Prognostic Discrimination of Alternative Lymph Node Classification Systems for Patients with Radically Resected Non-Metastatic Colorectal Cancer: A Cohort Study from a Single Tertiary Referral Center
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Cohort
2.2. Tumor Staging and LN Classifications
2.3. Statistical Analysis
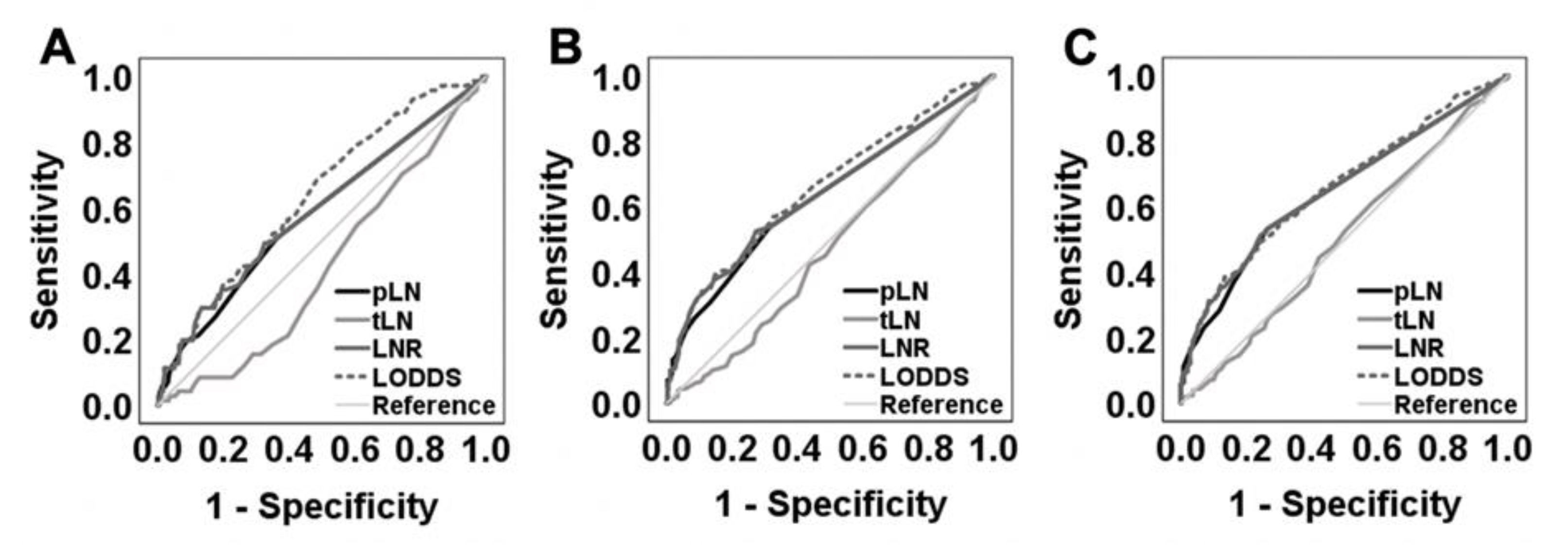
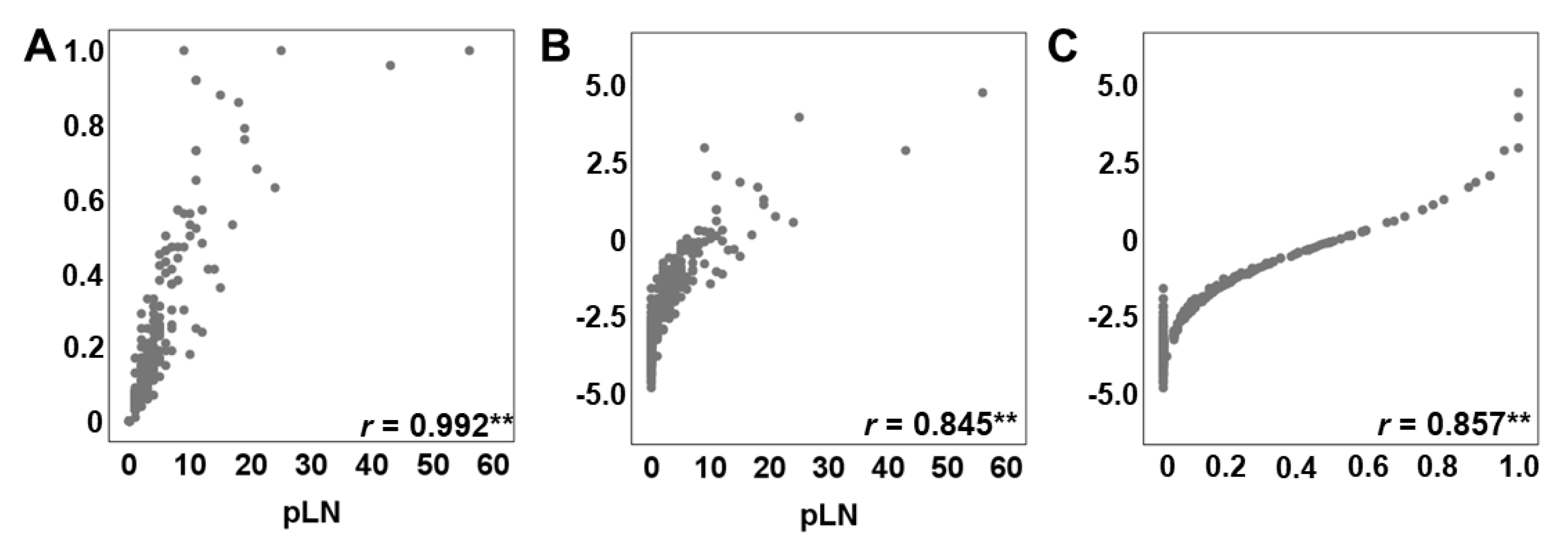
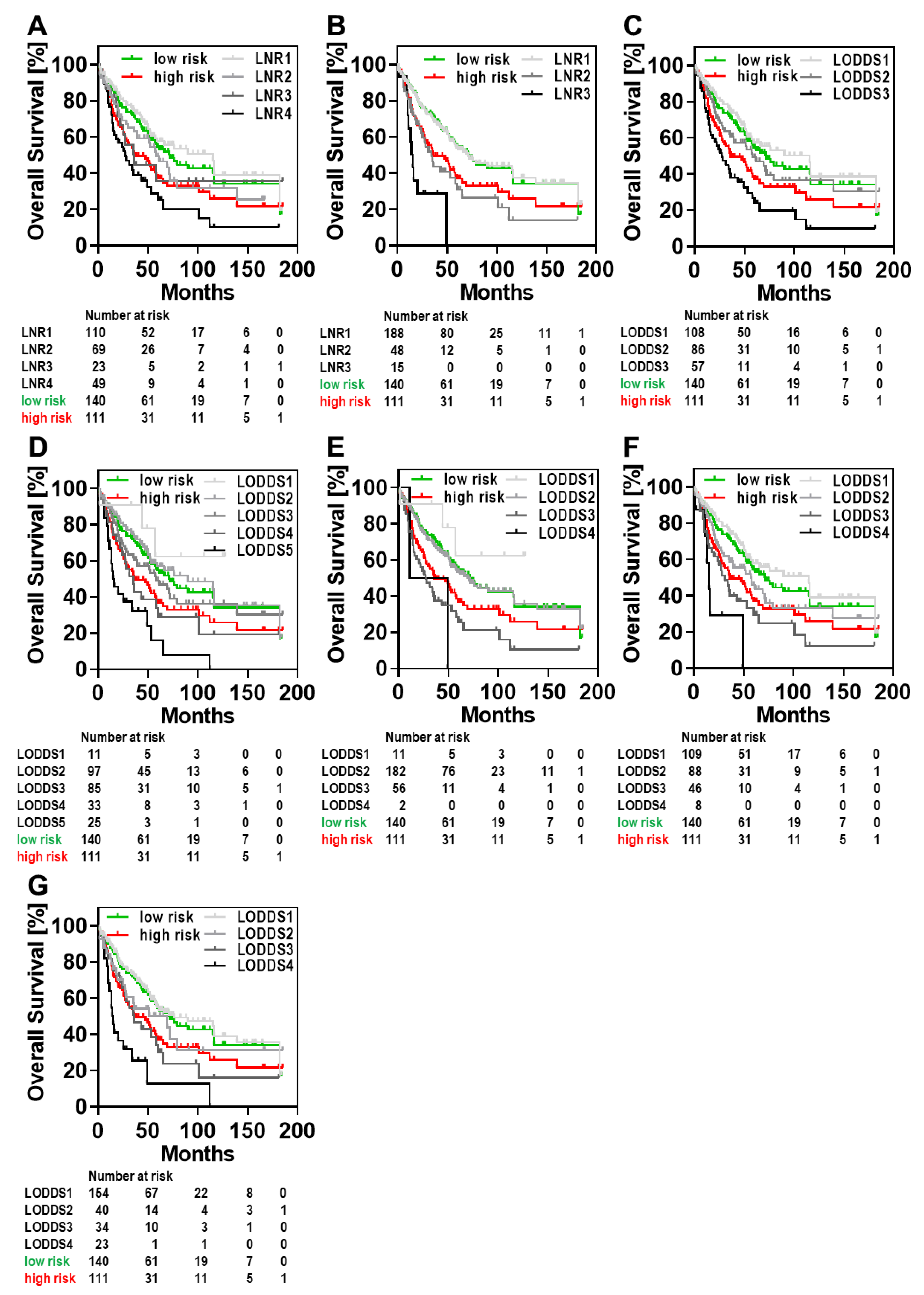
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Fortea-Sanchis, C.; Martinez-Ramos, D.; Escrig-Sos, J. The lymph node status as a prognostic factor in colon cancer: Comparative population study of classifications using the logarithm of the ratio between metastatic and nonmetastatic nodes (LODDS) versus the pN-TNM classification and ganglion ratio systems. BMC Cancer 2018, 18, 1208. [Google Scholar] [CrossRef]
- Byrd, D.R.; Carducci, M.A.; Compton, C.C.; Fritz, A.G.; Greene, F. AJCC Cancer Staging Manual, 8th ed.; Springer International Publishing: New York, NY, USA, 2017. [Google Scholar]
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, C. TNM Classification of Malignant Tumours, 8th ed.; Wiley-Blackwell: Oxford, UK, 2017. [Google Scholar]
- Namm, J.; Ng, M.; Roy-Chowdhury, S.; Morgan, J.W.; Lum, S.S.; Wong, J.H. Quantitating the impact of stage migration on staging accuracy in colorectal cancer. J. Am. Coll. Surg. 2008, 207, 882–887. [Google Scholar] [CrossRef]
- Baxter, N.N.; Virnig, D.J.; Rothenberger, D.A.; Morris, A.M.; Jessurun, J.; Virnig, B.A. Lymph node evaluation in colorectal cancer patients: A population-based study. J. Natl. Cancer Inst. 2005, 97, 219–225. [Google Scholar] [CrossRef]
- Resch, A.; Langner, C. Lymph node staging in colorectal cancer: Old controversies and recent advances. World J. Gastroenterol. 2013, 19, 8515–8526. [Google Scholar] [CrossRef]
- Zhou, D.; Ye, M.; Bai, Y.; Rong, L.; Hou, Y. Prognostic value of lymph node ratio in survival of patients with locally advanced rectal cancer. Can. J. Surg. 2015, 58, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Chung, S.M.; Choi, B.O.; Lee, I.K.; An, C.H.; Won, J.M.; Ryu, M.R. Prognostic significance of the lymph node ratio regarding recurrence and survival in rectal cancer patients treated with postoperative chemoradiotherapy. Gut Liver 2012, 6, 203–209. [Google Scholar] [CrossRef]
