Oncologic Outcomes of Radical Prostatectomy and High-Dose Intensity-Modulated Radiotherapy with Androgen-Deprivation Therapy for Relatively Young Patients with Unfavorable Intermediate-Risk Prostate Adenocarcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Database
2.2. Study Cohort
2.3. Study Covariates
2.4. Endpoints
2.5. Propensity Score Matching
2.6. Statistics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PC | Prostate cancer |
| TCRD | Taiwan Cancer Registry database |
| NCCN | National Comprehensive Cancer Network |
| PSA | Prostate-specific antigen; AUA, American Urological Association |
| ASTRO | American Society for Radiation Oncology |
| UIR | Unfavorable intermediate risk |
| RP | Radical prostatectomy; RT, radiotherapy |
| ADT | Androgen-deprivation therapy; RCT, randomized controlled trial |
| 3D-CRT | Three-dimensional conformal radiotherapy |
| IMRT | Intensity-modulated radiotherap |
| PSM | Propensity score matching |
| NHIRD | National health insurance research data |
| BF | Biochemical failure; LRR, locoregional recurrence |
| DM | Distant metastasis |
| ICD-9-CM | International Classification of Diseases, Ninth Revision, Clinical Modification |
| CCI | Charlson Comorbidity Index |
| OS | Overall survival |
| HR | Hazard ratio |
| EBRT | External-beam radiotherapy |
| CI | Confidence interval |
| BFS | Biochemical failure–free survival |
| aHR | Adjusted hazard ratio |
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Butler, S.S.; Muralidhar, V.; Zhao, S.G.; Sanford, N.N.; Franco, I.; Fullerton, Z.H.; Chavez, J.; D’Amico, A.V.; Feng, F.Y.; Rebbeck, T.R.; et al. Prostate cancer incidence across stage, NCCN risk groups, and age before and after USPSTF Grade D recommendations against prostate-specific antigen screening in 2012. Cancer 2020, 126, 717–724. [Google Scholar] [CrossRef]
- Health Promotion Administration, Ministry of Health and Welfare. Taiwan Cancer Registry. Available online: hpa.gov.tw/Pages/List.aspx?nodeid=119 (accessed on 29 December 2020).
- NCCN Clinical Practice Guidelines in Oncology. Available online: https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf (accessed on 21 May 2020).
- Bekelman, J.E.; Rumble, R.B.; Chen, R.C.; Pisansky, T.M.; Finelli, A.; Feifer, A.; Nguyen, P.L.; Loblaw, D.A.; Tagawa, S.T.; Gillessen, S.; et al. Clinically Localized Prostate Cancer: ASCO Clinical Practice Guideline Endorsement of an American Urological Association/American Society for Radiation Oncology/Society of Urologic Oncology Guideline. J. Clin. Oncol. 2018, 36, 3251–3258. [Google Scholar] [CrossRef]
- Sanda, M.G.; Cadeddu, J.A.; Kirkby, E.; Chen, R.C.; Crispino, T.; Fontanarosa, J.; Freedland, S.J.; Greene, K.; Klotz, L.H.; Makarov, D.V.; et al. Clinically Localized Prostate Cancer: AUA/ASTRO/SUO Guideline. Part I: Risk Stratification, Shared Decision Making, and Care Options. J. Urol. 2018, 199, 683–690. [Google Scholar] [CrossRef]
- Sanda, M.G.; Cadeddu, J.A.; Kirkby, E.; Chen, R.C.; Crispino, T.; Fontanarosa, J.; Freedland, S.J.; Greene, K.; Klotz, L.H.; Makarov, D.V.; et al. Clinically Localized Prostate Cancer: AUA/ASTRO/SUO Guideline. Part II: Recommended Approaches and Details of Specific Care Options. J. Urol. 2018, 199, 990–997. [Google Scholar] [CrossRef]
