Consistency of Pituitary Adenoma: Prediction by Pharmacokinetic Dynamic Contrast-Enhanced MRI and Comparison with Histologic Collagen Content
Abstract
:Simple Summary
Abstract
1. Introduction
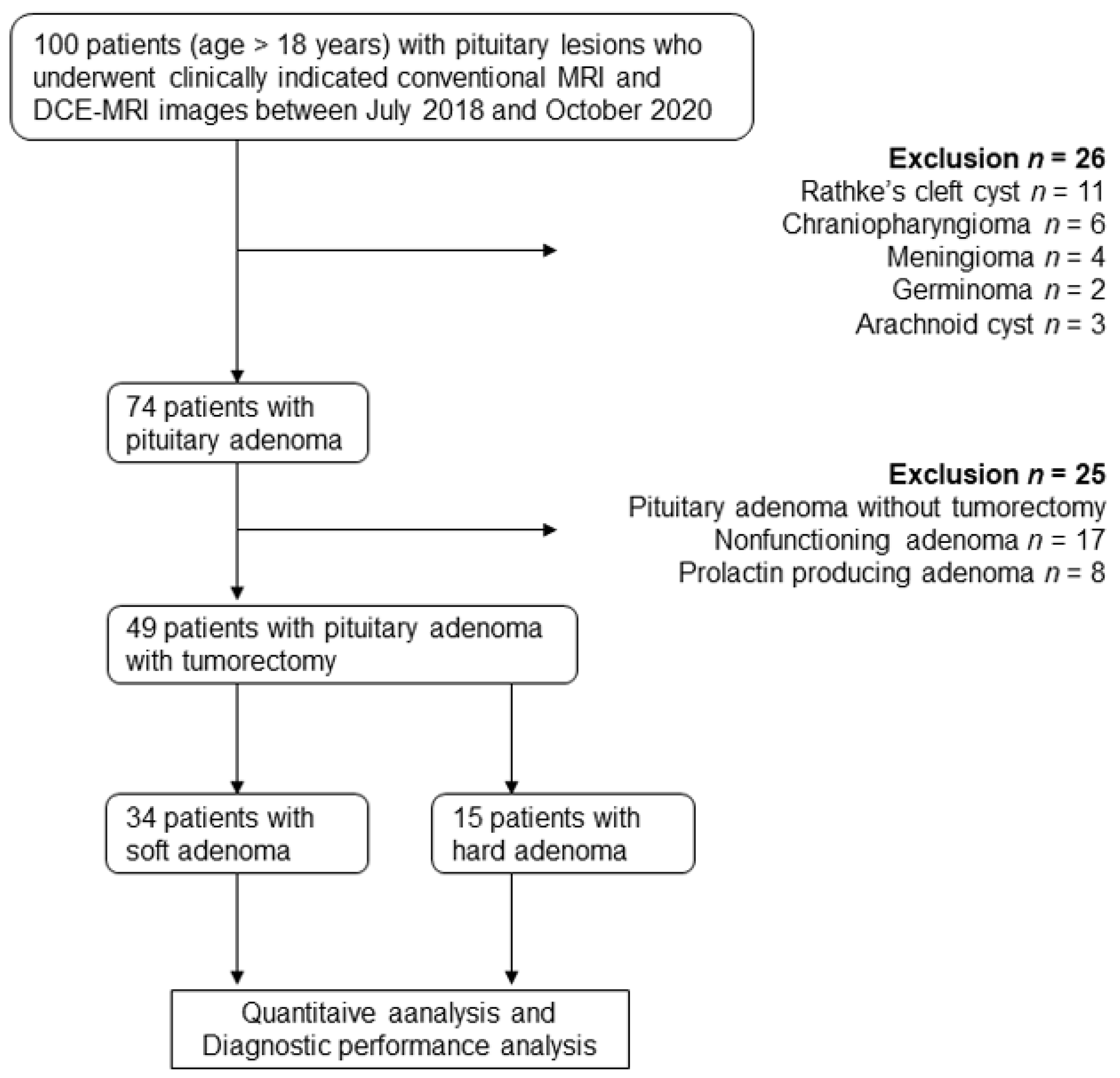
2. Materials and Methods
2.1. Participant Characteristics
2.2. Endocrine Studies
2.3. MRI Examinations
2.4. Measurement of Maximum Tumor Diameter and Volume
2.5. Parasellar Extension on MRI (Grading System)
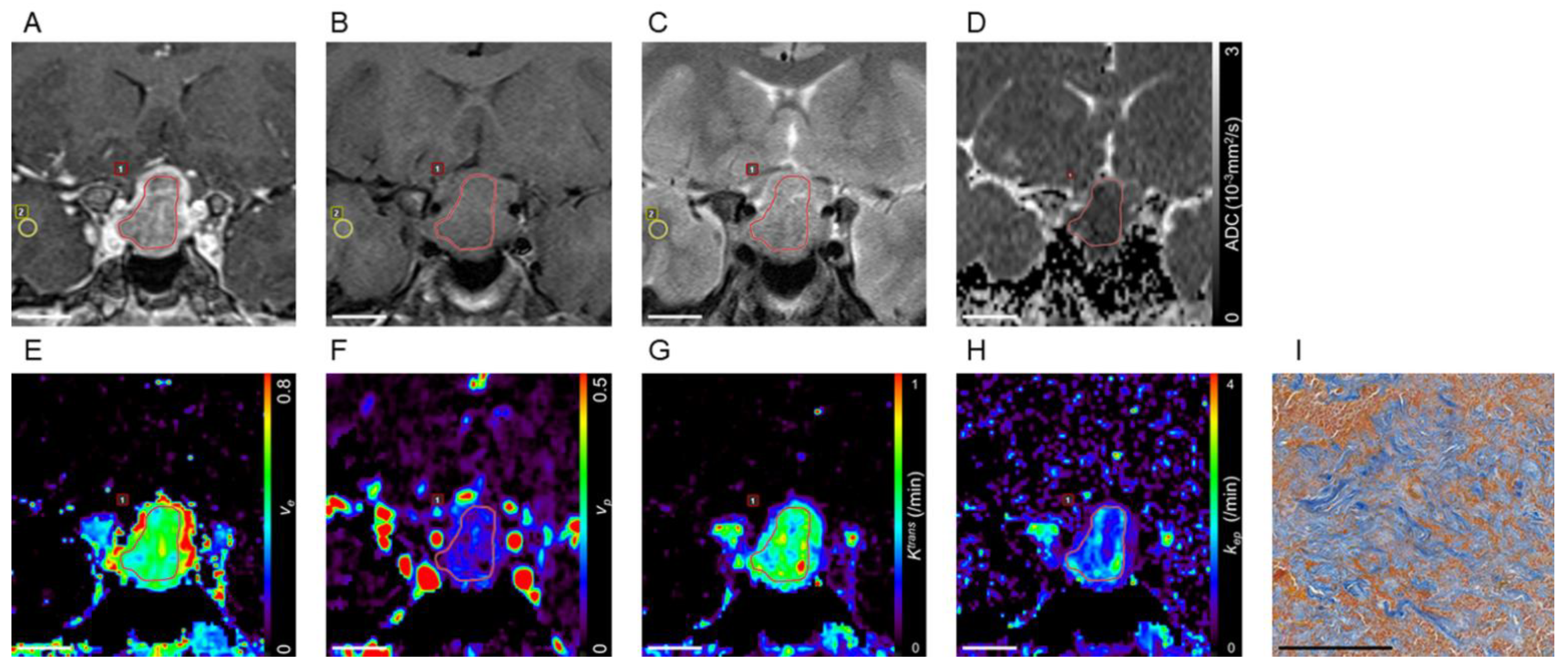
2.6. Pharmacokinetic Analysis of DCE-MRI
2.7. Intraoperative Findings
2.8. Histologic Examination
2.9. Postoperative MRI Examinations
2.10. Statistical Analyses
3. Results
3.1. Characteristics of Participants and Adenomas
3.2. Maximum Diameter and Volume of Pituitary Adenomas
3.3. Interobserver Agreement
3.4. Comparisons of Imaging and Histologic Parameters between Nonfunctioning and GH Producing Adenomas
3.5. Correlation of Imaging and Histologic Parameters, and Levels of GH and IGF-1 in Participants with GH-Producing Adenoma
3.6. Hypopituitarism and Correlation of Imaging and Histologic Parameters, and Cortisol of Nonfunctioning Adenomas
3.7. Comparisons of Imaging and Histologic Parameters between the Low and High Grade of Knosp Classification
3.8. Comparisons of Imaging and Histologic Parameters between Total Resection and Residual Tumor
3.9. Comparisons of Imaging and Histologic Parameters between Soft and Hard Adenomas of All Adenomas
3.10. Comparisons of Imaging and Histologic Parameters between Soft and Hard Nonfunctioning Adenomas
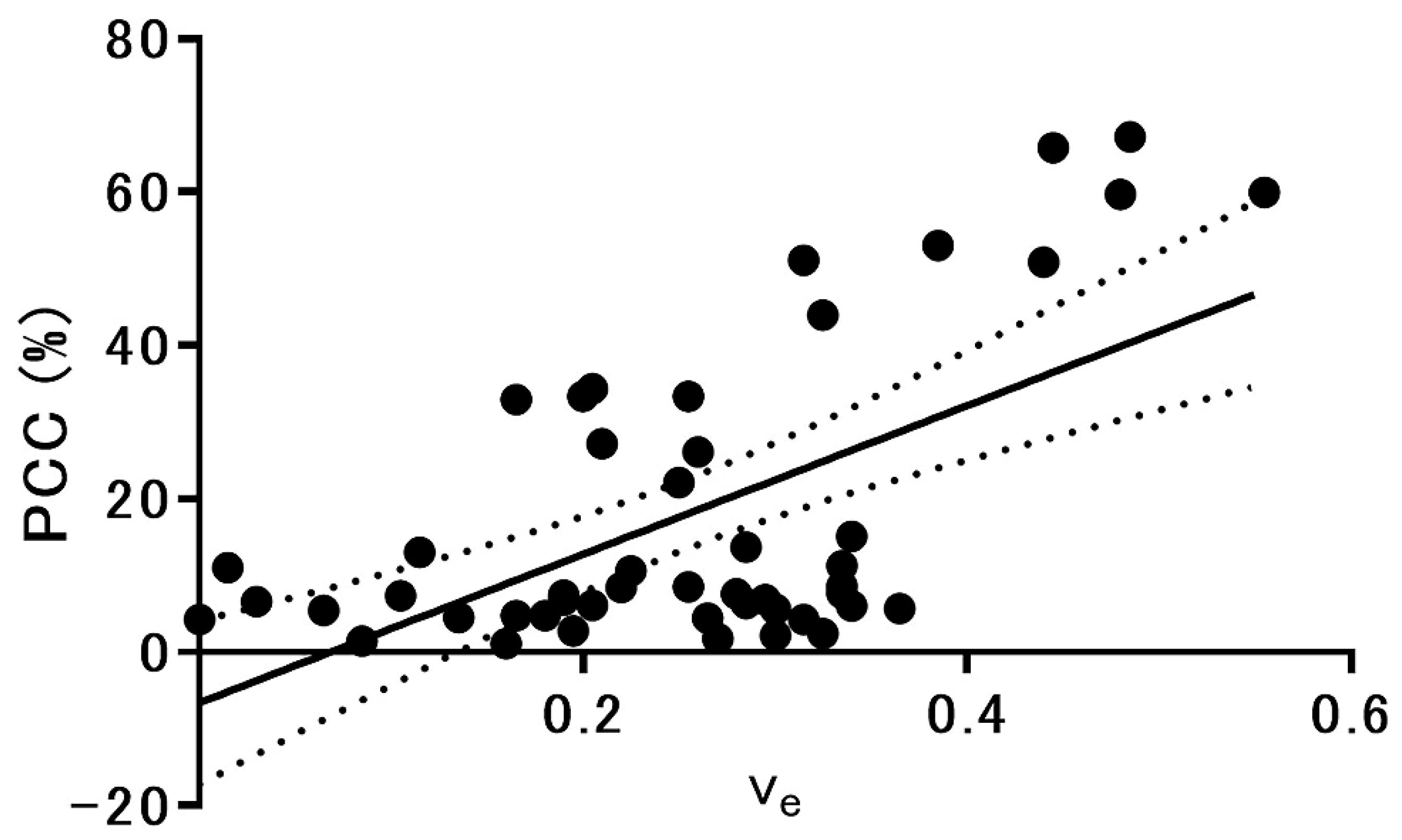
3.11. MRI Parameters Correlated with Percentage of Collagen Content in Pituitary Adenomas
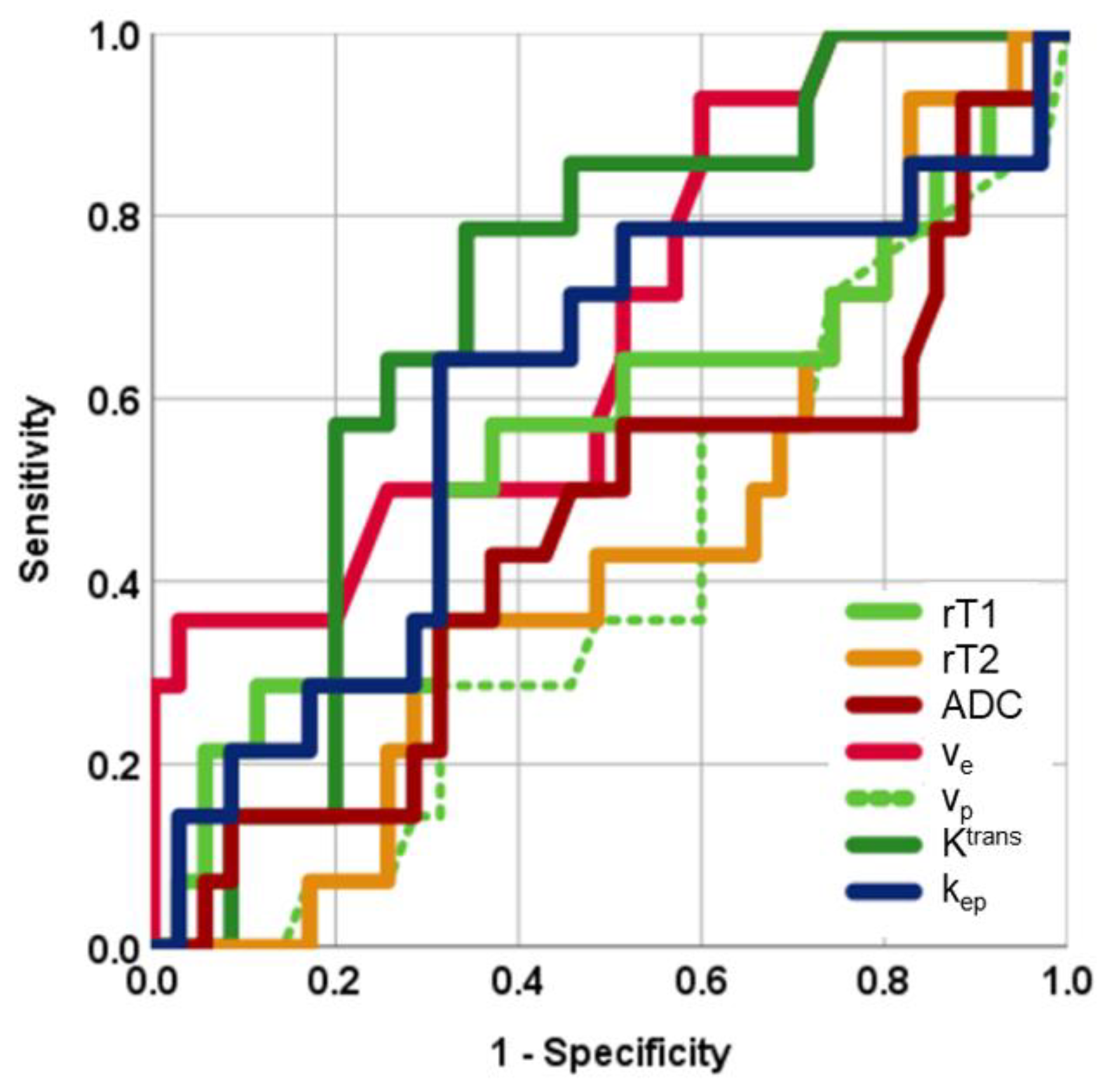
3.12. Diagnostic Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Osamura, R.Y.; Lopes, M.B.S.; Grossman, A.; Kontogeorgos, G.; Trouillas, J. Tumors of the pituitary gland. In WHO Classification of Tumors of Endocrine Organs, 4th ed.; Ricardo, V.L., Osamura, R.Y., Gunter, K., Juan, R., Eds.; International Agency for Research on Cancer: Lyon, France, 2017; pp. 11–64. [Google Scholar]
- Boxerman, J.L.; Rogg, J.M.; Donahue, J.E.; Machan, J.T.; Goldman, M.A.; Doberstein, C.E. Preoperative MRI evaluation of pituitary macroadenoma: Imaging features predictive of successful transsphenoidal surgery. AJR Am. J. Roentgenol. 2010, 195, 720–728. [Google Scholar] [CrossRef] [PubMed]
- Snow, R.B.; Lavyne, M.H.; Lee, B.C.; Morgello, S.; Patterson, R.H., Jr. Craniotomy versus transsphenoidal excision of large pituitary tumors: The usefulness of magnetic resonance imaging in guiding the operative approach. Neurosurgery 1986, 19, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Alimohamadi, M.; Sanjari, R.; Mortazavi, A.; Shirani, M.; Tabriz, M.H.; Kharazi, H.H.; Amirjamshidi, A. Predictive value of diffusion-weighted MRI for tumor consistency and resection rate of nonfunctional pituitary macroadenomas. Acta Neurochir. 2014, 156, 2245–2252. [Google Scholar] [CrossRef] [PubMed]
