Genotyping and Characterization of HPV Status, Hypoxia, and Radiosensitivity in 22 Head and Neck Cancer Cell Lines
Abstract
Simple Summary
Abstract
1. Introduction
2. Results
2.1. HNSCC Cell Line Panel Characteristics and Genotyping
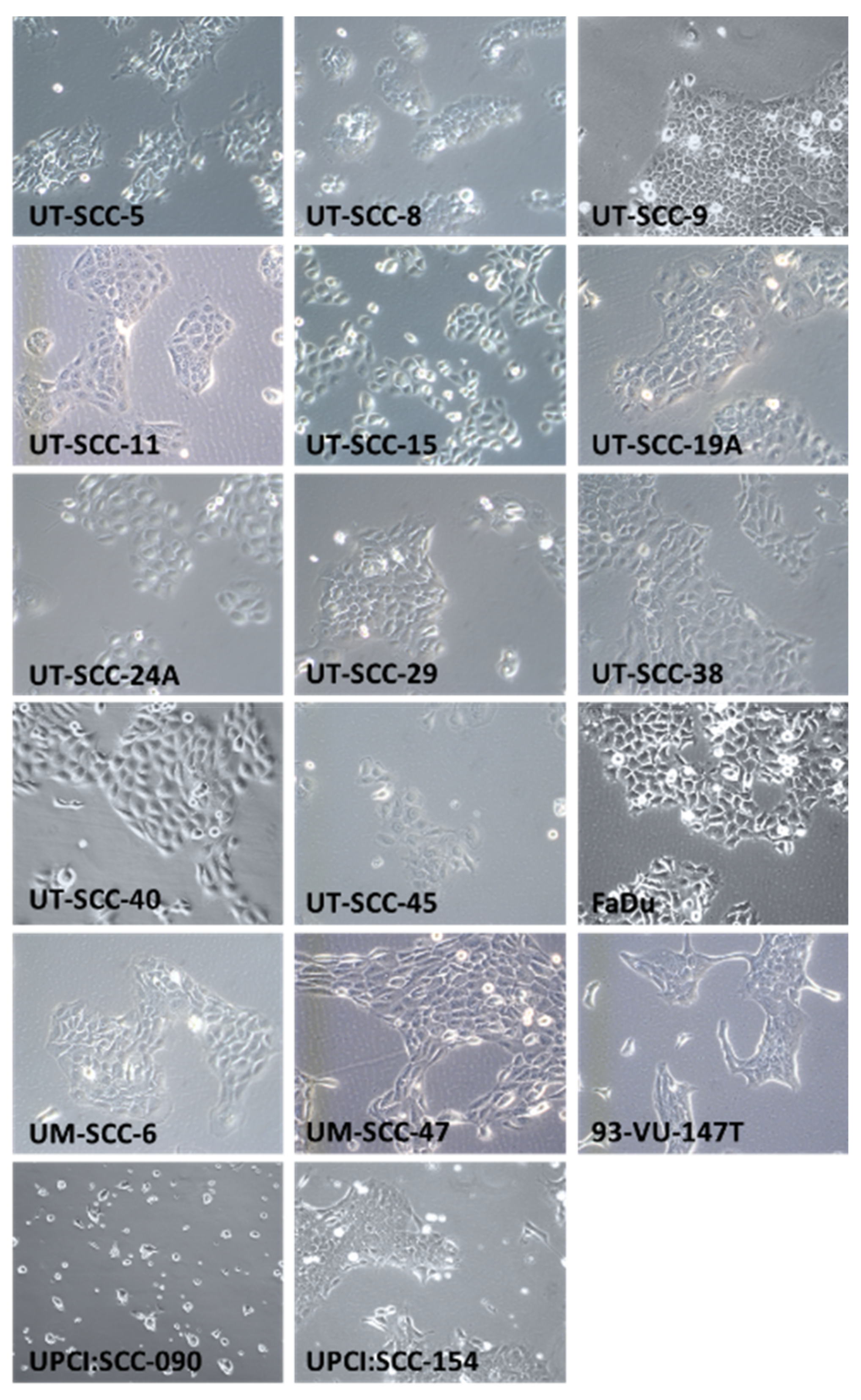
2.2. HNSCC Cell Line Morphology
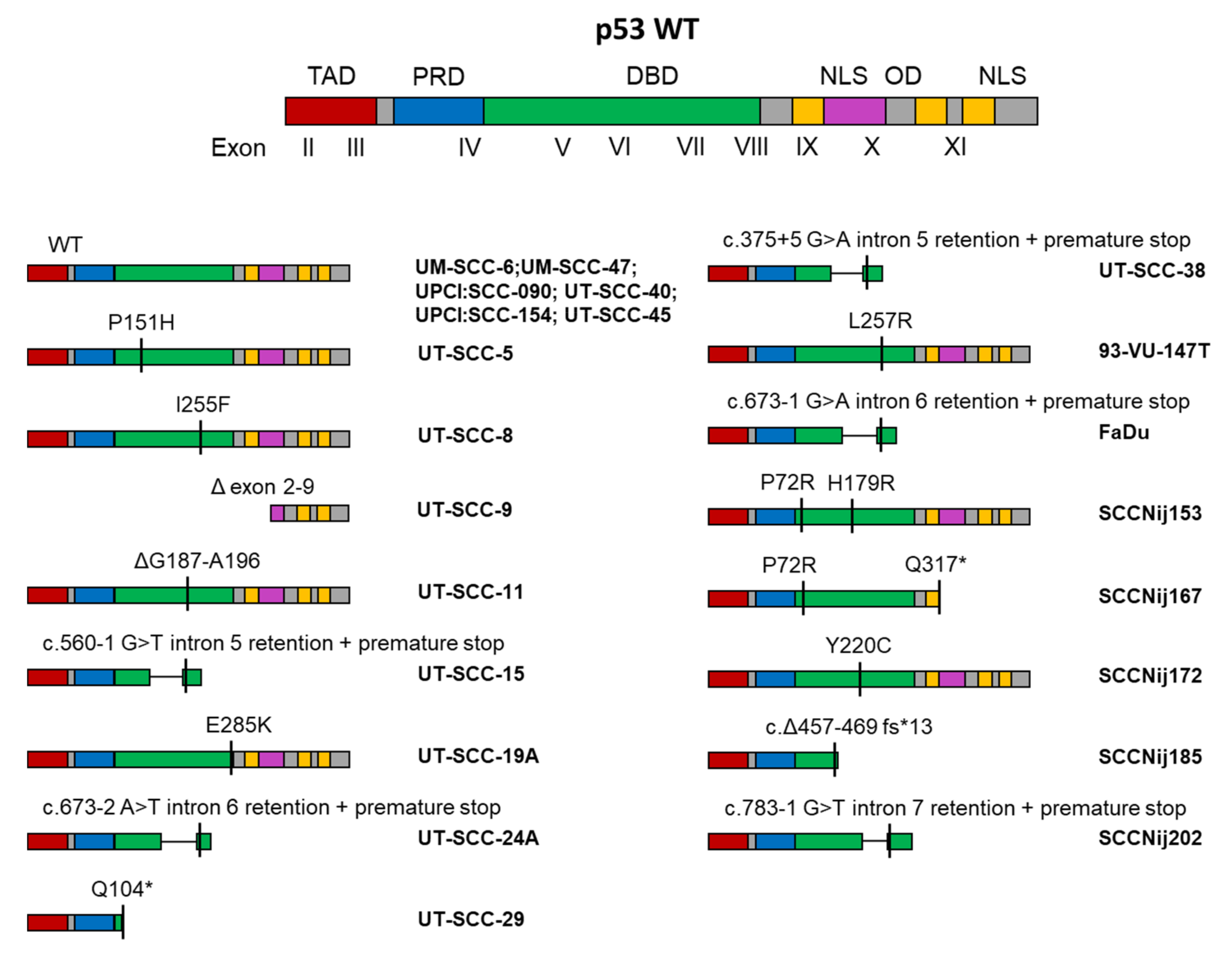
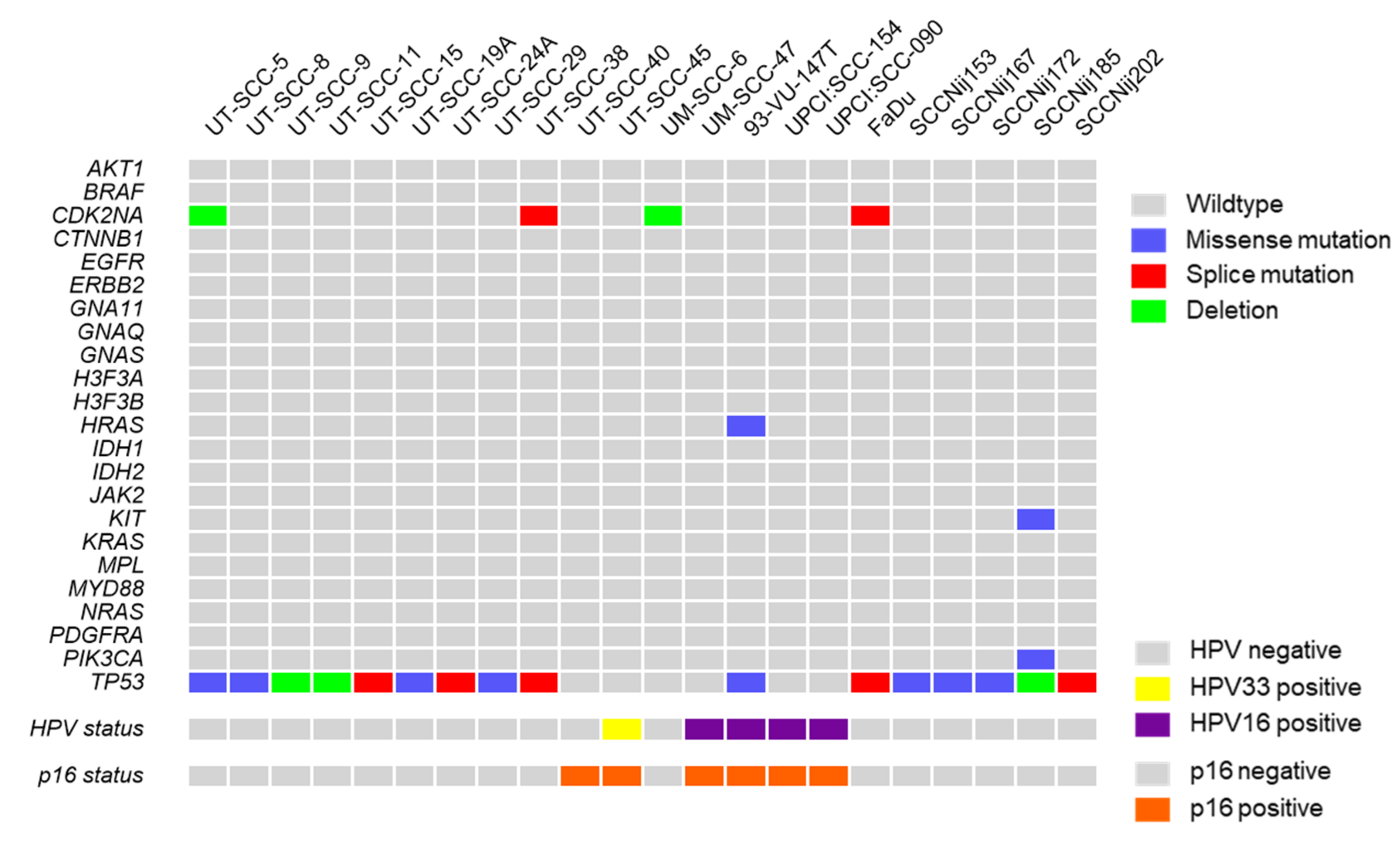
2.3. Mutations in HNSCC Cell Lines
2.4. HPV and p16 Status
2.5. Radiosensitivity and Hypoxia Sensitivity
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. Microscopy
4.3. Genomic DNA Extraction
4.4. Mutation Analysis
4.5. STR Profiling
4.6. Colony Forming Assays
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ang, K.K.; Harris, J.; Wheeler, R.; Weber, R.; Rosenthal, D.I.; Nguyen-Tan, P.F.; Westra, W.H.; Chung, C.H.; Jordan, R.C.; Lu, C.; et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N. Engl. J. Med. 2010, 363, 24–35. [Google Scholar] [CrossRef]
- Chow, L.Q.M. Head and Neck Cancer. N. Engl. J. Med. 2020, 382, 60–72. [Google Scholar] [CrossRef]
- Chow, L.Q.M.; Haddad, R.; Gupta, S.; Mahipal, A.; Mehra, R.; Tahara, M.; Berger, R.; Eder, J.P.; Burtness, B.; Lee, S.H.; et al. Antitumor Activity of Pembrolizumab in Biomarker-Unselected Patients With Recurrent and/or Metastatic Head and Neck Squamous Cell Carcinoma: Results From the Phase Ib KEYNOTE-012 Expansion Cohort. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2016, 34, 3838–3845. [Google Scholar] [CrossRef] [PubMed]
- Burtness, B.; Harrington, K.J.; Greil, R.; Soulieres, D.; Tahara, M.; de Castro, G., Jr.; Psyrri, A.; Baste, N.; Neupane, P.; Bratland, A.; et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): A randomised, open-label, phase 3 study. Lancet 2019, 394, 1915–1928. [Google Scholar] [CrossRef]
- Cramer, J.D.; Burtness, B.; Le, Q.T.; Ferris, R.L. The changing therapeutic landscape of head and neck cancer. Nat. Rev. Clin. Oncol. 2019, 16, 669–683. [Google Scholar] [CrossRef] [PubMed]
- Stephen, J.K.; Divine, G.; Chen, K.M.; Chitale, D.; Havard, S.; Worsham, M.J. Significance of p16 in Site-specific HPV Positive and HPV Negative Head and Neck Squamous Cell Carcinoma. Cancer Clin. Oncol. 2013, 2, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Mehanna, H.; Beech, T.; Nicholson, T.; El-Hariry, I.; McConkey, C.; Paleri, V.; Roberts, S. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer--systematic review and meta-analysis of trends by time and region. Head Neck 2013, 35, 747–755. [Google Scholar] [CrossRef]
