Evaluation of Glutaminase Expression in Prostate Adenocarcinoma and Correlation with Clinicopathologic Parameters
Abstract
Simple Summary
Abstract
1. Introduction
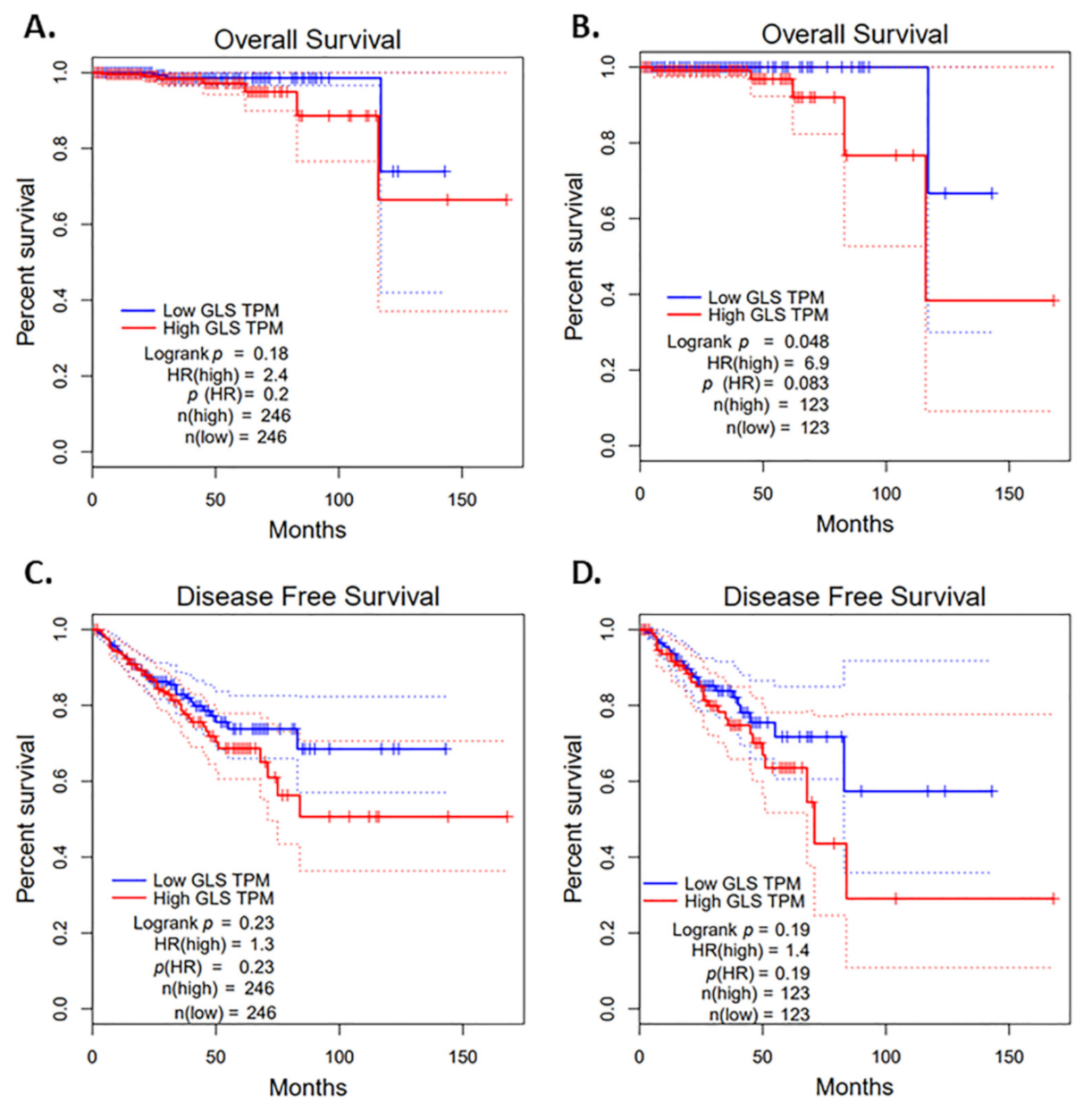
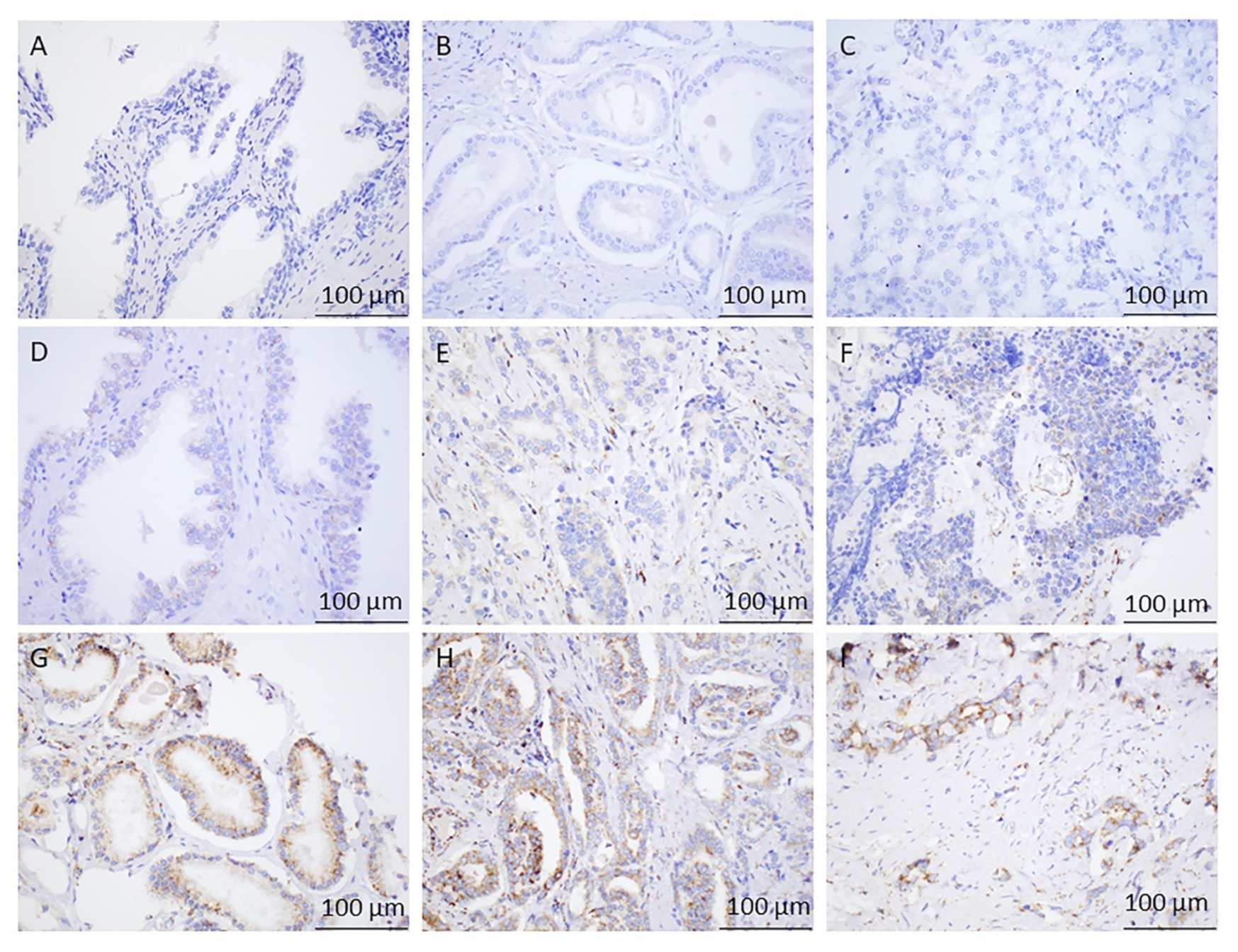
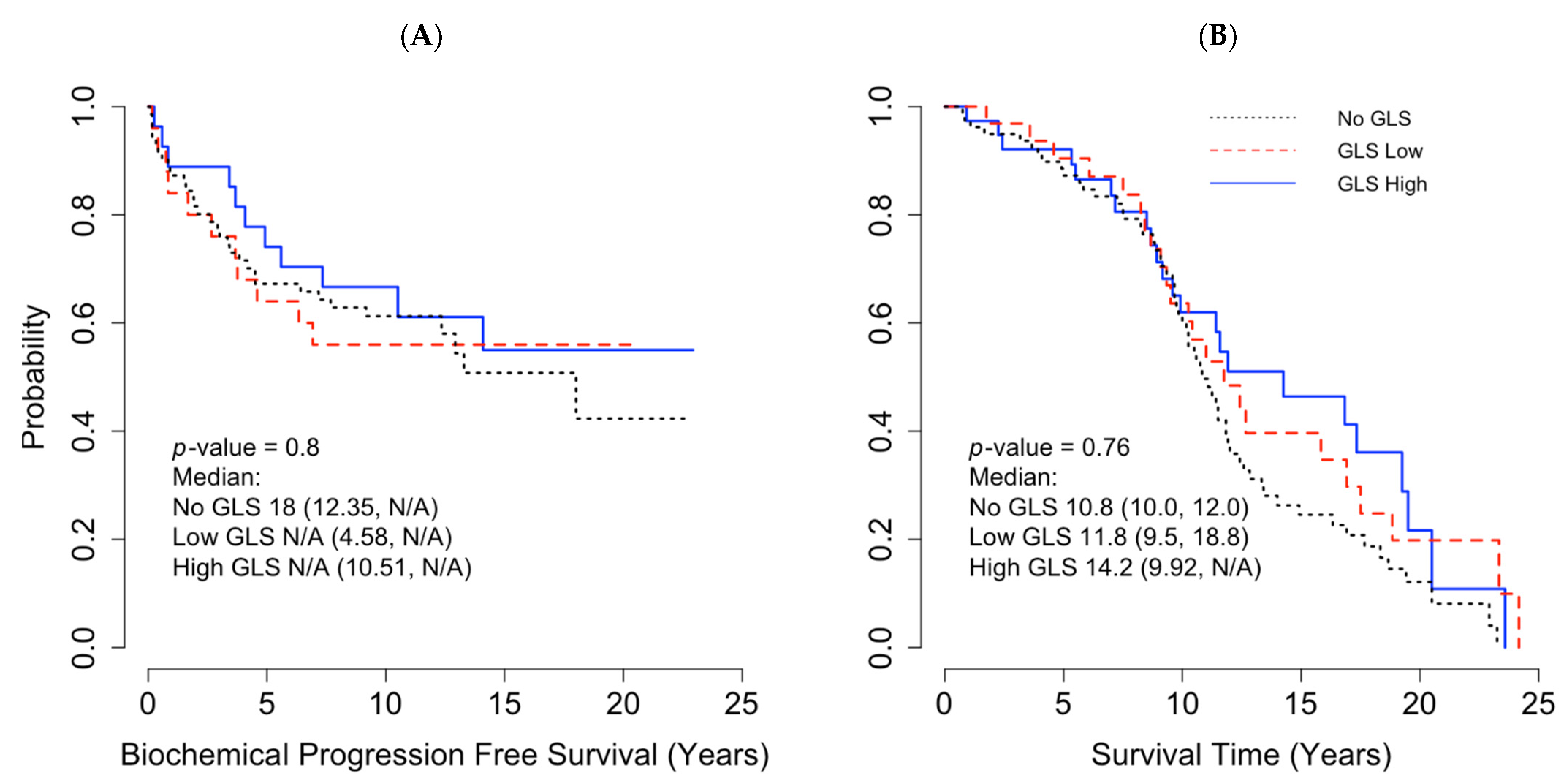
2. Results
3. Discussion
4. Materials and Methods
4.1. TCGA Cohort
4.2. TMA Cohort
4.3. Statistical Analysis
4.3.1. TCGA Cohort
4.3.2. TMA Cohort
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Warburg, O. The Metabolism of Carcinoma Cells. J. Cancer Res. 1925, 9, 148–163. [Google Scholar] [CrossRef]
- Warburg, O.; Wind, F.; Negelein, E. The Metabolism of Tumors in the Body. J. Gen. Physiol. 1927, 8, 519–530. [Google Scholar] [CrossRef]
- Heiden, M.G.V.; Cantley, L.C.; Thompson, C.B. Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science 2009, 324, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Dang, C.V. Links between metabolism and cancer. Genes Dev. 2012, 26, 877–890. [Google Scholar] [CrossRef]
- Altman, B.J.; Stine, Z.E.; Dang, B.J.A.Z.E.S.C.V. From Krebs to clinic: Glutamine metabolism to cancer therapy. Nat. Rev. Cancer 2016, 16, 619–634. [Google Scholar] [CrossRef] [PubMed]
- Gao, P.; Tchernyshyov, I.; Chang, T.-C.; Lee, Y.-S.; Kita, K.; Ochi, T.; Zeller, K.I.; De Marzo, A.M.; Van Eyk, J.E.; Mendell, J.T.; et al. c-Myc suppression of miR-23a/b enhances mitochondrial glutaminase expression and glutamine metabolism. Nat. Cell Biol. 2009, 458, 762–765. [Google Scholar] [CrossRef]
