Image-Guided Adaptive Brachytherapy (IGABT) for Primary Vaginal Cancer: Results of the International Multicenter RetroEMBRAVE Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
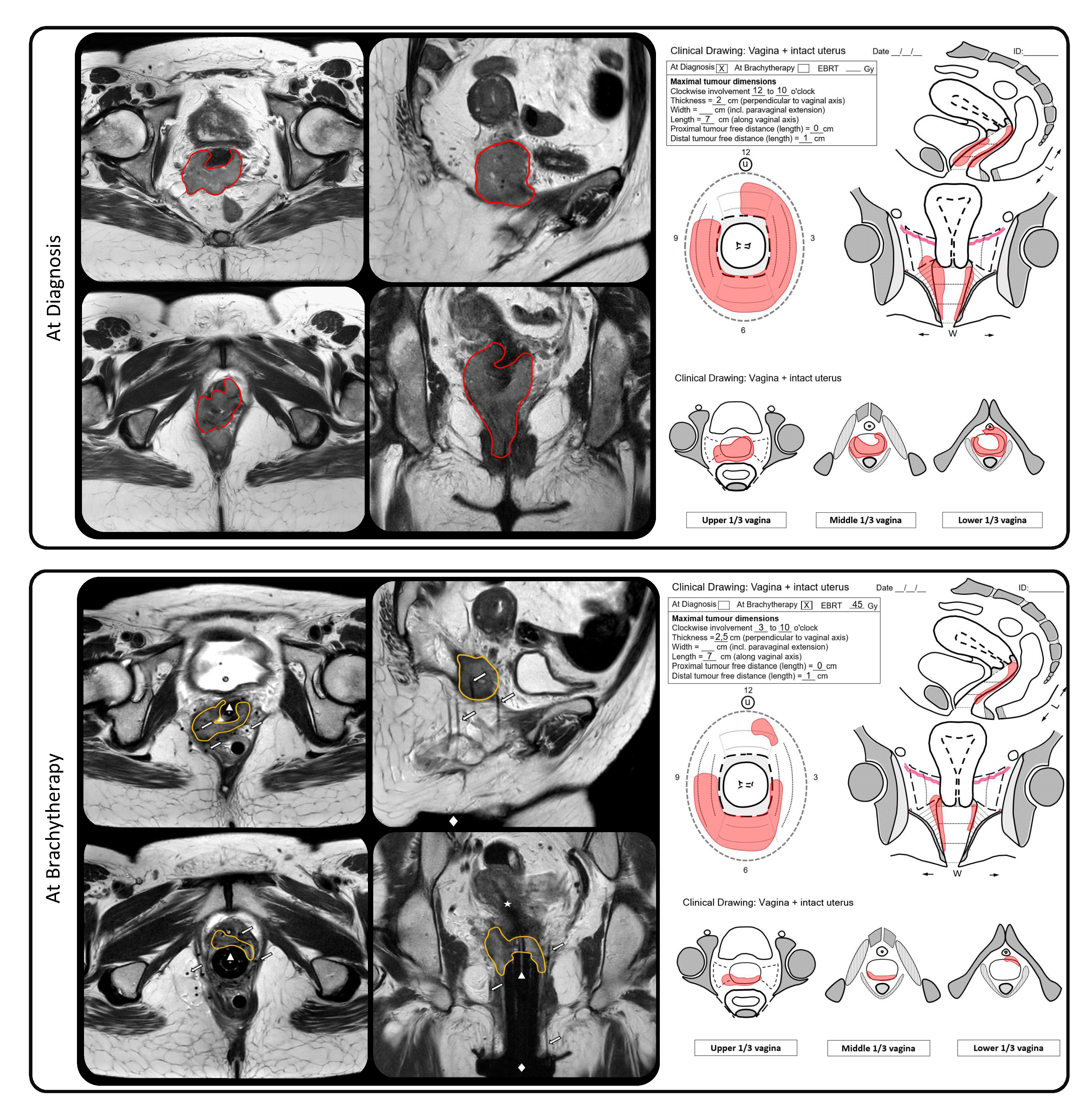
2. Materials and Methods
2.1. Patients
2.2. Treatment
2.3. Statistical Analyses
3. Results
3.1. Patients Characteristics
3.2. Treatment Characteristics
3.3. Dose Volume Parameters
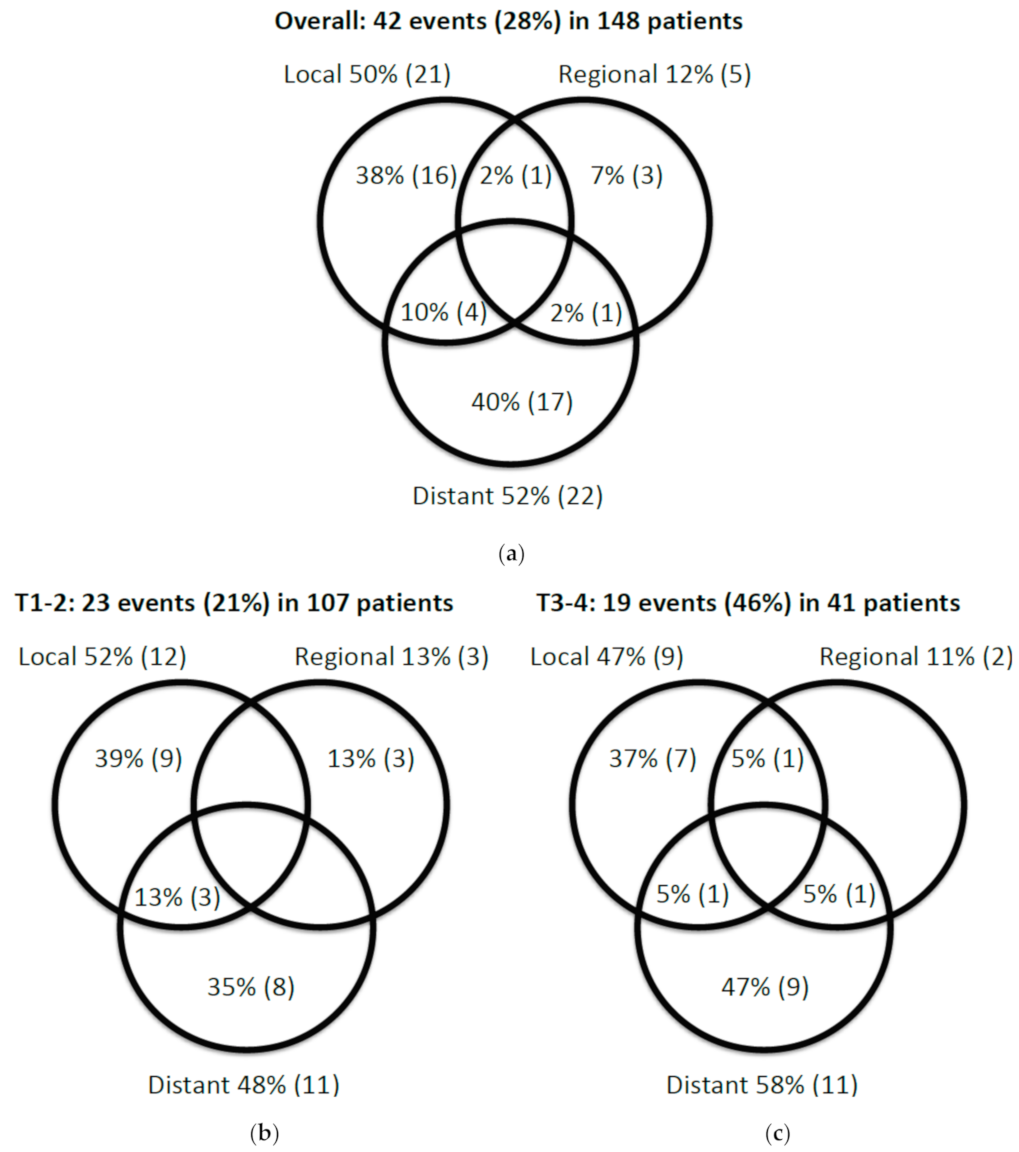
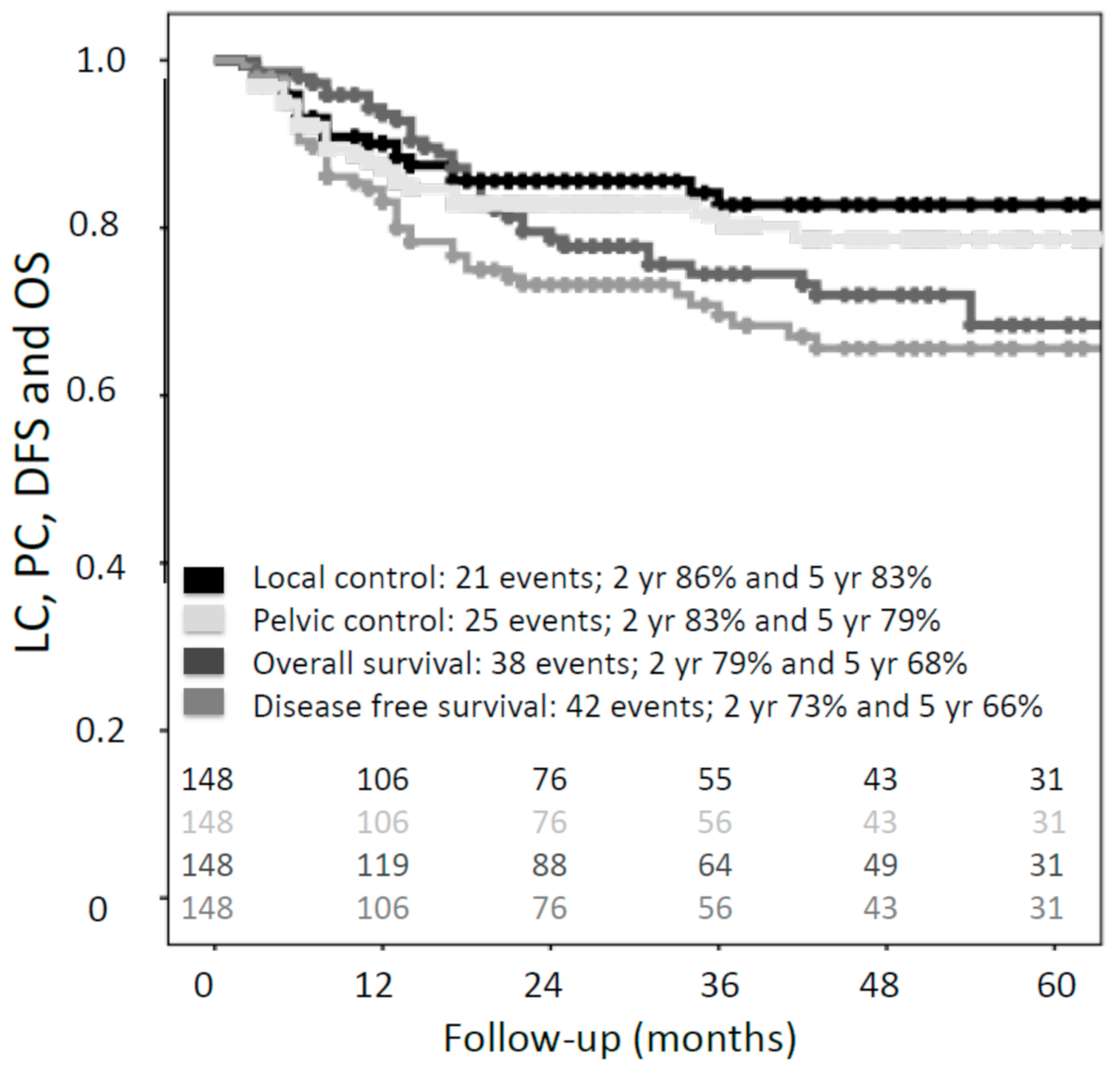
3.4. Oncological Outcomes
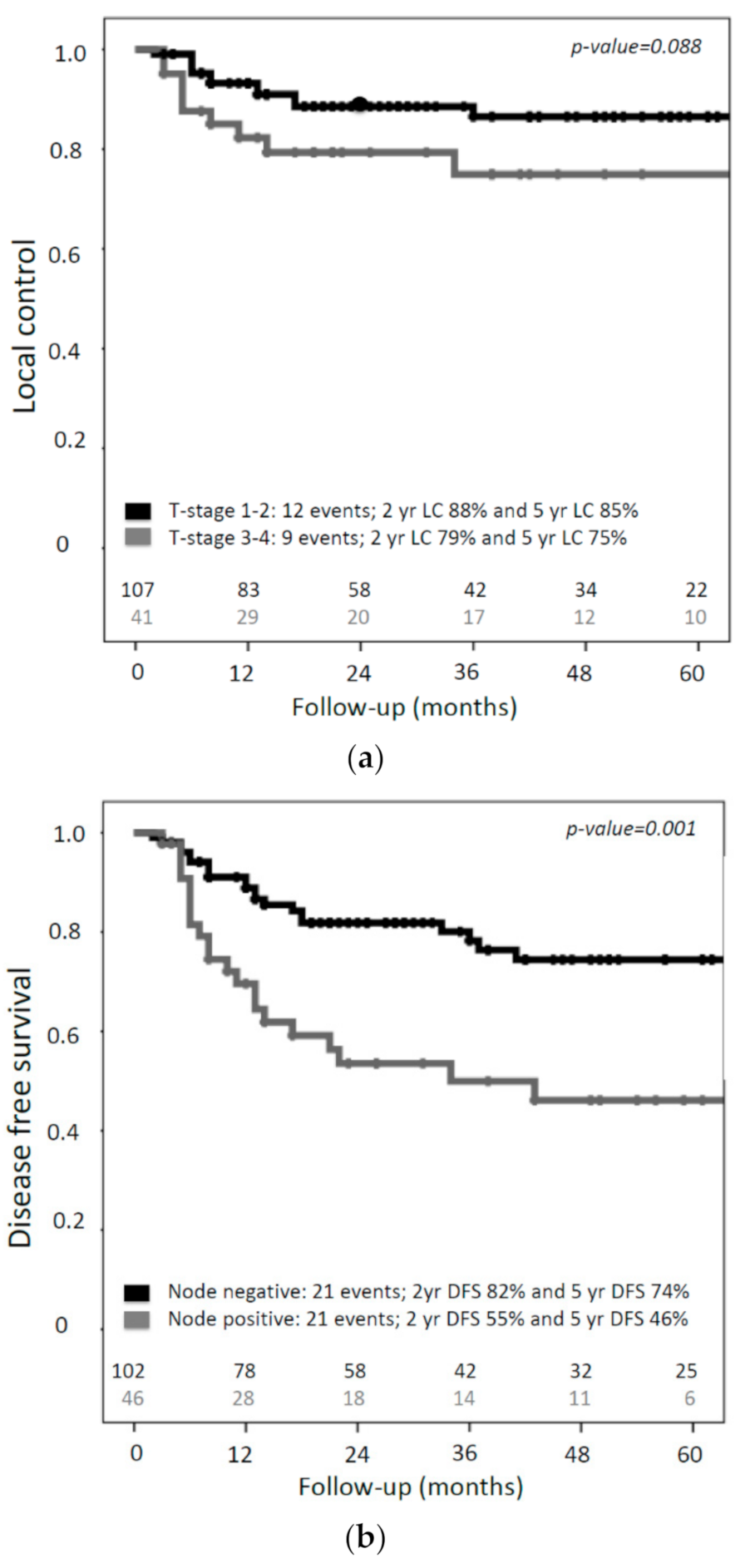
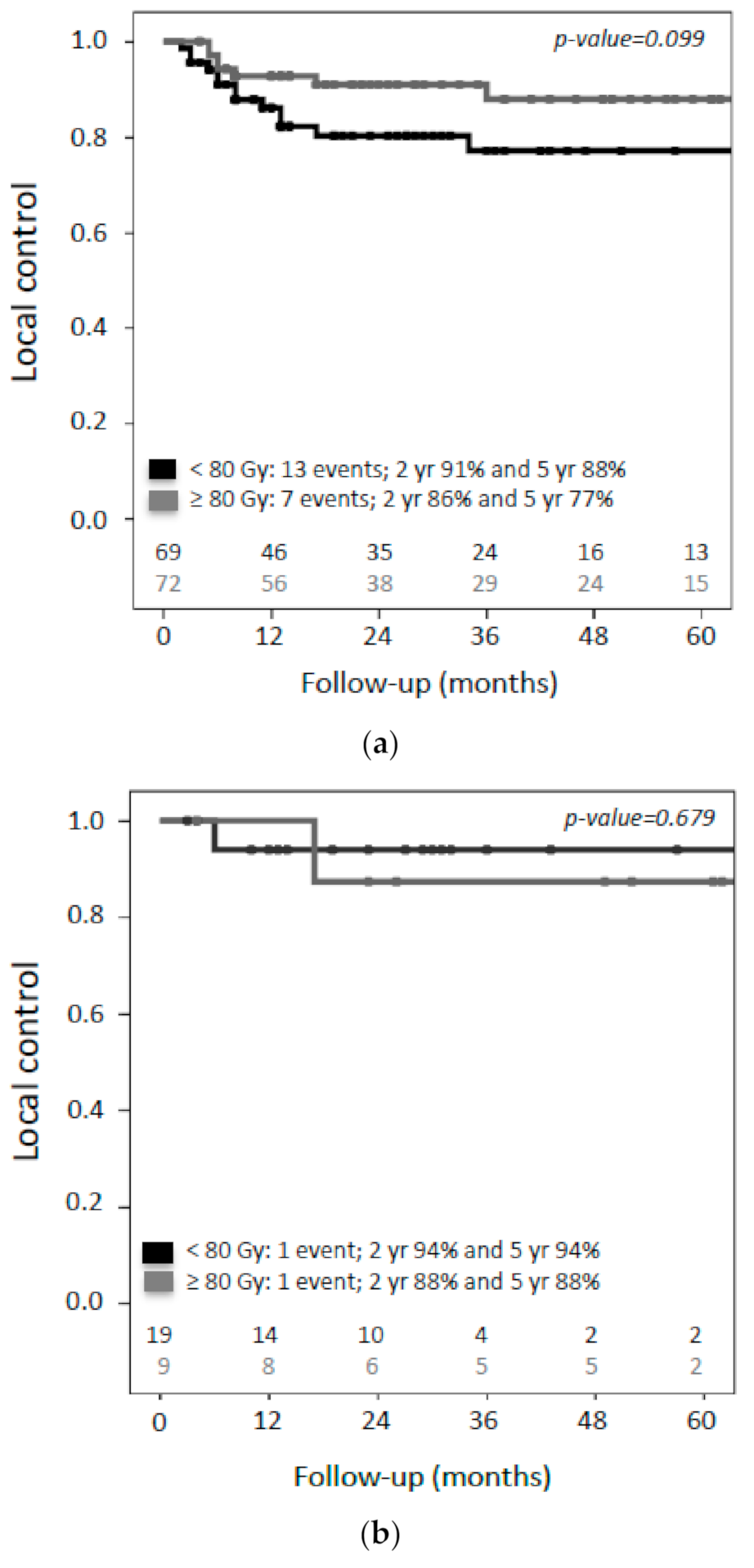
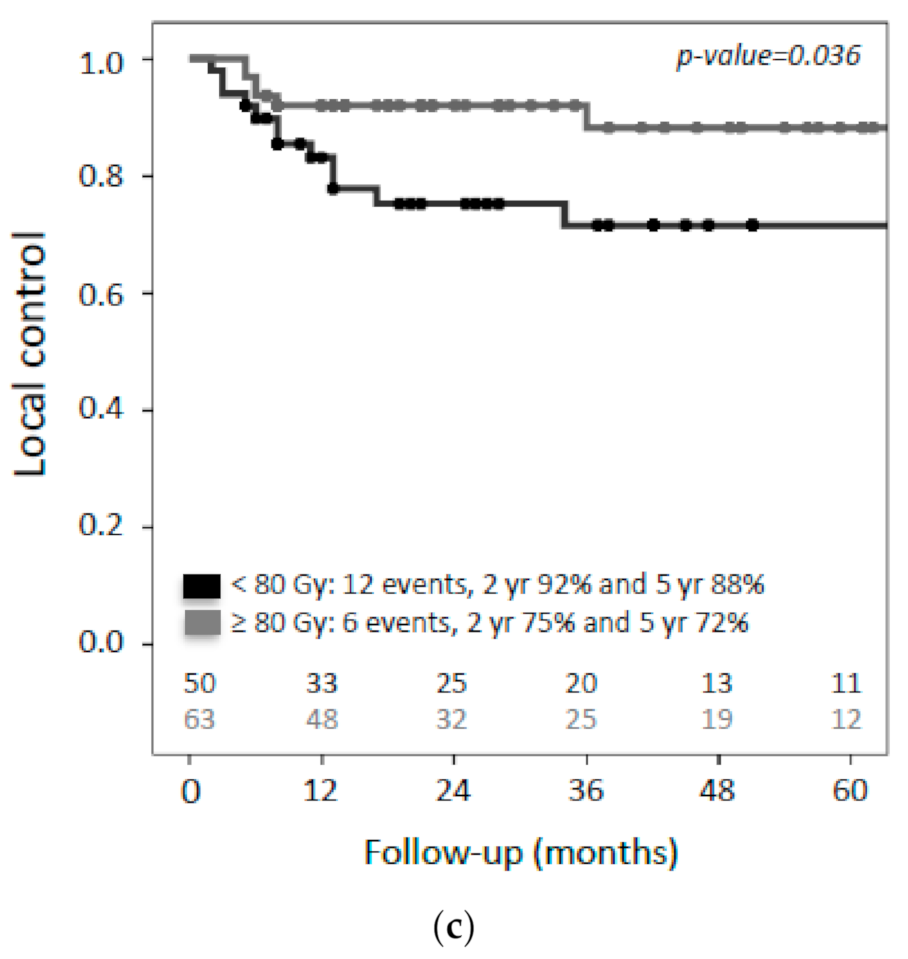
3.5. Prognostic Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Daling, J.R.; Madeleine, M.M.; Schwartz, S.M.; Shera, K.A.; Carter, J.J.; McKnight, B.; Porter, P.L.; Galloway, D.A.; McDougall, J.K.; Tamimi, H. A population-based study of squamous cell vaginal cancer: HPV and cofactors. Gynecol. Oncol. 2002, 84, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Westerveld, H.; Nesvacil, N.; Fokdal, L.; Chargari, C.; Schmid, M.P.; Milosevic, M.; Mahantshetty, U.M.; Nout, R.A. Definitive radiotherapy with image-guided adaptive brachytherapy for primary vaginal cancer. Lancet Oncol. 2020, 21, e157–e167. [Google Scholar] [CrossRef]
- Miyamoto, D.T.; Viswanathan, A.N. Concurrent chemoradiation for vaginal cancer. PLoS ONE 2013, 8, e65048. [Google Scholar] [CrossRef] [PubMed]
