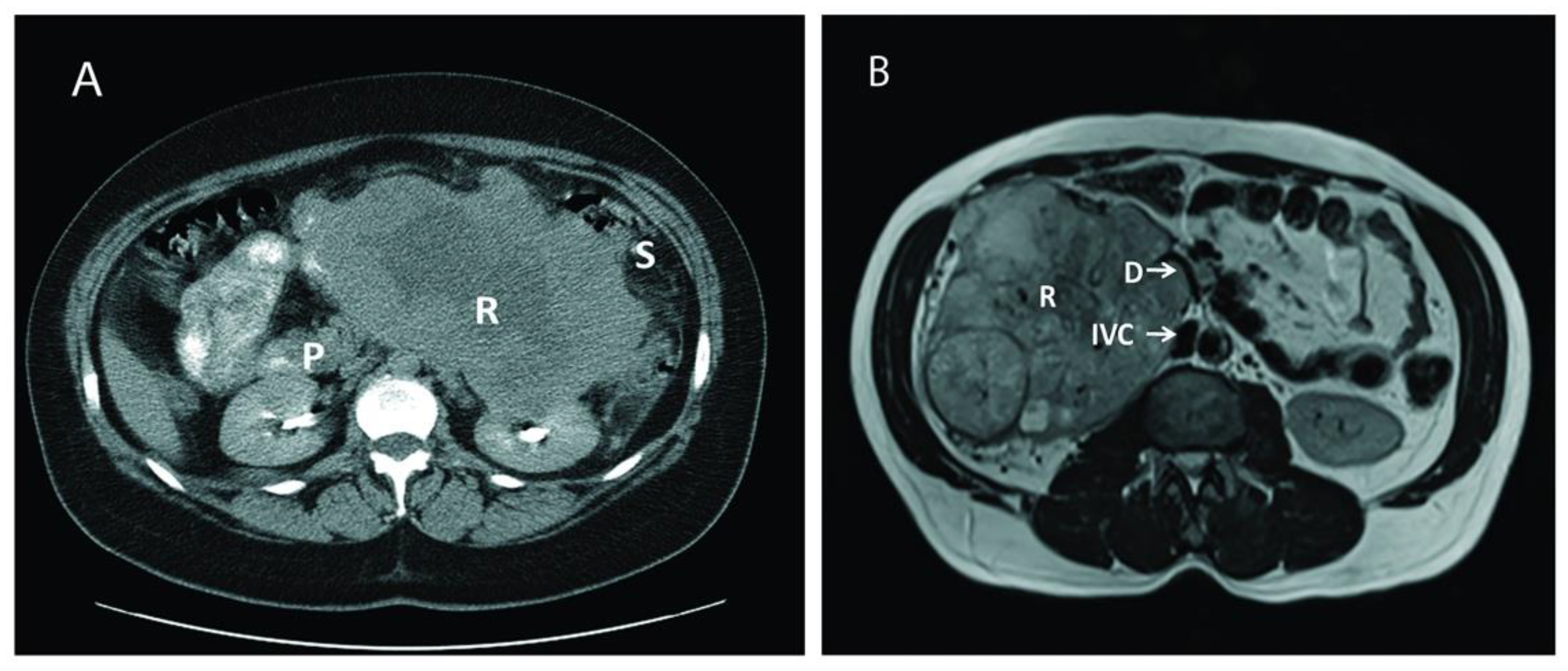
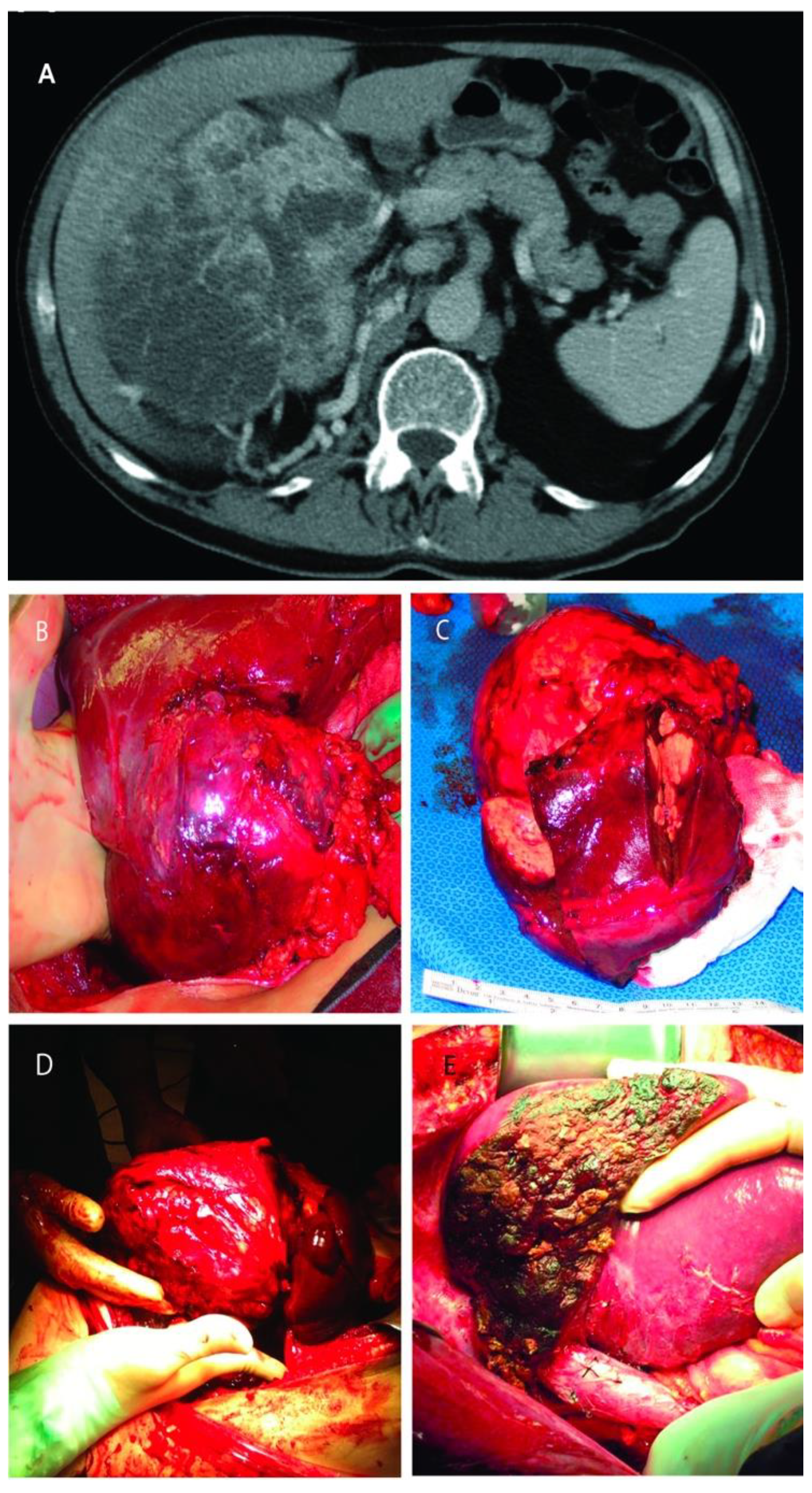
Renal Cell Carcinoma with or without Tumor Thrombus Invading the Liver, Pancreas and Duodenum
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
Surgical Technique
3. Results
3.1. Patient Demographics
3.2. Intra-Operative Outcomes
3.3. Surgical Outcomes
3.4. Oncological Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Thuret, R.; Abdollah, F.; Lughezzani, G.; Schmitges, J.; Tian, Z.; Shariat, S.F.; Montorsi, F.; Patard, J.J.; Perrotte, P.; et al. Age-adjusted incidence, mortality, and survival rates of stage-specific renal cell carcinoma in North America: A trend analysis. Eur. Urol. 2011, 59, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Frees, S.K.; Kamal, M.M.; Nestler, S.; Levien, P.M.; Bidnur, S.; Brenner, W.; Thomas, C.; Jaeger, W.; Thüroff, J.W.; Roos, F.C. Risk-adjusted proposal for >60 months follow up after surgical treatment of organ-confined renal cell carcinoma according to life expectancy. Int. J. Urol. 2019, 26, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Ciancio, G.; Gonzalez, J.; Shirodkar, S.P.; Angulo, J.C.; Soloway, M.S. Liver transplantation techniques for the surgical management of renal cell carcinoma with tumor thrombus in the inferior vena cava: Step-by-step description. Eur. Urol. 2011, 59, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Ciancio, G.; Livingstone, A.S.; Soloway, M. Surgical management of renal cell carcinoma with tumor thrombus in the renal and inferior vena cava: The University of Miami experience in using liver transplantation techniques. Eur. Urol. 2007, 51, 988–994. [Google Scholar] [CrossRef]
- Gupta, K.; Miller, J.D.; Li, J.Z.; Russell, M.W.; Charbonneau, C. Epidemiologic and socioeconomic burden of metastatic renal cell carcinoma (mRCC): A literature review. Cancer Treat. Rev. 2008, 34, 193–205. [Google Scholar] [CrossRef]
