Immunomodulatory Effects of Bendamustine in Hematopoietic Cell Transplantation
Abstract
Simple Summary
Abstract
1. Introduction
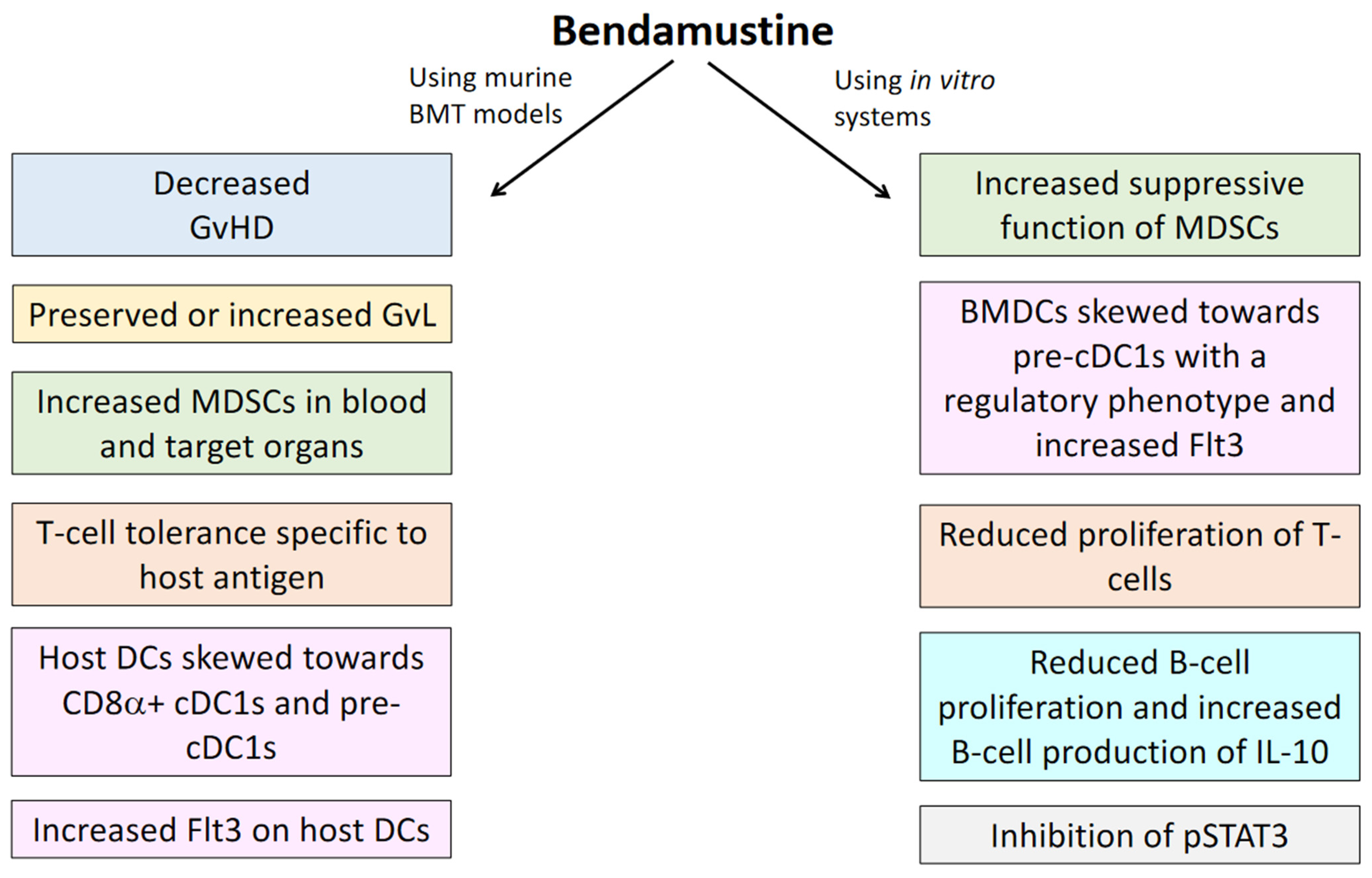
2. BEN as Pre-Transplant Conditioning in Murine Models
3. Clinical Application of BEN as Pre-Transplant Conditioning
4. Post-Transplant BEN in Murine Models
5. Clinical Application of BEN Post-Transplant
6. Immunomodulatory Effects of BEN
6.1. Myeloid Derived Suppressor Cells (MDSCs)
6.2. Effector T-cells and T Regulatory Cells
6.3. B-Cells
6.4. Dendritic Cells
6.5. Immunomodulatory Pathways
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cephalon. Cephalon Receives FDA Approval for TREANDA, a Novel Chemotherapy for Chronic Lymphocytic Leukemia. 2008. Available online: www.cephalon.com (accessed on 21 October 2017).
