. The remaining study (n = 1; 4.00%) investigated the use of MT and music medicine each as single treatment components [37].
In the selected literature, the primary outcome variables for the MT consisted of improvements in pain, anxiety, quality of life, mood, sleep disorders, fatigue, heart rate, blood pressure, respiratory rate, and oxygen saturation [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. Of the 25 studies, 22 (91.7%) reported statistically and clinically significant improvements across the parameters listed above, with the remaining 2 (8.00%) reporting no significant positive effect from the MT [24,25,26,27,28,29,30,32,33,34,35,36,37,38,40,41,42,43,44,45,46,47,48]. The 2 papers that studied solitary and combination MT found that while standalone MT provided significant improvements, mixed treatments provided even better results [24,35].
4. Discussion
Our review reveals a nearly unanimous positive benefit for MT across all physical, emotional, and mental parameters, including pain levels, anxiety, quality of life, mood and sleep disorders, fatigue, HR, BP, RR, and saturation [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. The purpose of this review was to provide a systematic qualitative analysis of the current literature surrounding MT as a form of cancer treatment. MT was defined as the use of music or audio stimulation, regardless of form, administration, duration, or timing [49]. Studies including the use of MT alone or in conjunction with additional therapies were included as well. Records were not limited to forms of cancer or patient demographics such as age, race, sex, or gender. The results of this review are consistent with other studies [50,51,52].
92.0% of the selected articles found that MT, either alone or as part of a combination therapy, provided improvement or reduction in one or more of those categories. Interestingly, the two studies that had both an MT group and a combination therapy group found MT to be effective alone but more effective as part of a joint treatment, demonstrating a possible synergistic effect between these modalities [24,35]. Only one study investigated the use of MT with both its short- and long-term effects, demonstrating immediate rapid improvement in all forms of fatigue and progressively improving symptomology at 6, 12, and 24 weeks [38].
The anti-depressive and anti-anxiety effects of MT have shown to be useful for the mental rigors of illness, especially those associated with cancer [22]. Historically, MT has shown the capacity to elicit both positive and negative emotions via music association, ultimately leading to its perceived effects on fatigue, depression, anxiety, and pain [53]. The exact process by which this occurs is not fully understood, as music and its interpretation are highly personalized [53]. However, beyond the known psychosocial aspects that can be relieved with MT, there are a multitude of physical manifestations associated with cancer, many of which are affected not only by emotion, but also by the autonomic nervous system (ANS) [54]. Sympathetic nervous system (SNS) hyperactivity is highly implicated in the development, maintenance, and metastatic nature of neoplastic growth via the release of epinephrine, norepinephrine, and resultant glucocorticoid secretion [54]. Overstimulation of β-adrenergic receptors and glucocorticoid secretion through this mechanism creates a highly oncogenic environment, frequently increasing the incidence of tumor formation and spread [55,56]. Additionally, MT has become useful in the treatment of this pro-cancerous state via the induction of emotional response and SNS homeostasis regulation [55,56]. In this regard, MT can not only exert a beneficial effect emotionally, it can also positively impact the development, growth, and spread of cancer via music-mediated SNS downregulation [55,56].
As is often the case, there are inherent limitations in this analysis. The current literature available on the topic is limited, both in quantity and content. Of the studies included in this review, the average number of participants was 75.0, with a range of only 27 to 160 [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. For all clinical trials, accurate calculation of a sample size is required for statistical and clinical significance, depending on a number of factors such as p-value, effect size, variance, and dropout rate [57]. With several studies holding such a small sample size, the ability to draw significance from the data is increasingly difficult. Additionally, there are limitations within the cancers represented in the included studies. Of the 25 studies, only 11 identified a single form of cancer, whereas the remaining 14 either treated patients with a list of multiple cancers or treated patients with cancer in general and did not make a designation of type. The most heavily represented cancers were breast and lung cancer, making up 16.0% and 8.00%, respectively. These cancers are both included in the top five most common cancers in the U.S. By contrast, the remaining forms presented in these studies can be categorized as rarer; these include brain cancer, which makes up less than 3% of cancer deaths in American men and women [1,58]. Moreover, while the study includes all MT aids in an attempt to create a broad recommendation for the effect of music in oncologic medicine, there are limitations in the generalizability of the data due to the wide variability in administration. This represents another point for improvement in the field regarding the most optimal techniques of MT and its applications. Patients may benefit from personalized music selections as opposed to preselected music, live music as opposed to recorded music, being an active participant in creating music, or from different forms of music such as instrumentals, vocals, and so on [59,60]. The possibilities of MT and music medicine are vast, not only in their array of uses but also in the patients themselves, who may have differing connections and experiences with music [14].
