Validation of “Self-Evaluation of Communication Experiences after Laryngectomy” (SECEL) Questionnaire for Spanish-Speaking Laryngectomized Patients
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
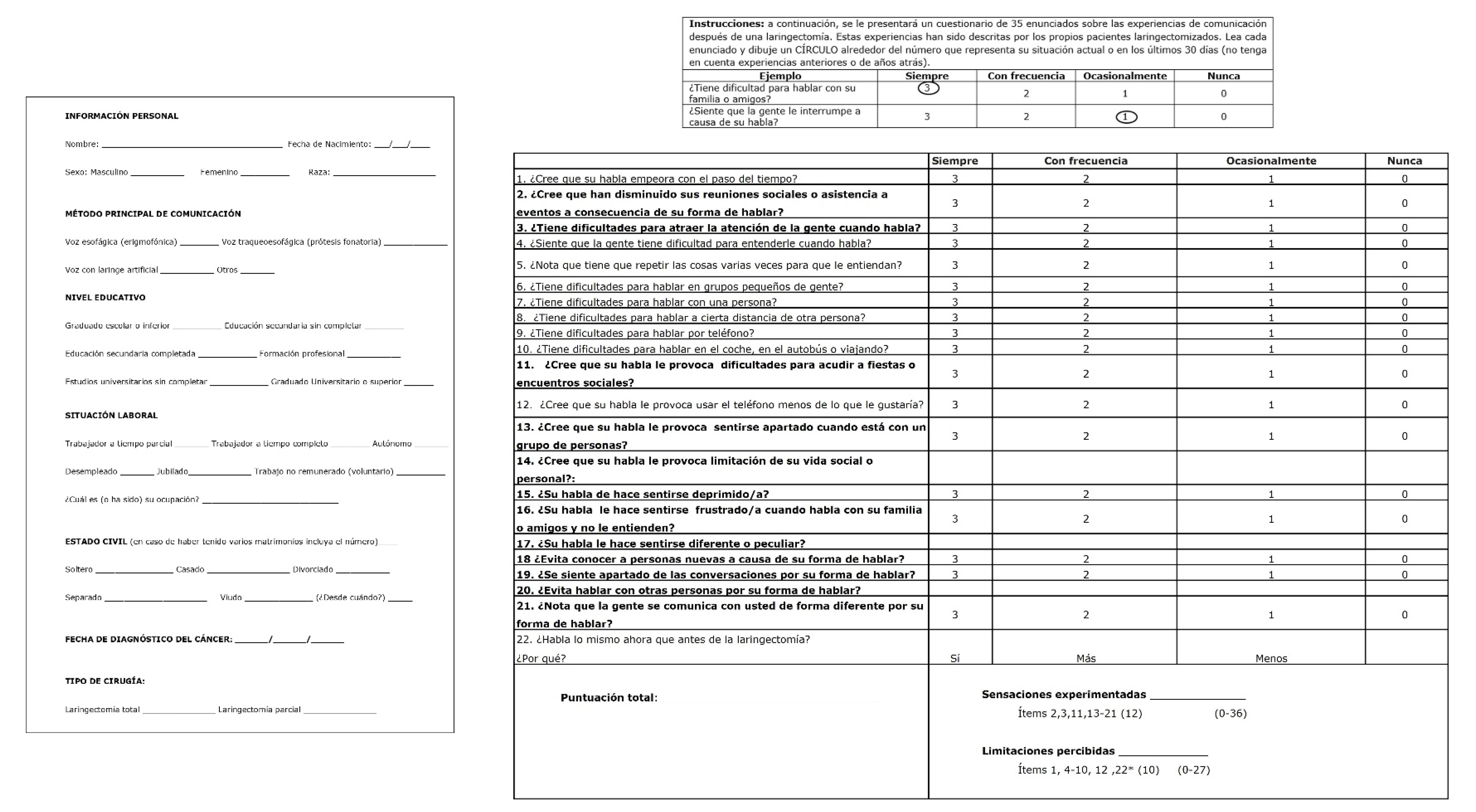
2.2. Translation and Cultural Adaptation
2.3. Measuring Instruments and Questionnaires
- -
- QLQ-H&N35 [8]: a self-administered questionnaire developed by EORTC to assess the perceived QoL in patients with head and neck cancer. It consists of 7 subscales with 35 items. Each item has a four-point scale (1: not at all, 2: a little bit 3: pretty much, 4: a lot). The scale score is transformed into a 0-to-100 scale and a high score on a symptom scale indicates a high symptom level. In this study, those patients who exceed the 75th percentile score are considered to have a poor QoL.
