Holistic Approach to the Diagnosis and Treatment of Patients with Tumor Metastases to the Spine
Abstract
:Simple Summary
Abstract
1. Introduction
2. Scales Assessing the Severity of the Disease, Algorithms Setting Out Treatment Strategies, and Qualifications for the Surgical Treatment
3. Diagnostics
3.1. Imaging
3.1.1. X-ray Examination
3.1.2. Magnetic Resonance Imaging (MRI)
3.1.3. Computed Tomography (CT)
3.1.4. Bone Scintigraphy
3.2. Invasive Diagnostics—Biopsy
4. The Ways of the Surgical Treatment
5. Radiotherapy
6. Other Ways of Treatment
7. Therapeutic Perspectives
8. Prognosis
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chi, J.H.; Bydon, A.; Hsieh, P.; Witham, T.; Wolinsky, J.P.; Gokaslan, Z.L. Epidemiology and demographics for primary vertebral tumors. Neurosurg. Clin. N. Am. 2008, 19, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Maccauro, G.; Spinelli, M.S.; Mauro, S.; Perisano, C.; Graci, C.; Rosa, M.A. Physiopathology of spine metastasis. Int. J. Surg. Oncol. 2011, 2011, 107969. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Youk, T.; Lee, S.J.; Kim, K.M.; Vajdic, C.M. Bone metastasis and skeletal-related events in patients with solid cancer: A Korean nationwide health insurance database study. PLoS ONE 2020, 15, e0234927. [Google Scholar] [CrossRef] [PubMed]
- Phanphaisarn, A.; Patumanond, J.; Settakorn, J.; Chaiyawat, P.; Klangjorhor, J.; Pruksakorn, D. Prevalence and Survival Patterns of Patients with Bone Metastasis from Common Cancers in Thailand. Asian Pac. J. Cancer Prev. 2016, 17, 4335–4340. [Google Scholar]
- Lorkowski, J.; Grzegorowska, O.; Kozień, M.S.; Kotela, I. Effects of Breast and Prostate Cancer Metastases on Lumbar Spine Biomechanics: Rapid In Silico Evaluation. Adv. Exp. Med. Biol. 2018, 1096, 31–39. [Google Scholar] [CrossRef]
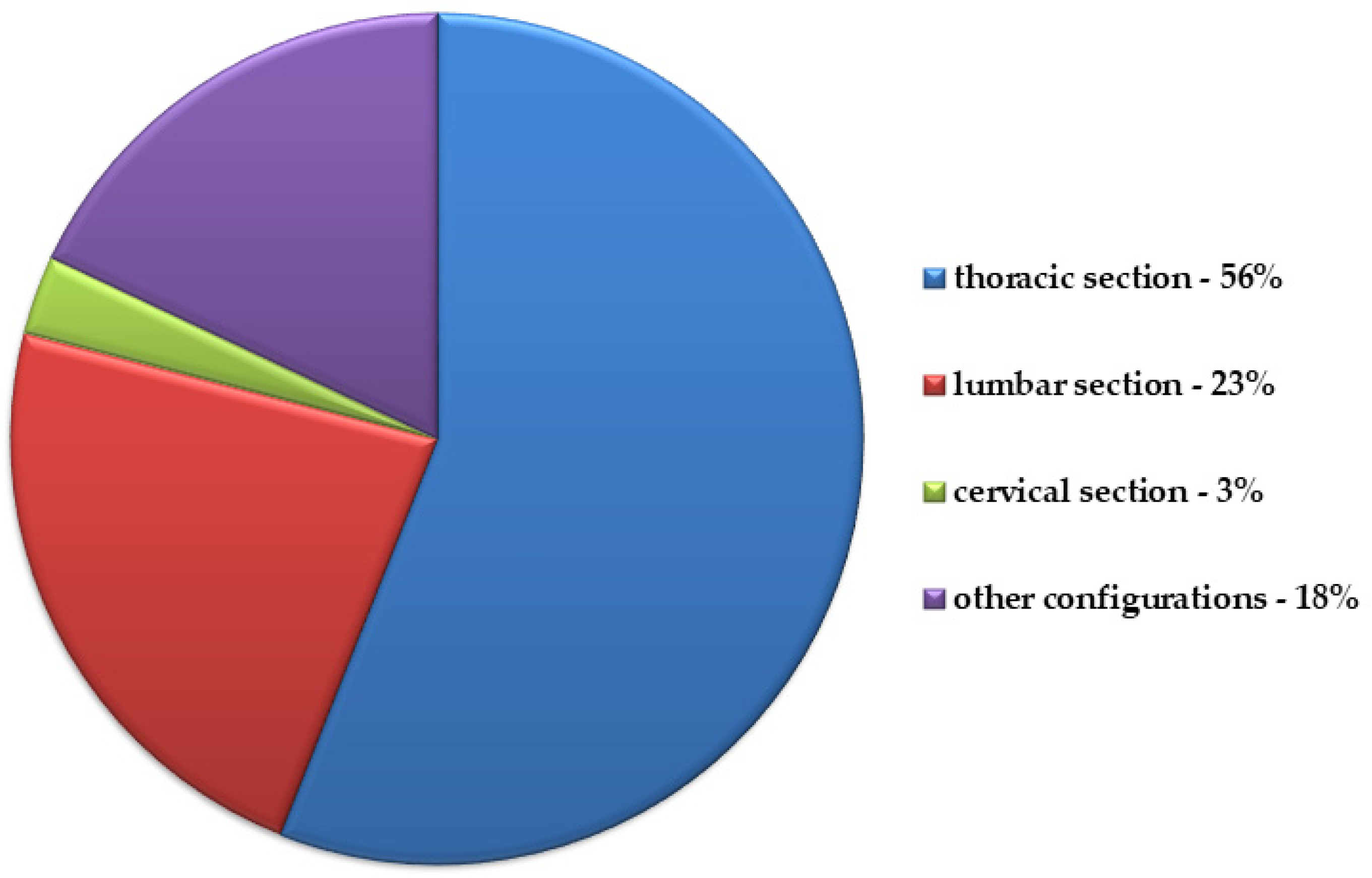
- Guzik, G. Current Incidence of Different Morphological Types of Malignant Metastases to the Spine Based on Magnetic Resonance Imaging. Ortop. Traumatol. Rehabil. 2017, 19, 137–144. [Google Scholar] [CrossRef]
- Gilbert, R.W.; Kim, J.H.; Posner, J.B. Epidural spinal cord compression from metastatic tumor: Diagnosis and treatment. Ann. Neurol. 1978, 3, 40–51. [Google Scholar] [CrossRef]
- Fornetti, J.; Welm, A.L.; Stewart, S.A. Understanding the Bone in Cancer Metastasis. J. Bone Miner. Res. 2018, 33, 2099–2113. [Google Scholar] [CrossRef] [Green Version]
- Yin, J.J.; Pollock, C.B.; Kelly, K. Mechanisms of cancer metastasis to the bone. Cell Res. 2005, 15, 57–62. [Google Scholar] [CrossRef]