- Rajagopalan, M.S.; Xu, K.M.; Lin, J.F.; Sukumvanich, P.; Krivak, T.C.; Beriwal, S. Adoption and impact of concurrent chemoradiation therapy for vaginal cancer: A national cancer data base (NCDB) study. Gynecol. Oncol. 2014, 135, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Guy, J.B.; Falk, A.T.; Auberdiac, P.; Cartier, L.; Vallard, A.; Ollier, E.; Trone, J.C.; Khodri, M.; Chargari, C.; Magne, N. Dosimetric study of volumetric arc modulation with rapidarc and intensity-modulated radiotherapy in patients with cervical cancer and comparison with 3-dimensional conformal technique for definitive radiotherapy in patients with cervical cancer. Med Dosim. 2016, 41, 9–14. [Google Scholar] [CrossRef]
- Klopp, A.H.; Yeung, A.R.; Deshmukh, S.; Gil, K.M.; Wenzel, L.; Westin, S.N.; Gifford, K.; Gaffney, D.K.; Small, W.; Thompson, S., Jr.; et al. Patient-reported toxicity during pelvic intensity-modulated radiation therapy: NRG oncology-RTOG 1203. J. Clin. Oncol. 2018, 36, 2538–2544. [Google Scholar] [CrossRef]
- Potter, R.; Kirisits, C.; Erickson, B.; Haie Meder, C.; Van Limbergen, E.; Lindegaard, J.C.; Rownd, J.; Tanderup, K.; Thomadsen, B.R. ICRU report no. 89. Prescribing, recording, and reporting brachytherapy for cancer of the cervix. J. ICRU 2013, 13, 1–274. [Google Scholar]
- Sturdza, A.; Potter, R.; Fokdal, L.U.; Haie-Meder, C.; Tan, L.T.; Mazeron, R.; Petric, P.; Segedin, B.; Jurgenliemk-Schulz, I.M.; Nomden, C.; et al. Image guided brachytherapy in locally advanced cervical cancer: Improved pelvic control and survival in retroembrace, a multicenter cohort study. Radiother. Oncol. 2016, 120, 428–433. [Google Scholar] [CrossRef]
