Radiogenomics in Colorectal Cancer
Abstract
Simple Summary
Abstract
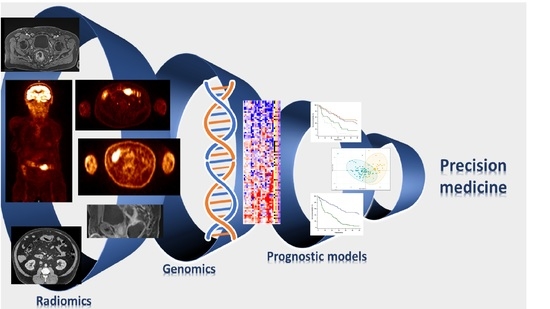
1. Introduction
2. Radiomics
2.1. Radiomics Workflow
2.2. Features Extraction
2.3. Radiomics in Colorectal Cancer
3. Genomics and Transcriptomics
4. Radiogenomics in Colorectal Cancer
4.1. 18F-FDG PET
4.2. Magnetic Resonance Imaging
4.3. CT SCAN
5. Limitations of Radiogenomics Studies
6. Discussion and Future Directions
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.T.; Giovannucci, E.L. Primary prevention of colorectal cancer. Gastroenterology 2010, 138, 2029–2043.e2010. [Google Scholar] [CrossRef]
- Quirke, P.; Williams, G.T.; Ectors, N.; Ensari, A.; Piard, F.; Nagtegaal, I. The future of the TNM staging system in colorectal cancer: Time for a debate? Lancet Oncol. 2007, 8, 651–657. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Goding Sauer, A.; Fedewa, S.A.; Butterly, L.F.; Anderson, J.C.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 145–164. [Google Scholar] [CrossRef]
- Brenner, H.; Kloor, M.; Pox, C.P. Colorectal cancer. Lancet 2014, 383, 1490–1502. [Google Scholar] [CrossRef]
- Chung, D.C. The genetic basis of colorectal cancer: Insights into critical pathways of tumorigenesis. Gastroenterology 2000, 119, 854–865. [Google Scholar] [CrossRef] [PubMed]
- Dagogo-Jack, I.; Shaw, A.T. Tumour heterogeneity and resistance to cancer therapies. Nat. Rev. Clin. Oncol. 2018, 15, 81–94. [Google Scholar] [CrossRef]
- Fass, L. Imaging and cancer: A review. Mol. Oncol. 2008, 2, 115–152. [Google Scholar] [CrossRef]
- Vallieres, M.; Zwanenburg, A.; Badic, B.; Cheze Le Rest, C.; Visvikis, D.; Hatt, M. Responsible Radiomics Research for Faster Clinical Translation. J. Nucl. Med. 2018, 59, 189–193. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.J.W.L.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The Image Biomarker Standardization Initiative: Standardized Quantitative Radiomics for High-Throughput Image-based Phenotyping. Radiology 2020, 295, 328–338. [Google Scholar] [CrossRef]
- Sanduleanu, S.; Woodruff, H.C.; de Jong, E.E.C.; van Timmeren, J.E.; Jochems, A.; Dubois, L.; Lambin, P. Tracking tumor biology with radiomics: A systematic review utilizing a radiomics quality score. Radiother. Oncol. 2018, 127, 349–360. [Google Scholar] [CrossRef] [PubMed]
- Starmans, M.P.A.; van der Voort, S.R.; Castillo Tovar, J.M.; Veenland, J.F.; Klein, S.; Niessen, W.J. Radiomics. In Handbook of Medical Image Computing and Computer Assisted Intervention; Academic Press: London, UK, 2020; pp. 429–456. [Google Scholar] [CrossRef]
- Sharma, N.; Aggarwal, L.M. Automated medical image segmentation techniques. J. Med. Phys. 2010, 35, 3–14. [Google Scholar] [CrossRef]
- Badic, B.; Desseroit, M.C.; Hatt, M.; Visvikis, D. Potential Complementary Value of Noncontrast and Contrast Enhanced CT Radiomics in Colorectal Cancers. Acad. Radiol. 2019, 26, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Horvat, N.; Bates, D.D.B.; Petkovska, I. Novel imaging techniques of rectal cancer: What do radiomics and radiogenomics have to offer? A literature review. Abdom. Radiol. 2019, 44, 3764–3774. [Google Scholar] [CrossRef]
- Stanzione, A.; Gambardella, M.; Cuocolo, R.; Ponsiglione, A.; Romeo, V.; Imbriaco, M. Prostate MRI radiomics: A systematic review and radiomic quality score assessment. Eur. J. Radiol. 2020, 129, 109095. [Google Scholar] [CrossRef]
- Ronneberger, O.; Fischer, P.; Brox, T. U-Net: Convolutional Networks for Biomedical Image Segmentation. In Medical Image Computing and Computer-Assisted Intervention—MICCAI 2015; Springer: Cham, Germany, 2015; pp. 234–241. [Google Scholar]
- Kotsiantis, S.B.; Zaharakis, I.; Pintelas, P. Supervised machine learning: A review of classification techniques. Emerg. Artif. Intell. Appl. Comput. Eng. 2007, 160, 3–24. [Google Scholar]
- Wang, Z.; Wang, E.; Zhu, Y. Image segmentation evaluation: A survey of methods. Artif. Intell. Rev. 2020, 53, 5637–5674. [Google Scholar] [CrossRef]
- Hatt, M.; Tixier, F.; Pierce, L.; Kinahan, P.E.; Le Rest, C.C.; Visvikis, D. Characterization of PET/CT images using texture analysis: The past, the present... any future? Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Parekh, V.S.; Jacobs, M.A. Deep learning and radiomics in precision medicine. Expert Rev. Precis. Med. Drug Dev. 2019, 4, 59–72. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, S.; Dong, D.; Wei, J.; Fang, C.; Zhou, X.; Sun, K.; Li, L.; Li, B.; Wang, M.; et al. The Applications of Radiomics in Precision Diagnosis and Treatment of Oncology: Opportunities and Challenges. Theranostics 2019, 9, 1303–1322. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression shrinkage and selection via the lasso: A retrospective. J. R. Stat. Soc. Ser. B (Stat. Methodol.) 2011, 73, 273–282. [Google Scholar] [CrossRef]
- Breiman, L. Random forest. Mach. Learn. 2001, 45, 5–23. [Google Scholar] [CrossRef]
- Hearst, M.A.; Dumais, S.T.; Osuna, E.; Platt, J.; Scholkopf, B. Support vector machines. IEEE Intell. Syst. Appl. 1998, 13, 18–28. [Google Scholar] [CrossRef]
- Liu, Y.; Dou, Y.; Lu, F.; Liu, L. A study of radiomics parameters from dual-energy computed tomography images for lymph node metastasis evaluation in colorectal mucinous adenocarcinoma. Medicine 2020, 99, e19251. [Google Scholar] [CrossRef]