- Ritchie, C.K.; Andrews, L.R.; Thomas, K.G.; Tindall, D.J.; Fitzpatrick, L.A. The effects of growth factors associated with osteoblasts on prostate carcinoma proliferation and chemotaxis: Implications for the development of metastatic disease. Endocrinology 1997, 138, 1145–1150. [Google Scholar] [CrossRef]
- Lin, S.C.; Yu-Lee, L.Y.; Lin, S.H. Osteoblastic Factors in Prostate Cancer Bone Metastasis. Curr. Osteoporos. Rep. 2018, 16, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, W.B.; Perrin, R.G. Evaluation and treatment of spinal metastases: An overview. Neurosurg. Focus 2001, 11, e10. [Google Scholar] [CrossRef] [Green Version]
- Ecker, R.D.; Endo, T.; Wetjen, N.M.; Krauss, W.E. Diagnosis and treatment of vertebral column metastases. Mayo Clin. Proc. 2005, 80, 1177–1186. [Google Scholar] [CrossRef] [Green Version]
- Vialle, L.R.; Gokaslan, Z.L.; Boriani, S.; Fisher, C.G. Metastatic Spinal Tumors; AOSpine Masters Series; Thieme Medical Publishers: New York, NY, USA, 2015; Volume 1. [Google Scholar]
- Yasui, H.; Ozawa, N.; Mikami, S.; Shimizu, K.; Hatta, T.; Makino, N.; Fukushima, M.; Baba, S.; Makino, Y. Spinal Cord Ischemia Secondary to Epidural Metastasis from Small Cell Lung Carcinoma. Am. J. Case Rep. 2017, 18, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Eleraky, M.; Setzer, M.; Vrionis, F.D. Posterior transpedicular corpectomy for malignant cervical spine tumors. Eur. Spine J. 2010, 19, 257–262. [Google Scholar] [CrossRef] [Green Version]
- Clausen, C. Preoperative embolization in surgical treatment of metastatic spinal cord compression. Dan. Med. J. 2017, 64, B5393. [Google Scholar] [PubMed]
- Boussios, S.; Cooke, D.; Hayward, C.; Kanellos, F.S.; Tsiouris, A.K.; Chatziantoniou, A.A.; Zakynthinakis-Kyriakou, N.; Karathanasi, A. Metastatic Spinal Cord Compression: Unraveling the Diagnostic and Therapeutic Challenges. Anticancer. Res. 2018, 38, 4987–4997. [Google Scholar] [CrossRef] [Green Version]
- Curtin, M.; Piggott, R.P.; Murphy, E.P.; Munigangaiah, S.; Baker, J.F.; McCabe, J.P.; Devitt, A. Spinal Metastatic Disease: A Review of the Role of the Multidisciplinary Team. Orthop. Surg. 2017, 9, 145–151. [Google Scholar] [CrossRef] [Green Version]
- Péus, D.; Newcomb, N.; Hofer, S. Appraisal of the Karnofsky Performance Status and proposal of a simple algorithmic system for its evaluation. BMC Med. Inform. Decis. Mak. 2013, 13, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ASA Physical Status Classification System Committee of Oversight: Economics, guidelines of the American Society of Anesthesiologists. 2014, Revision from 2020. Available online: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system (accessed on 27 December 2020).