- Ciancio, G.; Hawke, C.; Soloway, M. The use of liver transplant techniques to aid in the surgical management of urological tumors. J. Urol. 2000, 164, 665–672. [Google Scholar] [CrossRef]
- Pikoulis, E.; Margonis, G.A.; Antoniou, E. Surgical Management of Renal Cell Cancer Liver Metastases. Scand J. Surg. 2016, 105, 263–268. [Google Scholar] [CrossRef]
- Benhaim, R.; Oussoultzoglou, E.; Saeedi, Y.; Mouracade, P.; Bachellier, P.; Lang, H. Pancreatic metastasis from clear cell renal cell carcinoma: Outcome of an aggressive approach. Urology 2015, 85, 135–140. [Google Scholar] [CrossRef]
- Chatzizacharias, N.A.; Rosich-Medina, A.; Dajani, K.; Harper, S.; Huguet, E.; Liau, S.S.; Praseedom, R.K.; Jah, A. Surgical management of hepato-pancreatic metastasis from renal cell carcinoma. World J. Gastrointest. Oncol. 2017, 9, 70–77. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Huntington, J.T.; Butterfield, M.; Fisher, J.; Torrent, D.; Bloomston, M. The Social Security Death Index (SSDI) most accurately reflects true survival for older oncology patients. Am. J. Cancer Res. 2013, 3, 518–522. [Google Scholar] [PubMed]
- Ciancio, G.; Vaidya, A.; Shirodkar, S.; Manoharan, M.; Hakky, T.; Soloway, M. En bloc mobilization of the pancreas and spleen to facilitate resection of large tumors, primarily renal and adrenal, in the left upper quadrant of the abdomen: Techniques derived from multivisceral transplantation. Eur. Urol. 2009, 55, 1106–1111. [Google Scholar] [CrossRef]
- Ciancio, G.; Vaidya, A.; Soloway, M. Early ligation of the renal artery using the posterior approach: A basic surgical concept reinforced during resection of large hypervascular renal cell carcinoma with or without inferior vena cava thrombus. BJU Int. 2003, 92, 488–489. [Google Scholar] [CrossRef] [PubMed]
