Significance of the Overexpression of Substance P and Its Receptor NK-1R in Head and Neck Carcinogenesis: A Systematic Review and Meta-Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Data Extraction
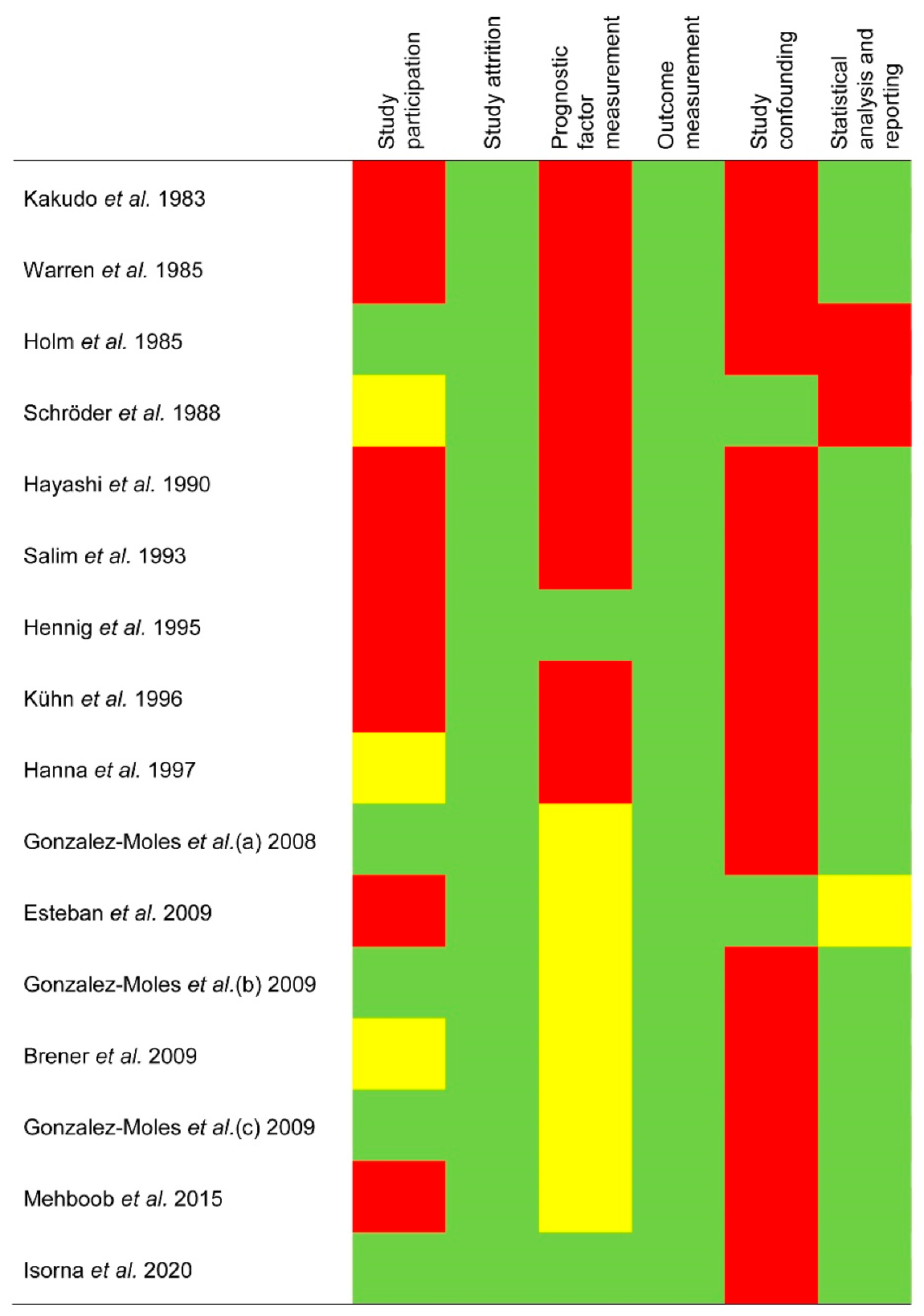
2.5. Evaluation of Quality and Risk of Bias
2.6. Statistical Analysis
3. Results
3.1. Literature Search
3.2. Study Characteristics
3.3. Qualitative Evaluation
3.4. Quantitative Evaluation (Meta-Analysis)
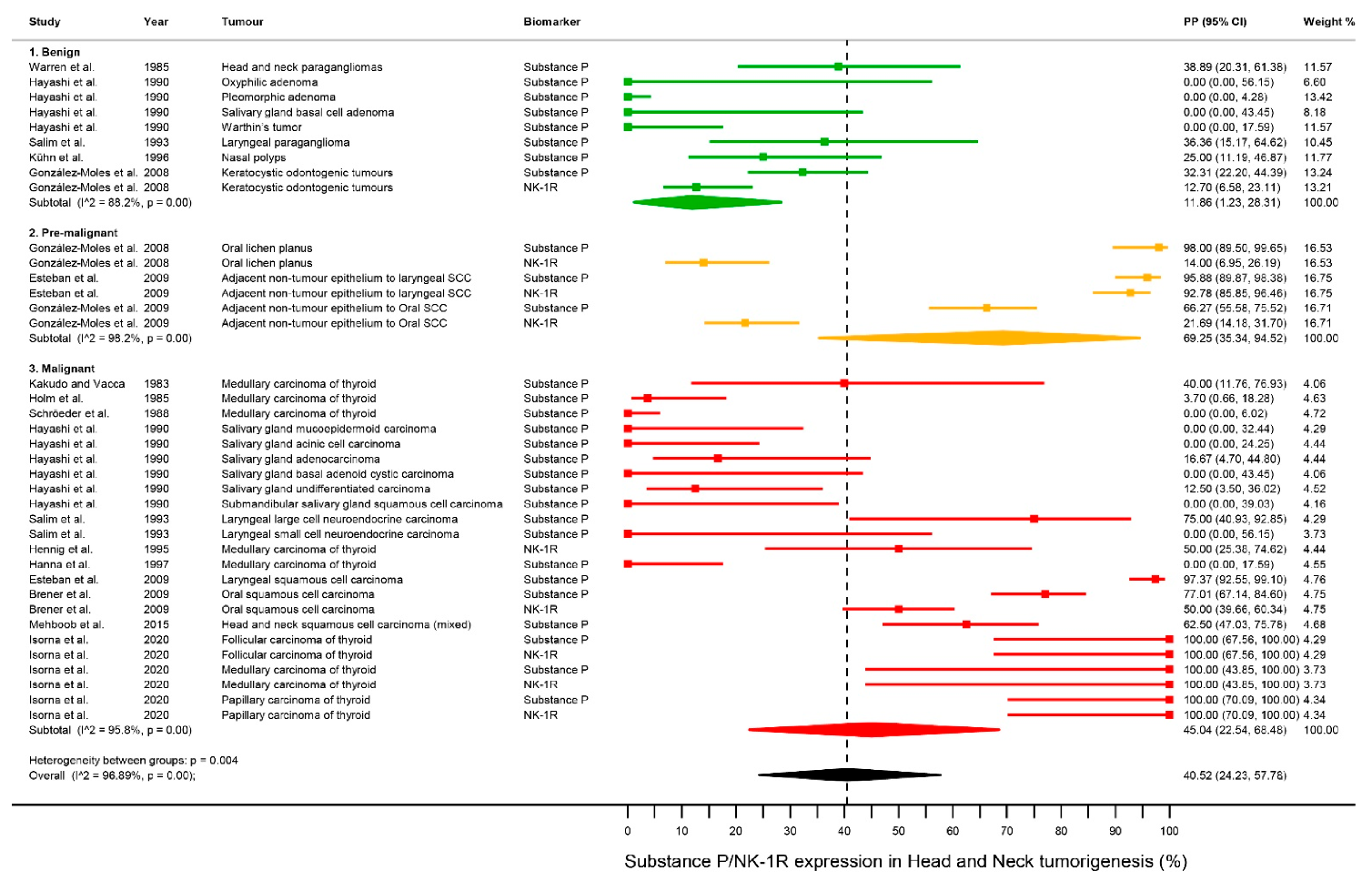
3.4.1. Differential Expression of SP/NK-1R in Head & Neck Tumorigenesis
3.4.2. Differential Expression of SP/NK-1R in Benign Tumors
3.4.3. Differential Expression of SP/NK-1R in Pre-Malignant Tissues
3.4.4. Differential Expression of SP/NK-1R in Pre-Malignant Tissues
3.5. Quantitative Evaluation (Secondary Analyses)
3.5.1. Sensitivity Analysis
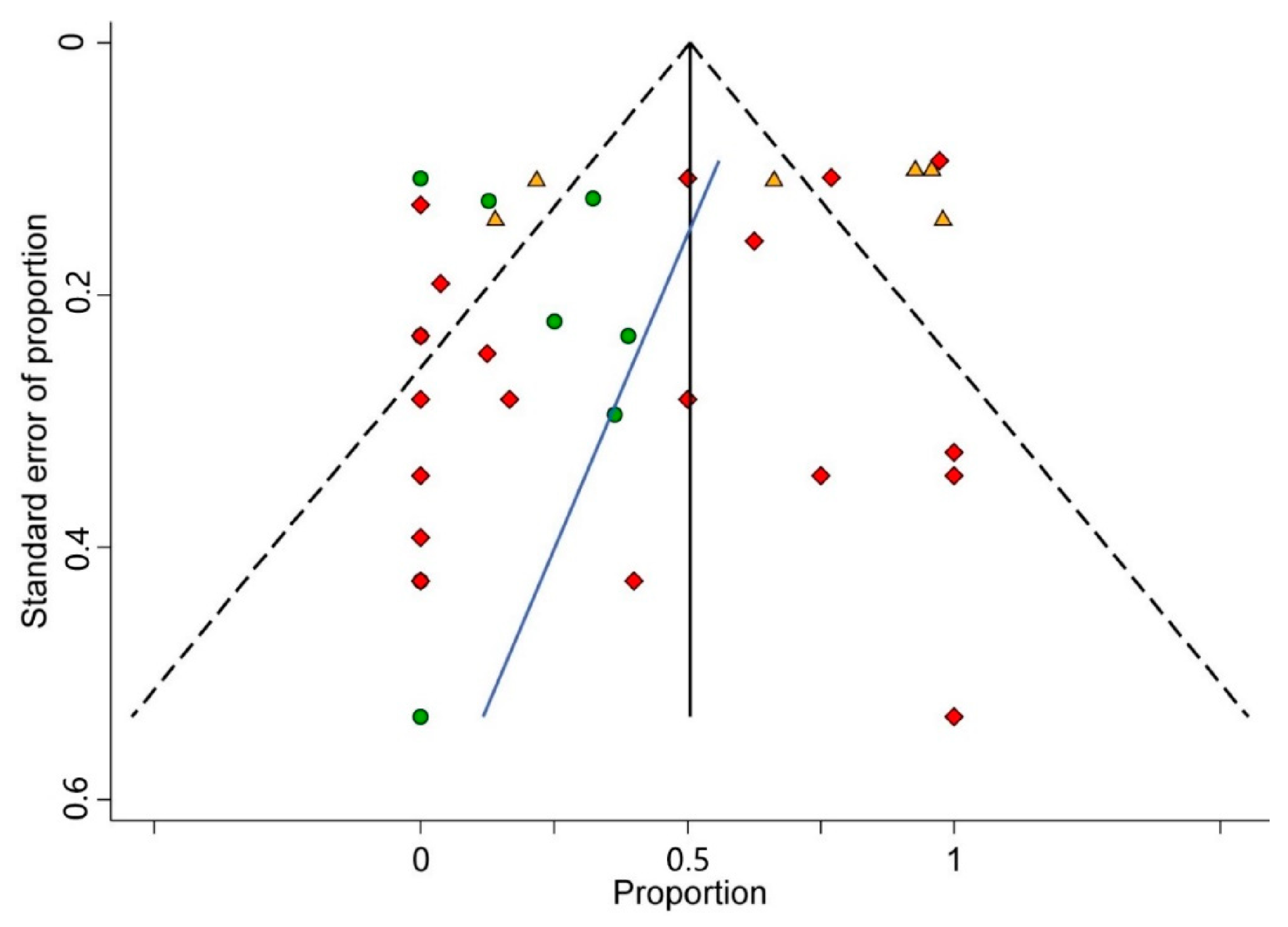
3.5.2. Analysis of Small-Study Effects
3.6. Biological and Oncogenic Roles of SP/NK-1R
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Argiris, A.; Karamouzis, M.V.; Raben, D.; Ferris, R.L. Head and neck cancer. Lancet 2008, 371, 1695–1709. [Google Scholar] [CrossRef]
- Siegel, R.; Ma, J.; Zou, Z.; Jemal, A. Cancer statistics, 2014. CA Cancer J. Clin. 2014, 64, 9–29. [Google Scholar] [CrossRef] [PubMed]
- Leemans, C.R.; Braakhuis, B.J.M.; Brakenhoff, R.H. The molecular biology of head and neck cancer. Nat. Rev. Cancer 2010, 11, 9–22. [Google Scholar] [CrossRef]
- Chi, A.C.; Day, T.A.; Neville, B.W. Oral cavity and oropharyngeal squamous cell carcinoma-an update. CA Cancer J. Clin. 2015, 65, 401–421. [Google Scholar] [CrossRef]
- Steuer, C.E.; El-Deiry, M.; Parks, J.R.; Higgins, K.A.; Saba, N.F. An update on larynx cancer. CA Cancer J. Clin. 2017, 67, 31–50. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.G.; Shah, J.P. TNM Staging of Cancers of the Head and Neck: Striving for Uniformity among Diversity. CA Cancer J. Clin. 2005, 55, 242–258. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, S.D.; Ferlito, A.; Takes, R.P.; Brakenhoff, R.H.; Valentin, M.D.; Woolgar, J.A.; Bradford, C.R.; Rodrigo, J.P.; Rinaldo, A.; Hier, M.P.; et al. Advances and applications of oral cancer basic research. Oral Oncol. 2011, 47, 783–791. [Google Scholar] [CrossRef]