The literature search was limited to PubMed/MEDLINE, CINAHL, and the Cochrane Library, and studies had to have been published in English. It is highly likely that other otherwise suitable studies were not included.
Ultimately, these points serve to emphasize both the general recommendation of MT for cancer patients and the necessity for more research on the topic. There is sufficient, albeit limited, data available which we have shown to corroborate the validity of MT in treating the physical, emotional, and mental suffering associated with cancer. While this review helps add to the current literature on the topic, there remains a relative disparity in this data as compared to data on other forms of treatment. As seen in the initial query, it is evident that the literature on this topic is limited, and even more so when analyzing specific parameters. Knowledge on this topic can be further improved with in-depth analyses on music therapy across each specific form of cancer, different forms of music therapy (i.e., live, recorded, vocal, instrumental, combination), self-preferred versus preselected music, receptive versus active, and so on [14,59,60]. This review both reaffirms music therapy to be effective via a variety of measures, and emphasizes the potential for continuing studies to help us better understand the use of music therapy and help tailor treatments to the needs of cancer patients.
Although there are limitations to this review as acknowledged above, there are numerous points of strength as well. This review provides a comprehensive and robust evaluation of the current literature surrounding this topic. The literature search featured multiple databases, and the search sequence was intentionally broad so as to allow for a larger range of articles to be processed. The inclusion criteria allowed this review to analyze data with no constraint on age, geographic location, time of study, number of participants, type of cancer, stage of cancer, or type of music therapy performed. The exclusion methodology maintained the integrity of the analysis via a blind independent review and an article quality assessment. The data presented here can be reported with confidence and practical applicability, allowing us to emphasize a substantial recommendation for MT as a form of pain modulation in cancer patients.
5. Conclusions
Cancer is an illness that is physically and mentally taxing, both inherently and due to the treatments necessary for survival. The currently available therapies have advanced significantly in modern medicine; however, a majority of them pose substantial and oftentimes lethal risks. Here we have successfully synthesized the available data pertaining to the implementation of MT—a nonpharmacologic modality which we have shown to possess substantial psychosocial and physiologic benefits with minimal to no patient harm.
Author Contributions
C.R.: methodology, writing—original draft, data extraction; D.S.I.: writing—review and editing; E.H.: review and editing; J.H.: methodology, data extraction, writing—original draft, review, and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors thank UCF Librarian Shalu Gillum, JD, MLS, D-AHIP for her contributions to the literature search process.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
BP: Blood Pressure; EBV, Epstein-Barr Virus; HBMI, Home-Based Music Intervention; HMGB-1, High Mobility Group Box 1; HR, Heart Rate; IL-6, Interleukin-6; LP, Lumbar Puncture; MBSR, Mindfulness-Based Stress Reduction; MT, Music Therapy; PET, Positron Emission Tomography; PPLM, Patient-Preferred Live Music; RCT, Randomized Control Trial; RR, Respiratory Rate; SAS, Symptom Assessment Scale; US, United States; UV, Ultraviolet; VAS, Visual Analogue Scale; VR, Virtual Reality.
References
- American Cancer Society. Cancer Facts & Figures 2021; American Cancer Society: Atlanta, GA, USA, 2021; Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf (accessed on 1 May 2022).
