Pancreatic Cancer Meets Human Microbiota: Close Encounters of the Third Kind
Abstract
:Simple Summary
Abstract
1. Introduction
2. Oral Microbiota and PDAC Risk
3. Gastrointestinal Microbiota and PDAC
3.1. Gastric Microbiota and PDAC-Related Helicobacter pylori
3.2. Gut Microbiota
4. Intratumoral Microbiota
Intratumoral Microbiota as a Prognostic Biomarker for PDAC
5. Microbiota Studies in Animal Models Are Paving the Way for Future Microbiota-Based Treatment Strategies for Pancreatic Cancer
6. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA. Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- Midha, S.; Chawla, S.; Garg, P.K. Modifiable and non-modifiable risk factors for pancreatic cancer: A review. Cancer Lett. 2016, 381, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Silverman, D.T.; Dunn, J.A.; Hoover, R.N.; Schiffiman, M.; Lillemoe, K.D.; Schoenberg, J.B.; Brown, L.M.; Greenberg, R.S.; Hayes, R.B.; Swanson, G.M.; et al. Cigarette Smoking and Pancreas Cancer: A Case—Control Study Based on Direct Interviews. JNCI J. Natl. Cancer Inst. 1994, 86, 1510–1516. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, C.; Lucenteforte, E.; Silverman, D.T.; Petersen, G.; Bracci, P.M.; Ji, B.T.; Negri, E.; Li, D.; Risch, H.A.; Olson, S.H.; et al. Cigarette smoking and pancreatic cancer: An analysis from the International Pancreatic Cancer Case-Control Consortium (Panc4). Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2012, 23, 1880–1888. [Google Scholar] [CrossRef] [PubMed]
- Iodice, S.; Gandini, S.; Maisonneuve, P.; Lowenfels, A.B. Tobacco and the risk of pancreatic cancer: A review and meta-analysis. Langenbeck’s Arch. Surg. 2008, 393, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Arslan, A.A.; Helzlsouer, K.J.; Kooperberg, C.; Shu, X.-O.; Steplowski, E.; Bueno-de-Mesquita, H.B.; Fuchs, C.S.; Gross, M.D.; Jacobs, E.J.; LaCroix, A.Z.; et al. Anthropometric Measures, Body Mass Index, and Pancreatic Cancer: A Pooled Analysis From the Pancreatic Cancer Cohort Consortium (PanScan). Arch. Intern. Med. 2010, 170, 791–802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.-T.; Gou, Y.-W.; Jin, W.-W.; Xiao, M.; Fang, H.-Y. Association between alcohol intake and the risk of pancreatic cancer: A dose–response meta-analysis of cohort studies. BMC Cancer 2016, 16, 212. [Google Scholar] [CrossRef] [Green Version]
- Huxley, R.; Ansary-Moghaddam, A.; Berrington de González, A.; Barzi, F.; Woodward, M. Type-II diabetes and pancreatic cancer: A meta-analysis of 36 studies. Br. J. Cancer 2005, 92, 2076–2083. [Google Scholar] [CrossRef] [Green Version]
- Bosetti, C.; Rosato, V.; Li, D.; Silverman, D.; Petersen, G.M.; Bracci, P.M.; Neale, R.E.; Muscat, J.; Anderson, K.; Gallinger, S.; et al. Diabetes, antidiabetic medications, and pancreatic cancer risk: An analysis from the International Pancreatic Cancer Case-Control Consortium. Ann. Oncol. 2014, 25, 2065–2072. [Google Scholar] [CrossRef]
- Stolzenberg-Solomon, R.Z.; Graubard, B.I.; Chari, S.; Limburg, P.; Taylor, P.R.; Virtamo, J.; Albanes, D. Insulin, Glucose, Insulin Resistance, and Pancreatic Cancer in Male Smokers. JAMA 2005, 294, 2872–2878. [Google Scholar] [CrossRef] [Green Version]
- Ben, Q.; Cai, Q.; Li, Z.; Yuan, Y.; Ning, X.; Deng, S.; Wang, K. The relationship between new-onset diabetes mellitus and pancreatic cancer risk: A case–control study. Eur. J. Cancer 2011, 47, 248–254. [Google Scholar] [CrossRef]
