Risk-Predictive and Diagnostic Biomarkers for Colorectal Cancer; a Systematic Review of Studies Using Pre-Diagnostic Blood Samples Collected in Prospective Cohorts and Screening Settings
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
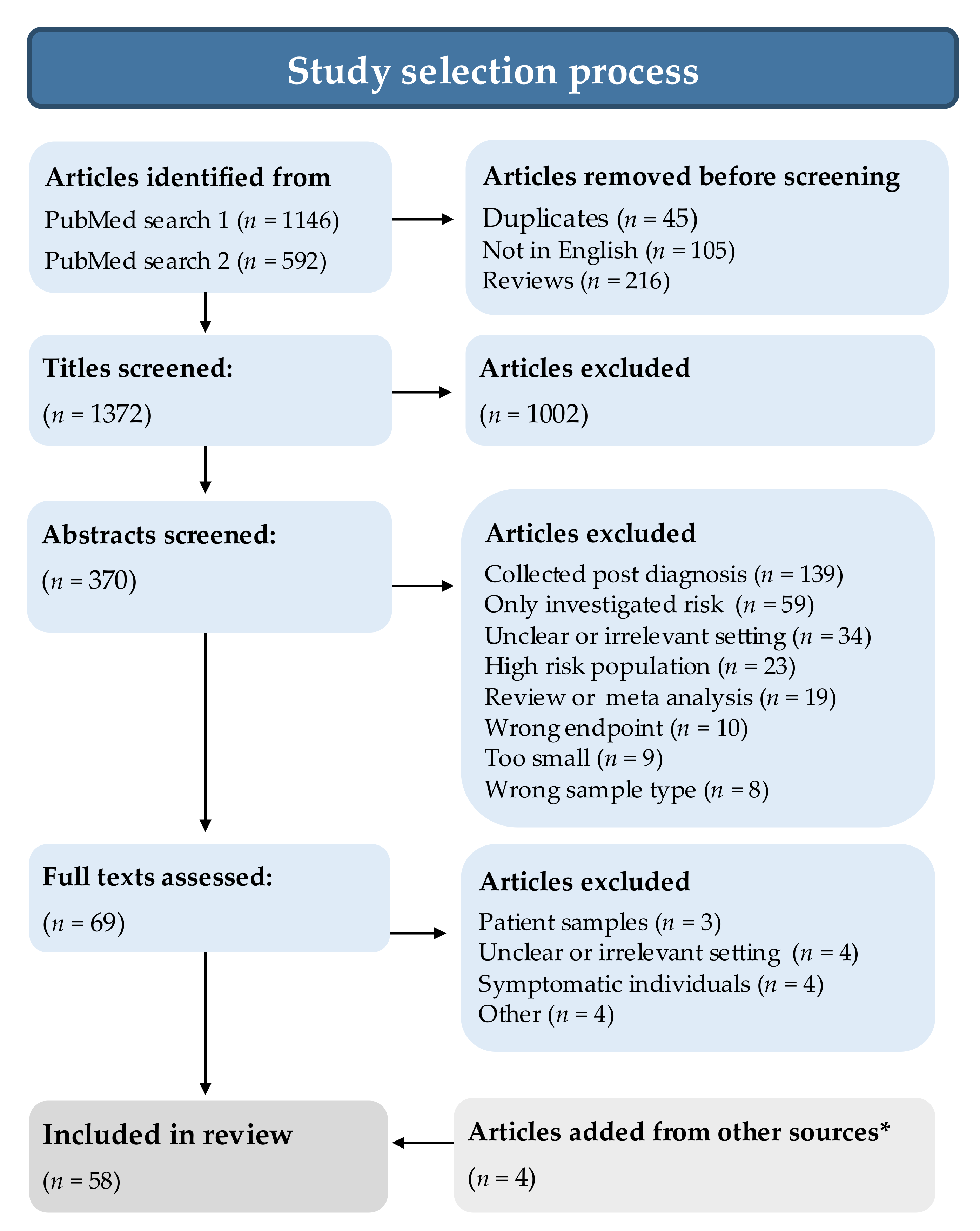
2.4. Selection Process
2.5. Data Collection Process
2.6. Data Items
2.7. Quality Assessment
3. Results and Interpretation
3.1. Study Selection
3.2. Study Characteristics
3.3. Biomarkers
3.3.1. Proteins
3.3.2. Metabolites
3.3.3. Antibodies
3.3.4. Nucleic Acids
3.3.5. Other Markers
4. Discussion
4.1. Limitations of the Evidence
4.2. Limitations of Review Processes
4.3. Implications for Practice and Policy
4.4. Future Research Perspectives
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Goding Sauer, A.; Fedewa, S.A.; Butterly, L.F.; Anderson, J.C.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Stock, C.; Hoffmeister, M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: Systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ 2014, 348, g2467. [Google Scholar] [CrossRef] [PubMed]
- De Klerk, C.M.; Gupta, S.; Dekker, E.; Essink-Bot, M.L. Socioeconomic and ethnic inequities within organised colorectal cancer screening programmes worldwide. Gut 2018, 67, 679–687. [Google Scholar] [CrossRef]
- Imperiale, T.F.; Ransohoff, D.F.; Itzkowitz, S.H.; Levin, T.R.; Lavin, P.; Lidgard, G.P.; Ahlquist, D.A.; Berger, B.M. Multitarget stool DNA testing for colorectal-cancer screening. N. Engl. J. Med. 2014, 370, 1287–1297. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.E.; Paik, H.Y.; Yoon, H.; Lee, J.E.; Kim, N.; Sung, M.K. Sex- and gender-specific disparities in colorectal cancer risk. World J. Gastroenterol. 2015, 21, 5167–5175. [Google Scholar] [CrossRef]
- Yang, L.; Xiong, Z.; He, W.; Xie, K.; Liu, S.; Kong, P.; Jiang, C.; Guo, G.; Xia, L. Proximal shift of colorectal cancer with increasing age in different ethnicities. Cancer Manag. Res. 2018, 10, 2663–2673. [Google Scholar] [CrossRef]
- Church, T.R.; Wandell, M.; Lofton-Day, C.; Mongin, S.J.; Burger, M.; Payne, S.R.; Castanos-Velez, E.; Blumenstein, B.A.; Rosch, T.; Osborn, N.; et al. Prospective evaluation of methylated SEPT9 in plasma for detection of asymptomatic colorectal cancer. Gut 2014, 63, 317–325. [Google Scholar] [CrossRef]
- Potter, N.T.; Hurban, P.; White, M.N.; Whitlock, K.D.; Lofton-Day, C.E.; Tetzner, R.; Koenig, T.; Quigley, N.B.; Weiss, G. Validation of a real-time PCR-based qualitative assay for the detection of methylated SEPT9 DNA in human plasma. Clin. Chem. 2014, 60, 1183–1191. [Google Scholar] [CrossRef]
- Lin, J.S.; Perdue, L.A.; Henrikson, N.B.; Bean, S.I.; Blasi, P.R. Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2021, 325, 1978–1998. [Google Scholar] [CrossRef]
- Hull, M.A.; Rees, C.J.; Sharp, L.; Koo, S. A risk-stratified approach to colorectal cancer prevention and diagnosis. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Akimoto, N.; Ugai, T.; Zhong, R.; Hamada, T.; Fujiyoshi, K.; Giannakis, M.; Wu, K.; Cao, Y.; Ng, K.; Ogino, S. Rising incidence of early-onset colorectal cancer—A call to action. Nat. Rev. Clin. Oncol. 2021, 18, 230–243. [Google Scholar] [CrossRef]
- Aleksandrova, K.; Reichmann, R.; Kaaks, R.; Jenab, M.; Bueno-de-Mesquita, H.B.; Dahm, C.C.; Eriksen, A.K.; Tjonneland, A.; Artaud, F.; Boutron-Ruault, M.C.; et al. Development and validation of a lifestyle-based model for colorectal cancer risk prediction: The LiFeCRC score. BMC Med. 2021, 19, 1. [Google Scholar] [CrossRef] [PubMed]
- Jeon, J.; Du, M.; Schoen, R.E.; Hoffmeister, M.; Newcomb, P.A.; Berndt, S.I.; Caan, B.; Campbell, P.T.; Chan, A.T.; Chang-Claude, J.; et al. Determining Risk of Colorectal Cancer and Starting Age of Screening Based on Lifestyle, Environmental, and Genetic Factors. Gastroenterology 2018, 154, 2152–2164.e2119. [Google Scholar] [CrossRef] [PubMed]
- Schmit, S.L.; Edlund, C.K.; Schumacher, F.R.; Gong, J.; Harrison, T.A.; Huyghe, J.R.; Qu, C.; Melas, M.; Van Den Berg, D.J.; Wang, H.; et al. Novel Common Genetic Susceptibility Loci for Colorectal Cancer. J. Natl. Cancer Inst. 2019, 111, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.; Muller, D.C.; Moons, K.G.M.; Cross, A.J.; Johansson, M.; Ferrari, P.; Fagherazzi, G.; Peeters, P.H.M.; Severi, G.; Husing, A.; et al. Comparison of prognostic models to predict the occurrence of colorectal cancer in asymptomatic individuals: A systematic literature review and external validation in the EPIC and UK Biobank prospective cohort studies. Gut 2019, 68, 672–683. [Google Scholar] [CrossRef]
- Bhardwaj, M.; Gies, A.; Werner, S.; Schrotz-King, P.; Brenner, H. Blood-Based Protein Signatures for Early Detection of Colorectal Cancer: A Systematic Review. Clin. Transl. Gastroenterol. 2017, 8, e128. [Google Scholar] [CrossRef]
- Nikolaou, S.; Qiu, S.; Fiorentino, F.; Rasheed, S.; Tekkis, P.; Kontovounisios, C. Systematic review of blood diagnostic markers in colorectal cancer. Tech. Coloproctol. 2018, 22, 481–498. [Google Scholar] [CrossRef]
- Chen, X.; Gole, J.; Gore, A.; He, Q.; Lu, M.; Min, J.; Yuan, Z.; Yang, X.; Jiang, Y.; Zhang, T.; et al. Non-invasive early detection of cancer four years before conventional diagnosis using a blood test. Nat. Commun. 2020, 11, 3475. [Google Scholar] [CrossRef]
- Cohen, J.D.; Li, L.; Wang, Y.; Thoburn, C.; Afsari, B.; Danilova, L.; Douville, C.; Javed, A.A.; Wong, F.; Mattox, A.; et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 2018, 359, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 26 June 2021).