- Potter, R.; Tanderup, K.; Kirisits, C.; de Leeuw, A.; Kirchheiner, K.; Nout, R.; Tan, L.T.; Haie-Meder, C.; Mahantshetty, U.; Segedin, B.; et al. The Embrace II study: The outcome and prospect of two decades of evolution within the GEC-estro GYN working group and the embrace studies. Clin. Transl. Radiat. Oncol. 2018, 9, 48–60. [Google Scholar] [CrossRef]
- FIGO Committee. Current FIGO staging for cancer of the vagina, fallopian tube, ovary, and gestational trophoblastic neoplasia. Int. J. Gynaecol. Obstet. 2009, 105, 3–4. [Google Scholar] [CrossRef]
- Haie-Meder, C.; Potter, R.; Van Limbergen, E.; Briot, E.; De Brabandere, M.; Dimopoulos, J.; Dumas, I.; Hellebust, T.P.; Kirisits, C.; Lang, S.; et al. Recommendations from gynaecological (GYN) GEC-ESTRO working group (i): Concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother. Oncol. 2005, 74, 235–245. [Google Scholar] [CrossRef]
- Potter, R.; Haie-Meder, C.; Van Limbergen, E.; Barillot, I.; De Brabandere, M.; Dimopoulos, J.; Dumas, I.; Erickson, B.; Lang, S.; Nulens, A.; et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (ii): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy—3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother. Oncol. 2006, 78, 67–77. [Google Scholar] [CrossRef]
- Dimopoulos, J.C.; Schmid, M.P.; Fidarova, E.; Berger, D.; Kirisits, C.; Potter, R. Treatment of locally advanced vaginal cancer with radiochemotherapy and magnetic resonance image-guided adaptive brachytherapy: Dose-volume parameters and first clinical results. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 1880–1888. [Google Scholar] [CrossRef]