- Emanuel, E.J.; Gudbranson, E.; Van Parys, J.; Gørtz, M.; Helgeland, J.; Skinner, J. Comparing Health Outcomes of Privileged US Citizens With Those of Average Residents of Other Developed Countries. JAMA Intern. Med. 2021, 181, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Rahib, L.; Wehner, M.R.; Matrisian, L.M.; Nead, K.T. Estimated Projection of US Cancer Incidence and Death to 2040. JAMA Netw. Open 2021, 4, e214708. [Google Scholar] [CrossRef] [PubMed]
- Takeshima, H.; Ushijima, T. Accumulation of genetic and epigenetic alterations in normal cells and cancer risk. NPJ Precis. Oncol. 2019, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Kruper, L.; Dieli-Conwright, C.M.; Mortimer, J.E. The Impact of Obesity on Breast Cancer Diagnosis and Treatment. Curr. Oncol. Rep. 2019, 21, 41. [Google Scholar] [CrossRef]
- Key, T.J.; Bradbury, K.E.; Perez-Cornago, A.; Sinha, R.; Tsilidis, K.K.; Tsugane, S. Diet, nutrition, and cancer risk: What do we know and what is the way forward? BMJ 2020, 368, m511, Correction in BMJ 2020, 368, m996. [Google Scholar] [CrossRef]
- Yasunaga, J.-I.; Matsuoka, M. Oncogenic spiral by infectious pathogens: Cooperation of multiple factors in cancer development. Cancer Sci. 2017, 109, 24–32. [Google Scholar] [CrossRef]
- Olsson, A.; Kromhout, H. Occupational cancer burden: The contribution of exposure to process-generated substances at the workplace. Mol. Oncol. 2021, 15, 753–763. [Google Scholar] [CrossRef]
- Smith, R.A.; Ba, K.S.A.; Brooks, D.; Fedewa, S.A.; Manassaram-Baptiste, D.; Saslow, D.; Wender, R.C. Cancer screening in the United States, 2019: A review of current American Cancer Society guidelines and current issues in cancer screening. CA A Cancer J. Clin. 2019, 69, 184–210. [Google Scholar] [CrossRef]
- Saito, Y.; Oka, S.; Kawamura, T.; Shimoda, R.; Sekiguchi, M.; Tamai, N.; Hotta, K.; Matsuda, T.; Misawa, M.; Tanaka, S.; et al. Colonoscopy screening and surveillance guidelines. Dig. Endosc. 2021, 33, 486–519. [Google Scholar] [CrossRef]
- Weber, W. Clinical PET/MR. Recent Results Cancer Res. 2020, 216, 747–764. [Google Scholar] [CrossRef]
- Anzai, Y.; Nishizawa, S.; Shinke, T.; Takesono, S.; Asai, T.; Okada, H. Prospective Employer-Initiated Whole-Body Cancer Screening—Costs and Outcomes of a Cancer Screening Program in Japan. J. Am. Coll. Radiol. 2021, 18, 140–147. [Google Scholar] [CrossRef]
- Kitajima, K.; Kaida, H.; Nakatani, K.; Ishibashi, M.; Morita, T.; Nakajo, M.; Tamaki, Y.; Minamimoto, R. Assessment of tumor response to definitive chemoradiotherapy and prognosis prediction in patients with esophageal cancer judged by PET response criteria in solid tumors: Multicenter study in Japan. Nucl. Med. Commun. 2020, 41, 443–451. [Google Scholar] [CrossRef]
- Nitya, K.; Keerthinarayan, V.; Rajprakash, B.; Shanmugam, K.T.; Dhamodhar, M.D.; Mohan, R.; Karthikeyan, M.; Solomon, N. Biopsy—As a Diagnostic Tool. Recent Dev. Med. Med. Res. 2021, 15, 154–166. [Google Scholar] [CrossRef]
- Hahlweg, P.; Kriston, L.; Scholl, I.; Brähler, E.; Faller, H.; Schulz, H.; Weis, J.; Koch, U.; Wegscheider, K.; Mehnert, A.; et al. Cancer patients’ preferred and perceived level of involvement in treatment decision-making: An epidemiological study. Acta Oncol. 2020, 59, 967–974. [Google Scholar] [CrossRef]
- Shariati, M.; Meric-Bernstam, F. Targeting AKT for cancer therapy. Expert Opin. Investig. Drugs 2019, 28, 977–988. [Google Scholar] [CrossRef]
- Cillessen, L.; Johannsen, M.; Speckens, A.E.; Zachariae, R. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: A systematic review and meta-analysis of randomized controlled trials. Psycho-Oncology 2019, 28, 2257–2269. [Google Scholar] [CrossRef]