- Bailey, S.E.; Ukoumunne, O.C.; Shephard, E.A.; Hamilton, W. Clinical relevance of thrombocytosis in primary care: A prospective cohort study of cancer incidence using English electronic medical records and cancer registry data. Br. J. Gen. Pract. 2017, 67, e405–e413. [Google Scholar] [CrossRef]
- Song, M.; Mehta, R.S.; Wu, K.; Fuchs, C.S.; Ogino, S.; Giovannucci, E.L.; Chan, A.T. Plasma Inflammatory Markers and Risk of Advanced Colorectal Adenoma in Women. Cancer Prev. Res. 2016, 9, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Cock, C.; Anwar, S.; Byrne, S.E.; Meng, R.; Pedersen, S.; Fraser, R.J.L.; Young, G.P.; Symonds, E.L. Low Sensitivity of Fecal Immunochemical Tests and Blood-Based Markers of DNA Hypermethylation for Detection of Sessile Serrated Adenomas/Polyps. Dig. Dis. Sci. 2019, 64, 2555–2562. [Google Scholar] [CrossRef]
- De Chiara, L.; Paez de la Cadena, M.; Rodriguez-Berrocal, J.; Alvarez-Pardinas, M.C.; Pardinas-Anon, M.C.; Varela-Calvino, R.; Cordero, O.J. CD26-Related Serum Biomarkers: sCD26 Protein, DPP4 Activity, and Anti-CD26 Isotype Levels in a Colorectal Cancer-Screening Context. Dis. Markers 2020, 2020, 4347936. [Google Scholar] [CrossRef] [PubMed]
- Ivancic, M.M.; Anson, L.W.; Pickhardt, P.J.; Megna, B.; Pooler, B.D.; Clipson, L.; Reichelderfer, M.; Sussman, M.R.; Dove, W.F. Conserved serum protein biomarkers associated with growing early colorectal adenomas. Proc. Natl. Acad. Sci. USA 2019, 116, 8471–8480. [Google Scholar] [CrossRef] [PubMed]
- King, W.D.; Ashbury, J.E.; Taylor, S.A.; Tse, M.Y.; Pang, S.C.; Louw, J.A.; Vanner, S.J. A cross-sectional study of global DNA methylation and risk of colorectal adenoma. BMC Cancer 2014, 14, 488. [Google Scholar] [CrossRef][Green Version]
- Chen, H.; Zucknick, M.; Werner, S.; Knebel, P.; Brenner, H. Head-to-Head Comparison and Evaluation of 92 Plasma Protein Biomarkers for Early Detection of Colorectal Cancer in a True Screening Setting. Clin. Cancer Res. 2015, 21, 3318–3326. [Google Scholar] [CrossRef] [PubMed]
- Ladd, J.J.; Busald, T.; Johnson, M.M.; Zhang, Q.; Pitteri, S.J.; Wang, H.; Brenner, D.E.; Lampe, P.D.; Kucherlapati, R.; Feng, Z.; et al. Increased plasma levels of the APC-interacting protein MAPRE1, LRG1, and IGFBP2 preceding a diagnosis of colorectal cancer in women. Cancer Prev Res. 2012, 5, 655–664. [Google Scholar] [CrossRef]
- Lim, D.H.; Lee, J.H.; Kim, J.W. Feasibility of CYFRA 21-1 as a serum biomarker for the detection of colorectal adenoma and advanced colorectal adenoma in people over the age of 45. J. Clin. Lab. Anal. 2018, 32. [Google Scholar] [CrossRef]
- Thomas, D.S.; Fourkala, E.O.; Apostolidou, S.; Gunu, R.; Ryan, A.; Jacobs, I.; Menon, U.; Alderton, W.; Gentry-Maharaj, A.; Timms, J.F. Evaluation of serum CEA, CYFRA21-1 and CA125 for the early detection of colorectal cancer using longitudinal preclinical samples. Br. J. Cancer 2015, 113, 268–274. [Google Scholar] [CrossRef]
- Wen, Y.H.; Chang, P.Y.; Hsu, C.M.; Wang, H.Y.; Chiu, C.T.; Lu, J.J. Cancer screening through a multi-analyte serum biomarker panel during health check-up examinations: Results from a 12-year experience. Clin. Chim. Acta 2015, 450, 273–276. [Google Scholar] [CrossRef]
- Werner, S.; Krause, F.; Rolny, V.; Strobl, M.; Morgenstern, D.; Datz, C.; Chen, H.; Brenner, H. Evaluation of a 5-Marker Blood Test for Colorectal Cancer Early Detection in a Colorectal Cancer Screening Setting. Clin. Cancer Res. 2016, 22, 1725–1733. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.; Clarke, L.; Pal, A.; Buchwald, P.; Eglinton, T.; Wakeman, C.; Frizelle, F. A Review of the Role of Carcinoembryonic Antigen in Clinical Practice. Ann. Coloproctol. 2019, 35, 294–305. [Google Scholar] [CrossRef]
- Toriola, A.T.; Cheng, T.Y.; Neuhouser, M.L.; Wener, M.H.; Zheng, Y.; Brown, E.; Miller, J.W.; Song, X.; Beresford, S.A.; Gunter, M.J.; et al. Biomarkers of inflammation are associated with colorectal cancer risk in women but are not suitable as early detection markers. Int. J. Cancer 2013, 132, 2648–2658. [Google Scholar] [CrossRef] [PubMed]
- Touvier, M.; Fezeu, L.; Ahluwalia, N.; Julia, C.; Charnaux, N.; Sutton, A.; Mejean, C.; Latino-Martel, P.; Hercberg, S.; Galan, P.; et al. Pre-diagnostic levels of adiponectin and soluble vascular cell adhesion molecule-1 are associated with colorectal cancer risk. World J. Gastroenterol. 2012, 18, 2805–2812. [Google Scholar] [CrossRef]
- Tao, S.; Haug, U.; Kuhn, K.; Brenner, H. Comparison and combination of blood-based inflammatory markers with faecal occult blood tests for non-invasive colorectal cancer screening. Br. J. Cancer 2012, 106, 1424–1430. [Google Scholar] [CrossRef]
- Qian, J.; Tikk, K.; Werner, S.; Balavarca, Y.; Saadati, M.; Hechtner, M.; Brenner, H. Biomarker discovery study of inflammatory proteins for colorectal cancer early detection demonstrated importance of screening setting validation. J. Clin. Epidemiol. 2018, 104, 24–34. [Google Scholar] [CrossRef]
- Chen, H.; Qian, J.; Werner, S.; Cuk, K.; Knebel, P.; Brenner, H. Development and validation of a panel of five proteins as blood biomarkers for early detection of colorectal cancer. Clin. Epidemiol. 2017, 9, 517–526. [Google Scholar] [CrossRef]
- Bhardwaj, M.; Gies, A.; Weigl, K.; Tikk, K.; Benner, A.; Schrotz-King, P.; Borchers, C.H.; Brenner, H. Evaluation and Validation of Plasma Proteins Using Two Different Protein Detection Methods for Early Detection of Colorectal Cancer. Cancers 2019, 11, 1426. [Google Scholar] [CrossRef]
- Bhardwaj, M.; Weigl, K.; Tikk, K.; Holland-Letz, T.; Schrotz-King, P.; Borchers, C.H.; Brenner, H. Multiplex quantitation of 270 plasma protein markers to identify a signature for early detection of colorectal cancer. Eur. J. Cancer 2020, 127, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Vermeire, S.; Van Assche, G.; Rutgeerts, P. The role of C-reactive protein as an inflammatory marker in gastrointestinal diseases. Nat. Clin. Pract. Gastroenterol. Hepatol. 2005, 2, 580–586. [Google Scholar] [CrossRef]
- Brown, D.A.; Hance, K.W.; Rogers, C.J.; Sansbury, L.B.; Albert, P.S.; Murphy, G.; Laiyemo, A.O.; Wang, Z.; Cross, A.J.; Schatzkin, A.; et al. Serum macrophage inhibitory cytokine-1 (MIC-1/GDF15): A potential screening tool for the prevention of colon cancer? Cancer Epidemiol. Biomark. Prev. 2012, 21, 337–346. [Google Scholar] [CrossRef]