- Parker, C.; Castro, E.; Fizazi, K.; Heidenreich, A.; Ost, P.; Procopio, G.; Tombal, B.; Gillessen, S. Prostate cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 1119–1134. [Google Scholar] [CrossRef]
- Rosser, C.J.; Chichakli, R.; Levy, L.B.; Kuban, D.A.; Smith, L.G.; Pisters, L.L. Biochemical disease-free survival in men Relatively younger than 60 years with prostate cancer treated with external beam radiation. J. Urol. 2002, 168, 536–541. [Google Scholar] [CrossRef]
- Cooperberg, M.R.; Vickers, A.J.; Broering, J.M.; Carroll, P.R.; for the Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) Investigators. Comparative risk-adjusted mortality outcomes after primary surgery, radiotherapy, or androgen-deprivation therapy for localized prostate cancer. Cancer 2010, 116, 5226–5234. [Google Scholar] [CrossRef]
- Potters, L.; Klein, E.A.; Kattan, M.W.; Reddy, C.A.; Ciezki, J.P.; Reuther, A.M.; Kupelian, P.A. Monotherapy for stage T1–T2 prostate cancer: Radical prostatectomy, external beam radiotherapy, or permanent seed implantation. Radiother. Oncol. 2004, 71, 29–33. [Google Scholar] [CrossRef]
- Kupelian, P.A.; Elshaikh, M.; Reddy, C.A.; Zippe, C.; Klein, E.A. Comparison of the Efficacy of Local Therapies for Localized Prostate Cancer in the Prostate-Specific Antigen Era: A Large Single-Institution Experience With Radical Prostatectomy and External-Beam Radiotherapy. J. Clin. Oncol. 2002, 20, 3376–3385. [Google Scholar] [CrossRef] [PubMed]
- Kupelian, P.A.; Potters, L.; Khuntia, D.; Ciezki, J.P.; Reddy, C.A.; Reuther, A.M.; Carlson, T.P.; Klein, E.A. Radical prostatec-tomy, external beam radiotherapy <72 Gy, external beam radiotherapy> or = 72 Gy, permanent seed implantation, or combined seeds/external beam radiotherapy for stage T1-T2 prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 2004, 58, 25–33. [Google Scholar] [CrossRef]
- Akakura, K.; Suzuki, H.; Ichikawa, T.; Fujimoto, H.; Maeda, O.; Usami, M.; Hirano, D.; Takimoto, Y.; Kamoto, T.; Ogawa, O.; et al. A Randomized Trial Comparing Radical Prostatectomy Plus Endocrine Therapy versus External Beam Radiotherapy Plus Endocrine Therapy for Locally Advanced Prostate Cancer: Results at Median Follow-up of 102 Months. Jpn. J. Clin. Oncol. 2006, 36, 789–793. [Google Scholar] [CrossRef]
- Paulson, D.F.; Lin, G.H.; Hinshaw, W.; Stephani, S. The Uro-Oncology Research Group Radical Surgery Versus Radiotherapy for Adenocarcinoma of the Prostate. J. Urol. 1982, 128, 502–504. [Google Scholar] [CrossRef]
- Zelefsky, M.J.; Marion, C.; Fuks, Z.; Leibel, S.A. Improved Biochemical Disease-Free Survival of Men Younger Than 60 Years With Prostate Cancer Treated With High Dose Conformal External Beam Radiotherapy. J. Urol. 2003, 170, 1828–1832. [Google Scholar] [CrossRef]
- Chiang, C.-J.; You, S.-L.; Chen, C.-J.; Yang, Y.-W.; Lo, W.-C.; Lai, M.-S. Quality assessment and improvement of nationwide cancer registration system in Taiwan: A review. Jpn. J. Clin. Oncol. 2015, 45, 291–296. [Google Scholar] [CrossRef]
