Neuroendocrine-Related Circulating Transcripts in Small-Cell Lung Cancers: Detection Methods and Future Perspectives
Abstract
Simple Summary
Abstract
1. Introduction
2. Circulating SSTRs Transcripts
3. Circulating nELAVs Transcripts
4. Circulating SYP, CHGA, and DLL3 Transcripts
5. Circulating ProGRP Transcript
6. Circulating SCG3 Transcript: State of the Art
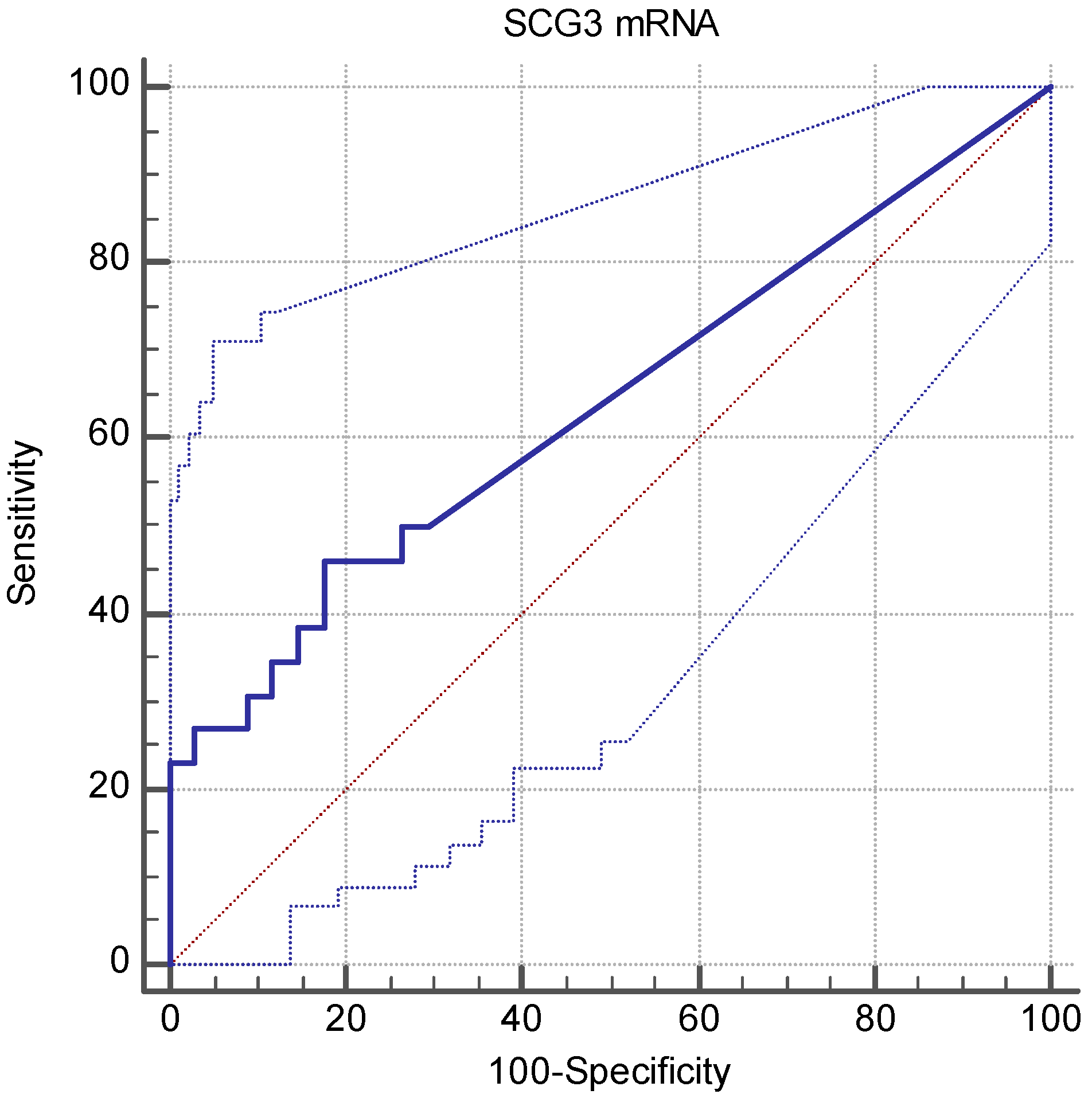
7. SCG3 Transcript in PB of SCLC Patients: New Unpublished Findings
7.1. Materials and Methods: Patients, Samples, RT-qPCR, and Statistical Methods
7.2. Expression of SCG3 Markers in Healthy Volunteers and SCLC-Affected Patients: Results and Discussion
8. General Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rossi, A.; Tay, R.; Chiramel, J.; Prelaj, A.; Califano, R. Current and future therapeutic approaches for the treatment of small cell lung cancer. Expert Rev. Anticancer Ther. 2018, 18, 473–486. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances since the 2004 Classification. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef]
- Blackhall, F.; Frese, K.K.; Simpson, K.; Kilgour, E.; Brady, G.; Dive, C. Will liquid biopsies improve outcomes for patients with small-cell lung cancer? Lancet Oncol. 2018, 19, e470–e481. [Google Scholar] [CrossRef]
- Saltos, A.; Shafique, M.; Chiappori, A. Update on the Biology, Management, and Treatment of Small Cell Lung Cancer (SCLC). Front. Oncol. 2020, 10, 1074. [Google Scholar] [CrossRef]
- Rudin, C.M.; Poirier, J.T.; Byers, L.A.; Dive, C.; Dowlati, A.; George, J.; Heymach, J.V.; Johnson, J.E.; Lehman, J.M.; MacPherson, D.; et al. Molecular subtypes of small cell lung cancer: A synthesis of human and mouse model data. Nat. Rev. Cancer 2019, 19, 289–297. [Google Scholar] [CrossRef]
- Alberter, B.; Klein, C.A.; Polzer, B. Single-cell analysis of CTCs with diagnostic precision: Opportunities and challenges for personalized medicine. Expert Rev. Mol. Diagn. 2016, 16, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Normanno, N.; Rossi, A.; Morabito, A.; Signoriello, S.; Bevilacqua, S.; Di Maio, M.; Costanzo, R.; De Luca, A.; Montanino, A.; Gridelli, C.; et al. Prognostic value of circulating tumor cells’ reduction in patients with extensive small-cell lung cancer. Lung Cancer 2014, 85, 314–319. [Google Scholar] [CrossRef]
- Killock, D. Lung cancer: Liquid biopsy of SCLC chemosensitivity. Nat. Rev. Clin. Oncol. 2017, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Filosso, P.L.; Kidd, M.; Roffinella, M.; Lewczuk, A.; Chung, K.M.; Kolasinska-Cwikla, A.; Cwikla, J.; Lowczak, A.; Doboszynska, A.; Malczewska, A.; et al. The utility of blood neuroendocrine gene transcript measurement in the diagnosis of bronchopulmonary neuroendocrine tumours and as a tool to evaluate surgical resection and disease progression. Eur. J. Cardiothorac. Surg. 2018, 53, 631–639. [Google Scholar] [CrossRef]
- Fujita, T.; Yamaji, Y.; Sato, M.; Murao, K.; Takahara, J. Gene expression of somatostatin receptor subtypes, SSTR1 and SSTR2, in human lung cancer cell lines. Life Sci. 1994, 55, 1797–1806. [Google Scholar] [CrossRef]