- -
- VHI-30 [9]: a self-administered questionnaire with 30 items divided into 3 subscales (Emotional, Functional and Physical) to assess voice disorders. Each item is scored from 0 to 5 (0: never, 1: hardly ever, 2: sometimes, 3: often, 4: always). According to the total score, four degrees of voice handicap are established, ranging from mild (0 to 30), moderate (31 to 60), severe (61 to 90) and grave (91 to 120).
- -
- HADS [21]: a self-administered mental health questionnaire developed for the detection and evaluation of mood disorders. It has 14 items divided into 2 subscales: Anxiety (HAD-A) and Depression (HAD-D). Patients rate each item on a 4-point scale (0–3), choosing the most representative number of their situation the week before. Scores > 11 in either of the subscales indicate probable psychological distress. Scores > 10 are considered indicative of morbidity. A score of 8–10 is interpreted as borderline or borderline case, and scores < 8 indicate the absence of significant morbidity.
2.4. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Validity Evidence Based on the Internal Structure and Reliability of Scale Score
3.3. Validity Evidence Based on the Relationship with Other Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brook, I. “The Laryngectomee Guide” is available in 18 languages (Free eBooks). World J. Otorhinolaryngol. Head Neck Surg. 2020, 7, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Morales-Puebla, J.M.; Morales-Puebla, A.F.; Jiménez-Antolín, J.A.; Muñoz-Platón, E.; Padilla-Parrado, M.; Chacón-Martínez, J. Olfactory rehabilitation after total laryngectomy. Acta Otorrinolaringol. Esp. 2010, 61, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Chaves, A.D.; Pernambuco, L.A.; Balata, P.M.; Santos, V.S.; de Lima, L.M.; de Souza, S.R.; da Silva, H.J. Limits on quality of life in communication after total laryngectomy. Int. Arch. Otorhinolaryngol. 2012, 16, 482–491. [Google Scholar] [PubMed]
- Roger, V.; De Raucourt, D.; Babin, E. Seguimiento y reinserción del paciente laringectomizado. EMC-Otorrinolaringol. 2014, 43, 1–10. [Google Scholar] [CrossRef]
- Biazevic, M.G.; Antunes, J.L.; Togni, J.; de Andrade, F.P.; de Carvalho, M.B.; Wünsch-Filho, V. Immediate impact of primary surgery on health-related quality of life of hospitalized patients with oral and oropharyngeal cancer. J. Oral Maxillofac. Surg. 2008, 66, 1343–1350. [Google Scholar] [CrossRef]
- Polat, B.; Orhan, K.S.; Kesimli, M.C.; Gorgulu, Y.; Ulusan, M.; Deger, K. The effects of indwelling voice prosthesis on the quality of life, depressive symptoms, and self-esteem in patients with total laryngectomy. Eur. Arch. Otorhinolaryngol. 2015, 272, 3431–3437. [Google Scholar] [CrossRef]
- Tanga, C.G.; Sinclair, C.F. Voice restoration after total laryngectomy. Otolaryngol. Clin. N. Am. 2015, 48, 687–702. [Google Scholar] [CrossRef]
- Carcamo, M.; Campo, V.; Behrmann, D.; Celedón, C.; Alvear, Á.; Vásquez, P.; Araya, C. Head and neck cancer: Validation of the QLQ-H&N35 quality of life questionnaire. Rev. Méd. Chile 2018, 146, 578–584. [Google Scholar]