- Polanska, H.; Raudenska, M.; Gumulec, J.; Sztalmachova, M.; Adam, V.; Kizek, R.; Masarik, M. Clinical significance of head and neck squamous cell cancer biomarkers. Oral Oncol. 2014, 50, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Isorna, I.; Esteban, F.; Solanellas, J.; Coveñas, R.; Muñoz, M. The substance P and neurokinin-1 receptor system in human thyroid cancer: An immunohistochemical study. Eur. J. Histochem. 2020, 64. [Google Scholar] [CrossRef]
- Gonzalez-Moles, M.A.; Brener, S.; Ruiz-Avila, I.; Gil-Montoya, J.A.; Tostes, D.; Bravo, M.; Esteban, F. Substance P and NK-1R expression in oral precancerous epithelium. Oncol. Rep. 2009, 22, 1325–1331. [Google Scholar] [CrossRef][Green Version]
- Brener, S.; González-Moles, M.A.; Tostes, D.; Esteban, F.; Gil-Montoya, J.A.; Ruiz-Avila, I.; Bravo, M.; Muñoz, M. A role for the substance P/NK-1 receptor complex in cell proliferation in oral squamous cell carcinoma. Anticancer Res. 2009, 29, 2323–2329. [Google Scholar] [PubMed]
- Esteban, F.; Gonzalez-Moles, M.A.; Castro, D.; Martin-Jaen, M.D.M.; Redondo, M.; Ruiz-Ávila, I.; Munoz, M. Expression of substance P and neurokinin-1-receptor in laryngeal cancer: Linking chronic inflammation to cancer promotion and progression. Histopathology 2009, 54, 258–260. [Google Scholar] [CrossRef]
- Hökfelt, T.; Pernow, B.; Wahren, J. Substance P: A pioneer amongst neuropeptides. J. Intern. Med. 2001, 249, 27–40. [Google Scholar] [CrossRef]
- Muñoz, M.; Coveñas, R. Involvement of substance P and the NK-1 receptor in human pathology. Amino Acids 2014, 46, 1727–1750. [Google Scholar] [CrossRef] [PubMed]
- Munoz, M.; Rosso, M.; Zamarriego, C.; Soult, J.A.; Montero, I.; Pérez, A.; Coveñas, R. Antitumoral Action of the Neurokinin-1-Receptor Antagonist L-733,060 and Mitogenic Action of Substance P on Human Retinoblastoma Cell Lines. Investig. Opthalmol. Vis. Sci. 2005, 46, 2567–2570. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Sharif, T.R.; Sharif, M. Substance P-induced mitogenesis in human astrocytoma cells correlates with activation of the mitogen-activated protein kinase signaling pathway. Cancer Res. 1996, 56, 4983–4991. [Google Scholar] [PubMed]
- Muñoz, M.; Pérez, A.; Rosso, M.; Zamarriego, C.; Rosso, R. Antitumoral action of the neurokinin-1 receptor antagonist L-733 060 on human melanoma cell lines. Melanoma Res. 2004, 14, 183–188. [Google Scholar] [CrossRef]
- Muñoz, M.; Rosso, M.; Pérez, A.; Coveñas, R.; Rosso, R.; Zamarriego, C.; Piruat, J. The NK1 receptor is involved in the antitumoural action of L-733,060 and in the mitogenic action of substance P on neuroblastoma and glioma cell lines. Neuropeptides 2005, 39, 427–432. [Google Scholar] [CrossRef]
