Perineal Wound Closure Following Abdominoperineal Resection and Pelvic Exenteration for Cancer: A Systematic Review and Meta-Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Data Collection
2.2. Inclusion and Exclusion Criteria
2.3. Outcome Parameters
2.4. Data Collection and Extraction
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
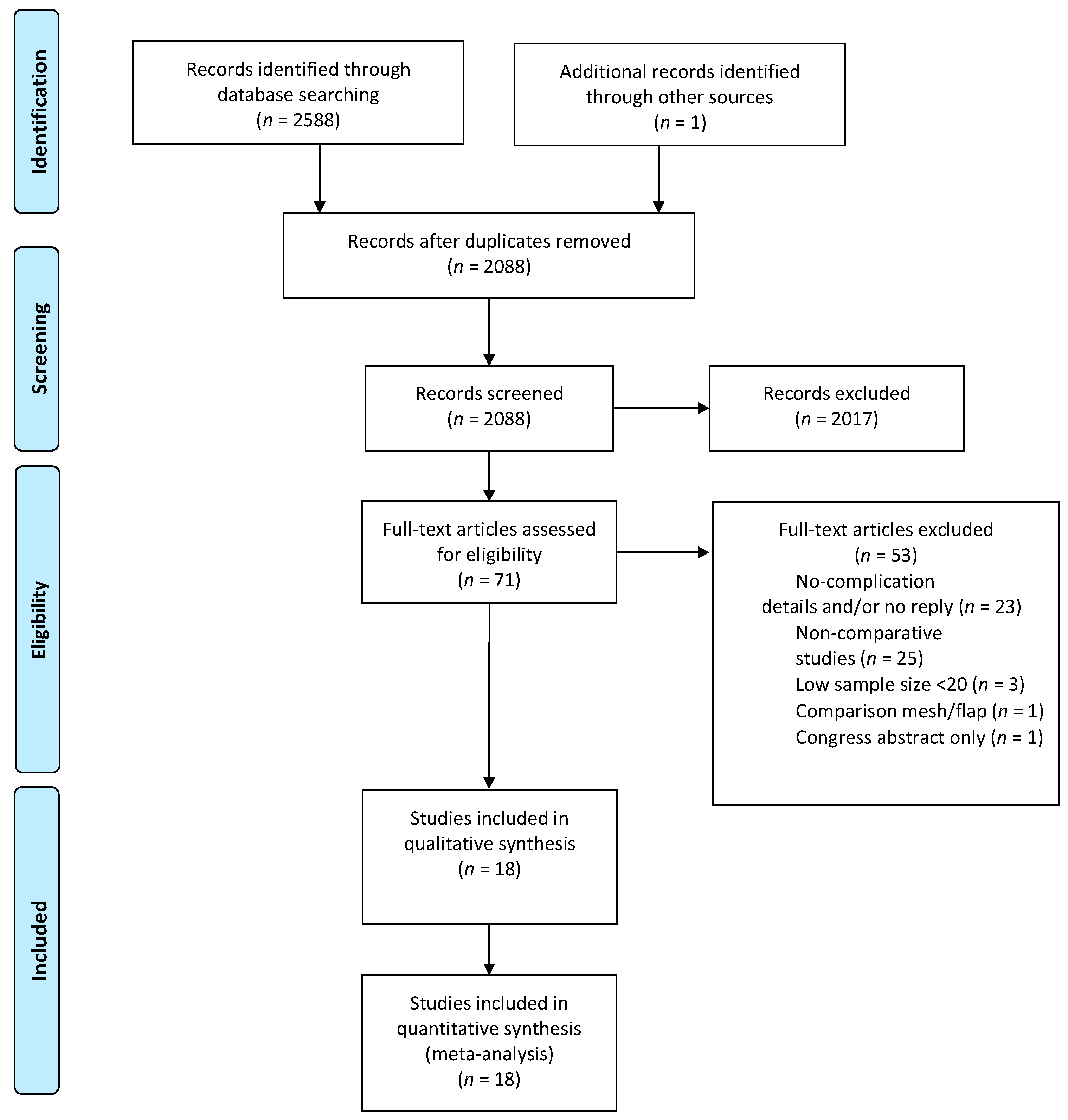
3.1. Literature Search and Results
3.2. Study and Patient Characteristics
3.3. Study Endpoints
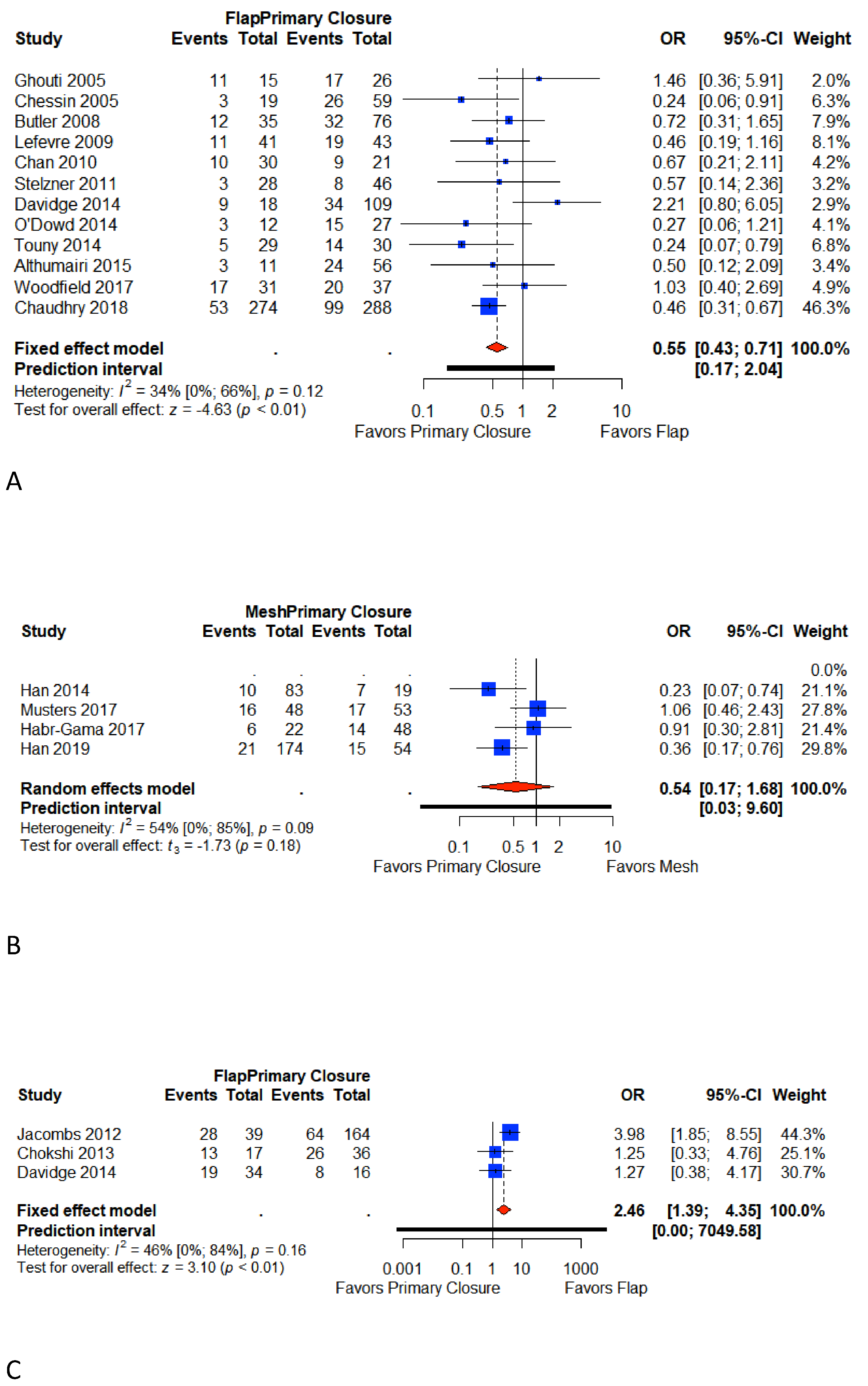
3.4. Total Perineal Wound Complication
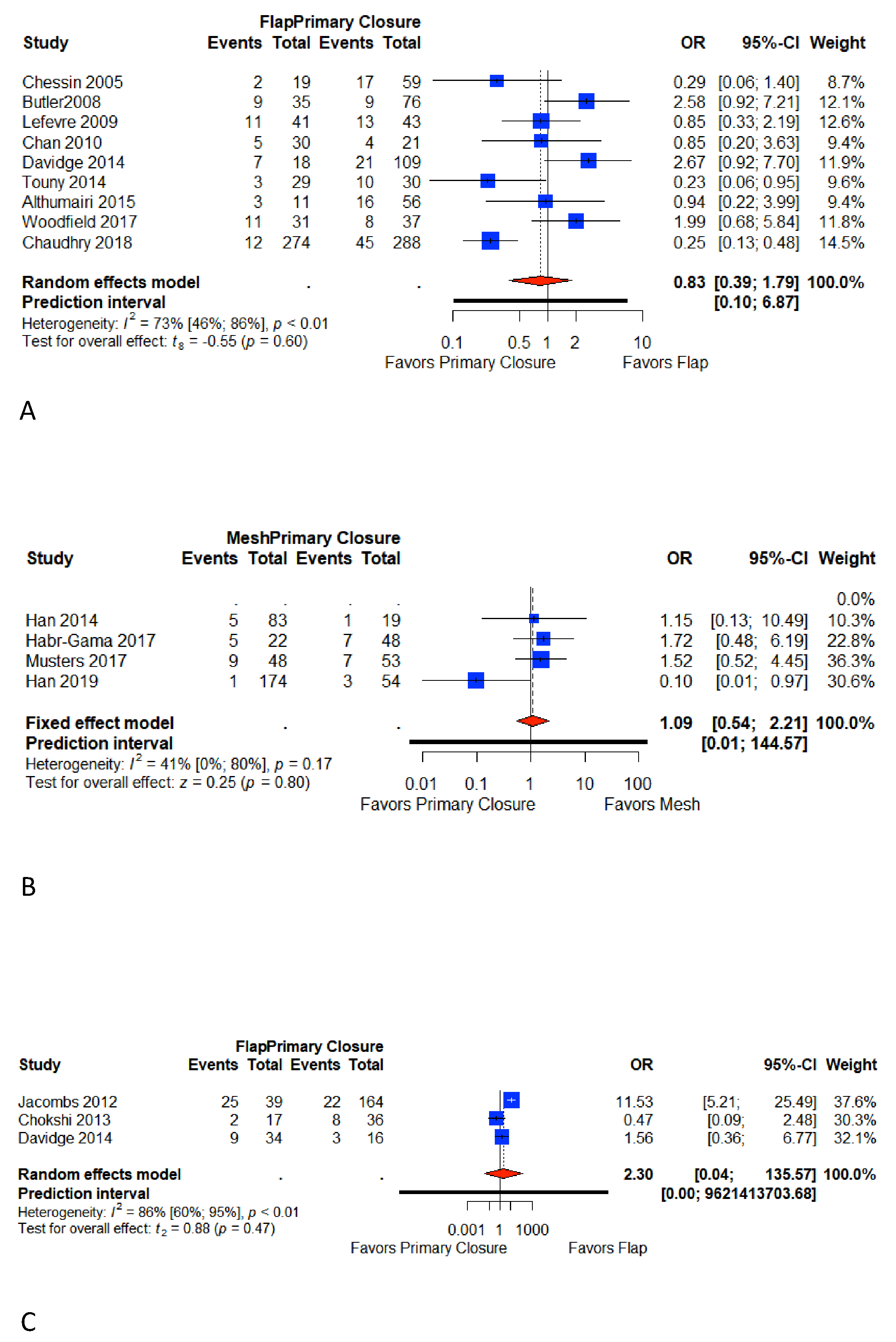
3.5. Major Wound Complications
3.6. Minor Wound Complications
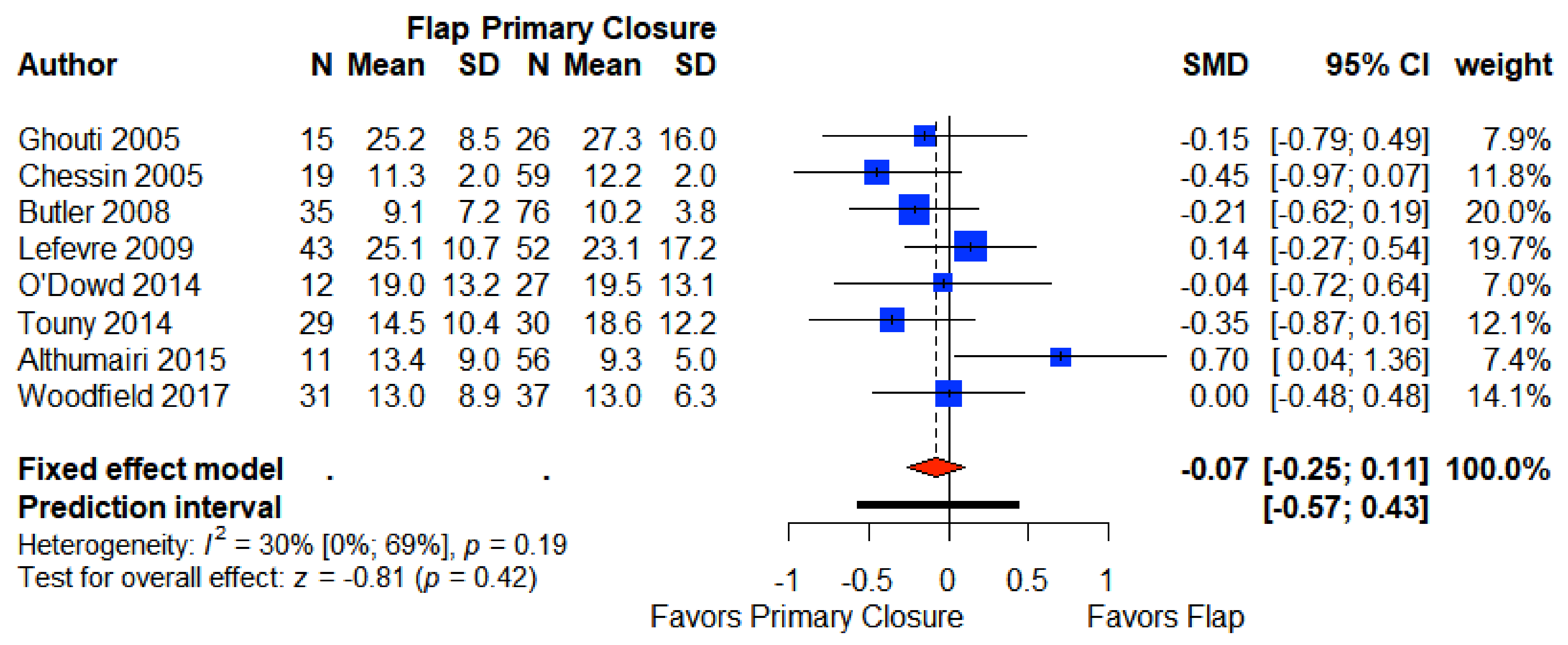
3.7. Length of Stay
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Devulapalli, C.; Wei, A.T.J.; di Biagio, J.R.; Baez, M.L.; Baltodano, F.P.; Seal, S.M.; Broyles, J.M.; Cooney, C.M.; Rosson, G.D. Primary versus Flap Closure of Perineal Defects following Oncologic Resection. Plast. Reconstr. Surg. 2016, 137, 1602–1613. [Google Scholar] [CrossRef] [PubMed]
- West, N.P.; Anderin, C.; Smith, K.J.E.; Holm, T.; Quirke, P. Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. BJS 2010, 97, 588–599. [Google Scholar] [CrossRef]
- Tuech, J.-J.; Pinson, J.; Nouhaud, F.-X.; Wood, G.; Clavier, T.; Sabourin, J.-C.; di Fiore, F.; Monge, M.; Papet, E.; Coget, J. Total Pelvic Exenteration, Cytoreductive Surgery, and Hyperthermic Intraperitoneal Chemotherapy for Rectal Cancer with Associate Peritoneal Metastases: Surgical Strategies to Optimize Safety. Cancers 2020, 12, 3478. [Google Scholar] [CrossRef] [PubMed]
- Denost, Q.; Solomon, M.; Tuech, J.-J.; Ghouti, L.; Cotte, E.; Panis, Y.; Lelong, B.; Rouanet, P.; Faucheron, J.-L.; Jafari, M.; et al. International variation in managing locally advanced or recurrent rectal cancer: Prospective benchmark analysis. BJS 2020, 107, 1846–1854. [Google Scholar] [CrossRef] [PubMed]
- Musters, G.D.; Buskens, C.J.; Bemelman, W.A.; Tanis, P.J. Perineal Wound Healing After Abdominoperineal Resection for Rectal Cancer. Dis. Colon Rectum 2014, 57, 1129–1139. [Google Scholar] [CrossRef]