- Pierallini, A.; Caramia, F.; Falcone, C.; Tinelli, E.; Paonessa, A.; Ciddio, B.A.; Fiorelli, M.; Bianco, F.; Natalizi, S.; Ferrante, L.; et al. Pituitary macroadenomas: Preoperative evaluation of consistency with diffusion-weighted MR imaging—Initial experience. Radiology 2006, 239, 223–231. [Google Scholar] [CrossRef]
- Romano, A.; Coppola, V.; Lombardi, M.; Lavorato, L.; Di Stefano, D.; Caroli, E.; Rossi Espagnet, M.C.; Tavanti, F.; Minniti, G.; Trillò, G.; et al. Predictive role of dynamic contrast enhanced T1-weighted MR sequences in pre-surgical evaluation of macroadenomas consistency. Pituitary 2017, 20, 201–209. [Google Scholar] [CrossRef]
- Yiping, L.; Ji, X.; Daoying, G.; Bo, Y. Prediction of the consistency of pituitary adenoma: A comparative study on diffusion-weighted imaging and pathological results. J. Neuroradiol. 2016, 43, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; He, W.; Zhao, Y.; Yuan, J.; Zhang, O.; Wu, Y.; Chen, H.; Yao, Z.; Li, S.; Wang, Y. Predictive value of PWI for blood supply and T1-spin echo MRI for consistency of pituitary adenoma. Neuroradiology 2016, 58, 51–57. [Google Scholar] [CrossRef]
- Iuchi, T.; Saeki, N.; Tanaka, M.; Sunami, K.; Yamaura, A. MRI prediction of fibrous pituitary adenomas. Acta Neurochir. 1998, 140, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, C.; Maeda, M.; Hori, K.; Kozuka, Y.; Sakuma, H.; Taki, W.; Takeda, K. Apparent diffusion coefficient of pituitary macroadenoma evaluated with line-scan diffusion-weighted imaging. J. Neuroradiol. 2007, 34, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, O.M.; Tominaga, A.; Amatya, V.J.; Ohtaki, M.; Sugiyama, K.; Saito, T.; Sakoguchi, T.; Kinoshita, Y.; Shrestha, P.; Abe, N.; et al. Role of PROPELLER diffusion-weighted imaging and apparent diffusion coefficient in the evaluation of pituitary adenomas. Eur. J. Radiol. 2011, 80, 412–417. [Google Scholar] [CrossRef]
- Choyke, P.L.; Dwyer, A.J.; Knopp, M.V. Functional tumor imaging with dynamic contrast-enhanced magnetic resonance imaging. J. Magn. Reson. Imaging 2003, 17, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Sourbron, S.P.; Buckley, D.L. On the scope and interpretation of the Tofts models for DCE-MRI. Magn. Reson. Med. 2011, 66, 735–745. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Zhang, L.; Qiu, B.; Meng, L.; Wang, X.; Hou, B.L. Correlation of volume transfer coefficient Ktrans with histopathologic grades of gliomas. J. Magn. Reson. Imaging 2012, 36, 355–363. [Google Scholar] [CrossRef] [Green Version]
