A New Clinical Instrument for Estimating the Ambulatory Status after Irradiation for Malignant Spinal Cord Compression
Abstract
:Simple Summary
Abstract
1. Introduction
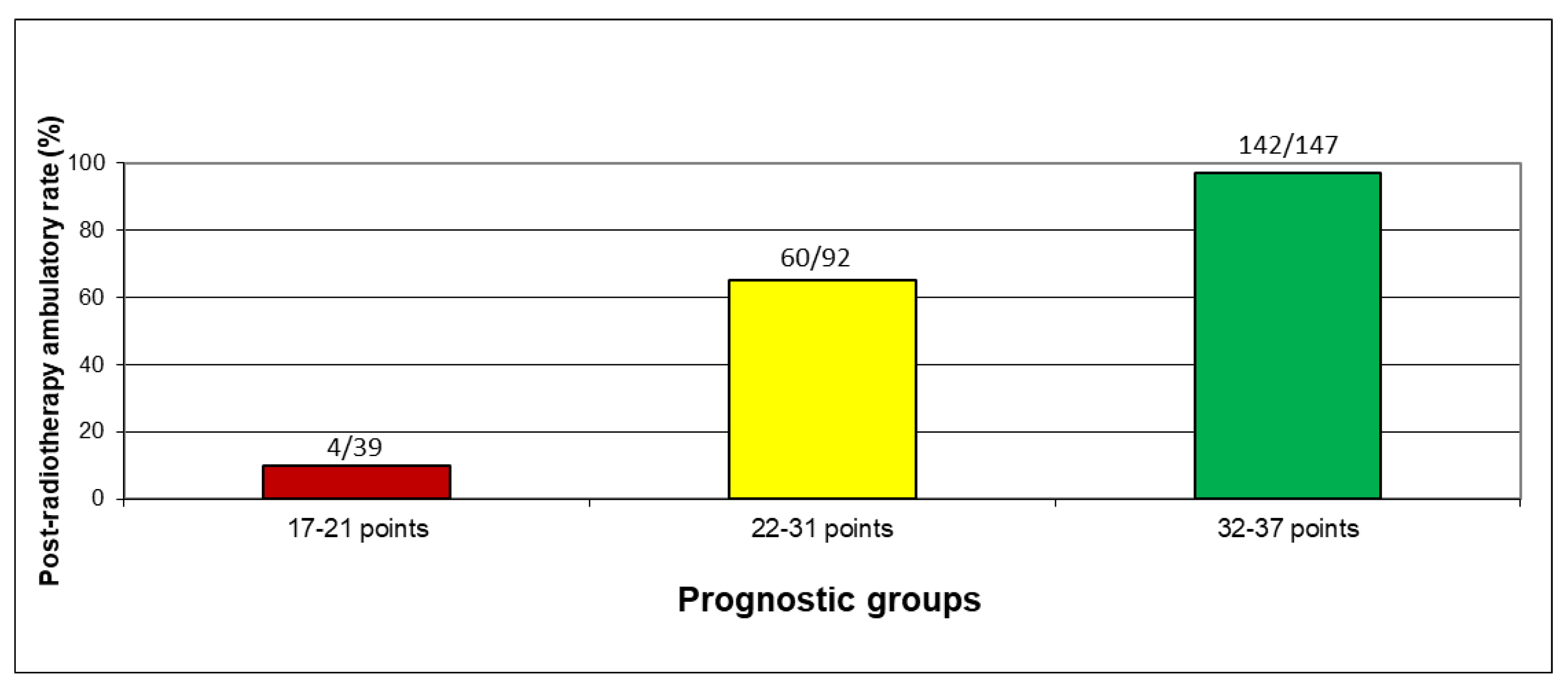
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prasad, D.; Schiff, D. Malignant spinal cord compression. Lancet Oncol. 2005, 6, 15–24. [Google Scholar] [CrossRef]
- Rades, D.; Abrahm, J.L. The role of radiotherapy for metastatic epidural spinal cord compression. Nat. Rev. Clin. Oncol. 2010, 7, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Lawton, A.J.; Lee, K.A.; Cheville, A.L.; Ferrone, M.L.; Rades, D.; Balboni, T.A.; Abrahm, J.L. Assessment and management of patients with metastatic spinal cord compression: A multidisciplinary review. J. Clin. Oncol. 2019, 37, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Patchell, R.; Tibbs, P.A.; Regine, W.F.; Payne, R.; Saris, S.; Kryscio, R.J.; Mohiuddin, M.; Young, B. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: A randomised trial. Lancet 2005, 366, 643–648. [Google Scholar] [CrossRef] [Green Version]
- Rades, D.; Huttenlocher, S.; Dunst, J.; Bajrovic, A.; Karstens, J.H.; Rudat, V.; Schild, S.E. Matched pair analysis comparing surgery followed by radiotherapy and radiotherapy alone for metastatic spinal cord compression. J. Clin. Oncol. 2010, 28, 3597–3604. [Google Scholar] [CrossRef]
- Rades, D.; Küchler, J.; Graumüller, L.; Abusamha, A.; Schild, S.E.; Gliemroth, J. Radiotherapy with or without decompressive surgery for metastatic spinal cord compression: A retrospective matched-pair study including data from prospectively evaluated patients. Cancers 2022, 14, 1260. [Google Scholar] [CrossRef]
- Rades, D.; Rudat, V.; Veninga, T.; Stalpers, L.J.A.; Bazic, H.; Karstens, J.H.; Hoskin, P.J.; Schild, S.E. A score predicting post-treatment ambulatory status in patients irradiated for metastatic spinal cord compression. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 905–908. [Google Scholar] [CrossRef]
- Rades, D.; Šegedin, B.; Conde-Moreno, A.J.; Garcia, R.; Perpar, A.; Metz, M.; Badakhshi, H.; Schreiber, A.; Nitsche, M.; Hipp, P.; et al. Radiotherapy with 4 Gy × 5 versus 3 Gy × 10 for metastatic epidural spinal cord compression: Final results of the SCORE-2 trial (ARO 2009/01). J. Clin. Oncol. 2016, 34, 597–602. [Google Scholar] [CrossRef]
- Rades, D.; Cacicedo, J.; Conde-Moreno, A.J.; Doemer, C.; Dunst, J.; Lomidze, D.; Segedin, B.; Olbrich, D.; Holländer, N.H. High-precision radiotherapy of motor deficits due to metastatic spinal cord compression (PRE-MODE): A multicenter phase 2 study. BMC Cancer 2017, 17, 818. [Google Scholar] [CrossRef] [Green Version]