- Dekker, J.; Graves, K.D.; Badger, T.A.; Diefenbach, M.A. Management of Distress in Patients with Cancer—Are We Doing the Right Thing? Ann. Behav. Med. 2020, 54, 978–984. [Google Scholar] [CrossRef]
- Deng, G. Integrative Medicine Therapies for Pain Management in Cancer Patients. Cancer J. 2019, 25, 343–348. [Google Scholar] [CrossRef]
- Stanczyk, M.M. Music therapy in supportive cancer care. Rep. Pr. Oncol. Radiother. 2011, 16, 170–172. [Google Scholar] [CrossRef]
- Palmer, J.B.; Lane, D.; Mayo, D.; Schluchter, M.; Leeming, R. Effects of Music Therapy on Anesthesia Requirements and Anxiety in Women Undergoing Ambulatory Breast Surgery for Cancer Diagnosis and Treatment: A Randomized Controlled Trial. J. Clin. Oncol. 2015, 33, 3162–3168. [Google Scholar] [CrossRef] [Green Version]
- Köhler, F.; Martin, Z.-S.; Hertrampf, R.-S.; Gäbel, C.; Kessler, J.; Ditzen, B.; Warth, M. Music Therapy in the Psychosocial Treatment of Adult Cancer Patients: A Systematic Review and Meta-Analysis. Front. Psychol. 2020, 11, 651. [Google Scholar] [CrossRef]
- Montinari, M.R.; Giardina, S.; Minelli, P.; Minelli, S. History of Music Therapy and Its Contemporary Applications in Cardiovascular Diseases. South. Med. J. 2018, 111, 98–102. [Google Scholar] [CrossRef]
- Xiao, Y.; Li, L.; Xie, Y.; Xu, J.; Liu, Y. Effects of aroma therapy and music intervention on pain and anxious for breast cancer patients in the perioperative period. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2018, 43, 656–661. [Google Scholar] [CrossRef]
- Liu, H.; Gao, X.; Hou, Y. Effects of mindfulness-based stress reduction combined with music therapy on pain, anxiety, and sleep quality in patients with osteosarcoma. Rev. Bras. de Psiquiatr. 2019, 41, 540–545. [Google Scholar] [CrossRef]
- Nguyen, T.N.; Nilsson, S.; Hellström, A.-L.; Bengtson, A. Music Therapy to Reduce Pain and Anxiety in Children With Cancer Undergoing Lumbar Puncture: A Randomized Clinical Trial. J. Pediatr. Oncol. Nurs. 2010, 27, 146–155. [Google Scholar] [CrossRef]
- Tang, H.; Chen, L.; Wang, Y.; Zhang, Y.; Yang, N.; Yang, N. The efficacy of music therapy to relieve pain, anxiety, and promote sleep quality, in patients with small cell lung cancer receiving platinum-based chemotherapy. Support. Care Cancer 2021, 29, 7299–7306. [Google Scholar] [CrossRef]
- Reimnitz, L.; Silverman, M.J. A randomized pilot study of music therapy in the form of patient-preferred live music on fatigue, energy and pain in hospitalized adult oncology patients on a blood and marrow transplant unit. Arts Heal. 2018, 12, 154–168. [Google Scholar] [CrossRef]
- Warth, M.; Kessler, J.; Hillecke, T.K.; Bardenheuer, H.J. Trajectories of Terminally Ill Patients’ Cardiovascular Response to Receptive Music Therapy in Palliative Care. J. Pain Symptom Manag. 2016, 52, 196–204. [Google Scholar] [CrossRef]
- Tuinmann, G.; Preissler, P.; Böhmer, H.; Suling, A.; Bokemeyer, C. The effects of music therapy in patients with high-dose chemotherapy and stem cell support: A randomized pilot study. Psycho-Oncology 2016, 26, 377–384. [Google Scholar] [CrossRef]
- Kwekkeboom, K.L. Music Versus Distraction for Procedural Pain and Anxiety in Patients with Cancer. Oncol. Nurs. Forum 2003, 30, 433–440. [Google Scholar] [CrossRef]