- Sun, Z.; Xu, Y.; de Li, M.; Wang, Z.N.; Zhu, G.L.; Huang, B.J.; Li, K.; Xu, H.M. Log odds of positive lymph nodes: A novel prognostic indicator superior to the number-based and the ratio-based N category for gastric cancer patients with R0 resection. Cancer 2010, 116, 2571–2580. [Google Scholar] [CrossRef] [PubMed]
- Arslan, N.C.; Sokmen, S.; Canda, A.E.; Terzi, C.; Sarioglu, S. The prognostic impact of the log odds of positive lymph nodes in colon cancer. Colorectal Dis. 2014, 16, O386–O392. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Cao, J.; Wang, L.; Wang, Z.; Wang, Y.; Wu, Y.; Lv, W.; Hu, J. Prognostic performance of three lymph node staging schemes for patients with Siewert type II adenocarcinoma of esophagogastric junction. Sci. Rep. 2017, 7, 10123. [Google Scholar] [CrossRef] [PubMed]
- Malleo, G.; Maggino, L.; Capelli, P.; Gulino, F.; Segattini, S.; Scarpa, A.; Bassi, C.; Butturini, G.; Salvia, R. Reappraisal of Nodal Staging and Study of Lymph Node Station Involvement in Pancreaticoduodenectomy with the Standard International Study Group of Pancreatic Surgery Definition of Lymphadenectomy for Cancer. J. Am. Coll. Surg. 2015, 221, 367–379.e4. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Zhang, J.; Sun, H.; Liao, Y.; Liao, W. Comparison of three lymph node classifications for survival prediction in distant metastatic gastric cancer. Int. J. Surg. 2016, 35, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Riediger, H.; Kulemann, B.; Wittel, U.; Adam, U.; Sick, O.; Neeff, H.; Hoppner, J.; Hopt, U.T.; Makowiec, F. Prognostic Role of Log Odds of Lymph Nodes After Resection of Pancreatic Head Cancer. J. Gastrointest. Surg. 2016, 20, 1707–1715. [Google Scholar] [CrossRef]
- Fang, H.Y.; Yang, H.; He, Z.S.; Zhao, H.; Fu, Z.M.; Zhou, F.X.; Zhou, Y.F. Log odds of positive lymph nodes is superior to the number- and ratio-based lymph node classification systems for colorectal cancer patients undergoing curative (R0) resection. Mol. Clin. Oncol. 2017, 6, 782–788. [Google Scholar] [CrossRef][Green Version]
- Wang, W.; Xu, D.Z.; Li, Y.F.; Guan, Y.X.; Sun, X.W.; Chen, Y.B.; Kesari, R.; Huang, C.Y.; Li, W.; Zhan, Y.Q.; et al. Tumor-ratio-metastasis staging system as an alternative to the 7th edition UICC TNM system in gastric cancer after D2 resection--results of a single-institution study of 1343 Chinese patients. Ann. Oncol. 2011, 22, 2049–2056. [Google Scholar] [CrossRef] [PubMed]
