Successive Osteosarcoma Relapses after the First Line O2006/Sarcome-09 Trial: What Can We Learn for Further Phase-II Trials?
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
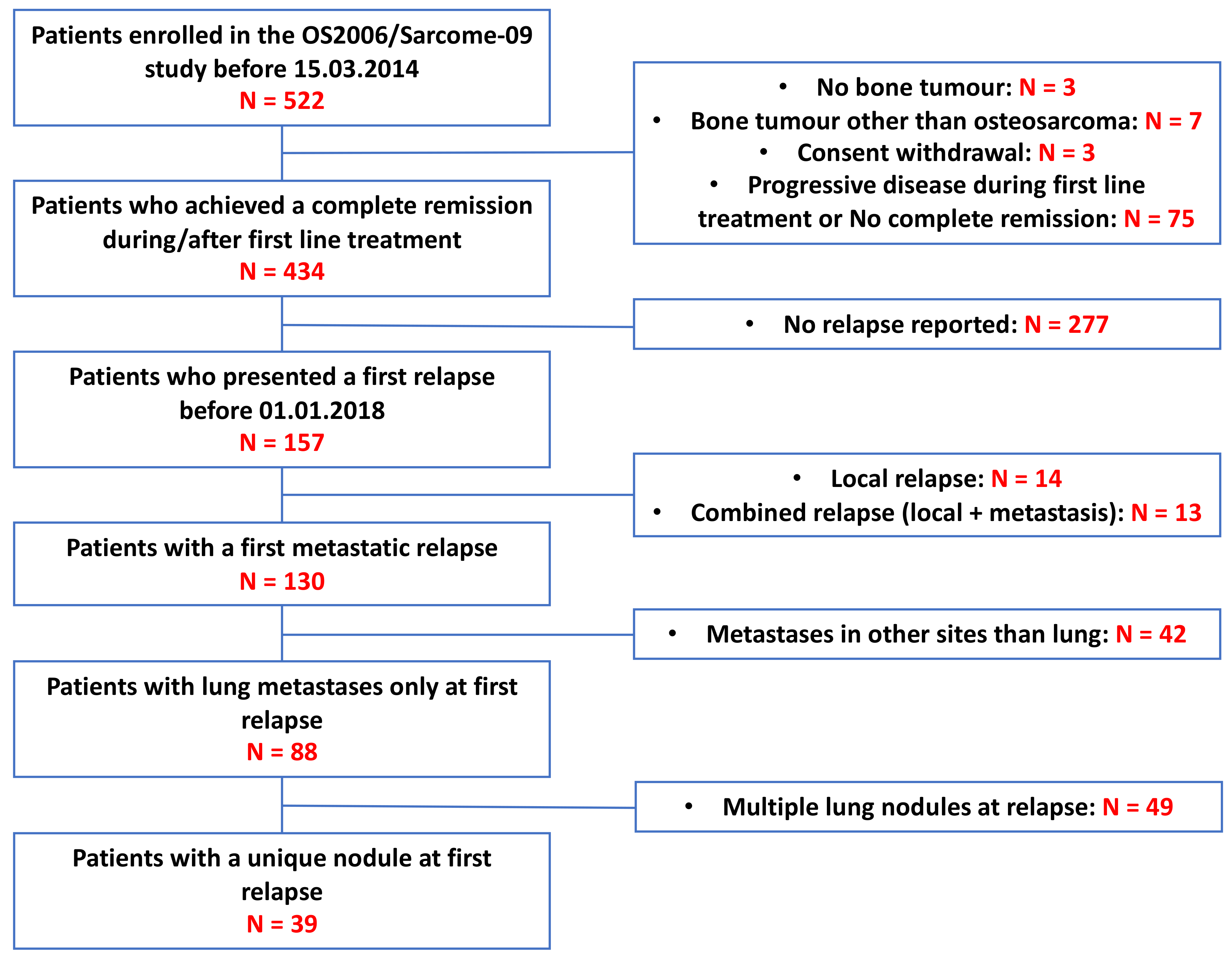
2.1. Population
2.2. Treatment Recommendations at Relapses
2.3. Data Management
2.4. Statistics
3. Results
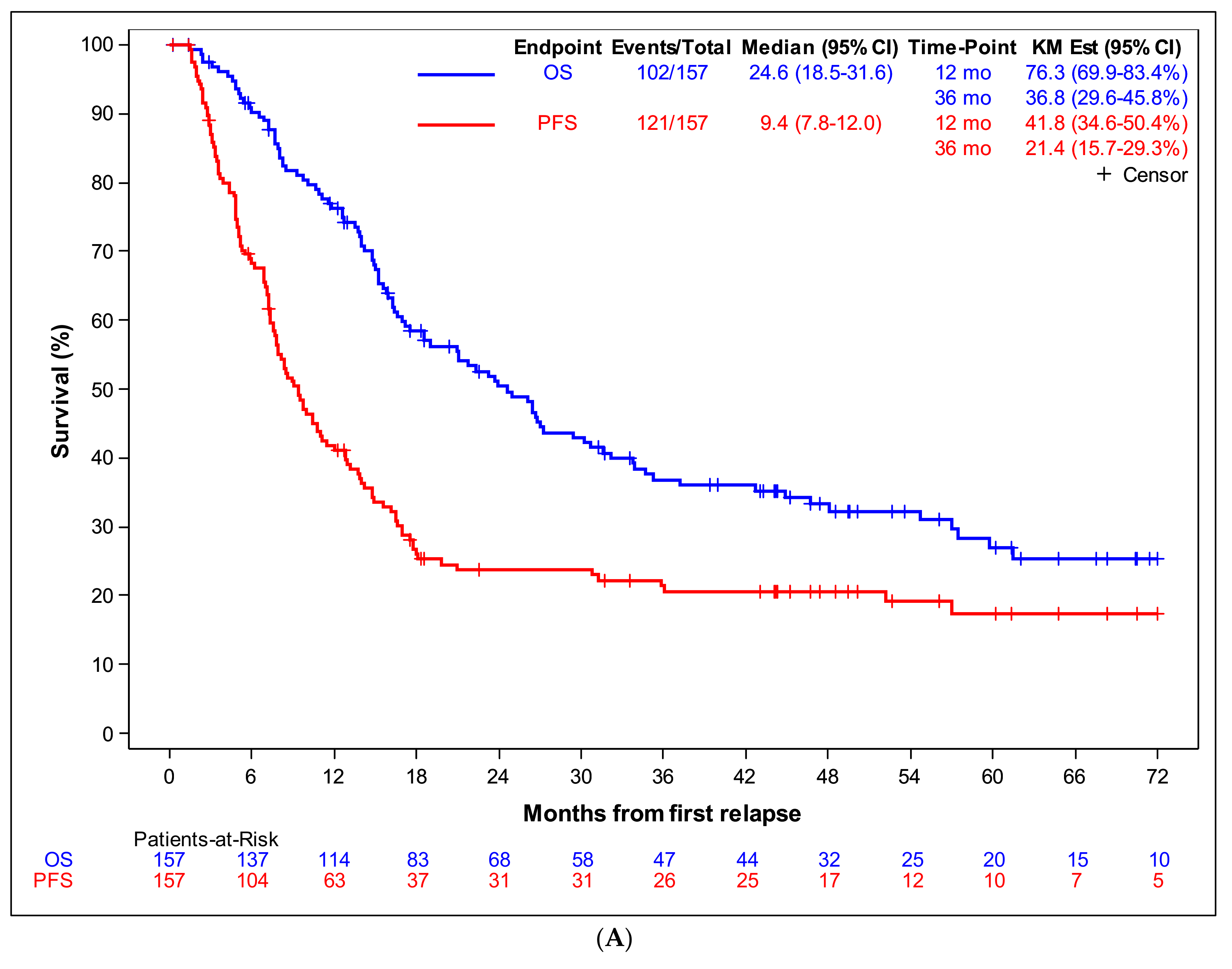
3.1. First Osteosarcoma Relapses
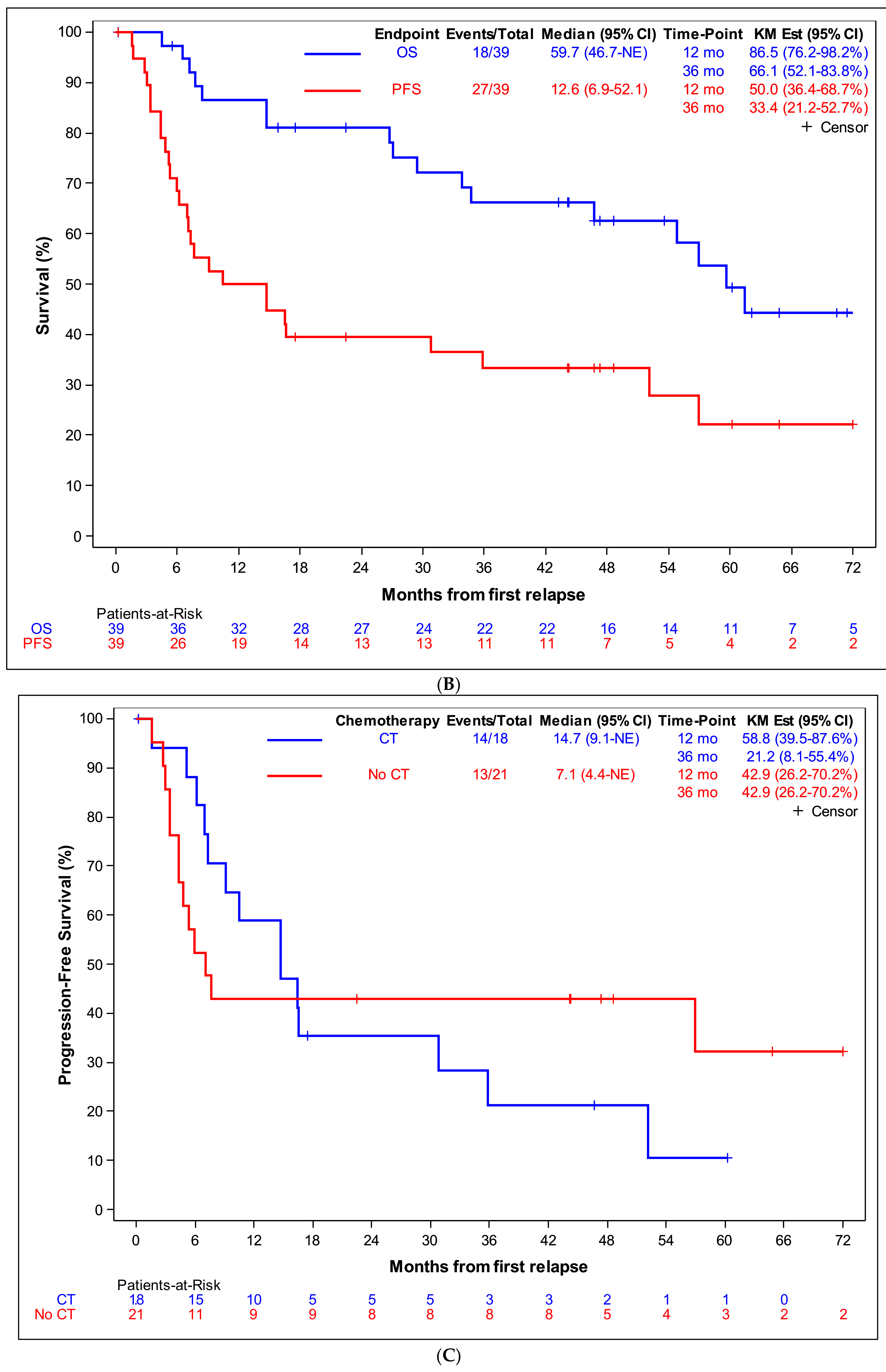
3.2. Unique Lung Metastasis as First Relapse
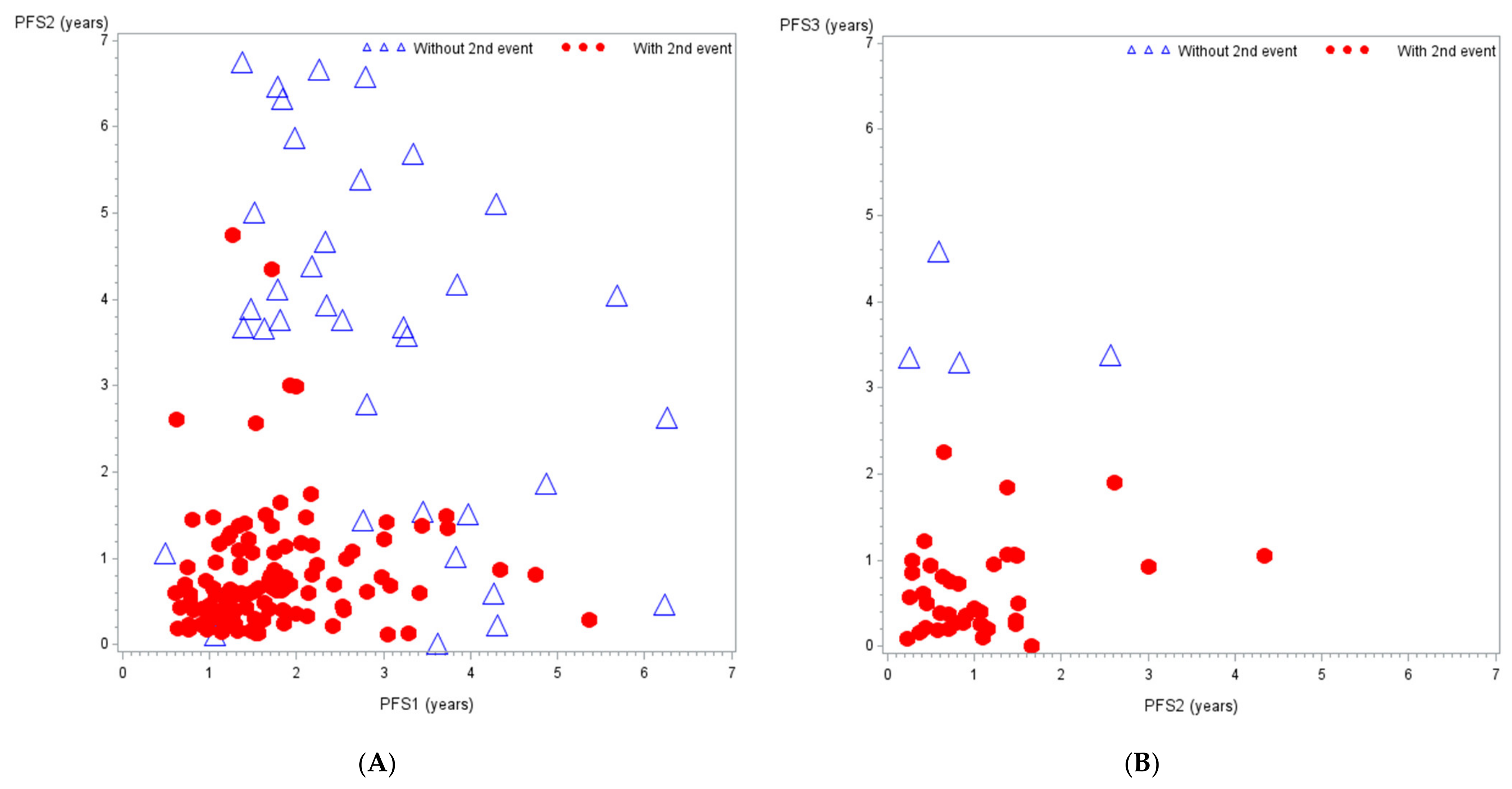
3.3. Subsequent Relapses
4. Discussion
- (1)
- The lack of dedicated phase-II trials, although more than three phase-II trials were open for osteosarcoma patients during the study period;
- (2)
- the willingness of physicians to treat patients with chemotherapy agents previously shown to have activity in osteosarcoma [6] and not already used in front-line treatment;
- (3)
- the perceived lack of attractiveness of the trial objectives, either in terms of type of compound (no new targeted or immune agent) or trial design (randomization against placebo poorly accepted, especially in paediatric population);
- (4)
- the eligibility criteria preventing participation of some patients based on their age or on the recurrence presentation (restricted to measurable disease according to RECIST criteria);
- (5)
- the lack of paediatric phase-I trials evaluating new drugs;
- (6)
- the prohibition of surgical treatment in phase-II trials, despite the importance of RC.
4.1. Trial Entry Criteria
4.2. Trial End-Points and Design
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Desandes, E.; Stark, D.P. Epidemiology of Adolescents and Young Adults with Cancer in Europe. Prog. Tumor. Res. 2016, 43, 1–15. [Google Scholar]
- Piperno-Neumann, S.; Le Deley, M.C.; Rédini, F.; Pacquement, H.; Marec-Bérard, P.; Petit, P.; Brisse, H.; Lervat, C.; Gentet, J.C.; Entz-Werlé, N.; et al. Zoledronate in combination with chemotherapy and surgery to treat osteosarcoma (OS2006): A randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2016, 17, 1070–1080. [Google Scholar] [CrossRef]
- Smeland, S.; Bielack, S.S.; Whelan, J.; Bernstein, M.; Hogendoorn, P.; Krailo, M.D.; Gorlick, R.; Janeway, K.A.; Ingleby, F.C.; Anninga, J.; et al. Survival and prognosis with osteosarcoma: Outcomes in more than 2000 patients in the EURAMOS-1 (European and American Osteosarcoma Study) cohort. Eur. J. Cancer 2019, 109, 36–50. [Google Scholar] [CrossRef] [PubMed]