- Wilhelmsen, M.; Christensen, I.J.; Rasmussen, L.; Jorgensen, L.N.; Madsen, M.R.; Vilandt, J.; Hillig, T.; Klaerke, M.; Nielsen, K.T.; Laurberg, S.; et al. Detection of colorectal neoplasia: Combination of eight blood-based, cancer-associated protein biomarkers. Int. J. Cancer. 2017, 140, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.; Nielsen, H.J.; Christensen, I.J. Early Detection and Recurrence of Colorectal Adenomas by Combination of Eight Cancer-Associated Biomarkers in Plasma. Clin. Exp. Gastroenterol. 2020, 13, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Wild, N.; Andres, H.; Rollinger, W.; Krause, F.; Dilba, P.; Tacke, M.; Karl, J. A combination of serum markers for the early detection of colorectal cancer. Clin. Cancer Res. 2010, 16, 6111–6121. [Google Scholar] [CrossRef]
- Harlid, S.; Harbs, J.; Myte, R.; Brunius, C.; Gunter, M.J.; Palmqvist, R.; Liu, X.; Van Guelpen, B. A two-tiered targeted proteomics approach to identify pre-diagnostic biomarkers of colorectal cancer risk. Sci. Rep. 2021, 11, 5151. [Google Scholar] [CrossRef]
- Qian, J.; Tikk, K.; Weigl, K.; Balavarca, Y.; Brenner, H. Fibroblast growth factor 21 as a circulating biomarker at various stages of colorectal carcinogenesis. Br. J. Cancer 2018, 119, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Bertuzzi, M.; Marelli, C.; Bagnati, R.; Colombi, A.; Fanelli, R.; Saieva, C.; Ceroti, M.; Bendinelli, B.; Caini, S.; Airoldi, L.; et al. Plasma clusterin as a candidate pre-diagnosis marker of colorectal cancer risk in the Florence cohort of the European Prospective Investigation into Cancer and Nutrition: A pilot study. BMC Cancer 2015, 15, 56. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.; Neely, B.A.; Kao, T.C.; Eckhaus, J.; Bourgeois, J.; Brooks, J.; Jones, E.E.; Drake, R.R.; Zhu, K. Proteomic Profiling of Serial Prediagnostic Serum Samples for Early Detection of Colon Cancer in the U.S. Military. Cancer Epidemiol. Biomark. Prev. 2017, 26, 711–718. [Google Scholar] [CrossRef]
- Song, M.; Sasazuki, S.; Camargo, M.C.; Shimazu, T.; Charvat, H.; Yamaji, T.; Sawada, N.; Kemp, T.J.; Pfeiffer, R.M.; Hildesheim, A.; et al. Circulating inflammatory markers and colorectal cancer risk: A prospective case-cohort study in Japan. Int. J. Cancer 2018, 143, 2767–2776. [Google Scholar] [CrossRef]
- Rho, J.H.; Ladd, J.J.; Li, C.I.; Potter, J.D.; Zhang, Y.; Shelley, D.; Shibata, D.; Coppola, D.; Yamada, H.; Toyoda, H.; et al. Protein and glycomic plasma markers for early detection of adenoma and colon cancer. Gut 2018, 67, 473–484. [Google Scholar] [CrossRef]
- Butt, J.; Werner, S.; Willhauck-Fleckenstein, M.; Michel, A.; Waterboer, T.; Zornig, I.; Boleij, A.; Dramsi, S.; Brenner, H.; Pawlita, M. Serology of Streptococcus gallolyticus subspecies gallolyticus and its association with colorectal cancer and precursors. Int. J. Cancer 2017, 141, 897–904. [Google Scholar] [CrossRef]
- Li, B.; Shen, K.; Zhang, J.; Jiang, Y.; Yang, T.; Sun, X.; Ma, X.; Zhu, J. Serum netrin-1 as a biomarker for colorectal cancer detection. Cancer Biomark. 2020, 28, 391–396. [Google Scholar] [CrossRef]
- Cross, A.J.; Moore, S.C.; Boca, S.; Huang, W.Y.; Xiong, X.; Stolzenberg-Solomon, R.; Sinha, R.; Sampson, J.N. A prospective study of serum metabolites and colorectal cancer risk. Cancer 2014, 120, 3049–3057. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, T.; Floegel, A.; Sookthai, D.; Johnson, T.; Rolle-Kampczyk, U.; Otto, W.; von Bergen, M.; Boeing, H.; Kaaks, R. Higher plasma levels of lysophosphatidylcholine 18:0 are related to a lower risk of common cancers in a prospective metabolomics study. BMC Med. 2016, 14, 13. [Google Scholar] [CrossRef] [PubMed]
- Perttula, K.; Schiffman, C.; Edmands, W.M.B.; Petrick, L.; Grigoryan, H.; Cai, X.; Gunter, M.J.; Naccarati, A.; Polidoro, S.; Dudoit, S.; et al. Untargeted lipidomic features associated with colorectal cancer in a prospective cohort. BMC Cancer 2018, 18, 996. [Google Scholar] [CrossRef]
- Shu, X.; Xiang, Y.B.; Rothman, N.; Yu, D.; Li, H.L.; Yang, G.; Cai, H.; Ma, X.; Lan, Q.; Gao, Y.T.; et al. Prospective study of blood metabolites associated with colorectal cancer risk. Int. J. Cancer 2018, 143, 527–534. [Google Scholar] [CrossRef]
- Farshidfar, F.; Weljie, A.M.; Kopciuk, K.A.; Hilsden, R.; McGregor, S.E.; Buie, W.D.; MacLean, A.; Vogel, H.J.; Bathe, O.F. A validated metabolomic signature for colorectal cancer: Exploration of the clinical value of metabolomics. Br. J. Cancer 2016, 115, 848–857. [Google Scholar] [CrossRef] [PubMed]
- Butt, J.; Blot, W.J.; Teras, L.R.; Visvanathan, K.; Le Marchand, L.; Haiman, C.A.; Chen, Y.; Bao, Y.; Sesso, H.D.; Wassertheil-Smoller, S.; et al. Antibody Responses to Streptococcus Gallolyticus Subspecies Gallolyticus Proteins in a Large Prospective Colorectal Cancer Cohort Consortium. Cancer Epidemiol. Biomark. Prev. 2018, 27, 1186–1194. [Google Scholar] [CrossRef]
- Butt, J.; Blot, W.J.; Visvanathan, K.; Le Marchand, L.; Wilkens, L.R.; Chen, Y.; Sesso, H.D.; Teras, L.; Ryser, M.D.; Hyslop, T.; et al. Auto-antibodies to p53 and the Subsequent Development of Colorectal Cancer in a U.S. Prospective Cohort Consortium. Cancer Epidemiol. Biomark. Prev. 2020, 29, 2729–2734. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Werner, S.; Butt, J.; Zornig, I.; Knebel, P.; Michel, A.; Eichmuller, S.B.; Jager, D.; Waterboer, T.; Pawlita, M.; et al. Prospective evaluation of 64 serum autoantibodies as biomarkers for early detection of colorectal cancer in a true screening setting. Oncotarget 2016, 7, 16420–16432. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, J.W.; Gentry-Maharaj, A.; Nostdal, A.; Fourkala, E.O.; Dawnay, A.; Burnell, M.; Zaikin, A.; Burchell, J.; Papadimitriou, J.T.; Clausen, H.; et al. Cancer-associated autoantibodies to MUC1 and MUC4—A blinded case-control study of colorectal cancer in UK collaborative trial of ovarian cancer screening. Int. J. Cancer 2014, 134, 2180–2188. [Google Scholar] [CrossRef] [PubMed]
- Teras, L.R.; Gapstur, S.M.; Maliniak, M.L.; Jacobs, E.J.; Gansler, T.; Michel, A.; Pawlita, M.; Waterboer, T.; Campbell, P.T. Prediagnostic Antibodies to Serum p53 and Subsequent Colorectal Cancer. Cancer Epidemiol. Biomark. Prev. 2018, 27, 219–223. [Google Scholar] [CrossRef]
- Luo, X.; Stock, C.; Burwinkel, B.; Brenner, H. Identification and evaluation of plasma microRNAs for early detection of colorectal cancer. PLoS ONE 2013, 8, e62880. [Google Scholar] [CrossRef] [PubMed]
- Mai, D.; Zheng, Y.; Guo, H.; Ding, P.; Bai, R.; Li, M.; Ye, Y.; Zhang, J.; Huang, X.; Liu, D.; et al. Serum piRNA-54265 is a New Biomarker for early detection and clinical surveillance of Human Colorectal Cancer. Theranostics 2020, 10, 8468–8478. [Google Scholar] [CrossRef]