- Lu, S.; Gao, Q.; Yu, J.; Li, Y.; Cao, P.; Shi, H.; Hong, X. Utility of dynamic contrast-enhanced magnetic resonance imaging for differentiating glioblastoma, primary central nervous system lymphoma and brain metastatic tumor. Eur. J. Radiol. 2016, 85, 1722–1727. [Google Scholar] [CrossRef] [PubMed]
- Tofts, P.S.; Brix, G.; Buckley, D.L.; Evelhoch, L.J.; Henderson, E.; Knopp, V.M.; Larsson, B.H.; Lee, Y.T.; Mayr, A.N.; Parker, J.G.; et al. Estimating kinetic parameters from dynamic contrast-enhanced T(1)-weighted MRI of a diffusable tracer: Standardized quantities and symbols. J. Magn. Reason. Imaging 1999, 10, 223–232. [Google Scholar] [CrossRef]
- Akisik, M.F.; Sandrasegaran, K.; Bu, G.; Lin, C.; Hutchins, G.D.; Chiorean, E.G. Pancreatic cancer: Utility of dynamic contrast-enhanced MR imaging in assessment of antiangiogenic therapy. Radiology 2010, 256, 441–449. [Google Scholar] [CrossRef]
- Ma, W.; Li, N.; Zhao, W.; Ren, J.; Wei, M.; Yang, Y.; Wang, Y.; Fu, X.; Zhang, Z.; Larson, C.A.; et al. Apparent diffusion coefficient and dynamic contrast-enhanced magnetic resonance imaging in pancreatic cancer: Characteristics and correlation with histopathologic parameters. J. Comput. Assist. Tomogr. 2016, 40, 709–716. [Google Scholar] [CrossRef]
- Anzalone, N.; Castellano, A.; Cadioli, M.; Conte, G.M.; Cuccarini, V.; Bizzi, A.; Grimaldi, M.; Costa, A.; Grillea, G.; Vitali, P.; et al. Brain gliomas: Multicenter standardized assessment of dynamic contrast-enhanced and dynamic susceptibility contrast MR images. Radiology 2018, 287, 933–943. [Google Scholar] [CrossRef] [Green Version]
- Zhai, J.; Zheng, W.; Zhang, Q.; Wu, J.; Zhang, X. Pharmacokinetic analysis for the differentiation of pituitary microadenoma subtypes through dynamic contrast-enhanced magnetic resonance imaging. Oncol. Lett. 2019, 17, 4237–4244. [Google Scholar] [CrossRef] [Green Version]
- Kamimura, K.; Nakajo, M.; Yoneyama, T.; Bohara, M.; Nakanosono, R.; Fujio, S.; Iwanaga, T.; Nickel, D.M.; Imai, H.; Fukukura, Y.; et al. Quantitative pharmacokinetic analysis of high-temporal-resolution dynamic contrast-enhanced MRI to differentiate the normal-appearing pituitary gland from pituitary macroadenoma. Jpn. J. Radiol. 2020, 38, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Honda, M.; Kataoka, M.; Onishi, N.; Iima, M.; Ohashi, A.; Kanao, S.; Nickel, D.M.; Toi, M.; Togashi, K. New parameters of ultrafast dynamic contrast-enhanced breast MRI using compressed sensing. J. Magn. Reason. Imaging 2020, 51, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Arima, H.; Inomoto, C.; Iwasaki, Y.; Otuki, M.; Oki, T.; Inyama, K.; Kanzaki, S.; Sugawara, A.; Sugino, N.; Sugimura, M.; et al. Diagnosis and treatment of hypothalamic pituitary dysfunction. Nihon Naibunpi Gakkai Zasshi. 2019, 95, 1–60. [Google Scholar] [CrossRef] [Green Version]