- Manoharan, A.; Lugo-Baruqui, A.; Ciancio, G. Radical Nephrectomy and Pulmonary Lobectomy for Renal Cell Carcinoma with Tumor Thrombus Extension into the Inferior Vena Cava and Pulmonary Arteries. Anticancer Res. 2020, 40, 5837–5844. [Google Scholar] [CrossRef] [PubMed]
- Neves, R.J.; Zincke, H. Surgical treatment of renal cancer with vena cava extension. Br. J. Urol. 1987, 59, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Ciancio, G.; Vaidya, A.; Savoie, M.; Soloway, M. Management of renal cell carcinoma with level III thrombus in the inferior vena cava. J. Urol. 2002, 168, 1374–1377. [Google Scholar] [CrossRef]
- González, J.; Gorin, M.A.; Garcia-Roig, M.; Ciancio, G. Inferior vena cava resection and reconstruction: Technical considerations in the surgical management of renal cell carcinoma with tumor thrombus. Urol. Oncol. 2014, 32, 34–e19. [Google Scholar] [CrossRef] [PubMed]
- Swami, U.; Nussenzveig, R.H.; Haaland, B.; Agarwal, N. Revisiting AJCC TNM staging for renal cell carcinoma: Quest for improvement. Ann. Transl. Med. 2019, 7, S18. [Google Scholar] [CrossRef] [PubMed]
- Yezhelyev, M.; Master, V.; Egnatashvili, V.; Kooby, D.A. Combined nephrectomy and major hepatectomy: Indications, outcomes, and recommendations. J. Am. Coll. Surg. 2009, 208, 410–418. [Google Scholar] [CrossRef]
- Karellas, M.E.; Jang, T.L.; Kagiwada, M.A.; Kinnaman, M.D.; Jarnagin, W.R.; Russo, P. Advanced-stage renal cell carcinoma treated by radical nephrectomy and adjacent organ or structure resection. BJU Int. 2009, 103, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Margulis, V.; Sanchez-Ortiz, R.F.; Tamboli, P.; Cohen, D.D.; Swanson, D.A.; Wood, C.G. Renal cell carcinoma clinically involving adjacent organs: Experience with aggressive surgical management. Cancer 2007, 109, 2025–2030. [Google Scholar] [CrossRef] [PubMed]