- Wise, D.R.; Ward, P.S.; Shay, J.E.S.; Cross, J.R.; Gruber, J.J.; Sachdeva, U.M.; Platt, J.M.; DeMatteo, R.G.; Simon, M.C.; Thompson, C.B. Hypoxia promotes isocitrate dehydrogenase-dependent carboxylation of α-ketoglutarate to citrate to support cell growth and viability. Proc. Natl. Acad. Sci. USA 2011, 108, 19611–19616. [Google Scholar] [CrossRef]
- Anderson, N.M.; Mucka, P.; Kern, J.G.; Feng, H. The emerging role and targetability of the TCA cycle in cancer metabolism. Protein Cell 2018, 9, 216–237. [Google Scholar] [CrossRef]
- Liang, Y.; Liu, J.; Feng, Z. The regulation of cellular metabolism by tumor suppressor p53. Cell Biosci. 2013, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Olumi, A.F.; Grossfeld, G.D.; Hayward, S.W.; Carroll, P.R.; Tlsty, T.D.; Cunha, G.R. Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res. 1999, 59, 5002–5011. [Google Scholar] [CrossRef]
- Thalmann, G.N.; Rhee, H.; Sikes, R.A.; Pathak, S.; Multani, A.; Zhau, H.E.; Marshall, F.F.; Chung, L.W. Human Prostate Fibroblasts Induce Growth and Confer Castration Resistance and Metastatic Potential in LNCaP Cells. Eur. Urol. 2010, 58, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Bonollo, F.; Thalmann, G.N.; Julio, M.K.-D.; Karkampouna, S. The Role of Cancer-Associated Fibroblasts in Prostate Cancer Tumorigenesis. Cancers 2020, 12, 1887. [Google Scholar] [CrossRef] [PubMed]
- Chiarugi, P.; Paoli, P.; Cirri, P. Tumor Microenvironment and Metabolism in Prostate Cancer. Semin. Oncol. 2014, 41, 267–280. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Achreja, A.; Yeung, T.-L.; Mangala, L.S.; Jiang, D.; Han, C.; Baddour, J.; Marini, J.C.; Ni, J.; Nakahara, R.; et al. Targeting Stromal Glutamine Synthetase in Tumors Disrupts Tumor Microenvironment-Regulated Cancer Cell Growth. Cell Metab. 2016, 24, 685–700. [Google Scholar] [CrossRef]