- Huang, Y.; He, L.; Dong, D.; Yang, C.; Liang, C.; Chen, X.; Ma, Z.; Huang, X.; Yao, S.; Liang, C.; et al. Individualized prediction of perineural invasion in colorectal cancer: Development and validation of a radiomics prediction model. Chin. J. Cancer Res. 2018, 30, 40–50. [Google Scholar] [CrossRef]
- Hu, T.; Wang, S.; Huang, L.; Wang, J.; Shi, D.; Li, Y.; Tong, T.; Peng, W. A clinical-radiomics nomogram for the preoperative prediction of lung metastasis in colorectal cancer patients with indeterminate pulmonary nodules. Eur. Radiol. 2019, 29, 439–449. [Google Scholar] [CrossRef] [PubMed]
- Beckers, R.C.J.; Trebeschi, S.; Maas, M.; Schnerr, R.S.; Sijmons, J.M.L.; Beets, G.L.; Houwers, J.B.; Beets-Tan, R.G.H.; Lambregts, D.M.J. CT texture analysis in colorectal liver metastases and the surrounding liver parenchyma and its potential as an imaging biomarker of disease aggressiveness, response and survival. Eur. J. Radiol. 2018, 102, 15–21. [Google Scholar] [CrossRef]
- Shur, J.; Orton, M.; Connor, A.; Fischer, S.; Moulton, C.A.; Gallinger, S.; Koh, D.M.; Jhaveri, K.S. A clinical-radiomic model for improved prognostication of surgical candidates with colorectal liver metastases. J. Surg. Oncol. 2019. [Google Scholar] [CrossRef]
- Dercle, L.; Lu, L.; Schwartz, L.H.; Qian, M.; Tejpar, S.; Eggleton, P.; Zhao, B.; Piessevaux, H. Radiomics Response Signature for Identification of Metastatic Colorectal Cancer Sensitive to Therapies Targeting EGFR Pathway. J. Natl. Cancer Inst. 2020. [Google Scholar] [CrossRef]
- Dohan, A.; Gallix, B.; Guiu, B.; Le Malicot, K.; Reinhold, C.; Soyer, P.; Bennouna, J.; Ghiringhelli, F.; Barbier, E.; Boige, V.; et al. Early evaluation using a radiomic signature of unresectable hepatic metastases to predict outcome in patients with colorectal cancer treated with FOLFIRI and bevacizumab. Gut 2020, 69, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Simpson, A.L.; Doussot, A.; Creasy, J.M.; Adams, L.B.; Allen, P.J.; DeMatteo, R.P.; Gönen, M.; Kemeny, N.E.; Kingham, T.P.; Shia, J.; et al. Computed Tomography Image Texture: A Noninvasive Prognostic Marker of Hepatic Recurrence after Hepatectomy for Metastatic Colorectal Cancer. Ann. Surg. Oncol. 2017, 24, 2482–2490. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Jimenez, C.; Antunes, J.T.; Talasila, N.; Bera, K.; Brady, J.T.; Gollamudi, J.; Marderstein, E.; Kalady, M.F.; Purysko, A.; Willis, J.E.; et al. Radiomic Texture and Shape Descriptors of the Rectal Environment on Post-Chemoradiation T2-Weighted MRI are Associated with Pathologic Tumor Stage Regression in Rectal Cancers: A Retrospective, Multi-Institution Study. Cancers 2020, 12, 2027. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, R.; Akiyoshi, T.; Toda, S.; Murakami, Y.; Taguchi, S.; Oba, K.; Hanaoka, Y.; Nagasaki, T.; Yamaguchi, T.; Konishi, T.; et al. Radiomics Approach Outperforms Diameter Criteria for Predicting Pathological Lateral Lymph Node Metastasis after Neoadjuvant (Chemo)Radiotherapy in Advanced Low Rectal Cancer. Ann. Surg. Oncol. 2020. [Google Scholar] [CrossRef]
- Huang, Y.-Q.; Liang, C.-H.; He, L.; Tian, J.; Liang, C.-S.; Chen, X.; Ma, Z.-L.; Liu, Z.-Y. Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J. Clin. Oncol. 2016, 34, 2157–2164. [Google Scholar] [CrossRef]
- Petkovska, I.; Tixier, F.; Ortiz, E.J.; Golia Pernicka, J.S.; Paroder, V.; Bates, D.D.; Horvat, N.; Fuqua, J.; Schilsky, J.; Gollub, M.J.; et al. Clinical utility of radiomics at baseline rectal MRI to predict complete response of rectal cancer after chemoradiation therapy. Abdom. Radiol. 2020. [Google Scholar] [CrossRef]
- Antunes, J.T.; Ofshteyn, A.; Bera, K.; Wang, E.Y.; Brady, J.T.; Willis, J.E.; Friedman, K.A.; Marderstein, E.L.; Kalady, M.F.; Stein, S.L.; et al. Radiomic Features of Primary Rectal Cancers on Baseline T2—Weighted MRI Are Associated With Pathologic Complete Response to Neoadjuvant Chemoradiation: A Multisite Study. J. Magn. Reson. Imaging 2020, 52, 1531–1541. [Google Scholar] [CrossRef] [PubMed]
- Fearon, E.R.; Vogelstein, B. A genetic model for colorectal tumorigenesis. Cell 1990, 61, 759–767. [Google Scholar] [CrossRef]
- Tariq, K.; Ghias, K. Colorectal cancer carcinogenesis: A review of mechanisms. Cancer Biol. Med. 2016, 13, 120–135. [Google Scholar] [CrossRef] [PubMed]
- Grady, W.M. Genomic instability and colon cancer. Cancer Metastasis Rev. 2004, 23, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Pino, M.S.; Chung, D.C. The chromosomal instability pathway in colon cancer. Gastroenterology 2010, 138, 2059–2072. [Google Scholar] [CrossRef]
- Walther, A.; Houlston, R.; Tomlinson, I. Association between chromosomal instability and prognosis in colorectal cancer: A meta-analysis. Gut 2008, 57, 941. [Google Scholar] [CrossRef] [PubMed]
- Toyota, M.; Ahuja, N.; Ohe-Toyota, M.; Herman, J.G.; Baylin, S.B.; Issa, J.P. CpG island methylator phenotype in colorectal cancer. Proc. Natl. Acad. Sci. USA 1999, 96, 8681–8686. [Google Scholar] [CrossRef]
- Nazemalhosseini Mojarad, E.; Kuppen, P.J.; Aghdaei, H.A.; Zali, M.R. The CpG island methylator phenotype (CIMP) in colorectal cancer. Gastroenterol. Hepatol. Bed Bench 2013, 6, 120–128. [Google Scholar] [PubMed]