- Esteban, F.; Muñoz, M.; Gonzalez-Moles, M.A.; Rosso, M. A role for substance P in cancer promotion and progression: A mechanism to counteract intracellular death signals following oncogene activation or DNA damage. Cancer Metastasis Rev. 2006, 25, 137–145. [Google Scholar] [CrossRef]
- Seegers, H.C.; Hood, V.C.; Kidd, B.L.; Cruwys, S.C.; Walsh, D.A. Enhancement of Angiogenesis by Endogenous Substance P Release and Neurokinin-1 Receptors During Neurogenic Inflammation. J. Pharmacol. Exp. Ther. 2003, 306, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ma, G.; Ma, Q.; Li, W.; Liu, J.; Han, L.; Duan, W.; Xu, Q.; Liu, H.; Wang, Z.; et al. Neurotransmitter Substance P Mediates Pancreatic Cancer Perineural Invasion via NK-1R in Cancer Cells. Mol. Cancer Res. 2013, 11, 294–302. [Google Scholar] [CrossRef]
- Ma, J.; Yuan, S.; Cheng, J.; Kang, S.; Zhao, W.; Zhang, J. Substance P Promotes the Progression of Endometrial Adenocarcinoma. Int. J. Gynecol. Cancer 2016, 26, 845–850. [Google Scholar] [CrossRef]
- Wang, L.; Wang, N.; Zhang, R.; Dong, D.; Liu, R.; Zhang, L.; Ji, W.; Yu, M.; Zhang, F.; Niu, R.; et al. TGFβ regulates NK1R-Tr to affect the proliferation and apoptosis of breast cancer cells. Life Sci. 2020, 256, 117674. [Google Scholar] [CrossRef]
- Muñoz, M.; Coveñas, R. Neurokinin receptor antagonism: A patent review (2014-present). Expert Opin. Ther. Patents 2020, 30, 527–539. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Coveñas, R. The Neurokinin-1 Receptor Antagonist Aprepitant: An Intelligent Bullet against Cancer? Cancers 2020, 12, 2682. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Coveñas, R. The Neurokinin-1 Receptor Antagonist Aprepitant, a New Drug for the Treatment of Hematological Malignancies: Focus on Acute Myeloid Leukemia. J. Clin. Med. 2020, 9, 1659. [Google Scholar] [CrossRef] [PubMed]
- Hennig, I.M.; Laissue, J.A.; Horisberger, U.; Reubi, J.-C. Substance-P receptors in human primary neoplasms: Tumoral and vascular localization. Int. J. Cancer 1995, 61, 786–792. [Google Scholar] [CrossRef]
- Moles, M.G.; Esteban, F.; Ruiz-Ávila, I.; Gil Montoya, J.; Brener, S.; Bascones-Martínez, A.; Muñoz, M. A role for the substance P/NK-1 receptor complex in cell proliferation and apoptosis in oral lichen planus. Oral Dis. 2009, 15, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B.; et al. Meta-analysis of Observational Studies in Epidemiology A Proposal for Reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Riley, R.D.; Ridley, G.; Williams, K.; Altman, D.G.; Hayden, J.; de Vet, H.C. Letter to the Editor. J. Clin. Epidemiol. 