Recurrent Endometrial Cancer: Which Is the Best Treatment? Systematic Review of the Literature
Abstract
:Simple Summary
Abstract
1. Introduction
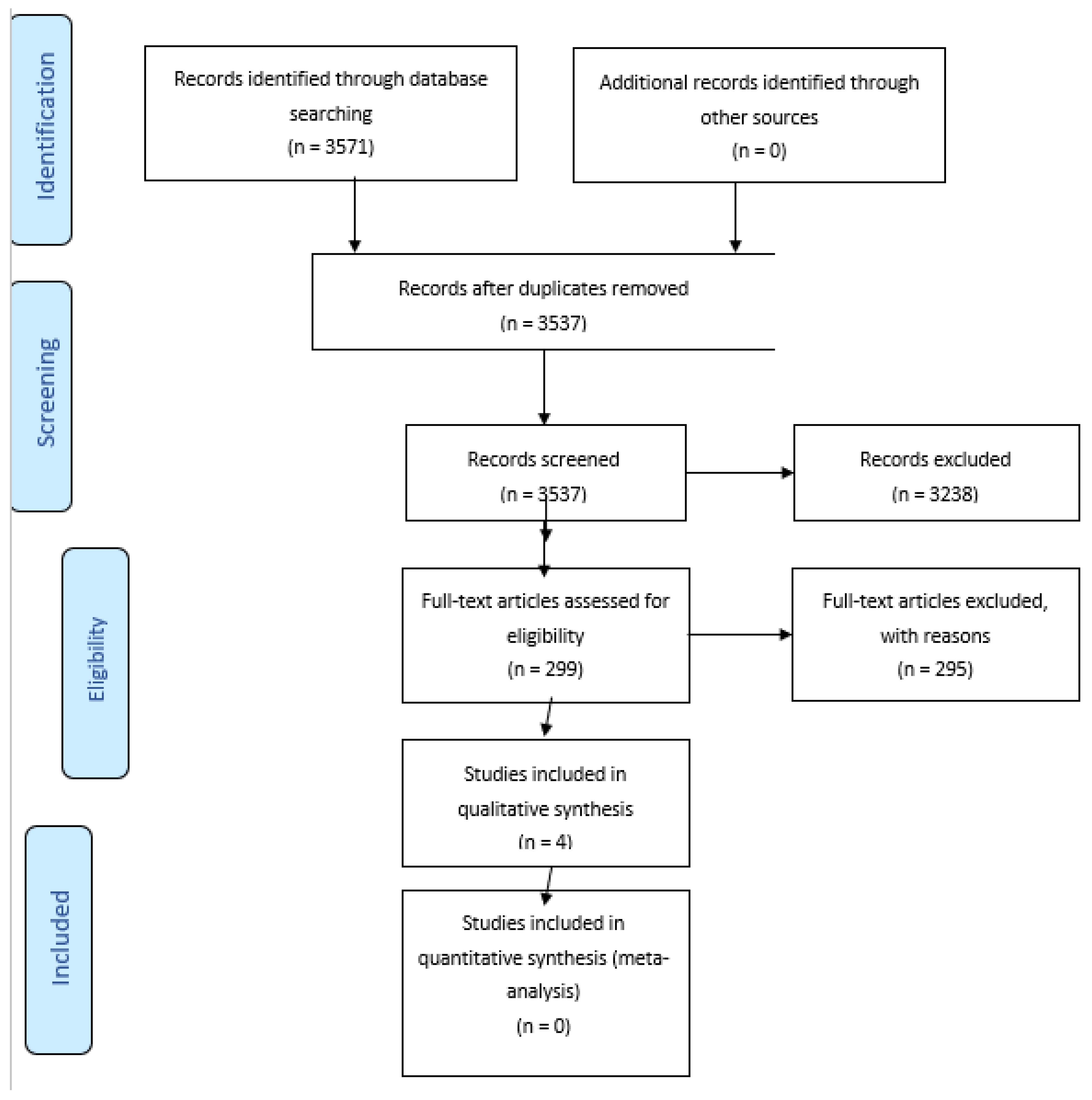
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction
2.3. Inclusion Criteria
- -
- comparison of outcomes of different therapeutic strategies in the management of patients with endometrial cancer recurrences. In particular, women treated surgically compared to those who underwent a non-surgical treatment (to radiotherapy (RT), chemotherapy, hormonal treatment and/or radio-chemotherapy);
- -
- available data on OS and DFS by clinical or surgical stage or both;
- -
- patients’ medical data;
- -
- only full-text articles were considered eligible for inclusion.