- Juo, Y.Y.; Johnston, F.M.; Zhang, D.Y.; Juo, H.H.; Wang, H.; Pappou, E.P.; Yu, T.; Easwaran, H.; Baylin, S.; van Engeland, M.; et al. Prognostic value of CpG island methylator phenotype among colorectal cancer patients: A systematic review and meta-analysis. Ann. Oncol. 2014, 25, 2314–2327. [Google Scholar] [CrossRef]
- Jiricny, J. The multifaceted mismatch-repair system. Nat. Rev. Mol. Cell Biol. 2006, 7, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Battaglin, F.; Naseem, M.; Lenz, H.J.; Salem, M.E. Microsatellite instability in colorectal cancer: Overview of its clinical significance and novel perspectives. Clin. Adv. Hematol. Oncol. 2018, 16, 735–745. [Google Scholar]
- Shaikh, F.A.; Kolowitz, B.J.; Awan, O.; Aerts, H.J.; von Reden, A.; Halabi, S.; Mohiuddin, S.A.; Malik, S.; Shrestha, R.B.; Deible, C. Technical Challenges in the Clinical Application of Radiomics. JCO Clin. Cancer Inform. 2017, 1–8. [Google Scholar] [CrossRef]
- Guinney, J.; Dienstmann, R.; Wang, X.; de Reynies, A.; Schlicker, A.; Soneson, C.; Marisa, L.; Roepman, P.; Nyamundanda, G.; Angelino, P.; et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 2015, 21, 1350–1356. [Google Scholar] [CrossRef]
- Corti, G.; Bartolini, A.; Crisafulli, G.; Novara, L.; Rospo, G.; Montone, M.; Negrino, C.; Mussolin, B.; Buscarino, M.; Isella, C.; et al. A Genomic Analysis Workflow for Colorectal Cancer Precision Oncology. Clin. Colorectal Cancer 2019, 18, 91–101.e103. [Google Scholar] [CrossRef]
- Lievre, A.; Blons, H.; Laurent-Puig, P. Oncogenic mutations as predictive factors in colorectal cancer. Oncogene 2010, 29, 3033–3043. [Google Scholar] [CrossRef]
- Andreyev, H.J.; Norman, A.R.; Cunningham, D.; Oates, J.R.; Clarke, P.A. Kirsten ras mutations in patients with colorectal cancer: The multicenter “RASCAL” study. J. Natl. Cancer Inst. 1998, 90, 675–684. [Google Scholar] [CrossRef]
- Lievre, A.; Bachet, J.B.; Le Corre, D.; Boige, V.; Landi, B.; Emile, J.F.; Cote, J.F.; Tomasic, G.; Penna, C.; Ducreux, M.; et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006, 66, 3992–3995. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Cervantes, A.; Adam, R.; Sobrero, A.; Van Krieken, J.H.; Aderka, D.; Aranda Aguilar, E.; Bardelli, A.; Benson, A.; Bodoky, G.; et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann. Oncol. 2016, 27, 1386–1422. [Google Scholar] [CrossRef]
- Jo, W.S.; Carethers, J.M. Chemotherapeutic implications in microsatellite unstable colorectal cancer. Cancer Biomark. Sect. A Dis. Markers 2006, 2, 51–60. [Google Scholar] [CrossRef]
- Bao, X.; Zhang, H.; Wu, W.; Cheng, S.; Dai, X.; Zhu, X.; Fu, Q.; Tong, Z.; Liu, L.; Zheng, Y.; et al. Analysis of the molecular nature associated with microsatellite status in colon cancer identifies clinical implications for immunotherapy. J. Immunother. Cancer 2020, 8, e001437. [Google Scholar] [CrossRef]
- Xie, Y.H.; Chen, Y.X.; Fang, J.Y. Comprehensive review of targeted therapy for colorectal cancer. Signal Transduct. Target. Ther. 2020, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kang, J.; Baik, S.H.; Lee, K.Y.; Lim, B.J.; Jeon, T.J.; Ryu, Y.H.; Sohn, S.K. Relationship Between 18F-Fluorodeoxyglucose Uptake and V-Ki-Ras2 Kirsten Rat Sarcoma Viral Oncogene Homolog Mutation in Colorectal Cancer Patients: Variability Depending on C-Reactive Protein Level. Medicine 2016, 95, e2236. [Google Scholar] [CrossRef]
- Kawada, K.; Nakamoto, Y.; Kawada, M.; Hida, K.; Matsumoto, T.; Murakami, T.; Hasegawa, S.; Togashi, K.; Sakai, Y. Relationship between 18F-fluorodeoxyglucose accumulation and KRAS/BRAF mutations in colorectal cancer. Clin. Cancer Res. 2012, 18, 1696–1703. [Google Scholar] [CrossRef]
- Diederichs, C.G.; Staib, L.; Glasbrenner, B.; Guhlmann, A.; Glatting, G.; Pauls, S.; Beger, H.G.; Reske, S.N. F-18 Fluorodeoxyglucose (FDG) and C-Reactive Protein (CRP). Clin. Positron Imaging 1999, 2, 131–136. [Google Scholar] [CrossRef]
- Arslan, E.; Aksoy, T.; Gursu, R.U.; Dursun, N.; Cakar, E.; Cermik, T.F. The Prognostic Value of (18)F-FDG PET/CT and KRAS Mutation in Colorectal Cancers. Mol. Imaging Radionucl. Ther. 2020, 29, 17–24. [Google Scholar] [CrossRef]
- Han, C.B.; Li, F.; Ma, J.T.; Zou, H.W. Concordant KRAS mutations in primary and metastatic colorectal cancer tissue specimens: A meta-analysis and systematic review. Cancer Investig. 2012, 30, 741–747. [Google Scholar] [CrossRef]
- Mao, C.; Wu, X.Y.; Yang, Z.Y.; Threapleton, D.E.; Yuan, J.Q.; Yu, Y.Y.; Tang, J.L. Concordant analysis of KRAS, BRAF, PIK3CA mutations, and PTEN expression between primary colorectal cancer and matched metastases. Sci. Rep. 2015, 5, 8065. [Google Scholar] [CrossRef] [PubMed]
- Krikelis, D.; Skoura, E.; Kotoula, V.; Rondogianni, P.; Pianou, N.; Samartzis, A.; Xanthakis, I.; Fountzilas, G.; Datseris, I.E. Lack of association between KRAS mutations and 18F-FDG PET/CT in Caucasian metastatic colorectal cancer patients. Anticancer Res. 2014, 34, 2571–2579. [Google Scholar]
- Kawada, K.; Toda, K.; Nakamoto, Y.; Iwamoto, M.; Hatano, E.; Chen, F.; Hasegawa, S.; Togashi, K.; Date, H.; Uemoto, S.; et al. Relationship Between 18F-FDG PET/CT Scans and KRAS Mutations in Metastatic Colorectal Cancer. J. Nucl. Med. 2015, 56, 1322–1327. [Google Scholar] [CrossRef]