- Huang, S.-T.; Good, M.; Zauszniewski, J.A. The effectiveness of music in relieving pain in cancer patients: A randomized controlled trial. Int. J. Nurs. Stud. 2010, 47, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Shabanloei, R.; Golchin, M.; Esfahani, A.; Dolatkhah, R.; Rasoulian, M. Effects of Music Therapy on Pain and Anxiety in Patients Undergoing Bone Marrow Biopsy and Aspiration. AORN J. 2010, 91, 746–751. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-M.; Yan, H.; Zhou, K.-N.; Dang, S.-N.; Wang, D.-L.; Zhang, Y.-P. Effects of music therapy on pain among female breast cancer patients after radical mastectomy: Results from a randomized controlled trial. Breast Cancer Res. Treat. 2011, 128, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Deng, C.; Xie, Y.; Liu, Y.; Li, Y.; Xiao, Y. Aromatherapy Plus Music Therapy Improve Pain Intensity and Anxiety Scores in Patients With Breast Cancer During Perioperative Periods: A Randomized Controlled Trial. Clin. Breast Cancer 2021, 22, 115–120. [Google Scholar] [CrossRef]
- Bieligmeyer, S.; Helmert, E.; Hautzinger, M.; Vagedes, J. Feeling the sound—Short-term effect of a vibroacoustic music interven-tion on well-being and subjectively assessed warmth distribution in cancer patients-A randomized controlled trial. Complement Ther. Med. 2018, 40, 171–178. [Google Scholar] [CrossRef]
- Bradt, J.; Potvin, N.; Kesslick, A.; Shim, M.; Radl, D.; Schriver, E.; Gracely, E.J.; Komarnicky-Kocher, L.T. The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: A mixed methods study. Support. Care Cancer 2014, 23, 1261–1271. [Google Scholar] [CrossRef]
- Hsieh, F.; Miao, N.; Tseng, I.; Chiu, H.; Kao, C.; Liu, D.; Chen, R.; Tsai, H.; Chou, K. Effect of home-based music intervention versus ambient music on breast cancer survivors in the community: A feasibility study in Taiwan. Eur. J. Cancer Care 2019, 28, e13064. [Google Scholar] [CrossRef]
- Alam, M.; Roongpisuthipong, W.; Kim, N.A.; Goyal, A.; Swary, J.H.; Brindise, R.T.; Iyengar, S.; Pace, N.; West, D.P.; Polavarapu, M.; et al. Utility of recorded guided imagery and relaxing music in reducing patient pain and anxiety, and surgeon anxiety, during cutaneous surgical procedures: A single-blinded randomized controlled trial. J. Am. Acad. Dermatol. 2016, 75, 585–589. [Google Scholar] [CrossRef]
- Hilliard, R.E. The Effects of Music Therapy on the Quality and Length of Life of People Diagnosed with Terminal Cancer. J. Music Ther. 2003, 40, 113–137. [Google Scholar] [CrossRef]
- Bates, D.; Bolwell, B.; Majhail, N.S.; Rybicki, L.; Yurch, M.; Abounader, D.; Kohuth, J.; Jarancik, S.; Koniarczyk, H.; McLellan, L.; et al. Music Therapy for Symptom Management After Autologous Stem Cell Transplantation: Results From a Randomized Study. Biol. Blood Marrow Transplant. 2017, 23, 1567–1572. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Tang, H.; Guo, Q.; Liu, J.; Liu, X.; Luo, J.; Yang, W. Effects of Intravenous Patient-Controlled Sufentanil Analgesia and Music Therapy on Pain and Hemodynamics After Surgery for Lung Cancer: A Randomized Parallel Study. J. Altern. Complement. Med. 2015, 21, 667–672. [Google Scholar] [CrossRef]
- Burrai, F.; Micheluzzi, V.; Bugani, V. Effects of live sax music on various physiological parameters, pain level, and mood level in cancer patients: A randomized controlled trial. Holist. Nurs. Pr. 2014, 28, 301–311. [Google Scholar] [CrossRef]
- Clark, M.; Isaacks-Downton, G.; Wells, N.; Redlin-Frazier, S.; Eck, C.; Hepworth, J.T.; Chakravarthy, B. Use of Preferred Music to Reduce Emotional Distress and Symptom Activity During Radiation Therapy. J. Music Ther. 2006, 43, 247–265. [Google Scholar] [CrossRef]
- Walworth, D.; Rumana, C.S.; Nguyen, J.; Jarred, J. Effects of Live Music Therapy Sessions on Quality of Life Indicators, Medications Administered and Hospital Length of Stay for Patients Undergoing Elective Surgical Procedures for Brain. J. Music Ther. 2008, 45, 349–359. [Google Scholar] [CrossRef]