- Wen, C.P.; Tsai, D.S.P.; Chung, W.-S.I. A 10-Year Experience with Universal Health Insurance in Taiwan: Measuring Changes in Health and Health Disparity. Ann. Intern. Med. 2008, 148, 258–267. [Google Scholar] [CrossRef]
- Chang, C.-L.; Yuan, K.S.-P.; Wu, A.T.; Wu, S.-Y. Toxicity Profiles of Fractionated Radiotherapy, Contemporary Stereotactic Radiosurgery, and Transsphenoidal Surgery in Nonfunctioning Pituitary Macroadenomas. Cancers 2019, 11, 1658. [Google Scholar] [CrossRef]
- Chang, C.-L.; Yuan, K.S.-P.; Wu, A.T.; Wu, S.-Y. Adjuvant Therapy for High-Risk Stage II or III Colon Adenocarcinoma: A Propensity Score-Matched, Nationwide, Population-Based Cohort Study. Cancers 2019, 11, 2003. [Google Scholar] [CrossRef]
- Chang, S.-C.; Chen, H.-M.; Wu, S.-Y. There Are No Differences in Positive Surgical Margin Rates or Biochemical Failure–Free Survival among Patients Receiving Open, Laparoscopic, or Robotic Radical Prostatectomy: A Nationwide Cohort Study from the National Cancer Database. Cancers 2020, 13, 106. [Google Scholar] [CrossRef]
- Chang, S.-C.; Hsu, C.-H.; Lin, Y.-C.; Wu, S.-Y. Effects of 1-Year Hospital Volume on Surgical Margin and Biochemical-Failure-Free Survival in Patients Undergoing Robotic versus Nonrobotic Radical Prostatectomy: A Nationwide Cohort Study from the National Taiwan Cancer Database. Cancers 2021, 13, 488. [Google Scholar] [CrossRef]
- Lin, W.-C.; Chang, C.-L.; Hsu, H.-L.; Yuan, K.S.-P.; Wu, A.T.H.; Wu, S.-Y. Three-Dimensional Conformal Radiotherapy-Based or Intensity-Modulated Radiotherapy-Based Concurrent Chemoradiotherapy in Patients with Thoracic Esophageal Squamous Cell Carcinoma. Cancers 2019, 11, 1529. [Google Scholar] [CrossRef]
- Qin, L.; Chen, T.-M.; Kao, Y.-W.; Lin, K.-C.; Yuan, K.S.-P.; Wu, A.T.H.; Shia, B.-C.; Wu, S.-Y. Predicting 90-Day Mortality in Locoregionally Advanced Head and Neck Squamous Cell Carcinoma after Curative Surgery. Cancers 2018, 10, 392. [Google Scholar] [CrossRef] [PubMed]
- Shia, B.-C.; Qin, L.; Lin, K.-C.; Fang, C.-Y.; Tsai, L.-L.; Kao, Y.-W.; Wu, S.-Y. Outcomes for Elderly Patients Aged 70 to 80 Years or Older with Locally Advanced Oral Cavity Squamous Cell Carcinoma: A Propensity Score–Matched, Nationwide, Oldest Old Patient–Based Cohort Study. Cancers 2020, 12, 258. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.-Y.; Fang, S.-C.; Hwang, O.R.; Shih, H.-J.; Shao, Y.-H.J. Influence of Baseline Cardiovascular Comorbidities on Mortality after Androgen Deprivation Therapy for Metastatic Prostate Cancer. Cancers 2020, 12, 189. [Google Scholar] [CrossRef] [PubMed]
- Lepor, H. A Review of Surgical Techniques for Radical Prostatectomy. Rev. Urol. 2005, 7, S11–S17. [Google Scholar]
- Cookson, M.S.; Aus, G.; Burnett, A.L.; Canby-Hagino, E.D.; D’Amico, A.V.; Dmochowski, R.R.; Eton, D.T.; Forman, J.D.; Goldenberg, S.L.; Hernandez, J.; et al. Variation in the Definition of Biochemical Recurrence in Patients Treated for Localized Prostate Cancer: The American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel Report and Recommendations for a Standard in the Reporting of Surgical Outcomes. J. Urol. 2007, 177, 540–545. [Google Scholar] [CrossRef]