- Gasbarrini, A.; Cappuccio, M.; Mirabile, L.; Bandiera, S.; Terzi, S.; Barbanti Bròdano, G.; Boriani, S. Spinal metastases: Treatment evaluation algorithm. Eur. Rev. Med. Pharmacol. Sci. 2004, 8, 265–274. [Google Scholar]
- Frankel, H.L.; Hancock, D.O.; Hyslop, G.; Melzak, J.; Michaelis, L.S.; Ungar, G.H.; Vernon, J.D.; Walsh, J.J. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Spinal Cord 1969, 7, 179–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazurkiewicz, T. Surgical management of bone metastases of the spine. Ortho Trauma 2006, 1, 17–23. [Google Scholar]
- Roberts, T.T.; Leonard, G.R.; Cepela, D.J. Classifications in Brief: American Spinal Injury Association (ASIA) Impairment Scale. Clin. Orthop. Relat. Res. 2017, 475, 1499–1504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of Digital Visual Analog Scale Pain Scoring with a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef] [PubMed]
- Fox, S.; Spiess, M.; Hnenny, L.; Fourney, D.R. Spinal Instability Neoplastic Score (SINS): Reliability Among Spine Fellows and Resident Physicians in Orthopedic Surgery and Neurosurgery. Glob. Spine J. 2017, 7, 744–748. [Google Scholar] [CrossRef]
- Fisher, C.G.; DiPaola, C.P.; Ryken, T.C.; Bilsky, M.H.; Shaffrey, C.I.; Berven, S.H.; Harrop, J.S.; Fehlings, M.G.; Boriani, S.; Chou, D.; et al. A novel classification system for spinal instability in neoplastic disease: An evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine 2010, 35, E1221–E1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeWald, R.L.; Bridwell, K.H.; Prodromas, C.; Rodts, M.F. Reconstructive spinal surgery as palliation for metastatic malignancies of the spine. Spine 1985, 10, 21–26. [Google Scholar] [CrossRef]
- Tomita, K.; Kawahara, N.; Murakami, H.; Demura, S. Total en bloc spondylectomy for spinal tumors: Improvement of the technique and its associated basic background. J. Orthop. Sci. 2006, 11, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Bilsky, M.H.; Laufer, I.; Fourney, D.R.; Groff, M.; Schmidt, M.H.; Varga, P.P.; Vrionis, F.D.; Yamada, Y.; Gerszten, P.C.; Kuklo, T.R. Reliability analysis of the epidural spinal cord compression scale. J. Neurosurg. Spine 2010, 13, 324–328. [Google Scholar] [CrossRef]
- Quraishi, N.A.; Arealis, G.; Salem, K.M.; Purushothamdas, S.; Edwards, K.L.; Boszczyk, B.M. The surgical management of metastatic spinal tumors based on an Epidural Spinal Cord Compression (ESCC) scale. Spine J. 2015, 15, 1738–1743. [Google Scholar] [CrossRef]
- Boriani, S.; Weinstein, J.N.; Biagini, R. Primary bone tumors of the spine. Terminology and surgical staging. Spine 1997, 22, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Patt, J.C.; Leas, D.P. Spinal Instability in Metastatic Disease. In Metastatic Spine Disease; Marco, R.A.W., Ed.; Springer: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Tokuhashi, Y.; Uei, H.; Oshima, M.; Ajiro, Y. Scoring system for prediction of metastatic spine tumor prognosis. World J. Orthop. 2014, 5, 262–271. [Google Scholar] [CrossRef]
- Tokuhashi, Y.; Matsuzaki, H.; Oda, H.; Oshima, M.; Ryu, J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine 2005, 30, 2186–2191. [Google Scholar] [CrossRef] [PubMed]
- Tomita, K.; Kawahara, N.; Kobayashi, T.; Yoshida, A.; Murakami, H.; Akamaru, T. Surgical strategy for spinal metastases. Spine 2001, 26, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Barzilai, O.; Fisher, C.G.; Bilsky, M.H. State of the Art Treatment of Spinal Metastatic Disease. Neurosurgery 2018, 82, 757–769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laufer, I.; Rubin, D.G.; Lis, E.; Cox, B.W.; Stubblefield, M.D.; Yamada, Y.; Bilsky, M.H. The NOMS framework: Approach to the treatment of spinal metastatic tumors. Oncologist 2013, 18, 744–751. [Google Scholar] [CrossRef] [Green Version]
- Wald, J.T. Imaging of spine neoplasm. Radiol. Clin. N. Am. 2012, 50, 749–776. [Google Scholar] [CrossRef]