- Mao, W.; Zhou, J.; Zhang, H.; Qiu, L.; Tan, H.; Hu, Y.; Shi, H. Relationship between KRAS mutations and dual time point (18)F-FDG PET/CT imaging in colorectal liver metastases. Abdom. Radiol. 2019, 44, 2059–2066. [Google Scholar] [CrossRef]
- Chen, S.W.; Lin, C.Y.; Ho, C.M.; Chang, Y.S.; Yang, S.F.; Kao, C.H.; Chang, J.G. Genetic Alterations in Colorectal Cancer Have Different Patterns on 18F-FDG PET/CT. Clin. Nucl. Med. 2015, 40, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Miles, K.A.; Ganeshan, B.; Rodriguez-Justo, M.; Goh, V.J.; Ziauddin, Z.; Engledow, A.; Meagher, M.; Endozo, R.; Taylor, S.A.; Halligan, S.; et al. Multifunctional imaging signature for V-KI-RAS2 Kirsten rat sarcoma viral oncogene homolog (KRAS) mutations in colorectal cancer. J. Nucl. Med. 2014, 55, 386–391. [Google Scholar] [CrossRef]
- Oner, A.O.; Budak, E.S.; Yıldırım, S.; Aydın, F.; Sezer, C. The value of (18)FDG PET/CT parameters, hematological parameters and tumor markers in predicting KRAS oncogene mutation in colorectal cancer. Hell. J. Nucl. Med. 2017, 20, 160–165. [Google Scholar] [CrossRef]
- Bhoday, J.; Balyasnikova, S.; Wale, A.; Brown, G. How Should Imaging Direct/Orient Management of Rectal Cancer? Clin. Colon Rectal Surg. 2017, 30, 297–312. [Google Scholar] [CrossRef]
- Shin, Y.R.; Kim, K.A.; Im, S.; Hwang, S.S.; Kim, K. Prediction of KRAS Mutation in Rectal Cancer Using MRI. Anticancer Res. 2016, 36, 4799–4804. [Google Scholar] [CrossRef]
- Jo, S.J.; Kim, S.H. Association between oncogenic RAS mutation and radiologic-pathologic findings in patients with primary rectal cancer. Quant. Imaging Med. Surg. 2019, 9, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Xu, Q.; Sun, H.; Liu, T.; Shi, K.; Wang, W. Could IVIM and ADC help in predicting the KRAS status in patients with rectal cancer? Eur. Radiol. 2018, 28, 3059–3065. [Google Scholar] [CrossRef]
- Xu, Y.; Xu, Q.; Ma, Y.; Duan, J.; Zhang, H.; Liu, T.; Li, L.; Sun, H.; Shi, K.; Xie, S.; et al. Characterizing MRI features of rectal cancers with different KRAS status. BMC Cancer 2019, 19, 1111. [Google Scholar] [CrossRef]
- Cui, Y.; Cui, X.; Yang, X.; Zhuo, Z.; Du, X.; Xin, L.; Yang, Z.; Cheng, X. Diffusion kurtosis imaging-derived histogram metrics for prediction of KRAS mutation in rectal adenocarcinoma: Preliminary findings. J. Magn. Reson. Imaging 2019, 50, 930–939. [Google Scholar] [CrossRef]
- Cui, Y.; Liu, H.; Ren, J.; Du, X.; Xin, L.; Li, D.; Yang, X.; Wang, D. Development and validation of a MRI-based radiomics signature for prediction of KRAS mutation in rectal cancer. Eur. Radiol. 2020, 30, 1948–1958. [Google Scholar] [CrossRef]
- Meng, X.; Xia, W.; Xie, P.; Zhang, R.; Li, W.; Wang, M.; Xiong, F.; Liu, Y.; Fan, X.; Xie, Y.; et al. Preoperative radiomic signature based on multiparametric magnetic resonance imaging for noninvasive evaluation of biological characteristics in rectal cancer. Eur. Radiol. 2019, 29, 3200–3209. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.S.; Kim, S.H.; Park, H.J.; Park, M.S.; Kim, K.W.; Kim, W.H.; Kim, N.K.; Lee, J.M.; Cho, H.J. Correlations of dynamic contrast-enhanced magnetic resonance imaging with morphologic, angiogenic, and molecular prognostic factors in rectal cancer. Yonsei Med. J. 2013, 54, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Horvat, N.; Veeraraghavan, H.; Pelossof, R.A.; Fernandes, M.C.; Arora, A.; Khan, M.; Marco, M.; Cheng, C.T.; Gonen, M.; Golia Pernicka, J.S.; et al. Radiogenomics of rectal adenocarcinoma in the era of precision medicine: A pilot study of associations between qualitative and quantitative MRI imaging features and genetic mutations. Eur. J. Radiol. 2019, 113, 174–181. [Google Scholar] [CrossRef]
- Huang, Z.; Zhang, W.; He, D.; Cui, X.; Tian, S.; Yin, H.; Song, B. Development and validation of a radiomics model based on T2WI images for preoperative prediction of microsatellite instability status in rectal cancer. Medicine 2020, 99. [Google Scholar] [CrossRef]
- Lubner, M.G.; Stabo, N.; Lubner, S.J.; del Rio, A.M.; Song, C.; Halberg, R.B.; Pickhardt, P.J. CT textural analysis of hepatic metastatic colorectal cancer: Pre-treatment tumor heterogeneity correlates with pathology and clinical outcomes. Abdom. Imaging 2015, 40, 2331–2337. [Google Scholar] [CrossRef] [PubMed]
- He, K.; Liu, X.; Li, M.; Li, X.; Yang, H.; Zhang, H. Noninvasive KRAS mutation estimation in colorectal cancer using a deep learning method based on CT imaging. BMC Med. Imaging 2020, 20, 59. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Dong, D.; Fang, M.; Zhu, Y.; Zang, Y.; Liu, Z.; Zhang, H.; Ying, J.; Zhao, X.; Tian, J. Can CT-based radiomics signature predict KRAS/NRAS/BRAF mutations in colorectal cancer? Eur. Radiol. 2018, 28, 2058–2067. [Google Scholar] [CrossRef]
- Taguchi, N.; Oda, S.; Yokota, Y.; Yamamura, S.; Imuta, M.; Tsuchigame, T.; Nagayama, Y.; Kidoh, M.; Nakaura, T.; Shiraishi, S.; et al. CT texture analysis for the prediction of KRAS mutation status in colorectal cancer via a machine learning approach. Eur. J. Radiol. 2019, 118, 38–43. [Google Scholar] [CrossRef]