- Jansen, R.J.; Tan, X.-L.; Petersen, G.M. Focus: A Multifaceted Battle Against Cancer: Gene-by-Environment Interactions in Pancreatic Cancer: Implications for Prevention. Yale J. Biol. Med. 2015, 88, 115. [Google Scholar]
- Wolpin, B.M.; Chan, A.T.; Hartge, P.; Chanock, S.J.; Kraft, P.; Hunter, D.J.; Giovannucci, E.L.; Fuchs, C.S. ABO blood group and the risk of pancreatic cancer. J. Natl. Cancer Inst. 2009, 101, 424–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amundadottir, L.; Kraft, P.; Stolzenberg-Solomon, R.Z.; Fuchs, C.S.; Petersen, G.M.; Arslan, A.A.; Bueno-de-Mesquita, H.B.; Gross, M.; Helzlsouer, K.; Jacobs, E.J. Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer. Nat. Genet. 2009, 41, 986–990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solomon, S.; Das, S.; Brand, R.; Whitcomb, D.C. Inherited Pancreatic Cancer Syndromes. Cancer J. 2012, 18, 485–491. [Google Scholar] [CrossRef] [Green Version]
- Magnúsdóttir, S.; Heinken, A.; Kutt, L.; Ravcheev, D.A.; Bauer, E.; Noronha, A.; Greenhalgh, K.; Jäger, C.; Baginska, J.; Wilmes, P. Generation of genome-scale metabolic reconstructions for 773 members of the human gut microbiota. Nat. Biotechnol. 2017, 35, 81. [Google Scholar] [CrossRef]
- Ursell, L.K.; Metcalf, J.L.; Parfrey, L.W.; Knight, R. Defining the human microbiome. Nutr. Rev. 2012, 70, S38–S44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sender, R.; Fuchs, S.; Milo, R. Are we really vastly outnumbered? Revisiting the ratio of bacterial to host cells in humans. Cell 2016, 164, 337–340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lukens, J.R.; Gurung, P.; Vogel, P.; Johnson, G.R.; Carter, R.A.; McGoldrick, D.J.; Bandi, S.R.; Calabrese, C.R.; Walle, L. Vande; Lamkanfi, M. Dietary modulation of the microbiome affects autoinflammatory disease. Nature 2014, 516, 246–249. [Google Scholar] [CrossRef] [Green Version]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desai, M.S.; Seekatz, A.M.; Koropatkin, N.M.; Kamada, N.; Hickey, C.A.; Wolter, M.; Pudlo, N.A.; Kitamoto, S.; Terrapon, N.; Muller, A. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell 2016, 167, 1339–1353. [Google Scholar] [CrossRef] [Green Version]
- Akshintala, V.S.; Talukdar, R.; Singh, V.K.; Goggins, M. The Gut Microbiome in Pancreatic Disease. Clin. Gastroenterol. Hepatol. 2019, 17, 290–295. [Google Scholar] [CrossRef]
- Carding, S.; Verbeke, K.; Vipond, D.T.; Corfe, B.M.; Owen, L.J. Dysbiosis of the gut microbiota in disease. Microb. Ecol. Health Dis. 2015, 26, 26191. [Google Scholar] [CrossRef] [PubMed]
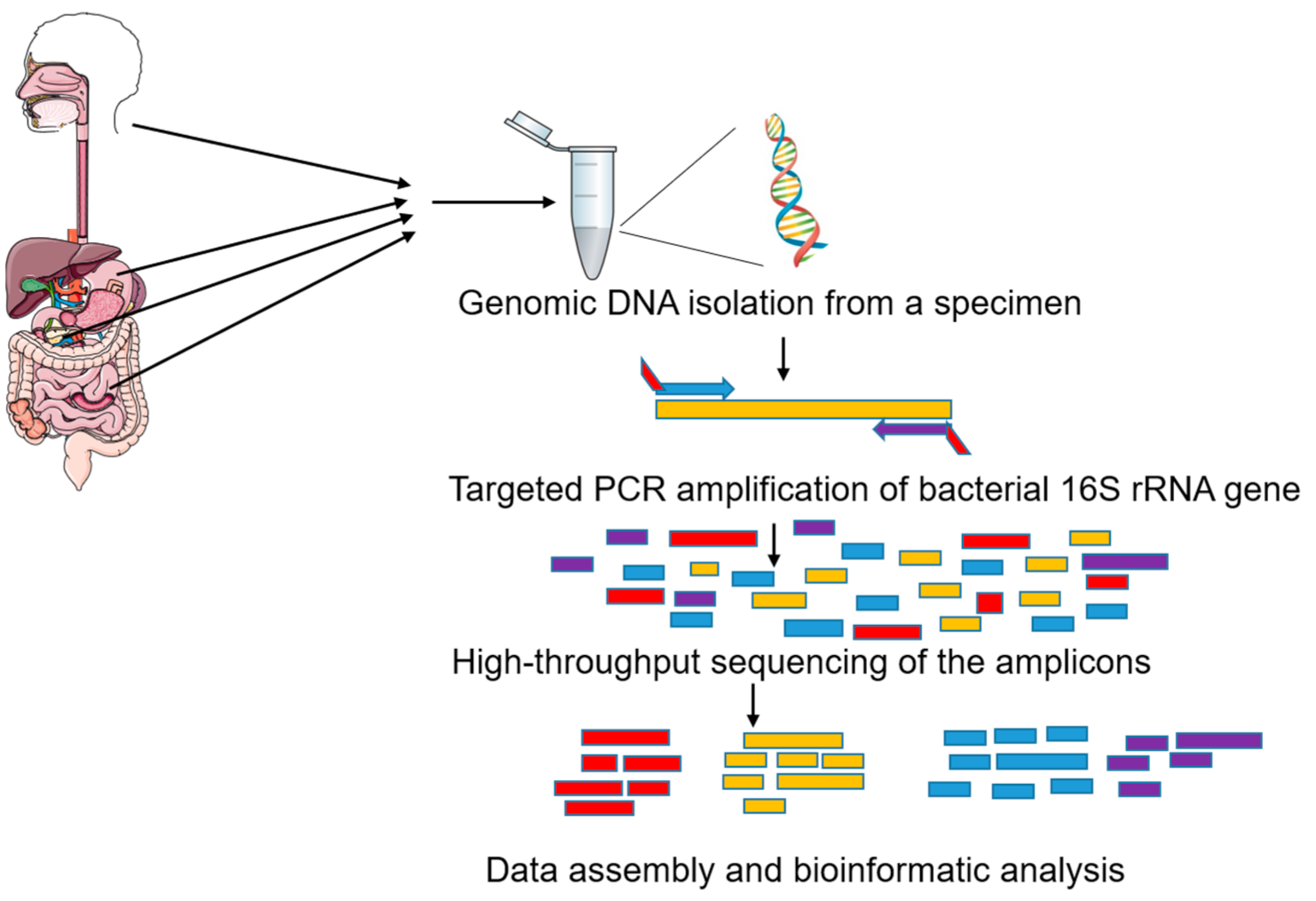
- Sambo, F.; Finotello, F.; Lavezzo, E.; Baruzzo, G.; Masi, G.; Peta, E.; Falda, M.; Toppo, S.; Barzon, L.; Di Camillo, B. Optimizing PCR primers targeting the bacterial 16S ribosomal RNA gene. BMC Bioinformatics 2018, 19, 343. [Google Scholar] [CrossRef] [PubMed]
- Aas, J.A.; Paster, B.J.; Stokes, L.N.; Olsen, I.; Dewhirst, F.E. Defining the normal bacterial flora of the oral cavity. J. Clin. Microbiol. 2005, 43, 5721–5732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Genco, R.J. Consensus report, periodontal disease; pathogenesis and microbial factors. Ann. Periodontol. 1996, 1, 926–932. [Google Scholar]
- Ahn, J.; Segers, S.; Hayes, R.B. Periodontal disease, Porphyromonas gingivalis serum antibody levels and orodigestive cancer mortality. Carcinogenesis 2012, 33, 1055–1058. [Google Scholar] [CrossRef] [Green Version]