- Leoni, L.M.; Bailey, B.; Reifert, J.; Bendall, H.H.; Zeller, R.W.; Corbeil, J.; Elliott, G.; Niemeyer, C.C. Bendamustine (Treanda) displays a distinct pattern of cytotoxicity and unique mechanistic features compared with other alkylating agents. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008, 14, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Konstantinov, S.M.; Kostovski, A.; Topashka-Ancheva, M.; Genova, M.; Berger, M.R. Cytotoxic efficacy of bendamustine in human leukemia and breast cancer cell lines. J. Cancer Res. Clin. Oncol. 2002, 128, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, V.; Burger, J.A. Bendamustine in B-Cell Malignancies: The New 46-Year-Old Kid on the Block. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2009, 15, 7456–7461. [Google Scholar] [CrossRef] [PubMed]
- Strumberg, D.; Harstrick, A.; Doll, K.; Hoffmann, B.; Seeber, S. Bendamustine hydrochloride activity against doxorubicin-resistant human breast carcinoma cell lines. Anticancer Drugs 1996, 7, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Gaul, L.; Mandl-Weber, S.; Baumann, P.; Emmerich, B.; Schmidmaier, R. Bendamustine induces G2 cell cycle arrest and apoptosis in myeloma cells: The role of ATM-Chk2-Cdc25A and ATM-p53-p21-pathways. J. Cancer Res. Clin. Oncol. 2008, 134, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Beeharry, N.; Rattner, J.B.; Bellacosa, A.; Smith, M.R.; Yen, T.J. Dose Dependent Effects on Cell Cycle Checkpoints and DNA Repair by Bendamustine. PLoS ONE 2012, 7, e40342. [Google Scholar] [CrossRef]
- Iwamoto, K.; Uehara, Y.; Inoue, Y.; Taguchi, K.; Muraoka, D.; Ogo, N.; Matsuno, K.; Asai, A. Inhibition of STAT3 by Anticancer Drug Bendamustine. PLoS ONE 2017, 12, e0170709. [Google Scholar] [CrossRef]
- Chantepie, S.P.; Garciaz, S.; Tchernonog, E.; Peyrade, F.; Larcher, M.-V.; Diouf, M.; Fornecker, L.-M.; Houot, R.; Gastinne, T.; Soussain, C.; et al. Bendamustine-based conditioning prior to autologous stem cell transplantation (ASCT): Results of a French multicenter study of 474 patients from LYmphoma Study Association (LYSA) centers. Am. J. Hematol. 2018, 93, 729–735. [Google Scholar] [CrossRef]
- Hueso, T.; Gastinne, T.; Garciaz, S.; Tchernonog, E.; Delette, C.; Casasnovas, R.O.; Durot, E.; Houot, R.; Tessoulin, B.; Tournilhac, O.; et al. Bendamustine-EAM versus BEAM regimen in patients with mantle cell lymphoma undergoing autologous stem cell transplantation in the frontline setting: A multicenter retrospective study from Lymphoma Study Association (LYSA) centers. Bone Marrow Transpl. 2020. [Google Scholar] [CrossRef]
- Knauf, W.U.; Lissichkov, T.; Aldaoud, A.; Liberati, A.; Loscertales, J.; Herbrecht, R.; Juliusson, G.; Postner, G.; Gercheva, L.; Goranov, S.; et al. Phase III Randomized Study of Bendamustine Compared With Chlorambucil in Previously Untreated Patients With Chronic Lymphocytic Leukemia. J. Clin. Oncol. 2009, 27, 4378–4384. [Google Scholar] [CrossRef]
- Cephalon. Cephalon Receives FDA Approval for TREANDA to Treat Patients with Relapsed Indolent Non-Hodgkin’s Lymphoma. 2008. Available online: www.cephalon.com (accessed on 21 October 2017).
- Kalos, M.; Levine, B.L.; Porter, D.L.; Katz, S.; Grupp, S.A.; Bagg, A.; June, C.H. T Cells with Chimeric Antigen Receptors Have Potent Antitumor Effects and Can Establish Memory in Patients with Advanced Leukemia. Sci. Transl. Med. 2011, 3, 95ra73. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Arteaga, A.; Mark, T.M.; Guarneri, D.; Christos, P.J.; Gergis, U.; Greenberg, J.D.; Hsu, J.; Mayer, S.A.; Niesvizky, R.; Pearse, R.N.; et al. High-dose bendamustine and melphalan conditioning for autologous stem cell transplantation for patients with multiple myeloma. Bone Marrow Transplant. 2019, 54, 2027–2038. [Google Scholar] [CrossRef] [PubMed]
- Martino, M.; Tripepi, G.; Messina, G.; Vincelli, I.D.; Console, G.; Recchia, A.G.; Gentile, M.; Molica, S.; Morabito, F. A phase II, single-arm, prospective study of bendamustine plus melphalan conditioning for second autologous stem cell transplantation in de novo multiple myeloma patients through a tandem transplant strategy. Bone Marrow Transpl. 2016, 51, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Visani, G.; Malerba, L.; Stefani, P.M.; Capria, S.; Galieni, P.; Gaudio, F.; Specchia, G.; Meloni, G.; Gherlinzoni, F.; Giardini, C.; et al. BeEAM (bendamustine, etoposide, cytarabine, melphalan) before autologous stem cell transplantation is safe and effective for resistant/relapsed lymphoma patients. Blood 2011, 118, 3419–3425. [Google Scholar] [CrossRef] [PubMed]
- Saleh, K.; Danu, A.; Koscielny, S.; Legoupil, C.; Pilorge, S.; Castilla-Llorente, C.; Ghez, D.; Lazarovici, J.; Michot, J.M.; Khalife-Saleh, N.; et al. A retrospective, matched paired analysis comparing bendamustine containing BeEAM versus BEAM conditioning regimen: Results from a single center experience. Leuk. Lymphoma 2018, 59, 2580–2587. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, E.; Uphoff, D.; Reid, T.R.; Shelton, E. Modification of irradiation injury in mice and guinea pigs by bone marrow injections. J. Natl. Cancer Inst. 1951, 12, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Ford, C.E.; Hamerton, J.L.; Barnes, D.W.; Loutit, J.F. Cytological identification of radiation-chimaeras. Nature 1956, 177, 452–454. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.W.; Corp, M.J.; Loutit, J.F.; Neal, F.E. Treatment of murine leukaemia with X rays and homologous bone marrow; preliminary communication. Br. Med. J. 1956, 2, 626–627. [Google Scholar] [CrossRef]