2.4. Exclusion Criteria
- -
- review, letters, editorials, case reports;
- -
- studies not published in English;
- -
- studies reporting on only one treatment of the EC recurrence without comparison
- -
- studies with missing data on outcomes.
3. Results
- -
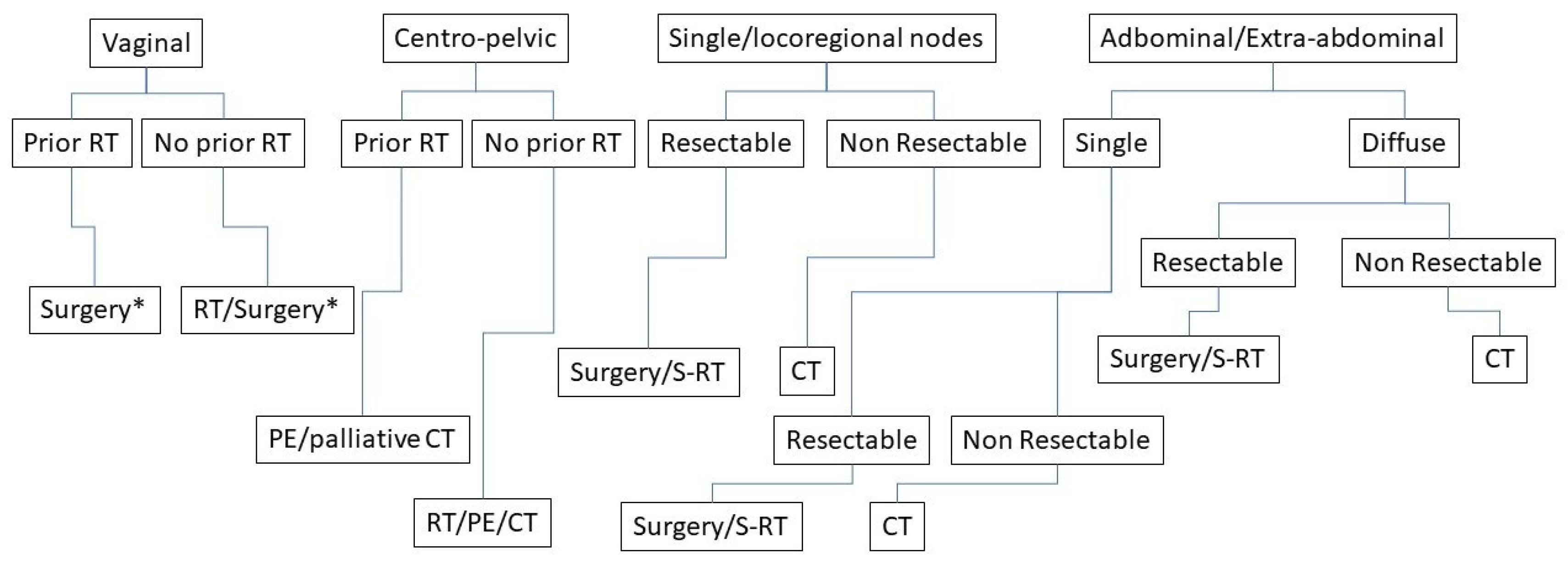
- Locoregional recurrence: vaginal only or pelvic (which could also have concurrent vaginal recurrence)
- -
- Abdominal recurrence: Greater pelvis (pelvic sidewall, pelvic or paraortic lymph nodes, and sigmoid colon) Abdomen (surface of liver, omentum and abdominal wall)
- -
- Extra abdominal recurrence: distance recurrence out of abdomen
3.1. Locoregional Recurrence
3.2. Abdominal Recurrence
3.3. Extra-Abdominal Recurrence
4. Discussion
4.1. Locoregional Recurrence
- -
- central pelvic recurrence; the treatment of choice is surgery or radiation therapy based according to previous RT, size of disease, complete removal of macroscopic disease, easily accessible vaginal tumour.