- Michaud, D.S.; Joshipura, K.; Giovannucci, E.; Fuchs, C.S. A prospective study of periodontal disease and pancreatic cancer in US male health professionals. J. Natl. Cancer Inst. 2007, 99, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Ansai, T.; Takata, Y.; Yoshida, A.; Soh, I.; Awano, S.; Hamasaki, T.; Sogame, A.; Shimada, N. Association between tooth loss and orodigestive cancer mortality in an 80-year-old community-dwelling Japanese population: A 12-year prospective study. BMC Public Health 2013, 13, 814. [Google Scholar] [CrossRef] [Green Version]
- Stolzenberg-Solomon, R.Z.; Dodd, K.W.; Blaser, M.J.; Virtamo, J.; Taylor, P.R.; Albanes, D. Tooth loss, pancreatic cancer, and Helicobacter pylori. Am. J. Clin. Nutr. 2003, 78, 176–181. [Google Scholar] [CrossRef]
- Hujoel, P.P.; Drangsholt, M.; Spiekerman, C.; Weiss, N.S. An exploration of the periodontitis–cancer association. Ann. Epidemiol. 2003, 13, 312–316. [Google Scholar] [CrossRef]
- Farrell, J.J.; Zhang, L.; Zhou, H.; Chia, D.; Elashoff, D.; Akin, D.; Paster, B.J.; Joshipura, K.; Wong, D.T.W. Variations of oral microbiota are associated with pancreatic diseases including pancreatic cancer. Gut 2012, 61, 582–588. [Google Scholar] [CrossRef]
- Torres, P.J.; Fletcher, E.M.; Gibbons, S.M.; Bouvet, M.; Doran, K.S.; Kelley, S.T. Characterization of the salivary microbiome in patients with pancreatic cancer. PeerJ 2015, 3, e1373. [Google Scholar] [CrossRef] [PubMed]
- Olson, S.H.; Satagopan, J.; Xu, Y.; Ling, L.; Leong, S.; Orlow, I.; Saldia, A.; Li, P.; Nunes, P.; Madonia, V.; et al. The oral microbiota in patients with pancreatic cancer, patients with IPMNs, and controls: A pilot study. Cancer Causes Control 2017, 28, 959–969. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Ren, Z.; Li, A.; Li, J.; Xu, S.; Zhang, H.; Jiang, J.; Yang, J.; Luo, Q.; Zhou, K.; et al. Tongue coating microbiome data distinguish patients with pancreatic head cancer from healthy controls. J. Oral Microbiol. 2019, 11, 1563409. [Google Scholar] [CrossRef]
- Vogtmann, E.; Han, Y.; Caporaso, J.G.; Bokulich, N.; Mohamadkhani, A.; Moayyedkazemi, A.; Hua, X.; Kamangar, F.; Wan, Y.; Suman, S. Oral microbial community composition is associated with pancreatic cancer: A case-control study in Iran. Cancer Med. 2020, 9, 797–806. [Google Scholar] [CrossRef] [Green Version]
- Michaud, D.S.; Izard, J.; Wilhelm-Benartzi, C.S.; You, D.-H.; Grote, V.A.; Tjønneland, A.; Dahm, C.C.; Overvad, K.; Jenab, M.; Fedirko, V.; et al. Plasma antibodies to oral bacteria and risk of pancreatic cancer in a large European prospective cohort study. Gut 2013, 62, 1764–1770. [Google Scholar] [CrossRef]
- Fan, X.; Alekseyenko, A.V.; Wu, J.; Peters, B.A.; Jacobs, E.J.; Gapstur, S.M.; Purdue, M.P.; Abnet, C.C.; Stolzenberg-Solomon, R.; Miller, G.; et al. Human oral microbiome and prospective risk for pancreatic cancer: A population-based nested case-control study. Gut 2018, 67, 120–127. [Google Scholar] [CrossRef] [Green Version]
- Gupta, V.K.; Paul, S.; Dutta, C. Geography, ethnicity or subsistence-specific variations in human microbiome composition and diversity. Front. Microbiol. 2017, 8, 1162. [Google Scholar] [CrossRef] [Green Version]