- Fokdal, L.; Sturdza, A.; Mazeron, R.; Haie-Meder, C.; Tan, L.T.; Gillham, C.; Segedin, B.; Jurgenliemk-Schultz, I.; Kirisits, C.; Hoskin, P.; et al. Image guided adaptive brachytherapy with combined intracavitary and interstitial technique improves the therapeutic ratio in locally advanced cervical cancer: Analysis from the retroembrace study. Radiother. Oncol. 2016, 120, 434–440. [Google Scholar] [CrossRef]
- Gebhardt, B.J.; Vargo, J.A.; Kim, H.; Houser, C.J.; Glaser, S.M.; Sukumvanich, P.; Olawaiye, A.B.; Kelley, J.L.; Edwards, R.P.; Comerci, J.T.; et al. Image-based multichannel vaginal cylinder brachytherapy for the definitive treatment of gynecologic malignancies in the vagina. Gynecol. Oncol. 2018, 150, 293–299. [Google Scholar] [CrossRef]
- Huertas, A.; Dumas, I.; Escande, A.; Del Campo, R.E.; Felefly, T.; Canova, C.H.; Tailleur, A.; Gouy, S.; Bentivegna, E.; Morice, P.; et al. Image-guided adaptive brachytherapy in primary vaginal cancers: A monocentric experience. Brachytherapy 2018, 17, 571–579. [Google Scholar] [CrossRef]
- Lee, L.J.; Damato, A.L.; Viswanathan, A.N. Clinical outcomes of high-dose-rate interstitial gynecologic brachytherapy using real-time ct guidance. Brachytherapy 2013, 12, 303–310. [Google Scholar] [CrossRef]
- Manuel, M.M.; Cho, L.P.; Catalano, P.J.; Damato, A.L.; Miyamoto, D.T.; Tempany, C.M.; Schmidt, E.J.; Viswanathan, A.N. Outcomes with image-based interstitial brachytherapy for vaginal cancer. Radiother. Oncol. 2016, 120, 486–492. [Google Scholar] [CrossRef]