- -
- regional pelvic recurrences; the treatment is radiation therapy, associated if possible with chemotherapy, or we can also consider exenterative surgery in selected patients.
4.2. Abdominal Recurrence
4.3. Extra-Abdominal Recurrence
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Amant, F.; Moerman, P.; Neven, P.; Timmerman, D.; Van Limbergen, E.; Vergote, I. Endometrial cancer. Lancet 2005, 366, 491–505. [Google Scholar] [CrossRef] [PubMed]
- Survival of Cancer Patients in Italy, Italian Cancer Figures-Report 2020. Airtum Working Group. Available online: https://www.registri-tumori.it/cms/ (accessed on 18 April 2022).
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2015. CA Cancer J. Clin. 2015, 65, 5–29. [Google Scholar] [CrossRef] [PubMed]
- Creutzberg, C.L.; Nout, R.A.; Lybeert, M.L.; Wárlám-Rodenhuis, C.C.; Jobsen, J.J.; Mens, J.W.; Lutgens, L.C.; Pras, E.; van de Poll-Franse, L.V.; van Putten, W.L.; et al. Fifteen-year radiotherapy outcomes of the randomized PORTEC-1 trial for endometrial carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, e631–e638. [Google Scholar]
- Colombo, N.; Creutzberg, C.; Amant, F.; Bosse, T.; González-Martín, A.; Ledermann, J.; Marth, C.; Nout, R.; Querleu, D.; Mirza, M.R.; et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, Treatment and Follow-up. Int. J. Gynecol. Cancer 2016, 26, 2–30. [Google Scholar] [CrossRef]
- Restaino, S.; Tortorella, L.; Dinoi, G.; Zannoni, G.F.; Baroni, A.; Capasso, I.; Distefano, E.; Sozzi, G.; Chiantera, V.; Scambia, G.; et al. Semiquantitative evaluation of lymph-vascular space invasion in patients affected by endometrial cancer: Prognostic and clinical implications. Eur. J. Cancer 2021, 142, 29–37. [Google Scholar] [CrossRef]
- Tortorella, L.; Restaino, S.; Zannoni, G.F.; Vizzielli, G.; Chiantera, V.; Cappuccio, S.; Gioè, A.; La Fera, E.; Dinoi, G.; Angelico, G.; et al. Substantial lymph-vascular space invasion (LVSI) as predictor of distant relapse and poor prognosis in low-risk early-stage endometrial cancer. J. Gynecol. Oncol. 2021, 32, e11. [Google Scholar] [CrossRef]
- Barlin, J.N.; Wysham, W.Z.; Ferda, A.M.; Khoury-Collado, F.; Cassella, D.K.; Alektiar, K.M.; Hensley, M.L.; Chi, D.S.; Barakat, R.R.; Abu-Rustum, N.R. Location of disease in patients who die from endometrial cancer: A study of 414 patients from a single institution. Int. J. Gynecol. Cancer 2012, 22, 1527–1531. [Google Scholar] [CrossRef]
- Radiation Therapy with or without Cisplatin in Treating Patients with Recurrent Endometrial Cancer. 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT00492778 (accessed on 18 April 2022).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Zorzela, L.; Loke, Y.K.; Ioannidis, J.P.; Golder, S.; Santaguida, P.; Altman, D.G.; Moher, D.; Vohra, S.; PRISMAHarms Group. PRISMA harms checklist: Improving harms reporting in systematic reviews. BMJ 2016, 352, i157, Erratum in BMJ 2016, 353, i2229. [Google Scholar] [CrossRef]
