Biomarkers of Response to Etoposide-Platinum Chemotherapy in Patients with Grade 3 Neuroendocrine Neoplasms
Abstract
Simple Summary
Abstract
1. Introduction
2. Results
2.1. Patient Characteristics
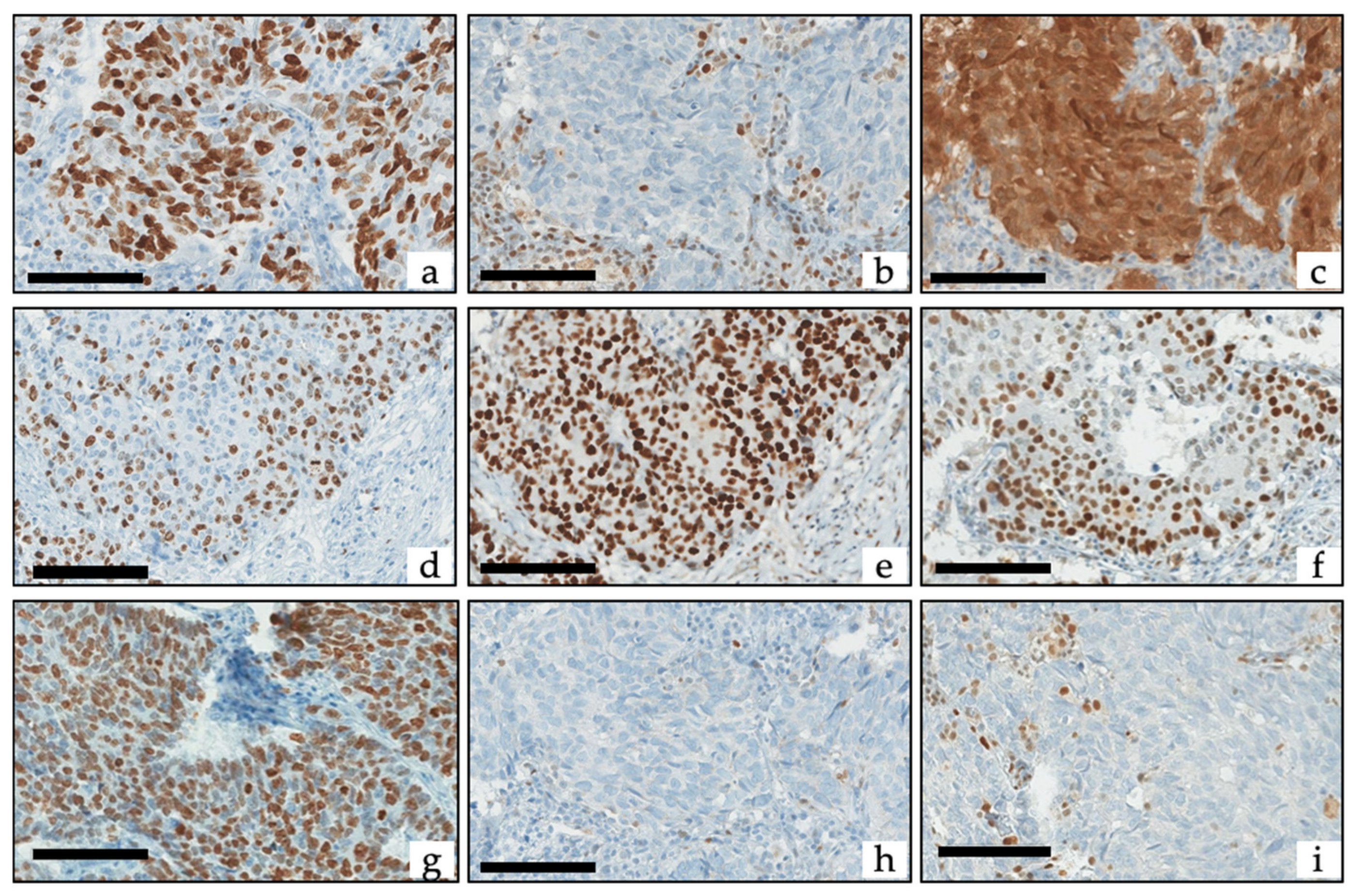
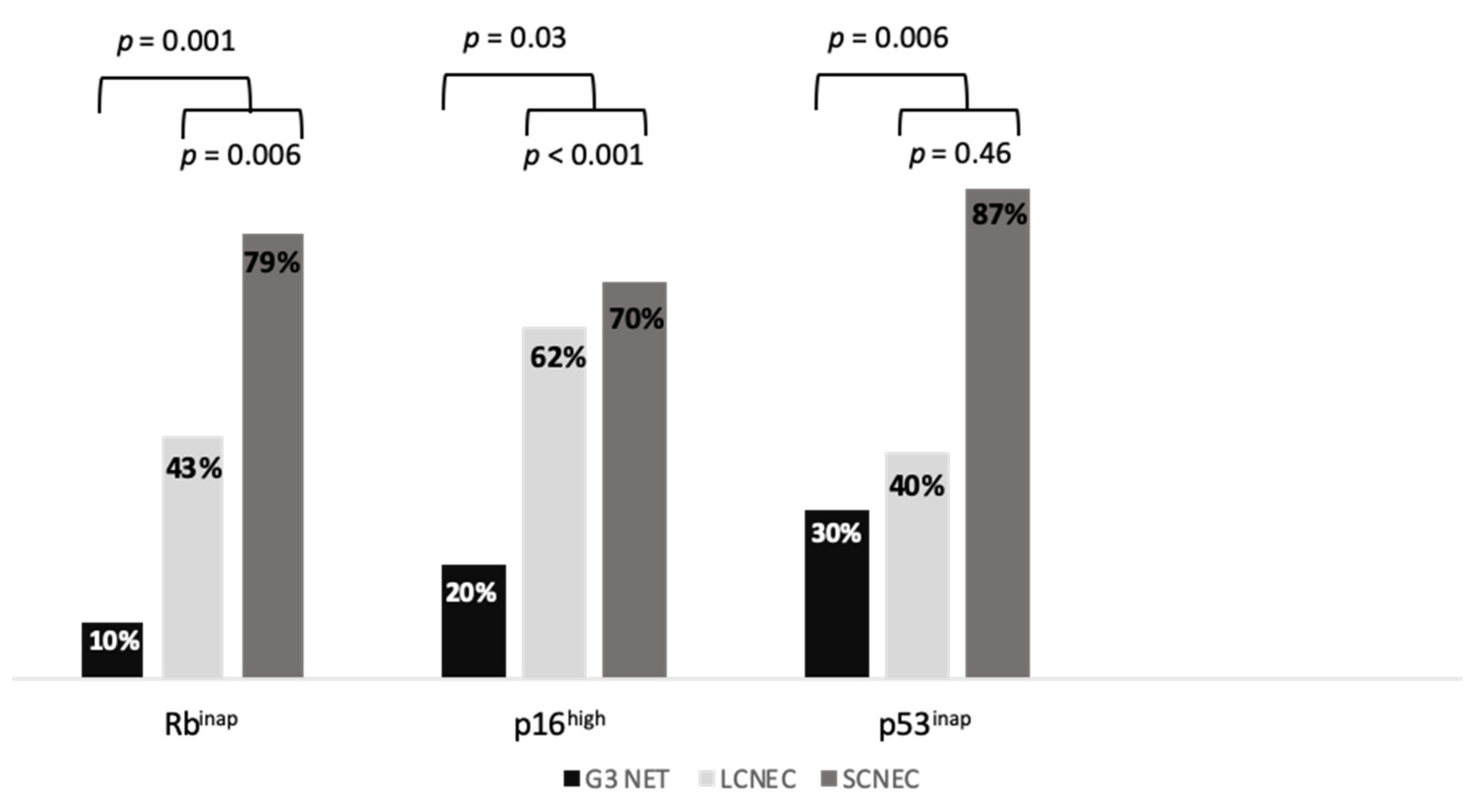
2.2. Biomarker Immunohistochemistry
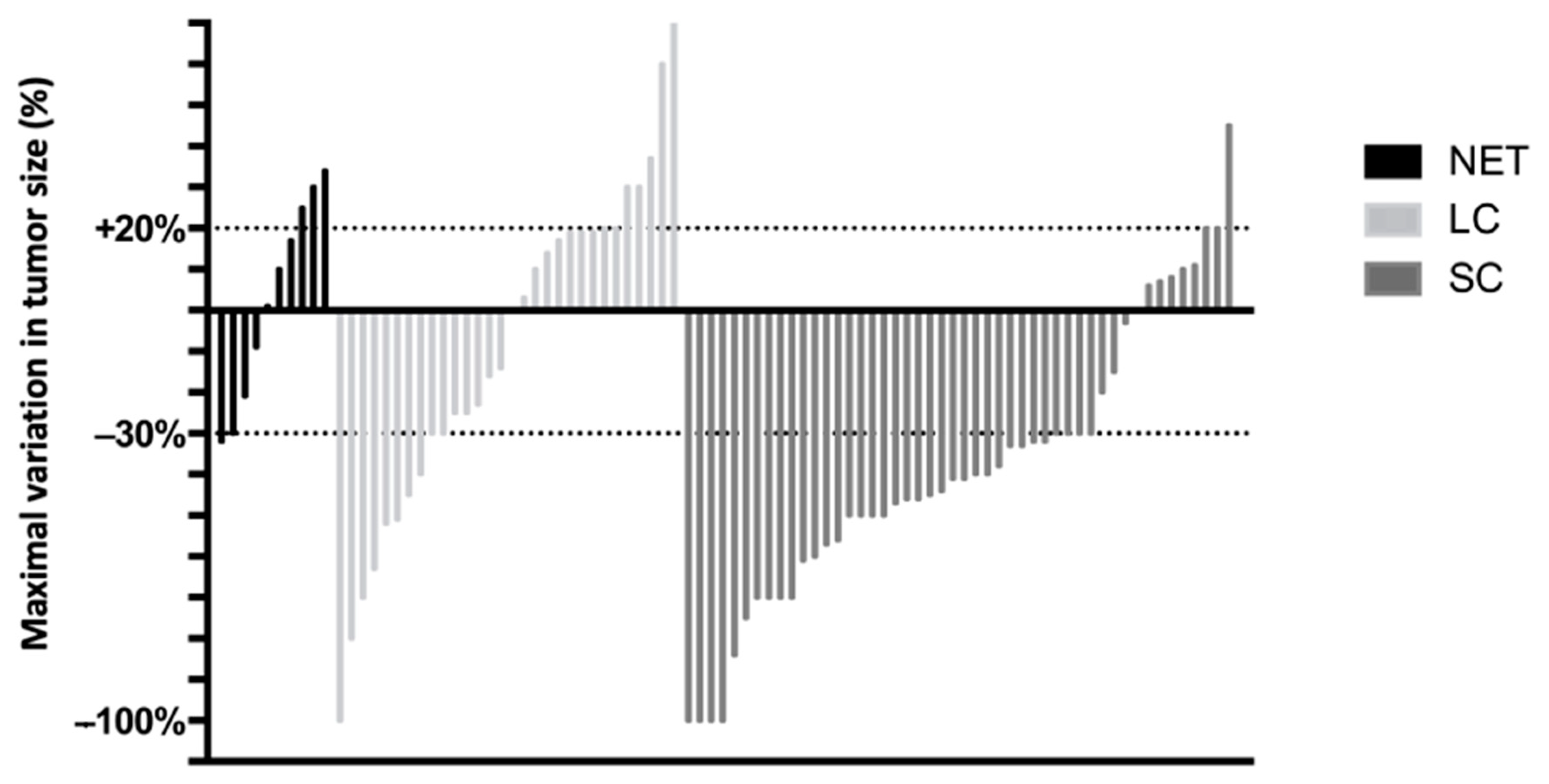
2.3. Association between Biomarkers and Response to EP
2.4. Association between Biomarkers and PFS under EP
2.5. Association between Biomarkers and OS
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Data Collected
4.3. Histopathogical and Immunohistochemical Evaluation
4.4. Statistical Analyses
4.5. Ethical Considerations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Classification of Tumours. Digestive System Tumours. WHO/IARC Classification of Tumours, 5th ed.IARC: Lyon, France, 2019; Volume 1, ISBN 978-92-832-4499-8. [Google Scholar]
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef]
- De Mestier, L.; Lepage, C.; Baudin, E.; Coriat, R.; Courbon, F.; Couvelard, A.; Do Cao, C.; Frampas, E.; Gaujoux, S.; Gincul, R.; et al. Digestive Neuroendocrine Neoplasms (NEN): French Intergroup Clinical Practice Guidelines for Diagnosis, Treatment and Follow-up (SNFGE, GTE, RENATEN, TENPATH, FFCD, GERCOR, UNICANCER, SFCD, SFED, SFRO, SFR). Dig. Liver Dis. 2020, 52, 473–492. [Google Scholar] [CrossRef]
- Quinn, A.M.; Chaturvedi, A.; Nonaka, D. High-Grade Neuroendocrine Carcinoma of the Lung With Carcinoid Morphology: A Study of 12 Cases. Am. J. Surg. Pathol. 2017, 41, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Cros, J.; Théou-Anton, N.; Gounant, V.; Nicolle, R.; Reyes, C.; Humez, S.; Hescot, S.; Thomas de Montpréville, V.; Guyétant, S.; Scoazec, J.-Y.; et al. Specific Genomic Alterations in High Grade Pulmonary Neuroendocrine Tumours with Carcinoid Morphology. Neuroendocrinology 2020. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Walter, V.; Peifer, M.; Alexandrov, L.B.; Seidel, D.; Leenders, F.; Maas, L.; Müller, C.; Dahmen, I.; Delhomme, T.M.; et al. Integrative Genomic Profiling of Large-Cell Neuroendocrine Carcinomas Reveals Distinct Subtypes of High-Grade Neuroendocrine Lung Tumors. Nat. Commun. 2018, 9, 1048. [Google Scholar] [CrossRef]