- Marcuello, M.; Duran-Sanchon, S.; Moreno, L.; Lozano, J.J.; Bujanda, L.; Castells, A.; Gironella, M. Analysis of A 6-Mirna Signature in Serum from Colorectal Cancer Screening Participants as Non-Invasive Biomarkers for Advanced Adenoma and Colorectal Cancer Detection. Cancers 2019, 11, 1542. [Google Scholar] [CrossRef]
- Wikberg, M.L.; Myte, R.; Palmqvist, R.; van Guelpen, B.; Ljuslinder, I. Plasma miRNA can detect colorectal cancer, but how early? Cancer Med. 2018, 7, 1697–1705. [Google Scholar] [CrossRef]
- Zanutto, S.; Ciniselli, C.M.; Belfiore, A.; Lecchi, M.; Masci, E.; Delconte, G.; Primignani, M.; Tosetti, G.; Dal Fante, M.; Fazzini, L.; et al. Plasma miRNA-based signatures in CRC screening programs. Int. J. Cancer 2020, 146, 1164–1173. [Google Scholar] [CrossRef] [PubMed]
- Bartak, B.K.; Kalmar, A.; Peterfia, B.; Patai, A.V.; Galamb, O.; Valcz, G.; Spisak, S.; Wichmann, B.; Nagy, Z.B.; Toth, K.; et al. Colorectal adenoma and cancer detection based on altered methylation pattern of SFRP1, SFRP2, SDC2, and PRIMA1 in plasma samples. Epigenetics 2017, 12, 751–763. [Google Scholar] [CrossRef]
- Barth, S.D.; Schulze, J.J.; Kuhn, T.; Raschke, E.; Husing, A.; Johnson, T.; Kaaks, R.; Olek, S. Treg-Mediated Immune Tolerance and the Risk of Solid Cancers: Findings From EPIC-Heidelberg. J. Natl. Cancer Inst. 2015, 107. [Google Scholar] [CrossRef]
- Heiss, J.A.; Brenner, H. Epigenome-wide discovery and evaluation of leukocyte DNA methylation markers for the detection of colorectal cancer in a screening setting. Clin. Epigenet. 2017, 9, 24. [Google Scholar] [CrossRef] [PubMed]
- Onwuka, J.U.; Li, D.; Liu, Y.; Huang, H.; Xu, J.; Liu, Y.; Zhang, Y.; Zhao, Y. A panel of DNA methylation signature from peripheral blood may predict colorectal cancer susceptibility. BMC Cancer 2020, 20, 692. [Google Scholar] [CrossRef]
- Warren, J.D.; Xiong, W.; Bunker, A.M.; Vaughn, C.P.; Furtado, L.V.; Roberts, W.L.; Fang, J.C.; Samowitz, W.S.; Heichman, K.A. Septin 9 methylated DNA is a sensitive and specific blood test for colorectal cancer. BMC Med. 2011, 9, 133. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Gao, Y.T.; Shu, X.O.; Wen, W.; Yang, G.; Li, G.; Courtney, R.; Ji, B.T.; Li, H.L.; Purdue, M.P.; et al. Association of leukocyte mitochondrial DNA copy number with colorectal cancer risk: Results from the Shanghai Women’s Health Study. Cancer Epidemiol. Biomark. Prev. 2014, 23, 2357–2365. [Google Scholar] [CrossRef]
- Nian, J.; Sun, X.; Ming, S.; Yan, C.; Ma, Y.; Feng, Y.; Yang, L.; Yu, M.; Zhang, G.; Wang, X. Diagnostic Accuracy of Methylated SEPT9 for Blood-based Colorectal Cancer Detection: A Systematic Review and Meta-Analysis. Clin. Transl. Gastroenterol. 2017, 8, e216. [Google Scholar] [CrossRef] [PubMed]
- Maffei, F.; Zolezzi Moraga, J.M.; Angelini, S.; Zenesini, C.; Musti, M.; Festi, D.; Cantelli-Forti, G.; Hrelia, P. Micronucleus frequency in human peripheral blood lymphocytes as a biomarker for the early detection of colorectal cancer risk. Mutagenesis 2014, 29, 221–225. [Google Scholar] [CrossRef]
- Myint, N.N.M.; Verma, A.M.; Fernandez-Garcia, D.; Sarmah, P.; Tarpey, P.S.; Al-Aqbi, S.S.; Cai, H.; Trigg, R.; West, K.; Howells, L.M.; et al. Circulating tumor DNA in patients with colorectal adenomas: Assessment of detectability and genetic heterogeneity. Cell Death Dis. 2018, 9, 894. [Google Scholar] [CrossRef] [PubMed]
- Okamura, T.; Hashimoto, Y.; Hamaguchi, M.; Obora, A.; Kojima, T.; Fukui, M. Triglyceride-glucose index (TyG index) is a predictor of incident colorectal cancer: A population-based longitudinal study. BMC Endocr. Disord. 2020, 20, 113. [Google Scholar] [CrossRef]
- Perttula, K.; Edmands, W.M.; Grigoryan, H.; Cai, X.; Iavarone, A.T.; Gunter, M.J.; Naccarati, A.; Polidoro, S.; Hubbard, A.; Vineis, P.; et al. Evaluating Ultra-long-Chain Fatty Acids as Biomarkers of Colorectal Cancer Risk. Cancer Epidemiol. Biomark. Prev. 2016, 25, 1216–1223. [Google Scholar] [CrossRef]
- Prizment, A.E.; Linabery, A.M.; Lutsey, P.L.; Selvin, E.; Nelson, H.H.; Folsom, A.R.; Church, T.R.; Drake, C.G.; Platz, E.A.; Joshu, C. Circulating Beta-2 Microglobulin and Risk of Cancer: The Atherosclerosis Risk in Communities Study (ARIC). Cancer Epidemiol. Biomark. Prev. 2016, 25, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Doherty, M.; Theodoratou, E.; Walsh, I.; Adamczyk, B.; Stockmann, H.; Agakov, F.; Timofeeva, M.; Trbojevic-Akmacic, I.; Vuckovic, F.; Duffy, F.; et al. Plasma N-glycans in colorectal cancer risk. Sci. Rep. 2018, 8, 8655. [Google Scholar] [CrossRef] [PubMed]
- Pilling, L.C.; Atkins, J.L.; Kuchel, G.A.; Ferrucci, L.; Melzer, D. Red cell distribution width and common disease onsets in 240,477 healthy volunteers followed for up to 9 years. PLoS ONE 2018, 13, e0203504. [Google Scholar] [CrossRef]
- Le Cornet, C.; Schildknecht, K.; Rossello Chornet, A.; Fortner, R.T.; Gonzalez Maldonado, S.; Katzke, V.A.; Kuhn, T.; Johnson, T.; Olek, S.; Kaaks, R. Circulating Immune Cell Composition and Cancer Risk: A Prospective Study Using Epigenetic Cell Count Measures. Cancer Res. 2020, 80, 1885–1892. [Google Scholar] [CrossRef]
- Murphy, G.; Cross, A.J.; Dawsey, S.M.; Stanczyk, F.Z.; Kamangar, F.; Weinstein, S.J.; Taylor, P.R.; Mannisto, S.; Albanes, D.; Abnet, C.C.; et al. Serum ghrelin is associated with risk of colorectal adenocarcinomas in the ATBC study. Gut 2018, 67, 1646–1651. [Google Scholar] [CrossRef]
- Sundkvist, A.; Myte, R.; Palmqvist, R.; Harlid, S.; Van Guelpen, B. Plasma ghrelin is probably not a useful biomarker for risk prediction or early detection of colorectal cancer. Gut 2018. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Altenhofen, L.; Tao, S. Matching of controls may lead to biased estimates of specificity in the evaluation of cancer screening tests. J. Clin. Epidemiol. 2013, 66, 202–208. [Google Scholar] [CrossRef]
- Gertsman, I.; Barshop, B.A. Promises and pitfalls of untargeted metabolomics. J. Inherit. Metab. Dis 2018, 41, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Ransohoff, D.F. Evaluating a New Cancer Screening Blood Test: Unintended Consequences and the Need for Clarity in Policy Making. J. Natl. Cancer Inst. 2021, 113, 109–111. [Google Scholar] [CrossRef]
- Williams, T.G.; Cubiella, J.; Griffin, S.J.; Walter, F.M.; Usher-Smith, J.A. Risk prediction models for colorectal cancer in people with symptoms: A systematic review. BMC Gastroenterol. 2016, 16, 63. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. [NG12] Suspected Cancer: Recognition and Referral. Available online: https://www.nice.org.uk/guidance/ng12 (accessed on 29 January 2021).