2007, 60, 863–865. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Cochrane: London, UK, 2008. [Google Scholar]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; Côté, P.; Bombardier, C. Evaluation of the Quality of Prognosis Studies in Systematic Reviews. Ann. Intern. Med. 2006, 144, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing Bias in Studies of Prognostic Factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Agresti, A.; Coull, B.A. Approximate is Better than “Exact” for Interval Estimation of Binomial Proportions. Am. Stat. 1998, 52, 119–126. [Google Scholar] [CrossRef]
- Freeman, M.F.; Tukey, J.W. Transformations Related to the Angular and the Square Root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- Nyaga, V.N.; Arbyn, M.; Aerts, M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch. Public Health 2014, 72, 1–10. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Viechtbauer, W.; Cheung, M.W.-L. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods 2010, 1, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.-C.; Zhou, X.-H.; He, J. Statistical methods for dealing with publication bias in meta-analysis. Stat. Med. 2015, 34, 343–360. [Google Scholar] [CrossRef]
- Palmer, T.M.; Sterne, J.A.C. Meta-Analysis in Stata: An Updated Collection from the Stata Journal, 2nd ed.; Stata Press: College Station, TX, USA, 2016. [Google Scholar]
- Altman, D.G.; Lausen, B.; Sauerbrei, W.; Schumacher, M. Dangers of Using “Optimal” Cutpoints in the Evaluation of Prognostic Factors. J. Natl. Cancer Inst. 1994, 86, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Moles, M.G.; Mosqueda-Taylor, A.; Esteban, F.; Gil-Montoya, J.; Díaz-Franco, M.; Delgado, M.; Muñoz, M. Cell proliferation associated with actions of the substance P/NK-1 receptor complex in keratocystic odontogenic tumours. Oral Oncol. 2008, 44, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Neth, O.; Ilmer, M.; Garnier, A.; Salinas-Martín, M.V.; Asencio, J.C.D.A.; von Schweinitz, D.; Kappler, R.; Muñoz, M. Hepatoblastoma cells express truncated neurokinin-1 receptor and can be growth inhibited by aprepitant in vitro and in vivo. J. Hepatol. 2014, 60, 985–994. [Google Scholar] [CrossRef]
- Nowicki, M.; Ostalska-Nowicka, D.; Konwerska, A.; Miskowiak, B. The predicting role of substance P in the neoplastic transformation of the hypoplastic bone marrow. J. Clin. Pathol. 2006, 59, 935–941. [Google Scholar] [CrossRef]