- Friebele, J.C.; Peck, J.; Pan, X.; Abdel-Rasoul, M.; Mayerson, J.L. Osteosarcoma: A Meta-Analysis and Review of the Literature. Am. J. Orthop. 2015, 44, 547–553. [Google Scholar] [PubMed]
- Isakoff, M.S.; Bielack, S.S.; Meltzer, P.; Gorlick, R. Osteosarcoma: Current Treatment and a Collaborative Pathway to Success. J. Clin. Oncol. 2015, 33, 3029–3035. [Google Scholar] [CrossRef] [PubMed]
- Anninga, J.K.; Gelderblom, H.; Fiocco, M.; Kroep, J.R.; Taminiau, A.H.; Hogendoorn, P.C.; Egeler, R.M. Chemotherapeutic adjuvant treatment for osteosarcoma: Where do we stand? Eur. J. Cancer 2011, 47, 2431–2445. [Google Scholar] [CrossRef]
- Bielack, S.; Carrle, D.; Casali, P.G. ESMO Guidelines Working Group. Osteosarcoma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann. Oncol. 2009, 20 (Suppl. 4), 137–139. [Google Scholar] [CrossRef]
- Mirabello, L.; Troisi, R.J.; Savage, S.A. Osteosarcoma incidence and survival rates from 1973 to 2004: Data from the Surveillance, Epidemiology, and End Results Program. Cancer 2009, 115, 1531–1543. [Google Scholar] [CrossRef]
- Kempf-Bielack, B.; Bielack, S.S.; Jürgens, H.; Branscheid, D.; Berdel, W.E.; Exner, G.U.; Göbel, U.; Helmke, K.; Jundt, G.; Kabisch, H.; et al. Osteosarcoma relapse after combined modality therapy: An analysis of unselected patients in the Cooperative Osteosarcoma Study Group (COSS). J. Clin. Oncol. 2005, 23, 559–568. [Google Scholar] [CrossRef]
- Gelderblom, H.; Jinks, R.C.; Sydes, M.; Bramwell, V.H.; van Glabbeke, M.; Grimer, R.J.; Hogendoorn, P.C.; McTiernan, A.; Lewis, I.J.; Nooij, M.A.; et al. Survival after recurrent osteosarcoma: Data from 3 European Osteosarcoma Intergroup (EOI) randomized controlled trials. Eur. J. Cancer 2011, 47, 895–902. [Google Scholar] [CrossRef]
- Leary, S.E.; Wozniak, A.W.; Billups, C.A.; Wu, J.; McPherson, V.; Neel, M.D.; Rao, B.N.; Daw, N.C. Survival of pediatric patients after relapsed osteosarcoma: The St. Jude Children’s Research Hospital experience. Cancer 2013, 119, 2645–2653. [Google Scholar] [CrossRef]
- Bacci, G.; Briccoli, A.; Longhi, A.; Ferrari, S.; Mercuri, M.; Faggioli, F.; Versari, M.; Picci, P. Treatment and outcome of recurrent osteosarcoma: Experience at Rizzoli in 235 patients initially treated with neoadjuvant chemotherapy. Acta Oncol. 2005, 44, 748–755. [Google Scholar] [CrossRef]