- Conci, S.; Ruzzenente, A.; Sandri, M.; Bertuzzo, F.; Campagnaro, T.; Bagante, F.; Capelli, P.; D’Onofrio, M.; Piccino, M.; Dorna, A.E.; et al. What is the most accurate lymph node staging method for perihilar cholangiocarcinoma? Comparison of UICC/AJCC pN stage, number of metastatic lymph nodes, lymph node ratio, and log odds of metastatic lymph nodes. Eur. J. Surg. Oncol. 2017, 43, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Chen, C.; Ni, M.; Mo, S.; Cai, G.; Cai, S. Log odds of positive lymph nodes is a superior prognostic indicator in stage III rectal cancer patients: A retrospective analysis of 17,632 patients in the SEER database. Int. J. Surg. 2016, 32, 24–30. [Google Scholar] [CrossRef]
- Calero, A.; Escrig-Sos, J.; Mingol, F.; Arroyo, A.; Martinez-Ramos, D.; de Juan, M.; Salvador-Sanchis, J.L.; Garcia-Granero, E.; Calpena, R.; Lacueva, F.J. Usefulness of the log odds of positive lymph nodes to predict and discriminate prognosis in gastric carcinomas. J. Gastrointest. Surg. 2015, 19, 813–820. [Google Scholar] [CrossRef]
- Lee, J.W.; Ali, B.; Park, C.H.; Song, K.Y. Different lymph node staging systems in patients with gastric cancer from Korean: What is the best prognostic assessment tool? Medicine 2016, 95, e3860. [Google Scholar] [CrossRef]
- Negi, S.S.; Singh, A.; Chaudhary, A. Lymph nodal involvement as prognostic factor in gallbladder cancer: Location, count or ratio? J. Gastrointest. Surg. 2011, 15, 1017–1025. [Google Scholar] [CrossRef]
- Bagante, F.; Tran, T.; Spolverato, G.; Ruzzenente, A.; Buttner, S.; Ethun, C.G.; Groot Koerkamp, B.; Conci, S.; Idrees, K.; Isom, C.A.; et al. Perihilar Cholangiocarcinoma: Number of Nodes Examined and Optimal Lymph Node Prognostic Scheme. J. Am. Coll. Surg. 2016, 222, 750–759.e2. [Google Scholar] [CrossRef]
- Jian-Hui, C.; Shi-Rong, C.; Hui, W.; Si-le, C.; Jian-Bo, X.; Er-Tao, Z.; Chuang-Qi, C.; Yu-Long, H. Prognostic value of three different lymph node staging systems in the survival of patients with gastric cancer following D2 lymphadenectomy. Tumour Biol. 2016, 37, 11105–11113. [Google Scholar] [CrossRef]
- Smith, D.D.; Nelson, R.A.; Schwarz, R.E. A comparison of five competing lymph node staging schemes in a cohort of resectable gastric cancer patients. Ann. Surg. Oncol. 2014, 21, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Deng, J.; Zhang, R.; Hao, X.; Jiao, X.; Liang, H. The RML of lymph node metastasis was superior to the LODDS for evaluating the prognosis of gastric cancer. Int. J. Surg. 2013, 11, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.J.; Chang, Y.J.; Chen, L.J.; Chung, K.P.; Lai, M.S. Evaluation of lymph nodes in patients with colon cancer undergoing colon resection: A population-based study. World J. Surg. 2012, 36, 1906–1914. [Google Scholar] [CrossRef]