- Massie, C.E.; Lynch, A.; Ramos-Montoya, A.; Boren, J.; Stark, R.; Fazli, L.; Warren, A.; Scott, H.; Madhu, B.; Sharma, N.; et al. The androgen receptor fuels prostate cancer by regulating central metabolism and biosynthesis. EMBO J. 2011, 30, 2719–2733. [Google Scholar] [CrossRef]
- Tennakoon, J.B.; Shi, Y.; Han, J.J.; Tsouko, E.; White, M.A.; Burns, A.R.; Zhang, A.; Xia, X.; Ilkayeva, O.R.; Xin, L.; et al. Androgens regulate prostate cancer cell growth via an AMPK-PGC-1α-mediated metabolic switch. Oncogene 2014, 33, 5251–5261. [Google Scholar] [CrossRef]
- Huang, F.; Zhang, Q.; Ma, H.; Lv, Q.; Zhang, T. Expression of glutaminase is upregulated in colorectal cancer and of clinical significance. Int. J. Clin. Exp. Pathol. 2014, 7, 1093–1100. [Google Scholar]
- Vidula, N.; Yau, C.; Rugo, H.S. Glutaminase (GLS) expression in primary breast cancer (BC): Correlations with clinical and tumor characteristics. J. Clin. Oncol. 2019, 37, 558. [Google Scholar] [CrossRef]
- Cao, J.; Zhang, C.; Jiang, G.; Jin, S.; Gao, Z.; Wang, Q.; Yu, D.; Ke, A.; Fan, Y.; Li, D.; et al. Expression of GLS1 in intrahepatic cholangiocarcinoma and its clinical significance. Mol. Med. Rep. 2019, 20, 1915–1924. [Google Scholar] [CrossRef]
- Kim, H.M.; Lee, Y.K.; Koo, J.S. Expression of glutamine metabolism-related proteins in thyroid cancer. Oncotarget 2016, 7, 53628–53641. [Google Scholar] [CrossRef]