- Garcia-Albeniz, X.; Chan, A.T. Aspirin for the prevention of colorectal cancer. Best Pract. Res. Clin. Gastroenterol. 2011, 25, 461–472. [Google Scholar] [CrossRef]
- Higurashi, T.; Hosono, K.; Takahashi, H.; Komiya, Y.; Umezawa, S.; Sakai, E.; Uchiyama, T.; Taniguchi, L.; Hata, Y.; Uchiyama, S.; et al. Metformin for chemoprevention of metachronous colorectal adenoma or polyps in post-polypectomy patients without diabetes: A multicentre double-blind, placebo-controlled, randomised phase 3 trial. Lancet Oncol. 2016, 17, 475–483. [Google Scholar] [CrossRef]
- Rothwell, P.M.; Wilson, M.; Elwin, C.E.; Norrving, B.; Algra, A.; Warlow, C.P.; Meade, T.W. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet 2010, 376, 1741–1750. [Google Scholar] [CrossRef]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, D.; de Vet, H.C.; et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015, 351, h5527. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): The TRIPOD statement. Ann. Intern. Med. 2015, 162, 55–63. [Google Scholar] [CrossRef]

| Reference | Cohort (Design) | Time from Sampling to Diagnosis (Cohort Setting Only) | CRC | Adenoma | Contr./ Cohort | Biomarker/ Platform | Main Findings | Adapted NOS Scale ** Max: Selection = ★★★★ Comp. = ★★ Exp./Outc. = ★★★ |
|---|---|---|---|---|---|---|---|---|
| Cohort setting | ||||||||
| Ladd et al. Cancer Prev. Res, 2012 [29] | WHI (Nested case control) | 245 days (mean) 109 days (mean) | 90 32 | - | 90 * 32 * | Proteomics (MS): (1) 5022 unique protein IDs (2) 1779 quantified (3) 6 significant (p < 0.05) | Top markers: MAPRE1, LRG1, IGFBP2, Enolase 1, ARMET, PDIA3 Panel: MAPRE1, LRG1, IGFBP2 + CEA Validation set (4 marker panel): AUC: 0.72 Sensitivity: 41% Specificity: 95% | ★★★ ★★ ★★★ |
| Touvier et al. World J Gastroentero, 2012 [36] | SUVIMAX (Nested case control) | 6.5 years (median) | 50 | - | 100 * | Proteins: hs-CRP, Adiponectin, Leptin, sVCAM-1, sICAM-1, sE-selectin, MCP-1 | Top markers: Adiponectin Panel: Adiponectin, sVCAM Adiponectin: OR: 0.45 (95% CI: 0.22–0.91. p = 0.03) Panel (Adiponectin, sVCAM): AUC: 0.98 | ★★★ ★★ ★★★ |
| Toriola et al. Int J Cancer, 2013 [35] | WHI (Nested case control) | 3 years (cutoff, follow up) | 988 | - | 988 * | CRP, SAA | CRP (5th vs. 1st quintile, colon) OR: 1.37 (95% CI: 0.95–1.97) SAA (5th vs. 1st quintile, colon) OR: 1.26 (95% CI: 0.88–1.80) AUC (Both): 0.62 (95% CI: 0.55–0.68) | ★★★ ★★ ★★ |
| Thomas et al. Brit J Cancer, 2015 [31] | UKCTOCS (Nested case control) | 4 years (cutoff, serial samples) | 40 | - | 40 * | CEA, CYFRA21-1, CA12 | Top marker: CEA All stages AUC (CEA): 0–1 year before diagnosis: 0.74 1–2 years before diagnosis: 0.64 2–3 years before diagnosis: 0.61 3–4 years before diagnosis: 0.59 | ★★★★ ★★ ★★★ |
| Bertuzzi et al. BMC Cancer, 2015 [49] | EPIC- FLORENCE (Nested case control) | 3 years (mean) | 48 | - | 48 * | Global proteome analysis (phase 1 + 2) Targeted proteome analysis (phase 3): APOC2, CLU, CO4-B, CO9, FETUA, MASP2, MBL2, GRP2 | CLU (men only) AUC: 0.72 Sensitivity: 95% Specificity: 75% | ★★★ ★★ ★★★ |
| Song et al. Cancer Prev Res, 2016 [23] | NHS (Nested case control) | 10 years (median) | 757 | 757 * | MIC-1, CRP, IL-6, sTNFR-2 | MIC-1: (5th vs. 1st quintile) OR: 1.55 (95% CI: 1.03–2.32) | ★★★★ ★★ ★★★ | |
| Shao et al. Cancer Epidemiol Biomarkers Prev, 2017 [50] | AFHSC/DoDSR (Nested case control) | 8 years (cutoff, serial samples) | 397 | - | 397 * | Proteomics (MALDI-TOF MS) | Proteomic peaks: 2886.67, 2939.24, 3119.32, and 5078.81 The 4 peaks associated with CRC 1 year before diagnosis. Sensitivity: 69% Specificity: 67% | ★★★★ ★★ ★★★ |
| Song et al. Int. J Cancer, 2018 [51] | JPHC (Case- cohort) | 9.5 years (median) | 457 | - | 751 | 67 inflammatory and immunity markers | Top markers: CCL2/MCP1, CCL3/MIP1A, CCL15/MIP1D, CCL27/CTACK, CXCL6/GCP2, sTNFR2 HR (4th vs. 1st quartile) CCL2/MCP1: 1.69 sTNFR2: 1.61 CCL15/MIP1D: 1.39 CCL27/CTACK: 1.35 CXCL6/GCP2: 0.70 CCL3/MIP1A: 0.61 Significance lost after adjustments | ★★★★ ★★ ★★★ |
| Rho et al. Gut 2018 [52] | CHS(Nested case control) | 0–1 years (31 cases) 1–3 years (35 cases) | 79 | - | 79 * | Discovery: 1100 markers Pre validation: 78 markers | Final panel: BAG4, IL6ST, VWF, EGFR, CD44 Panel, all cancers versus all controls: AUC: 0.86 Sensitivity: 73% Specificity: 90% | ★★★ ★★ ★★★ |
| Harlid et al. Sci Rep, 2021 [47] | NSHDS (Nested case control) | 0.7 years (median) 6.7 years (median) | 58 450 | - | 58 * 450 * | Olink proteomic panels (Inflammation and Oncology II) | Top markers: FGF-21, PPY FGF-21, colon OR: 1.23 95% CI 1.03–1.47 6 marker panel, colon AUC: 0.63 PPY, rectum OR: 1.47 95% CI 1.12–1.9 AUC: 0.61 | ★★★★ ★★ ★★★ |
| Screening setting | ||||||||
| Chen H et al. Clin Cancer Res, 2015 [28] | BliTz (discovery set) | - | 35 | - | 54 | PEA (Olink Oncology I), 92 proteins | Top markers: (AUC > 6): AREG, CEA, GDF-15, IL-6 Multi-marker (8 proteins): AUC 0.76 (0.65–0.85), sensitivity 44% at 90% specificity | ★★★★ - ★★★ |
| Wen Y-H et al. Clin Chim Acta, 2015 [32] | General health screening at patient’s expense, Taoyuan, Taiwan | - | 26 | - | See footnote *** | AFP, CA 15-3, CA 125, PSA, SCC, CEA, CA 19-9, CYFRA 21-1 | Top markers: CEA, sensitivity 53.8%, CYFRA 21-1 sensitivity 38.9 Multi-marker panel (all 8 markers): sensitivity 76.9% | ★★★★ - ★★★ |
| Tao S, et al. Br J. Cancer, 2015 [37] | BliTz | - | - | AA: 193 | 225 | CRP, sCD26, complement C3a anaphylatoxin, TIMP-1 | CRP: AUC 0.50 (0.45–0.55) C3a: AUC 0.52 (0.47–0.57) sCD26: AUC 0.54 (0.49–0.59) TIMP-1: AUC 0.58 (0.53–0.63) | ★★★★ ★ ★★★ |