- Núñez-Batalla, F.; Corte-Santos, P.; Señaris-González, B.; Llorente-Pendás, J.L.; Górriz-Gil, C.; Suárez-Nieto, C. Adaptation and validation to the Spanish of the Voice Handicap Index (VHI-30) and its shortened version (VHI-10). Acta. Otorrinolaringol. Esp. 2007, 58, 386–392. [Google Scholar] [CrossRef]
- Núñez-Batalla, F.; Morato-Galán, M.; García-López, I.; Ávila-Menéndez, A. Validation of the Spanish adaptation of the Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V). Acta Otorrinolaringol. Esp. 2015, 66, 249–257. [Google Scholar] [CrossRef]
- Blood, G.W. Development and assessment of a scale addressing communication needs of patients with laryngectomies. Am. J. Speech Lang Pathol. 1993, 2, 82–90. [Google Scholar] [CrossRef]
- Johansson, M.; Rydén, A.; Finizia, C. Self-Evaluation of communication experiences after laryngeal cancer–A longitudinal questionnaire study in patients with laryngeal cancer. BMC Cancer 2008, 8, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finizia, C.; Bergman, B.; Lindström, J. A cross-sectional validation study of Self-Evaluation of Communication Experiences after Laryngeal Cancer-A questionnaire for use in the voice rehabilitation of laryngeal cancer patients. Acta Oncol. 1999, 38, 573–580. [Google Scholar] [PubMed]
- Schindler, A.; Mozzanica, F.; Brignoli, F.; Maruzzi, P.; Evitts, P.; Ottaviani, F. Reliability and validity of the Italian self-evaluation of communication experiences after laryngeal cancer questionnaire: Reliability and Validity of the I-SECEL Questionnaire. Head Neck 2013, 35, 1606–1615. [Google Scholar] [CrossRef]
- Guimarães, I.; Torrejano, G.; Aires, R.; Gonçalves, F.; Freitas, S.V.; Correia, P.; Romeiro, C.; Silvestre, I.; Bom, R.; Martins, P.; et al. Self-evaluation of communication experiences after laryngectomy (SECEL): Translation and psychometric properties in European Portuguese. Logoped. Phoniatr. Vocol. 2020, 45, 66–72. [Google Scholar] [CrossRef]
- Fahl, G.B.; Goulart, B.N.G. Transcultural adaptation of the Self-Evaluation of Communication Experiences After Laryngectomy (SECEL) instrument into Brazilian Portuguese. Audiol. Commun. Res. 2016, 21, e1678. [Google Scholar] [CrossRef]
- Evitts, P.M.; Kasapoglu, F.; Demirci, U.; Miller, J.S. Communication adjustment of patients with a laryngectomy in Turkey: Analysis by type of surgery and mode of speech. Psychol. Health Med. 2011, 16, 650–660. [Google Scholar] [CrossRef]
- Carvajal, A.; Centeno, C.; Watson, R.; Martínez, M.; Rubiales, A.S. How is an instrument for measuring health to be validated? An. Sist. Sanit. Navar. 2011, 34, 63–72. [Google Scholar]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [Green Version]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P.; ISPOR Task Force for Translation and Cultural Adaptation. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005, 8, 94–104. [Google Scholar] [CrossRef] [Green Version]