- Rekhtman, N.; Pietanza, M.C.; Hellmann, M.D.; Naidoo, J.; Arora, A.; Won, H.; Halpenny, D.F.; Wang, H.; Tian, S.K.; Litvak, A.M.; et al. Next-Generation Sequencing of Pulmonary Large Cell Neuroendocrine Carcinoma Reveals Small Cell Carcinoma-like and Non-Small Cell Carcinoma-like Subsets. Clin. Cancer Res. 2016, 22, 3618–3629. [Google Scholar] [CrossRef]
- Lázaro, S.; Pérez-Crespo, M.; Lorz, C.; Bernardini, A.; Oteo, M.; Enguita, A.B.; Romero, E.; Hernández, P.; Tomás, L.; Morcillo, M.Á.; et al. Differential Development of Large-Cell Neuroendocrine or Small-Cell Lung Carcinoma upon Inactivation of 4 Tumor Suppressor Genes. Proc. Natl. Acad. Sci. USA 2019, 116, 22300–22306. [Google Scholar] [CrossRef]
- Derks, J.L.; Leblay, N.; Lantuejoul, S.; Dingemans, A.-M.C.; Speel, E.-J.M.; Fernandez-Cuesta, L. New Insights into the Molecular Characteristics of Pulmonary Carcinoids and Large Cell Neuroendocrine Carcinomas, and the Impact on Their Clinical Management. J. Thorac. Oncol. 2018, 13, 752–766. [Google Scholar] [CrossRef] [PubMed]
- Derks, J.L.; van Suylen, R.J.; Thunnissen, E.; den Bakker, M.A.; Groen, H.J.; Smit, E.F.; Damhuis, R.A.; van den Broek, E.C.; Speel, E.-J.M.; Dingemans, A.-M.C.; et al. Chemotherapy for Pulmonary Large Cell Neuroendocrine Carcinomas: Does the Regimen Matter? Eur. Respir. J. 2017, 49, 1601838. [Google Scholar] [CrossRef]
- Klöppel, G.; Couvelard, A.; Hruban, R.H.; Klimstra, D.S.; Komminoth, P.; Osamura, R.Y.; Perren, A.; Rindi, G. Neoplasms of the neuroendocrine pancreas. In WHO Classification of Tumours of the Endocrine Organs; WHO/IARC Classification of Tumours; IARC Press: Lyon, France, 2017; Volume 10, pp. 210–239. ISBN 978-92-832-4493-6. [Google Scholar]
- Sigel, C.S.; Krauss Silva, V.W.; Reid, M.D.; Chhieng, D.; Basturk, O.; Sigel, K.M.; Daniel, T.D.; Klimstra, D.S.; Tang, L.H. Assessment of Cytologic Differentiation in High-Grade Pancreatic Neuroendocrine Neoplasms: A Multi-Institutional Study: Pancreatic Neuroendocrine Neoplasms. Cancer Cytopathol. 2018, 126, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Sorbye, H.; Baudin, E.; Perren, A. The Problem of High-Grade Gastroenteropancreatic Neuroendocrine Neoplasms: Well-Differentiated Neuroendocrine Tumors, Neuroendocrine Carcinomas, and Beyond. Endocrinol. Metab. Clin. North Am. 2018, 47, 683–698. [Google Scholar] [CrossRef]