| Werner S, et al. Clin Cancer Res, 2016 [33] | BliTz (validation study) | - | 36 | AA: 420 | 1200 | CEA, ferritin, seprase, osteopontin, anti-p53 antibody **** | 5-marker panel, CRC: AUC 0.78 (0.68–0.87), sensitivity 42% (26–59) at 95% specificity 5-marker panel, AA: AUC 0.56 (0.53–0.59), sensitivity 9% (6–12) at 95% specificity CEA+anti-p53, CRC: AUC 0.85 (0.78–0.91), sensitivity 45% at 95% specificity CEA+anti-p53, AA: AUC 0.56 (0.53–0.59), sensitivity 6% at 95% specificity | ★★★★ - ★★★ |
| Butt J et al. Int J Cancer, 2017 [53] | BliTz | - | 50 | AA: 100 NAA: 30 | 228 | Multiplex serology (11 proteins) for Streptococcus gallolyticus subsp. gallolyticus Tested: individual proteins, any protein, ≥2 of 6-protein panel, Gallo2178-Gallo217 double-positivity | CRC: Gallo2178: OR 3.19 (1.11–9.21) AA: Gallo0933: OR 2.02 (CI: 1.01–4.04) | ★★★★ ★★ ★★★ |
| Chen H et al. Clin Epidemiol, 2017 [39] | BliTz (validation set) | - | 41 | AA: 106 | 107 | PEA (Olink Oncology I v.2, 92 proteins) and serum p53 antibodies | Top markers, CRC: 12 proteins in both discovery and validation sets using Wilcoxon (10 with AUC > 6) Multi-marker (GDF-15, AREG, FasL, Flt3L), CRC: AUC 0.81 (0.73–0.88), sensitivity 53.6% at 90% specificity, AA: AUC 0.58 (0.51–0.65), sensitivity 18.9 at 90% specificity Multi-marker + p53, CRC: AUC 0.82 (0.74–0.90), sensitivity 56.4 at 90% specificity, AA: 0.60 (0.52–0.69), sens. 22.0 at 90% specificity | ★★★★ ★★ ★★★ |
| Qian J et al. Br J Cancer 2018 [48] | BliTz (validation set) | - | 45 | AA: 80 NAA: 72 | 250 * | PEA (Olink Inflammation I, 92 proteins) | FGF-21, CRC: AUC 0.71 (0.61–0.81), sensitivity 37.1% at 90% specificity, OR highest vs. lowest tertile 3.92 (1.51–12.18) FGF-21, AA: 0.57 (0.50–0.63), sensitivity 11.1% at 90% specificity, OR highest vs. lowest tertile 2.24 (1.18–4.44) | ★★★★ ★★ ★★★ |
| Qian et al. J Clin Epidemiol, 2018 [38] | BliTz (validation set) | - | 42 | - | 84 * | PEA (Olink Inflammation I, 92 proteins) | Individual proteins: AUC > 6 for 13 proteins, of which 5 overlapped with discovery set results. Sensitivity >25% at 90% specificity for 5 proteins, of which one overlapped with discovery results. 5-protein panel (FGF-23, CSF-1, Flt3L, DNER, MCP-1): AUC 0.59 (0.47–0.70), sensitivity 28.6% and 11.9% at 90% and 95% specificity, respectively | ★★★★ ★★ ★★★ |
| Lim DH, et al. J Clin Lab Anal, 2018 [30] | Screening patients, Cheonan, South Korea | - | - | AA: 59 NAA: 232 | 223 | CYFRA 21- 1, CEA, CA19- 9, AFP, hsCRP | Top markers, AA: CYFRA 21-1: AUC 0.732 (0.656–0.809), sensitivity 30.5%, CEA: AUC 0.628 (0.542–0.714) sensitivity 11.8%, hsCRP: AUC 0.637 (0.559–0.715), sensitivity not presented | ★★★ - ★★ |
| Bhardwaj M et al. Cancers, 2019 [40] | BliTz (validation set) | - | 56 | AA: 101 | 102 * | PEA. Tested 12 overlapping proteins from LC/MRM-MS and PEA (Olink Oncology II, Immune response and Cardiovascular III): CDH5, Gal, IGFBP2, MASP1, MMP9, MPO, OPN, PON3, PRTN3, SPARC, TFRC (TR), AREG | Top markers, CRC (AUC > 6): CDH5, OPN, TR, AREG Multi-marker, CRC (MASP1, OPN, PON3, TR, AREG): AUC 0.82 (0.74–0.89), sensitivity 50% at 90% specificity Multi-marker, AA (MASP1, OPN, PON3, TR, AREG): AUC 0.60 (0.51–0.69) | ★★★★ ★★ ★★★ |
| Bhardwaj M et al. Eur J Cancer, 2020 [41] | BliTz (validation set) | - | 56 | AA: 99 | 99 * | LC/MRM-MS, 270 proteins | Individual markers, CRC (44 proteins): AUC range 0.53 (0.44–0.63) to 0.77 (0.69–0.84) Multi-marker, CRC (A1AT, APOA1, HP, LRG1, PON3): AUC 0.79 (0.70–0.86), sensitivity 46% at 90% specificity Multi-marker, AA (early-stage CRC panel: HP, LRG1, PON3): AUC 0.65 (0.56–0.73), sensitivity 25% at 90% specificity | ★★★★ ★★ ★★★ |
| Li B, et al. Cancer Biomarkers, 2020 [54] | Health exam project, not otherwise specified, Jiangsu, China | - | 50 | AA: 50 | 150 * | Netrin-1 | CRC: OR highest vs. lowest (optimal cut-off) = 7.731 (3.618–16.519), AUC 0.759 (0.680–0.837), sensitivity 46% at 90% specificity AA: null | ★★ ★★ ★★★ |
| Reference | Cohort (Design) | Time from Sampling to Diagnosis (Cohort Setting Only) | CRC | Adenoma | Contr./ Cohort | Biomarker/ Platform | Main Findings | Adapted NOS Scale ** Max: Selection = ★★★★ Comp. = ★★ Exp./Outc. = ★★★ |
|---|---|---|---|---|---|---|---|---|
| Cohort setting | ||||||||
| Kühn et al. BMC Med, 2016 [56] | EPIC-HEIDELBERG (Case-cohort) | 6.6 years (median) | 163 | - | 774 | 120 metabolites: (acylcarnitines, amino acids, biogenic amines, phosphatidylcholines, sphingolipids, and hexoses) | Top markers: LysoPC a C18:0, PC ae C30:0 LysoPC a C18:0 (4th vs. 1st quartile) OR: 1.84 (95% CI: 1.02–3.34) PC ae C30:0 (4th vs. 1st quartile) OR: 0.50 (95% CI: 0.28–0.90) | ★★★ ★★ ★★★ |
| Shu et al. Int J Cancer, 2018 [58] | SWHS/SMHS (Nested case control) | Time stratification: <4 years and >4 years | 250 | - | 250 * | Metabolites in plasma: 35 metabolites associated with CRC at FDR-p < 0.05 | Top 9 panel: AUC: 0.76 Top 2 single metabolites: Picolinic acid: OR: 5.11 (95% CI: 2.33–11.20) PE(20:0/18:2): OR: 0.45 (95% CI: 0.29–0.70) | ★★★★ ★★ ★★★ |
| Cross et al. Cancer, 2014 [55] | PLCO (Nested case control) | 7.8 years (median) | 254 | - | 254 * | 676 serum metabolites (metabolon) | Leucyl-leucine (90th vs. 10th percentile)OR: 0.50 (95% CI: 0.32–0.80) Glycochenodeoxycholate (90th vs. 10th percentile, sex stratified) OR: 5.34 (95% CI: 2.09–13.68) Significance lost after adjustments | ★★★★ ★★ ★★★ |