- Francis, S.R.; Ager, B.J.; Do, O.A.; Huang, Y.J.; Soisson, A.P.; Dodson, M.K.; Werner, T.L.; Sause, W.T.; Grant, J.D.; Gaffney, D.K. Recurrent early stage endometrial cancer: Patterns of recurrence and results of salvage therapy. Gynecol. Oncol. 2019, 154, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Hardarson, H.A.; Heidemann, L.N.; dePont Christensen, R.; Mogensen, O.; Jochumsen, K.M. Vaginal vault recurrences of endometrial cancer in non-irradiated patients-Radiotherapy or surgery. Gynecol. Oncol. Rep. 2015, 11, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Dowdy, S.C.; Mariani, A.; Bakkum, J.N.; Cliby, W.A.; Keeney, G.L.; Podratz, K.C. Treatment of pulmonary recurrences in patients with endometrial cancer. Gynecol. Oncol. 2007, 107, 242–247. [Google Scholar] [CrossRef] [PubMed]
- McAlarnen, L.A.; Ryan, K.; Adams, W.; Gliniewicz, A.; Winder, A.D.; Liotta, M.R.; Potkul, R.K.; Small, W., Jr. Harkenrider MM.Salvage treatment in recurrent endometrial cancer of the pelvis and peritoneal cavity. Gynecol. Oncol. Rep. 2019, 29, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rauh-Hain, J.A.; Del Carmen, M.G. Treatment for advanced and recurrent endometrial carcinoma: Combined modalities. Oncologist 2010, 15, 852–861. [Google Scholar] [CrossRef]
- Del Carmen, M.G.; Boruta, D.M., 2nd; Schorge, J.O. Recurrent endometrial cancer. Clin. Obstet. Gynecol. 2011, 54, 266–277. [Google Scholar] [CrossRef]
- Campagnutta, E.; Giorda, G.; De Piero, G.; Sopracordevole, F.; Visentin, M.C.; Martella, L. Carlo Scarabelli. Surgical treatment of recurrent endometrial carcinoma. Cancer 2004, 100, 89–96. [Google Scholar] [CrossRef]
- Morice, P.; Leary, A.; Creutzberg, C.; Abu-Rustum, N.; Darai, E. Endometrial cancer. Lancet 2016, 387, 1094–1108. [Google Scholar] [CrossRef]
- Koh, W.J.; Abu-Rustum, N.R.; Bean, S.; Bradley, K.; Campos, S.M.; Cho, K.R.; Chon, H.S.; Chu, C.; Cohn, D.; Crispens, M.A.; et al. Uterine Neoplasms, Version 1.2018, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2018, 16, 170–199. [Google Scholar] [CrossRef]
- Huijgens, A.N.; Mertens, H.J. Factors predicting recurre.ent endometrial cancer. Facts Views Vis. Obgyn. 2013, 5, 179–186. [Google Scholar]
- Bendifallah, S.; Ouldamer, L.; Lavoue, V.; Canlorbe, G.; Raimond, E.; Coutant, C.; Graesslin, O.; Touboul, C.; Collinet, P.; Daraï, E.; et al. Groupe de Recherche FRANCOGYN. Patterns of recurrence and outcomes in surgically treated women with endometrial cancer according to ESMO-ESGO-ESTRO Consensus Conference risk groups: Results from the FRANCOGYN study Group. Gynecol. Oncol. 2017, 144, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Gaudet Chardonnet, A.; Azaïs, H.; Ballester, M.; Raimond, E.; Bendifallah, S.; Ouldamer, L.; Coutant, C.; Graesslin, O.; Touboul, C.; Collinet, P.; et al. Prognostic Value and Risk Factors of Peritoneal Carcinomatosis Recurrence for Patients with Endometrial Cancer: A Multicenter Study from the FRANCOGYN Group. Ann. Surg. Oncol. 2021, 28, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Barlin, J.N.; Puri, I.; Bristow, R.E. Cytoreductive surgery for advanced or recurrent endometrial cancer: A meta-analysis. Gynecol. Oncol. 2010, 118, 14–18. [Google Scholar] [CrossRef]