- Reubi, J.C.; Waser, B.; Sheppard, M.; Macaulay, V. Somatostatin receptors are present in small-cell but not in non-small-cell primary lung carcinomas: Relationship to EGF-receptors. Int. J. Cancer 1990, 45, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Kwekkeboom, D.J.; Krenning, E.P.; Bakker, W.H.; Oei, H.Y.; Splinter, T.A.; Kho, G.S.; Lamberts, S.W. Radioiodinated somatostatin analog scintigraphy in small-cell lung cancer. J. Nucl. Med. 1991, 32, 1845–1848. [Google Scholar]
- Lapa, C.; Hanscheid, H.; Wild, V.; Pelzer, T.; Schirbel, A.; Werner, R.A.; Droll, S.; Herrmann, K.; Buck, A.K.; Luckerath, K. Somatostatin receptor expression in small cell lung cancer as a prognostic marker and a target for peptide receptor radionuclide therapy. Oncotarget 2016, 7, 20033–20040. [Google Scholar] [CrossRef]
- Reisinger, I.; Bohuslavitzki, K.H.; Brenner, W.; Braune, S.; Dittrich, I.; Geide, A.; Kettner, B.; Otto, H.J.; Schmidt, S.; Munz, D.L. Somatostatin receptor scintigraphy in small-cell lung cancer: Results of a multicenter study. J. Nucl. Med. 1998, 39, 224–227. [Google Scholar] [PubMed]
- Tsuta, K.; Wistuba, I.I.; Moran, C.A. Differential expression of somatostatin receptors 1-5 in neuroendocrine carcinoma of the lung. Pathol. Res. Pract. 2012, 208, 470–474. [Google Scholar] [CrossRef]
- Filice, A.; Fraternali, A.; Frasoldati, A.; Asti, M.; Grassi, E.; Massi, L.; Sollini, M.; Froio, A.; Erba, P.A.; Versari, A. Radiolabeled somatostatin analogues therapy in advanced neuroendocrine tumors: A single centre experience. J. Oncol. 2012, 2012, 320198. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Liu, S.V.; Subramaniam, D.S.; Torres, T.; Loda, M.; Esposito, G.; Giaccone, G. Phase I study of the (177)Lu-DOTA(0)-Tyr(3)-Octreotate (lutathera) in combination with nivolumab in patients with neuroendocrine tumors of the lung. J. Immunother. Cancer 2020, 8, e000980. [Google Scholar] [CrossRef]
- Sollini, M.; Farioli, D.; Froio, A.; Chella, A.; Asti, M.; Boni, R.; Grassi, E.; Roncali, M.; Versari, A.; Erba, P.A. Brief report on the use of radiolabeled somatostatin analogs for the diagnosis and treatment of metastatic small-cell lung cancer patients. J. Thorac. Oncol. 2013, 8, 1095–1101. [Google Scholar] [CrossRef]
- Udyavar, A.R.; Wooten, D.J.; Hoeksema, M.; Bansal, M.; Califano, A.; Estrada, L.; Schnell, S.; Irish, J.M.; Massion, P.P.; Quaranta, V. Novel Hybrid Phenotype Revealed in Small Cell Lung Cancer by a Transcription Factor Network Model That Can Explain Tumor Heterogeneity. Cancer Res. 2017, 77, 1063–1074. [Google Scholar] [CrossRef] [PubMed]