- Renson, A.; Jones, H.E.; Beghini, F.; Segata, N.; Zolnik, C.P.; Usyk, M.; Moody, T.U.; Thorpe, L.; Burk, R.; Waldron, L. Sociodemographic variation in the oral microbiome. Ann. Epidemiol. 2019, 35, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Blekhman, R.; Goodrich, J.K.; Huang, K.; Sun, Q.; Bukowski, R.; Bell, J.T.; Spector, T.D.; Keinan, A.; Ley, R.E.; Gevers, D. Host genetic variation impacts microbiome composition across human body sites. Genome Biol. 2015, 16, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Mason, M.R.; Nagaraja, H.N.; Camerlengo, T.; Joshi, V.; Kumar, P.S. Deep sequencing identifies ethnicity-specific bacterial signatures in the oral microbiome. PLoS ONE 2013, 8, e77287. [Google Scholar] [CrossRef]
- Fan, X.; Peters, B.A.; Min, D.; Ahn, J.; Hayes, R.B. Comparison of the oral microbiome in mouthwash and whole saliva samples. PLoS ONE 2018, 13, e0194729. [Google Scholar]
- Teng, F.; Darveekaran Nair, S.S.; Zhu, P.; Li, S.; Huang, S.; Li, X.; Xu, J.; Yang, F. Impact of DNA extraction method and targeted 16S-rRNA hypervariable region on oral microbiota profiling. Sci. Rep. 2018, 8, 16321. [Google Scholar] [CrossRef]
- Tremblay, J.; Singh, K.; Fern, A.; Kirton, E.S.; He, S.; Woyke, T.; Lee, J.; Chen, F.; Dangl, J.L.; Tringe, S.G. Primer and platform effects on 16S rRNA tag sequencing. Front. Microbiol. 2015, 6, 771. [Google Scholar] [CrossRef] [Green Version]
- Walker, A.W.; Martin, J.C.; Scott, P.; Parkhill, J.; Flint, H.J.; Scott, K.P. 16S rRNA gene-based profiling of the human infant gut microbiota is strongly influenced by sample processing and PCR primer choice. Microbiome 2015, 3, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gihring, T.M.; Green, S.J.; Schadt, C.W. Massively parallel rRNA gene sequencing exacerbates the potential for biased community diversity comparisons due to variable library sizes. Environ. Microbiol. 2012, 14, 285–290. [Google Scholar] [CrossRef]
- Li, X.; Kolltveit, K.M.; Tronstad, L.; Olsen, I. Systemic diseases caused by oral infection. Clin. Microbiol. Rev. 2000, 13, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Gaiser, R.A.; Halimi, A.; Alkharaan, H.; Lu, L.; Davanian, H.; Healy, K.; Hugerth, L.W.; Ateeb, Z.; Valente, R.; Fernández Moro, C.; et al. Enrichment of oral microbiota in early cystic precursors to invasive pancreatic cancer. Gut 2019, 68. [Google Scholar] [CrossRef] [Green Version]
- Mitsuhashi, K.; Nosho, K.; Sukawa, Y.; Matsunaga, Y.; Ito, M.; Kurihara, H.; Kanno, S.; Igarashi, H.; Naito, T.; Adachi, Y.; et al. Association of Fusobacterium species in pancreatic cancer tissues with molecular features and prognosis. Oncotarget 2015, 6, 7209–7220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marshall, B.; Warren, J.R. Unidentified Curved Bacilli In The Stomach Of Patients With Gastritis And Peptic Ulceration. Lancet 1984, 323, 1311–1315. [Google Scholar] [CrossRef]
- Kalaf, E.A.; Al-Khafaji, Z.M.; Yassen, N.Y.; Al-Abbudi, F.A.; Sadwen, S.N. Study of the cytoxin-associated gene a (CagA gene) in Helicobacter pylori using gastric biopsies of Iraqi patients. Saudi J. Gastroenterol. Off. J. Saudi Gastroenterol. Assoc. 2013, 19, 69. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Duan, G.; Zhang, R.; Fan, Q. Helicobacter pylori cytotoxin-associated gene A protein upregulates α-enolase expression via Src/MEK/ERK pathway: Implication for progression of gastric cancer. Int. J. Oncol. 2014, 45, 764–770. [Google Scholar] [CrossRef]
- Schistosomes, liver flukes and Helicobacter pylori. In IARC Monographs on the Evaluation of Carcinogenic Risks to Humans; IARC: Lyon, France, 1994; Volume 61, pp. 1–241.