- Chessin, D.B.; Hartley, J.; Cohen, A.M.; Mazumdar, M.; Cordeiro, P.; Disa, J.; Mehrara, B.; Minsky, B.D.; Paty, P.; Weiser, M.; et al. Rectus Flap Reconstruction Decreases Perineal Wound Complications After Pelvic Chemoradiation and Surgery: A Cohort Study. Ann. Surg. Oncol. 2005, 12, 104–110. [Google Scholar] [CrossRef]
- Butler, C.E.; Gündeslioglu, A.Ö.; Rodriguez-Bigas, M.A. Outcomes of Immediate Vertical Rectus Abdominis Myocutaneous Flap Reconstruction for Irradiated Abdominoperineal Resection Defects. J. Am. Coll. Surg. 2008, 206, 694–703. [Google Scholar] [CrossRef]
- Thomas, P.W.; Blackwell, J.E.M.; Herrod, P.J.J.; Peacock, O.; Singh, R.; Williams, J.P.; Hurst, N.G.; Speake, W.J.; Bhalla, A.; Lund, J.N. Long-term outcomes of biological mesh repair following extra levator abdominoperineal excision of the rectum: An observational study of 100 patients. Tech. Coloproctol. 2019, 23, 761–767. [Google Scholar] [CrossRef]
- Han, J.G.; Wang, Z.J.; Gao, Z.G.; Wei, G.H.; Yang, Y.; Zhai, Z.W.; Zhao, B.C.; Yi, B.Q. Perineal Wound Complications After Extralevator Abdominoperineal Excision for Low Rectal Cancer. Dis. Colon Rectum 2019, 62, 1477–1484. [Google Scholar] [CrossRef]
- Musters, G.D.; Klaver, C.E.L.; Bosker, R.J.I.; Burger, J.W.A.; van Duijvendijk, P.; van Etten, B.; van Geloven, A.A.W.; de Graaf, E.J.R.; Hoff, C.; Leijtens, J.W.A.; et al. Biological Mesh Closure of the Pelvic Floor After Extralevator Abdominoperineal Resection for Rectal Cancer. Ann. Surg. 2017, 265, 1074–1081. [Google Scholar] [CrossRef]
- Foster, J.D.; Tou, S.; Curtis, N.J.; Smart, N.J.; Acheson, A.; Maxwell-Armstrong, C.; Watts, A.; Singh, B.; Francis, N.K. Closure of the perineal defect after abdominoperineal excision for rectal adenocarcinoma—ACPGBI Position Statement. Color. Dis. 2018, 20, 5–23. [Google Scholar] [CrossRef]