- Hur, J.; Yoon, C.S.; Ryu, Y.H.; Yun, M.J.; Suh, J.S. Comparative study of fluorodeoxyglucose positron emission tomography and magnetic resonance imaging for the detection of spinal bone marrow infiltration in untreated patients with multiple myeloma. Acta Radiol. 2008, 49, 427–435. [Google Scholar] [CrossRef]
- Ridley, L.J.; Han, J.; Ridley, W.E.; Xiang, H. Winking owl sign: Unilateral absent pedicle. J. Med. Imaging Radiat. Oncol. 2018, 62 (Suppl. 1), 168. [Google Scholar] [CrossRef] [Green Version]
- Guillevin, R.; Vallee, J.N.; Lafitte, F.; Menuel, C.; Duverneuil, N.M.; Chiras, J. Spine metastasis imaging: Review of the literature. J. Neuroradiol. 2007, 34, 311–321. [Google Scholar] [CrossRef]
- Leake, R.L.; Mills, M.K.; Hanrahan, C.J. Spinal Marrow Imaging: Clues to Disease. Radiol. Clin. N. Am. 2019, 57, 359–375. [Google Scholar] [CrossRef] [PubMed]
- Pinter, N.K.; Pfiffner, T.J.; Mechtler, L.L. Neuroimaging of spine tumors. Handb. Clin. Neurol. 2016, 136, 689–706. [Google Scholar] [CrossRef] [PubMed]
- Shah, L.M.; Salzman, K.L. Imaging of spinal metastatic disease. Int. J. Surg. Oncol. 2011, 2011, 769753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, M.; Sequeiros, R.B.; Xu, Y.; He, X.; Zhu, T.; Li, L.; Lü, Y.; Huang, J.; Li, C. MRI-guided percutaneous transpedicular biopsy of thoracic and lumbar spine using a 0.23t scanner with optical instrument tracking. J. Magn. Reson. Imaging 2015, 42, 1740–1746. [Google Scholar] [CrossRef] [PubMed]
- Santiago, F.R.; Kelekis, A.; Alvarez, L.G.; Filippiadis, D.K. Interventional procedures of the spine. Semin Musculoskelet. Radiol. 2014, 18, 309–317. [Google Scholar] [CrossRef]
- Akhtar, I.; Manucha, V. Rapid On-site Evaluation of Spine Lesions. Neuroimaging Clin. N. Am. 2019, 29, 635–642. [Google Scholar] [CrossRef]
- Nourbakhsh, A.; Grady, J.J.; Garges, K.J. Percutaneous spine biopsy: A meta-analysis. J. Bone Jt. Surg. Am. 2008, 90, 1722–1725. [Google Scholar] [CrossRef]
- Guzik, G. Surgical Treatment in Patients with Spinal Tumors—Differences in Surgical Strategies and Malignancy-Associated Problems. An Analysis of 474 Patients. Ortop. Traumatol. Rehabil. 2015, 17, 229–240. [Google Scholar] [CrossRef]
- Guo, Q.; Cui, Y.; Wang, L.; Lu, X.; Ni, B. Single anterior approach for cervical spine fractures at C5-T1 complicating ankylosing spondylitis. Clin. Neurol. Neurosurg. 2016, 147, 1–5. [Google Scholar] [CrossRef]
- Kumar, N.; Tan, B.; Zaw, A.S.; Khine, H.E.; Maharajan, K.; Lau, L.L.; Rajendran, P.C.; Gopinathan, A. The role of preoperative vascular embolization in surgery for metastatic spinal tumours. Eur. Spine J. 2016, 25, 3962–3970. [Google Scholar] [CrossRef]
- Yang, B.; Lu, T.; Li, H. Single-Session Combined Anterior-Posterior Approach for Treatment of Ankylosing Spondylitis with Obvious Displaced Lower Cervical Spine Fractures and Dislocations. Biomed Res. Int. 2017, 2017, 9205834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, A.; Xie, D.; Cai, X.; Qu, B.; Kong, Q.; Xu, C.; Yang, L.; Chen, X.; Jia, L. One-stage surgical treatment of cervical spine fracture-dislocation in patients with ankylosing spondylitis via the combined anterior-posterior approach. Medicine 2017, 96, e7432. [Google Scholar] [CrossRef]
- Novegno, F.; Granaroli, P.; Ciccoritti, L.; Lunardi, P.; Fraioli, M.F. Chylous fistula: Management of a rare complication following right anterior cervical spine approach. Eur. Spine J. 2019, 28 (Suppl. 2), 61–67. [Google Scholar] [CrossRef]
- Cole, J.S.; Patchell, R.A. Metastatic epidural spinal cord compression. Lancet Neurol. 2008, 7, 459–466. [Google Scholar] [CrossRef]
- Shan, J.; Jiang, H.; Ren, D.; Wang, C. Anatomic Relationship Between Right Recurrent Laryngeal Nerve and Cervical Fascia and Its Application Significance in Anterior Cervical Spine Surgical Approach. Spine 2017, 42, E443–E447. [Google Scholar] [CrossRef] [PubMed]