- Badic, B.; Hatt, M.; Durand, S.; Jossic-Corcos, C.L.; Simon, B.; Visvikis, D.; Corcos, L. Radiogenomics-based cancer prognosis in colorectal cancer. Sci. Rep. 2019, 9, 9743. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.C.; Yang, Z.B.; Cheng, X.S.; Fang, X.B.; Shen, T.; Xia, C.F.; Liu, P.; Qian, H.H.; Sun, B.; Yin, Z.F.; et al. CXCL8, overexpressed in colorectal cancer, enhances the resistance of colorectal cancer cells to anoikis. Cancer Lett. 2015, 361, 22–32. [Google Scholar] [CrossRef]
- Chu, Y.; Li, J.; Zeng, Z.; Huang, B.; Zhao, J.; Liu, Q.; Wu, H.; Fu, J.; Zhang, Y.; Zhang, Y.; et al. A Novel Model Based on CXCL8-Derived Radiomics for Prognosis Prediction in Colorectal Cancer. Front. Oncol. 2020, 10. [Google Scholar] [CrossRef]
- Golia Pernicka, J.S.; Gagniere, J.; Chakraborty, J.; Yamashita, R.; Nardo, L.; Creasy, J.M.; Petkovska, I.; Do, R.R.K.; Bates, D.D.B.; Paroder, V.; et al. Radiomics-based prediction of microsatellite instability in colorectal cancer at initial computed tomography evaluation. Abdom. Radiol. 2019, 44, 3755–3763. [Google Scholar] [CrossRef]
- Fan, S.; Li, X.; Cui, X.; Zheng, L.; Ren, X.; Ma, W.; Ye, Z. Computed Tomography-Based Radiomic Features Could Potentially Predict Microsatellite Instability Status in Stage II Colorectal Cancer: A Preliminary Study. Acad. Radiol. 2019, 26, 1633–1640. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zhang, Q.; Zhao, Y.; Liu, Y.; Chen, A.; Li, X.; Wu, T.; Li, J.; Guo, Y.; Liu, A. Radiomics Analysis of Iodine-Based Material Decomposition Images With Dual-Energy Computed Tomography Imaging for Preoperatively Predicting Microsatellite Instability Status in Colorectal Cancer. Front. Oncol. 2019, 9, 1250. [Google Scholar] [CrossRef]
- Neri, E.; Del Re, M.; Paiar, F.; Erba, P.; Cocuzza, P.; Regge, D.; Danesi, R. Radiomics and liquid biopsy in oncology: The holons of systems medicine. Insights Imaging 2018, 9, 915–924. [Google Scholar] [CrossRef]
- Traverso, A.; Wee, L.; Dekker, A.; Gillies, R. Repeatability and Reproducibility of Radiomic Features: A Systematic Review. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 1143–1158. [Google Scholar] [CrossRef]
- Berenguer, R.; Pastor-Juan, M.D.R.; Canales-Vazquez, J.; Castro-Garcia, M.; Villas, M.V.; Mansilla Legorburo, F.; Sabater, S. Radiomics of CT Features May Be Nonreproducible and Redundant: Influence of CT Acquisition Parameters. Radiology 2018, 288, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Torres, H.R.; Queiros, S.; Morais, P.; Oliveira, B.; Fonseca, J.C.; Vilaca, J.L. Kidney segmentation in ultrasound, magnetic resonance and computed tomography images: A systematic review. Comput. Methods Programs Biomed. 2018, 157, 49–67. [Google Scholar] [CrossRef] [PubMed]
- Lenchik, L.; Heacock, L.; Weaver, A.A.; Boutin, R.D.; Cook, T.S.; Itri, J.; Filippi, C.G.; Gullapalli, R.P.; Lee, J.; Zagurovskaya, M.; et al. Automated Segmentation of Tissues Using CT and MRI: A Systematic Review. Acad. Radiol. 2019, 26, 1695–1706. [Google Scholar] [CrossRef] [PubMed]
- Guyon, I.; Elisseeff, A. An introduction to variable and feature selection. J. Mach. Learn. Res. 2003, 3, 1157–1182. [Google Scholar]
- Parmar, C.; Rios Velazquez, E.; Leijenaar, R.; Jermoumi, M.; Carvalho, S.; Mak, R.H.; Mitra, S.; Shankar, B.U.; Kikinis, R.; Haibe-Kains, B.; et al. Robust Radiomics Feature Quantification Using Semiautomatic Volumetric Segmentation. PLoS ONE 2014, 9, e102107. [Google Scholar] [CrossRef]
- Van Timmeren, J.E.; Leijenaar, R.T.H.; van Elmpt, W.; Wang, J.; Zhang, Z.; Dekker, A.; Lambin, P. Test-Retest Data for Radiomics Feature Stability Analysis: Generalizable or Study-Specific? Tomography 2016, 2, 361–365. [Google Scholar] [CrossRef]
- Pannucci, C.J.; Wilkins, E.G. Identifying and avoiding bias in research. Plast. Reconstr. Surg. 2010, 126, 619–625. [Google Scholar] [CrossRef]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Prz. Gastroenterol. 2019, 14, 89–103. [Google Scholar] [CrossRef]
- Lieu, C.H.; Golemis, E.A.; Serebriiskii, I.G.; Newberg, J.; Hemmerich, A.; Connelly, C.; Messersmith, W.A.; Eng, C.; Eckhardt, S.G.; Frampton, G.; et al. Comprehensive Genomic Landscapes in Early and Later Onset Colorectal Cancer. Clin. Cancer Res. 2019, 25, 5852–5858. [Google Scholar] [CrossRef]
- Sagaert, X.; Vanstapel, A.; Verbeek, S. Tumor Heterogeneity in Colorectal Cancer: What Do We Know So Far? Pathobiology 2018, 85, 72–84. [Google Scholar] [CrossRef]
- Raut, C.P.; Pawlik, T.M.; Rodriguez-Bigas, M.A. Clinicopathologic features in colorectal cancer patients with microsatellite instability. Mutat. Res. 2004, 568, 275–282. [Google Scholar] [CrossRef]
- Berntsson, J.; Svensson, M.C.; Leandersson, K.; Nodin, B.; Micke, P.; Larsson, A.H.; Eberhard, J.; Jirstrom, K. The clinical impact of tumour-infiltrating lymphocytes in colorectal cancer differs by anatomical subsite: A cohort study. Int. J. Cancer 2017, 141, 1654–1666. [Google Scholar] [CrossRef] [PubMed]
- Jakubowska, K.; Kisielewski, W.; Kanczuga-Koda, L.; Koda, M.; Famulski, W. Diagnostic value of inflammatory cell infiltrates, tumor stroma percentage and disease-free survival in patients with colorectal cancer. Oncol. Lett. 2017, 14, 3869–3877. [Google Scholar] [CrossRef] [PubMed]