- Konukiewitz, B.; Schlitter, A.M.; Jesinghaus, M.; Pfister, D.; Steiger, K.; Segler, A.; Agaimy, A.; Sipos, B.; Zamboni, G.; Weichert, W.; et al. Somatostatin Receptor Expression Related to TP53 and RB1 Alterations in Pancreatic and Extrapancreatic Neuroendocrine Neoplasms with a Ki67-Index above 20%. Mod. Pathol. 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Yachida, S.; Vakiani, E.; White, C.M.; Zhong, Y.; Saunders, T.; Morgan, R.; de Wilde, R.F.; Maitra, A.; Hicks, J.; DeMarzo, A.M.; et al. Small Cell and Large Cell Neuroendocrine Carcinomas of the Pancreas Are Genetically Similar and Distinct From Well-Differentiated Pancreatic Neuroendocrine Tumors. Am. J. Surg. Pathol. 2012, 36, 173–184. [Google Scholar] [CrossRef] [PubMed]
- Li, A.F.-Y.; Li, A.C.-H.; Tsay, S.-H.; Li, W.-Y.; Liang, W.-Y.; Chen, J.-Y. Alterations in the P16 INK4a /Cyclin D1/RB Pathway in Gastrointestinal Tract Endocrine Tumors. Am. J. Clin. Pathol. 2008, 130, 535–542. [Google Scholar] [CrossRef][Green Version]
- Coriat, R.; Walter, T.; Terris, B.; Couvelard, A.; Ruszniewski, P. Gastroenteropancreatic Well-Differentiated Grade 3 Neuroendocrine Tumors: Review and Position Statement. Oncologist 2016, 21, 1191–1199. [Google Scholar] [CrossRef] [PubMed]
- Velayoudom-Cephise, F.-L.; Duvillard, P.; Foucan, L.; Hadoux, J.; Chougnet, C.N.; Leboulleux, S.; Malka, D.; Guigay, J.; Goere, D.; Debaere, T.; et al. Are G3 ENETS Neuroendocrine Neoplasms Heterogeneous? Endocr. Relat. Cancer 2013, 20, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Heetfeld, M.; Chougnet, C.N.; Olsen, I.H.; Rinke, A.; Borbath, I.; Crespo, G.; Barriuso, J.; Pavel, M.; O’Toole, D.; Walter, T.; et al. Characteristics and Treatment of Patients with G3 Gastroenteropancreatic Neuroendocrine Neoplasms. Endocr. Relat. Cancer 2015, 22, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Sorbye, H.; Welin, S.; Langer, S.W.; Vestermark, L.W.; Holt, N.; Osterlund, P.; Dueland, S.; Hofsli, E.; Guren, M.G.; Ohrling, K.; et al. Predictive and Prognostic Factors for Treatment and Survival in 305 Patients with Advanced Gastrointestinal Neuroendocrine Carcinoma (WHO G3): The NORDIC NEC Study. Ann. Oncol. 