- Thomas, E.D.; Lochte, H.L., Jr.; Lu, W.C.; Ferrebee, J.W. Intravenous infusion of bone marrow in patients receiving radiation and chemotherapy. N. Engl. J. Med. 1957, 257, 491–496. [Google Scholar] [CrossRef]
- Reddy, P.; Negrin, R.; Hill, G.R. Mouse Models of Bone Marrow Transplantation. Biol. Blood Marrow. Transplant. J. Am. Soc. Blood Marrow Transplant. 2008, 14, 129–135. [Google Scholar] [CrossRef]
- Graves, S.S.; Parker, M.H.; Storb, R. Animal Models for Preclinical Development of Allogeneic Hematopoietic Cell Transplantation. ILAR J. 2018, 59, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Zeiser, R.; Blazar, B.R. Preclinical models of acute and chronic graft-versus-host disease: How predictive are they for a successful clinical translation? Blood 2016, 127, 3117–3126. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.A.; Kelly, R.M.; Bade, N.D.; Smith, M.J.; Stefanski, H.E.; Blazar, B.R. FTY720 markedly increases alloengraftment but does not eliminate host anti-donor T cells that cause graft rejection on its withdrawal. Biol. Blood Marrow. Transpl. 2012, 18, 1341–1352. [Google Scholar] [CrossRef] [PubMed]
- Mielcarek, M.; Storer, B.E.; Boeckh, M.; Carpenter, P.A.; McDonald, G.B.; Deeg, H.J.; Nash, R.A.; Flowers, M.E.; Doney, K.; Lee, S.; et al. Initial therapy of acute graft-versus-host disease with low-dose prednisone does not compromise patient outcomes. Blood 2009, 113, 2888–2894. [Google Scholar] [CrossRef] [PubMed]
- Garnett, C.; Apperley, J.F.; Pavlů, J. Treatment and management of graft-versus-host disease: Improving response and survival. Adv. Hematol. 2013, 4, 366–378. [Google Scholar] [CrossRef]
- Weiss, L.; Reich, S.; Slavin, S. Effect of cyclosporine A and methylprednisolone on the graft-versus-leukemia effects across major histocompatibility barriers in mice following allogeneic bone marrow transplantation. Bone Marrow. Transpl. 1990, 6, 229–233. [Google Scholar]
- You-Ten, K.E.; Seemayer, T.A.; Wisse, B.; Bertley, F.M.; Lapp, W.S. Induction of a glucocorticoid-sensitive F1-anti-parental mechanism that affects engraftment during graft-versus-host disease. J. Immunol. 1995, 155, 172–180. [Google Scholar]
- Socié, G.; Blazar, B.R. Acute graft-versus-host disease: From the bench to the bedside. Blood 2009, 114, 4327–4336. [Google Scholar] [CrossRef]
- Gyurkocza, B.; Sandmaier, B.M. Conditioning regimens for hematopoietic cell transplantation: One size does not fit all. Blood 2014, 124, 344–353. [Google Scholar] [CrossRef]
- Stokes, J.; Hoffman, E.A.; Molina, M.S.; Eremija, J.; Larmonier, N.; Zeng, Y.; Katsanis, E. Bendamustine with Total Body Irradiation Limits Murine Graft-versus-Host Disease in Part Through Effects on Myeloid-Derived Suppressor Cells. Biol. Blood Marrow. Transpl. 2019, 25, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Stokes, J.; Hoffman, E.A.; Zeng, Y.; Larmonier, N.; Katsanis, E. Post-transplant bendamustine reduces GvHD while preserving GvL in experimental haploidentical bone marrow transplantation. Br. J. Haematol. 2016, 174, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Nakasone, H.; Fukuda, T.; Kanda, J.; Mori, T.; Yano, S.; Kobayashi, T.; Miyamura, K.; Eto, T.; Kanamori, H.; Iwato, K.; et al. Impact of conditioning intensity and TBI on acute GVHD after hematopoietic cell transplantation. Bone Marrow. Transpl. 2015, 50, 559–565. [Google Scholar] [CrossRef]
- Khouri, I.F.; Sui, D.; Jabbour, E.J.; Samuels, B.I.; Turturro, F.; Alatrash, G.; Anderlini, P.; Ahmed, S.; Oran, B.; Ciurea, S.O.; et al. Bendamustine added to allogeneic conditioning improves long-term outcomes in patients with CLL. Bone Marrow. Transpl. 2017, 52, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Khouri, I.F.; Wei, W.; Korbling, M.; Turturro, F.; Ahmed, S.; Alousi, A.; Anderlini, P.; Ciurea, S.; Jabbour, E.; Oran, B.; et al. BFR (bendamustine, fludarabine, and rituximab) allogeneic conditioning for chronic lymphocytic leukemia/lymphoma: Reduced myelosuppression and GVHD. Blood 2014, 124, 2306–2312. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Reddy, P. Pathophysiology of acute graft-versus-host disease. Hematol. Oncol. 2003, 21, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Hill, G.R.; Teshima, T.; Gerbitz, A.; Pan, L.; Cooke, K.R.; Brinson, Y.S.; Crawford, J.M.; Ferrara, J.L. Differential roles of IL-1 and TNF-alpha on graft-versus-host disease and graft versus leukemia. J. Clin. Investig. 1999, 104, 459–467. [Google Scholar] [CrossRef]
- Sadeghi, B.; Aghdami, N.; Hassan, Z.; Forouzanfar, M.; Rozell, B.; Abedi-Valugerdi, M.; Hassan, M. GVHD after chemotherapy conditioning in allogeneic transplanted mice. Bone Marrow. Transplant. 2008, 42, 807–818. [Google Scholar] [CrossRef]
- Riesner, K.; Kalupa, M.; Shi, Y.; Elezkurtaj, S.; Penack, O. A preclinical acute GVHD mouse model based on chemotherapy conditioning and MHC-matched transplantation. Bone Marrow. Transplant. 2016, 51, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Nagler, A.; Rocha, V.; Labopin, M.; Unal, A.; Ben Othman, T.; Campos, A.; Volin, L.; Poire, X.; Aljurf, M.; Masszi, T.; et al. Allogeneic hematopoietic stem-cell transplantation for acute myeloid leukemia in remission: Comparison of intravenous busulfan plus cyclophosphamide (Cy) versus total-body irradiation plus Cy as conditioning regimen--a report from the acute leukemia working party of the European group for blood and marrow transplantation. J. Clin. Oncol. 2013, 31, 3549–3556. [Google Scholar] [CrossRef]