- Giustina, A.; Chanson, P.; Bronstein, M.D.; Klibanski, A.; Lamberts, S.; Casanueva, F.F.; Trainer, P.; Ghigo, E.; Ho, K.; Melmed, S. Acromegaly Consensus Group. A consensus on criteria for cure of acromegaly. J. Clin. Endocrinol. Metab. 2010, 95, 3141–3148. [Google Scholar] [CrossRef] [Green Version]
- Koyasu, S.; Iima, M.; Umeoka, S.; Morisawa, N.; Porter, A.D.; Ito, J.; Bihan, L.D.; Togashi, K. The clinical utility of reduced-distortion readout-segmented echo-planar imaging in the head and neck region: Initial experience. Eur. Radiol. 2014, 24, 3088–3096. [Google Scholar] [CrossRef]
- Holdsworth, S.J.; Skare, S.; Newbould, R.D.; Guzmann, R.; Blevins, N.H.; Bammer, R. Readout-segmented EPI for rapid high resolution diffusion imaging at 3T. Eur. J. Radiol. 2008, 65, 36–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Chiro, G.; Nelson, K.B. The volume of the sella turcica. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1962, 87, 989–1008. [Google Scholar] [PubMed]
- Knosp, E.; Steiner, E.; Kitz, K.; Matula, C. Pituitary adenomas with invasion of the cavernous sinus space: A magnetic resonance imaging classification compared with surgical findings. Neurosurgery 1993, 33, 610–618. [Google Scholar] [CrossRef]
- Micko, A.S.; Wöhrer, A.; Wolfsberger, S.; Knosp, E. Invasion of the cavernous sinus space in pituitary adenomas: Endoscopic verification and its correlation with an MRI-based classification. J. Neurosurg. 2015, 122, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Yamamoto, J.; Kakeda, S.; Shimajiri, S.; Takahashi, M.; Watanabe, K.; Kai, Y.; Moriya, J.; Korogi, Y.; Nishizawa, S. Tumor consistency of pituitary macroadenomas: Predictive analysis on the basis of imaging features with contrast-enhanced 3D Fiesta at 3T. AJNR Am. J. Neuroradiol. 2014, 35, 297–303. [Google Scholar] [CrossRef] [Green Version]
- Naganuma, H.; Satoh, E.; Nukui, H. Technical considerations of transsphenoidal removal of fibrous pituitary adenomas and evaluation of collagen content and subtype in the adenomas. Neurol. Med. Chir. 2002, 42, 202–212. [Google Scholar] [CrossRef] [Green Version]
- Tofrizal, A.; Fujiwara, K.; Yashiro, T.; Yamada, S. Alterations of collagen-producing cells in human pituitary adenomas. Med. Mol. Morphol. 2016, 49, 224–232. [Google Scholar] [CrossRef]
- Tofrizal, A.; Fujiwara, K.; Azuma, M.; Kikuchi, M.; Jindatip, D.; Yashiro, T.; Yamada, S. Tissue inhibitors of metalloproteinase-expressing cells in human anterior pituitary and pituitary adenoma. Med. Mol. Morphol. 2017, 50, 145–154. [Google Scholar] [CrossRef]