- Papotti, M.; Croce, S.; Bello, M.; Bongiovanni, M.; Allia, E.; Schindler, M.; Bussolati, G. Expression of somatostatin receptor types 2, 3 and 5 in biopsies and surgical specimens of human lung tumours. Correlation with preoperative octreotide scintigraphy. Virchows Arch. 2001, 439, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Righi, L.; Volante, M.; Tavaglione, V.; Bille, A.; Daniele, L.; Angusti, T.; Inzani, F.; Pelosi, G.; Rindi, G.; Papotti, M. Somatostatin receptor tissue distribution in lung neuroendocrine tumours: A clinicopathologic and immunohistochemical study of 218 ‘clinically aggressive’ cases. Ann. Oncol. 2010, 21, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Muscarella, L.A.; D’Alessandro, V.; la Torre, A.; Copetti, M.; De Cata, A.; Parrella, P.; Sperandeo, M.; Pellegrini, F.; Frusciante, V.; Maiello, E.; et al. Gene expression of somatostatin receptor subtypes SSTR2a, SSTR3 and SSTR5 in peripheral blood of neuroendocrine lung cancer affected patients. Cell Oncol. (Dordr.) 2011, 34, 435–441. [Google Scholar] [CrossRef]
- Stathopoulou, A.; Vlachonikolis, I.; Mavroudis, D.; Perraki, M.; Kouroussis, C.; Apostolaki, S.; Malamos, N.; Kakolyris, S.; Kotsakis, A.; Xenidis, N.; et al. Molecular detection of cytokeratin-19-positive cells in the peripheral blood of patients with operable breast cancer: Evaluation of their prognostic significance. J. Clin. Oncol. 2002, 20, 3404–3412. [Google Scholar] [CrossRef]
- Pantel, K.; Alix-Panabieres, C. Liquid biopsy and minimal residual disease—Latest advances and implications for cure. Nat. Rev. Clin. Oncol. 2019, 16, 409–424. [Google Scholar] [CrossRef]
- Kong, G.; Hicks, R.J. Peptide Receptor Radiotherapy: Current Approaches and Future Directions. Curr. Treat. Options Oncol. 2019, 20, 77. [Google Scholar] [CrossRef] [PubMed]
- Strosberg, J.R.; Wolin, E.M.; Chasen, B.; Kulke, M.H.; Bushnell, D.L.; Caplin, M.E.; Baum, R.P.; Kunz, P.L.; Hobday, T.J.; Hendifar, A.E.; et al. NETTER-1 phase III: Progression-free survival, radiographic response, and preliminary overall survival results in patients with midgut neuroendocrine tumors treated with 177-Lu-dotatate. Am. Soc. Clin. Oncol. 2016, 34, 194. [Google Scholar] [CrossRef]
- Ready, N.; Farago, A.F.; de Braud, F.; Atmaca, A.; Hellmann, M.D.; Schneider, J.G.; Spigel, D.R.; Moreno, V.; Chau, I.; Hann, C.L.; et al. Third-Line Nivolumab Monotherapy in Recurrent SCLC: CheckMate 032. J. Thorac. Oncol. 2019, 14, 237–244. [Google Scholar] [CrossRef]
- Graus, F.; Dalmau, J. Paraneoplastic neurological syndromes in the era of immune-checkpoint inhibitors. Nat. Rev. Clin. Oncol. 2019, 16, 535–548. [Google Scholar] [CrossRef] [PubMed]
- Spiro, M.K.G.; Colice, G.L. American College of Chest Physicians Initial evaluation of the patient with lung cancer: Symptoms, signs, laboratory tests, and paraneoplastic syndromes: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest 2007, 132, 149S–160S. [Google Scholar] [CrossRef] [PubMed]
- Monstad, S.E.; Knudsen, A.; Salvesen, H.B.; Aarseth, J.H.; Vedeler, C.A. Onconeural antibodies in sera from patients with various types of tumours. Cancer Immunol. Immunother. 2009, 58, 1795–1800. [Google Scholar] [CrossRef]
- List, M.; Jamous, F.; Gupta, A.; Huntington, M. Anti-Hu Positive Antibodies and Small Cell Carcinoma: A Single Center Review. SD Med. 2015, 68, 253–255. [Google Scholar]