- De Crevoisier, R.; Sanfilippo, N.; Gerbaulet, A.; Morice, P.; Pomel, C.; Castaigne, D.; Pautier, P.; Lhomme, C.; Duvillard, P.; Haie-meder, C. Exclusive radiotherapy for primary squamous cell carcinoma of the vagina. Radiother. Oncol. 2007, 85, 362–370. [Google Scholar] [CrossRef]
- Ikushima, H.; Wakatsuki, M.; Ariga, T.; Kaneyasu, Y.; Tokumaru, S.; Isohashi, F.; Ii, N.; Uno, T.; Ohno, T.; Arisawa, K.; et al. Radiotherapy for vaginal cancer: A multi-institutional survey study of the Japanese radiation oncology study group. Int. J. Clin. Oncol. 2018, 23, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Hiniker, S.M.; Roux, A.; Murphy, J.D.; Harris, J.P.; Tran, P.T.; Kapp, D.S.; Kidd, E.A. Primary squamous cell carcinoma of the vagina: Prognostic factors, treatment patterns, and outcomes. Gynecol. Oncol. 2013, 131, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Lian, J.; Dundas, G.; Carlone, M.; Ghosh, S.; Pearcey, R. Twenty-year review of radiotherapy for vaginal cancer: An institutional experience. Gynecol. Oncol. 2008, 111, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Frank, S.J.; Jhingran, A.; Levenback, C.; Eifel, P.J. Definitive radiation therapy for squamous cell carcinoma of the vagina. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62, 138–147. [Google Scholar] [CrossRef]
- Lee, W.R.; Marcus, R.B.; Sombeck, M.D., Jr.; Mendenhall, W.M.; Morgan, L.S.; Freeman, D.E.; Million, R.R. Radiotherapy alone for carcinoma of the vagina: The importance of overall treatment time. Int. J. Radiat. Oncol. Biol. Phys. 1994, 29, 983–988. [Google Scholar] [CrossRef]