- Woods, W.G.; Ramsay, N.K.; Weisdorf, D.J.; Haake, R.; Vallera, D.A.; Kim, T.H.; Lasky, L.; Nesbit, M.E.; Bostrom, B.; Uckun, F.; et al. Bone marrow transplantation for acute lymphocytic leukemia utilizing total body irradiation followed by high doses of cytosine arabinoside: Lack of superiority over cyclophosphamide-containing conditioning regimens. Bone Marrow. Transpl. 1990, 6, 9–16. [Google Scholar]
- Marks, D.I.; Forman, S.J.; Blume, K.G.; Perez, W.S.; Weisdorf, D.J.; Keating, A.; Gale, R.P.; Cairo, M.S.; Copelan, E.A.; Horan, J.T.; et al. A comparison of cyclophosphamide and total body irradiation with etoposide and total body irradiation as conditioning regimens for patients undergoing sibling allografting for acute lymphoblastic leukemia in first or second complete remission. Biol. Blood Marrow. Transpl. 2006, 12, 438–453. [Google Scholar] [CrossRef] [PubMed]
- Kornblit, B.; Maloney, D.G.; Storb, R.; Storek, J.; Hari, P.; Vucinic, V.; Maziarz, R.T.; Chauncey, T.R.; Pulsipher, M.A.; Bruno, B.; et al. Fludarabine and 2-Gy TBI is superior to 2 Gy TBI as conditioning for HLA-matched related hematopoietic cell transplantation: A phase III randomized trial. Biol. Blood Marrow. Transpl. 2013, 19, 1340–1347. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stokes, J.; Hoffman, E.A.; Molina, M.S.; Kummet, N.; Simpson, R.J.; Zeng, Y.; Katsanis, E. Bendamustine with total body irradiation conditioning yields tolerant T-cells while preserving T-cell-dependent graft-versus-leukemia. OncoImmunology 2020, 9, 1758011. [Google Scholar] [CrossRef] [PubMed]
- Philip, T.; Armitage, J.O.; Spitzer, G.; Chauvin, F.; Jagannath, S.; Cahn, J.Y.; Colombat, P.; Goldstone, A.H.; Gorin, N.C.; Flesh, M.; et al. High-dose therapy and autologous bone marrow transplantation after failure of conventional chemotherapy in adults with intermediate-grade or high-grade non-Hodgkin’s lymphoma. N. Engl. J. Med. 1987, 316, 1493–1498. [Google Scholar] [CrossRef] [PubMed]
- Philip, T.; Guglielmi, C.; Hagenbeek, A.; Somers, R.; Van der Lelie, H.; Bron, D.; Sonneveld, P.; Gisselbrecht, C.; Cahn, J.Y.; Harousseau, J.L.; et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin’s lymphoma. N. Engl. J. Med. 1995, 333, 1540–1545. [Google Scholar] [CrossRef] [PubMed]
- Gribben, J.; Linch, D.; Singer, C.; McMillan, A.; Jarrett, M.; Goldstone, A. Successful treatment of refractory Hodgkin’s disease by high-dose combination chemotherapy and autologous bone marrow transplantation. Blood 1989, 73, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Attal, M.; Harousseau, J.L.; Stoppa, A.M.; Sotto, J.J.; Fuzibet, J.G.; Rossi, J.F.; Casassus, P.; Maisonneuve, H.; Facon, T.; Ifrah, N.; et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Français du Myélome. N. Engl. J. Med. 1996, 335, 91–97. [Google Scholar] [CrossRef]
- Moreau, P.; Avet-Loiseau, H.; Harousseau, J.L.; Attal, M. Current trends in autologous stem-cell transplantation for myeloma in the era of novel therapies. J. Clin. Oncol. 2011, 29, 1898–1906. [Google Scholar] [CrossRef]
- Child, J.A.; Morgan, G.J.; Davies, F.E.; Owen, R.G.; Bell, S.E.; Hawkins, K.; Brown, J.; Drayson, M.T.; Selby, P.J. High-Dose Chemotherapy with Hematopoietic Stem-Cell Rescue for Multiple Myeloma. N. Engl. J. Med. 2003, 348, 1875–1883. [Google Scholar] [CrossRef]
- Schmitz, N.; Pfistner, B.; Sextro, M.; Sieber, M.; Carella, A.M.; Haenel, M.; Boissevain, F.; Zschaber, R.; Müller, P.; Kirchner, H.; et al. Aggressive conventional chemotherapy compared with high-dose chemotherapy with autologous haemopoietic stem-cell transplantation for relapsed chemosensitive Hodgkin’s disease: A randomised trial. Lancet 2002, 359, 2065–2071. [Google Scholar] [CrossRef]
- Mills, W.; Chopra, R.; McMillan, A.; Pearce, R.; Linch, D.C.; Goldstone, A.H. BEAM chemotherapy and autologous bone marrow transplantation for patients with relapsed or refractory non-Hodgkin’s lymphoma. J. Clin. Oncol. 1995, 13, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Seiden, M.V.; Elias, A.; Ayash, L.; Hunt, M.; Eder, J.P.; Schnipper, L.E.; Frei, E., 3rd; Antman, K.H. Pulmonary toxicity associated with high dose chemotherapy in the treatment of solid tumors with autologous marrow transplant: An analysis of four chemotherapy regimens. Bone Marrow. Transpl. 1992, 10, 57–63. [Google Scholar]
- Cao, T.M.; Negrin, R.S.; Stockerl-Goldstein, K.E.; Johnston, L.J.; Shizuru, J.A.; Taylor, T.L.; Rizk, N.W.; Wong, R.M.; Blume, K.G.; Hu, W.W. Pulmonary toxicity syndrome in breast cancer patients undergoing BCNU-containing high-dose chemotherapy and autologous hematopoietic cell transplantation. Biol. Blood Marrow. Transpl. 2000, 6, 387–394. [Google Scholar] [CrossRef][Green Version]
- Alessandrino, E.P.; Bernasconi, P.; Colombo, A.; Caldera, D.; Martinelli, G.; Vitulo, P.; Malcovati, L.; Nascimbene, C.; Varettoni, M.; Volpini, E.; et al. Pulmonary toxicity following carmustine-based preparative regimens and autologous peripheral blood progenitor cell transplantation in hematological malignancies. Bone Marrow. Transplant. 2000, 25, 309–313. [Google Scholar] [CrossRef]