- Liu, Y.Q.; Gao, B.B.; Dong, B.; Cheriyath, P.S.S.; Song, W.Q.; Xu, B.; Wei, Q.; Xie, Z.L.; Guo, Y.; Miao, W.Y. Preoperative vascular heterogeneity and aggressiveness assessment of pituitary macroadenoma based on dynamic contrast-enhanced MRI texture analysis. Eur. J. Radiol. 2020, 129, 109125. [Google Scholar] [CrossRef]
- Vreemann, S.; Rodriguez-Ruiz, A.; Nickel, D.; Heacock, L.; Appelman, L.; van Zelst, J.; Karssemeijer, N.; Weiland, E.; Maas, M.; Moy, L.; et al. Compressed sensing for breast MRI: Resolving the trade-off between spatial and temporal resolution. Investig. Radiol. 2017, 52, 574–582. [Google Scholar] [CrossRef]
- Rutkowski, M.J.; Chang, K.E.; Cardinal, T.; Du, R.; Tafreshi, A.R.; Donoho, D.A.; Brunswick, A.; Micko, A.; Liu, C.J.; Shiroishi, M.S.; et al. Development and clinical validation of a grading system for pituitary adenoma consistency. J. Neurosurg. 2020, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Qian, P.; Zhang, X.; Zhang, M.; Wang, H.; Wu, M.; Kong, X.; Tan, S.; Ding, K.; Perry, J.K.; et al. Autocrine/paracrine human growth hormone-stimulated micro-RNA 96-182-183 cluster promotes epithelial-mesenchymal transition and invasion in breast cancer. J. Biol. Chem. 2015, 290, 13812–13829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chesnokova, V.; Zonis, S.; Zhou, C.; Recouvreux, M.V.; Ben-Shlomo, A.; Araki, T.; Barrett, R.; Workman, M.; Wawrowsky, K.; Ljubimov, V.A.; et al. Growth hormone is permissive for neoplastic colon growth. Proc. Natl. Acad. Sci. USA 2016, 113, 3250–3259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subramani, R.; Lopez-Valdez, R.; Salcido, A.; Boopalan, T.; Arumugam, A.; Nandy, S.; Lakshmanaswamy, R. Growth hormone receptor inhibition decreases the growth and metastasis of pancreatic ductal adenocarcinoma. Exp. Mol. Med. 2014, 46, e117. [Google Scholar] [CrossRef] [PubMed]
- Brittain, A.L.; Basu, R.; Qian, Y.; Kopchick, J.J. Growth Hormone and the Epithelial-to-Mesenchymal Transition. J. Clin. Endocrinol. Metab. 2017, 102, 3662–3673. [Google Scholar] [CrossRef] [Green Version]
- Cavallaro, U.; Christofori, G. Cell adhesion and signalling by cadherins and Ig-CAMs in cancer. Nat. Rev. Cancer 2004, 4, 118–132. [Google Scholar] [CrossRef]
- Yamada, S.; Fukuhara, N.; Horiguchi, K.; Yamaguchi-Okada, M.; Nishioka, H.; Takeshita, A.; Takeuchi, Y.; Ito, J.; Inoshita, N. Clinicopathological characteristics and therapeutic outcomes in thyrotropin-secreting pituitary adenomas: A single-center study of 90 cases. J. Neurosurg. 2014, 121, 1462–1473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagiwara, A.; Inoue, Y.; Wakasa, K.; Haba, T.; Tashiro, T.; Miyamoto, T. Comparison of growth hormone-producing and nongrowth hormone-producing pituitary adenomas: Imaging characteristics and pathologic correlation. Radiology 2003, 228, 533–538. [Google Scholar] [CrossRef] [PubMed]