- Rades, D.; Cacicedo, J.; Conde-Moreno, A.J.; Segedin, B.; But-Hadzic, J.; Groselj, B.; Kevlishvili, G.; Lomidze, D.; Ciervide-Jurio, R.; Rubio, C.; et al. Precision radiation therapy for metastatic spinal cord compression: Final results of the PRE-MODE Trial. Int. J. Radiat. Oncol. Biol. Phys. 2020, 106, 780–789. [Google Scholar] [CrossRef]
- Rades, D.; Hansen, O.; Jensen, L.H.; Dziggel, L.; Staackmann, C.; Doemer, C.; Cacicedo, J.; Conde-Moreno, A.J.; Segedin, B.; Ciervide-Jurio, R.; et al. Radiotherapy for metastatic spinal cord compression with increased radiation doses (RAMSES-01): A prospective multicenter study. BMC Cancer 2019, 19, 1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rades, D.; Huttenlocher, S.; Bajrovic, A.; Karstens, J.H.; Adamietz, I.A.; Kazic, N.; Rudat, V.; Schild, S.E. Surgery followed by radiotherapy versus radiotherapy alone for metastatic spinal cord compression from unfavorable tumors. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, e861–e868. [Google Scholar] [CrossRef] [PubMed]
- Rades, D.; Douglas, S.; Huttenlocher, S.; Rudat, V.; Veninga, T.; Stalpers, L.J.; Basic, H.; Karstens, J.H.; Hoskin, P.J.; Adamietz, I.A.; et al. Validation of a score predicting post-treatment ambulatory status after radiotherapy for metastatic spinal cord compression. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 1503–1506. [Google Scholar] [CrossRef]
- Bach, F.; Larsen, B.H.; Rohde, K.; Børgesen, S.E.; Gjerris, F.; Bøge-Rasmussen, T.; Agerlin, N.; Rasmusson, B.; Stjernholm, P.; Sørensen, P.S. Metastatic spinal cord compression. Occurrence, symptoms, clinical presentations and prognosis in 398 patients with spinal cord compression. Acta Neurochir. Wien 1990, 107, 37–43. [Google Scholar] [CrossRef]
- Gilbert, R.W.; Kim, J.H.; Posner, J.B. Epidural spinal cord compression from metastatic tumor: Diagnosis and treatment. Ann. Neurol. 1978, 3, 40–51. [Google Scholar] [CrossRef] [PubMed]
- Helweg-Larsen, S.; Sørensen, P.S. Symptoms and signs in metastatic spinal cord compression: A study of progression from first symptom until diagnosis in 153 patients. Eur. J. Cancer 1994, 30, 396–398. [Google Scholar] [CrossRef]