- Song, Y.X.; Gao, P.; Wang, Z.N.; Tong, L.L.; Xu, Y.Y.; Sun, Z.; Xing, C.Z.; Xu, H.M. Which is the most suitable classification for colorectal cancer, log odds, the number or the ratio of positive lymph nodes? PLoS ONE 2011, 6, e28937. [Google Scholar] [CrossRef]
- La Torre, M.; Nigri, G.; Petrucciani, N.; Cavallini, M.; Aurello, P.; Cosenza, G.; Balducci, G.; Ziparo, V.; Ramacciato, G. Prognostic assessment of different lymph node staging methods for pancreatic cancer with R0 resection: pN staging, lymph node ratio, log odds of positive lymph nodes. Pancreatology 2014, 14, 289–294. [Google Scholar] [CrossRef]
- Agnes, A.; Biondi, A.; Cananzi, F.M.; Rausei, S.; Reddavid, R.; Laterza, V.; Galli, F.; Quagliuolo, V.; Degiuli, M.; D’Ugo, D.; et al. Ratio-based staging systems are better than the 7th and 8th editions of the TNM in stratifying the prognosis of gastric cancer patients: A multicenter retrospective study. J. Surg Oncol 2019, 119, 948–957. [Google Scholar] [CrossRef]
- Rosenberg, R.; Friederichs, J.; Schuster, T.; Gertler, R.; Maak, M.; Becker, K.; Grebner, A.; Ulm, K.; Hofler, H.; Nekarda, H.; et al. Prognosis of patients with colorectal cancer is associated with lymph node ratio: A single-center analysis of 3026 patients over a 25-year time period. Ann. Surg. 2008, 248, 968–978. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Tang, Z.; Yu, Z.; Wang, Q.; Li, Z.; Lu, Q.; Wu, Y. Comparison of the 8th union for international cancer control lymph node staging system for gastric cancer with two other lymph node staging systems. Oncol. Lett. 2019, 17, 1299–1305. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Hassett, J.M.; Dayton, M.T.; Kulaylat, M.N. The prognostic superiority of log odds of positive lymph nodes in stage III colon cancer. J. Gastrointest. Surg. 2008, 12, 1790–1796. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Zhang, H.; Ma, Z.; Gong, L.; Chen, C.; Ren, P.; Shang, X.; Tang, P.; Jiang, H.; Yu, Z. Log odds of positive lymph nodes is a novel prognostic indicator for advanced ESCC after surgical resection. J. Thorac. Dis. 2017, 9, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Mao, Y.; Wang, J.; Huang, X.; Lin, X.; Li, S. Surgical management of periampullary adenocarcinoma: Defining an optimal prognostic lymph node stratification schema. J. Cancer 2018, 9, 1667–1679. [Google Scholar] [CrossRef]