- Visani, G.; Stefani, P.M.; Capria, S.; Malerba, L.; Galieni, P.; Gaudio, F.; Specchia, G.; Meloni, G.; Gherlinzoni, F.; Gonella, R.; et al. Bendamustine, etoposide, cytarabine, melphalan, and autologous stem cell rescue produce a 72% 3-year PFS in resistant lymphoma. Blood 2014, 124, 3029–3031. [Google Scholar] [CrossRef][Green Version]
- Khouri, I.F.; Jabbour, E.J.; Ledesma, C.; Korbling, M.; Alousi, A.M.; Anderlini, P.; Oran, B.; Ciurea, S.O.; Fayad, L.E.; Bassett, R.L., Jr.; et al. Bfr (bendamustine, fludarabine, rituximab) Nonmyeloablative Allogeneic Conditioning for Lymphoid Malignancies: 8-Year Results. Blood 2017, 130, 2036-2036. [Google Scholar] [CrossRef]
- Switzer, G.E.; Bruce, J.G.; Myaskovsky, L.; DiMartini, A.; Shellmer, D.; Confer, D.L.; Abress, L.K.; King, R.J.; Harnaha, A.G.; Ohngemach, S.; et al. Race and ethnicity in decisions about unrelated hematopoietic stem cell donation. Blood 2013, 121, 1469–1476. [Google Scholar] [CrossRef]
- Gragert, L.; Eapen, M.; Williams, E.; Freeman, J.; Spellman, S.; Baitty, R.; Hartzman, R.; Rizzo, J.D.; Horowitz, M.; Confer, D.; et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N. Engl. J. Med. 2014, 371, 339–348. [Google Scholar] [CrossRef]
- Pidala, J.; Kim, J.; Schell, M.; Lee, S.J.; Hillgruber, R.; Nye, V.; Ayala, E.; Alsina, M.; Betts, B.; Bookout, R.; et al. Race/ethnicity affects the probability of finding an HLA-A, -B, -C and -DRB1 allele-matched unrelated donor and likelihood of subsequent transplant utilization. Bone Marrow. Transpl. 2013, 48, 346–350. [Google Scholar] [CrossRef]
- Handgretinger, R. Haploidentical transplantation: The search for the best donor. Blood 2014, 124, 827–828. [Google Scholar] [CrossRef]
- Katsanis, E.; Sapp, L.N.; Reid, S.C.; Reddivalla, N.; Stea, B. T-Cell Replete Myeloablative Haploidentical Bone Marrow Transplantation Is an Effective Option for Pediatric and Young Adult Patients With High-Risk Hematologic Malignancies. Front. Pediatrics 2020, 8. [Google Scholar] [CrossRef]
- Martelli, M.F.; Di Ianni, M.; Ruggeri, L.; Pierini, A.; Falzetti, F.; Carotti, A.; Terenzi, A.; Reisner, Y.; Aversa, F.; Falini, B.; et al. "Designed" grafts for HLA-haploidentical stem cell transplantation. Blood 2014, 123, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Martelli, M.F.; Ianni, M.D.; Ruggeri, L.; Falzetti, F.; Carotti, A.; Reisner, Y.; Velardi, A. Next generation HLA-haploidentical HSCT. Bone Marrow Transpl. 2015, 50 (Suppl. 2), S63–S66. [Google Scholar] [CrossRef] [PubMed]
- Raiola, A.; Dominietto, A.; Varaldo, R.; Ghiso, A.; Galaverna, F.; Bramanti, S.; Todisco, E.; Sarina, B.; Giordano, L.; Ibatici, A.; et al. Unmanipulated haploidentical BMT following non-myeloablative conditioning and post-transplantation CY for advanced Hodgkin’s lymphoma. Bone Marrow. Transpl. 2014, 49, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, E.J. Haploidentical transplantation for hematologic malignancies: Where do we stand? Hematol. Am. Soc. Hematol. Educ. Program. 2012, 2012, 230–236. [Google Scholar] [CrossRef]
- Lee, C.J.; Savani, B.N.; Mohty, M.; Labopin, M.; Ruggeri, A.; Schmid, C.; Baron, F.; Esteve, J.; Gorin, N.C.; Giebel, S.; et al. Haploidentical hematopoietic cell transplantation for adult acute myeloid leukemia: A position statement from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica 2017, 102, 1810–1822. [Google Scholar] [CrossRef]
- Zheng, F.-M.; Zhang, X.; Li, C.-F.; Cheng, Y.-F.; Gao, L.; He, Y.-L.; Wang, Y.; Huang, X.-J. Haploidentical- versus identical-sibling transplant for high-risk pediatric AML: A multi-center study. Cancer Commun. 2020, 40, 93–104. [Google Scholar] [CrossRef]
- Sanz, J.; Galimard, J.-E.; Labopin, M.; Afanasyev, B.; Angelucci, E.; Ciceri, F.; Blaise, D.; Cornelissen, J.J.; Meijer, E.; Diez-Martin, J.L.; et al. Post-transplant cyclophosphamide after matched sibling, unrelated and haploidentical donor transplants in patients with acute myeloid leukemia: A comparative study of the ALWP EBMT. J. Hematol. Oncol. 2020, 13, 1–13. [Google Scholar] [CrossRef]
- Luznik, L.; O’Donnell, P.V.; Fuchs, E.J. Post-transplantation cyclophosphamide for tolerance induction in HLA-haploidentical bone marrow transplantation. Semin. Oncol. 2012, 39, 683–693. [Google Scholar] [CrossRef]
- Luznik, L.; Fuchs, E.J. High-dose, post-transplantation cyclophosphamide to promote graft-host tolerance after allogeneic hematopoietic stem cell transplantation. Immunol. Res. 2010, 47, 65–77. [Google Scholar] [CrossRef]
- Brodsky, R.A.; Luznik, L.; Bolanos-Meade, J.; Leffell, M.S.; Jones, R.J.; Fuchs, E.J. Reduced intensity HLA-haploidentical BMT with post transplantation cyclophosphamide in nonmalignant hematologic diseases. Bone Marrow. Transplant. 2008, 42, 523–527. [Google Scholar] [CrossRef] [PubMed]
- McCurdy, S.R.; Kanakry, J.A.; Showel, M.M.; Tsai, H.L.; Bolaños-Meade, J.; Rosner, G.L.; Kanakry, C.G.; Perica, K.; Symons, H.J.; Brodsky, R.A.; et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood 2015, 125, 3024–3031. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, E.J. HLA-haploidentical blood or marrow transplantation with high-dose, post-transplantation cyclophosphamide. Bone Marrow. Transpl. 2015, 50 (Suppl. 2), S31–S36. [Google Scholar] [CrossRef]