- Manley, G.T.; Smitt, P.S.; Dalmau, J.; Posner, J.B. Hu antigens: Reactivity with Hu antibodies, tumor expression, and major immunogenic sites. Ann. Neurol. 1995, 38, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Marusich, M.F.; Furneaux, H.M.; Henion, P.D.; Weston, J.A. Hu neuronal proteins are expressed in proliferating neurogenic cells. J. Neurobiol. 1994, 25, 143–155. [Google Scholar] [CrossRef]
- D’Alessandro, V.; Muscarella, L.A.; Copetti, M.; Zelante, L.; Carella, M.; Vendemiale, G. Molecular detection of neuron-specific ELAV-like-positive cells in the peripheral blood of patients with small-cell lung cancer. Cell Oncol. 2008, 30, 291–297. [Google Scholar] [PubMed]
- Gill, S.; Murray, N.; Dalmau, J.; Thiessen, B. Paraneoplastic sensory neuronopathy and spontaneous regression of small cell lung cancer. Can. J. Neurol. Sci. 2003, 30, 269–271. [Google Scholar] [CrossRef]
- Hirano, S.; Nakajima, Y.; Morino, E.; Fujikura, Y.; Mochizuki, M.; Takeda, Y.; Sugiyama, H.; Kobayashi, N.; Tanaka, K.; Kudo, K. A case of spontaneous regression of small cell lung cancer with progression of paraneoplastic sensory neuropathy. Lung Cancer 2007, 58, 291–295. [Google Scholar] [CrossRef]
- Mawhinney, E.; Gray, O.M.; McVerry, F.; McDonnell, G.V. Paraneoplastic sensorimotor neuropathy associated with regression of small cell lung carcinoma. BMJ Case Rep. 2010, 2010. [Google Scholar] [CrossRef]
- Hardy-Werbin, M.; Arpi, O.; Taus, A.; Rocha, P.; Joseph-Pietras, D.; Nolan, L.; Danson, S.; Griffiths, R.; Lopez-Botet, M.; Rovira, A.; et al. Assessment of neuronal autoantibodies in patients with small cell lung cancer treated with chemotherapy with or without ipilimumab. Oncoimmunology 2017, 7, e1395125. [Google Scholar] [CrossRef]
- Manson, G.; Maria, A.T.J.; Poizeau, F.; Danlos, F.X.; Kostine, M.; Brosseau, S.; Aspeslagh, S.; Du Rusquec, P.; Roger, M.; Pallix-Guyot, M.; et al. Worsening and newly diagnosed paraneoplastic syndromes following anti-PD-1 or anti-PD-L1 immunotherapies, a descriptive study. J. Immunother. Cancer 2019, 7, 337. [Google Scholar] [CrossRef]
- Guinee, D.G., Jr.; Fishback, N.F.; Koss, M.N.; Abbondanzo, S.L.; Travis, W.D. The spectrum of immunohistochemical staining of small-cell lung carcinoma in specimens from transbronchial and open-lung biopsies. Am. J. Clin. Pathol. 1994, 102, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Saunders, L.R.; Bankovich, A.J.; Anderson, W.C.; Aujay, M.A.; Bheddah, S.; Black, K.; Desai, R.; Escarpe, P.A.; Hampl, J.; Laysang, A.; et al. A DLL3-targeted antibody-drug conjugate eradicates high-grade pulmonary neuroendocrine tumor-initiating cells in vivo. Sci. Transl. Med. 2015, 7, 302ra136. [Google Scholar] [CrossRef]
- Furuta, M.; Kikuchi, H.; Shoji, T.; Takashima, Y.; Kikuchi, E.; Kikuchi, J.; Kinoshita, I.; Dosaka-Akita, H.; Sakakibara-Konishi, J. DLL3 regulates the migration and invasion of small cell lung cancer by modulating Snail. Cancer Sci. 2019, 110, 1599–1608. [Google Scholar] [CrossRef] [PubMed]