- Harel, R.; Stylianou, P.; Knoller, N. Cervical Spine Surgery: Approach-Related Complications. World Neurosurg. 2016, 94, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, M.P.; Mekhail, A.; Benzel, E.C. Management of metastatic tumors of the spine: Strategies and operative indications. Neurosurg. Focus 2001, 11, e2. [Google Scholar] [CrossRef]
- Cheung, K.M.; Mak, K.C.; Luk, K.D. Anterior approach to cervical spine. Spine 2012, 37, E297–E302. [Google Scholar] [CrossRef] [Green Version]
- Prezerakos, G.K.; Sayal, P.; Kourliouros, A.; Pericleous, P.; Ladas, G.; Casey, A. Paravertebral tumours of the cervicothoracic junction extending into the mediastinum: Surgical strategies in a no man’s land. Eur. Spine J. 2018, 27, 902–912. [Google Scholar] [CrossRef]
- Joubert, C.; Adetchessi, T.; Peltier, E.; Graillon, T.; Dufour, H.; Blondel, B.; Fuentes, S. Corpectomy and Vertebral Body Reconstruction with Expandable Cage Placement and Osteosynthesis via the single stage Posterior Approach: A Retrospective Series of 34 Patients with Thoracic and Lumbar Spine Vertebral Body Tumors. World Neurosurg. 2015, 84, 1412–1422. [Google Scholar] [CrossRef]
- Abduljabbar, F.H.; Teles, A.R.; Bokhari, R.; Weber, M.; Santaguida, C. Laminectomy with or Without Fusion to Manage Degenerative Cervical Myelopathy. Neurosurg. Clin. N. Am. 2018, 29, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Chaichana, K.L.; Sciubba, D.M.; Li, K.W.; Gokaslan, Z.L. Surgical management of thoracic spinal cord herniation: Technical consideration. J. Spinal Disord. Tech. 2009, 22, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Lubelski, D.; Abdullah, K.G.; Steinmetz, M.P.; Masters, F.; Benzel, E.C.; Mroz, T.E.; Shin, J.H. Lateral extracavitary, costotransversectomy, and transthoracic thoracotomy approaches to the thoracic spine: Review of techniques and complications. J. Spinal Disord. Tech. 2013, 26, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Teng, H.; Xinghai, Y.; Wei, H.; Huang, Q.; Xiao, J.; Zhang, C. Malignant fibrous histiocytoma of the spine: A series of 13 clinical case reports and review of 17 published cases. Spine 2011, 36, E1453–E1462. [Google Scholar] [CrossRef] [PubMed]
- Howell, E.P.; Williamson, T.; Karikari, I.; Abd-El-Barr, M.; Erickson, M.; Goodwin, M.L.; Reynolds, J.; Sciubba, D.M.; Goodwin, C.R. Total en bloc resection of primary and metastatic spine tumors. Ann. Transl. Med. 2019, 7, 226. [Google Scholar] [CrossRef]
- Kato, S.; Demura, S.; Shinmura, K.; Yokogawa, N.; Yonezawa, N.; Shimizu, T.; Oku, N.; Kitagawa, R.; Murakami, H.; Kawahara, N.; et al. Clinical outcomes and survivals after total en bloc spondylectomy for metastatic leiomyosarcoma in the spine. Eur. Spine J. 2020, 29, 3237–3244. [Google Scholar] [CrossRef]
- Shimizu, T.; Murakami, H.; Sangsin, A.; Demura, S.; Kato, S.; Shinmura, K.; Yokogawa, N.; Oku, N.; Kitagawa, R.; Tsuchiya, H. En bloc corpectomy for late gastrointestinal stromal tumor metastasis: A case report and review of the literature. J. Med. Case Rep. 2018, 12, 300. [Google Scholar] [CrossRef]
- Guzik, G. Outcomes of Corpectomy in Patients with Metastatic Cancer. Ortop. Traumatol. Rehabil. 2017, 19, 23–32. [Google Scholar] [CrossRef]
- Meyer, S.A.; Singh, H.; Jenkins, A.L. Surgical treatment of metastatic spinal tumors. Mt. Sinai J. Med. 2010, 77, 124–129. [Google Scholar] [CrossRef]
- Holman, P.J.; Suki, D.; McCutcheon, I.; Wolinsky, J.P.; Rhines, L.D.; Gokaslan, Z.L. Surgical management of metastatic disease of the lumbar spine: Experience with 139 patients. J. Neurosurg. Spine 2005, 2, 550–563. [Google Scholar] [CrossRef]