- Ramacciato, G.; Nigri, G.; Petrucciani, N.; Pinna, A.D.; Ravaioli, M.; Jovine, E.; Minni, F.; Grazi, G.L.; Chirletti, P.; Tisone, G.; et al. Prognostic role of nodal ratio, LODDS, pN in patients with pancreatic cancer with venous involvement. BMC Surg. 2017, 17, 109. [Google Scholar] [CrossRef]
- Toth, D.; Biro, A.; Varga, Z.; Torok, M.; Arkosy, P. Comparison of different lymph node staging systems in prognosis of gastric cancer: A bi-institutional study from Hungary. Chin. J. Cancer Res. 2017, 29, 323–332. [Google Scholar] [CrossRef]
- Xu, J.; Bian, Y.H.; Jin, X.; Cao, H. Prognostic assessment of different metastatic lymph node staging methods for gastric cancer after D2 resection. World J. Gastroenterol. 2013, 19, 1975–1983. [Google Scholar] [CrossRef]
- Cao, J.; Yuan, P.; Ma, H.; Ye, P.; Wang, Y.; Yuan, X.; Bao, F.; Lv, W.; Hu, J. Log Odds of Positive Lymph Nodes Predicts Survival in Patients After Resection for Esophageal Cancer. Ann. Thorac. Surg. 2016, 102, 424–432. [Google Scholar] [CrossRef]
- Amini, N.; Kim, Y.; Wilson, A.; Margonis, G.A.; Ethun, C.G.; Poultsides, G.; Tran, T.; Idrees, K.; Isom, C.A.; Fields, R.C.; et al. Prognostic Implications of Lymph Node Status for Patients With Gallbladder Cancer: A Multi-Institutional Study. Ann. Surg. Oncol. 2016, 23, 3016–3023. [Google Scholar] [CrossRef]
- Wu, S.G.; Sun, J.Y.; Yang, L.C.; Zhou, J.; Li, F.Y.; Li, Q.; Lin, H.X.; Lin, Q.; He, Z.Y. Prognosis of patients with esophageal squamous cell carcinoma after esophagectomy using the log odds of positive lymph nodes. Oncotarget 2015, 6, 36911–36922. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Appleby, D.H.; Zhang, X.; Gan, L.; Wang, J.J.; Wan, F. Comparison of three lymph node staging schemes for predicting outcome in patients with gastric cancer. Br. J. Surg. 2013, 100, 505–514. [Google Scholar] [CrossRef]
- Persiani, R.; Cananzi, F.C.; Biondi, A.; Paliani, G.; Tufo, A.; Ferrara, F.; Vigorita, V.; D’Ugo, D. Log odds of positive lymph nodes in colon cancer: A meaningful ratio-based lymph node classification system. World J. Surg. 2012, 36, 667–674. [Google Scholar] [CrossRef]
- Team TRDC. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Xie, Y. Dynamic Documents with R and Knitr; Chapman and Hall/CRC: Boca Raton, FL, USA, 2015. [Google Scholar]
- Therneau, T. A Package for Survival Analysis in R. R Package Version 3.1–12. 2020. Available online: https://CRAN.R-project.org/package=survival (accessed on 4 May 2020).