- Morgan, J.D., 3rd; Reddy, S.; Sarin, P.; Yordan, E.; DeGeest, K.; Hendrickson, F.R. Isolated vaginal recurrences of endometrial carcinoma. Radiology 1993, 189, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Legge, F.; Restaino, S.; Leone, L.; Carone, V.; Ronsini, C.; Di Fiore, G.L.M.; Pasciuto, T.; Pelligra, S.; Ciccarone, F.; Scambia, G.; et al. Clinical outcome of recurrent endometrial cancer: Analysis of post-relapse survival by pattern of recurrence and secondary treatment. Int. J. Gynecol. Cancer 2020, 30, 193–200. [Google Scholar] [CrossRef]
- Papadia, A.; Bellati, F.; Ditto, A.; Bogani, G.; Gasparri, M.L.; Di Donato, V.; Martinelli, F.; Lorusso, D.; Benedetti-Panici, P.; Raspagliesi, F. Surgical Treatment of Recurrent Endometrial Cancer: Time for a Paradigm Shift. Ann. Surg. Oncol. 2015, 22, 4204–4210. [Google Scholar] [CrossRef]
- Chapman, C.H.; Maghsoudi, K.; Littell, R.D.; Chen, L.M.; Hsu, I.C. Salvage high-dose-rate brachytherapy and external beam radiotherapy for isolated vaginal recurrences of endometrial cancer with no prior adjuvant therapy. Brachytherapy 2017, 16, 1152–1158. [Google Scholar] [CrossRef]
- Concin, N.; Matias-Guiu, X.; Vergote, I.; Cibula, D.; Mirza, M.R.; Marnitz, S.; Ledermann, J.; Bosse, T.; Chargari, C.; Fagotti, A.; et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int. J. Gynecol. Cancer 2021, 31, 12–39. [Google Scholar] [CrossRef]
- Creutzberg, C.L.; van Putten, W.L.; Koper, P.C.; Lybeert, M.L.; Jobsen, J.J.; Wárlám-Rodenhuis, C.C.; De Winter, K.A.; Lutgens, L.C.; van den Bergh, A.C.; van der Steen-Banasik, E.; et al. PORTEC Study Group. Survival after relapse in patients with endometrial cancer: Results from a randomized trial. Gynecol. Oncol. 2003, 89, 201–209. [Google Scholar] [CrossRef]
- Barakat, R.R.; Goldman, N.A.; Patel, D.A.; Venkatraman, E.S.; Curtin, J.P. Pelvic exenteration for recurrent endometrial cancer. Gynecol. Oncol. 1999, 75, 99–102. [Google Scholar] [CrossRef]
- Chiantera, V.; Rossi, M.; De Iaco, P.; Koehler, C.; Marnitz, S.; Gallotta, V.; Margariti, A.P.; Parazzini, F.; Scambia, G.; Schneider, A.; et al. Pelvic exenteration for recurrent endometrial adenocarcinoma: A retrospective multi-institutional study about 21 patients. Int. J. Gynecol. Cancer 2014, 24, 880–884. [Google Scholar] [CrossRef] [PubMed]
- Vizzielli, G.; Naik, R.; Dostalek, L.; Bizzarri, N.; Kucukmetin, A.; Tinelli, G.; Scambia, G.; Cibula, D. Laterally Extended Pelvic Resection for Gynaecological Malignancies: A Multicentric Experience with Out-of-the-Box Surgery. Ann. Surg. Oncol. 2019, 26, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Scarabelli, C.; Campagnutta, E.; Giorda, G.; DePiero, G.; Sopracordevole, F.; Quaranta, M.; DeMarco, L. Maximal cytoreductive surgery as a reasonable therapeutic alternative for recurrent endometrial carcinoma. Gynecol. Oncol. 1998, 70, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Awtrey, C.S.; Cadungog, M.G.; Leitao, M.M.; Alektiar, K.M.; Aghajanian, C.; Hummer, A.J.; Barakat, R.R.; Chi, D.S. Surgical resection of recurrent endometrial carcinoma. Gynecol. Oncol. 2006, 102, 480–488. [Google Scholar] [CrossRef]