- Briccoli, A.; Rocca, M.; Salone, M.; Guzzardella, G.A.; Balladelli, A.; Bacci, G. High grade osteosarcoma of the extremities metastatic to the lung: Long-term results in 323 patients treated combining surgery and chemotherapy, 1985–2005. Surg. Oncol. 2010, 19, 193–199. [Google Scholar] [CrossRef]
- Marec-Berard, P.; Segura-Ferlay, C.; Tabone, M.D.; Pacquement, H.; Lervat, C.; Gentet, J.C.; Schmitt, C.; Gaspar, N.; Brugières, L. High Dose Thiotepa in Patients with Relapsed or Refractory Osteosarcomas: Experience of the SFCE Group. Sarcoma 2014, 2014, 475067. [Google Scholar] [CrossRef] [PubMed]
- Errani, C.; Longhi, A.; Rossi, G.; Rimondi, E.; Biazzo, A.; Toscano, A.; Alì, N.; Ruggieri, P.; Alberghini, M.; Picci, P.; et al. Palliative therapy for osteosarcoma. Expert Rev. Anticancer Ther. 2011, 11, 217–227. [Google Scholar] [CrossRef]
- Kager, L.; Tamamyan, G.; Bielack, S. Novel insights and therapeutic interventions for pediatric osteosarcoma. Future Oncol. 2017, 13, 357–368. [Google Scholar] [CrossRef]
- Omer, N.; Le Deley, M.C.; Piperno-Neumann, S.; Marec-Berard, P.; Italiano, A.; Corradini, N.; Bellera, C.; Brugières, L.; Gaspar, N. Phase-II trials in osteosarcoma recurrences: A systematic review of past experience. Eur. J. Cancer 2017, 75, 98–108. [Google Scholar] [CrossRef]
- Von Hoff, D.D. There are no bad anticancer agents, only bad clinical trial designs—Twenty-first Richard and Hinda Rosenthal Foundation Award Lecture. Clin. Cancer Res. 1998, 4, 1079–1086. [Google Scholar]
- Piperno-Neumann, S.; Ray-Coquard, I.; Occean, B.V.; Laurence, V.; Cupissol, D.; Perrin, C.; Penel, N.; Bompas, E.; Rios, M.; Le Cesne, A.; et al. Results of API-AI based regimen in osteosarcoma adult patients included in the French OS2006/Sarcome-09 study. Int. J. Cancer 2020, 146, 413–423. [Google Scholar] [CrossRef]
- Gaspar, N.; Occean, B.V.; Pacquement, H.; Bompas, E.; Bouvier, C.; Brisse, H.J.; Castex, M.P.; Cheurfa, N.; Corradini, N.; Delaye, J.; et al. Results of methotrexate-etoposide-ifosfamide based regimen (M-EI) in osteosarcoma patients included in the French OS2006/sarcome-09 study. Eur. J. Cancer 2018, 88, 57–66. [Google Scholar] [CrossRef]