- López-Roig, S.; Terol Cantero, M.C.; Pastor, M.-A.; Neipp, M.C.; Massutí, B.; Rodríguez-Marín, J.; Leyda, J.I.; Gelabert, M.M.A.; Sitges, E. Ansiedad y depresión. Validación de la escala HAD en pacientes oncológicos. Rev. Psicol. Salud 2000, 12, 127–155. [Google Scholar]
- Ferrando, P.J.; Lorenzo-Seva, U. Assessing the quality and appropriateness of factor solutions and factor score estimates in exploratory item factor analysis. Educ. Psychol. Meas. 2017, 78, 762–780. [Google Scholar] [CrossRef]
- Ferrando, P.J.; Lorenzo-Seva, U. Exploratory item factor analysis: Some additional considerations. An. Psicol. 2014, 30, 1170–1175. [Google Scholar]
- Lorenzo-Seva, U.; Ferrando, P.J. FACTOR: A computer program to fit the exploratory factor analysis model. Behav. Res. Methods 2006, 38, 88–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curran, P.J.; West, S.G.; Finch, J.F. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol. Methods 1996, 51, 16–29. [Google Scholar] [CrossRef]
- Timmerman, M.E.; Lorenzo-Seva, U. Dimensionality assessment of ordered polytomous items with parallel analysis. Psychol. Methods 2011, 16, 209–220. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 3rd ed.; The Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Bentler, P.M. Factor simplicity index and transformations. Psychometrika 1977, 42, 277–295. [Google Scholar] [CrossRef]
- Ferrando, P.J.; Lorenzo-Seva, U. On the added value of multiple factor score estimates in essentially unidimensional models. Educ. Psychol. Meas. 2019, 79, 249–271. [Google Scholar] [CrossRef]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. 2003, 8, 23–74. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Gadermann, A.M.; Guhn, M.; Zumbo, B.D. Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. Pract. Assess. Res. Eval. 2012, 17, 3. [Google Scholar] [CrossRef]
- Ferguson, C.J. An Effect Size Primer: A Guide for Clinicians and Researchers. In Methodological Issues and Strategies in Clinical Research; Kazdin, A.E., Ed.; American Psychological Association: Washington, DC, USA, 2016; pp. 301–310. [Google Scholar] [CrossRef]
- Suárez Álvarez, J.; Pedrosa, I.; Lozano, L.M.; García Cueto, E.; Cuesta Izquierdo, M.; Muñiz Fernández, J. Using reversed items in Likert scales: A questionable practice. Psicothema 2018, 30, 149–158. [Google Scholar]
- Finizia, C.; Palmé, C.; Bergman, B. A longitudinal study of the swedish self-evaluation of communication experiences after laryngeal cancer questionnaire in patients treated for laryngeal cancer. Acta Oncol. 2002, 41, 262–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vallejo Seco, G.; Ato, M.; Fernández García, M.P.; Livacic Rojas, P.E. Sample size estimation for heterogeneous growth curve models with attrition. Behav. Res. Methods 2019, 51, 1216–1243. [Google Scholar] [CrossRef] [PubMed]
- Fernández-García, M.P.; Vallejo-Seco, G.; Livácic-Rojas, P.; Tuero-Herrero, E. the (ir)responsibility of (under)estimating missing data. Front. Psychol. 2018, 20, 556. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristics | No. (%) |