- Roach, M.; Hanks, G.; Thames, H.; Schellhammer, P.; Shipley, W.U.; Sokol, G.H.; Sandler, H. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: Recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int. J. Radiat. Oncol. 2006, 65, 965–974. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Chen, J.-H.; Yen, Y.-C.; Yang, H.-C.; Liu, S.-H.; Yuan, S.-P.; Wu, L.-L.; Lee, F.-P.; Lin, K.-C.; Lai, M.-T.; Wu, C.-C.; et al. Curative-Intent Aggressive Treatment Improves Survival in Elderly Patients With Locally Advanced Head and Neck Squamous Cell Carcinoma and High Comorbidity Index. Medicine 2016, 95, e3268. [Google Scholar] [CrossRef]
- Rassen, J.A.; Shelat, A.A.; Myers, J.; Glynn, R.J.; Rothman, K.J.; Schneeweiss, S. One-to-many propensity score matching in cohort studies. Pharmacoepidemiol. Drug Saf. 2012, 21, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm. Stat. 2011, 10, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.-C.; Liu, H.-E.; Kao, Y.-W.; Qin, L.; Lin, K.-C.; Fang, C.-Y.; Tsai, L.-L.; Shia, B.-C.; Wu, S.-Y. Definitive radiotherapy or surgery for early oral squamous cell carcinoma in old and very old patients: A propensity-score-matched, nationwide, population-based cohort study. Radiother. Oncol. 2020, 151. [Google Scholar] [CrossRef]
- D’Agostino, R.B. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. Med. 1998, 17, 2265–2281. [Google Scholar] [CrossRef]
- Austin, P.C. The performance of different propensity score methods for estimating marginal hazard ratios. Stat. Med. 2012, 32, 2837–2849. [Google Scholar] [CrossRef]
- Nguyen, T.-L.; Collins, G.S.; Spence, J.; Daurès, J.-P.; Devereaux, P.J.; Landais, P.; Le Manach, Y. Double-adjustment in propensity score matching analysis: Choosing a threshold for considering residual imbalance. BMC Med. Res. Methodol. 2017, 17, 1–8. [Google Scholar] [CrossRef]
- Berry, S.D.; Ngo, L.; Samelson, E.J.; Kiel, U.P. Competing Risk of Death: An Important Consideration in Studies of Older Adults. J. Am. Geriatr. Soc. 2010, 58, 783–787. [Google Scholar] [CrossRef]
- Lau, B.; Cole, S.R.; Gange, S.J. Competing Risk Regression Models for Epidemiologic Data. Am. J. Epidemiol. 2009, 170, 244–256. [Google Scholar] [CrossRef]
- Austin, P.C. The use of propensity score methods with survival or time-to-event outcomes: Reporting measures of effect similar to those used in randomized experiments. Stat. Med. 2014, 33, 1242–1258. [Google Scholar] [CrossRef]
- O’Reilly, P.; Martin, L.; Collins, G. Few patients with prostate cancer are willing to be randomised to treatment. BMJ 1999, 318, 1556. [Google Scholar] [CrossRef][Green Version]
- Crawford, E.D.; Hussain, M.; DeAntoni, E.P.; Thompson, I.M.; Eisenberger, M.A.; Blumenstein, B.; Coltman, C.A. Southwest oncology group strategies in prostatic carcinoma. Semin. Surg. Oncol. 1995, 11, 60–64. [Google Scholar] [CrossRef]
- Hamdy, F.C.; Donovan, J.L.; Lane, J.A.; Mason, M.; Metcalfe, C.; Holding, P.; Davis, M.; Peters, T.J.; Turner, E.L.; Martin, R.M.; et al. 10-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Localized Prostate Cancer. N. Engl. J. Med. 2016, 375, 1415–1424. [Google Scholar] [CrossRef]