- Bufalini, A. Ruolo della musica interattiva nel paziente pediatrico oncologico sottoposto a procedure dolorose [Role of interac-tive music in oncological pediatric patients undergoing painful procedures]. Minerva Pediatr. 2009, 61, 379–389. [Google Scholar]
- Wint, S.S.; Eshelman, D.; Steele, J.; Guzzetta, C.E. Effects of Distraction Using Virtual Reality Glasses During Lumbar Punctures in Adolescents With Cancer. Oncol. Nurs. Forum 2002, 29, E8–E15. [Google Scholar] [CrossRef]
- Ramirez, R.; Planas, J.; Escude, N.; Mercade, J.; Farriols, C. EEG-Based Analysis of the Emotional Effect of Music Therapy on Palliative Care Cancer Patients. Front. Psychol. 2018, 9, 254. [Google Scholar] [CrossRef]
- Donald, D.E.; Pinson, J. Music Therapy in Principle and Practice; Charles C Thomas Publisher: Springfield, IL, USA, 2012. [Google Scholar]
- Bradt, J.; Dileo, C.; Magill, L.; Teague, A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst. Rev. 2016, 8, CD006911. [Google Scholar] [CrossRef]
- Gramaglia, C.; Gambaro, E.; Vecchi, C.; Licandro, D.; Raina, G.; Pisani, C.; Burgio, V.; Farruggio, S.; Rolla, R.; Deantonio, L.; et al. Outcomes of music therapy interventions in cancer patients-A review of the litera-ture. Crit. Rev. Oncol. Hematol. 2019, 138, 241–254. [Google Scholar] [CrossRef]
- Yang, T.; Wang, S.; Wang, R.; Wei, Y.; Kang, Y.; Liu, Y.; Zhang, C. Effectiveness of five-element music therapy in cancer patients: A systematic review and meta-analysis. Complement. Ther. Clin. Pr. 2021, 44, 101416. [Google Scholar] [CrossRef]
- Cook, T.; Roy, A.R.K.; Welker, K.M. Music as an emotion regulation strategy: An examination of genres of music and their roles in emotion regulation. Psychol. Music 2017, 47, 144–154. [Google Scholar] [CrossRef]
- Ginsberg, J.P.; Raghunathan, K.; Bassi, G.; Ulloa, L. Review of Perioperative Music Medicine: Mechanisms of Pain and Stress Reduction Around Surgery. Front. Med. 2022, 9, 821022. [Google Scholar] [CrossRef]
- Hiller, J.G.; Cole, S.W.; Crone, E.M.; Byrne, D.J.; Shackleford, D.M.; Pang, J.-M.B.; Henderson, M.A.; Nightingale, S.S.; Ho, K.M.; Myles, P.S.; et al. Preoperative β-Blockade with Propranolol Reduces Biomarkers of Metastasis in Breast Cancer: A Phase II Randomized Trial. Clin. Cancer Res. 2020, 26, 1803–1811. [Google Scholar] [CrossRef] [PubMed]
- Ayroldi, E.; Cannarile, L.; Adorisio, S.; Delfino, D.V.; Riccardi, C. Role of Endogenous Glucocorticoids in Cancer in the Elderly. Int. J. Mol. Sci. 2018, 19, 3774. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.K.; Attri, J.P.; Singh, A.; Kaur, H.; Kaur, G. Basic concepts for sample size calculation: Critical step for any clinical trials! Saudi J. Anaesth. 2016, 10, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Kalan Farmanfarma, K.H.; Mohammadian, M.; Shahabinia, Z.; Hassanipour, S.; Salehiniya, H. Brain cancer in the world: An epidemiological review. World Cancer Res. J. 2019, 6, e1356. [Google Scholar] [CrossRef]
- Hiller, J.; Gardstrom, S.C. The Selection of Music Experiences in Music Therapy. Music Ther. Perspect. 2018, 36, 79–86. [Google Scholar] [CrossRef]
- Tsoi, K.K.; Chan, J.Y.; Ng, Y.-M.; Lee, M.M.; Kwok, T.C.; Wong, S.Y.-S. Receptive Music Therapy Is More Effective than Interactive Music Therapy to Relieve Behavioral and Psychological Symptoms of Dementia: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2018, 19, 568–576.e3. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).