- Raderer, M.; Wrba, F.; Kornek, G.; Maca, T.; Koller, D.Y.; Weinlaender, G.; Hejna, M.; Scheithauer, W. Association between Helicobacter pylori infection and pancreatic cancer. Oncology 1998, 55, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Stolzenberg-Solomon, R.Z.; Blaser, M.J.; Limburg, P.J.; Perez-Perez, G.; Taylor, P.R.; Virtamo, J.; Albanes, D. Helicobacter pylori seropositivity as a risk factor for pancreatic cancer. J. Natl. Cancer Inst. 2001, 93, 937–941. [Google Scholar] [CrossRef]
- Lindkvist, B.; Johansen, D.; Borgström, A.; Manjer, J. A prospective study of Helicobacter pylori in relation to the risk for pancreatic cancer. BMC Cancer 2008, 8, 321. [Google Scholar] [CrossRef] [Green Version]
- Bao, Y.; Spiegelman, D.; Li, R.; Giovannucci, E.; Fuchs, C.S.; Michaud, D.S. History of peptic ulcer disease and pancreatic cancer risk in men. Gastroenterology 2010, 138, 541–549. [Google Scholar] [CrossRef] [Green Version]
- Risch, H.A. Etiology of pancreatic cancer, with a hypothesis concerning the role of N-nitroso compounds and excess gastric acidity. J. Natl. Cancer Inst. 2003, 95, 948–960. [Google Scholar] [CrossRef]
- de Martel, C.; Llosa, A.E.; Friedmana, G.D.; Vogelman, J.H.; Orentreich, N.; Stolzenberg-Solomon, R.Z.; Parsonnet, J. Helicobacter pylori infection and development of pancreatic cancer. Cancer Epidemiol. Prev. Biomarkers 2008, 17, 1188–1194. [Google Scholar] [CrossRef] [Green Version]
- Gawin, A.; Wex, T.; Ławniczak, M.; Malfertheiner, P.; Starzyńska, T. Helicobacter pylori infection in pancreatic cancer. Pol. Merkur. Lek. organ Pol. Tow. Lek. 2012, 32, 103. [Google Scholar]
- Frulloni, L.; Lunardi, C.; Simone, R.; Dolcino, M.; Scattolini, C.; Falconi, M.; Benini, L.; Vantini, I.; Corrocher, R.; Puccetti, A. Identification of a novel antibody associated with autoimmune pancreatitis. N. Engl. J. Med. 2009, 361, 2135–2142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nilsson, H.-O.; Stenram, U.; Ihse, I.; Wadstrom, T. Helicobacter species ribosomal DNA in the pancreas, stomach and duodenum of pancreatic cancer patients. World J. Gastroenterol. 2006, 12, 3038–3043. [Google Scholar] [CrossRef] [PubMed]
- Rogers, M.B.; Aveson, V.; Firek, B.; Yeh, A.; Brooks, B.; Brower-Sinning, R.; Steve, J.; Banfield, J.F.; Zureikat, A.; Hogg, M.; et al. Disturbances of the Perioperative Microbiome Across Multiple Body Sites in Patients Undergoing Pancreaticoduodenectomy. Pancreas 2017, 46, 260–267. [Google Scholar] [CrossRef] [Green Version]
- Geller, L.T.; Barzily-Rokni, M.; Danino, T.; Jonas, O.H.; Shental, N.; Nejman, D.; Gavert, N.; Zwang, Y.; Cooper, Z.A.; Shee, K.; et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science 2017, 357, 1156–1160. [Google Scholar] [CrossRef] [Green Version]
- del Castillo, E.; Meier, R.; Chung, M.; Koestler, D.C.; Chen, T.; Paster, B.J.; Charpentier, K.P.; Kelsey, K.T.; Izard, J.; Michaud, D.S. The Microbiomes of Pancreatic and Duodenum Tissue Overlap and Are Highly Subject Specific but Differ between Pancreatic Cancer and Noncancer Subjects. Cancer Epidemiol. Biomarkers Prev. 2019, 28, 370–383. [Google Scholar] [CrossRef] [Green Version]
- Riquelme, E.; Zhang, Y.; Zhang, L.; Jenq, R.; Wargo, J.; Mcallister, F. Tumor Microbiome Diversity and Composition Article Tumor Microbiome Diversity and Composition Influence Pancreatic Cancer Outcomes. Cell 2019, 178. [Google Scholar] [CrossRef] [PubMed]
- Nejman, D.; Livyatan, I.; Fuks, G.; Gavert, N.; Zwang, Y.; Geller, L.T.; Rotter-Maskowitz, A.; Weiser, R.; Mallel, G.; Gigi, E.; et al. The human tumor microbiome is composed of tumor type–specific intracellular bacteria. Science 2020, 368. [Google Scholar] [CrossRef] [PubMed]
- Aykut, B.; Pushalkar, S.; Chen, R.; Li, Q.; Abengozar, R.; Kim, J.I.; Shadaloey, S.A.; Wu, D.; Preiss, P.; Verma, N.; et al. The fungal mycobiome promotes pancreatic oncogenesis via activation of MBL. Nature 2019, 574, 264–267. [Google Scholar] [CrossRef]
- Risch, H.A. Pancreatic cancer: Helicobacter pylori colonization, N-Nitrosamine exposures, and ABO blood group. Mol. Carcinog. 2012, 51, 109–118. [Google Scholar] [CrossRef]
- Jesenofsky, R.; Isaksson, B.; Möhrcke, C.; Bertsch, C.; Bulajic, M.; Schneider-Brachert, W.; Klöppel, G.; Lowenfels, A.B.; Maisonneuve, P.; Löhr, J.-M. Helicobacter pylori in autoimmune pancreatitis and pancreatic carcinoma. Pancreatology 2010, 10, 462–466. [Google Scholar]
- Takayama, S.; Takahashi, H.; Matsuo, Y.; Okada, Y.; Manabe, T. Effects of Helicobacter pylori infection on human pancreatic cancer cell line. Hepatogastroenterology 2008, 54, 2387–2391. [Google Scholar]
- Plottel, C.S.; Blaser, M.J. Microbiome and Malignancy. Cell Host Microbe 2011, 10, 324–335. [Google Scholar] [CrossRef] [Green Version]