|---|---|
| Age | 68 (43–88) |
| Sex | |
| Man | 92 (91.1) |
| Woman | 9 (8.9) |
| Nationality | |
| Spanish | 98 (97) |
| Foreign | 9 (8.9) |
| Working condition | |
| Retired | 89 (88.1) |
| Not retired | 13 (11.9) |
| Marital status | |
| Married | 70 (69.3) |
| Other | 31 (30.7) |
| Education | |
| Primary | 62 (61.2) |
| Secondary | 25 (24.8) |
| University | 14 (13.9) |
| Clinical features | |
| Adjuvant treatment after TL | |
| RT | 37 (36.6) |
| CT | 7 (6.9) |
| CRT | 13 (12.9) |
| No | 44 (43.6) |
| Type of voice | |
| Esophageal | 80(79.2) |
| Tracheoesophageal prosthesis | 4 (4) |
| Artificial larynx | 7 (6.9) |
| Other | 10 (9.9) |
| Perceptual intelligibility | |
| Does not speak | 11 (10.9) |
| Monosyllabic | 39 (38) |
| Faulty speech | 21 (20.8) |
| Intelligibility speech | 30 (29.7) |
| No. (%) | |||
|---|---|---|---|
| Mental health variables | HAD-A (n = 101) | No | 82 (81.2) |
| Doubtful | 10 (9.9) | ||
| Probable | 9 (8.9) | ||
| HAD-D 1 (n = 99) | No | 82 (82.8) | |
| Doubtful | 9 (9.1) | ||
| Probable | 8 (8.1) | ||
| HAD-A&D 1 (n = 99) | No anxiety and no depression | 70 (70.7) | |
| Anxiety and depression | 29 (29.3) | ||
| Quality of life | QLQ-H&N35 2 (n = 101) | <P25 (46) | 28 (27.7) |
| P25–P75 | 46 (45.5) | ||
| >P75 (60) | 27 (26.7) | ||
| Variable referring to vocal disability | VHI 3 (n = 101) | Mild | 19 (18.8) |
| Moderate | 58 (57.4) | ||
| Severe | 24 (23.8) |
| Item | Original SECEL | Spanish Version of SECEL |
|---|---|---|
| 1 | Are you relaxed and comfortable around other people in speaking situations? | ¿Se siente relajado y cómodo al hablar con otras personas? |
| 2 | Would you describe yourself as a low-keyed, calm person? | ¿Se describiría como una persona tranquila y reservada? |
| 3 | Are you an active, “outgoing”, talkative person? | ¿Se considera una persona activa, extrovertida y habladora? |
| 4 | Do you admit to the person you are speaking to that you had a laryngectomy? | ¿Suele decirle a la gente con la que habla que está laringectomizado? |
| 5 | Do you think your speech improves with the amount of time you use it? | ¿Cree que su habla empeora con el paso del tiempo? |
| 6 | Do you find that you frequent clubs, meetings, or lodges less often because of your speech? | ¿Cree que han disminuido sus reuniones sociales o asistencia a eventos a consecuencia de su forma de hablar? |
| 7 | Do you have difficulty having getting people’s attention to speak? | ¿Tiene dificultades para atraer la atención de la gente cuando habla? |
| 8 | Do you have difficulty yelling or calling out to people? | ¿Tiene dificultad para gritar o dar voces a la gente? |
| 9 | Do you find that people are unable to understand you? | ¿Siente que la gente tiene dificultad para entenderle cuando habla? |
| 10 | Do you find that people are unable to understand you? | ¿Nota que tiene que repetir las cosas varias veces para que le entiendan? |