- Georgy, B.A. Metastatic spinal lesions: State-of-the-art treatment options and future trends. AJNR Am. J. Neuroradiol. 2008, 29, 1605–1611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boucher, H.H. A method of spinal fusion. J. Bone Jt. Surg. Br. 1959, 41-B, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Vieweg, U.; van Roost, D.; Wolf, H.K.; Schyma, C.A.; Schramm, J. Corrosion on an Internal Spinal Fixator System. Spine 1999, 24, 946–951. [Google Scholar] [CrossRef] [PubMed]
- Lonstein, J.E.; Denis, F.; Perra, J.H.; Pinto, M.R.; Smith, M.D.; Winter, R.B. Complications associated with pedicle screws. J. Bone Jt. Surg. Am. 1999, 81, 1519–1528. [Google Scholar] [CrossRef]
- Ringel, F.; Ryang, Y.M.; Kirschke, J.S.; Müller, B.S.; Wilkens, J.J.; Brodard, J.; Combs, S.E.; Meyer, B. Radiolucent Carbon Fiber-Reinforced Pedicle Screws for Treatment of Spinal Tumors: Advantages for Radiation Planning and Follow-up Imaging. World Neurosurg. 2017, 105, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Facchini, G.; Di Tullio, P.; Battaglia, M.; Bartalena, T.; Tetta, C.; Errani, C.; Mavrogenis, A.F.; Rossi, G. Palliative embolization for metastases of the spine. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 247–252. [Google Scholar] [CrossRef]
- Clausen, C.; Dahl, B.; Frevert, S.C.; Hansen, L.V.; Nielsen, M.B.; Lönn, L. Preoperative embolization in surgical treatment of spinal metastases: Single-blind, randomized controlled clinical trial of efficacy in decreasing intraoperative blood loss. J. Vasc. Interv. Radiol. 2015, 26, 402–412.e1. [Google Scholar] [CrossRef]
- Geraets, S.E.W.; Bos, P.K.; van der Stok, J. Preoperative embolization in surgical treatment of long bone metastasis: A systematic literature review. EFORT Open Rev. 2020, 5, 17–25. [Google Scholar] [CrossRef]
- Houten, J.K.; Swiggett, S.J.; Hadid, B.; Choueka, D.M.; Kinon, M.D.; Buciuc, R.; Zumofen, D.W. Neurologic Complications of Preoperative Embolization of Spinal Metastasis: A Systemic Review of the Literature Identifying Distinct Mechanisms of Injury. World Neurosurg. 2020, 143, 374–388. [Google Scholar] [CrossRef]
- Winkler, E.A.; Rowland, N.C.; Yue, J.K.; Birk, H.; Ozpinar, A.; Tay, B.; Ames, C.P.; Mummaneni, P.V.; El-Sayed, I.H. A Tunneled Subcricoid Approach for Anterior Cervical Spine Reoperation: Technical and Safety Results. World Neurosurg. 2016, 86, 328–335. [Google Scholar] [CrossRef]
- Behnke, N.K.; Baker, D.K.; Xu, S.; Niemeier, T.E.; Watson, S.L.; Ponce, B.A. Risk factors for same-admission mortality after pathologic fracture secondary to metastatic cancer. Support. Care Cancer 2017, 25, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Aebi, M. Spinal metastasis in the elderly. Eur. Spine J. 2003, 12 (Suppl. 2), S202–S213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polly, D.W., Jr.; Chou, D.; Sembrano, J.N.; Ledonio, C.G.; Tomita, K. An analysis of decision making and treatment in thoracolumbar metastases. Spine 2009, 34 (Suppl. 22), S118–S127. [Google Scholar] [CrossRef]
- Barzilai, O.; Robin, A.M.; O’Toole, J.E.; Laufer, I. Minimally Invasive Surgery Strategies: Changing the Treatment of Spine Tumors. Neurosurg. Clin. N. Am. 2020, 31, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.Y.; Wu, M.H.; Li, Y.Y.; Cheng, C.C.; Lee, C.Y.; Huang, T.J. Video-Assisted Thoracoscopic Surgery and Minimal Access Spinal Surgery Compared in Anterior Thoracic or Thoracolumbar Junctional Spinal Reconstruction: A Case-Control Study and Review of the Literature. Biomed Res. Int. 2016, 2016, 6808507. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.J.; Hsu, R.W.; Li, Y.Y.; Cheng, C.C. Minimal access spinal surgery (MASS) in treating thoracic spine metastasis. Spine 2006, 31, 1860–1863. [Google Scholar] [CrossRef]
- Gu, Y.; Dong, J.; Jiang, X.; Wang, Y. Minimally Invasive Pedicle Screws Fixation and Percutaneous Vertebroplasty for the Surgical Treatment of Thoracic Metastatic Tumors with Neurologic Compression. Spine 2016, 41 (Suppl. 19), B14–B22. [Google Scholar] [CrossRef]