- Peters, N.; Lightner, C.; McCaffrey, J. An Unusual Case of Gastrointestinal Bleeding in Metastatic Renal Cell Carcinoma. Case Rep. Oncol. 2020, 13, 738–741. [Google Scholar] [CrossRef] [PubMed]
- Munir, A.; Khan, A.M.; McCarthy, L.; Mehdi, S. An Unusual Case of Renal Cell Carcinoma Metastasis to Duodenum Presenting as Gastrointestinal Bleeding. JCO Oncol. Pract. 2020, 16, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.O.; Al-Rubaye, S.; Reilly, I.W.; McGoldrick, S. Renal cell carcinoma presenting as an upper gastrointestinal bleeding. BMJ Case Rep. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Schlussel, A.T.; Fowler, A.B.; Chinn, H.K.; Wong, L.L. Management of locally advanced renal cell carcinoma with invasion of the duodenum. Case Rep. Surg. 2013, 2013, 596362. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.; Gaynor, J.J.; Alameddine, M.; Esteban, M.; Ciancio, G. Indications, complications, and outcomes following surgical management of locally advanced and metastatic renal cell carcinoma. Expert Rev. Anticancer. Therapy 2018, 18, 237–250. [Google Scholar] [CrossRef]
- Dabestani, S.; Marconi, L.; Hofmann, F.; Stewart, F.; Lam, T.B.L.; E Canfield, S.; Staehler, M.; Powles, T.; Ljungberg, B.; Bex, A. Local treatments for metastases of renal cell carcinoma: A systematic review. Lancet Oncol. 2014, 15, e549–e561. [Google Scholar] [CrossRef]
- Achkar, T.; Maranchie, J.K.; Appleman, L.J. Metastasectomy in advanced renal cell carcinoma: A systematic review. Kidney Cancer 2019, 3, 31–40. [Google Scholar] [CrossRef]
- Alt, A.L.; Boorjian, S.A.; Ms, C.M.L.; Costello, B.A.; Leibovich, B.C.; Blute, M.L. Survival after complete surgical resection of multiple metastases from renal cell carcinoma. Cancer 2011, 117, 2873–2882. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Kidney Cancer (Version 2.2020). Available online: Https://www.nccn.org/professionals/physician_gls/pdf/kidney.pdf (accessed on 2 October 2020).