- Muñoz, M.; Pérez, A.; Coveñas, R.; Rosso, M.; Castro, E. Antitumoural action of L-733,060 on neuroblastoma and glioma cell lines. Arch. Ital. Biol. 2004, 142, 105–112. [Google Scholar] [PubMed]
- Muñoz, M.; Rosso, M.; Aguilar, F.J.; A González-Moles, M.; Redondo, M.; Esteban, F. NK-1 receptor antagonists induce apoptosis and counteract substance P-related mitogenesis in human laryngeal cancer cell line HEp-2. Investig. New Drugs 2007, 26, 111–118. [Google Scholar] [CrossRef]
- Muñoz, M.; Rosso, M.; Coveñas, R.; Montero, I.; González-Moles, M.A.; Robles, M.J. Neurokinin-1 Receptors Located in Human Retinoblastoma Cell Lines: Antitumor Action of Its Antagonist, L-732,138. Investig. Opthalmol. Vis. Sci. 2007, 48, 2775–2781. [Google Scholar] [CrossRef]
- Muñoz, M.; Rosso, M.; Coveñas, R. Triple Negative Breast Cancer: How Neurokinin-1 Receptor Antagonists Could Be Used as a New Therapeutic Approach. Mini-Rev. Med. Chem. 2020, 20, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Rosso, M.; Coveñas, R. Neurokinin-1 Receptor Antagonists against Hepatoblastoma. Cancers 2019, 11, 1258. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Parrilla, J.; Rosso, M.; Coveñas, R. Antipruritic vs. Antitumour Action of Aprepitant: A Question of Dose. Acta Derm. Venereol. 2019, 99, 620–621. [Google Scholar] [CrossRef] [PubMed]
- Murugan, A.K.; Munirajan, A.K.; Tsuchida, N. Ras oncogenes in oral cancer: The past 20 years. Oral Oncol. 2012, 48, 383–392. [Google Scholar] [CrossRef]
- Reitsma, M.B.; Fullman, N.; Ng, M.; Salama, J.S.; Abajobir, A.; Abate, K.H.; Abbafati, C.; Abera, S.F.; Abraham, B.; Abyu, G.Y.; et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: A systematic analysis from the Global Burden of Disease Study 2015. Lancet 2017, 389, 1885–1906. [Google Scholar] [CrossRef]
- Sekizawa, S.-I.; Joad, J.P.; E Pinkerton, K.; Bonham, A.C. Distinct tachykinin NK1receptor function in primate nucleus tractus solitarius neurons is dysregulated after second-hand tobacco smoke exposure. Br. J. Pharmacol. 2011, 163, 782–791. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S. Can Meta-analysis Be Salvaged? Am. J. Epidemiol. 1994, 140, 783–787. [Google Scholar] [CrossRef]
- Ndiaye, C.; Mena, M.; Alemany, L.; Arbyn, M.; Castellsagué, X.; Laporte, L.; Bosch, F.X.; de Sanjosé, S.; Trottier, H. HPV DNA, E6/E7 mRNA, and p16INK4a detection in head and neck cancers: A systematic review and meta-analysis. Lancet Oncol. 2014, 15, 1319–1331. [Google Scholar] [CrossRef]