- Lassen, P.; Primdahl, H.; Johansen, J.; Kristensen, C.A.; Andersen, E.; Andersen, L.J.; Evensen, J.F.; Eriksen, J.G.; Overgaard, J.; Danish, H.; et al. Impact of HPV-associated p16-expression on radiotherapy outcome in advanced oropharynx and non-oropharynx cancer. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2014, 113, 310–316. [Google Scholar] [CrossRef]
- Lin, C.J.; Grandis, J.R.; Carey, T.E.; Gollin, S.M.; Whiteside, T.L.; Koch, W.M.; Ferris, R.L.; Lai, S.Y. Head and neck squamous cell carcinoma cell lines: Established models and rationale for selection. Head Neck 2007, 29, 163–188. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Sano, D.; Pickering, C.R.; Jasser, S.A.; Henderson, Y.C.; Clayman, G.L.; Sturgis, E.M.; Ow, T.J.; Lotan, R.; Carey, T.E.; et al. Assembly and initial characterization of a panel of 85 genomically validated cell lines from diverse head and neck tumor sites. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2011, 17, 7248–7264. [Google Scholar] [CrossRef]
- Johansson, N.; Airola, K.; Grenman, R.; Kariniemi, A.L.; Saarialho-Kere, U.; Kahari, V.M. Expression of collagenase-3 (matrix metalloproteinase-13) in squamous cell carcinomas of the head and neck. Am. J. Pathol. 1997, 151, 499–508. [Google Scholar] [PubMed]
- Soukka, T.; Salmi, M.; Joensuu, H.; Hakkinen, L.; Sointu, P.; Koulu, L.; Kalimo, K.; Klemi, P.; Grenman, R.; Jalkanen, S. Regulation of CD44v6-containing isoforms during proliferation of normal and malignant epithelial cells. Cancer Res. 1997, 57, 2281–2289. [Google Scholar] [PubMed]
- Lansford, C.D.; Grenman, R.; Bier, H.; Somers, K.D.; Kim, S.Y.; Whiteside, T.L.; Clayman, G.L.; Welkoborsky, H.J.; Carey, T.E. Head and neck cancers. In Human Cell Culture; Cancer Cell Lines, Part 2; Masters, J.R., Palsson, B., Eds.; Kluwer Academic Publishers: Dordrecht, The Netherland, 1999; Volume 2, pp. 185–255. [Google Scholar]
- Elomaa, L.; Joensuu, H.; Kulmala, J.; Klemi, P.; Grenman, R. Squamous cell carcinoma is highly sensitive to taxol, a possible new radiation sensitizer. Acta Oto Laryngol. 1995, 115, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Grenman, R.; Carey, T.E.; McClatchey, K.D.; Wagner, J.G.; Pekkola-Heino, K.; Schwartz, D.R.; Wolf, G.T.; Lacivita, L.P.; Ho, L.; Baker, S.R.; et al. In vitro radiation resistance among cell lines established from patients with squamous cell carcinoma of the head and neck. Cancer 1991, 67, 2741–2747. [Google Scholar] [CrossRef]