- Castagna, L.; Bramanti, S.; Furst, S.; Giordano, L.; Crocchiolo, R.; Sarina, B.; Mauro, E.; Morabito, L.; Bouabdallah, R.; Coso, D.; et al. Nonmyeloablative conditioning, unmanipulated haploidentical SCT and post-infusion CY for advanced lymphomas. Bone Marrow. Transpl. 2014, 49, 1475–1480. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bacigalupo, A.; Dominietto, A.; Ghiso, A.; Di Grazia, C.; Lamparelli, T.; Gualandi, F.; Bregante, S.; Van Lint, M.T.; Geroldi, S.; Luchetti, S.; et al. Unmanipulated haploidentical bone marrow transplantation and post-transplant cyclophosphamide for hematologic malignanices following a myeloablative conditioning: An update. Bone Marrow Transpl. 2015, 50 (Suppl. 2), S37–S39. [Google Scholar] [CrossRef]
- Locatelli, F.; Bauquet, A.; Palumbo, G.; Moretta, F.; Bertaina, A. Negative depletion of alpha/beta+ T cells and of CD19+ B lymphocytes: A novel frontier to optimize the effect of innate immunity in HLA-mismatched hematopoietic stem cell transplantation. Immunol. Lett. 2013, 155, 21–23. [Google Scholar] [CrossRef] [PubMed]
- Federmann, B.; Bornhauser, M.; Meisner, C.; Kordelas, L.; Beelen, D.W.; Stuhler, G.; Stelljes, M.; Schwerdtfeger, R.; Christopeit, M.; Behre, G.; et al. Haploidentical allogeneic hematopoietic cell transplantation in adults using CD3/CD19 depletion and reduced intensity conditioning: A phase II study. Haematologica 2012, 97, 1523–1531. [Google Scholar] [CrossRef]
- Dvorak, C.C.; Gilman, A.L.; Horn, B.; Oon, C.Y.; Dunn, E.A.; Baxter-Lowe, L.A.; Cowan, M.J. Haploidentical related-donor hematopoietic cell transplantation in children using megadoses of CliniMACs-selected CD34(+) cells and a fixed CD3(+) dose. Bone Marrow. Transpl. 2013, 48, 508–513. [Google Scholar] [CrossRef]
- Munchel, A.T.; Kasamon, Y.L.; Fuchs, E.J. Treatment of hematological malignancies with nonmyeloablative, HLA-haploidentical bone marrow transplantation and high dose, post-transplantation cyclophosphamide. Best Pract. Res. Clin. Haematol. 2011, 24, 359–368. [Google Scholar] [CrossRef]
- Katsanis, E.; Sapp, L.N.; Varner, N.; Koza, S.; Stea, B.; Zeng, Y. Haploidentical Bone Marrow Transplantation with Post-Transplant Cyclophosphamide/Bendamustine in Pediatric and Young Adult Patients with Hematologic Malignancies. Biol Blood Marrow. Transpl. 2018, 24, 2034–2039. [Google Scholar] [CrossRef]
- Katsanis, E.; Maher, K.; Roe, D.J.; Simpson, R.J. Progressive substitution of posttransplant cyclophosphamide with bendamustine: A phase I study in haploidentical bone marrow transplantation. eJHaem 2020, 1, 286–292. [Google Scholar] [CrossRef]
- Moiseev, I.S.; Bondarenko, S.N.; Darskaya, E.I.; Alyanski, A.; Borzenkova, E.; Dotcenko, A.; Kudyasheva, O.; Lapin, S.; Surkova, E.; Ovechkina, V.N.; et al. Graft-Versus Host Disease Prophylaxis with Postransplantation Bendamustine in Refractory Leaukemia Patients. Blood 2019, 134, 5746-5746. [Google Scholar] [CrossRef]
- The 46th Annual Meeting of the European Society for Blood and Marrow Transplantation: Physicians Poster Session (P001-P706). Bone Marrow. Transplant. 2020, 55, 181–714. [CrossRef] [PubMed]
- Highfill, S.L.; Rodriguez, P.C.; Zhou, Q.; Goetz, C.A.; Koehn, B.H.; Veenstra, R.; Taylor, P.A.; Panoskaltsis-Mortari, A.; Serody, J.S.; Munn, D.H.; et al. Bone marrow myeloid-derived suppressor cells (MDSCs) inhibit graft-versus-host disease (GVHD) via an arginase-1–dependent mechanism that is up-regulated by interleukin-13. Blood 2010, 116, 5738–5747. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Yu, Y.; Haarberg, K.; Fu, J.; Kaosaard, K.; Nagaraj, S.; Anasetti, C.; Gabrilovich, D.; Yu, X.Z. Dynamic change and impact of myeloid-derived suppressor cells in allogeneic bone marrow transplantation in mice. Biol. Blood Marrow. Transpl. 2013, 19, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Joo, Y.D.; Lee, S.M.; Lee, S.W.; Lee, W.S.; Lee, S.M.; Park, J.K.; Choi, I.W.; Park, S.G.; Choi, I.; Seo, S.K. Granulocyte colony-stimulating factor-induced immature myeloid cells inhibit acute graft-versus-host disease lethality through an indoleamine dioxygenase-independent mechanism. Immunology 2009, 128, e632–e640. [Google Scholar] [CrossRef] [PubMed]
- Messmann, J.J.; Reisser, T.; Leithauser, F.; Lutz, M.B.; Debatin, K.M.; Strauss, G. In vitro-generated MDSCs prevent murine GVHD by inducing type 2 T cells without disabling antitumor cytotoxicity. Blood 2015, 126, 1138–1148. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Chen, H.-M.; Ma, G.; Zhou, Z.; Raulet, D.; Rivera, A.L.; Chen, S.-H.; Pan, P.-Y. The mechanistic study behind suppression of GVHD while retaining GVL activities by myeloid-derived suppressor cells. Leukemia 2019, 33, 2078–2089. [Google Scholar] [CrossRef]
- Fan, Q.; Liu, H.; Liang, X.; Yang, T.; Fan, Z.; Huang, F.; Ling, Y.; Liao, X.; Xuan, L.; Xu, N.; et al. Superior GVHD-free, relapse-free survival for G-BM to G-PBSC grafts is associated with higher MDSCs content in allografting for patients with acute leukemia. J. Hematol. Oncol. 2017, 10, 135. [Google Scholar] [CrossRef] [PubMed]
- Vendramin, A.; Gimondi, S.; Bermema, A.; Longoni, P.; Rizzitano, S.; Corradini, P.; Carniti, C. Graft monocytic myeloid-derived suppressor cell content predicts the risk of acute graft-versus-host disease after allogeneic transplantation of granulocyte colony-stimulating factor-mobilized peripheral blood stem cells. Biol. Blood Marrow. Transpl. 2014, 20, 2049–2055. [Google Scholar] [CrossRef]