- Escudier, B.; Porta, C.; Schmidinger, M.; Rioux-Leclercq, N.; Bex, A.; Khoo, V.; Grünwald, V.; Gillessen, S.; Horwich, A. ESMO Guidelines Committee. Renal cell carcinoma: ESMO clinical practice guidelines for diagnosis, treatment, and follow-up. Ann. Oncol. 2019, 30, 706–720. [Google Scholar] [CrossRef]
- Krishnamurthi, V.; Novick, A.C.; Bukowski, R.M. Efficacy of multimodality therapy in advanced renal cell carcinoma. Urology 1998, 51, 933–937. [Google Scholar] [CrossRef]
- Margulis, V.; Matin, S.F.; Tannir, N.; Tamboli, P.; Swanson, D.A.; Jonasch, E.; Wood, C.G. Surgical morbidity associated with administration of targeted molecular therapies before cytoreductive nephrectomy or resection of locally recurrent renal cell carcinoma. J. Urol. 2008, 180, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Karam, J.A.; Rini, B.I.; Varella, L.; Garcia, J.A.; Dreicer, R.; Choueiri, T.K.; Jonasch, E.; Matin, S.F.; Campbell, S.C.; Wood, C.G.; et al. Metastasectomy after targeted therapy in patients with advanced renal cell carcinoma. J Urol. 2011, 185, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Shuch, B.; Riggs, S.B.; LaRochelle, J.C.; Kabbinavar, F.F.; Avakian, R.; Pantuck, A.J.; Belldegrun, A.S.; Patard, J.-J. Neoadjuvant targeted therapy and advanced kidney cancer: Observations and implications for a new treatment paradigm. BJU Int. 2008, 102, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Patard, J.-J.; Thuret, R.; Raffi, A.; Laguerre, B.; Bensalah, K.; Culine, S. Treatment with sunitinib enabled complete resection of massive lymphadenopathy not previously amenable to excision in a patient with renal cell carcinoma. Eur. Urol. 2009, 55, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Sternberg, C.N.; Hawkins, R.E.; Wagstaff, J.; Salman, P.; Mardiak, J.; Barrios, C.H.; Zarba, J.J.; Gladkov, O.A.; Lee, E.; Szczylik, C.; et al. Randomized, double-blind phase III study of pazopanib versus placebo in patients with metastatic renal cell carcinoma who have no evidence of disease following metastasectomy: A trial of the ECOG-ACRIN cancer research group (E2810). J. Clin. Oncol. 2019, 37, 4502. [Google Scholar] [CrossRef]
- Procopio, G.; Apollonio, G.; Cognetti, F.; Miceli, R.; Milella, M.; Mosca, A.; Chiuri, V.E.; Bearz, A.; Morelli, F.; Ortega, C.; et al. Sorafenib versus observation following radical metastasectomy for clear-cell renal cell carcinoma: Results from the phase 2 randomized open label RESORT study. Eur. Urol. Oncol. 2019, 2, 699–707. [Google Scholar] [CrossRef]

| Parameter | Value |
|---|---|
| No. of patients | 18 |
| Male, n (%) | 7 (38.9%) |
| Female, n (%) | 11 (61.1%) |
| Age, median (years) | 56 (40–76) |
| Follow up, median (months) | 24 months (0–108); 3 deaths at 13, 24, and 108 months post-surgery, respectively |
| Asymptomatic, n (%) | 4 (22%) |
| Symptomatic, n (%) | 14 (78%) |
| Abdominal pain | 8 (42%) |