- Augustyn, A.; Borromeo, M.; Wang, T.; Fujimoto, J.; Shao, C.; Dospoy, P.D.; Lee, V.; Tan, C.; Sullivan, J.P.; Larsen, J.E.; et al. ASCL1 is a lineage oncogene providing therapeutic targets for high-grade neuroendocrine lung cancers. Proc. Natl. Acad. Sci. USA 2014, 111, 14788–14793. [Google Scholar] [CrossRef]
- Allison Stewart, C.M.G.; Xi, Y.; Sivajothi, S.; Sivakamasundari, V.; Fujimoto, J.; Bolisetty, M.; Hartsfield, P.M.; Balasubramaniyan, V.; Chalishazar, M.D.; Moran, C.; et al. Single-cell analyses reveal increased intratumoral heterogeneity after the onset of therapy resistance in small-cell lung cancer. Nat. Cancer 2020, 1, 423–436. [Google Scholar] [CrossRef]
- Zhang, W.; Girard, L.; Zhang, Y.A.; Haruki, T.; Papari-Zareei, M.; Stastny, V.; Ghayee, H.K.; Pacak, K.; Oliver, T.G.; Minna, J.D.; et al. Small cell lung cancer tumors and preclinical models display heterogeneity of neuroendocrine phenotypes. Transl. Lung Cancer Res. 2018, 7, 32–49. [Google Scholar] [CrossRef]
- Geffers, I.; Serth, K.; Chapman, G.; Jaekel, R.; Schuster-Gossler, K.; Cordes, R.; Sparrow, D.B.; Kremmer, E.; Dunwoodie, S.L.; Klein, T.; et al. Divergent functions and distinct localization of the Notch ligands DLL1 and DLL3 in vivo. J. Cell Biol. 2007, 178, 465–476. [Google Scholar] [CrossRef]
- Sabari, J.K.; Lok, B.H.; Laird, J.H.; Poirier, J.T.; Rudin, C.M. Unravelling the biology of SCLC: Implications for therapy. Nat. Rev. Clin. Oncol. 2017, 14, 549–561. [Google Scholar] [CrossRef]
- Obermayr, E.; Agreiter, C.; Schuster, E.; Fabikan, H.; Weinlinger, C.; Baluchova, K.; Hamilton, G.; Hochmair, M.; Zeillinger, R. Molecular Characterization of Circulating Tumor Cells Enriched by A Microfluidic Platform in Patients with Small-Cell Lung Cancer. Cells 2019, 8, 880. [Google Scholar] [CrossRef]
- Pal, S.K.; He, M.; Chen, L.; Yang, L.; Pillai, R.; Twardowski, P.; Hsu, J.; Kortylewski, M.; Jones, J.O. Synaptophysin expression on circulating tumor cells in patients with castration resistant prostate cancer undergoing treatment with abiraterone acetate or enzalutamide. Urol. Oncol. 2018, 36, 162.e161–162.e166. [Google Scholar] [CrossRef] [PubMed]
- Cuttitta, F.; Carney, D.N.; Mulshine, J.; Moody, T.W.; Fedorko, J.; Fischler, A.; Minna, J.D. Bombesin-like peptides can function as autocrine growth factors in human small-cell lung cancer. Nature 1985, 316, 823–826. [Google Scholar] [CrossRef] [PubMed]
- Kane, M.A.B.P. Biology of Lung Cancer. Lung Biology in Health and Disease; Marcel Dekker: New York, NY, USA, 1998; p. 122. [Google Scholar]
- Iida, Y.; Masuda, S.; Nakanishi, Y.; Shimizu, T.; Nishimaki, H.; Takahashi, M.; Hikichi, M.; Maruoka, S.; Gon, Y.; Takahashi, N.; et al. Clinicopathological characteristics of thyroid transcription factor 1-negative small cell lung cancers. Hum. Pathol. 2018, 79, 127–134. [Google Scholar] [CrossRef]