| Total | 16 Studies |
|---|---|
| Year of publication | 1983–2020 |
| Number of cases | |
| Total | 909 |
| Sample size, range | 5–114 |
| Biomarkers analyzed * | |
| SP | 15 studies (897 cases) |
| NK-1R | 7 studies (411 cases) |
| Affected sites | |
| Oral cavity | 4 studies (285 cases) |
| Nasal cavity | 1 study (20 cases) |
| Larynx | 2 studies (233 cases) |
| Salivary glands | 1 study (171 cases) |
| Thyroid gland | 6 studies (142 cases) |
| Head and neck mixed | 2 studies (58 cases) |
| Type of tumors * | |
| Benign | 5 studies (226 cases) |
| Pre-malignant | 3 studies (230 cases) |
| Malignant | 11 studies (453 cases) |
| Study design | |
| Retrospective cohort | 16 studies |
| Geographical region | |
| Europe | 11 studies (610 patients) |
| Asia | 3 studies (216 cases) |
| North-Central America | 2 studies (83 cases) |
| Pooled Data | Heterogeneity | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Meta-Analyses | No. of Studies * | No. of Tumors | Stat. Model | Wt | PP (95% CI) | p-Value | Phet | I2 (%) | Supplementary Materialsa |
| 1. All tumors | |||||||||
| All b | 38 | 1308 | REM | D-L | 40.52% (24.23–57.78) | ── | <0.001 | 96.89 | Figure 3 |
| Classification of tumors by malignant behavior c | 0.004 d | Figure 3 | |||||||
| Benign | 9 | 289 | REM | D-L | 11.86% (1.23–28.31) | <0.001 | 88.2 | ||
| Pre-malignant | 6 | 460 | REM | D-L | 69.25% (35.34–94.52) | <0.001 | 98.2 | ||
| Malignant | 23 | 559 | REM | D-L | 45.04% (22.54, 68.48) | <0.001 | 95.8 | ||
| Classification of tumors by malignant behavior —combining the pre-malignant and malignant groups- c | 0.002 d | Figure S1, p. 6 | |||||||
| Benign | 9 | 289 | REM | D-L | 11.86% (1.23–28.31) | <0.001 | 88.2 | ||
| Non-Benign | 29 | 1019 | REM | D-L | 50.93% (32.13–69.61) | <0.001 | 96.6 | ||
| Paired analysis by malignant behavior | 0.003 | Figure S2, p. 7 | |||||||
| Benign | 9 | 289 | REM | D-L | 11.86% (1.23–28.31) | <0.001 | 88.2 | ||
| Pre-malignant | 6 | 460 | REM | D-L | 69.25% (35.34–94.52) | <0.001 | 98.2 | ||
| Paired analysis by malignant behavior | 0.02 | Figure S3, p. 8 | |||||||
| Benign | 9 | 289 | REM | D-L | 11.86% (1.23–28.31) | <0.001 | 88.2 | ||
| Malignant | 23 | 559 | REM | D-L | 45.04% (22.54, 68.48) | <0.001 | 95.8 | ||
| Paired analysis by malignant behavior | 0.24 | Figure S4, p. 9 | |||||||