| Perttula et al. BMC Cancer, 2018 [57] | EPIC-TURIN (Nested case control) | 7.5 years (median) | 66 | - | 66 * | Lipophilic metabolites incl. (ULCFAs): 8690 features, 9 selected | Top markers: IDs: 5080, 3207, 6054 and 839 Classification rate: 72% | ★★ ★★ ★★★ |
| Screening setting | ||||||||
| Farshidfar F et al. Br J Cancer, 2016 [59] | Screening patients, Calgary, Canada (discovery) | - | - | A: 31 | 254 | GC-MS untargeted metabolomics | Multi-marker profile: (14 metabolites): AUC 0.81 (0.70–0.92) | ★★★ ★★ ★★★ |
| Reference | Cohort (Design) | Time from Sampling to Diagnosis (Cohort Setting Only) | CRC | Adenoma | Contr./ Cohort | Biomarker/ Platform | Main Findings | Adapted NOS Scale ** Max: Selection = ★★★★ Comp. = ★★ Exp./Outc. = ★★★ |
|---|---|---|---|---|---|---|---|---|
| Cohort setting | ||||||||
| Pedersen et al. Int J Cancer, 2014 [63] | UKCTOCS (Nested case control) | 6.8 years (median) | 97 | - | 94 * | Autoantibodies: MUC1, MUC2 and MUC4 | Top markers: MUC1-STn, MUC1-Core3 MUC1-STn Sensitivity: 8.2% Specificity: 95% MUC1-Core3 Sensitivity: 13.4% Specificity: 95% | ★★★★ ★ ★★★ |
| Butt et al. Cancer Epidemiol Biomarkers Prev, 2018 [60] | CLUE, CPSII, HPFS, MEC, NHS, NYUWHS, PHS, PLCO, SCCS and WHI (Nested case control) | 4–18 years (median, different studies) | 4210 | - | 4210 * | Antibody responses to 9 Streptococcus gallolyticus (SGG) proteins | Top marker: Gallo2178 Gallo2178 All cases: OR: 1.23 (95% CI: 0.99–1.52) Diagnosed <10 years after blood draw: OR: 1.40 (95% CI: 1.09–1.79) | ★★★ ★★ ★★★ |
| Teras et al. Cancer Epidemiol Biomarkers Prev, 2018 [64] | CPSII (Nested case control) | 11 years (follow up) | 392 | - | 774 * | p53 autoantibodies | All cases: RR: 1.77 (95% CI: 1.12–2.78) Diagnosed <3 years after blood draw: RR: 2.26 (95% CI: 1.06–4.83) | ★★★★ ★★ ★★★ |
| Butt et al. Cancer Epidemiol Biomarkers Prev, 2020 [61] | CLUE, CPSII, HPFS, MEC, NHS, NYUWHS, PHS, PLCO, SCCS and WHI (Nested case control) | 7 years (median) | 3702 | - | 3702 * | p53 autoantibodies | All cases: OR: 1.33 (95% CI: 1.09–1.61) Diagnosed <4 years after blood draw: OR: 2.27 (95% CI: 1.62–3.19) | ★★★ ★★ ★★★ |
| Screening setting | ||||||||
| Chen H et al. Oncotarget, 2016 [62] | BliTz (validation study) | - | 49 | AA: 99 NAA: 29 | 100 | Autoantibodies to 64 tumor associated antigens Tested: individual proteins and 2- to 6-marker panels | Top hits: TP53, anti-IMPDH2, anti-MDM2, anti-MAGEA4 Best 2-marker panel (TP53, anti-IMPDH2): sensitivity CRC 10% (4–22), sensitivity AA 7 (3–14), specificity 95 (89–98) Best 6-marker panel (TP53+IMPDH2+MDM2 +MAGEA4+CTAG1 +MTDH), Sensitivity CRC 24% (15–38), sensitivity AA 25% (18–35), specificity 85% (77–91) | ★★★★ - ★★★ |
| Reference | Cohort (Design) | Time from Sampling to Diagnosis (Cohort Setting Only) | CRC | Adenoma | Contr./ Cohort | Biomarker/ Platform | Main Findings | Adapted NOS Scale ** Max: Selection = ★★★★ Comp. = ★★ Exp./Outc. = ★★★ |
|---|---|---|---|---|---|---|---|---|
| Cohort setting | ||||||||
| Wikberg et al. Cancer Med, 2018 [68] | NSHDS/VIP (Nested case control) | 20 years (maximum follow up) | 58 | - | 147 * | 12 miRNAs | Top panel: miRNA-21, miR-18a, miR-22, miR-25 4 marker panel: AUC: 0.93 Sensitivity: 67% Specificity: 90% | ★★★★ ★★ ★★★ |
| Mai et al. Theranostics, 2020 [66] | DFTJ (Nested case control) | 9 years (follow up) | 307 | - | 614 * | Serum piR-54265 | All cases: OR: 2.10 (95% CI: 1.66–2.65) Diagnosed <1 years after blood draw: OR: 2.80 (95% CI: 1.60–4.89) Diagnosed <2 years after blood draw: OR: 2.45 (95% CI: 1.49–4.03) Diagnosed <3 years after blood draw: OR: 1.24 (95% CI: 0.90–1.72) | ★★★ ★ ★★★ |
| Huang et al. Cancer Epidemiol Biomarkers Prev, 2014 [75] | SWHS (Nested case control) | Time stratification: <5 years and >5 years | 444 | - | 1423 | mtDNA copy number | OR (2nd vs. 3rd tertile): 1.26 (95% CI: 0.93–1.70) OR (1st vs. 3rd tertile): 1.44 (95% CI: 1.06–1.94) | ★★★★ ★ ★★★ |
| Dietmar Barth et al. J Natl Cancer Inst, 2015 [71] | EPIC-HEIDELBERG (Nested case control) | 6.4 years (mean) | 185 | - | 807 | “ImmunoCRIT” Cell type specific DNA methylation in Foxp3, CD3 and GAPDH loci | ImmunoCRIT HR (3rd vs. 1st tertile): 1.59 (95% CI: 0.99–2.54) | ★★★★ ★★ ★★★ |
| Onwuka et al. BMC Cancer, 2020 [73] | EPIC-TURIN (Nested case control) | 6.2 years (mean) | 166 | - | 424 * | Blood DNA methylation CpG- sites | Methylation risk score (MRS), based on 16 CpGs. OR (original dataset): 2.68 (95% CI: 2.13–3.38) OR (testing dataset): 2.02 (95% CI: 1.48–2.74) AUC: 0.82 | ★★★ ★ ★★★ |
| Chen et al. Nat Commun, 2020 [19] | TZL (Nested case control) | 4 years (cutoff, follow up) | 35 | - | 414 | PanSeer panel: Circulating tumor DNA from pre-diagnostic stomach, esophageal, colorectal, lung or liver cancer patients | Pre-diagnosis sensitivity (all cancers): 94.9 (95% CI: 88.5–98.3) | ★★★★ ★★ ★★★ |
| Screening setting | ||||||||
| Warren JD, et al. BMC Med, 2011 [74] | Screening patients, single community clinic, USA (validation) | - | - | A: 78 | See footnote *** | SEPT9 methylation, rtPCR in triplicate | Sensitivity 10% | ★★★★ - ★★★ |
| Luo X, et al., PLoS ONE, 2013 [65] | BliTz (validation set) | - | - | AA: 50 | 50 | Five miRNAs from discovery phase (miR-29a, -106b, -133a, -342-3p, -532-3p), seven candidate miRNAs (miR-18a, -20a, -21, -92a, -143, -145, -181b) | Null | ★★★★ - ★★★ |
| Church T, et al., Gut, 2014 [8] | PRESEPT **** (validation study) | - | 53 | AA: 314 NAA: 209 | 934 | SEPT9 methylation (Epi proColon Assay) | ≥1/2 runs positive, CRC: Sensitivity 48.2% (32.4–63.6), specificity 91.5% (89.7–93.1) ≥1/3 runs positive, CRC (post hoc): Sensitivity 63.9% (47.5–79.2), specificity 88.4% (86.2–90.4) ≥1/2 runs positive, AA: Sensitivity 11.2% (7.2–15.7) compared to 9.2% positive rate in controls | ★★★★ ★★ ★★★ |