- Marec-Berard, P.; Laurence, V.; Occean, B.V.; Ray-Coquard, I.; Linassier, C.; Corradini, N.; Collard, O.; Chaigneau, L.; Cupissol, D.; Kerbrat, P.; et al. Methotrexate-Etoposide-Ifosfamide Compared with Doxorubicin-Cisplatin-Ifosfamide Chemotherapy in Osteosarcoma Treatment, Patients Aged 18–25 Years. J. Adolesc. Young Adult Oncol. 2019, 2, 172–182. [Google Scholar] [CrossRef]
- Hogendoorn, P.C.W.; Athanasou, N.; Bielack, S.; De Alava, E.; Dei Tos, A.P.; Ferrari, S.; Gelderblom, H.; Grimer, R.; Hall, K.S.; Hassan, B.; et al. Bone sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2010, 21, v204–v213. [Google Scholar] [CrossRef]
- Bielack, S.S.; Smeland, S.; Whelan, J.S.; Marina, N.; Jovic, G.; Hook, J.M.; Krailo, M.D.; Gebhardt, M.; Pápai, Z.; Meyer, J.; et al. Methotrexate, Doxorubicin, and Cisplatin (MAP) Plus Maintenance Pegylated Interferon Alfa-2b Versus MAP Alone in Patients With Resectable High-Grade Osteosarcoma and Good Histologic Response to Preoperative MAP: First Results of the EURAMOS-1 Good Response Randomized Controlled Trial. J. Clin. Oncol. 2015, 33, 2279–2287. [Google Scholar]
- Marina, N.M.; Smeland, S.; Bielack, S.S.; Bernstein, M.; Jovic, G.; Krailo, M.D.; Hook, J.M.; Arndt, C.; van den Berg, H.; Brennan, B.; et al. Comparison of MAPIE versus MAP in patients with a poor response to preoperative chemotherapy for newly diagnosed high-grade osteosarcoma (EURAMOS-1): An open-label, international, randomised controlled trial. Lancet Oncol. 2016, 17, 1396–1408. [Google Scholar] [CrossRef]
- Le Deley, M.C.; Guinebretière, J.M.; Gentet, J.C.; Pacquement, H.; Pichon, F.; Marec-Bérard, P.; Entz-Werlé, N.; Schmitt, C.; Brugières, L.; Vanel, D.; et al. SFOP OS94: A randomised trial comparing preoperative high-dose methotrexate plus doxorubicin to high-dose methotrexate plus etoposide and ifosfamide in osteosarcoma patients. Eur. J. Cancer 2007, 43, 752–761. [Google Scholar] [CrossRef]
- Bielack, S.S.; Kempf-Bielack, B.; Branscheid, D.; Carrle, D.; Friedel, G.; Helmke, K.; Kevric, M.; Jundt, G.; Kühne, T.; Maas, R.; et al. Second and subsequent recurrences of osteosarcoma: Presentation, treatment, and outcomes of 249 consecutive cooperative osteosarcoma study group patients. J. Clin. Oncol. 2009, 27, 557–565. [Google Scholar] [CrossRef]
- Whelan, J.S.; Bielack, S.S.; Marina, N.; Smeland, S.; Jovic, G.; Hook, J.M.; Krailo, M.; Anninga, J.; Butterfass-Bahloul, T.; Böhling, T.; et al. EURAMOS-1, an international randomised study for osteosarcoma: Results from pre-randomisation treatment. Ann. Oncol. 2015, 26, 407–414. [Google Scholar] [CrossRef]