- Akervall, J.; Guo, X.; Qian, C.N.; Schoumans, J.; Leeser, B.; Kort, E.; Cole, A.; Resau, J.; Bradford, C.; Carey, T.; et al. Genetic and expression profiles of squamous cell carcinoma of the head and neck correlate with cisplatin sensitivity and resistance in cell lines and patients. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2004, 10, 8204–8213. [Google Scholar] [CrossRef]
- Steenbergen, R.D.; Hermsen, M.A.; Walboomers, J.M.; Joenje, H.; Arwert, F.; Meijer, C.J.; Snijders, P.J. Integrated human papillomavirus type 16 and loss of heterozygosity at 11q22 and 18q21 in an oral carcinoma and its derivative cell line. Cancer Res. 1995, 55, 5465–5471. [Google Scholar]
- White, J.S.; Weissfeld, J.L.; Ragin, C.C.; Rossie, K.M.; Martin, C.L.; Shuster, M.; Ishwad, C.S.; Law, J.C.; Myers, E.N.; Johnson, J.T.; et al. The influence of clinical and demographic risk factors on the establishment of head and neck squamous cell carcinoma cell lines. Oral Oncol. 2007, 43, 701–712. [Google Scholar] [CrossRef]
- Azrak, R.G.; Cao, S.; Slocum, H.K.; Toth, K.; Durrani, F.A.; Yin, M.B.; Pendyala, L.; Zhang, W.; McLeod, H.L.; Rustum, Y.M. Therapeutic synergy between irinotecan and 5-fluorouracil against human tumor xenografts. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2004, 10, 1121–1129. [Google Scholar] [CrossRef]
- Rangan, S.R. A new human cell line (FaDu) from a hypopharyngeal carcinoma. Cancer 1972, 29, 117–121. [Google Scholar] [CrossRef]
- Hoeben, B.A.; Starmans, M.H.; Leijenaar, R.T.; Dubois, L.J.; van der Kogel, A.J.; Kaanders, J.H.; Boutros, P.C.; Lambin, P.; Bussink, J. Systematic analysis of 18F-FDG PET and metabolism, proliferation and hypoxia markers for classification of head and neck tumors. BMC Cancer 2014, 14, 130. [Google Scholar] [CrossRef]
- Brenner, J.C.; Graham, M.P.; Kumar, B.; Saunders, L.M.; Kupfer, R.; Lyons, R.H.; Bradford, C.R.; Carey, T.E. Genotyping of 73 UM-SCC head and neck squamous cell carcinoma cell lines. Head Neck 2010, 32, 417–426. [Google Scholar] [CrossRef]