- Sweat, S.D.; Bergstralh, E.J.; Slezak, J.; Blute, M.L.; Zincke, H. Competing risk analysis after radical prostatectomy for clinically nonmetastatic prostate adenocarcinoma according to clinical Gleason score and patient age. J. Urol. 2002, 168, 525–529. [Google Scholar] [CrossRef]
- Sebastian, N.T.; McElroy, J.P.; Martin, D.D.; Sundi, D.; Diaz, D.A. Survival after radiotherapy vs. radical prostatectomy for unfavorable intermediate-risk prostate cancer. Urol. Oncol. Semin. Orig. Investig. 2019, 37, 813.e11–813.e19. [Google Scholar] [CrossRef]
- Hanks, G.E. More on the uro-oncology research group report of radical surgery vs. radiotherapy for adenocarcinoma of the prostate. Int. J. Radiat. Oncol. 1988, 14, 1053. [Google Scholar] [CrossRef]
- Zhang, Z.; written on behalf of AME Big-Data Clinical Trial Collaborative Group; Kim, H.J.; Lonjon, G.; Zhu, Y. Balance diagnostics after propensity score matching. Ann. Transl. Med. 2019, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D.J.; Curtis, R.E.; Hall, E.J.; Ron, E. Second malignancies in prostate carcinoma patients after radiotherapy compared with surgery. Cancer 2000, 88, 398–406. [Google Scholar] [CrossRef]
- Sanda, M.G.; Dunn, R.L.; Michalski, J.; Sandler, H.M.; Northouse, L.; Hembroff, L.; Lin, X.; Greenfield, T.K.; Litwin, M.S.; Saigal, C.S.; et al. Quality of Life and Satisfaction with Outcome among Prostate-Cancer Survivors. N. Engl. J. Med. 2008, 358, 1250–1261. [Google Scholar] [CrossRef]
- Donovan, J.L.; Hamdy, F.C.; Lane, J.A.; Mason, M.; Metcalfe, C.; Walsh, E.; Blazeby, J.M.; Peters, T.J.; Holding, P.; Bonnington, S.; et al. Patient-Reported Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N. Engl. J. Med. 2016, 375, 1425–1437. [Google Scholar] [CrossRef]
- Austin, P.C.; Grootendorst, P.; Anderson, G.M. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: A Monte Carlo study. Stat. Med. 2006, 26, 734–753. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Staffa, S.J.; Zurakowski, D. Five Steps to Successfully Implement and Evaluate Propensity Score Matching in Clinical Research Studies. Anesth. Analg. 2018, 127, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
| Variables | RP n = 318 | IMRT n = 193 | p-Value | |||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | |||
| Age | Mean (SD) | 61.8 | (2.9) | 61.8 | (2.3) | 0.6079 |
| - | Median (IQR, Q1–Q3) | 62 | (58–64) | 62 | (59–64) | - |
| - | 20–59 | 59 | (18.6) | 31 | (16.1) | 0.9641 |
| - | 60–65 | 259 | (81.4) | 162 | (83.9) | - |
| Year of diagnosis | 2011 | 55 | (17.3) | 37 | (19.2) | 0.9993 |
| - | 2012 | 59 | (18.6) | 34 | (17.6) | - |
| - | 2013 | 62 | (19.5) | 40 | (20.7) | - |
| - | 2014 | 73 | (23.0) | 42 | (21.8) | - |
| - | 2015 | 69 | (21.7) | 40 | (20.7) | - |
| CCI scores | 0 | 161 | (50.6) | 93 | (48.2) | 0.9623 |
| - | 1 | 85 | (26.7) | 53 | (27.5) | - |
| - | 2+ | 72 | (22.6) | 47 | (24.4) | - |
| Income | <NTD$21,000 | 84 | (26.4) | 47 | (24.4) | 0.9093 |
| - | NTD$21,000–NTD$30,000 | 104 | (32.7) | 67 | (34.7) | - |
| - | NTD$30,000–NTD$45,000 | 73 | (23.0) | 51 | (26.4) | - |
| - | NTD$45,000+ | 57 | (17.9) | 28 | (14.5) | - |
| Hospital area | North | 160 | (50.3) | 95 | (49.2) | 0.8864 |
| - | Central | 80 | (25.2) | 42 | (21.8) | - |
| - | South | 70 | (22.0) | 53 | (27.5) | - |
| - | East | 8 | (2.5) | 3 | (1.6) | - |