- Gaspar, N.; Marshall, L.V.; Binner, D.; Herold, R.; Rousseau, R.; Blanc, P.; Capdeville, R.; Carleer, J.; Copland, C.; Kerloeguen, Y.; et al. Joint adolescent-adult early phase clinical trials to improve access to new drugs for adolescents with cancer: Proposals from the multi-stakeholder platform-ACCELERATE. Ann. Oncol. 2018, 29, 766–771. [Google Scholar] [CrossRef]
- Wolford, J.E.; Tewari, K.S. US FDA oncology drug approvals in 2014. Future Oncol. 2015, 11, 1931–1945. [Google Scholar] [CrossRef]
- McHugh, K.; Kao, S. Response evaluation criteria in solid tumours (RECIST): Problems and need for modifications in paediatric oncology? Br. J. Radiol. 2003, 76, 433–436. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Van Meerten, E.L.V.P.; Gelderblom, H.; Bloem, J.L. RECIST revised: Implications for the radiologist. A review article on the modified RECIST guideline. Eur. Radiol. 2010, 20, 1456–1467. [Google Scholar] [CrossRef]
- Lagmay, J.P.; Krailo, M.D.; Dang, H.; Kim, A.; Hawkins, D.S.; Beaty, O., III; Widemann, B.C.; Zwerdling, T.; Bomgaars, L.; Langevin, A.M.; et al. Outcome of Patients With Recurrent Osteosarcoma Enrolled in Seven Phase II Trials Through Children’s Cancer Group, Pediatric Oncology Group, and Children’s Oncology Group: Learning From the Past to Move Forward. J. Clin. Oncol. 2016, 34, 3031–3038. [Google Scholar] [CrossRef]
- Kansara, M.; Teng, M.W.; Smyth, M.J.; Thomas, D.M. Translational biology of osteosarcoma. Nat. Rev. Cancer 2014, 14, 722–735. [Google Scholar] [CrossRef] [PubMed]
- Van Glabbeke, M.; Verweij, J.; Judson, I.; Nielsen, O.S. EORTC Soft Tissue and Bone Sarcoma Group. Progression-free rate as the principal end-point for phase II trials in soft-tissue sarcomas. Eur. J. Cancer 2002, 38, 543–549. [Google Scholar] [CrossRef]
- Italiano, A.; Mir, O.; Mathoulin-Pelissier, S.; Penel, N.; Piperno-Neumann, S.; Bompas, E.; Chevreau, C.; Duffaud, F.; Entz-Werlé, N.; Saada, E.; et al. Cabozantinib in patients with advanced Ewing sarcoma or osteosarcoma (CABONE): A multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020, 21, 446–455. [Google Scholar] [CrossRef]
- Penel, N.; Demetri, G.D.; Blay, J.Y.; Cousin, S.; Maki, R.G.; Chawla, S.P.; Judson, I.; Von Mehren, M.; Schöffski, P.; Verweij, J.; et al. Growth modulation index as metric of clinical benefit assessment among advanced soft tissue sarcoma patients receiving trabectedin as a salvage therapy. Ann. Oncol. 2013, 24, 537–542. [Google Scholar] [CrossRef]