- Kalu, N.N.; Mazumdar, T.; Peng, S.; Shen, L.; Sambandam, V.; Rao, X.; Xi, Y.; Li, L.; Qi, Y.; Gleber-Netto, F.O.; et al. Genomic characterization of human papillomavirus-positive and -negative human squamous cell cancer cell lines. Oncotarget 2017, 8, 86369–86383. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.; Abba, M.C.; Molinolo, A.A.; Vitale-Cross, L.; Wang, Z.; Zaida, M.; Delic, N.C.; Samuels, Y.; Lyons, J.G.; Gutkind, J.S. The head and neck cancer cell oncogenome: A platform for the development of precision molecular therapies. Oncotarget 2014, 5, 8906–8923. [Google Scholar] [CrossRef]
- Jamieson, S.M.; Tsai, P.; Kondratyev, M.K.; Budhani, P.; Liu, A.; Senzer, N.N.; Chiorean, E.G.; Jalal, S.I.; Nemunaitis, J.J.; Kee, D.; et al. Evofosfamide for the treatment of human papillomavirus-negative head and neck squamous cell carcinoma. JCI Insight 2018, 3. [Google Scholar] [CrossRef]
- Yu, M.; Selvaraj, S.K.; Liang-Chu, M.M.; Aghajani, S.; Busse, M.; Yuan, J.; Lee, G.; Peale, F.; Klijn, C.; Bourgon, R.; et al. A resource for cell line authentication, annotation and quality control. Nature 2015, 520, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Bukvic, N.; Gentile, M.; Susca, F.; Fanelli, M.; Serio, G.; Buonadonna, L.; Capurso, A.; Guanti, G. Sex chromosome loss, micronuclei, sister chromatid exchange and aging: A study including 16 centenarians. Mutat. Res. 2001, 498, 159–167. [Google Scholar] [CrossRef]
- Van Dyke, D.L.; Worsham, M.J.; Benninger, M.S.; Krause, C.J.; Baker, S.R.; Wolf, G.T.; Drumheller, T.; Tilley, B.C.; Carey, T.E. Recurrent cytogenetic abnormalities in squamous cell carcinomas of the head and neck region. Genes Chromosomes Cancer 1994, 9, 192–206. [Google Scholar] [CrossRef]
- Briske-Anderson, M.J.; Finley, J.W.; Newman, S.M. The influence of culture time and passage number on the morphological and physiological development of Caco-2 cells. Proc. Soc. Exp. Biol. Med. Soc. Exp. Biol. Med. 1997, 214, 248–257. [Google Scholar] [CrossRef]
- Wenger, S.L.; Senft, J.R.; Sargent, L.M.; Bamezai, R.; Bairwa, N.; Grant, S.G. Comparison of established cell lines at different passages by karyotype and comparative genomic hybridization. Biosci. Rep. 2004, 24, 631–639. [Google Scholar] [CrossRef]
- Puck, T.T.; Marcus, P.I. Action of x-rays on mammalian cells. J. Exp. Med. 1956, 103, 653–666. [Google Scholar] [CrossRef] [PubMed]