- Saito, T.; Kobayashi, M.; Harada, R.; Uemura, Y.; Taguchi, H. Sensitive detection of small cell lung carcinoma cells by reverse transcriptase-polymerase chain reaction for prepro-gastrin-releasing peptide mRNA. Cancer 2003, 97, 2504–2511. [Google Scholar] [CrossRef]
- Huang, Z.; Xu, D.; Zhang, F.; Ying, Y.; Song, L. Pro-gastrin-releasing peptide and neuron-specific enolase: Useful predictors of response to chemotherapy and survival in patients with small cell lung cancer. Clin. Transl. Oncol. 2016, 18, 1019–1025. [Google Scholar] [CrossRef]
- Li, M.; Han, D.; Wang, W.; Zhang, Y.; Li, D.; Dai, C.; Qian, L.; Lin, W. Decline in serum progastrin-releasing peptide predicts the response of patients with small cell lung cancer to chemotherapy. Oncol. Lett. 2020, 20, 301. [Google Scholar] [CrossRef] [PubMed]
- Chong, J.A.; Tapia-Ramirez, J.; Kim, S.; Toledo-Aral, J.J.; Zheng, Y.; Boutros, M.C.; Altshuller, Y.M.; Frohman, M.A.; Kraner, S.D.; Mandel, G. REST: A mammalian silencer protein that restricts sodium channel gene expression to neurons. Cell 1995, 80, 949–957. [Google Scholar] [CrossRef]
- Schoenherr, C.J.; Anderson, D.J. The neuron-restrictive silencer factor (NRSF): A coordinate repressor of multiple neuron-specific genes. Science 1995, 267, 1360–1363. [Google Scholar] [CrossRef] [PubMed]
- Coulson, J.M. Transcriptional regulation: Cancer, neurons and the REST. Curr. Biol. 2005, 15, R665–R668. [Google Scholar] [CrossRef]
- Majumder, S. REST in good times and bad: Roles in tumor suppressor and oncogenic activities. Cell Cycle 2006, 5, 1929–1935. [Google Scholar] [CrossRef] [PubMed]
- Kreisler, A.; Strissel, P.L.; Strick, R.; Neumann, S.B.; Schumacher, U.; Becker, C.M. Regulation of the NRSF/REST gene by methylation and CREB affects the cellular phenotype of small-cell lung cancer. Oncogene 2010, 29, 5828–5838. [Google Scholar] [CrossRef]
- Coulson, J.M.; Ocejo-Garcia, M.; Woll, P.J. Neuroendocrine phenotype of small cell lung cancer. Methods Mol. Med. 2003, 74, 61–73. [Google Scholar]
- Coulson, J.M.; Edgson, J.L.; Woll, P.J.; Quinn, J.P. A splice variant of the neuron-restrictive silencer factor repressor is expressed in small cell lung cancer: A potential role in derepression of neuroendocrine genes and a useful clinical marker. Cancer Res. 2000, 60, 1840–1844. [Google Scholar]
- Gurrola-Diaz, C.; Lacroix, J.; Dihlmann, S.; Becker, C.M.; von Knebel Doeberitz, M. Reduced expression of the neuron restrictive silencer factor permits transcription of glycine receptor alpha1 subunit in small-cell lung cancer cells. Oncogene 2003, 22, 5636–5645. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Neumann, S.B.; Seitz, R.; Gorzella, A.; Heister, A.; Doeberitz, M.; Becker, C.M. Relaxation of glycine receptor and onconeural gene transcription control in NRSF deficient small cell lung cancer cell lines. Brain Res. Mol. Brain Res. 2004, 120, 173–181. [Google Scholar] [CrossRef]
- Spencer, E.M.; Chandler, K.E.; Haddley, K.; Howard, M.R.; Hughes, D.; Belyaev, N.D.; Coulson, J.M.; Stewart, J.P.; Buckley, N.J.; Kipar, A.; et al. Regulation and role of REST and REST4 variants in modulation of gene expression in in vivo and in vitro in epilepsy models. Neurobiol. Dis. 2006, 24, 41–52. [Google Scholar] [CrossRef]