- Brodowicz, T.; Mir, O.; Wallet, J.; Italiano, A.; Blay, J.Y.; Bertucci, F.; Eisterer, W.; Chevreau, C.; Piperno-Neumann, S.; Bompas, E.; et al. Efficacy and safety of regorafenib compared to placebo and to post-cross-over regorafenib in advanced non-adipocytic soft tissue sarcoma. Eur. J. Cancer 2018, 99, 28–36. [Google Scholar] [CrossRef]
- Buonadonna, A.; Benson, C.; Casanova, J.; Kasper, B.; López Pousa, A.; Mazzeo, F.; Brodowicz, T.; Penel, N. A noninterventional, multicenter, prospective phase IV study of trabectedin in patients with advanced soft tissue sarcoma. Anticancer Drugs 2017, 28, 1157–1165. [Google Scholar] [CrossRef]
- Cousin, S.; Blay, J.Y.; Bertucci, F.; Isambert, N.; Italiano, A.; Bompas, E.; Ray-Coquard, I.; Perrot, D.; Chaix, M.; Bui-Nguyen, B.; et al. Correlation between overall survival and growth modulation index in pre-treated sarcoma patients: A study from the French Sarcoma Group. Ann. Oncol. 2013, 24, 2681–2685. [Google Scholar] [CrossRef]
| Characteristics of the First Relapse | N (%) or Median (Range) |
|---|---|
| Gender | |
| Male, N (%) | 85 (54.1%) |
| Female, N (%) | 72 (45.9%) |
| Age at relapse (years) | |
| Median (range) | 17.5 (7.7–51.6) |
| Less than 12 years, N (%) | 16 (10.2%) |
| 12–17 years, N (%) | 69 (42.9%) |
| 18–25 years, N (%) | 52 (33.1%) |
| >25 years, N (%) | 20 (12.7%) |
| Time interval from diagnosis to 1st relapse (years) | |
| Median (range) | 1.7 (0.5–7.6) |
| <1 year, N (%) | 22 (14.0%) |
| 1–1.5 years, N (%) | 40 (25.5%) |
| 1.5–2 years, N (%) | 40 (25.5%) |
| ≥2 years, N (%) | 55 (35.0%) |
| Site of relapse | |
| Local relapse, N (%) | 14 (8.9%) |
| Metastases only, N (%) | 130 (82.8%) |
| Combined (local relapse + metastases), N (%) | 13 (8.3%) |
| Metastatic sites (possible combined) | |
| Lung, N (%) | 127 (80.9%) |
| Unilateral | 74 |
| Single nodule | 44 |
| Multiple nodule | 30 |
| Bilateral | 53 |
| Bone, N (%) | 26 (16.6%) |
| Pleura, N (%) | 20 (12.7%) |
| Other metastases, N (%) | 21 (13.4%) |
| Relapse with measurable disease matching RECIST criteria, N (%) | |
| No, N (%) | 36 (22.9%) |
| Yes, N (%) | 121 (77.7%) |
| Treatment allocated by randomisation | |
| No randomisation, N (%) | 58 (36.9%) |
| Without Zoledronate, N (%) | 45 (28.7%) |