| Hematuria | 3 (16.6%) |
| Fatigue | 3 (16.6%) |
| GI bleeding | 1 (5.5%) |
| Collapsed lung | 1 (5.5%) |
| Parameter | Value |
|---|---|
| Side of lesion, n (%) | |
| Left | 8 (38.8%) |
| Right | 11 (61.2%) |
| IVC involvement 1, n (%) | |
| Level I | 3 (16.6%) |
| Level II | 2 (11.1%) |
| Level III 2 | 2 (11.1%) |
| Tumor size (cm) | |
| Pancreatico-duodenal involvement | 14.5 (8.8–22) |
| Liver involvement | 10 (4–15) |
| EBL, median (mL) | 475 |
| Pancreatico-duodenal involvement | 300 (100–2500) |
| Liver involvement | 500 (200–4000) |
| IVC exploration | 750 (200–4000) |
| No IVC exploration | 300 (100–600) |
| Transfusion, median (PRBC units) | 1U for the total group of 18 patients; 4U among the 9 patients who required transfusions |
| Liver resection 3, n (%) | 7 (38.8%) |
| Pancreaticoduodenectomy, n (%) | 1 (5.5%) |
| Partial/subtotal pancreatectomy, n (%) | 7 (38.8%) |
| Distal pancreatectomy, n (%) | 1 (5.5%) |
| Other organs removed, n (%) | 2 (11%) |
| Partial duodenum | 3 (16.6%) |
| Spleen | 7 (38.8%) |
| Adrenal gland | 18 (100%) |
| Left colon | 1 (5.5%) |
| Complication | n (%) | Grade |
|---|---|---|
| Collection | 3 (16.6%) | IIIa |
| Pulmonary 1 | 2 (11.1%) | Iva |
| Atrial fibrillation | 1 (5.5%) | II |
| Wound infection | 1 (5.5%) | II |
| Deep venous thrombosis | 1 (5.5%) | IIIa |
| Pancreatitis | 1 (5.5%) | II |
| Pancreatic leak | 1 (5.5%) | IIIa |
| Variable | Value |
|---|---|
| AJCC pT4, n (%) | 18 (100%) |
| RCC conventional type, n (%) | 14 (77.7%) |
| Fuhrman Grade, median | |
| Pancreatico-duodenal involvement | IV |
| Liver involvement | III |
| Lymph node metastases, n (%) | |
| Pacreatico-duodenal involvement | 1 (9%) |
| Liver involvement | 2 (28.5%) |
| Median survival from time of resection (months) | |
| Pancreatico-duodenal involvement | 36 (13–108) |
| Liver involvement | 24 (12–96) |
| Actuarial 5-yr OS (%) | |
| Pancreatico-duodenal involvement | 84.6% |
| Liver involvement | 75% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González, J.; Gaynor, J.J.; Ciancio, G. Renal Cell Carcinoma with or without Tumor Thrombus Invading the Liver, Pancreas and Duodenum. Cancers 2021, 13, 1695. https://doi.org/10.3390/cancers13071695
González J, Gaynor JJ, Ciancio G. Renal Cell Carcinoma with or without Tumor Thrombus Invading the Liver, Pancreas and Duodenum. Cancers. 2021; 13(7):1695. https://doi.org/10.3390/cancers13071695
Chicago/Turabian StyleGonzález, Javier, Jeffrey J. Gaynor, and Gaetano Ciancio. 2021. "Renal Cell Carcinoma with or without Tumor Thrombus Invading the Liver, Pancreas and Duodenum" Cancers 13, no. 7: 1695. https://doi.org/10.3390/cancers13071695
APA StyleGonzález, J., Gaynor, J. J., & Ciancio, G. (2021). Renal Cell Carcinoma with or without Tumor Thrombus Invading the Liver, Pancreas and Duodenum. Cancers, 13(7), 1695. https://doi.org/10.3390/cancers13071695