| 11 | Do you have trouble with speaking: in large groups of people? | ¿Tiene dificultades para hablar en grupos grandes de gente? |
| 12 | In small groups of people? | ¿Tiene dificultades para hablar en grupos pequeños de gente? |
| 13 | With one person? | ¿Tiene dificultades para hablar con una persona? |
| 14 | In different rooms of your house (apartment, residence) | ¿Tiene dificultades para hablar a cierta distancia de otra persona? |
| 15 | In loud or noisy places | ¿Tiene dificultades para hablar en ambientes ruidosos? |
| 16 | On the telephone? | ¿Tiene dificultades para hablar por teléfono? |
| 17 | In the car, bus or while traveling? | ¿Tiene dificultades para hablar en el coche, en el autobús o viajando? |
| 18 | Does your speech cause you to:Have difficulty when attending parties or social gatherings? | ¿Cree que su habla le provoca dificultades para acudir a fiestas o encuentros sociales? |
| 19 | Use the telephone less often than you would like? | ¿Cree que su habla le provoca usar el teléfono menos de lo que le gustaría? |
| 20 | Feel left out when you are with a group of people? | ¿Cree que su habla le provoca sentirse apartado cuando está con un grupo de personas? |
| 21 | Limit your social life or personal life? | ¿Cree que su habla le provoca limitación de su vida social o personal? |
| 22 | Does your speech cause you to feel:Depressed? | ¿Su habla le hace sentirse deprimido/a? |
| 23 | Frustrated when talking to family and friends and they can’t understand you? | ¿Su habla le hace sentirse frustrado/a cuando habla con su familia o amigos y no lo entienden? |
| 24 | Different or peculiar? | ¿Su habla le hace sentirse diferente o peculiar? |
| 25 | Do you hesitate to meet new people because of your speech? | ¿Evita conocer a personas nuevas a causa de su forma de hablar? |
| 26 | Do you get left out of conversations because of your speech? | ¿Se siente apartado de las conversaciones por su forma de hablar? |
| 27 | Do you avoid speaking with other people because of your speech? | ¿Evita hablar con otras personas por su forma de hablar? |
| 28 | Do people tend to fill in words or complete sentences for you? | ¿La gente tiende a completar sus frases cuando habla? |
| 29 | Do people interrupt you while you are speaking? | ¿La gente le interrumpe mientras está hablando? |
| 30 | Do people tell you that they can’t understand you? | ¿La gente le dice que no le entienden cuando habla? |
| 31 | Do the people you speak with get annoyed with you because of your speech? | ¿Cree que la gente se molesta por su forma de comunicarse? |
| 32 | Do people avoid you because of your speech? | ¿Cree que la gente le evita por su forma de hablar? |
| 33 | Do people speak to you differently because of your speech? | ¿Nota que la gente se comunica con usted de forma diferente por su forma de hablar? |
| 34 | Do your family and friends fail to understand what it’s like to communicate with this type of speech? | ¿Su familia o amigos no entienden sus dificultades por su forma de comunicarse? |