- Bilsky, M.H.; Laufer, I.; Fourney, D.R.; Groff, M.; Schmidt, M.H.; Varga, P.P.; Vrionis, F.D.; Yamada, Y.; Gerszten, P.C.; Kuklo, T.R. Reliability analysis of the epidural spinal cord compression scale. J. Neurosurg. Spine 2010, 13, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Fisher, C.G.; DiPaola, C.P.; Ryken, T.C.; Bilsky, M.H.; Shaffrey, C.I.; Berven, S.H.; Harrop, J.S.; Fehlings, M.G.; Boriani, S.; Chou, D.; et al. A novel classification system for spinal instability in neoplastic disease: An evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine Phila Pa 1976 2010, 35, E1221–E1229. [Google Scholar] [CrossRef] [Green Version]
- Fourney, D.R.; Frangou, E.M.; Ryken, T.C.; Dipaola, C.P.; Shaffrey, C.I.; Berven, S.H.; Bilsky, M.H.; Harrop, J.S.; Fehlings, M.G.; Boriani, S.; et al. Spinal instability neoplastic score: An analysis of reliability and validity from the spine oncology study group. J. Clin. Oncol. 2011, 29, 3072–3077. [Google Scholar] [CrossRef] [Green Version]
- Wänman, J.; Jernberg, J.; Gustafsson, P.; Abul-Kasim, K.; Grabowski, P.; Bobinski, L.; Crnalic, S. Predictive Value of the Spinal Instability Neoplastic Score for Survival and Ambulatory Function After Surgery for Metastatic Spinal Cord Compression in 110 Patients with Prostate Cancer. Spine Phila Pa 1976 2021, 46, 550–558. [Google Scholar] [CrossRef]
- Hoskin, P.J.; Hopkins, K.; Misra, V.; Holt, T.; McMenemin, R.; Dubois, D.; McKinna, F.; Foran, B.; Madhavan, K.; MacGregor, C.; et al. Effect of Single-Fraction vs Multifraction Radiotherapy on Ambulatory Status Among Patients with Spinal Canal Compression from Metastatic Cancer: The SCORAD Randomized Clinical Trial. JAMA 2019, 322, 2084–2094. [Google Scholar] [CrossRef] [PubMed]

| Factor | Post-Radiotherapy Ambulatory Rate (%) | p-Value |
|---|---|---|
| Age | ||
| ≤67 years (n = 146) | 73 | 0.82 |
| >67 years (n = 137) | 75 | |
| Gender | ||
| Female (n = 108) | 75 | 0.73 |
| Male (n = 175) | 73 | |
| ECOG performance score | ||
| 1–2 (n = 119) | 95 | <0.0001 |
| 3–4 (n = 164) | 59 | |
| Primary tumor type | ||
| Breast cancer (n = 52) | 87 | 0.002 |
| Prostate cancer (n = 49) | 74 | |
| Myeloma/lymphoma (n = 30) | 87 | |
| Non-small-cell lung cancer (n = 59) | 73 | |
| Small-cell lung cancer (n = 13) | 92 | |
| Cancer of unknown primary (n = 23) | 65 | |
| Renal cell carcinoma (n = 11) | 82 | |
| Colorectal cancer (n = 10) | 40 | |
| Other tumor types (n = 36) | 53 | |
| Interval tumor diagnosis to MSCC | ||
| ≤6 months (n = 143) | 75 | 0.71 |
| >6 months (n = 140) | 73 | |
| Number of affected vertebrae | ||
| 1–2 (n = 162) | 78 | 0.044 |
| ≥3 (n = 121) | 68 | |
| Visceral metastases | ||
| No (n = 110) | 78 | 0.19 |
| Yes (n = 173) | 71 | |
| Other bone metastases | ||
| No (n = 44) | 68 | 0.35 |
| Yes (n = 239) | 75 | |