- Arnadottir, S.S.; Mattesen, T.B.; Vang, S.; Madsen, M.R.; Madsen, A.H.; Birkbak, N.J.; Bramsen, J.B.; Andersen, C.L. Transcriptomic and proteomic intra-tumor heterogeneity of colorectal cancer varies depending on tumor location within the colorectum. PLoS ONE 2020, 15, e0241148. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Ng, S.B.; Chua, C.; Leow, W.Q.; Chng, J.; Liu, S.Y.; Ramnarayanan, K.; Gan, A.; Ho, D.L.; Ten, R.; et al. Multiregion ultra-deep sequencing reveals early intermixing and variable levels of intratumoral heterogeneity in colorectal cancer. Mol. Oncol. 2017, 11, 124–139. [Google Scholar] [CrossRef]
- Liang, C.; Huang, Y.; He, L.; Chen, X.; Ma, Z.; Dong, D.; Tian, J.; Liang, C.; Liu, Z. The development and validation of a CT-based radiomics signature for the preoperative discrimination of stage I-II and stage III-IV colorectal cancer. Oncotarget 2016, 7, 31401–31412. [Google Scholar] [CrossRef]
- Rizzo, S.; Botta, F.; Raimondi, S.; Origgi, D.; Fanciullo, C.; Morganti, A.G.; Bellomi, M. Radiomics: The facts and the challenges of image analysis. Eur. Radiol. Exp. 2018, 2, 36. [Google Scholar] [CrossRef]
- Bleeker, S.E.; Moll, H.A.; Steyerberg, E.W.; Donders, A.R.T.; Derksen-Lubsen, G.; Grobbee, D.E.; Moons, K.G.M. External validation is necessary in prediction research. J. Clin. Epidemiol. 2003, 56, 826–832. [Google Scholar] [CrossRef]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef]
- Kalendralis, P.; Traverso, A.; Shi, Z.; Zhovannik, I.; Monshouwer, R.; Starmans, M.P.A.; Klein, S.; Pfaehler, E.; Boellaard, R.; Dekker, A.; et al. Multicenter CT phantoms public dataset for radiomics reproducibility tests. Med. Phys. 2019, 46, 1512–1518. [Google Scholar] [CrossRef] [PubMed]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. BMJ 2015, 350, g7594. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.; Ye, Z.; Zhong, X.; Li, L.; Wang, C.; Myers, R.E.; Palazzo, J.P.; Fortuna, D.; Yan, A.; Waldman, S.A.; et al. Multiregion whole-exome sequencing of matched primary and metastatic tumors revealed genomic heterogeneity and suggested polyclonal seeding in colorectal cancer metastasis. Ann. Oncol. 2017, 28, 2135–2141. [Google Scholar] [CrossRef] [PubMed]
| Year | Author | Study | N | Study Population | Aim | Segmentation | Radiomic Features | Main Results | Internal Validation | External Validation | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | Arslan | R | 83 | All stages | Prediction of the KRAS status | M | SUVmax | KRAS mutation mean SUVmax (24.0 ± 9.0); KRAS wild type mean SUVmax (17.7 ± 8.2) | N | N | Coexistence of KRAS mutation with higher SUVmax is a negative prognostic factor |
| 2020 | Popovic | R | 37 | Stage IV | Prediction of KRAS status in CRLM | M/A | SUV metrics corrected for tumor-to-blood standard uptake ratio (SUR) and partial volume effect (PVE) | SUV metrics(AUC 0.69–0.72); SUR metrics(AUC 0.73–0.75) | N | N | Corrected PET standard uptake values (SUV) correlated KRAS status |
| 2019 | Chen | R | 74 | All stages | Association between radiomics and genetic mutations | M | 63 radiomic features | KRAS predictor histograms (OR 1.99) and contrast (OR 1.52) from GLCM predictors; SRLGE associated TP53 (OR 243); LGZE predictor APC (OR < 0.001) | N | N | PET/CT-derived radiomics can determine KRAS, TP53, and APC genetic alterations |
| 2018 | Mao | R | 49 | Stage IV | Prediction of KRAS status in CRLM | M | Maximum standardized uptake value (SUVmax); change of SUVmax (DSUVmax); retention index (RI) | SUVearly AUC 0.694 (p = 0.002, 95% CI 0.582–0.807); SUVdelayed AUC 0.760 (p < 0.001, 95% CI 0.658–0.862); DSUVmax AUC 0.757 (p < 0.001, 95% CI 0.654–0.861); RI (%) AUC 0.684 (p = 0.003, 95% CI 0.571–0.797) | N | N | KRAS mutations predictors in CRLM: early and delayed SUVmax, DSUVmax, RI |
| 2017 | Oner | R | 55 | Na | Prediction of the KRAS status | A | SUVmax, SUVmean, MTV and TLG | SUVmax (AUC 0.54, OR 0.08, 95% CI, 0.38–0.7 p = 0.6); MTV (AUC 0.54, OR 0.08, 95% CI, 0.38–0.6 p = 0.6) | N | N | No significant association between KRAS gene mutations and SUVmax, MTV, TLG, NLR, PLR, CEA, CA 19-9 values |
| 2016 | Lee | P | 179 | All stages | Predict the KRAS status depending on C-reactive protein (CRP) levels | M/A | Maximum standardized uptake value (SUVmax), peak standardized uptake value (SUVpeak), metabolic tumor volume | None of the PET/CT-related parameters showed significant KRAS prediction; In normal CRP group, mutated KRAS associated with higher SUVmax (OR, 3.3; 95% CI, 1.4–7.4), SUVpeak (OR, 3.8; 95% CI, 1.5–9.3) | N | N | Higher SUVmax and SUVpeak values in KRAS mutated patients |
| 2016 | Lovinfosse | R | 151 | All stages | Prediction of KRAS, NRAS, BRAF | M | Standardized uptake values (SUVs), volume-based parameters and texture analysis | SUVcov highest AUC (0.65), sensitivity 56%, specificity 64%; SUVmax AUC 0.65 and sensibility 69% specificity 52% | N | N | The accuracy of 18F-FDG PET/CT quantitative metrics could not play a clinical role |
| 2015 | Chen | R | 103 | All stages | Prediction of TP53, KRAS, APC, BRAF, and PIK3CA | M | SUVmax, and various thresholds of metabolic tumor volume, total lesion glycolysis, and PET/CT-based tumor width (TW) were measured | SUVmax predicting TP53, OR 1.28 (95% CI, 1.01–1.61); TW 40% predicting KRAS, OR 1.15 (95% CI, 1.06–1.24) | N | N | Increased SUVmax and TW40% associated with TP53 and KRAS mutations |