- Eijkelenboom, A.; Kamping, E.J.; Kastner-van Raaij, A.W.; Hendriks-Cornelissen, S.J.; Neveling, K.; Kuiper, R.P.; Hoischen, A.; Nelen, M.R.; Ligtenberg, M.J.; Tops, B.B. Reliable Next-Generation Sequencing of Formalin-Fixed, Paraffin-Embedded Tissue Using Single Molecule Tags. J. Mol. Diagn. JMD 2016, 18, 851–863. [Google Scholar] [CrossRef]
- van Harten, A.M.; Poell, J.B.; Buijze, M.; Brink, A.; Wells, S.I.; Rene Leemans, C.; Wolthuis, R.M.F.; Brakenhoff, R.H. Characterization of a head and neck cancer-derived cell line panel confirms the distinct TP53-proficient copy number-silent subclass. Oral Oncol. 2019, 98, 53–61. [Google Scholar] [CrossRef]
- Servomaa, K.; Kiuru, A.; Grenman, R.; Pekkola-Heino, K.; Pulkkinen, J.O.; Rytomaa, T. p53 mutations associated with increased sensitivity to ionizing radiation in human head and neck cancer cell lines. Cell Prolif. 1996, 29, 219–230. [Google Scholar] [CrossRef]
- Eicheler, W.; Zips, D.; Dorfler, A.; Grenman, R.; Baumann, M. Splicing mutations in TP53 in human squamous cell carcinoma lines influence immunohistochemical detection. J. Histochem. Cytochem. Off. J. Histochem. Soc. 2002, 50, 197–204. [Google Scholar] [CrossRef]
- Mandic, R.; Schamberger, C.J.; Muller, J.F.; Geyer, M.; Zhu, L.; Carey, T.E.; Grenman, R.; Dunne, A.A.; Werner, J.A. Reduced cisplatin sensitivity of head and neck squamous cell carcinoma cell lines correlates with mutations affecting the COOH-terminal nuclear localization signal of p53. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2005, 11, 6845–6852. [Google Scholar] [CrossRef] [PubMed]
- Bradford, C.R.; Zhu, S.; Ogawa, H.; Ogawa, T.; Ubell, M.; Narayan, A.; Johnson, G.; Wolf, G.T.; Fisher, S.G.; Carey, T.E. P53 mutation correlates with cisplatin sensitivity in head and neck squamous cell carcinoma lines. Head Neck 2003, 25, 654–661. [Google Scholar] [CrossRef]
- Ferris, R.L.; Martinez, I.; Sirianni, N.; Wang, J.; Lopez-Albaitero, A.; Gollin, S.M.; Johnson, J.T.; Khan, S. Human papillomavirus-16 associated squamous cell carcinoma of the head and neck (SCCHN): A natural disease model provides insights into viral carcinogenesis. Eur. J. Cancer 2005, 41, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Dohmen, A.J.C.; Qiao, X.; Duursma, A.; Wijdeven, R.H.; Lieftink, C.; Hageman, F.; Morris, B.; Halonen, P.; Vens, C.; van den Brekel, M.W.M.; et al. Identification of a novel ATM inhibitor with cancer cell specific radiosensitization activity. Oncotarget 2017, 8, 73925–73937. [Google Scholar] [CrossRef] [PubMed]