- Pan, T.; Gao, L.; Wu, G.; Shen, G.; Xie, S.; Wen, H.; Yang, J.; Zhou, Y.; Tu, Z.; Qian, W. Elevated expression of glutaminase confers glucose utilization via glutaminolysis in prostate cancer. Biochem. Biophys. Res. Commun. 2015, 456, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Mao, S.Y.; Guo, Y.D.; Wu, Y.; Yao, X.D.; Huang, Y. Inhibition of GLS suppresses proliferation and promotes apoptosis in prostate cancer. Biosci. Rep. 2019, 39. [Google Scholar] [CrossRef]
- Dorai, T.; Dorai, B.; Pinto, J.T.; Grasso, M.; Cooper, A.J.L. Dorai High Levels of Glutaminase II Pathway Enzymes in Normal and Cancerous Prostate Suggest a Role in ‘Glutamine Addiction’. Biomolecules 2019, 10, 2. [Google Scholar] [CrossRef]
- Zacharias, N.M.; McCullough, C.; Shanmugavelandy, S.; Lee, J.; Lee, Y.; Dutta, P.; McHenry, J.; Nguyen, L.; Norton, W.; Jones, L.W.; et al. Metabolic Differences in Glutamine Utilization Lead to Metabolic Vulnerabilities in Prostate Cancer. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Cassago, A.; Ferreira, A.P.S.; Ferreira, I.M.; Fornezari, C.; Gomes, E.R.M.; Greene, K.S.; Pereira, H.D.; Garratt, R.C.; Dias, S.M.G.; Ambrosio, A.L.B. Mitochondrial localization and structure-based phosphate activation mechanism of Glutaminase C with implications for cancer metabolism. Proc. Natl. Acad. Sci. USA 2012, 109, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- de la Rosa, V.; Campos-Sandoval, J.A.; Martín-Rufián, M.; Cardona, C.; Matés, J.M.; Segura, J.A.; Alonso, F.J.; Márquez, J. A novel glutaminase isoform in mammalian tissues. Neurochem. Int. 2009, 55, 76–84. [Google Scholar] [CrossRef]