| Hospital level | Medical center | 201 | (63.2) | 108 | (56.0) | 0.5759 |
| - | Other | 117 | (36.8) | 85 | (44.0) | - |
| Clinical T-stage | T1 | 17 | (5.3) | 12 | (6.2) | 0.9660 |
| - | T2a | 68 | (21.4) | 41 | (21.2) | - |
| - | T2b | 154 | (48.4) | 88 | (45.6) | - |
| - | T2c | 79 | (24.8) | 52 | (26.9) | - |
| Grade group | 1–2 | 5 | (1.6) | 10 | (5.2) | 0.4969 |
| - | 3 | 313 | (98.4) | 183 | (94.8) | - |
| Pretreatment PSA (ng/mL) | Mean (SD) | 9.2 | (4.2) | 9.5 | (4.3) | 0.5228 |
| - | Median (Q1–Q3) | 8.8 | (6.0–11.7) | 9.4 | (6.2–12.0) | - |
| - | 0–5 | 35 | (11.0) | 19 | (9.8) | 0.9904 |
| - | 5–10 | 149 | (46.9) | 87 | (45.1) | - |
| - | 10–20 | 134 | (42.1) | 87 | (45.1) | - |
| D’Amico | Localized-low | 117 | (36.8) | 67 | (34.7) | 0.9908 |
| - | Localized-intermediate | 100 | (31.4) | 60 | (31.1) | - |
| - | Localized-high | 77 | (24.2) | 51 | (26.4) | - |
| - | Locally advanced | 24 | (7.5) | 15 | (7.7) | - |
| Follow-up time, months | Mean (SD) | 73.1 | (17.5) | 72.2 | (18.3) | - |
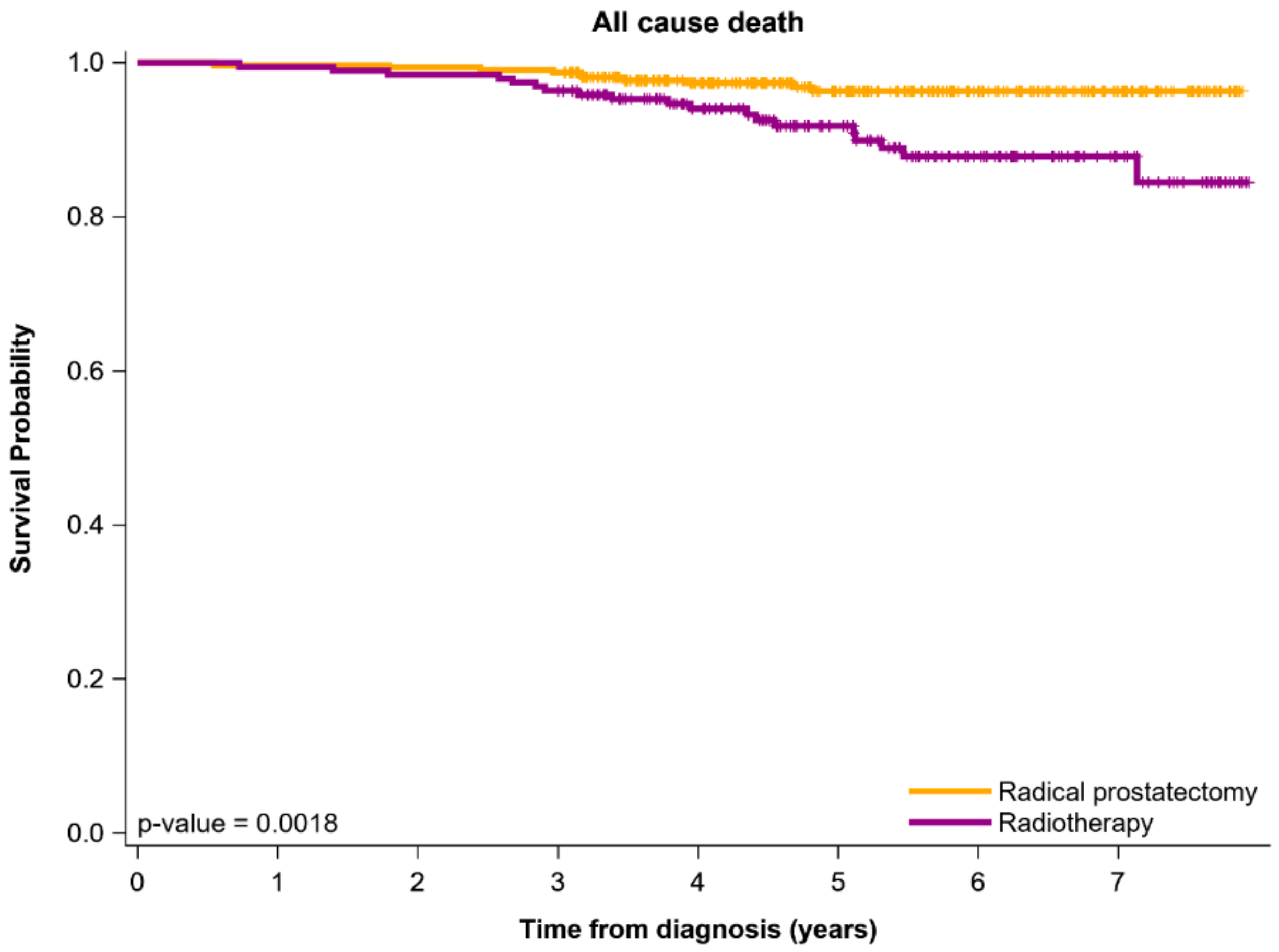
| All-cause death | - | 10 | (3.1) | 19 | (9.8) | 0.0037 |
| Biochemical recurrence | - | 31 | (14.7) | 40 | (20.7) | <0.0001 |
| Locoregional recurrence | - | 7 | (2.2) | 10 | (5.2) | 0.0061 |
| Distant metastasis | - | 9 | (2.8) | 18 | (9.3) | 0.0043 |
| Covariates | Category | Adjusted HR * | (95% CI) | p-Value |
|---|---|---|---|---|
| Curative treatment | RP | Ref | - | 0.0050 |
| - | IMRT | 2.76 | (1.36–5.60) | - |
| Age | 20–59 | Ref | - | 0.3907 |
| - | 60–65 | 1.59 | (0.55–4.56) | - |
| Year of diagnosis | 2011 | Ref | - | 0.3441 |
| - | 2012 | 1.07 | (0.43–2.71) | - |
| - | 2013 | 0.42 | (0.14–1.23) | - |
| - | 2014 | 0.56 | (0.18–1.73) | - |
| - | 2015 | 0.45 | (0.11–1.85) | - |
| CCI scores | 0 | Ref | - | 0.8774 |
| - | 1 | 0.79 | (0.31–2.04) | - |
| - | 2+ | 0.92 | (0.28–2.99) | - |
| Clinical T-stage | T1 | Ref | - | 0.0915 |
| - | T2a | 1.07 | (0.85–2.33) | - |
| - | T2b | 1.76 | (0.85–5.62) | - |
| - | T2c | 1.14 | (0.38–3.45) | - |
| Grade group (max Gleason grade) | 1–2 | Ref | - | 0.7284 |
| - | 3 | 1.13 | (0.56–2.28) | - |
| Pretreatment PSA (ng/mL) | 0–5 | Ref | - | 0.4279 |
| - | 5–10 | 1.01 | (0.52–1.22) | |
| - | 10–20 | 1.09 | (0.59–1.92) | |
| Income | <NTD$21,000 | Ref | 0.2333 | |
| - | NTD$21,000–NTD$30,000 | 0.87 | (0.39–1.95) | - |
| - | NTD$30,000–NTD$45,000 | 0.82 | (0.77–1.82) | - |
| - | NTD$45,000+ | 0.61 | (0.33–1.76) | - |
| Hospital level | Medical center | Ref | 0.5172 | |
| - | Others | 1.26 | (0.62–2.55) | - |
| Hospital area | North | Ref | 0.9958 | |
| - | Central | 1.03 | (0.43–2.47) | - |
| - | South | 1.07 | (0.44–2.59) | - |
| - | East | 1.24 | (0.88–3.68) | - |
| Clinical T-stage | T1 | Ref | - | 0.2871 |
| - | T2a | 0.64 | (0.24–1.68) | - |
| - | T2b | 1.91 | (0.69–12.36) | - |
| - | T2c | 2.25 | (0.41–3.78) | - |
| D’Amico | Localized-low | Ref | - | 0.1190 |
| - | Localized-intermediate/high | 1.02 | (0.42–1.12) | - |
| - | Locally advanced | 1.12 | (0.49–4.92) | - |
| Covariates | Category | Adjusted HR * | (95% CI) | p-Value |
|---|---|---|---|---|
| Curative treatment | RP | Ref | - | <0.0001 |
| - | IMRT | 2.74 | (1.72–4.84) | - |