- Dogansen, S.C.; Yalin, G.Y.; Tanrikulu, S.; Tekin, S.; Nizam, N.; Bilgic, B.; Sencer, S.; Yarman, S. Clinicopathological significance of baseline T2-weighted signal intensity in functional pituitary adenomas. Pituitary 2018, 21, 347–354. [Google Scholar] [CrossRef]
- Marques, P.; Barry, S.; Carlsen, E.; Collier, D.; Ronaldson, A.; Awad, S.; Dorward, N.; Grieve, J.; Mendoza, N.; Muquit, S.; et al. Pituitary tumour fibroblast-derived cytokines influence tumour aggressiveness. Endocr. Relat. Cancer 2019, 26, 853–865. [Google Scholar] [CrossRef]
- Heck, A.; Emblem, K.E.; Casar-Borota, O.; Ringstad, G.; Bollerslev, J. MRI T2 characteristics in somatotroph adenomas following somatostatin analog treatment in acromegaly. Endocrine 2016, 53, 327–330. [Google Scholar] [CrossRef] [PubMed]

| MRI Protocol | Pre-Contrast T1-Weighted Imaging | T2-Weighted Imaging | DWI | DCE Imaging | Post-Contrast T1-Weighted Imaging |
|---|---|---|---|---|---|
| Orientation | Coronal | Coronal | Coronal | Coronal | Coronal |
| Sequence | 2D SE | 2D TSE | RESOLVE | 3D VIBE | 3D FLASH |
| TR (ms) | 450 | 4000 | 4000 | 3.9 | 4.68 |
| TE (ms) | 12 | 95 | 49 | 0.97 | 1.74 |
| FA (degree) | 70/180 | 90/130 | 150 | 10 | 11 |
| Bandwidth (Hz/pixel) | 130 | 189 | 694 | 670 | 370 |
| Number of excitations | 1 | 2 | 1 and 3 for low and high b values | 1 | 2 |
| Turbo factor | N/A | 9 | N/A | N/A | N/A |
| Acceleration factor | 1 | 2 | 2 | N/A | N/A |
| CS factor | N/A | N/A | N/A | 7 | N/A |
| b values (s/mm2) | N/A | N/A | 0 and 1000 | N/A | N/A |
| Directions of motion-probing gradients | N/A | N/A | 3 | N/A | N/A |
| Readout segments | N/A | N/A | 9 | N/A | N/A |
| FOV (mm2) | 180 × 180 | 180 × 180 | 120 × 120 | 159 × 180 | 200 × 200 |
| Matrix | 240 × 320 | 313 × 448 | 84 × 120 | 163 × 192 | 320 × 256 |
| Thickness (mm) | 3 | 3 | 2 | 0.9 | 0.6 |
| Intersection gap (mm) | 0.3 | 0.3 | 0 | N/A | N/A |
| Temporal resolution (s) | N/A | N/A | N/A | 5 | N/A |
| Acquisition time (s) | 148 | 158 | 252 | 203 | 161 |
| Participants Characteristics | Total (n = 49) | Soft Adenoma (n = 34) | Hard Adenoma (n = 15) | p Value |
|---|---|---|---|---|
| Age (y) | 55 ± 17 | 53 ± 17 | 60 ± 17 | 0.12 a |
| No. of men | 23 (46.9) | 15 (44.1) | 8 (53.3) | 0.76 a |
| Maximum diameter (mm) | 24.2 ± 12.2 | 24.8 ± 14.0 | 26.1 ± 7.0 | 0.27 a |
| Volume (mm3) | 8090 ± 13,570 | 8830 ± 16,070 | 6420 ± 4210 | 0.18 a |
| Pituitary lesions | ||||
| Nonfunctioning | 33 (67.3) | 21 (61.8) | 12 (80.0) | 0.32 b |