| Time developing motor deficits | ||
| 0–7 days (n = 99) | 58 | <0.0001 |
| >7 days (n = 184) | 83 | |
| Pre-radiotherapy ambulatory status | ||
| Ambulatory without aid (n = 82) | 99 | <0.0001 |
| Ambulatory with aid (n = 99) | 91 | |
| Not ambulatory (n = 102) | 37 | |
| Pre-radiotherapy sensory deficits * | ||
| No (n = 144) | 90 | <0.0001 |
| Yes (n = 135) | 58 | |
| Pre-radiotherapy sphincter dysfunction ** | ||
| No (n = 219) | 86 | <0.0001 |
| Yes (n = 63) | 32 | |
| Radiotherapy regimen | ||
| 5 × 4 Gy (n = 97) | 68 | 0.002 |
| 10 × 3/5 × 5 Gy (n = 136) | 71 | |
| >40 Gy (n = 50) | 94 |
| Factor | Odds Ratio Estimate | 95% Confidence Limits | p-Value |
|---|---|---|---|
| Primary Tumor Type | |||
| Breast cancer vs. NSCLC | 3.00 | 0.71–12.62 | 0.036 |
| Prostate cancer vs. NSCLC | 7.57 | 1.78–32.12 | |
| Myeloma/lymphoma vs. NSCLC | 21.35 | 3.53–129.11 | |
| Small-cell lung cancer vs. NSCLC | 3.28 | 0.29–36.84 | |
| Cancer of unknown primary vs. NSCLC | 4.13 | 0.84–20.43 | |
| Renal cell carcinoma vs. NSCLC | 2.99 | 0.26–34.78 | |
| Colorectal cancer vs. NSCLC | 0.85 | 0.09–7.60 | |
| Other tumor types vs. NSCLC | 1.48 | 0.39–5.67 | |
| Pre-radiotherapy ambulatory status | |||
| Ambulatory without aid vs. no ambulatory | 102.20 | 12.18–857.32 | <0.0001 |
| Ambulatory with aid vs. no ambulatory | 12.23 | 4.72–31.72 | |
| Pre-radiotherapy sensory deficits | |||
| No vs. yes | 4.14 | 1.56–11.00 | 0.004 |
| Pre-radiotherapy sphincter dysfunction | |||
| No vs. yes | 4.07 | 1.44–11.46 | 0.008 |
| Factor | Post-Radiotherapy Ambulatory Rate (%) | Scoring Points |
|---|---|---|
| Primary Tumor Type | ||
| Breast cancer | 87 | 9 |
| Prostate cancer | 74 | 7 |
| Myeloma/lymphoma | 87 | 9 |
| Non-small-cell lung cancer | 73 | 7 |
| Small-cell lung cancer | 92 | 9 |
| Cancer of unknown primary | 65 | 7 |
| Renal cell carcinoma | 82 | 8 |
| Colorectal cancer | 40 | 4 |
| Other tumor types | 53 | 5 |
| Pre-radiotherapy ambulatory status | ||
| Ambulatory without aid | 99 | 10 |
| Ambulatory with aid | 91 | 9 |
| Not ambulatory | 37 | 4 |
| Pre-radiotherapy sensory deficits | ||
| No | 90 | 9 |
| Yes | 58 | 6 |
| Pre-radiotherapy sphincter dysfunction | ||
| No | 86 | 9 |
| Yes | 32 | 3 |
| Factor | Number of Patients | Proportion (%) |
|---|---|---|
| Age | ||
| ≤67 years | 146 | 52 |
| >67 years | 137 | 48 |
| Gender | ||
| Female | 108 | 38 |
| Male | 175 | 62 |
| ECOG performance score | ||
| 1–2 | 119 | 42 |
| 3–4 | 164 | 58 |
| Primary tumor type | ||
| Breast cancer | 52 | 18 |
| Prostate cancer | 49 | 17 |
| Myeloma/lymphoma | 30 | 11 |