2013, 24, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Milione, M.; Maisonneuve, P.; Spada, F.; Pellegrinelli, A.; Spaggiari, P.; Albarello, L.; Pisa, E.; Barberis, M.; Vanoli, A.; Buzzoni, R.; et al. The Clinicopathologic Heterogeneity of Grade 3 Gastroenteropancreatic Neuroendocrine Neoplasms: Morphological Differentiation and Proliferation Identify Different Prognostic Categories. NEN 2017, 104, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Beasley, M.B.; Lantuejoul, S.; Abbondanzo, S.; Chu, W.-S.; Hasleton, P.S.; Travis, W.D.; Brambilla, E. The P16/Cyclin D1/Rb Pathway in Neuroendocrine Tumors of the Lung. Hum. Pathol. 2003, 34, 136–142. [Google Scholar] [CrossRef]
- Yuan, J.; Knorr, J.; Altmannsberger, M.; Goeckenjan, G.; Ahr, A.; Scharl, A.; Strebhardt, K. Expression of P16 and Lack of PRB in Primary Small Cell Lung Cancer. J. Pathol. 1999, 189, 358–362. [Google Scholar] [CrossRef]
- Furlan, D. Different Molecular Profiles Characterize Well-Differentiated Endocrine Tumors and Poorly Differentiated Endocrine Carcinomas of the Gastroenteropancreatic Tract. Clin. Cancer Res. 2004, 10, 947–957. [Google Scholar] [CrossRef]
- Ali, A.S.; Grönberg, M.; Federspiel, B.; Scoazec, J.-Y.; Hjortland, G.O.; Grønbæk, H.; Ladekarl, M.; Langer, S.W.; Welin, S.; Vestermark, L.W.; et al. Expression of P53 Protein in High-Grade Gastroenteropancreatic Neuroendocrine Carcinoma. PLoS ONE 2017, 12, e0187667. [Google Scholar] [CrossRef] [PubMed]
- Dowlati, A.; Lipka, M.B.; McColl, K.; Dabir, S.; Behtaj, M.; Kresak, A.; Miron, A.; Yang, M.; Sharma, N.; Fu, P.; et al. Clinical Correlation of Extensive-Stage Small-Cell Lung Cancer Genomics. Ann. Oncol. 2016, 27, 642–647. [Google Scholar] [CrossRef]
- Derks, J.L.; Leblay, N.; Thunnissen, E.; van Suylen, R.J.; den Bakker, M.; Groen, H.J.M.; Smit, E.F.; Damhuis, R.; van den Broek, E.C.; Charbrier, A.; et al. Molecular Subtypes of Pulmonary Large-Cell Neuroendocrine Carcinoma Predict Chemotherapy Treatment Outcome. Clin. Cancer Res. 2018, 24, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Hijioka, S.; Hosoda, W.; Matsuo, K.; Ueno, M.; Furukawa, M.; Yoshitomi, H.; Kobayashi, N.; Ikeda, M.; Ito, T.; Nakamori, S.; et al. Rb Loss and KRAS Mutation Are Predictors of the Response to Platinum-Based Chemotherapy in Pancreatic Neuroendocrine Neoplasm with Grade 3: A Japanese Multicenter Pancreatic NEN-G3 Study. Clin. Cancer Res. 2017, 23, 4625–4632. [Google Scholar] [CrossRef]