- Cho, I.; Blaser, M.J. The human microbiome: At the interface of health and disease. Nat. Rev. Genet. 2012, 13, 260–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwabe, R.F.; Jobin, C. The microbiome and cancer. Nat. Rev. Cancer 2013, 13, 800–812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gopalakrishnan, V.; Helmink, B.A.; Spencer, C.N.; Reuben, A.; Wargo, J.A. The Influence of the Gut Microbiome on Cancer, Immunity, and Cancer Immunotherapy. Cancer Cell 2018, 33, 570–580. [Google Scholar] [CrossRef] [Green Version]
- Ren, Z.; Jiang, J.; Xie, H.; Li, A.; Lu, H.; Xu, S.; Zhou, L.; Zhang, H.; Cui, G.; Chen, X.; et al. Gut microbial profile analysis by MiSeq sequencing of pancreatic carcinoma patients in China. Oncotarget 2017, 8, 95176–95191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mei, Q.-X.; Huang, C.-L.; Luo, S.-Z.; Zhang, X.-M.; Zeng, Y.; Lu, Y.-Y. Characterization of the duodenal bacterial microbiota in patients with pancreatic head cancer vs. healthy controls. Pancreatology 2018, 18, 438–445. [Google Scholar] [CrossRef]
- Kohi, S.; Macgregor-Das, A.; Dbouk, M.; Yoshida, T.; Chuidian, M.; Abe, T.; Borges, M.; Lennon, A.M.; Shin, E.J.; Canto, M.I.; et al. Alterations In The Duodenal Fluid Microbiome Of Patients With Pancreatic Cancer. Clin. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef]
- Pushalkar, S.; Hundeyin, M.; Daley, D.; Zambirinis, C.P.; Kurz, E.; Mishra, A.; Mohan, N.; Aykut, B.; Usyk, M.; Torres, L.E.; et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov. 2018, 8, 403–416. [Google Scholar] [CrossRef] [Green Version]
- Thomas, R.M.; Gharaibeh, R.Z.; Gauthier, J.; Beveridge, M.; Pope, J.L.; Guijarro, M.V.; Yu, Q.; He, Z.; Ohland, C.; Newsome, R. Intestinal microbiota enhances pancreatic carcinogenesis in preclinical models. Carcinogenesis 2018, 39, 1068–1078. [Google Scholar] [CrossRef]
- Sethi, V.; Kurtom, S.; Tarique, M.; Lavania, S.; Malchiodi, Z.; Hellmund, L.; Zhang, L.; Sharma, U.; Giri, B.; Garg, B.; et al. Gut Microbiota Promotes Tumor Growth in Mice by Modulating Immune Response. Gastroenterology 2018, 155, 33–37. [Google Scholar] [CrossRef] [PubMed]

| Ref. | Study Design | N. PDAC Patients | N. Controls | Detection Method | Microbiota Association | Main Findings/Authors’ Conclusion |
|---|---|---|---|---|---|---|
| Farrell et al., 2012 [32] | Case-control | 38 | 38 HC 27 CP | Saliva, 16S rRNA amplicon hybridized on HOMIM array | Granulicatella adiacens increased, Neisseria elongata and Streptococcus mitis decreased abundance in PDAC cases | Combination of salivary N. elongata and S. mitis abundance distinguished cancer patients from healthy controls (AUC = 0.90) and proposed as a specific biomarker for PDAC. G. adiacens and S. mitis distinguished cancer patients from chronic pancreatitis (AUC = 0.68). |
| Torres et al., 2015 [33] | Case-control | 8 | 22 HC | Saliva, 16S rRNA V3-V4 amplicon sequencing | Leptotrichia and Porphyromonas increased abundance Neisseria and Aggregatibacter decreased abundance in PDAC | Overall microbiota diversity of the groups was very similar. Salivary Leptotrichia to Porphyromonas ratio proposed as PDAC biomarker. |
| Olson et al., 2017 [34] | Case-control | 40 | 58 HC 39 IPMN | Saliva, 16S rRNA V4–V5 amplicon sequencing | Increased abundance of Firmicutes and related taxa in PDAC versus higher levels of Proteobacteria and related taxa in healthy controls | No differences in overall saliva microbiota diversity (alpha diversity) between PDAC and IPMN patients. |
| Lu et al., 2019 [35] | Case-control | 30 | 25 HC | Tongue swab, 16S rRNA V3–V4 amplicon sequencing | Fusobacterium, Leptotrichia, Actinomyces, Corynebacterium, Rothia, Moraxella and Atopobium preponderance in PDAC | Haemophilus, Porphyromonas, Leptotrichia and Fusobacterium could distinguish PDAC patients from healthy subjects (AUC = 0.802). |
| Vogtmann et al., 2020 [36] | Case-control | 273 | 285 HC | Saliva, 16S rRNA V4 amplicon sequencing | Increased abundance of Enterobacteriaceae, Lachnospiraceae G7, Bacteroidaceae or Staphylococcaceae and decreased abundance of Haemophilus associated with PDAC | No differences in overall saliva microbiota diversity (alpha diversity) between PDAC and HC. Significant association between PDAC and microbial community composition (beta diversity). |
| Michaud et al., 2013 [37] | Prospectivenested case-control | 405 | 410 HC | Plasma (blood) samples, ELISA | Porphyromonas gingivalis ATCC 53978 increased IgG in PDAC | Individuals with high levels of antibodies to P. gingivalis ATCC 53978 are at a 2-fold higher risk of developing PDAC. |
| Fan et al., 2018 [38] | Prospectivenested case-control study | 361 | 371 HC | Mouthwash, 16S rRNA V3-V4 amplicon sequencing | P. gingivalis and A. actinomycetemcomitans increased abundance | P. gingivalis and A. actinomycetemcomitans were associated with a higher risk of PDAC, while Fusobacteria and Leptotrichia were associated with a decreased risk. |
| Ref. | Study Design | N. PDAC Patients | N. Controls | Detection Method | Microbiota Association | Main Findings/Authors’ Conclusion |
|---|---|---|---|---|---|---|