- Greenwalt, J.C.; Amdur, R.J.; Morris, C.G.; Morgan, L.S.; Castagno, J.; Markham, M.J.; Rich, S.; Yeung, A.R. Outcomes of definitive radiation therapy for primary vaginal carcinoma. Am. J. Clin. Oncol. 2015, 38, 583–587. [Google Scholar] [CrossRef]
- Taylor, M.B.; Dugar, N.; Davidson, S.E.; Carrington, B.M. Magnetic resonance imaging of primary vaginal carcinoma. Clin. Radiol. 2007, 62, 549–555. [Google Scholar] [CrossRef]
- Lamoreaux, W.T.; Grigsby, P.W.; Dehdashti, F.; Zoberi, I.; Powell, M.A.; Gibb, R.K.; Rader, J.S.; Mutch, D.G.; Siegel, B.A. Fdg-pet evaluation of vaginal carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62, 733–737. [Google Scholar] [CrossRef]
- Schmid, M.P.; Fokdal, L.; Westerveld, H.; Chargari, C.; Rohl, L.; Morice, P.; Nesvacil, N.; Mazeron, R.; Haie-Meder, C.; Potter, R.; et al. Recommendations from gynaecological (GYN) GEC-ESTRO working group—ACROP: Target concept for image guided adaptive brachytherapy in primary vaginal cancer. Radiother. Oncol. 2019, 145, 36–44. [Google Scholar] [CrossRef]
- Beriwal, S.; Demanes, D.J.; Erickson, B.; Jones, E.; De Los Santos, J.F.; Cormack, R.A.; Yashar, C.; Rownd, J.J.; Viswanathan, A.N. American brachytherapy society consensus guidelines for interstitial brachytherapy for vaginal cancer. Brachytherapy 2012, 11, 68–75. [Google Scholar] [CrossRef]
| T-classification | |
| 1 | 28 (19%) |
| 2 | 79 (53%) |
| 3 | 21 (14%) |
| 4 | 20 (14%) |
| N-classification | |
| 0 | 102 (69%) |
| 1 | 46 (31%) |
| Histology | |
| Squamous cell carcinoma | 134 (91%) |
| Adenocarcinoma | 8 (5%) |
| Adenosquamous carcinoma | 6 (4%) |