- Tanaka, H.; Hijioka, S.; Hosoda, W.; Ueno, M.; Kobayashi, N.; Ikeda, M.; Ito, T.; Kodama, Y.; Morizane, C.; Notohara, K.; et al. Pancreatic Neuroendocrine Carcinoma G3 May Be Heterogeneous and Could Be Classified into Two Distinct Groups. Pancreatology 2020, 20, 1421–1427. [Google Scholar] [CrossRef] [PubMed]
- Chan, B.A.; Coward, J.I.G. Chemotherapy Advances in Small-Cell Lung Cancer. J. Thorac. Dis. 2013, 5, 14. [Google Scholar]
- Tang, L.H.; Basturk, O.; Sue, J.J.; Klimstra, D.S. A Practical Approach to the Classification of WHO Grade 3 (G3) Well-Differentiated Neuroendocrine Tumor (WD-NET) and Poorly Differentiated Neuroendocrine Carcinoma (PD-NEC) of the Pancreas. Am. J. Surg. Pathol. 2016, 40, 1192–1202. [Google Scholar] [CrossRef]
- Travis, W.D.; Gal, A.A.; Colby, T.V.; Klimstra, D.S.; Falk, R.; Koss, M.N. Reproducibility of Neuroendocrine Lung Tumor Classification. Hum. Pathol. 1998, 29, 272–279. [Google Scholar] [CrossRef]
- Rossi, A.; Di Maio, M.; Chiodini, P.; Rudd, R.M.; Okamoto, H.; Skarlos, D.V.; Früh, M.; Qian, W.; Tamura, T.; Samantas, E.; et al. Carboplatin- or Cisplatin-Based Chemotherapy in First-Line Treatment of Small-Cell Lung Cancer: The COCIS Meta-Analysis of Individual Patient Data. JCO 2012, 30, 1692–1698. [Google Scholar] [CrossRef]
- Hiroshima, K.; Iyoda, A.; Shida, T.; Shibuya, K.; Iizasa, T.; Kishi, H.; Tanizawa, T.; Fujisawa, T.; Nakatani, Y. Distinction of Pulmonary Large Cell Neuroendocrine Carcinoma from Small Cell Lung Carcinoma: A Morphological, Immunohistochemical, and Molecular Analysis. Mod. Pathol. 2006, 19, 1358–1368. [Google Scholar] [CrossRef] [PubMed]
- Takizawa, N.; Ohishi, Y.; Hirahashi, M.; Takahashi, S.; Nakamura, K.; Tanaka, M.; Oki, E.; Takayanagi, R.; Oda, Y. Molecular Characteristics of Colorectal Neuroendocrine Carcinoma; Similarities with Adenocarcinoma Rather than Neuroendocrine Tumor. Hum. Pathol. 2015, 46, 1890–1900. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, T.; Jiang, S.-X.; Kameya, T.; Asamura, H.; Sato, Y.; Nagai, K.; Okayasu, I. Divergent Cyclin B1 Expression and Rb/P16/Cyclin D1 Pathway Aberrations among Pulmonary Neuroendocrine Tumors. Mod. Pathol. 2004, 17, 1259–1267. [Google Scholar] [CrossRef][Green Version]