| Functioning | 16 (32.7) | 13 (38.2) | 3 (20.0) | |
| GH producing | 13 (26.5) | 10 (29.4) Densely granulated | 3 (20.0) Sparsely granulated | |
| TSH producing | 2 (4.1) | 2 (5.9) Densely granulated | 0 (0) | |
| ACTH producing | 1 (2.1) | 1 (2.9) Densely granulated | 0 (0) | |
| Knosp classification | ||||
| 0 | 3 (6.1) | 3 (8.8) | 0 (0) | 0.01 a |
| 1 | 13 (26.5) | 11 (32.4) | 2 (13.3) | |
| 2 | 12 (24.5) | 10 (29.4) | 2 (13.3) | |
| 3 | 18 (36.8) | 8 (23.5) | 10 (66.7) | |
| 4 | 3 (6.1) | 2 (5.9) | 1 (6.7) | |
| Residual tumor | 12 (24.5) | 6 (17.6) | 6 (40.0) | 0.09 c |
| Hypopituitarism | 24 (49.0) | 13 (38.2) | 11 (73.3) | <0.01 c |
| Tumor regrowth | 4 (8.2) | 3 (8.8) | 1 (6.7) |
| Parameters | Nonfunctioning (n = 33) | GH-Producing (n = 13) | p Value |
|---|---|---|---|
| rT1 | 0.837 ± 0.079 | 0.850 ± 0.074 | 0.81 a |
| rT2 | 1.763 ± 0.377 | 1.359 ± 0.335 | <0.01 a |
| ADC (10−3 mm2/s) | 0.856 ± 0.270 | 0.748 ± 0.121 | 0.18 a |
| ve | 0.250 ± 0.124 | 0.266 ± 0.131 | 0.70 b |
| vp | 0.069 ± 0.084 | 0.047 ± 0.052 | 0.70 a |
| Ktrans (/min) | 0.734 ± 0.646 | 0.482 ± 0.301 | 0.40 a |
| kep (/min) | 2.558 ± 1.891 | 1.918 ± 1.147 | 0.26 b |
| PCC (%) | 19.88 ± 20.33 | 15.61 ± 19.51 | 0.35 a |
| Parameters | Low Grade (n = 28) | High Grade (n = 21) | p Value |
|---|---|---|---|
| rT1 | 0.842 ± 0.081 | 0.847 ± 0.080 | 0.85 a |
| rT2 | 1.590 ± 0.467 | 1.697 ± 0.319 | 0.37 a |
| ADC (10−3 mm2/s) | 0.849 ± 0.292 | 0.764 ± 0.156 | 0.20 b |
| ve | 0.237 ± 0.116 | 0.279 ± 0.126 | 0.24 a |
| vp | 0.065 ± 0.086 | 0.056 ± 0.057 | 0.69 b |
| Ktrans (/min) | 0.617 ± 0.534 | 0.703 ± 0.608 | 0.61 b |
| kep (/min) | 2.268 ± 1.629 | 2.490 ± 1.773 | 0.66 b |
| PCC (%) | 12.58 ± 15.27 | 25.43 ± 22.28 | 0.03 b |
| Parameters | Total Resection (n = 36) | Residual Tumor (n = 13) | p Value |
|---|---|---|---|
| rT1 | 0.854 ± 0.080 | 0.819 ± 0.078 | 0.18 a |
| rT2 | 1.650 ± 0.444 | 1.600 ± 0.310 | 0.71 a |
| ADC (10−3 mm2/s) | 0.820 ± 0.267 | 0.793 ± 0.179 | 0.69 b |
| ve | 0.243 ± 0.121 | 0.288 ± 0.120 | 0.25 a |
| vp | 0.062 ± 0.075 | 0.057 ± 0.077 | 0.85 b |
| Ktrans (/min) | 0.567 ± 0.466 | 0.894 ± 0.739 | 0.16 b |
| kep (/min) | 2.109 ± 1.472 | 3.067 ± 2.052 | 0.14 b |
| PCC (%) | 16.45 ± 18.71 | 22.64 ± 21.58 | 0.37 b |
| Parameters | Tumor Consistency Group | p Value | |
|---|---|---|---|
| Soft Adenoma (n = 34) | Hard Adenoma (n = 15) | ||
| rT1 | 0.840 ± 0.077 | 0.854 ± 0.088 | 0.40 a |
| rT2 | 1.661 ± 0.453 | 1.580 ± 0.295 | 0.55 a |
| ADC (10−3 mm2/s) | 0.832 ± 0.263 | 0.769 ± 0.201 | 0.47 a |
| ve | 0.221 ± 0.104 | 0.332 ± 0.124 | <0.01 b |
| vp | 0.070 ± 0.084 | 0.040 ± 0.042 | 0.36 a |
| Ktrans (/min) | 0.601 ± 0.612 | 0.775 ± 0.401 | 0.02 a |
| kep (/min) | 2.240 ± 1.691 | 2.641 ± 1.672 | 0.37 a |