- Yin, J.; Wang, C.; Huang, M.; Mao, X.; Zhou, J.; Zhang, Y. Circulating CD14(+) HLA-DR(-/low) myeloid-derived suppressor cells in leukemia patients with allogeneic hematopoietic stem cell transplantation: Novel clinical potential strategies for the prevention and cellular therapy of graft-versus-host disease. Cancer Med. 2016, 5, 1654–1669. [Google Scholar] [CrossRef]
- Betts, B.C.; Bastian, D.; Iamsawat, S.; Nguyen, H.; Heinrichs, J.L.; Wu, Y.; Daenthanasanmak, A.; Veerapathran, A.; O’Mahony, A.; Walton, K.; et al. Targeting JAK2 reduces GVHD and xenograft rejection through regulation of T cell differentiation. Proc. Natl. Acad. Sci. USA 2018, 115, 1582–1587. [Google Scholar] [CrossRef]
- Nikolic, B.; Lee, S.; Bronson, R.T.; Grusby, M.J.; Sykes, M. Th1 and Th2 mediate acute graft-versus-host disease, each with distinct end-organ targets. J. Clin. Investig. 2000, 105, 1289–1298. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.C.; Joller, N.; Kuchroo, V.K. Lag-3, Tim-3, and TIGIT: Co-inhibitory Receptors with Specialized Functions in Immune Regulation. Immunity 2016, 44, 989–1004. [Google Scholar] [CrossRef]
- Taylor, P.A.; Panoskaltsis-Mortari, A.; Freeman, G.J.; Sharpe, A.H.; Noelle, R.J.; Rudensky, A.Y.; Mak, T.W.; Serody, J.S.; Blazar, B.R. Targeting of inducible costimulator (ICOS) expressed on alloreactive T cells down-regulates graft-versus-host disease (GVHD) and facilitates engraftment of allogeneic bone marrow (BM). Blood 2005, 105, 3372–3380. [Google Scholar] [CrossRef] [PubMed]
- Hotta, M.; Yoshimura, H.; Satake, A.; Tsubokura, Y.; Ito, T.; Nomura, S. GM-CSF therapy inhibits chronic graft-versus-host disease via expansion of regulatory T cells. Eur. J. Immunol. 2019, 49, 179–191. [Google Scholar] [CrossRef]
- Taylor, P.A.; Lees, C.J.; Blazar, B.R. The infusion of ex vivo activated and expanded CD4(+)CD25(+) immune regulatory cells inhibits graft-versus-host disease lethality. Blood 2002, 99, 3493–3499. [Google Scholar] [CrossRef] [PubMed]
- Pierini, A.; Colonna, L.; Alvarez, M.; Schneidawind, D.; Nishikii, H.; Baker, J.; Pan, Y.; Florek, M.; Kim, B.-S.; Negrin, R.S. Donor Requirements for Regulatory T Cell Suppression of Murine Graft-versus-Host Disease. J. Immunol. 2015, 195, 347. [Google Scholar] [CrossRef]
- Nagaraj, S.; Gupta, K.; Pisarev, V.; Kinarsky, L.; Sherman, S.; Kang, L.; Herber, D.L.; Schneck, J.; Gabrilovich, D.I. Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer. Nat. Med. 2007, 13, 828. Available online: https://www.nature.com/articles/nm1609#supplementary-information (accessed on 29 January 2020). [CrossRef]
- Yang, F.; Li, Y.; Wu, T.; Na, N.; Zhao, Y.; Li, W.; Han, C.; Zhang, L.; Lu, J.; Zhao, Y. TNFalpha-induced M-MDSCs promote transplant immune tolerance via nitric oxide. J. Mol. Med. 2016, 94, 911–920. [Google Scholar] [CrossRef]
- Zeiser, R.; Leveson-Gower, D.B.; Zambricki, E.A.; Kambham, N.; Beilhack, A.; Loh, J.; Hou, J.Z.; Negrin, R.S. Differential impact of mammalian target of rapamycin inhibition on CD4+CD25+Foxp3+ regulatory T cells compared with conventional CD4+ T cells. Blood 2008, 111, 453–462. [Google Scholar] [CrossRef]
- Nguyen, V.H.; Shashidhar, S.; Chang, D.S.; Ho, L.; Kambham, N.; Bachmann, M.; Brown, J.M.; Negrin, R.S. The impact of regulatory T cells on T-cell immunity following hematopoietic cell transplantation. Blood 2008, 111, 945–953. [Google Scholar] [CrossRef]
- Ermann, J.; Hoffmann, P.; Edinger, M.; Dutt, S.; Blankenberg, F.G.; Higgins, J.P.; Negrin, R.S.; Fathman, C.G.; Strober, S. Only the CD62L+ subpopulation of CD4+CD25+ regulatory T cells protects from lethal acute GVHD. Blood 2005, 105, 2220–2226. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, S.; Ross, D.B.; Panoskaltsis-Mortari, A.; Kanakry, C.G.; Blazar, B.R.; Levy, R.B.; Luznik, L. Donor CD4(+) Foxp3(+) regulatory T cells are necessary for posttransplantation cyclophosphamide-mediated protection against GVHD in mice. Blood 2014, 124, 2131–2141. [Google Scholar] [CrossRef] [PubMed]
- Schultz, K.R.; Paquet, J.; Bader, S.; HayGlass, K.T. Requirement for B cells in T cell priming to minor histocompatibility antigens and development of graft-versus-host disease. Bone Marrow. Transpl. 1995, 16, 289–295. [Google Scholar]
- Srinivasan, M.; Flynn, R.; Price, A.; Ranger, A.; Browning, J.L.; Taylor, P.A.; Ritz, J.; Antin, J.H.; Murphy, W.J.; Luznik, L.; et al. Donor B-cell alloantibody deposition and germinal center formation are required for the development of murine chronic GVHD and bronchiolitis obliterans. Blood 2012, 119, 1570–1580. [Google Scholar] [CrossRef] [PubMed]
- Young, J.S.; Wu, T.; Chen, Y.; Zhao, D.; Liu, H.; Yi, T.; Johnston, H.; Racine, J.; Li, X.; Wang, A.; et al. Donor B cells in transplants augment clonal expansion and survival of pathogenic CD4+ T cells that mediate autoimmune-like chronic graft-versus-host disease. J. Immunol. 2012, 189, 222–233. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Gao, Q.; Feng, Y.; Zhang, X. Developing role of B cells in the pathogenesis and treatment of chronic GVHD. Br. J. Haematol. 2019, 184, 323–336. [Google Scholar] [CrossRef] [PubMed]
- Le Huu, D.; Matsushita, T.; Jin, G.; Hamaguchi, Y.; Hasegawa, M.; Takehara, K.; Tedder, T.F.; Fujimoto, M. Donor-derived regulatory B cells are important for suppression of murine sclerodermatous chronic graft-versus-host disease. Blood 2013, 121, 3274–3283. [Google Scholar] [CrossRef]