- Švajdler, M.; Mezencev, R.; Ondič, O.; Šašková, B.; Mukenšnábl, P.; Michal, M. P16 Is a Useful Supplemental Diagnostic Marker of Pulmonary Small Cell Carcinoma in Small Biopsies and Cytology Specimens. Ann. Diagn. Pathol. 2018, 33, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Fouquet, C.; Antoine, M.; Tisserand, P.; Favis, R.; Wislez, M.; Commo, F.; Rabbe, N.; Carette, M.F.; Milleron, B.; Barany, F.; et al. Rapid and Sensitive P53 Alteration Analysis in Biopsies from Lung Cancer Patients Using a Functional Assay and a Universal Oligonucleotide Array: A Prospective Study. Clin. Cancer Res. 2004, 10, 3479–3489. [Google Scholar] [CrossRef][Green Version]
- Soussi, T.; Béroud, C. Assessing TP53 Status in Human Tumours to Evaluate Clinical Outcome. Nat. Rev. Cancer 2001, 1, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Reid, M.D.; Bagci, P.; Ohike, N.; Saka, B.; Erbarut Seven, I.; Dursun, N.; Balci, S.; Gucer, H.; Jang, K.-T.; Tajiri, T.; et al. Calculation of the Ki67 Index in Pancreatic Neuroendocrine Tumors: A Comparative Analysis of Four Counting Methodologies. Mod. Pathol. 2015, 28, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A Simulation Study of the Number of Events per Variable in Logistic Regression Analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]

| Baseline Characteristics | All (n = 89) |
|---|---|
| Age (years), median (IQR) | 61.6 (54.2–68.6) |
| Male gender, n (%) | 60 (67.4) |
| Hereditary syndrome, n (%) | 1 (1.1) |
| Current or previous tobacco use, n (%) | 49/71 (69) |
| Performance status, n (%) | |
| 0–1 | 61/78 (78.2) |
| ≥2 | 17/78 (21.7) |
| Primary NEN, n (%) | |
| Lung | 37 (41.6) |
| Pancreas | 27 (30.3) |
| Other digestive | 25 (28.1) |
| Functioning syndrome, n (%) | 1 (1.1) |
| Tumor stage, n (%) | |
| Localized or locally advanced | 18 (20.2) |
| Liver metastases | 61 (68.5) |
| Extra-hepatic metastases | 43 (48.3) |
| 2019 WHO classification, n (%) | |
| G3 NET | 10 (11.2) |