- Bristow, R.E.; Santillan, A.; Zahurak, M.L.; Gardner, G.J.; Giuntoli, R.L., 2nd; Armstrong, D.K. Salvage cytoreductive surgery for recurrent endometrial cancer. Gynecol. Oncol. 2006, 103, 281–287. [Google Scholar] [CrossRef]
- Zanfagnin, V.; Ferrero, A.; Biglia, N.; Aletti, G.; Gill, S.E.; Makdisi, P.B.; Multinu, F.; Mariani, A. The role of surgery in recurrent endometrial cancer. Expert Rev. Anticancer Ther. 2016, 16, 741–750. [Google Scholar] [CrossRef]
- Miller, D.; Filiaci, V.; Fleming, G.; Mannel, R.; Cohn, D.; Matsumoto, T.; Tewari, K.; DiSilvestro, P.; Pearl, M.; Zaino, R. Randomized phase III noninferiority trial of first line chemotherapy for metastatic or recurrent endometrial carcinoma: A Gynecologic Oncology Group study. Gynecol. Oncol. 2012, 125, 771. [Google Scholar]
- Oza, A.M.; Elit, L.; Biagi, J.; Chapman, W.; Tsao, M.; Hedley, D.; Hansen, C.; Dancey, J.; Eisenhauer, E. Molecular correlates associated with a phase II study of temsirolimus (CCI-779) in patients with metastatic or recurrent endometrial cancer. NCIC IND 160. J. Clin. Oncol. 2006, 24, 3003. [Google Scholar] [CrossRef]
- Fleming, G.F.; Sill, M.W.; Darcy, K.M.; McMeekin, D.S.; Thigpen, J.T.; Adler, L.M.; Berek, J.S.; Chapman, J.A.; DiSilvestro, P.A.; Horowitz, I.R.; et al. Phase II trial of trastuzumab in women with advanced or recurrent, HER2-positive endometrial carcinoma: A Gynecologic Oncology Group study. Gynecol. Oncol. 2010, 116, 15–20. [Google Scholar] [CrossRef]
- Dresler, C.M.; Goldberg, M. Surgical management of lung metastases: Selection factors and results. Oncology 1996, 10, 649–655. [Google Scholar] [PubMed]
- Mariani, A.; Webb, M.J.; Keeney, G.L.; Calori, G.; Podratz, K.C. Hematogenous dissemination in corpus cancer. Gynecol. Oncol. 2001, 80, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Anraku, M.; Yokoi, K.; Nakagawa, K.; Fujisawa, T.; Nakajima, J.; Akiyama, H.; Nishimura, Y.; Kobayashi, K.; Metastatic Lung Tumor Study Group of Japan. Pulmonary metastases from uterine malignancies: Results of surgical resection in 133 patients. J. Thorac. Cardiovasc. Surg. 2004, 127, 1107–1112. [Google Scholar] [CrossRef] [PubMed]
- Clavero, J.M.; Deschamps, C.; Cassivi, S.D.; Allen, M.S.; Nichols, F.C., 3rd; Barrette, B.A.; Larson, D.R.; Pairolero, P.C. Gynecologic cancers: Factors affecting survival after pulmonary metastasectomy. Ann. Thorac. Surg. 2006, 81, 2004–2007. [Google Scholar] [CrossRef] [PubMed]
- Bradford, L.S.; Rauh-Hain, J.A.; Schorge, J.; Birrer, M.J.; Dizon, D.S. Advances in the management of recurrent endometrial cancer. Am. J. Clin. Oncol. 2015, 38, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Toboni, M.D.; Powell, M.A. New Treatments for Recurrent Uterine Cancer. Curr. Oncol. Rep. 2021, 23, 13. [Google Scholar] [CrossRef]
- Connor, E.V.; Rose, P.G. Management Strategies for Recurrent Endometrial Cancer. Expert Rev. Anticancer Ther. 2018, 18, 873–885. [Google Scholar] [CrossRef]