- Watanabe, H.; Mizutani, T.; Haraguchi, T.; Yamamichi, N.; Minoguchi, S.; Yamamichi-Nishina, M.; Mori, N.; Kameda, T.; Sugiyama, T.; Iba, H. SWI/SNF complex is essential for NRSF-mediated suppression of neuronal genes in human nonsmall cell lung carcinoma cell lines. Oncogene 2006, 25, 470–479. [Google Scholar] [CrossRef][Green Version]
- Moss, A.C.; Jacobson, G.M.; Walker, L.E.; Blake, N.W.; Marshall, E.; Coulson, J.M. SCG3 transcript in peripheral blood is a prognostic biomarker for REST-deficient small cell lung cancer. Clin. Cancer Res. 2009, 15, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Bithell, A. REST: Transcriptional and epigenetic regulator. Epigenomics 2011, 3, 47–58. [Google Scholar] [CrossRef]
- Ooi, L.; Wood, I.C. Chromatin crosstalk in development and disease: Lessons from REST. Nat. Rev. Genet. 2007, 8, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Ireland, A.S.; Micinski, A.M.; Kastner, D.W.; Guo, B.; Wait, S.J.; Spainhower, K.B.; Conley, C.C.; Chen, O.S.; Guthrie, M.R.; Soltero, D.; et al. MYC Drives Temporal Evolution of Small Cell Lung Cancer Subtypes by Reprogramming Neuroendocrine Fate. Cancer Cell 2020, 38, 60–78.e12. [Google Scholar] [CrossRef] [PubMed]
- Pearsall, S.M.; Humphrey, S.; Revill, M.; Morgan, D.; Frese, K.K.; Galvin, M.; Kerr, A.; Carter, M.; Priest, L.; Blackhall, F.; et al. The Rare YAP1 Subtype of SCLC Revisited in a Biobank of 39 Circulating Tumor Cell Patient Derived Explant Models: A Brief Report. J. Thorac. Oncol. 2020, 15, 1836–1843. [Google Scholar] [CrossRef]
- Nicholson, S.A.; Beasley, M.B.; Brambilla, E.; Hasleton, P.S.; Colby, T.V.; Sheppard, M.N.; Falk, R.; Travis, W.D. Small cell lung carcinoma (SCLC): A clinicopathologic study of 100 cases with surgical specimens. Am. J. Surg. Pathol. 2002, 26, 1184–1197. [Google Scholar] [CrossRef] [PubMed]
| Clinical Characteristics | Value |
|---|---|
| Number of Patients | 26 |
| Age (years) | |
| Median (range) | 70 (42–82) |
| Sex, n (%) | |
| Male | 26 (100) |
| Female | 0 (0) |
| Smoking status, n (%) | |
| Former and current smoker | 25 (96) |
| Never smoker | 1 (4) |
| Pack/year (median ± SD) | 50 ± 21 |
| Disease stage, n (%) | |
| LD | 7 (27) |
| ED | 19 (73) |
| Median (range) survival (months) | 7 (1–28) |
| Gene Symbol | Molecular Assay | Cohort Size (N) | % Positive Patients | Results | Refs |
|---|---|---|---|---|---|
| SSTR2a | RT-qPCR | 14 | 93% (13/14) | The detection in PB was associated to SCLC | [22] |
| The positivity in PB was correlated to OctreoScan captation | [22] | ||||
| SSTR5 | RT-qPCR | 14 | 8/14 (57%) | The detection in PB was associated to SCLC | [22] |
| The positivity in PB was correlated to OctreoScan captation | [22] | ||||
| HuB (ELAVL2) | RT-qPCR | 25 | 13/25 (52%) | The detection in PB was associated to SCLC | [34] |
| The HuB/HuD positivity in PB was observed in LD SCLC stage | [34] | ||||