| LCNEC | 31 (34.8) |
| SCNEC | 48 (54.0) |
| Ki67 (%), median (IQR) * | 80.0 (57.5–90.0) |
| Biology, median (IQR) | |
| Albumin (g/L) ** | 32.0 (28.0–36.7) |
| Platelets (G/L) *** | 288.0 (210.2–381.8) |
| Hemoglobin (g/dl) *** | 11.9 (10.7–13.3) |
| Leukocytes (G/L) *** | 8.3 (6.3–10.8) |
| Alkaline phosphatase (UNL) *** | 1.3 (0.6–2.5) |
| OR (95%CI) | p Value | |
|---|---|---|
| Model 1: Rbinap | ||
| Lung primary (vs. other locations) | 0.70 (0.21–2.38) | 0.570 |
| SCNEC (vs. NET or LCNEC) | 8.89 (2.26–30.4) | 0.001 |
| Rbinap (vs. Rbapp) | 1.70 (0.54–5.37) | 0.368 |
| Ki-67 (each additional 1%) | 1 50.97–1.02) | 0.550 |
| Model 2: Rb < 150 | ||
| Lung primary (vs. other locations) | 0.70 (0.20–2.41) | 0.566 |
| SCNEC (vs. NET or LCNEC) | 7.83 (2.25–27.28) | 0.001 |
| Rb < 150 (vs. Rb score ≥ 150) | 4.16 (1.11–15.53) | 0.034 |
| Ki-67 (each additional 1%) | 0.99 (0.96–1.01) | 0.309 |
| Model 3: p16high | ||
| Lung primary (vs. other locations) | 0.71 (0.21–2.47) | 0.602 |
| SCNEC (vs. NET or LCNEC) | 7.63 (2.19–26.57) | 0.001 |
| p16high (vs. p16low) | 1.61 (0.47–5.56) | 0.449 |
| Ki-67 (each additional 1%) | 1 (0.97–1.02) | 0.804 |
| HR (95%CI) | p Value | |
|---|---|---|
| Model 1: Rbinap | ||
| Lung primary (vs. other locations) | 1.39 (0.75–2.58) | 0.301 |
| SCNEC (vs. LCNEC) | 0.54 (0.29–1.03) | 0.06 |
| Ki-67 (each additional 1%) | 1.02 (1–1.03) | 0.028 |
| Extra-hepatic metastases (vs. absence) | 1.04 (0.62–1.75) | 0.87 |
| Rbinap (vs. Rbapp) | 0.57 (0.32–1.02) | 0.058 |
| Model 2: Rb < 150 | ||
| Lung primary (vs. other locations) | 1.31 (0.71–2.42) | 0.393 |
| SCNEC (vs. LCNEC) | 0.59 (0.31–1.1) | 0.097 |
| Ki-67 (each additional 1%) | 1.02 (1.00–1.04) | 0.014 |
| Extra-hepatic metastases (vs. absence) | 1.1 (0.66–1.84) | 0.712 |
| Rb < 150 (vs. Rb score ≥ 150) | 0.37 (0.17–0.8) | 0.012 |
| Model 3: p16high | ||
| Lung primary (vs. other locations) | 1.59 (0.82–3.09) | 0.167 |
| SCNEC (vs. LCNEC) | 0.54 (0.27–1.09) | 0.086 |
| Ki-67 (each additional 1%) | 1.02 (1–1.04) | 0.018 |
| Extra-hepatic metastases (vs. absence) | 1.19 (0.71–1.98) | 0.518 |
| p16high (vs. p16low) | 0.39 (0.19–0.79) | 0.009 |
| HR (95%CI) | p Value | |
|---|---|---|
| Model 1: Rbinap | ||