- Yang, T.; Shen, Y.; Wang, Z. Perineal Wound Complications After Extralevator Abdominoperineal Excision for Low Rectal Cancer: A Call to Introduce a Standard Definition and Classification. Dis. Colon Rectum 2020, 63, e496. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B.; et al. Meta-analysis of Observational Studies in EpidemiologyA Proposal for Reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Bailey, I.S.; Karran, S.E.; Toyn, K.; Brough, P.; Ranaboldo, C. Community surveillance of complications after hernia surgery. BMJ 1992, 304, 469–471. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’connell, D.L.; Peterson, J.; Welch; Losos, M.; Tugwell, P.; Ga, S.W.; Zello, G.A.; Petersen, J.; et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2014. [Google Scholar]
- Habr-Gama, A.; Julião, G.P.S.; Mattacheo, A.; de Campos-Lobato, L.F.; Aleman, E.; Vailati, B.B.; Gama-Rodrigues, J.; Perez, R.O. Extralevator Abdominal Perineal Excision Versus Standard Abdominal Perineal Excision: Impact on Quality of the Resected Specimen and Postoperative Morbidity. World J. Surg. 2017, 41, 2160–2167. [Google Scholar] [CrossRef]
- Perdawood, S.K.; Lund, T. Extralevator versus standard abdominoperineal excision for rectal cancer. Tech. Coloproctol. 2015, 19, 145–152. [Google Scholar] [CrossRef]
- Colov, E.P.; Klein, M.; Gögenur, I. Wound Complications and Perineal Pain After Extralevator Versus Standard Abdominoperineal Excision. Dis. Colon Rectum 2016, 59, 813–821. [Google Scholar] [CrossRef]
- Ghouti, L.; Houvenaeghel, G.; Moutardier, V.; Giovannini, M.; Magnin, V.; Lelong, B.; Bardou, V.-J.; Delpero, J.-R. Salvage Abdominoperineal Resection After Failure of Conservative Treatment in Anal Epidermoid Cancer. Dis. Colon Rectum 2005, 48, 16–22. [Google Scholar] [CrossRef]
- Lefevre, J.H.; Parc, Y.; Kernéis, S.; Shields, C.; Touboul, E.; Chaouat, M.; Tiret, E. Abdomino-Perineal Resection for Anal Cancer. Ann. Surg. 2009, 250, 707–711. [Google Scholar] [CrossRef]