| With Zoledronate, N (%) | 54 (34.4%) |
| Treatment for Relapse | N (%) or Median (Range) |
|---|---|
| Treatment modalities | |
| Systemic treatment, N (%) | 116 (73.9%) |
| Surgery, N (%) | 107 (68.2%) |
| Radiation therapy, N (%) | 17 (10.8%) |
| Thermoablation, N (%) | 2 (1.3%) |
| Other (1), N (%) | 1 (0.7%) |
| Treatment combination | |
| No treatment, N (%) | 2 (1.3%) |
| Local treatment alone: | |
| Surgery alone, N (%) | 37 (23.6%) |
| Other local treatment (2) +/− surgery N (%) | 2 (1.3%) |
| Systemic treatment alone, N (%) | 35 (22.3%) |
| Systemic treatment + Surgery, N (%) | 65 (41.4%) |
| Systemic treatment + other local treatment (2) +/− surgery, N (%) | 16 (10.2%) |
| Details of systemic treatment (N = 112, 4 missing data) | |
| Type of molecules | |
| Chemotherapy, N (%) | 109 (97.3%) |
| Targeted agent (3), N (%) | 17 (15.2%) |
| Targeted agent + chemotherapy | 14 (12.5%) |
| Targeted agent alone | 3 (2.7%) |
| Combination | |
| Monotherapy, N (%) | 37 (33.0%) |
| Multi-agent therapy, N (%) | 75 (67.0%) |
| Treatment scheme | |
| Conventional courses only, N (%) | 85 (75.9%) |
| Conventional courses followed by HD chemo (4), N (%) | 12 (10.7%) |
| Metronomic treatment only, N (%) | 6 (5.4%) |
| Conventional courses & metronomic treatment, N (%) | 6 (5.4%) |
| Conventional courses + HD chemo (4) & metronomic treatment, N (%) | 3 (2.7%) |
| Participation in a clinical trial | 29 (25.9%) |
| Factors | N | Univariate Analysis | Multivariate Analysis (1) | ||||
|---|---|---|---|---|---|---|---|
| Patient and Tumour Characteristics | N | HR | 95%CI | p-Value | HR | 95%CI | p-Value |
| Metastasis at diagnosis | 0.20 | ‒ | |||||
| No | 133 | 1 | |||||
| Yes | 24 | 1.38 | (0.86–2.21) | ||||
| Chemotherapy as first-line treatment | 0.65 | ‒ | |||||
| Methotrexate-etoposide-ifosfamide | 124 | 1 | |||||
| API-AI | 33 | 1.11 | (0.71–1.72) | ||||
| Histological response of primary tumour | 0.26 | ‒ | |||||
| Good histological response | 89 | 1 | |||||
| Poor histological response | 68 | 1.23 | (0.86–1.76) | ||||
| Treatment allocated by randomisation (2) | 0.040 | 0.015 | |||||
| Without Zoledronate | 45 | 1 | 1 | ||||
| With Zoledronate | 54 | 1.61 | (1.02–2.53) | 1.79 | (1.12–2.86) | ||
| Age at relapse (years) | 0.02 | 0.52 | |||||
| Less than 12 years | 16 | 1 | 1 | ||||
| 12–17 years | 69 | 1.43 | (0.78–2.62) | 1.26 | (0.47–3.38) | ||