- Sargent, D.; Sobrero, A.; Grothey, A.; O’Connell, M.J.; Buyse, M.; Andre, T.; Zheng, Y.; Green, E.; Labianca, R.; O’Callaghan, C.; et al. Evidence for cure by adjuvant therapy in colon cancer: Observations based on individual patient data from 20,898 patients on 18 randomized trials. J. Clin. Oncol. 2009, 27, 872–877. [Google Scholar] [CrossRef] [PubMed]
- Grothey, A.; Sobrero, A.F.; Shields, A.F.; Yoshino, T.; Paul, J.; Taieb, J.; Souglakos, J.; Shi, Q.; Kerr, R.; Labianca, R.; et al. Duration of Adjuvant Chemotherapy for Stage III Colon Cancer. N. Engl. J. Med. 2018, 378, 1177–1188. [Google Scholar] [CrossRef] [PubMed]
- Tomita, N.; Kunieda, K.; Maeda, A.; Hamada, C.; Yamanaka, T.; Sato, T.; Yoshida, K.; Boku, N.; Nezu, R.; Yamaguchi, S.; et al. Phase III randomised trial comparing 6 vs. 12-month of capecitabine as adjuvant chemotherapy for patients with stage III colon cancer: Final results of the JFMC37–0801 study. Br. J. Cancer 2019, 120, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Occhionorelli, S.; Andreotti, D.; Vallese, P.; Morganti, L.; Lacavalla, D.; Forini, E.; Pascale, G. Evaluation on prognostic efficacy of lymph nodes ratio (LNR) and log odds of positive lymph nodes (LODDS) in complicated colon cancer: The first study in emergency surgery. World J. Surg. Oncol. 2018, 16, 186. [Google Scholar] [CrossRef] [PubMed]
- Iveson, T.J.; Kerr, R.S.; Saunders, M.P.; Cassidy, J.; Hollander, N.H.; Tabernero, J.; Haydon, A.; Glimelius, B.; Harkin, A.; Allan, K.; et al. 3 versus 6 months of adjuvant oxaliplatin-fluoropyrimidine combination therapy for colorectal cancer (SCOT): An international, randomised, phase 3, non-inferiority trial. Lancet Oncol. 2018, 19, 562–578. [Google Scholar] [CrossRef]
- Conticchio, M.; Papagni, V.; Notarnicola, M.; Delvecchio, A.; Riccelli, U.; Ammendola, M.; Currò, G.; Pessaux, P.; Silvestris, N.; Memeo, R. Laparoscopic vs. open mesorectal excision for rectal cancer: Are these approaches still comparable? A systematic review and meta-analysis. PLoS ONE 2020, 15, e0235887. [Google Scholar] [CrossRef]
- Lorenzon, L.; La Torre, M.; Ziparo, V.; Montebelli, F.; Mercantini, P.; Balducci, G.; Ferri, M. Evidence based medicine and surgical approaches for colon cancer: Evidences, benefits and limitations of the laparoscopic vs open resection. World J. Gastroenterol. 2014, 20, 3680–3692. [Google Scholar] [CrossRef]
- Wu, Z.; Zhang, S.; Aung, L.H.; Ouyang, J.; Wei, L. Lymph node harvested in laparoscopic versus open colorectal cancer approaches: A meta-analysis. Surg. Laparosc. Endosc. Percutan Tech. 2012, 22, 5–11. [Google Scholar] [CrossRef]
- Truong, A.; Lopez, N.; Fleshner, P.; Zaghiyan, K. Preservation of Pathologic Outcomes in Robotic versus Open Resection for Rectal Cancer: Can the Robot Fill the Minimally Invasive Gap? Am. Surg. 2018, 84, 1876–1881. [Google Scholar] [CrossRef]
- Barnajian, M.; Pettet, D., 3rd; Kazi, E.; Foppa, C.; Bergamaschi, R. Quality of total mesorectal excision and depth of circumferential resection margin in rectal cancer: A matched comparison of the first 20 robotic cases. Colorectal Dis. 2014, 16, 603–609. [Google Scholar] [CrossRef] [PubMed]