| Age | 20–59 | Ref | - | 0.2723 |
| - | 60–65 | 1.01 | (0.53–1.05) | - |
| Year of diagnosis | 2011 | Ref | - | 0.7540 |
| - | 2012 | 1.41 | (0.74–2.66) | - |
| - | 2013 | 1.20 | (0.63–2.29) | - |
| - | 2014 | 1.03 | (0.53–2.01) | - |
| - | 2015 | 1.36 | (0.73–2.52) | - |
| CCI scores | 0 | Ref | - | 0.2526 |
| - | 1 | 1.04 | (0.59–1.84) | - |
| - | 2+ | 1.68 | (0.86–3.28) | - |
| Clinical T-stage | T1 | Ref | - | 0.4324 |
| - | T2a | 1.05 | (0.22–1.90) | - |
| - | T2b | 1.09 | (0.46–2.61) | - |
| - | T2c | 1.53 | (0.79–2.94) | - |
| Grade group (max Gleason grade) | 1–2 | Ref | - | 0.1313 |
| - | 3 | 1.38 | (0.91–2.11) | - |
| Pretreatment PSA (ng/mL) | 0–5 | Ref | - | 0.5167 |
| - | 5–10 | 1.16 | (0.51–2.26) | - |
| - | 10–20 | 2.18 | (0.63–3.92) | - |
| Income | <NTD$21,000 | Ref | - | 0.9229 |
| - | NTD$21,000–NTD$30,000 | 1.02 | (0.60–1.73) | - |
| - | NTD$30,000–NTD$45,000 | 1.09 | (0.63–1.87) | - |
| - | NTD$45,000+ | 0.87 | (0.44–1.72) | - |
| Hospital level | Medical center | Ref | - | 0.2786 |
| - | Others | 1.27 | (0.83–1.95) | - |
| Hospital area | North | Ref | - | 0.2751 |
| - | Central | 1.16 | (0.87–2.46) | - |
| - | South | 1.25 | (0.75–2.92) | - |
| - | East | 1.30 | (0.60–6.39) | - |
| Clinical T-stage | T1 | Ref | - | 0.5458 |
| - | T2a | 1.04 | (0.49–1.44) | - |
| - | T2b | 1.09 | (0.41–1.98) | - |
| - | T2c | 1.18 | (0.40–2.16) | - |
| D’Amico | Localized-low | Ref | - | 0.1444 |
| - | Localized-intermediate/high | 1.26 | (0.41–2.26) | - |
| - | Locally advanced | 2.08 | (0.63–3.92) | - |
| Covariates | Category | Adjusted HR * | (95% CI) | p-Value |
|---|---|---|---|---|
| Curative treatment | RP | Ref | - | 0.0324 |
| - | IMRT | 1.28 | (1.09–1.90) | - |
| Age | 20–59 | Ref | - | 0.2958 |
| - | 60–65 | 1.04 | (0.27–1.49) | - |
| Year of diagnosis | 2011 | Ref | - | 0.4456 |
| - | 2012 | 0.65 | (0.22–1.92) | - |
| - | 2013 | 0.66 | (0.21–2.03) | - |
| - | 2014 | 0.13 | (0.02–1.11) | - |
| - | 2015 | 0.78 | (0.22–2.76) | - |
| CCI scores | 0 | Ref | - | 0.6160 |
| - | 1 | 1.44 | (0.60–3.46) | - |
| - | 2+ | 1.08 | (0.17–4.65) | - |
| Clinical T-stage | T1 | Ref | - | 0.4876 |
| - | T2a | 1.09 | (0.31–1.67) | - |
| - | T2b | 1.51 | (0.70–2.47) | - |
| - | T2c | 1.79 | (0.37–3.31) | - |
| Grade group (max Gleason grade) | 1–2 | Ref | - | 0.6298 |
| - | 3 | 1.02 | (0.36–1.86) | - |
| Pretreatment PSA (ng/mL) | 0–5 | Ref | - | 0.4772 |
| - | 5–10 | 1.14 | (0.72–2.72) | - |
| - | 10–20 | 2.07 | (0.53–3.25) | - |
| Income | <NTD$21,000 | Ref | - | 0.4134 |
| - | NTD$21,000–NTD$30,000 | 0.82 | (0.70–1.81) | - |
| - | NTD$30,000–NTD$45,000 | 0.76 | (0.52–1.75) | - |
| - | NTD$45,000+ | 0.43 | (0.38–1.64) | - |
| Hospital level | Medical center | Ref | - | 0.7466 |
| - | Others | 1.15 | (0.49–2.69) | - |
| Hospital area | North | Ref | - | 0.7801 |
| - | Central | 1.72 | (0.82–2.00) | - |
| - | South | 2.70 | (0.91–3.04) | - |
| - | East | 2.90 | (0.89–4.10) | |
| Clinical T-stage | T1 | Ref | 0.5088 | |
| - | T2a | 2.07 | (0.79–5.45) | |
| - | T2b | 1.30 | (0.26–6.48) | |
| - | T2c | 1.23 | (0.47–3.25) | |
| D’Amico | Localized-low | Ref | 0.4473 | |
| - | Localized-intermediate/high | 1.95 | (0.83–4.61) | |