- López, I.; Oliveira, L.P.; Tucci, P.; Álvarez-Valín, F.; Coudry, R.A.; Marín, M. Different mutation profiles associated to P53 accumulation in colorectal cancer. Gene 2012, 499, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Gottgens, E.L.; van den Heuvel, C.N.; de Jong, M.C.; Kaanders, J.H.; Leenders, W.P.; Ansems, M.; Bussink, J.; Span, P.N. ACLY (ATP Citrate Lyase) Mediates Radioresistance in Head and Neck Squamous Cell Carcinomas and is a Novel Predictive Radiotherapy Biomarker. Cancers 2019, 11, 1971. [Google Scholar] [CrossRef]
- Gottgens, E.L.; Bussink, J.; Leszczynska, K.B.; Peters, H.; Span, P.N.; Hammond, E.M. Inhibition of CDK4/CDK6 Enhances Radiosensitivity of HPV Negative Head and Neck Squamous Cell Carcinomas. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, 548–558. [Google Scholar] [CrossRef] [PubMed]
- Dok, R.; Glorieux, M.; Holacka, K.; Bamps, M.; Nuyts, S. Dual role for p16 in the metastasis process of HPV positive head and neck cancers. Mol. Cancer 2017, 16, 113. [Google Scholar] [CrossRef] [PubMed]
- Stegeman, H.; Kaanders, J.H.; Wheeler, D.L.; van der Kogel, A.J.; Verheijen, M.M.; Waaijer, S.J.; Iida, M.; Grenman, R.; Span, P.N.; Bussink, J. Activation of AKT by hypoxia: A potential target for hypoxic tumors of the head and neck. BMC Cancer 2012, 12, 463. [Google Scholar] [CrossRef] [PubMed]
- Gillison, M.L.; Chaturvedi, A.K.; Anderson, W.F.; Fakhry, C. Epidemiology of Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 3235–3242. [Google Scholar] [CrossRef]
- Bryant, H.E.; Schultz, N.; Thomas, H.D.; Parker, K.M.; Flower, D.; Lopez, E.; Kyle, S.; Meuth, M.; Curtin, N.J.; Helleday, T. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 2005, 434, 913–917. [Google Scholar] [CrossRef] [PubMed]
- Tutt, A.; Robson, M.; Garber, J.E.; Domchek, S.M.; Audeh, M.W.; Weitzel, J.N.; Friedlander, M.; Arun, B.; Loman, N.; Schmutzler, R.K.; et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: A proof-of-concept trial. Lancet 2010, 376, 235–244. [Google Scholar] [CrossRef]
- Cancer Genome Atlas, N. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015, 517, 576–582. [Google Scholar] [CrossRef]
- Lane, D.P. Cancer. p53, guardian of the genome. Nature 1992, 358, 15–16. [Google Scholar] [CrossRef]
- Surget, S.; Khoury, M.P.; Bourdon, J.C. Uncovering the role of p53 splice variants in human malignancy: A clinical perspective. Oncotargets Ther. 2013, 7, 57–68. [Google Scholar] [CrossRef]