- Chan, S.; Miller, M.; Ng, R.; Ross, D.; Roblin, P.; Carapeti, E.; Williams, A.B.; George, M.L. Use of myocutaneous flaps for perineal closure following abdominoperineal excision of the rectum for adenocarcinoma. Color. Dis. 2009, 12, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Stelzner, S.; Hellmich, G.; Schubert, C.; Puffer, E.; Haroske, G.; Witzigmann, H. Short-term outcome of extra-levator abdominoperineal excision for rectal cancer. Int. J. Color. Dis. 2011, 26, 919–925. [Google Scholar] [CrossRef] [PubMed]
- Davidge, K.M.; Raghuram, K.; Hofer, S.; Ferguson, P.C.; Wunder, J.S.; Swallow, C.J.; Zhong, T. Impact of Flap Reconstruction on Perineal Wound Complications Following Ablative Surgery for Advanced and Recurrent Rectal Cancers. Ann. Surg. Oncol. 2014, 21, 2068–2073. [Google Scholar] [CrossRef] [PubMed]
- Althumairi, A.A.; Canner, J.K.; Ahuja, N.; Sacks, J.M.; Safar, B.; Efron, J. Time to Chemotherapy After Abdominoperineal Resection: Comparison Between Primary Closure and Perineal Flap Reconstruction. World J. Surg. 2016, 40, 225–230. [Google Scholar] [CrossRef] [PubMed]
- O’Dowd, V.; Burke, J.P.; Condon, E.; Waldron, D.; Ajmal, N.; Deasy, J.; McNamara, D.A.; Coffey, J.C. Vertical rectus abdominis myocutaneous flap and quality of life following abdominoperineal excision for rectal cancer: A multi-institutional study. Tech. Coloproctol. 2014, 18, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Touny, A.; Othman, H.; Maamoon, S.; Ramzy, S.; Elmarakby, H. Perineal reconstruction using pedicled vertical rectus abdominis myocutaneous flap (VRAM). J. Surg. Oncol. 2014, 110, 752–757. [Google Scholar] [CrossRef]
- Woodfield, J.; Hulme-Moir, M.; Ly, J. A comparison of the cost of primary closure or rectus abdominis myocutaneous flap closure of the perineum after abdominoperineal excision. Color. Dis. 2017, 19, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, A.; Oliver, J.D.; Vyas, K.S.; Tran, N.V.; Martinez-Jorge, J.; Larson, D.; Dozois, E.; Nelson, H.; Manrique, O.J. Comparison of Outcomes in Oncoplastic Pelvic Reconstruction with VRAM versus Omental Flaps: A Large Cohort Analysis. J. Reconstr. Microsurg. 2019, 35, 425–429. [Google Scholar] [CrossRef]