| - | Locally advanced | 2.59 | (0.42–6.19) |
| Covariates | Category | Adjusted HR * | (95% CI) | p-Value |
|---|---|---|---|---|
| Curative treatment | RP | Ref | - | 0.0052 |
| - | IMRT | 2.11 | (1.40–4.88) | - |
| Age | 20–59 | Ref | - | 0.7013 |
| - | 60–65 | 1.25 | (0.40–3.87) | - |
| Year of diagnosis | 2011 | Ref | - | 0.9648 |
| - | 2012 | 0.91 | (0.31–2.64) | - |
| - | 2013 | 0.89 | (0.29–2.71) | - |
| - | 2014 | 0.71 | (0.22–2.29) | - |
| - | 2015 | 0.68 | (0.20–2.31) | - |
| CCI scores | 0 | Ref | - | 0.4858 |
| - | 1 | 1.02 | (0.89–1.90) | - |
| - | 2+ | 1.05 | (0.71–1.72) | - |
| Clinical T-stage | T1 | Ref | - | 0.7425 |
| - | T2a | 1.04 | (0.64–4.27) | - |
| - | T2b | 1.07 | (0.73–7.57) | - |
| - | T2c | 1.15 | (0.37–3.58) | - |
| Grade group (max Gleason grade) | 1–2 | Ref | - | 0.7957 |
| - | 3 | 1.11 | (0.43–1.91) | - |
| Pretreatment PSA (ng/mL) | 0–5 | Ref | 0.2498 | |
| - | 5–10 | 1.05 | (0.61–1.55) | - |
| - | 10–20 | 1.27 | (0.88–2.24) | - |
| Income | <NTD$21,000 | Ref | - | 0.1661 |
| - | NTD$21,000–NTD$30,000 | 0.88 | (0.52–2.14) | - |
| - | NTD$30,000–NTD$45,000 | 0.73 | (0.25–2.13) | - |
| - | NTD$45,000+ | 0.52 | (0.55–2.07) | - |
| Hospital level | Academic centers | Ref | 0.1403 | |
| - | Nonacademic centers | 0.80 | (0.71–1.96) | - |
| Hospital area | North | Ref | 0.1769 | |
| - | Central | 1.38 | (0.99–2.71) | - |
| - | South | 1.60 | (0.99–2.82) | - |
| - | East | 2.03 | (0.56–2.76) | - |
| Clinical T-stage | T1 | Ref | 0.3597 | |
| - | T2a | 0.97 | (0.38–1.44) | - |
| - | T2b | 1.04 | (0.37–2.83) | - |
| - | T2c | 1.19 | (0.42–2.25) | - |
| D’Amico | Localized-low | Ref | 0.0981 | |
| - | Localized-intermediate/high | 1.15 | (0.46–1.86) | - |
| - | Locally advanced | 1.72 | (0.98–3.24) | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, S.-Y.; Chang, S.-C.; Chen, C.-I.; Huang, C.-C. Oncologic Outcomes of Radical Prostatectomy and High-Dose Intensity-Modulated Radiotherapy with Androgen-Deprivation Therapy for Relatively Young Patients with Unfavorable Intermediate-Risk Prostate Adenocarcinoma. Cancers 2021, 13, 1517. https://doi.org/10.3390/cancers13071517
Wu S-Y, Chang S-C, Chen C-I, Huang C-C. Oncologic Outcomes of Radical Prostatectomy and High-Dose Intensity-Modulated Radiotherapy with Androgen-Deprivation Therapy for Relatively Young Patients with Unfavorable Intermediate-Risk Prostate Adenocarcinoma. Cancers. 2021; 13(7):1517. https://doi.org/10.3390/cancers13071517
Chicago/Turabian StyleWu, Szu-Yuan, Shyh-Chyi Chang, Chang-I Chen, and Chung-Chien Huang. 2021. "Oncologic Outcomes of Radical Prostatectomy and High-Dose Intensity-Modulated Radiotherapy with Androgen-Deprivation Therapy for Relatively Young Patients with Unfavorable Intermediate-Risk Prostate Adenocarcinoma" Cancers 13, no. 7: 1517. https://doi.org/10.3390/cancers13071517
APA StyleWu, S.-Y., Chang, S.-C., Chen, C.-I., & Huang, C.-C. (2021). Oncologic Outcomes of Radical Prostatectomy and High-Dose Intensity-Modulated Radiotherapy with Androgen-Deprivation Therapy for Relatively Young Patients with Unfavorable Intermediate-Risk Prostate Adenocarcinoma. Cancers, 13(7), 1517. https://doi.org/10.3390/cancers13071517