| Maximum tumor diameter at diagnosis | |
| ≤4 cm | 77 (52%) |
| >4 cm | 71 (48%) |
| Vaginal involvement at diagnosis | |
| Upper third | 26 (18%) |
| Middle third | 16 (11%) |
| Lower third | 38 (26%) |
| Upper two-thirds | 14 (9%) |
| Lower two-thirds | 14 (9%) |
| Entire vagina | 23 (16%) |
| Unknown | 17 (11%) |
| Concurrent cisplatin | |
| No | 54 (36%) |
| Yes | 94 (64%) |
| EBRT technique | |
| APPA/box | 8 (5%) |
| 3DCRT IMRT/VMAT | 82 (57%) 55 (38%) |
| Dose rate | |
| PDR | 115 (78%) |
| HDR | 33 (22%) |
| Number of applications | |
| 1 | 100 (68%) |
| 2 | 36 (24%) |
| 3 | 12 (8%) |
| Imaging at time of BT | |
| CT | 42 (28%) |
| MRI | 77 (52%) |
| MRI/CT # | 29 (20%) |
| BT technique | |
| Intracavitary | 67 (45%) |
| Interstitial +/− intracavitary | 81 (55%) |
| Variable | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age | ||||||
| <63 vs. ≥63 | 0.72 | 0.38–1.36 | 0.288 | |||
| Chronic disease | ||||||
| Yes vs. No | 0.63 | 0.30–1.31 | 0.215 | |||
| Hysterectomy | ||||||
| Yes vs. No | 1.02 | 0.55–1.89 | 0.947 | |||
| Tumor-stage | ||||||
| T1/T2 vs. T3/T4 | 2.27 | 1.23–4.16 | 0.008 * | 1.65 | 0.86–3.15 | 0.134 |
| Tumor diameter at diagnosis | ||||||
| ≤4 cm vs. >4 cm | 1.92 | 1.03–3.57 | 0.041 * | 1.42 | 0.73–2.73 | 0.301 |
| Lymph node metastases | ||||||
| Yes vs. No | 2.75 | 1.50–5.03 | 0.001 * | 2.24 | 1.18–4.22 | 0.013 * |
| Concomitant chemotherapy | ||||||
| Yes vs. No | 1.72 | 0.38–1.36 | 0.311 | |||
| CTV volume at brachytherapy | ||||||