- Han, J.G.; Wang, Z.J.; Qian, Q.; Dai, Y.; Zhang, Z.Q.; Yang, J.S.; Li, F.; Bin Li, X. A Prospective Multicenter Clinical Study of Extralevator Abdominoperineal Resection for Locally Advanced Low Rectal Cancer. Dis. Colon Rectum 2014, 57, 1333–1340. [Google Scholar] [CrossRef]
- Chokshi, R.J.; Kuhrt, M.P.; Arrese, D.; Martin, E.W. Reconstruction of total pelvic exenteration defects with rectus abdominus myocutaneous flaps versus primary closure. Am. J. Surg. 2013, 205, 64–70. [Google Scholar] [CrossRef]
- Jacombs, A.S.W.; Rome, P.; Harrison, J.D.; Solomon, M.J. Assessment of the selection process for myocutaneous flap repair and surgical complications in pelvic exenteration surgery. BJS 2013, 100, 561–567. [Google Scholar] [CrossRef]
- Buscail, E.; Blondeau, V.; Adam, J.-P.; Pontallier, A.; Laurent, C.; Rullier, E.; Denost, Q. Surgery for rectal cancer after high-dose radiotherapy for prostate cancer: Is sphincter preservation relevant? Color. Dis. 2015, 17, 973–979. [Google Scholar] [CrossRef]
- West, N.P.; Finan, P.J.; Anderin, C.; Lindholm, J.; Holm, T.; Quirke, P. Evidence of the Oncologic Superiority of Cylindrical Abdominoperineal Excision for Low Rectal Cancer. J. Clin. Oncol. 2008, 26, 3517–3522. [Google Scholar] [CrossRef]
- Holm, T. Abdominoperineal Excision: Technical Challenges in Optimal Surgical and Oncological Outcomes after Abdominoperineal Excision for Rectal Cancer. Clin. Colon Rectal Surg. 2017, 30, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, A.T.; Berger, D.L.; Shellito, P.C.; Sylla, P.; Bordeianou, L. Wound Dehiscence After Abdominoperineal Resection for Low Rectal Cancer Is Associated with Decreased Survival. Dis. Colon Rectum 2014, 57, 143–150. [Google Scholar] [CrossRef]
- Weichman, K.E.; Matros, E.; Disa, J.J. Reconstruction of Peripelvic Oncologic Defects. Plast. Reconstr. Surg. 2017, 140, 601e–612e. [Google Scholar] [CrossRef] [PubMed]