| HuC (ELAVL3) | RT-qPCR | 25 | 4/25 (16%) | The detection in PB was associated to SCLC | [34] |
| HuD (ELAVL4) | RT-qPCR | 25 | 6/25 (24%) | The detection in PB was associated to SCLC | [34] |
| The HuD/HuB positivity in PB was observed in LD SCLC stage | [34] | ||||
| SYP | microfluidic Parsortix/RT-qPCR | 51 | 11/51 (21.6%) | The detection in PB was associated to SCLC | [48] |
| The SYP/CHGA positivity was associated to shorter OS | [48] | ||||
| CHGA | microfluidic Parsortix/RT-qPCR | 51 | 6/51 (12%) | The detection in PB was associated to SCLC | [48] |
| The CHGA/SYP positivity associated to shorter OS | [48] | ||||
| DLL3 | microfluidic Parsortix/RT-qPCR | 51 | 4/51 (7.8%) | The detection in PB was associated to SCLC | [48] |
| The positivity in PB was associated to shorter OS | [48] | ||||
| ProGRP | RT-qPCR | 32 | 16/32 (50%) | The positivity in PB was associated to SCLC condition | [53] |
| RT-qPCR | 122 | nr | The detection in PB was associated to SCLC | [54] | |
| The positivity in PB was correlated to ProGRP serum positivity | [54] | ||||
| The positivity in PB was correlated to tumor size, disease stage and distant metastasis | [54] | ||||
| SCG3 | RT-qPCR | 67 | 24/67 (36%) | The detection in PB was associated to SCLC | [67] |
| The positivity in PB was associated to poor survival and worse treatment response. | [67] | ||||
| SCG3 | RT-qPCR | 26 | 12/26 (46%) | The detection in PB was associated to SCLC | present work |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muscarella, L.A.; Mazza, T.; Fabrizio, F.P.; Sparaneo, A.; D’Alessandro, V.; Tancredi, A.; Trombetta, D.; Centra, F.; Muscarella, S.P.; Di Micco, C.M.; et al. Neuroendocrine-Related Circulating Transcripts in Small-Cell Lung Cancers: Detection Methods and Future Perspectives. Cancers 2021, 13, 1339. https://doi.org/10.3390/cancers13061339
Muscarella LA, Mazza T, Fabrizio FP, Sparaneo A, D’Alessandro V, Tancredi A, Trombetta D, Centra F, Muscarella SP, Di Micco CM, et al. Neuroendocrine-Related Circulating Transcripts in Small-Cell Lung Cancers: Detection Methods and Future Perspectives. Cancers. 2021; 13(6):1339. https://doi.org/10.3390/cancers13061339
Chicago/Turabian StyleMuscarella, Lucia Anna, Tommaso Mazza, Federico Pio Fabrizio, Angelo Sparaneo, Vito D’Alessandro, Antonio Tancredi, Domenico Trombetta, Flavia Centra, Silvana Pia Muscarella, Concetta Martina Di Micco, and et al. 2021. "Neuroendocrine-Related Circulating Transcripts in Small-Cell Lung Cancers: Detection Methods and Future Perspectives" Cancers 13, no. 6: 1339. https://doi.org/10.3390/cancers13061339
APA StyleMuscarella, L. A., Mazza, T., Fabrizio, F. P., Sparaneo, A., D’Alessandro, V., Tancredi, A., Trombetta, D., Centra, F., Muscarella, S. P., Di Micco, C. M., & Rossi, A. (2021). Neuroendocrine-Related Circulating Transcripts in Small-Cell Lung Cancers: Detection Methods and Future Perspectives. Cancers, 13(6), 1339. https://doi.org/10.3390/cancers13061339