- Westra, W.H.; Taube, J.M.; Poeta, M.L.; Begum, S.; Sidransky, D.; Koch, W.M. Inverse relationship between human papillomavirus-16 infection and disruptive p53 gene mutations in squamous cell carcinoma of the head and neck. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008, 14, 366–369. [Google Scholar] [CrossRef]
- Kropveld, A.; Rozemuller, E.H.; Leppers, F.G.; Scheidel, K.C.; de Weger, R.A.; Koole, R.; Hordijk, G.J.; Slootweg, P.J.; Tilanus, M.G. Sequencing analysis of RNA and DNA of exons 1 through 11 shows p53 gene alterations to be present in almost 100% of head and neck squamous cell cancers. Lab. Investig. J. Tech. Methods Pathol. 1999, 79, 347–353. [Google Scholar]
- Ruttkay-Nedecky, B.; Jimenez Jimenez, A.M.; Nejdl, L.; Chudobova, D.; Gumulec, J.; Masarik, M.; Adam, V.; Kizek, R. Relevance of infection with human papillomavirus: The role of the p53 tumor suppressor protein and E6/E7 zinc finger proteins (Review). Int. J. Oncol. 2013, 43, 1754–1762. [Google Scholar] [CrossRef] [PubMed]
- Kimple, R.J.; Smith, M.A.; Blitzer, G.C.; Torres, A.D.; Martin, J.A.; Yang, R.Z.; Peet, C.R.; Lorenz, L.D.; Nickel, K.P.; Klingelhutz, A.J.; et al. Enhanced radiation sensitivity in HPV-positive head and neck cancer. Cancer Res. 2013, 73, 4791–4800. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, B.S.; Busk, M.; Olthof, N.; Speel, E.J.; Horsman, M.R.; Alsner, J.; Overgaard, J. Radiosensitivity and effect of hypoxia in HPV positive head and neck cancer cells. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2013, 108, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Rieckmann, T.; Tribius, S.; Grob, T.J.; Meyer, F.; Busch, C.J.; Petersen, C.; Dikomey, E.; Kriegs, M. HNSCC cell lines positive for HPV and p16 possess higher cellular radiosensitivity due to an impaired DSB repair capacity. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2013, 107, 242–246. [Google Scholar] [CrossRef] [PubMed]
| Cell Line | Age | Sex | TNM Status | Primary Tumor Location | Lesion Type | Reference |
|---|---|---|---|---|---|---|
| UT-SCC-5 | 58 | Male | T1N1M0 | Tongue | Primary | [11] |
| UT-SCC-8 | 42 | Male | T2N0M0 | Supraglottic larynx | Primary | [11] |
| UT-SCC-9 | 81 | Male | T2N0M0 | Glottic larynx | Primary | [11] |
| UT-SCC-11 | 58 | Male | T1N0M0 | Glottic larynx | Recurrence | [12] |