| Lung primary (vs. other locations) | 1.61 (0.87–2.99) | 0.131 |
| SCNEC (vs. LCNEC) | 0.69 (0.37–1.27) | 0.230 |
| Ki-67 (each additional 1%) | 1 (1.00–1.02) | 0.166 |
| Extra-hepatic metastases | 1.95 (1.12–3.25) | 0.010 |
| Rbinap (vs. Rbapp) | 0.54 (0.31–0.95) | 0.033 |
| Model 2: Rb < 150 | ||
| Lung primary (vs. other locations) | 1.56 (0.84–2.91) | 0.157 |
| SCNEC (vs. LCNEC) | 0.74 (0.40–1.39) | 0.350 |
| Ki-67 (each additional 1%) | 1.01 (1–1.02) | 0.151 |
| Extra-hepatic metastases | 2.03 (1.21–3.41) | 0.007 |
| Rb < 150 (vs. Rb score ≥ 150) | 0.50 (0.25–1.01) | 0.053 |
| Model 3: p16high | ||
| Lung primary (vs. other locations) | 1.55 (0.82–2.95) | 0.179 |
| SCNEC (vs. LCNEC) | 0.79 (0.39–1.59) | 0.507 |
| Ki-67 (each additional 1%) | 1.01 (1–1.02) | 0.172 |
| Extra-hepatic metastases | 2.08 (1.24–3.49) | 0.005 |
| p16high (vs. p16low) | 0.52 (0.26–1.05) | 0.067 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lacombe, C.; De Rycke, O.; Couvelard, A.; Turpin, A.; Cazes, A.; Hentic, O.; Gounant, V.; Zalcman, G.; Ruszniewski, P.; Cros, J.; et al. Biomarkers of Response to Etoposide-Platinum Chemotherapy in Patients with Grade 3 Neuroendocrine Neoplasms. Cancers 2021, 13, 643. https://doi.org/10.3390/cancers13040643
Lacombe C, De Rycke O, Couvelard A, Turpin A, Cazes A, Hentic O, Gounant V, Zalcman G, Ruszniewski P, Cros J, et al. Biomarkers of Response to Etoposide-Platinum Chemotherapy in Patients with Grade 3 Neuroendocrine Neoplasms. Cancers. 2021; 13(4):643. https://doi.org/10.3390/cancers13040643
Chicago/Turabian StyleLacombe, Caroline, Ophélie De Rycke, Anne Couvelard, Anthony Turpin, Aurélie Cazes, Olivia Hentic, Valérie Gounant, Gérard Zalcman, Philippe Ruszniewski, Jérôme Cros, and et al. 2021. "Biomarkers of Response to Etoposide-Platinum Chemotherapy in Patients with Grade 3 Neuroendocrine Neoplasms" Cancers 13, no. 4: 643. https://doi.org/10.3390/cancers13040643
APA StyleLacombe, C., De Rycke, O., Couvelard, A., Turpin, A., Cazes, A., Hentic, O., Gounant, V., Zalcman, G., Ruszniewski, P., Cros, J., & de Mestier, L. (2021). Biomarkers of Response to Etoposide-Platinum Chemotherapy in Patients with Grade 3 Neuroendocrine Neoplasms. Cancers, 13(4), 643. https://doi.org/10.3390/cancers13040643