| Author, Year | Type of Study | Sample (N) | Site of First Recurrence (N) | Type of Treatment (N) | Secondary Recurrence Rate (%) | 2-Year Desease Free Survival (%) | Overall Survival (Median, Years) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Hardarson HA, 2015 | Retrospective | 33 | Vaginal, 33 | RT Surgery RT + Surgery | 26 (78.8) 5 (15.1) 2 (6.1%) | RT Surgery RT + Surgery | 40% 0% 0% | RT Surgery RT + Surgery | 83% 100% 100% | Not Analysed |
| Francis SR, 2019 | Retrospective | 194 | Vaginal, 43 | RT Surgery CHT Hormonal Combined tx None | 24 (55.8%) 3 (7%) 0 (0%) 0 (0%) 16 (37.2%) 0 (0%) | * LLR NONE DISTANCE | 10 (10.1%) 40 (40.4%) 49 (49.5%) | ** LLR DISTANCE NONE | 50% 14.3% 94.1% | 14 |
| Pelvic, 56 | RT Surgery CHT Hormonal Combined tx None | 9 (16%) 6 (10.7%) 2 (3.6%) 2 (3.6%) 31 (55.4%) 6 (10.7%) | 1.2 | |||||||
| Distance, 96 | Not Analysed | Not Analysed | Not Analysed | 1.0 | ||||||
| Mc Alarnen L, 2019 | Case series Retrospective | 22 | Pelvic, 13 | Surgery No Surgery Combined treat. | 2 (15.4%) 3 (23.1%) 8 (61.5%) | Surgery No Surgery Combined treat. | 1 (50%) 1 (33.3%) 2 (24%) | Not Analysed | Not Analysed | |
| Abdominal, 9 | Surgery No Surgery Combined treat. | 2 (22.2%) 2 (22.2%) 5 (55.6%) | Surgery No Surgery Combined treat. | 1 (50%) 2 (100%) 2 (40%) | Not Analysed | |||||
| Pelvic + Abdominal, 22 | Surgery No Surgery Combined treat. | 4 (18%) 5 (22.7%) 13 (59.1%) | Surgery No Surgery Combined treat. | 2 (40%) 3 (60%) 4 (31%) | Surgery No Surgery Combined treat. | 67% 53% 68% | ||||
| Dowdy SC, 2007 | Retrospective | 82 | Pulmonary Isolated, 28 | CHT Hormonal Surgery Combined treat. | 9 (32%) 19 (68%) 14 (50%) 11 (13%) | Not Analysed | 50% | |||
| Multiple site, 54 (Abdominal and extrabdominal) | 4% | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Restaino, S.; Dinoi, G.; La Fera, E.; Gui, B.; Cappuccio, S.; Campitelli, M.; Vizzielli, G.; Scambia, G.; Fanfani, F. Recurrent Endometrial Cancer: Which Is the Best Treatment? Systematic Review of the Literature. Cancers 2022, 14, 4176. https://doi.org/10.3390/cancers14174176
Restaino S, Dinoi G, La Fera E, Gui B, Cappuccio S, Campitelli M, Vizzielli G, Scambia G, Fanfani F. Recurrent Endometrial Cancer: Which Is the Best Treatment? Systematic Review of the Literature. Cancers. 2022; 14(17):4176. https://doi.org/10.3390/cancers14174176
Chicago/Turabian StyleRestaino, Stefano, Giorgia Dinoi, Eleonora La Fera, Benedetta Gui, Serena Cappuccio, Maura Campitelli, Giuseppe Vizzielli, Giovanni Scambia, and Francesco Fanfani. 2022. "Recurrent Endometrial Cancer: Which Is the Best Treatment? Systematic Review of the Literature" Cancers 14, no. 17: 4176. https://doi.org/10.3390/cancers14174176
APA StyleRestaino, S., Dinoi, G., La Fera, E., Gui, B., Cappuccio, S., Campitelli, M., Vizzielli, G., Scambia, G., & Fanfani, F. (2022). Recurrent Endometrial Cancer: Which Is the Best Treatment? Systematic Review of the Literature. Cancers, 14(17), 4176. https://doi.org/10.3390/cancers14174176