| 18–25 years | 52 | 0.78 | (0.41–1.48) | 0.84 | (0.30–2.32) | ||
| >25 years | 20 | 1.52 | (0.73–3.17) | 1.26 | (0.47–3.38) | ||
| Time interval from diagnosis to 1st relapse | <0.0001 | 0.0004 | |||||
| <1 year | 22 | 3.92 | (2.23–6.91) | 4.54 | (2.13–9.68) | ||
| 1–1.5 year, N (%) | 40 | 2.44 | (1.50–3.95) | 2.87 | (1.53–5.38) | ||
| 1.5–2 years, N (%) | 40 | 1.64 | (1.00–2.68) | 1.76 | (0.91–3.38) | ||
| >2 years | 55 | 1 | 1 | ||||
| Type of relapse | |||||||
| Local relapse | 14 | 1 | 0.32 | ‒ | |||
| Unique lung metastasis | 39 | 0.72 | (0.36–1.45) | ||||
| Other | 104 | 1.00 | (0.53–1.88) | ||||
| Measurable disease matching RECIST criteria | |||||||
| No | 36 | 1 | 0.048 | 1 | 0.45 | ||
| Yes | 121 | 1.57 | (0.99–2.46) | 1.27 | (0.68–2.39) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thebault, E.; Piperno-Neumann, S.; Tran, D.; Pacquement, H.; Marec-Berard, P.; Lervat, C.; Castex, M.-P.; Cleirec, M.; Bompas, E.; Vannier, J.-P.; et al. Successive Osteosarcoma Relapses after the First Line O2006/Sarcome-09 Trial: What Can We Learn for Further Phase-II Trials? Cancers 2021, 13, 1683. https://doi.org/10.3390/cancers13071683
Thebault E, Piperno-Neumann S, Tran D, Pacquement H, Marec-Berard P, Lervat C, Castex M-P, Cleirec M, Bompas E, Vannier J-P, et al. Successive Osteosarcoma Relapses after the First Line O2006/Sarcome-09 Trial: What Can We Learn for Further Phase-II Trials? Cancers. 2021; 13(7):1683. https://doi.org/10.3390/cancers13071683
Chicago/Turabian StyleThebault, Eric, Sophie Piperno-Neumann, Diep Tran, Hélène Pacquement, Perrine Marec-Berard, Cyril Lervat, Marie-Pierre Castex, Morgane Cleirec, Emmanuelle Bompas, Jean-Pierre Vannier, and et al. 2021. "Successive Osteosarcoma Relapses after the First Line O2006/Sarcome-09 Trial: What Can We Learn for Further Phase-II Trials?" Cancers 13, no. 7: 1683. https://doi.org/10.3390/cancers13071683
APA StyleThebault, E., Piperno-Neumann, S., Tran, D., Pacquement, H., Marec-Berard, P., Lervat, C., Castex, M.-P., Cleirec, M., Bompas, E., Vannier, J.-P., Plantaz, D., Saumet, L., Verite, C., Collard, O., Pluchart, C., Briandet, C., Monard, L., Brugieres, L., Le Deley, M.-C., & Gaspar, N. (2021). Successive Osteosarcoma Relapses after the First Line O2006/Sarcome-09 Trial: What Can We Learn for Further Phase-II Trials? Cancers, 13(7), 1683. https://doi.org/10.3390/cancers13071683