- Pelv Ex Collaborative. Pelvic Exenteration for Advanced Nonrectal Pelvic Malignancy. Ann. Surg. 2019, 270, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Billig, J.I.; Hsu, J.J.; Zhong, L.; Wang, L.; Chung, K.C.; Kung, T.A. Comparison of Effective Cost and Complications after Abdominoperineal Resection. Plast. Reconstr. Surg. 2019, 144, 866e–875e. [Google Scholar] [CrossRef] [PubMed]
- Rutegård, J.; Rutegård, J.; Haapamäki, M.M. Multicentre, randomised trial comparing acellular porcine collagen implant versus gluteus maximus myocutaneous flap for reconstruction of the pelvic floor after extended abdominoperineal excision of rectum: Study protocol for the Nordic Extended Abdominoperineal Excision (NEAPE) study. BMJ Open 2019, 9, e027255. [Google Scholar] [CrossRef]
- Sharabiany, S.; Blok, R.D.; Lapid, O.; Hompes, R.; Bemelman, W.A.; Alberts, V.P.; Lamme, B.; Wijsman, J.H.; Tuynman, J.B.; Aalbers, A.G.J.; et al. Perineal wound closure using gluteal turnover flap or primary closure after abdominoperineal resection for rectal cancer: Study protocol of a randomised controlled multicentre trial (BIOPEX-2 study). BMC Surg. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]

| Study (Author) | Year | Country | Design | Quality * | Disease | Patient (n = 2180) | Primary Closure ** (n = 1206) | Flap closure ** (n = 647) | Mesh Closure ** (n = 327) |
|---|---|---|---|---|---|---|---|---|---|
| Ghouti et al. [21] | 2005 | France | Retrospective cohort study | 5 | Anal cancer | 41 | 15 | 26 | - |
| Chessin et al. [6] | 2005 | USA | Retrospective cohort study | 5 | Rectal cancer and anal cancer | 78 | 59 | 19 | - |
| Butler et al. [7] | 2008 | USA | Retrospective cohort study | 5 | Rectal and anal cancer | 111 | 76 | 35 | - |
| Lefevre et al. [22] | 2009 | France | Retrospective cohort study | 7 | Anal cancer | 95 | 52 | 43 | - |
| Chan et al. [23] | 2010 | UK | Retrospective cohort study | 4 | Rectal cancer | 51 | 21 | 30 | - |
| Stelzner et al. [24] | 2011 | Germany | Retrospective cohort study | 3 | Rectal cancer | 74 | 46 | 28 | - |
| Jacombs et al. [33] | 2012 | Australia | Retrospective cohort study | 5 | Rectal cancer | 203 | 164 | 39 | - |