| 2015 | Kawada | R | 55 | Stage IV | Prediction of the KRAS status | M | SUVmax | SUVmax (cutoff value 6.0) in tumors larger than 10 mm OR 0.78 (95% CI, 0.61–0.99) predicted KRAS status | N | N | 18F-FDG accumulation into metastatic CRC was associated with KRAS status |
| 2014 | Chen | R | 121 | All stages | Prediction of the KRAS status | A | SUVmax; metabolic tumor volume, total lesion glycolysis, PET/CT-based tumor width | SUVmax OR 1.23 (95% CI, 1.01–1.52); TW 40% OR 1.15 (95% CI, 1.02–1.30). | N | N | SUVmax and TW40% were associated in CRC with KRAS mutations |
| 2014 | Krikelis | R | 44 | Stage IV | Prediction of the KRAS status | M | SUVmax | No correlation of SUVmax with KRAS status | N | N | No statistically significant correlation between SUVmax values and KRAS mutation status or GLUT1 mRNA levels. |
| 2014 | Miles | P | 33 | All stages | Prediction of the KRAS status | M | SUVmax, mean of positive pixels [MPP]), blood flow (BF) | The true-positive rate, false-positive rate, and accuracy (95% confidence intervals) of the decision tree were 82.4% (63.9%–93.9%), 0% (0%–10.4%), and 90.1% (79.2%–96.0%), respectively. | Y | N | Combined measurements of tumor 18F-FDG uptake, CT texture, and perfusion has the potential to identify KRAS mutations |
| 2012 | Kawada | R | 51 | All stages | KRAS/BRAF mutations affect FDG accumulation in CRC | M | Radiomic features | KRAS and BRAF mutations correlated with SUVmax (OR, 1.17; 95% CI, 1.03–1.33), TLR (OR, 1.40; 95% CI, 1.08–1.80) | N | N | FDG accumulation was higher in CRC with KRAS/BRAF mutations |
| Year | Author | Study | N | Study Population | Aim | Segmentation | Radiomic Features | Main Results | Internal Validation | External Validation | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | Wang | R | 306 | Na | Deep model to independently predict the genetic status of KRAS mutations | M | DL model | MBCAM2 model- accuracy 90.50%, sens 92.79%, spec 87.64%, and AUC 96.00% | Y | N | Multi-branch cross attention model outperforms all the methods of DL |
| 2020 | Oh | R | 60 | All stages | Prediction of KRAS status | M | Three radiomic model | sens (84%), spec (80%), accuracy values (81.7%), AUC (0.884) of the decision tree for the whole dataset | Y | N | Three MRI imaging features that could predict KRAS status |
| 2020 | Cui | R | 304 + 86 | Na | Prediction of KRAS status | M | Seven radiomics features | Training dataset AUC of 0.722 (95% CI, 0.654–0.790); internal validation AUC 0.682 (95% CI, 0.569–0.794); external validation AUC 0.714 (95% CI, 0.602–0.827) | Y | Y | Moderate performance to predict KRAS status |
| 2019 | Horvat | R | 65 | Na | Correlations between genetic mutations and radiomics | M | Thirty-four texture features | No associations between clusters/qualitative features and gene mutations (except for PTPRT) | N | N | Associations between quantitative features and genetic mutations; pas de correlations between qualitative features and genetic mutations |
| 2019 | Cui | R | 148 | Exclusion Stage IV | Prediction of the status of KRAS | M | D, K, and apparent diffusion coefficient (ADC) values | K75th AUC value of 0.871 (0.806–0.920) sensitivity 81.43%, specificity78.21%, positive predictive value 77.03%, negative predictive value 82.43% | N | N | DKI metrics with whole-tumor volume histogram analysis is associated with KRAS mutation |
| 2019 | XU | R | 158 | Na | Prediction of KRAS status | M | Mean, Variance, Skewness, Entropy, gray-level nonuniformity, run length nonuniformity | texture features AUC (0.703–0.813); ADC values (AUC 0.682, 95% CI: 0.564–0.801), sensitivity (66.67) and specificity (62.12%) | N | N | Mean values (Mean, Variance, Skewness, Entropy, gray-level nonuniformity, run-length nonuniformity) higher in KRASmt group |
| 2018 | JO | R | 75 | Na | Prediction of KRAS status | M | Tumor length, ADC, relative contrast enhancement | The higher ratio of axial to LTL in the KRAS-mutant group AUC 0.640 (95% CI, 0.520 to 0.747, p = 0.0292), maximum accuracy of 64% | N | N | Ratio of axial to longitudinal tumor lengths predicted KRAS mutation (accuracy of 64%) |
| 2018 | XU | R | 51 | Na | Prediction of KRAS status | M | Max-ADC, Min-ADC, Mean-ADC, pure diffusion, perfusion fraction, pseudo-diffusion coefficient | Kras status AUC values of Max-ADC, Min- ADC, Mean-ADC, D, f and D* were 0.695, 0.604, 0.756, 0.701, 0.599 and 0.710 | N | N | Lower Max-ADC, Mean-ADC and D and higher D values observed in the KRAS mutant group |
| 2018 | Meng | R | 345 | Na | Radiomic model’s prediction of biological characteristics | M | DL model | Model Ki-67 (AUC 0.699 95% CI, 0.611–0.786); HER-2 (AUC 0.696, 95% CI, 0.610–0.782) Ki-67; KRAS-2 (AUC0.651, 95% CI, 0.539–0.763), | Y | N | Radiomic signatures correlated to HER-2, KRAS-2 gene status |
| 2016 | Shin | R | 275 | All stages | Prediction of KRAS status | M | Axial tumor length, ratio of the axial to the longitudinal tumor dimensions | KRASm tumors- longer axial length, larger ratio of the axial to the longitudinal dimensions. | N | N | KRAS status associated with gross tumor pattern, axial length, ratio of the axial to the longitudinal dimensions of the tumor |