| Variable | Overall | UICC I | UICC II | UICC III |
|---|---|---|---|---|
| Number of subjects | 654 | 171 | 232 | 251 |
| Age | ||||
| Median (range) | 70 (20–98) | 70 (37–89) | 69 (25–98) | 71 (20–96) |
| Gender | ||||
| Male | 364 (55.7) | 102 (59.6) | 129 (55.6) | 133 (53.0) |
| Female | 290 (44.3) | 69 (40.4) | 103 (44.4) | 118 (47.0) |
| Surgery type | ||||
| Right hemicolectomy | 178 (27.2) | 41 (24) | 63 (27.2) | 74 (29.5) |
| Extended right hemicolectomy | 32 (4.9) | 4 (2.3) | 20 (8.6) | 8 (3.2) |
| Transverse colectomy | 12(1.8) | 2 (1.2) | 6 (2.6) | 4 (1.6) |
| Extended left hemicolectomy | 13 (2.0) | 4 (2.3) | 7 (3.0) | 2 (0.8) |
| Left hemicolectomy | 40 (6.1) | 11 (6.4) | 11 (4.7) | 18 (7.2) |
| Sigmoid colectomy | 104 (15.9) | 24 (14.0) | 42 (18.1) | 38 (15.1) |
| Anterior resection | 216 (33) | 72 (42.1) | 59 (25.4) | 85 (33.9) |
| Abdominoperineal resection | 24 (3.7) | 7 (4.1) | 11 (4.7) | 6 (2.4) |
| others | 35 (5.4) | 6 (3.5) | 13 (5.6) | 16 (6.4) |
| Tumor location | ||||
| Caecum | 59 (9.0) | 14 (8.2) | 19 (8.2) | 26 (10.4) |
| Ascending colon | 127 (19.4) | 28 (16.4) | 22 (22.0) | 48 (19.1) |
| Transverse colon | 64 (9.8) | 9 (5.3) | 35 (15.1) | 20 (8.0) |
| Descending colon | 37 (5.7) | 14 (8.2) | 7 (3.0) | 16 (6.4) |
| Sigmoid colon | 112 (17.1) | 24 (14.0) | 47 (20.3) | 41 (16.3) |
| Rectum | 239 (36.5) | 80 (46.8) | 69 (29.7) | 90 (35.9) |
| Synchronous tumors | 16 (2.4) | 2 (1.2) | 4 (1.7) | 10 (4.0) |
| T stage | ||||
| T1 | 51 (7.8) | 45 (26.3) | 6 (2.4) | |
| T2 | 155 (23.7) | 126 (73.7) | 29 (11.6) | |
| T3 | 383 (58.6) | 207 (89.2) | 176 (70.1) | |
| T4 | 65 (9.9) | 25 (10.8) | 40 (15.9) | |
| N stage | ||||
| N0 | 403 (61.6) | 171 (100) | 232 (100) | |
| N1 | 163 (24.9) | 163 (64.9) | ||
| N2 | 88 (13.5) | 88 (35.1) | ||
| No. of examined LN, median (range) | 17 (2–68) | 15 (3–53) | 17 (2–62) | 19 (6–68) |
| No. of positive LN, median (range) | 0 (0–56) | 0 | 0 | 2 (0–56) * |
| Tumor differentiation | ||||
| G1 | 17 (2.6) | 7 (4.1) | 6 (2.6) | 4 (1.6) |
| G2 | 524 (80.1) | 146 (85.4) | 190 (81.9) | 188 (74.9) |
| G3 | 101 (15.4) | 14 (8.2) | 31 (13.4) | 56 (22.3) |
| G4 | 1 (0.2) | 1 (0.6) | 0 (0) | 0 (0) |
| Unknown | 11 (1.7) | 3 (1.8) | 5 (2.2) | 3 (1.2) |
| Neoadjuvant treatment | ||||
| No | 590 (90.2) | 149 (87.1) | 205 (88.4) | 236 (94) |
| Yes | 64 (9.8) | 22 (12.9) | 27 (11.6) | 15 (6.0) |
| Risk Factor | HR (95% CI) | p |
|---|---|---|
| Age | ||
| Age < 70 | 1.00 (reference) | <0.001 |
| Age ≥ 70 | 3.32 (2.53–4.36) | |
| Gender | ||
| Female | 1.00 (reference) | 0.108 |
| Male | 1.23 (0.95–1.59) | |
| Tumor size | ||
| <median | 1.00 (reference) | 0.044 |
| ≥median | 1.32 (1.01–1.73) | |
| Grading | ||
| G1 + G2 | 1.00 (reference) | 0.001 |
| G3 + G4 | 1.69 (1.23–2.30) | |
| T stage | ||
| T1 + T2 | 1.00 (reference) | 1.017 |
| T3 + T4 | 1.43 | |
| Tumor | ||
| localization | ||
| Colon | 1.00 (reference) | 0.005 |
| Rectum | 1.46 (1.12–1.89) |
| LN Classification | HR (95% CI) | C-Index (95% CI) | Delta C | Pc |
|---|---|---|---|---|