| Chokshi et al. [32] | 2013 | USA | Retrospective cohort study | 5 | Rectal cancer, anal cancer, and other cancers | 53 | 36 | 17 | - |
| Davidge et al. [25] | 2014 | Canada | Retrospective cohort study | 4 | Rectal cancer | 177 | 125 | 52 | - |
| O’Dowd et al. [27] | 2014 | Ireland | Retrospective cohort study | 8 | Rectal cancer | 39 | 27 | 12 | - |
| Touny et al. [28] | 2014 | Egypt | RCT | 9 | Rectal cancer | 60 | 30 | 30 | - |
| Althumairi et al. [26] | 2015 | USA | Retrospective cohort study | 4 | Rectal cancer | 67 | 56 | 11 | - |
| Woodfield et al. [29] | 2017 | New Zeland | Retrospective cohort study | 3 | Rectal cancer, anal cancer, and other cancers | 68 | 37 | 31 | - |
| Chaudhry et al. [30] | 2018 | USA | Retrospective cohort study | 5 | Rectal cancer, anal cancer, and other cancers | 562 | 288 | 274 | - |
| Han et al. # [31] | 2014 | China | RCT | 9 | Rectal cancer | 102 | 19 | - | 83 |
| Musters et al. # [10] | 2017 | Netherlands | RCT | 9 | Rectal cancer | 101 | 53 | - | 48 |
| Habr-Gama et al. # [18] | 2017 | Brazil | Retrospective cohort study | 6 | Rectal cancer | 72 *** | 48 | - | 22 |
| Han et al. # [9] | 2019 | China | Retrospective cohort study | 6 | Rectal cancer | 228 | 54 | - | 174 |
| Flap and Primary Closure (n = 1679) | Mesh and Primary Closure (n = 501) | |||||
|---|---|---|---|---|---|---|
| Flap (n = 647) * | Primary Closure (n = 1032) | Total (n = 1679) | Mesh (n = 327) | Primary Closure (n = 174) | Total (n = 501) | |
| Sex | ||||||
| Male | 463 (77%) | 716 (69%) | 1179 (70%) | 164 (37%) | 67 (38%) | 319 (63%) ** |
| NR | 35 (5%) | 76 (7%) | 312 (32%) | 67 (38%) | 0 | |
| Disease *** | ||||||
| Rectal cancer | 256 (40%) | 623 (60%) | 879 (53%) | 327 (100%) | 174 (100%) | 501 (100%) |
| Anal Cancer | 88 (13%) | 72 (7%) | 160 (9%) | 0 | 0 | 0 |
| Other cancers | 11 (2%) | 0 | 11 (0.5%) | 0 | 0 | 0 |
| NR | 292 (45%) | 337 (33%) | 629 (37.5%) | 0 | 0 | 0 |
| Neoadjuvant therapy | ||||||
| None | 141 (22%) | 220 (21%) | 361 (22%) | 85 (26%) | 35 (20%) | 120 (23%) |