- Lu, L.; Yoshimoto, K.; Morita, A.; Kameda, H.; Takeuchi, T. Bendamustine increases interleukin-10 secretion from B cells via p38 MAP kinase activation. Int. Immunopharmacol. 2016, 39, 273–279. [Google Scholar] [CrossRef]
- Shlomchik, W.D.; Couzens, M.S.; Tang, C.B.; McNiff, J.; Robert, M.E.; Liu, J.; Shlomchik, M.J.; Emerson, S.G. Prevention of graft versus host disease by inactivation of host antigen-presenting cells. Science 1999, 285, 412–415. [Google Scholar] [CrossRef]
- Blazar, B.R.; Murphy, W.J.; Abedi, M. Advances in graft-versus-host disease biology and therapy. Nat. Rev. Immunol. 2012, 12, 443–458. [Google Scholar] [CrossRef]
- Molina, M.S.; Stokes, J.; Hoffman, E.A.; Eremija, J.; Zeng, Y.; Simpson, R.J.; Katsanis, E. Bendamustine Conditioning Skews Murine Host DCs Toward Pre-cDC1s and Reduces GvHD Independently of Batf3. Front Immunol. 2020, 11, 1410. [Google Scholar] [CrossRef]
- Markey, K.A.; Kuns, R.D.; Browne, D.J.; Gartlan, K.H.; Robb, R.J.; Martins, J.P.; Henden, A.S.; Minnie, S.A.; Cheong, M.; Koyama, M.; et al. Flt-3L Expansion of Recipient CD8α(+) Dendritic Cells Deletes Alloreactive Donor T Cells and Represents an Alternative to Posttransplant Cyclophosphamide for the Prevention of GVHD. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2018, 24, 1604–1616. [Google Scholar] [CrossRef]
- Toubai, T.; Malter, C.; Tawara, I.; Liu, C.; Nieves, E.; Lowler, K.P.; Sun, Y.; Reddy, P. Immunization with host-type CD8{alpha}+ dendritic cells reduces experimental acute GVHD in an IL-10-dependent manner. Blood 2010, 115, 724–735. [Google Scholar] [CrossRef] [PubMed]
- Toubai, T.; Mathewson, N.; Oravecz-Wilson, K.; Reddy, P. Host CD8α+Dendritic Cells May Be a Key Factor for Separating Graft-versus-Host Disease from Graft-versus-Leukemia. Biol. Blood Marrow. Transplant. 2015, 21, 775–776. [Google Scholar] [CrossRef][Green Version]
- Kazi, J.U.; Ronnstrand, L. FMS-like Tyrosine Kinase 3/FLT3: From Basic Science to Clinical Implications. Physiol. Rev. 2019, 99, 1433–1466. [Google Scholar] [CrossRef]
- Ma, W.; Liang, F.; Zhan, H.; Jiang, X.; Gao, C.; Zhang, X.; Zhang, K.; Sun, Q.; Hu, H.; Zhao, Z. Activated FMS-like tyrosine kinase 3 ameliorates angiotensin II-induced cardiac remodelling. Acta Physiol. 2020, 230, e13519. [Google Scholar] [CrossRef]
- Ho, N.I.; Camps, M.G.M.; Verdoes, M.; Munz, C.; Ossendorp, F. Autophagy regulates long-term cross-presentation by murine dendritic cells. Eur. J. Immunol. 2020. [Google Scholar] [CrossRef]
- Park, D.; Lapteva, N.; Seethammagari, M.; Slawin, K.M.; Spencer, D.M. An essential role for Akt1 in dendritic cell function and tumor immunotherapy. Nat. Biotechnol. 2006, 24, 1581–1590. [Google Scholar] [CrossRef]
- Yu, H.; Pardoll, D.; Jove, R. STATs in cancer inflammation and immunity: A leading role for STAT3. Nat. Rev. Cancer 2009, 9, 798–809. [Google Scholar] [CrossRef]
- Yu, H.; Jove, R. The STATs of cancer—new molecular targets come of age. Nat. Rev. Cancer 2004, 4, 97–105. [Google Scholar] [CrossRef]
| N | Age | Donor Graft | Disease | Remission Status % | Regimen | Engraft % | aGvHD II-IV % | cGvHD % | NRM % | OS % | PFS % | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Khouri (Houston, Texas) 2009- NCT00880815 Phase I/II Dose escalation of BEN (70, 90, 110, and 130 mg/m2) | 69 closed | 30-72 | MSD or MUD PBSC or BM | CLL Lymph | 42 CR 46 PR 12 RD | RIC FLU-BEN- -Ritux | 100 | 17 | 31 | 9 | 74 @ 5y | 60 @ 5yr |
| Khouri (Houston, Texas) 2009- NCT00880815; NCT00899431 Evaluation of BFR conditioning compared to FCR | 26 closed | 49-72 | MSD or MUD PBSC or BM | CLL | 8 CR 54 PR 38 RD | RIC FLU-BEN- -Ritux or FLU-CY-Ritux | 100 | 23 | 45 | 8 | 82 @ 3y | 63 @ 3y |
| N | Age | Donor Graft | Disease | Remission Status % | Regimen | Engraft % | aGvHD III-IV % | cGvHD % | NRM % | Relapse % | OS % | EFS % | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Katsanis (Tucson, Arizona) 2016- NCT02996773 Phase I/Ib
de-escalation of PT-CY
| 9 ongoing | 9–42 | Haplo BM | Leuk Lymph | 33 CR1 22 CR2 22 >CR2 22 PR | MAC TBI-FLU or BU-FLU-MEL | 100 | 0 | 0 | 0 | 29 @ 2yr | 83 @ 2y | 71 @ 2yr |
| Moiseev (St. Petersburg, Russia) 2016- NCT02799147 Phase I/II
| 26 closed | 20–56 | MSD or MUD or Haplo PBSC | Leuk | RD | MAC BU-FLU | 92 | 43 30 33 | 70 | 43 | 19 | 29 40 70 @ 1y | 29 40 27 @ 1y |
| Khouri (Houston, Texas) 2019- NCT04022239 Phase I/II
| ongoing | 18–65 | Haplo or MMUD PBSC | Leuk Lymph | ? | RIC FLU-MEL-TBI or FLU-BEN-TBI ± Ritux | - | - | - | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stokes, J.; Molina, M.S.; Hoffman, E.A.; Simpson, R.J.; Katsanis, E. Immunomodulatory Effects of Bendamustine in Hematopoietic Cell Transplantation. Cancers 2021, 13, 1702. https://doi.org/10.3390/cancers13071702
Stokes J, Molina MS, Hoffman EA, Simpson RJ, Katsanis E. Immunomodulatory Effects of Bendamustine in Hematopoietic Cell Transplantation. Cancers. 2021; 13(7):1702. https://doi.org/10.3390/cancers13071702
Chicago/Turabian StyleStokes, Jessica, Megan S. Molina, Emely A. Hoffman, Richard J. Simpson, and Emmanuel Katsanis. 2021. "Immunomodulatory Effects of Bendamustine in Hematopoietic Cell Transplantation" Cancers 13, no. 7: 1702. https://doi.org/10.3390/cancers13071702
APA StyleStokes, J., Molina, M. S., Hoffman, E. A., Simpson, R. J., & Katsanis, E. (2021). Immunomodulatory Effects of Bendamustine in Hematopoietic Cell Transplantation. Cancers, 13(7), 1702. https://doi.org/10.3390/cancers13071702