- Emberley, E.; Bennett, M.; Chen, J.; Gross, M.; Huang, T.; Makkouk, A.; Parlati, F. The glutaminase inhibitor CB-839 synergizes with CDK4/6 and PARP inhibitors in pre-clinical tumor models. Cancer Res. 2018, 78, 3509. [Google Scholar]
- Ren, L.; Ruiz-Rodado, V.; Dowdy, T.; Huang, S.; Issaq, S.H.; Beck, J.; Wang, H.; Hoang, C.T.; Lita, A.; Larion, M.; et al. Glutaminase-1 (GLS1) inhibition limits metastatic progression in osteosarcoma. Cancer Metab. 2020, 8, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Meric-Bernstam, F.; Lee, R.J.; Carthon, B.C.; Iliopoulos, O.; Mier, J.W.; Patel, M.R.; Tannir, N.M.; Owonikoko, T.K.; Haas, N.B.; Voss, M.H.; et al. CB-839, a glutaminase inhibitor, in combination with cabozantinib in patients with clear cell and papillary metastatic renal cell cancer (mRCC): Results of a phase I study. J. Clin. Oncol. 2019, 37, 549. [Google Scholar] [CrossRef]
- Boysen, G.; Jamshidi-Parsian, A.; Davis, M.A.; Siegel, E.R.; Simecka, C.M.; Kore, R.A.; Dings, R.P.M.; Griffin, R.J. Glutaminase inhibitor CB-839 increases radiation sensitivity of lung tumor cells and human lung tumor xenografts in mice. Int. J. Radiat. Biol. 2019, 95, 436–442. [Google Scholar] [CrossRef]
- Xiang, L.; Mou, J.; Shao, B.; Wei, Y.; Liang, H.; Takano, N.; Semenza, G.L.; Xie, G. Glutaminase 1 expression in colorectal cancer cells is induced by hypoxia and required for tumor growth, invasion, and metastatic colonization. Cell Death Dis. 2019, 10, 40. [Google Scholar] [CrossRef] [PubMed]

| Clinicopathological Characteristics | Number of Prostate Cancer Cases, n (%) |
|---|---|
| Total n = 154 | |
| Age | |
| <60 | 84 (55%) |
| ≥60 | 65 (45%) |
| Race | |
| White | 121 (78.6%) |