| 35 | Do you talk the same amount now as before your laryngectomy? | ¿Habla lo mismo ahora que antes de la laringectomía?, ¿por qué? |
| FA | Model | χ2 (df) | χ2/df | BIC/ECVI | CFI | RMSEA 1 [90%CI] | RMSR/SRMR | S |
|---|---|---|---|---|---|---|---|---|
| CFA | M0 (k = 34) | 407.392 (524) | 0.77 | 5.549 | 1 | 0.000 (0–0) | 0.086 | 0.937 |
| EFA 2 | M1 (k = 21) | 481.09 | 0.994 | 0.036 | 0.075 | 0.976 | ||
| CFA | M1 (k = 21) | 93.98 (186) | 0.50 | 1.840 | 1 | 0.000 (0–0) | 0.065 | 0.991 |
| CFA | M2 (k = 21) | 126.37 (180) | 0.65 | 2.284 | 1 | 0.000 (0–0) | 0.073 | 0.985 |
| SECEL (Original Version) | Descriptive Statistics | Factor Loads 2 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CFA M0 k = 34 | EFA M1k = 21 | CFA M1 k = 21 | ||||||||||||
| Items 1 | M | SD | Asy | Kur | HIC | FAlpha | IAlpha | F1 | F2 | HIC | F1 | F2 | ||
| G.S | 1 3 | 1.13 | 0.997 | 0.417 | −0.915 | 0.560 | 0.208 | 0.903 | 0.623 | |||||
| 2 3 | 0.93 | 1.05 | 0.720 | −0.810 | −0.048 | 0.912 | −0.069 | |||||||
| 3 3 | 0.97 | 0.964 | 0.402 | −1.16 | 0.292 | 0.906 | 0.343 | |||||||
| 4 3 | 1.16 | 1.32 | 0.452 | −1.60 | 0.021 | 0.913 | 0.019 | |||||||
| 5 3 | 1.31 | 1.14 | 0.200 | −1.38 | 0.485 | 0.904 | 0.651 | 0.549 | 0.501 | 0.682 | ||||
| Env.S | 6 | 1.21 | 1.19 | 0.357 | −1.42 | 0.586 | 0.853 | 0.902 | 0.761 | 0.788 | 0.569 | 0.771 | ||
| 7 | 1.34 | 1.02 | 0.196 | −1.07 | 0.509 | 0.903 | 0.580 | 0.622 | 0.513 | 0.589 | ||||
| 8 | 2.48 | 0.986 | −1.59 | 0.990 | 0.301 | 0.906 | 0.288 | |||||||
| 9 | 1.86 | 0.849 | −0.130 | −0.856 | 0.675 | 0.901 | 0.644 | 0.612 | 0.685 | 0.688 | ||||
| 10 | 2.01 | 0.818 | −0.242 | −0.928 | 0.629 | 0.902 | 0.567 | 0.738 | 0.621 | 0.602 | ||||
| 11 | 2.12 | 1.02 | −0.872 | −0.445 | 0.457 | 0.904 | 0.488 | |||||||
| 12 | 1.35 | 1.06 | 0.234 | −1.16 | 0.697 | 0.900 | 0.835 | 0.633 | 0.709 | 0.889 | ||||
| 13 | 0.80 | 0.906 | 0.982 | 0.177 | 0.529 | 0.903 | 0.533 | 0.678 | 0.548 | 0.592 | ||||
| 14 | 2.23 | 0.904 | −0.801 | −0.516 | 0.452 | 0.904 | 0.451 | 0.575 | 0.470 | 0.505 | ||||
| 15 | 2.50 | .0.879 | −1.64 | 1.51 | 0.157 | 0.908 | 0.123 | |||||||
| 16 | 2.30 | 1.01 | −1.11 | −0.149 | 0.403 | 0.905 | 0.432 | 0.924 | 0.395 | 0.416 | ||||
| 17 | 1.71 | 1.13 | −0.225 | −1.35 | 0.499 | 0.903 | 0.603 | 0.784 | 0.508 | 0.660 | ||||
| 18 | 1.37 | 1.20 | 0.145 | −1.50 | 0.602 | 0.902 | 0.782 | 0.577 | 0.612 | 0.813 | ||||
| 19 | 2.22 | 1.08 | −1.07 | −0.303 | 0.385 | 0.905 | 0.442 | 0.738 | 0.379 | 0.445 | ||||
| Att.S | 20 | 1.11 | 1.11 | 0.447 | −1.22 | 0.578 | 0.858 | 0.902 | 0.710 | 0.893 | 0.570 | 0.728 | ||
| 21 | 1.23 | 1.17 | 0.301 | −1.43 | 0.616 | 0.901 | 0.815 | 0.630 | 0.626 | 0.827 | ||||
| 22 | 0.75 | 0.953 | 1.08 | 0.131 | 0.626 | 0.902 | 0.645 | 0.779 | 0.609 | 0.635 | ||||
| 23 | 1.23 | 1.12 | 0.361 | −1.25 | 0.560 | 0.902 | 0.616 | 0.510 | 0.562 | 0.694 | ||||
| 24 | 1.01 | 1.12 | 0.725 | −0.883 | 0.521 | 0.903 | 0.627 | 0.727 | 0.527 | 0.651 | ||||