| Nilsson et al., 2006 [63] | Case-control study | 40 | 7 HC 5 CP 14 NET 10 other | Surgical specimen, DNA genus-specific PCR | Helicobacter DNA detected in the pancreas of 75% of patients with adenocarcinoma but not detected in any control | Helicobacter DNA, mostly H. pylori genus, commonly detected in pancreatic cancer. |
| Rogers et al., 2017 [64] | Cross-sectional study | 50 | / | Pancreatic fluid, bile or jejunal contents, 16S rRNA V4 amplicon sequencing | An enrichment of Klebsiella spp. and a decrease in Faecalibacterium prausnitzii and Roseburia spp. in fecal samples of PDAC patients | Klebsiella pneumoniae and Klebsiella oxytosa prepondernace in PDAC. Death at 1 year was associated with decreased Klebsiella within fecal samples of PDAC patients. |
| Mitsuhashi et al., 2015 [50] | Cross-sectional study | 283 | / | Surgical specimen PCR | Fusobacterium increased in PDAC | Significantly shorter survival observed in the Fusobacterium species-positive group. |
| Geller et al., 2017 [65] | Cross-sectional study | 65 | 20 | Surgical specimen 16S rRNA V6 amplicon sequencing | Increased Proteobacteria in PDAC | Increased presence of Gammaproteobacteria in PDAC tissue contributes to gemcitabine resistance. |
| Gaiser et al. 2018 [49] | Case-control study | 27 | 57 IPMN PCy 21 non-IPMN PCy | Cyst fluid and plasma samples 16S rRNA qPCR and full-length gene sequencing | Firmicutes and/or Proteobacteria increased in PDAC | Higher overall microbial diversity in PDAC. |
| Del Castillo et al., 2019 [66] | Cross-sectional study | 31 | 18 CPPCy 8 other | 16S rRNA V3-V4 amplicon sequencing | Porphyromonas, Capnocytophaga, Prevotella, Selenomonas and Fusobacterium spp. higher abundance in PDAC patients | The authors observed that pancreatic and gut microbiota are highly subject-specific and differ between PDAC and noncancer subjects. |
| Riquelme et al., 2019 [67] | Case-control study | 37 LTS | 31 STS | Tumor cores 16S rRNA V4 amplicon sequencing | Pseudoxanthomonas- Streptomyces- Saccharopolyspora-Bacillus clausii highly predictive of long-term survivorship | Fecal microbiome transfer from LTS patients reduced tumor growth in mice compared to STS patients. |
| Nejman et al., 2020 [68] | Retrospective study | 67 | / | Tumor cores 16S rRNA V6 amplicon sequencing | Fusobacterium nucleatum enrichment in PDAC | The human tumor microbiome is composed of tumor type-specific intracellular bacteria present in both cancer and immune cells. |
| Aykut et al., 2019 [69] | Case-control study | 13 | 18 fecal samples | 18S ITS1 amplicon sequencing | Parastagonospora, Saccharomyces, Septoriella and Malassezia genera enriched in PDAC patients | Human PDAC samples markedly enriched for Malassezia spp. |
| Ref. | Study Design | N. PDAC Patients | N. Controls | Detection Method | Microbiota Association | Main Findings/Authors’ Conclusion |
|---|---|---|---|---|---|---|
| Ren et al., 2017 [77] | Case-control study | 85 | 57 | Fecal samples, 16S rRNA V3-V5 amplicon MiSeq sequencing | Bacteroidetes significantly increased, Firmicutes and Proteobacteria decreased in PDAC compared to HC | Gut microbial diversity (alpha diversity) is significantly decreased in PDAC patients. Microbial alterations in PDAC present an increase of potentially pathogenic bacteria and a decrease of probiotics and butyrate-producing bacteria. |
| Mei et al., 2018 [78] | Case-control study | 14 | 14 | Duodenal mucosa 16S rRNA V3-V4 amplicon sequencing | Duodenal microbiota of PDAC patients enriched in Acinetobacter, Aquabacterium, Oceanobacillus, Rahnella, Massilia, Delftia, Deinococcus and Sphingobium | The results showed species in PDAC patients and HC belong mainly to the phyla Firmicutes and Proteobacteria. |
| Kohi et al., 2020 [79] | Case-control study | 74 | 134 HC 98 PCy | 16S V3-V4 and 18S ITS1 rRNA amplicon sequencing | Duodenal microbiota of PDAC patients enriched in Escherichia-Shigella, Enterococcus, Clostridium and Bifidobacterium and Ascomycota compared to HC | Patients with PDAC had significantly decreased duodenal microbial alpha diversity with an enrichment of Bifidobacterium compared to controls. An enrichment of duodenal fluid Fusobacteria and Rothia was detected in PDAC patients with short survival. |
| Pushalkar et al., 2018 [80] | Retrospective study | 12 | Not reported | Fecal samples and PDAC surgical specimen 16S rRNA V3-V4 amplicon sequencing | Proteobacteria, Actinobacteria, Fusobacteria and Verrucomicrobia higher abundance in the gut of PDAC patients | Gut microbiome indicated significant differences in bacterial abundances between Stage I/II and Stage IV PDAC patients. |
| Del Castillo et al., 2019 [66] | Cross-sectional study | 31 | 18 CP PCy 8 other | Duodenal, PDAC and PCy samples 16S rRNA V3–V4 amplicon sequencing | Porphyromonas, Capnocytophaga, Prevotella, Selenomonas, Fusobacterium spp. higher abundance in PDAC patients | The authors observed that pancreatic and gut microbiota are highly subject-specific and differ between PDAC and noncancer subjects. |