| Short course (25 Gy) | 0 | 0 | 0 | 182 (56%) | 49 (28%) | 231 (47%) |
| Long course (40–60 Gy) | 381 (59%) | 541 (52%) | 922 (55%) | 60 (18%) | 90 (52%) | 150 (30%) |
| Chemotherapy | 305 (46%) | 455 (43%) | 760 (45%) | 232 (70%) | 129 (75%) | 361 (72%) |
| NR | 125 (19%) | 283 (27%) | 398 (23%) | 0 | 0 | 0 |
| Type of resection | ||||||
| APR | 460 (71%) | 749 (73%) | 1209 (72%) | 3 (1%) | 47 (27%) | 50 (9%) |
| ELAPE | 97 (15%) | 67 (6%) | 164 (10%) | 324 (99%) | 127 (73%) | 451 (91%) |
| Pelvic exenteration | 90 (14%) | 216 (21%) | 306 (18%) | 0 | 0 | 0 |
| NR | 0 | 0 | 0 | 0 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buscail, E.; Canivet, C.; Shourick, J.; Chantalat, E.; Carrere, N.; Duffas, J.-P.; Philis, A.; Berard, E.; Buscail, L.; Ghouti, L.; et al. Perineal Wound Closure Following Abdominoperineal Resection and Pelvic Exenteration for Cancer: A Systematic Review and Meta-Analysis. Cancers 2021, 13, 721. https://doi.org/10.3390/cancers13040721
Buscail E, Canivet C, Shourick J, Chantalat E, Carrere N, Duffas J-P, Philis A, Berard E, Buscail L, Ghouti L, et al. Perineal Wound Closure Following Abdominoperineal Resection and Pelvic Exenteration for Cancer: A Systematic Review and Meta-Analysis. Cancers. 2021; 13(4):721. https://doi.org/10.3390/cancers13040721
Chicago/Turabian StyleBuscail, Etienne, Cindy Canivet, Jason Shourick, Elodie Chantalat, Nicolas Carrere, Jean-Pierre Duffas, Antoine Philis, Emilie Berard, Louis Buscail, Laurent Ghouti, and et al. 2021. "Perineal Wound Closure Following Abdominoperineal Resection and Pelvic Exenteration for Cancer: A Systematic Review and Meta-Analysis" Cancers 13, no. 4: 721. https://doi.org/10.3390/cancers13040721
APA StyleBuscail, E., Canivet, C., Shourick, J., Chantalat, E., Carrere, N., Duffas, J.-P., Philis, A., Berard, E., Buscail, L., Ghouti, L., & Chaput, B. (2021). Perineal Wound Closure Following Abdominoperineal Resection and Pelvic Exenteration for Cancer: A Systematic Review and Meta-Analysis. Cancers, 13(4), 721. https://doi.org/10.3390/cancers13040721