| 25 | 0.69 | 1.05 | 1.24 | 0.084 | 0.550 | 0.903 | 0.603 | 0.713 | 0.529 | 0.609 | ||||
| 26 | 0.88 | 0.972 | 0.842 | −0.338 | 0.574 | 0.902 | 0.633 | 0.804 | 0.617 | 0.666 | ||||
| 27 | 0.88 | 1.09 | 0.857 | −0.695 | 0.581 | 0.902 | 0.712 | 0.666 | 0.592 | 0.708 | ||||
| 28 | 1.22 | 0.965 | 0.227 | −0.968 | 0.462 | 0.904 | 0.499 | |||||||
| 29 | 0.74 | 0.833 | 0.729 | −0.562 | 0.104 | 0.908 | 0.088 | |||||||
| 30 | 1.51 | 0.870 | 0.109 | −0.644 | 0.417 | 0.905 | 0.428 | |||||||
| 31 | 0.58 | 0.919 | 1.56 | 1.44 | 0.372 | 0.905 | 0.382 | |||||||
| 32 | 0.48 | 0.844 | 1.76 | 2.17 | 0.441 | 0.904 | 0.394 | |||||||
| 33 | 0.92 | 0.945 | 0.668 | −0.591 | 0.444 | 0.904 | 0.453 | 0.443 | 0.428 | 0.451 | ||||
| 34 | 0.46 | 0.900 | 1.90 | 2.36 | 0.363 | 0.905 | 0.373 | |||||||
| r | 0.636 | 0.702 | ||||||||||||
| CR | 0.916 | 0.845 | ||||||||||||
| Reliability of the S-SECEL | Correlation Test–Retest | |||
|---|---|---|---|---|
| Cronbach’s Alpha | McD ω | CR | Pearson’s | |
| F1 | 0.884 | 0.882 | 0.916 | 0.697 |
| F2 | 0.846 | 0.943 | 0.845 | 0.790 |
| T | 0.909 | 0.907 | - | 0.742 |
| Pearson’s Correlation | |||||||
|---|---|---|---|---|---|---|---|
| F1 | F2 | Total | Anxiety * | Depression * | VHI-30 * | QLQ-H&N35 | |
| F1 | 1 | 0.584 ** | 0.926 ** | 0.617 ** | 0.722 ** | 0.784 ** | 0.597 ** |
| F2 | 1 | 0.847 ** | 0.381 ** | 0.487 ** | 0.528 ** | 0.523 ** | |
| Total | 1 | 0.581 ** | 0.695 ** | 0.759 ** | 0.631 ** | ||
| Anxiety * | 1 | 0.731 ** | 0.669 ** | 0.658 ** | |||
| Depression * | 1 | 0.689 ** | 0.638 ** | ||||
| VHI-30 * | 1 | 0.633 ** | |||||
| QLQ-H&N35 | 1 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villanueva, E.; Fernández, M.P.; Arena, G.; Llorente, J.L.; Rodrigo, J.P.; López, F.; Álvarez-Marcos, C. Validation of “Self-Evaluation of Communication Experiences after Laryngectomy” (SECEL) Questionnaire for Spanish-Speaking Laryngectomized Patients. Cancers 2022, 14, 3347. https://doi.org/10.3390/cancers14143347
Villanueva E, Fernández MP, Arena G, Llorente JL, Rodrigo JP, López F, Álvarez-Marcos C. Validation of “Self-Evaluation of Communication Experiences after Laryngectomy” (SECEL) Questionnaire for Spanish-Speaking Laryngectomized Patients. Cancers. 2022; 14(14):3347. https://doi.org/10.3390/cancers14143347
Chicago/Turabian StyleVillanueva, Eva, María Paula Fernández, Giovanna Arena, José L. Llorente, Juan P. Rodrigo, Fernando López, and César Álvarez-Marcos. 2022. "Validation of “Self-Evaluation of Communication Experiences after Laryngectomy” (SECEL) Questionnaire for Spanish-Speaking Laryngectomized Patients" Cancers 14, no. 14: 3347. https://doi.org/10.3390/cancers14143347
APA StyleVillanueva, E., Fernández, M. P., Arena, G., Llorente, J. L., Rodrigo, J. P., López, F., & Álvarez-Marcos, C. (2022). Validation of “Self-Evaluation of Communication Experiences after Laryngectomy” (SECEL) Questionnaire for Spanish-Speaking Laryngectomized Patients. Cancers, 14(14), 3347. https://doi.org/10.3390/cancers14143347