| Maffei et al. Mutagenesis, 2014 [77] | FOB+ screening patients, Bologna, Italy | - | 25 | 26 “polyps” | 31 | Micronucleus frequency in peripheral blood lymphocytes | Mean micronucleus frequency in CRC > polyps > controls (all 3 t-tests p < 0.001) | ★★ ★★ ★★★ |
| Heiss JA, Brenner H Clin Epigenetics, 2017 [72] | BliTz (clinical+screening for discovery, divided for modelling) | - | 46 | - | 46 * | Leucocyte DNA methylation array | Top markers: cg04036920, cg14472551, cg12459502 Multi-marker (3 markers): C-statistic 0.74 (0.57–0.87) | ★★★★ ★★ ★★★ |
| Myint NNM, et al. Cell Death Dis, 2018 [78] | FOBT+ patients, BCSP | - | - | Pre- neoplastic lesions: 76 | 37 | Total cfDNA, and tumor-related mutations (BRAF, KRAS by ddPCR) and patient-specific assays for trunk mutations identified by multiregional targeted NGS of adenoma tissues | Null | ★★ - ★★★ |
| Barták BK, et al. Epigenetics, 2018 [70] | Screening patients, not otherwise specified (validation study) | - | 47 | AA: 37 | 37 | DNA methylation of SFRP1, SFRP2, SDC2 and PRIMA1 | Individual markers, CRC: all AUC >8, adenoma: all AUC > 6 Multi-marker (4 genes), CRC: AUC 0.978 (0.954–1.000), sensitivity 91.5%, specificity 97.3% Multi-marker (4 genes), adenoma: AUC 0.937 (0.885–0.989), sensitivity 89.2%, specificity 86.5% | ★★-★★★ |
| Marcuello M et al. Cancers, 2019 [67] | FIT+ screening patients, Barcelona, Spain (validation study) | - | 59 | AA: 74 | 80 | miR-29a-3p, miR-15b-5p, miR-18a-5p, miR-19a-3p, miR-19b-3p, miR-335-5p | Multi-marker (6 miRNAs), CRC: AUC 0.74 (0.65–0.82), sensitivity 81%, specificity 56% Multi-marker (6 miRNAs), AA: AUC 0.80 (0.72–0.87), sensitivity 81%, specificity 63% | ★★ - ★★ |
| Zanutto S, et al. Int J Cancer, 2020 [69] | FIT+ screening patients, Milan, Italy(discovery and validation sets) | - | Ext. valid. 33 | Ext. valid.AA:181 NAA: 313 | Ext. valid. 568 | miRNA Taqman array 13 miRNAS selected for validation (of which 4 excluded after hemolysis experiments) plus one candidate from a previous study | Individual markers, CRC: AUC ~0.6 for 5 best miRNAs, AA: AUC range for all miRNAs 0.589–0.608Multi-marker, CRC (hsa-miR-378, hsa-miR-342-3p): AUC 0.604 (0.504–0.704) Multi-marker, AA (hsa-miR-106b-5p, hsa-miR-483-5p, hsa-miR-323a-3p, hsa-miR-335-5p, hsa-miR-186-5p, hsa-miR-342-3p): AUC 0.608 (0.560–0.656) | ★★ ★★ ★★★ |
| Reference | Cohort (Design) | Time from Sampling to Diagnosis (Cohort Setting Only) | CRC | Adenoma | Contr./ Cohort | Biomarker/ Platform | Main Findings | Adapted NOS Scale ** Max: Selection = ★★★★ Comp. = ★★ Exp./Outc. = ★★★ |
|---|---|---|---|---|---|---|---|---|
| Cohort setting | ||||||||
| Perttula et al. Cancer Epidemiol Biomarkers Prev, 2016 [80] | EPIC-TURIN (Nested case control) | 7.1 years (baseline) | 95 | - | 95 * | Ultra-long Chain Fatty Acids (ULCFA) | Top markers: ULCFAs: 446, 466, 468, 492 and 494 Differences diminished with increasing time to diagnosis | ★★ ★★ ★★★ |
| Prizment et al. Cancer Epidemiol Biomarkers Prev, 2016 [81] | ARIC (Cohort) | 14.8 years (median follow up) | 255 | - | 12,300 | Beta-2-microglobulin (B2M) | HR (4th vs. 1st quartile): 2.21 (95% CI: 1.32–3.70) | ★★★ ★★ ★★★ |
| Doherty et al. Sci Rep, 2018 [82] | FINRISK (Nested case control) | 10 years (follow up) | 40 | - | 80 * | Plasma N-glycans | Top markers: F(6)A2G2, F(6)A2G2S(6)1 All peaks + age: AUC: 0.65 Sensitivity: 12.5% Specificity: 95% | ★★★ ★★ ★★★ |
| Pilling et al. Plos One, 2018 [83] | UK BIOBANK (Cohort) | 9 years (follow up) | 1327 | - | 240,477 | Red Blood Cell Distribution Width (RDW) | Higher RDW: sHR: 1.92 (95% CI: 1.36 to 2.72) | ★★★ ★★ ★★★ |
| Okamura et al. Bmc Endocr Disord, 2020 [79] | NAGALA (Cohort) | 4.4 years (median) | 116 | - | 27,921 | Triglyceride–glucose index (TyG index) | HR (TyG index): 1.38 (95% CI: 1.0–1.9) AUC: 0.69 Sensitivity: 62% Specificity: 67% | ★★ ★★ ★★★ |
| Le Cornet et al. Cancer Res, 2020 [84] | EPIC-HEIDELBERG (Case cohort) | 6.7 years (mean) | 111 | - | 465 | Immune cell counts (neutrophils, monocytes, and lymphocytes | Top finding: FOXP3+ T-cell counts HR: 1.59 (95% CI: 1.04–2.42) | ★★★★ ★★ ★★★ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harlid, S.; Gunter, M.J.; Van Guelpen, B. Risk-Predictive and Diagnostic Biomarkers for Colorectal Cancer; a Systematic Review of Studies Using Pre-Diagnostic Blood Samples Collected in Prospective Cohorts and Screening Settings. Cancers 2021, 13, 4406. https://doi.org/10.3390/cancers13174406
Harlid S, Gunter MJ, Van Guelpen B. Risk-Predictive and Diagnostic Biomarkers for Colorectal Cancer; a Systematic Review of Studies Using Pre-Diagnostic Blood Samples Collected in Prospective Cohorts and Screening Settings. Cancers. 2021; 13(17):4406. https://doi.org/10.3390/cancers13174406
Chicago/Turabian StyleHarlid, Sophia, Marc J. Gunter, and Bethany Van Guelpen. 2021. "Risk-Predictive and Diagnostic Biomarkers for Colorectal Cancer; a Systematic Review of Studies Using Pre-Diagnostic Blood Samples Collected in Prospective Cohorts and Screening Settings" Cancers 13, no. 17: 4406. https://doi.org/10.3390/cancers13174406
APA StyleHarlid, S., Gunter, M. J., & Van Guelpen, B. (2021). Risk-Predictive and Diagnostic Biomarkers for Colorectal Cancer; a Systematic Review of Studies Using Pre-Diagnostic Blood Samples Collected in Prospective Cohorts and Screening Settings. Cancers, 13(17), 4406. https://doi.org/10.3390/cancers13174406