| Ref. | Experimental Model | Microbiota Association | Main Findings/Authors’ Conclusion |
|---|---|---|---|
| Geller et al., 2017 [65] | Mouse model of colon cancer | Increased Gammaproteobacteria in PDAC | Gammaproteobacteria possessing a long isoform of cytidine deaminase can metabolize gemcitabine. |
| Pushalkar et al., 2018 [80] | KC and KPC mice | Bacteroidetes and Firmicutes and select Actinobacteria- and Deferribacteres-associated genera were more prevalent in the early-KPC and advanced-KPC cohorts compared with WT | Gut microbiota migrates into the pancreas in mice models. Germ-free mice are protected against PDAC progression. Modulation of gut microbiota influences PDAC tumor progression and has a potential to augment PDAC responsiveness to immune therapy. |
| Thomas et al., 2018 [81] | KrasG12D/PTENlox/+ mice | Acinetobacter, Enterobacter, Pseudomonas, Delftia, Enterococcus, Streptococcus, Corynebacterium, Propionibacterium, Klebsiella, Sphingomonas and Staphylococcus. Klebsiella as disproportionally overrepresented in PDAC versus HC | Intestinal microbiota exerts long-distance modulation and enhances PDAC carcinogenesis in transgenic and xenograft mouse models of PDAC. |
| Sethi et al., 2018 [82] | Rag1 KO, KPC, Ptenfl/fl mice | Antibiotics induced a significant decrease in α-diversity, decrease in the relative abundance of Bacteroidetes and Firmicutes in the stool of KPC-bearing mice as well as reversed Bacteroidales: Clostridiales abundance ratio and colonization of the gut by likely antibiotic-resistant Proteobacteria and Tenericutes | Gut microbiome depletion significantly reduced tumor burden in all the models tested, except for Rag1-knockout mice, which lack mature T and B cells. |
| Aykut et al., 2019 [69] | KC, KPC and WT mice | Malassezia, at about 20% abundance Malassezia spp., most prevalent genus in pancreata of KC mice and exerts a tumor-promoting effect. | Ablation of the mycobiome with the antifungal drugs in mice protected against the PDAC progression and enhanced the effects of gemcitabine by 15 to 25 percent. |
| NCT Number | Study Design | Intervention | Condition | Title | Number of Patients | Status |
|---|---|---|---|---|---|---|
| NCT04600154 | Interventional | Drug: MS-20 Other: Placebo | Pancreatic Cancer | MS-20 on Gut Microbiota and Risk/Severity of Cachexia in Pancreatic Cancer Patients | 40 | Recruiting |
| NCT04447443 | Interventional | Dietary Supplement: Prebiotic Fiber Supplement + loperamide hydrochloride capsule Dietary Supplement: Maltodextrin + loperamide hydrochloride capsule | Gastrointestinal Tumors | Impact of Dietary Fiber as Prebiotics on Chemotherapy-related Diarrhea in Patients With Gastrointestinal Tumors | 120 | Recruiting |
| NCT04363983 | Interventional | Biological: Blood sampling Procedure: Liver biopsy Biological: Stool collect | Gastrointestinal Neoplasms | Interaction Between Host, Microenvironment and Immunity on Gastrointestinal Neoplasms (HoMING) | 6300 | Not yet recruiting |
| NCT04193904 | Interventional Phase I | Drug: MRx0518 Radiation: Hypofractionated preoperative radiation | Pancreatic Cancer | A Study of Live Biotherapeutic Product MRx0518 With Hypofractionated Radiation Therapy in Resectable Pancreatic Cancer | 15 | Recruiting |
| NCT03891979 | Interventional Phase IV | Drug: Pembrolizumab Drug: Ciprofloxacin 500 mg PO BID days 1–29 Drug: Metronidazole 500 mg PO TID days 1–29 | Pancreatic Cancer | Gut Microbiome Modulation to Enable Efficacy of Checkpoint-based Immunotherapy in Pancreatic Adenocarcinoma | 0 | Withdrawn (suspended) |
| NCT03331562 | Interventional Phase II | Drug: Pembrolizumab Drug: Paricalcitol Drug: Placebo | Pancreatic Cancer | A SU2C Catalyst® Trial of a PD1 Inhibitor with or without a Vitamin D Analog for the Maintenance of Pancreatic Cancer | 24 | Completed |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arsenijevic, T.; Nicolle, R.; Bouchart, C.; D’Haene, N.; Demetter, P.; Puleo, F.; Van Laethem, J.-L. Pancreatic Cancer Meets Human Microbiota: Close Encounters of the Third Kind. Cancers 2021, 13, 1231. https://doi.org/10.3390/cancers13061231
Arsenijevic T, Nicolle R, Bouchart C, D’Haene N, Demetter P, Puleo F, Van Laethem J-L. Pancreatic Cancer Meets Human Microbiota: Close Encounters of the Third Kind. Cancers. 2021; 13(6):1231. https://doi.org/10.3390/cancers13061231
Chicago/Turabian StyleArsenijevic, Tatjana, Remy Nicolle, Christelle Bouchart, Nicky D’Haene, Pieter Demetter, Francesco Puleo, and Jean-Luc Van Laethem. 2021. "Pancreatic Cancer Meets Human Microbiota: Close Encounters of the Third Kind" Cancers 13, no. 6: 1231. https://doi.org/10.3390/cancers13061231
APA StyleArsenijevic, T., Nicolle, R., Bouchart, C., D’Haene, N., Demetter, P., Puleo, F., & Van Laethem, J.-L. (2021). Pancreatic Cancer Meets Human Microbiota: Close Encounters of the Third Kind. Cancers, 13(6), 1231. https://doi.org/10.3390/cancers13061231