| <17.6 cm3 vs. ≥17.6 cm3 | 1.10 | 0.55–2.18 | 0.794 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Westerveld, H.; Schmid, M.P.; Nout, R.A.; Chargari, C.; Pieters, B.R.; Creutzberg, C.L.; Sturdza, A.; Lindegaard, J.C.; van Kesteren, Z.; Mazeron, R.; et al. Image-Guided Adaptive Brachytherapy (IGABT) for Primary Vaginal Cancer: Results of the International Multicenter RetroEMBRAVE Cohort Study. Cancers 2021, 13, 1459. https://doi.org/10.3390/cancers13061459
Westerveld H, Schmid MP, Nout RA, Chargari C, Pieters BR, Creutzberg CL, Sturdza A, Lindegaard JC, van Kesteren Z, Mazeron R, et al. Image-Guided Adaptive Brachytherapy (IGABT) for Primary Vaginal Cancer: Results of the International Multicenter RetroEMBRAVE Cohort Study. Cancers. 2021; 13(6):1459. https://doi.org/10.3390/cancers13061459
Chicago/Turabian StyleWesterveld, Henrike, Maximilian P. Schmid, Remi A. Nout, Cyrus Chargari, Bradley R. Pieters, Carien L. Creutzberg, Alina Sturdza, Jacob C. Lindegaard, Zdenko van Kesteren, Renaud Mazeron, and et al. 2021. "Image-Guided Adaptive Brachytherapy (IGABT) for Primary Vaginal Cancer: Results of the International Multicenter RetroEMBRAVE Cohort Study" Cancers 13, no. 6: 1459. https://doi.org/10.3390/cancers13061459
APA StyleWesterveld, H., Schmid, M. P., Nout, R. A., Chargari, C., Pieters, B. R., Creutzberg, C. L., Sturdza, A., Lindegaard, J. C., van Kesteren, Z., Mazeron, R., Nesvacil, N., & Fokdal, L. U. (2021). Image-Guided Adaptive Brachytherapy (IGABT) for Primary Vaginal Cancer: Results of the International Multicenter RetroEMBRAVE Cohort Study. Cancers, 13(6), 1459. https://doi.org/10.3390/cancers13061459