- Barzilai, O.; DiStefano, N.; Lis, E.; Yamada, Y.; Lovelock, D.M.; Fontanella, A.N.; Bilsky, M.H.; Laufer, I. Safety and utility of kyphoplasty prior to spine stereotactic radiosurgery for metastatic tumors: A clinical and dosimetric analysis. J. Neurosurg. Spine 2018, 28, 72–78. [Google Scholar] [CrossRef]
- Yahanda, A.T.; Buchowski, J.M.; Wegner, A.M. Treatment, complications, and outcomes of metastatic disease of the spine: From Patchell to PROMIS. Ann. Transl. Med. 2019, 7, 216. [Google Scholar] [CrossRef] [Green Version]
- Ozdemir, Y.; Torun, N.; Guler, O.C.; Yildirim, B.A.; Besen, A.A.; Yetisken, A.G.; Onal, H.C.; Topkan, E. Local control and vertebral compression fractures following stereotactic body radiotherapy for spine metastases. J. Bone Oncol. 2019, 15, 100218. [Google Scholar] [CrossRef]
- Al Farii, H.; Frazer, A.; Farahdel, L.; Alfayez, S.; Weber, M. Zoledronic Acid Versus Denosumab for Prevention of Spinal Cord Compression in Advanced Cancers with Spine Metastasis: A Meta-Analysis of Randomized Controlled Trials. Glob. Spine J. 2020, 10, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, R. Neurologic complications of prostate cancer. Am. Fam. Physician 2002, 65, 1834–1840. [Google Scholar] [PubMed]
- Dong, P.; Chen, N.; Li, L.; Huang, R. An upper cervical cord compression secondary to occult follicular thyroid carcinoma metastases successfully treated with multiple radioiodine therapies: A clinical case report. Medicine 2017, 96, e8215. [Google Scholar] [CrossRef]
- Diaby, V.; Tawk, R.; Sanogo, V.; Xiao, H.; Montero, A.J. A review of systematic reviews of the cost-effectiveness of hormone therapy, chemotherapy, and targeted therapy for breast cancer. Breast Cancer Res. Treat. 2015, 151, 27–40. [Google Scholar] [CrossRef] [Green Version]
- Nader, R.; El Amm, J.; Aragon-Ching, J.B. Role of chemotherapy in prostate cancer. Asian J. Androl. 2018, 20, 221–229. [Google Scholar] [CrossRef]
- Coleman, R.; Body, J.J.; Aapro, M.; Hadji, P.; Herrstedt, J.; ESMO Guidelines Working Group. Bone health in cancer patients: ESMO Clinical Practice Guidelines. Ann. Oncol. 2014, 25 (Suppl. 3), iii124–iii137. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Park, S.J.; Lee, C.S. Incidence and prognosis of patients with spinal metastasis as the initial manifestation of malignancy: Analysis of 338 patients undergoing surgical treatment. Bone Jt. J. 2010, 101-B, 1379–1384. [Google Scholar] [CrossRef] [PubMed]
- Ejima, Y.; Matsuo, Y.; Sasaki, R. The current status and future of radiotherapy for spinal bone metastases. J. Orthop. Sci. 2015, 20, 585–592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kropczyński, G.; Gabriel, A.; Kusz, D.; Ryś, J.; Miszczyk, L.; Paściak, M. Influence of the type of neoplasm and treatment on the survival of patients with malignant spinal tumours. Ortop. Traumatol. Rehabil. 2009, 11, 27–36. [Google Scholar] [PubMed]
- Oh, M.C.; Kim, J.M.; Kaur, G.; Safaee, M.; Sun, M.Z.; Singh, A.; Aranda, D.; Molinaro, A.M.; Parsa, A.T. Prognosis by tumor location in adults with spinal ependymomas. J. Neurosurg. Spine 2013, 18, 226–235. [Google Scholar] [CrossRef]
- Gilbert, M.R.; Ruda, R.; Soffietti, R. Ependymomas in adults. Curr. Neurol. Neurosci. Rep. 2010, 10, 240–247. [Google Scholar] [CrossRef] [PubMed]

| Type of Spine Metastases | ||
|---|---|---|
| Osteoclastic | Osteoblastic | |
| Primary tumor | e.g., lungs, kidneys, multiple myeloma | e.g., prostate |
| Factors secreted by neoplasm cells | IL-1 IL-6 IL-8 IL-10 IL-11 TGF-α TGF-β PTHrP PgE2 TNF CSF-1 GM-CSF M-CSF VEGF EGF | ET-1 TGF-β PDGF BMP IGF FGF CXCL-1 uPA PSA |
| Factors released from the bone microenvironment | TGF-β | |
| FGF | ||
| IGF | ||
| BMP | ||
| PDGF | ||
| OPG | ||
| HGF | ||
| IL-6 | ||
| CTGF | ||
| M-CSF | ||
| VEGF | ||
| PTHrP activins | ||
| Scales Assessing the Severity of the Disease | |
|---|---|
| The Name of the Scale | What Does the Scale Evaluate? |