| Pre-malignant | 6 | 460 | REM | D-L | 69.25% (35.34–94.52) | <0.001 | 98.2 | ||
| Malignant | 23 | 559 | REM | D-L | 45.04% (22.54, 68.48) | <0.001 | 95.8 | ||
| 2. Benign tumors | |||||||||
| Benign tumors by geographical area c | <0.001 d | Figure S5, p. 10 | |||||||
| Asian | 4 | 112 | REM | D-L | 0.00% (0.00–0.00) | 0.74 | 0.0 | ||
| Non-Asian | 5 | 177 | REM | D-L | 26.43% (15.41–39.01) | 0.04 | 60.96 | ||
| Benign tumors by anatomical site c | <0.001 d | Figure S6, p. 11 | |||||||
| Larynx | 1 | 11 | ── | ── | 36.36% (15.17–64.62) | ── | ── | ||
| Nasal cavity | 1 | 20 | ── | ── | 25.00% (11.19–46.87) | ── | ── | ||
| Oral cavity | 2 | 128 | REM | D-L | 21.88% (15.04–29.56) | ── | ── | ||
| Salivary gland | 4 | 112 | REM | D-L | 0.00% (0.00–0.00) | 0.76 | 0.0 | ||
| Head and neck mixed | 1 | 18 | ── | ── | 38.89% (20.31–61.38) | ── | ── | ||
| Benign tumors by histological type c | <0.001 d | Figure S7, p. 12 | |||||||
| Glandular | 4 | 112 | REM | D-L | 0.00% (0.00–0.00) | 0.76 | 0.0 | ||
| Squamous | 4 | 159 | REM | D-L | 24.17% (12.56–37.86) | 0.04 | 64.01 | ||
| Nervous | 1 | 18 | ── | ── | 38.89% (20.31–61.38) | ── | ── | ||
| Benign tumors by biomarker c | 0.85 d | Figure S8, p. 13 | |||||||
| SP | 8 | 226 | REM | D-L | 11.77% (0.11–32.64) | <0.001 | 89.64 | ||
| NK-1R | 1 | 63 | ── | ── | 12.70% (6.58–23.11) | ── | ── | ||
| 3. Pre-malignant tissues | |||||||||
| Pre-malignant tissues by geographical area c | ── | ── | |||||||
| Asian | 0 | 0 | ── | ── | ── | ── | ── | ||
| Non-Asian | 6 | 460 | REM | D-L | 69.25% (35.34–94.52) | <0.001 | 98.2 | ||
| Pre-malignant tissues by anatomical site c | 0.02 d | Figure S9, p. 14 | |||||||
| Larynx | 2 | 194 | REM | D-L | 94.42% (90.63–97.34) | ── | ── | ||
| Oral cavity | 4 | 266 | REM | D-L | 52.24% (13.57–89.40) | 0.001 | 97.94 | ||
| Pre-malignant tissues by histological type c | ── | ── | |||||||
| Squamous | 6 | 460 | REM | D-L | 69.25% (35.34–94.52) | <0.001 | 98.2 | ||
| Other | 0 | 0 | ── | ── | ── | ── | ── | ||
| Pre-malignant tissues by clinical type c | <0.001 d | Figure S10, p. 15 | |||||||
| OLP | 2 | 100 | REM | D-L | 61.30% (51.45–70.72) | ── | ── | ||
| ANTE-OSCC | 2 | 166 | REM | D-L | 43.27% (35.78–50.93) | ── | ── | ||
| ANTE-LSCC | 2 | 194 | REM | D-L | 94.42% (90.63–97.34) | ── | ── | ||
| Pre-malignant tissues by biomarker c | 0.13 d | Figure S11, p. 16 | |||||||
| SP | 3 | 230 | REM | D-L | 89.60% (66.10–100.00) | <0.001 | 94.77 | ||