| Black | 31 (20.1%) |
| Other | 2 (1.3%) |
| Smoking | |
| Yes | 56 (36.4%) |
| No | 50 (32.5%) |
| Unknown | 48 (31.2%) |
| Pathological Tumor (pT) stage | |
| 2 | 81 (52.9%) |
| 3 | 66 (43.1%) |
| 4 | 6 (3.9%) |
| Missing | 1 |
| Pathological Node (pN) status | |
| Yes | 7 (5.3%) |
| No | 124 (94.7%) |
| Missing | 23 |
| Gleason Grade Group | |
| Grade Group 1 | 21(13.6%) |
| Grade Group 2 | 65(42.2%) |
| Grade Group 3 | 29(18.8%) |
| Grade Group 4 | 8(5.2%) |
| Grade Group 5 | 21(13.6%) |
| Missing | 10 (6.4%) |
| GLS1 Score | |
| High expression | 38 (25.5%) |
| Low expression | 32 (21.5%) |
| Negative | 79 (53%) |
| Missing * | 5 |
| Variables | GLS1 Score | p-Value | |||
|---|---|---|---|---|---|
| High Expression (n = 38) | Low Expression (n = 32) | No (n = 79) | Missing (n = 5) | ||
| Age | 0.29 | ||||
| <60 | 20 (24%) | 17 (20%) | 47 (56%) | ||
| ≥60 | 18 (28%) | 15 (23%) | 32 (49%) | ||
| Race | 0.3 | ||||
| White | 33 (86.8%) | 27 (84.4%) | 57 (72.2%) | 4 | |
| Black | 5 (13.2%) | 5 (15.6%) | 20 (25.3%) | 1 | |
| Other | 0 | 0 | 2 (2.5%) | ||
| pT stage | 0.6 | ||||
| pT2 | 19 (50%) | 18 (56.3%) | 40 (51.3%) | 4 | |
| pT3 | 19 (50%) | 12 (37.5%) | 34 (43.6%) | 1 | |
| pT4 | 0 | 2 (6.3%) | 4 (5.1%) | 0 | |
| Missing | 0 | 0 | 1 | ||
| pN | 0.2 | ||||
| Yes | 1 (2.9%) | 0 | 5 (7.9%) | 1 | |
| No | 34 (97.1%) | 29 (100%) | 58 (92.1%) | 3 | |
| Gleason Grade Group | 0.5 | ||||
| 1 | 9 (23.6%) | 6 (18%) | 5 (6.3%) | 1 | |
| 2 | 16 (42%) | 11 (34%) | 37 (46.8%) | 1 | |
| 3 | 4 (10.5%) | 6 (18.7%) | 18 (22.8) | 1 | |
| 4 | 3 (7.8%) | 1 (3%) | 4 (5%) | ||
| 5 | 5 (13%) | 5 (15.6%) | 11(13.9%) | ||