| LNR Lee et al. [21] | 0.6955 (0.6668–0.7242) | 0.0166 | 0.037 | |
| ≥0; ≤0.1 | 1.000 (Reference) | |||
| >0.1; ≤0.2 | 1.321 (0.836–2.087) | |||
| >0.2; ≤0.3 | 1.947 (1.006–3.767) | |||
| >0.3 | 2.133 (1.349–3.373) | |||
| LNR Fortea-Sanchis et al. [2] | 0.6995 (0.6708–0.7282) | 0.0207 | 0.031 | |
| 0; 0.24 | 1.000 (Reference) | |||
| 0.25; 0.60 | 1.811 (1.191–2.754) | |||
| >0.60 | 3.514 (1.785–6.915) | |||
| LODDS Fortea-Sanchis et al. [2] | 0.7020 (0.6732–0.7308) | 0.0231 | 0.027 | |
| <−2 | 1.000 (Reference) | |||
| ≥−2; ≤−1 | 1.299 (0.840–2.008) | |||
| >−1 | 2.387 (1.538–3.707) | |||
| LODDS He et al. [35] | 0.7023 (0.6735–0.7311) | 0.0235 | 0.036 | |
| <−3 | 1.000 (Reference) | |||
| ≥−3; <−2 | 1.397 (0.425–4.600) | |||
| ≥−2; <−1 | 1.794 (0.541–5.953) | |||
| ≥−1; <0 | 2.363 (0.685–8.157) | |||
| ≥0 | 5.457 (1.563–19.054) | |||
| LODDS Calero et al. [20] | 0.6998 (0.6710–0.7286) | 0.0210 | 0.036 | |
| ≤−3 | 1.000 (Reference) | |||
| >−3; ≤−1 | 1.552 (0.481–5.011) | |||
| >−1; ≤3 | 3.195 (0.962–10.607) | |||
| >3 | 3.324 (0.526–21.012) | |||
| LODDS Bagante et al. [23] | 0.6977 (0.6710–0.7290) | 0.0188 | 0.038 | |
| <−2 | 1.000 (Reference) | |||
| ≥−2; ≤−0.9 | 1.413 (0.921–2.168) | |||
| >0.9; ≤1.5 | 2.162 (1.354–3.453) | |||
| >1.5 | 3.396 (1.390–8.297) | |||
| LODDS Jian-Hui et al. [24] | 0.7080 (0.6790–0.7370) | 0.0180 | 0.027 | |
| ≤−1.5 | 1.000 (Reference) | |||
| >−1.5; ≤−1 | 1.233 (0.740–2.054) | |||
| >−1; ≤0 | 1.619 (0.992–2.641) | |||
| >0 | 4.324 (2.441–7.658) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prassas, D.; Verde, P.E.; Pavljak, C.; Rehders, A.; Krieg, S.; Luedde, T.; Knoefel, W.T.; Krieg, A. Prognostic Discrimination of Alternative Lymph Node Classification Systems for Patients with Radically Resected Non-Metastatic Colorectal Cancer: A Cohort Study from a Single Tertiary Referral Center. Cancers 2021, 13, 3898. https://doi.org/10.3390/cancers13153898
Prassas D, Verde PE, Pavljak C, Rehders A, Krieg S, Luedde T, Knoefel WT, Krieg A. Prognostic Discrimination of Alternative Lymph Node Classification Systems for Patients with Radically Resected Non-Metastatic Colorectal Cancer: A Cohort Study from a Single Tertiary Referral Center. Cancers. 2021; 13(15):3898. https://doi.org/10.3390/cancers13153898
Chicago/Turabian StylePrassas, Dimitrios, Pablo Emilio Verde, Carlo Pavljak, Alexander Rehders, Sarah Krieg, Tom Luedde, Wolfram Trudo Knoefel, and Andreas Krieg. 2021. "Prognostic Discrimination of Alternative Lymph Node Classification Systems for Patients with Radically Resected Non-Metastatic Colorectal Cancer: A Cohort Study from a Single Tertiary Referral Center" Cancers 13, no. 15: 3898. https://doi.org/10.3390/cancers13153898
APA StylePrassas, D., Verde, P. E., Pavljak, C., Rehders, A., Krieg, S., Luedde, T., Knoefel, W. T., & Krieg, A. (2021). Prognostic Discrimination of Alternative Lymph Node Classification Systems for Patients with Radically Resected Non-Metastatic Colorectal Cancer: A Cohort Study from a Single Tertiary Referral Center. Cancers, 13(15), 3898. https://doi.org/10.3390/cancers13153898