| 2013 | Hong | R | 29 | Na | correlations between parameters of dynamic contrast-enhanced magnetic resonance imaging and prognostic factors | M | Steepest slope (SLP), time to peak (Tp), relative enhancement during a rapid rise (Erise), maximal enhancement (Emax) | Erise was significantly correlated with N stage, and Tp was significantly correlated with histologic grade | N | N | no significant correlations between DCE-MRI parameters and K-ras mutation, microsatellite instability |
| Year | Author | Study | N | Study Population | Aim | Segmentation | Radiomic Features | Main Results | Internal Validation | External Validation | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | HE | R | 117 + 40 | All | Predictive performance by using residual neural network (ResNet) to estimate the KRAS status | M | 4 features radiomics model | Radiomics model training cohort, AUC 0.945 (sens: 0.75; spec: 0.94); testing cohort, AUC 0.818 (sens: 0.70; spec: 0.85). ResNet model AUC 0.90 testing cohort | Y | N | Better prediction of Kras status by residual neural network than radiomics model |
| 2020 | CHU | R | 99 + 42 | All | Relationship among prognosis, radiomics features, and gene expression | M | 12 radiomics features | Radiomic model training cohort AUC 0.829 (95% CI: 0.750–0.908) testing cohort AUC 0.727 (95% CI: 0.570–0.884) | Y | N | Radiomics model reflected by CXCL8 combined with tumor stage information predict the prognosis |
| 2020 | Negreros-Osuna | R | 145 | Stage IV | Prediction of BRAF mutation | M | Standard deviation (SD), the mean value of positive pixels (MPP) | Lower SD 22.31 (95% CI: 20.66, 24.62) and MPP 51.54 (95% CI: 47.14, 58.99) in BRAF mutant tumors | N | N | Radiomics texture features predictors of BRAF mutation status and 5-year OS |
| 2020 | González-Castro | R | 47 | All | Prediction of KRAS status | M | Radiomic model (second-order features) | Neural Networks model sens of 88.9%, spec 75.0%, accuracy of 83% | Y | N | Prediction of KRAS status in CRC |
| 2020 | Dercle | R | 667 | Stage IV (CRYSTAL trial (NCT00154102)) | Predict tumor sensitiveness to FOLFIRI ± cetuximab. | M | 4 features radiomics model | AUC 0.80 (95% CI: 0.69–0.94) sens 0.80, and spec 0.78); p < 0.001) | Y | N | Performance of the signature outperformed both KRAS-mutational status at baseline |
| 2019 | Pernicka | R | 139 + 59 | Stage II and III | Prediction of (MSI) status | M | 40 radiomic features | AUC of 0.80 for the training set and 0.79 for the test set (spec = 96.8% and 92.5%, respectively) | Y | N | The combined model performed slightly better than the other models |
| 2019 | Taguchi | R | 40 | Stage II-IV | Prediction of KRAS status | M | 14 CT radiomics et SUV max | Multivariate support vector machine CT radiomics model AUC of 0.82 superior compared to the SUVmax. | N | N | CT texture analysis was superior to the SUVmax for predicting the KRAS mutation status |
| 2019 | Wu | R | 102 | Na | Prediction of (MSI) status | M | 6 radiomics features | Training set AUC 0.961 (accuracy: 0.875; sens: 1.000; spec: 0.812); testing set AUC of 0.875 (accuracy: 0.788; sens: 0.909; spec: 0.727) | Y | N | Radiomics analysis of iodine-based material decomposition predict MSI status |
| 2019 | Fan | R | 119 | Stage II | Prediction of (MSI) status | Semiautomatic | 6 radiomics features | Radiomic model AUC = 0.688; accuracy = 0.713; sens = 0.517; spec = 0.858; clinical model 0.598 AUC value, 0.632accuracy, 0.371 sens, and 0.825 spec; combined model AUC 0.752 (accuracy = 0.765; sens = 0.663; spec = 0.842). | N | N | Better detection of MSI status with combined clinical and radiomics feature model than clinical/radiomics alone |
| 2019 | Badic | R | 64 | All | Prognostic value of gene expression and radiomics | M | Shape, second and third order texture features | PFS Cox model combining Stage 3, ABCC2 and EntropyGLMC HR 22.8 95% CI 3.7 to 141 p < 0.0001 OS Cox model with Ratio and ALDH1A HR 8.4 95% CI 3.4 to 20.6 p = 0.0005 | N | N | Model combining CE-CT radiomics, gene expression, histopathological examination could provide higher prognostic stratification power |
| 2018 | YANG | R | 61 + 56 | All | Predict KRAS/NRAS/BRAF mutations | M | 3 radiomics features | Testing cohort AUC 0.869, sens 0.757, and spec 0.833; Validation cohort AUC 0.829, sens 0.686, spec 0.857 | Y | N | Prediction of KRAS/NRAS/BRAF mutations |
| 2015 | Lubner | R | 77 | Stage IV | CT texture features relate to pathologic features and clinical outcomes | M | First class radiomics | Skewness was negatively associated KRAS mutation (p = 0.02). | N | N | MPP, SD, correlates overall survival |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badic, B.; Tixier, F.; Cheze Le Rest, C.; Hatt, M.; Visvikis, D. Radiogenomics in Colorectal Cancer. Cancers 2021, 13, 973. https://doi.org/10.3390/cancers13050973
Badic B, Tixier F, Cheze Le Rest C, Hatt M, Visvikis D. Radiogenomics in Colorectal Cancer. Cancers. 2021; 13(5):973. https://doi.org/10.3390/cancers13050973
Chicago/Turabian StyleBadic, Bogdan, Florent Tixier, Catherine Cheze Le Rest, Mathieu Hatt, and Dimitris Visvikis. 2021. "Radiogenomics in Colorectal Cancer" Cancers 13, no. 5: 973. https://doi.org/10.3390/cancers13050973
APA StyleBadic, B., Tixier, F., Cheze Le Rest, C., Hatt, M., & Visvikis, D. (2021). Radiogenomics in Colorectal Cancer. Cancers, 13(5), 973. https://doi.org/10.3390/cancers13050973