| Unknown | 1(2.6%) | 3 (9.3%) | 4 (5%) | 2 | |
| Smoking | 0.9 | ||||
| Yes | 12 (31.6%) | 13 (40.6%) | 28 (35.4%) | 3 | |
| No | 13 (34.2%) | 10 (31.3%) | 27 (34.2%) | 0 | |
| Unknown | 13 (34.2%) | 9 (28.1%) | 24 (30.4%) | 2 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myint, Z.W.; Sun, R.C.; Hensley, P.J.; James, A.C.; Wang, P.; Strup, S.E.; McDonald, R.J.; Yan, D.; St. Clair, W.H.; Allison, D.B. Evaluation of Glutaminase Expression in Prostate Adenocarcinoma and Correlation with Clinicopathologic Parameters. Cancers 2021, 13, 2157. https://doi.org/10.3390/cancers13092157
Myint ZW, Sun RC, Hensley PJ, James AC, Wang P, Strup SE, McDonald RJ, Yan D, St. Clair WH, Allison DB. Evaluation of Glutaminase Expression in Prostate Adenocarcinoma and Correlation with Clinicopathologic Parameters. Cancers. 2021; 13(9):2157. https://doi.org/10.3390/cancers13092157
Chicago/Turabian StyleMyint, Zin W., Ramon C. Sun, Patrick J. Hensley, Andrew C. James, Peng Wang, Stephen E. Strup, Robert J. McDonald, Donglin Yan, William H. St. Clair, and Derek B. Allison. 2021. "Evaluation of Glutaminase Expression in Prostate Adenocarcinoma and Correlation with Clinicopathologic Parameters" Cancers 13, no. 9: 2157. https://doi.org/10.3390/cancers13092157
APA StyleMyint, Z. W., Sun, R. C., Hensley, P. J., James, A. C., Wang, P., Strup, S. E., McDonald, R. J., Yan, D., St. Clair, W. H., & Allison, D. B. (2021). Evaluation of Glutaminase Expression in Prostate Adenocarcinoma and Correlation with Clinicopathologic Parameters. Cancers, 13(9), 2157. https://doi.org/10.3390/cancers13092157