| Non-small-cell lung cancer | 59 | 21 |
| Small-cell lung cancer | 13 | 5 |
| Cancer of unknown primary | 23 | 8 |
| Renal cell carcinoma | 11 | 4 |
| Colorectal cancer | 10 | 4 |
| Other tumor types | 36 | 13 |
| Interval tumor diagnosis to MSCC | ||
| ≤6 months | 143 | 51 |
| >6 months | 140 | 49 |
| Number of affected vertebrae | ||
| 1–2 | 162 | 57 |
| ≥3 | 121 | 43 |
| Visceral metastases | ||
| No | 110 | 39 |
| Yes | 173 | 61 |
| Other bone metastases | ||
| No | 44 | 16 |
| Yes | 239 | 84 |
| Time developing motor deficits | ||
| 0–7 days | 99 | 35 |
| >7 days | 184 | 65 |
| Pre-radiotherapy ambulatory status | ||
| Ambulatory without aid | 82 | 29 |
| Ambulatory with aid | 99 | 35 |
| Not ambulatory | 102 | 36 |
| Pre-radiotherapy sensory deficits | ||
| No | 144 | 51 |
| Yes | 135 | 48 |
| Unknown | 4 | 1 |
| Pre-radiotherapy sphincter dysfunction | ||
| No | 219 | 77 |
| Yes | 63 | 22 |
| Unknown | 1 | <1 |
| Radiotherapy regimen | ||
| 5 × 4 Gy | 97 | 34 |
| 10 × 3/5 × 5 Gy | 136 | 48 |
| >40 Gy | 50 | 18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rades, D.; Al-Salool, A.; Staackmann, C.; Cremers, F.; Cacicedo, J.; Lomidze, D.; Segedin, B.; Groselj, B.; Jankarashvili, N.; Conde-Moreno, A.J.; et al. A New Clinical Instrument for Estimating the Ambulatory Status after Irradiation for Malignant Spinal Cord Compression. Cancers 2022, 14, 3827. https://doi.org/10.3390/cancers14153827
Rades D, Al-Salool A, Staackmann C, Cremers F, Cacicedo J, Lomidze D, Segedin B, Groselj B, Jankarashvili N, Conde-Moreno AJ, et al. A New Clinical Instrument for Estimating the Ambulatory Status after Irradiation for Malignant Spinal Cord Compression. Cancers. 2022; 14(15):3827. https://doi.org/10.3390/cancers14153827
Chicago/Turabian StyleRades, Dirk, Ahmed Al-Salool, Christian Staackmann, Florian Cremers, Jon Cacicedo, Darejan Lomidze, Barbara Segedin, Blaz Groselj, Natalia Jankarashvili, Antonio J. Conde-Moreno, and et al. 2022. "A New Clinical Instrument for Estimating the Ambulatory Status after Irradiation for Malignant Spinal Cord Compression" Cancers 14, no. 15: 3827. https://doi.org/10.3390/cancers14153827
APA StyleRades, D., Al-Salool, A., Staackmann, C., Cremers, F., Cacicedo, J., Lomidze, D., Segedin, B., Groselj, B., Jankarashvili, N., Conde-Moreno, A. J., Ciervide, R., Kristiansen, C., & Schild, S. E. (2022). A New Clinical Instrument for Estimating the Ambulatory Status after Irradiation for Malignant Spinal Cord Compression. Cancers, 14(15), 3827. https://doi.org/10.3390/cancers14153827