| PCC (%) | 6.62 ± 3.47 | 44.08 ± 15.14 | <0.01 b |
| Parameters | Tumor Consistency Group | p Value | |
|---|---|---|---|
| Soft Adenoma (n = 21) | Hard Adenoma (n = 12) | ||
| rT1 | 0.824 ± 0.071 | 0.861 ± 0.090 | 0.24 a |
| rT2 | 1.880 ± 0.383 | 1.558 ± 0.273 | 0.01 a |
| ADC (10−3 mm2/s) | 0.913 ± 0.285 | 0.756 ± 0.217 | 0.09 a |
| ve | 0.215 ± 0.118 | 0.310 ± 0.114 | 0.03 b |
| vp | 0.089 ± 0.096 | 0.036 ± 0.043 | 0.04 a |
| Ktrans (/min) | 0.680 ± 0.752 | 0.829 ± 0.413 | 0.47 a |
| kep (/min) | 2.365 ± 2.006 | 2.894 ± 1.701 | 0.43 a |
| PCC (%) | 6.62 ± 3.51 | 43.08 ± 15.91 | <0.01 a |
| Parameters | AUC | Optimal Cut-Off Value | Sensitivity (%) | Specificity (%) | Accuracy (%) |
|---|---|---|---|---|---|
| rT1 | 0.578 | 0.866 | 60.0 (9/15) | 64.7 (22/34) | 63.3 (31/49) |
| rT2 | 0.555 | 1.551 | 53.3 (8/15) | 64.7 (22/34) | 61.2 (30/49) |
| ADC | 0.566 | 0.674 (10−3 mm2/s) | 46.7 (7/15) | 73.5 (25/34) | 65.3 (32/49) |
| ve | 0.712 | 0.365 | 40.0 (6/15) | 100 (34/34) | 81.6 (40/49) |
| vp | 0.583 | 0.100 | 93.3 (14/15) | 26.5 (9/34) | 46.9 (23/49) |
| Ktrans | 0.703 | 0.560 (/min) | 80.0 (12/15) | 67.7 (23/34) | 71.4 (35/49) |
| kep | 0.582 | 1.980 (/min) | 60.0 (9/15) | 67.7 (23/34) | 65.3 (40/49) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamimura, K.; Nakajo, M.; Bohara, M.; Nagano, D.; Fukukura, Y.; Fujio, S.; Takajo, T.; Tabata, K.; Iwanaga, T.; Imai, H.; et al. Consistency of Pituitary Adenoma: Prediction by Pharmacokinetic Dynamic Contrast-Enhanced MRI and Comparison with Histologic Collagen Content. Cancers 2021, 13, 3914. https://doi.org/10.3390/cancers13153914
Kamimura K, Nakajo M, Bohara M, Nagano D, Fukukura Y, Fujio S, Takajo T, Tabata K, Iwanaga T, Imai H, et al. Consistency of Pituitary Adenoma: Prediction by Pharmacokinetic Dynamic Contrast-Enhanced MRI and Comparison with Histologic Collagen Content. Cancers. 2021; 13(15):3914. https://doi.org/10.3390/cancers13153914
Chicago/Turabian StyleKamimura, Kiyohisa, Masanori Nakajo, Manisha Bohara, Daigo Nagano, Yoshihiko Fukukura, Shingo Fujio, Tomoko Takajo, Kazuhiro Tabata, Takashi Iwanaga, Hiroshi Imai, and et al. 2021. "Consistency of Pituitary Adenoma: Prediction by Pharmacokinetic Dynamic Contrast-Enhanced MRI and Comparison with Histologic Collagen Content" Cancers 13, no. 15: 3914. https://doi.org/10.3390/cancers13153914
APA StyleKamimura, K., Nakajo, M., Bohara, M., Nagano, D., Fukukura, Y., Fujio, S., Takajo, T., Tabata, K., Iwanaga, T., Imai, H., Nickel, M. D., & Yoshiura, T. (2021). Consistency of Pituitary Adenoma: Prediction by Pharmacokinetic Dynamic Contrast-Enhanced MRI and Comparison with Histologic Collagen Content. Cancers, 13(15), 3914. https://doi.org/10.3390/cancers13153914