| The Karnofsky scale | functional patient’s condition |
| ASA Physical Status Classification System | operational risk |
| the Frankel scale, the American Spinal Injury Association Impairment Scale (AIS) | patient’s neurological condition |
| The Visual Analogue Scale (VAS) | pain assessment |
| Spinal Instability Neoplastic Score (SINS), De Wald scale, Tomita’s surgical classification, Harrington scale, epidural spinal cord compression scale (ESCC), Weinstain–Boriani–Biagini classification, Asdourian scale, Tomita scale, Tokuhashi scale | assessment neoplastic lesions, their advancement and localization in bone and ligamentous structures of the spine and the spinal canal |
| Tokuhashi scale, modified Bauer scale | predicted survival time of a patient with neoplastic metastases to the spine |
| Approach | Level of Spine | Description |
|---|---|---|
| anterior | the upper part of the cervical spine, craniospinal junction: the base of the skull, atlas (C1), and axis (C2) | through the posterior wall of the pharynx, mandibular (with or without cut of the mandible) |
| C3 to C7 | proposed by Clovard Smith and Robinson—in front of the anterior edge the sternocleidomastoid muscle | |
| thoracic vertebrae | the anterior approach to the thoracic vertebrae is complex from Th2 to Th5 due to the limitations of the sternum (the need for sternotomy) and to the Th10 to L1 thoracolumbar spine junction caused by diaphragm attachments (the need to connect the post-pleural and retroperitoneal entrances) | |
| lumbar shafts L1 to L4 | provided by retroperitoneal access; the peritoneal approach enables surgery in the L5 vertebrae and sacral segments | |
| peritoneal | L5 sacral segments | - |
| posterior | - | routinely used laminectomy, which makes way to open the vertebral canal and exposes posterior surface of spinal cord |
| lateral | - | laminectomy and total excision of pedicles of vertebral arch at the same time enable lateral approach to vertebral canal and show lateral surface of spinal cord (intrapedicular approach); the excision of the intervertebral joint and head of rib in thoracic spine expose lateral side of vertebral body (lateral approach—costotransversectomy and postpleural lateral approach) |
| posterolateral | - | the body of the thoracic vertebra can be visualized via a posterolateral thoracotomy |
| en block | - | tumor excision in one piece with margin of surrounding tissue; the character of metastatic tumor and localization in the spine rarely allows the use of this kind of resection; usually debulking is used, the aim is to remove the pressure of the spinal cord |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowak, H.; Szwacka, D.M.; Pater, M.; Mrugalski, W.K.; Milczarek, M.G.; Staniszewska, M.; Jankowski, R.; Barciszewska, A.-M. Holistic Approach to the Diagnosis and Treatment of Patients with Tumor Metastases to the Spine. Cancers 2022, 14, 3480. https://doi.org/10.3390/cancers14143480
Nowak H, Szwacka DM, Pater M, Mrugalski WK, Milczarek MG, Staniszewska M, Jankowski R, Barciszewska A-M. Holistic Approach to the Diagnosis and Treatment of Patients with Tumor Metastases to the Spine. Cancers. 2022; 14(14):3480. https://doi.org/10.3390/cancers14143480
Chicago/Turabian StyleNowak, Hanna, Dominika Maria Szwacka, Monika Pater, Wojciech Krzysztof Mrugalski, Michał Grzegorz Milczarek, Magdalena Staniszewska, Roman Jankowski, and Anna-Maria Barciszewska. 2022. "Holistic Approach to the Diagnosis and Treatment of Patients with Tumor Metastases to the Spine" Cancers 14, no. 14: 3480. https://doi.org/10.3390/cancers14143480
APA StyleNowak, H., Szwacka, D. M., Pater, M., Mrugalski, W. K., Milczarek, M. G., Staniszewska, M., Jankowski, R., & Barciszewska, A.-M. (2022). Holistic Approach to the Diagnosis and Treatment of Patients with Tumor Metastases to the Spine. Cancers, 14(14), 3480. https://doi.org/10.3390/cancers14143480