| UT-SCC-15 | 51 | Male | T1N0M0 | Tongue | Recurrence | [13] |
| UT-SCC-19A | 44 | Male | T4N0M0 | Glottic larynx | Primary | [14] |
| UT-SCC-24A | 41 | Male | T2N0M0 | Tongue | Primary | [11] |
| UT-SCC-29 | 82 | Male | T2N0M0 | Glottic larynx | Primary | [11,14] |
| UT-SCC-38 | 66 | Male | T2N0M0 | Glottic larynx | Primary | [13] |
| UT-SCC-40 | 65 | Male | T3N0M0 | Tongue | Primary | [13] |
| UT-SCC-45 | 76 | Male | T3N1M0 | Floor of mouth | Primary | [13] |
| UM-SCC-6 | 37 | Male | T2N0M0 | Oropharynx | Primary | [15] |
| UM-SCC-47 | 53 | Male | T3N1M0 | Tongue | Primary | [16] |
| 93-VU-147T | 58 | Male | T4N2 | Floor of mouth | Primary | [17] |
| UPCI:SCC090 | 46 | Male | T2N0 | Base of tongue | Recurrence | [18] |
| UPCI:SCC154 | 54 | Male | T4N2 | Tongue | Primary | [18] |
| FaDu | 56 | Male | NA | Hypopharynx | Metastasis | [19,20] |
| SCCNij153 | Unknown | Unknown | T3N2M0 | Supraglottic larynx | Primary | [21] |
| SCCNij167 | Unknown | Unknown | T4N2M0 | Supraglottic larynx | Primary | [21] |
| SCCNij172 | Unknown | Unknown | T4N0M0 | Supraglottic larynx | Primary | [21] |
| SCCNij185 | Unknown | Unknown | T4N1M0 | Supraglottic larynx | Primary | [21] |
| SCCNij202 | Unknown | Unknown | T4N0M0 | Supraglottic larynx | Primary | [21] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Göttgens, E.-L.; Ansems, M.; Leenders, W.P.J.; Bussink, J.; Span, P.N. Genotyping and Characterization of HPV Status, Hypoxia, and Radiosensitivity in 22 Head and Neck Cancer Cell Lines. Cancers 2021, 13, 1069. https://doi.org/10.3390/cancers13051069
Göttgens E-L, Ansems M, Leenders WPJ, Bussink J, Span PN. Genotyping and Characterization of HPV Status, Hypoxia, and Radiosensitivity in 22 Head and Neck Cancer Cell Lines. Cancers. 2021; 13(5):1069. https://doi.org/10.3390/cancers13051069
Chicago/Turabian StyleGöttgens, Eva-Leonne, Marleen Ansems, William P. J. Leenders, Johan Bussink, and Paul N. Span. 2021. "Genotyping and Characterization of HPV Status, Hypoxia, and Radiosensitivity in 22 Head and Neck Cancer Cell Lines" Cancers 13, no. 5: 1069. https://doi.org/10.3390/cancers13051069
APA StyleGöttgens, E.-L., Ansems, M., Leenders, W. P. J., Bussink, J., & Span, P. N. (2021). Genotyping and Characterization of HPV Status, Hypoxia, and Radiosensitivity in 22 Head and Neck Cancer Cell Lines. Cancers, 13(5), 1069. https://doi.org/10.3390/cancers13051069