| NK-1R | 3 | 230 | REM | D-L | 43.92% (1.33–93.97) | <0.001 | 98.75 | ||
| 4. Malignant tumors | |||||||||
| Malignant tumors by geographical area c | 0.007 d | Figure S12, p. 17 | |||||||
| Asian | 8 | 104 | REM | D-L | 12.04% (0.00–35.87) | <0.001 | 83.55 | ||
| Non-Asian | 15 | 455 | REM | D-L | 65.03% (34.63–90.69) | <0.001 | 96.81 | ||
| Malignant tumors by anatomical site c | <0.001 d | Figure S13, p. 18 | |||||||
| Larynx | 3 | 125 | REM | D-L | 67.80% (8.94–100.00) | <0.001 | 90.58 | ||
| Oral cavity | 2 | 173 | REM | D-L | 64.14% (56.80–71.17) | ── | ── | ||
| Salivary gland | 6 | 59 | REM | D-L | 3.84% (0.00–12.24) | 0.55 | 0.0 | ||
| Thyroid gland | 11 | 162 | REM | D-L | 63.25% (22.83–96.04) | <0.001 | 95.15 | ||
| Head and neck mixed | 1 | 4 | ── | ── | 62.50% (47.03–75.78) | ── | ── | ||
| Malignant tumors by histological type c | 0.16 d | Figure S14, p. 19 | |||||||
| Glandular | 17 | 221 | REM | D-L | 37.31% (12.70–65.25) | <0.001 | 92.71 | ||
| Squamous | 4 | 327 | REM | D-L | 74.83% (47.01–94.77) | <0.001 | 96.27 | ||
| Neuroendocrine | 2 | 11 | REM | D-L | 51.42% (19.04–83.29) | ── | ── | ||
| Malignant tumors by biomarker c | 0.02 d | Figure S15, p. 20 | |||||||
| SP | 18 | 441 | REM | D-L | 33.60% (9.13–62.90) | <0.001 | 96.57 | ||
| NK-1R | 5 | 118 | REM | D-L | 83.67% (51.40–100.00) | <0.001 | 84.57 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Moles, M.Á.; Ramos-García, P.; Esteban, F. Significance of the Overexpression of Substance P and Its Receptor NK-1R in Head and Neck Carcinogenesis: A Systematic Review and Meta-Analysis. Cancers 2021, 13, 1349. https://doi.org/10.3390/cancers13061349
González-Moles MÁ, Ramos-García P, Esteban F. Significance of the Overexpression of Substance P and Its Receptor NK-1R in Head and Neck Carcinogenesis: A Systematic Review and Meta-Analysis. Cancers. 2021; 13(6):1349. https://doi.org/10.3390/cancers13061349
Chicago/Turabian StyleGonzález-Moles, Miguel Ángel, Pablo Ramos-García, and Francisco Esteban. 2021. "Significance of the Overexpression of Substance P and Its Receptor NK-1R in Head and Neck Carcinogenesis: A Systematic Review and Meta-Analysis" Cancers 13, no. 6: 1349. https://doi.org/10.3390/cancers13061349
APA StyleGonzález-Moles, M. Á., Ramos-García, P., & Esteban, F. (2021). Significance of the Overexpression of Substance P and Its Receptor NK-1R in Head and Neck Carcinogenesis: A Systematic Review and Meta-Analysis. Cancers, 13(6), 1349. https://doi.org/10.3390/cancers13061349








