Patients with Primary Central Nervous System Lymphoma Not Eligible for Clinical Trials: Prognostic Factors, Treatment and Outcome
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Characteristics
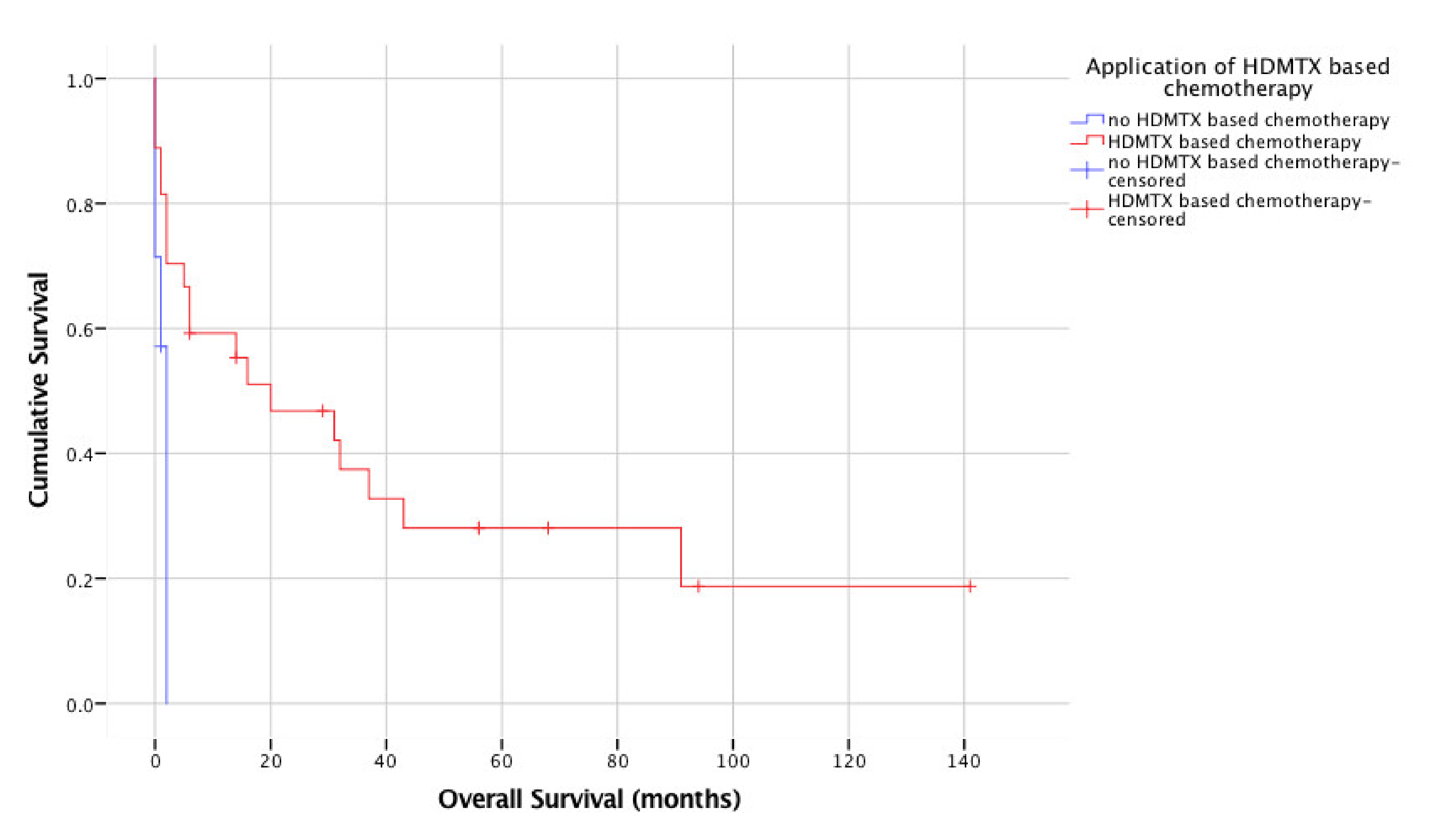
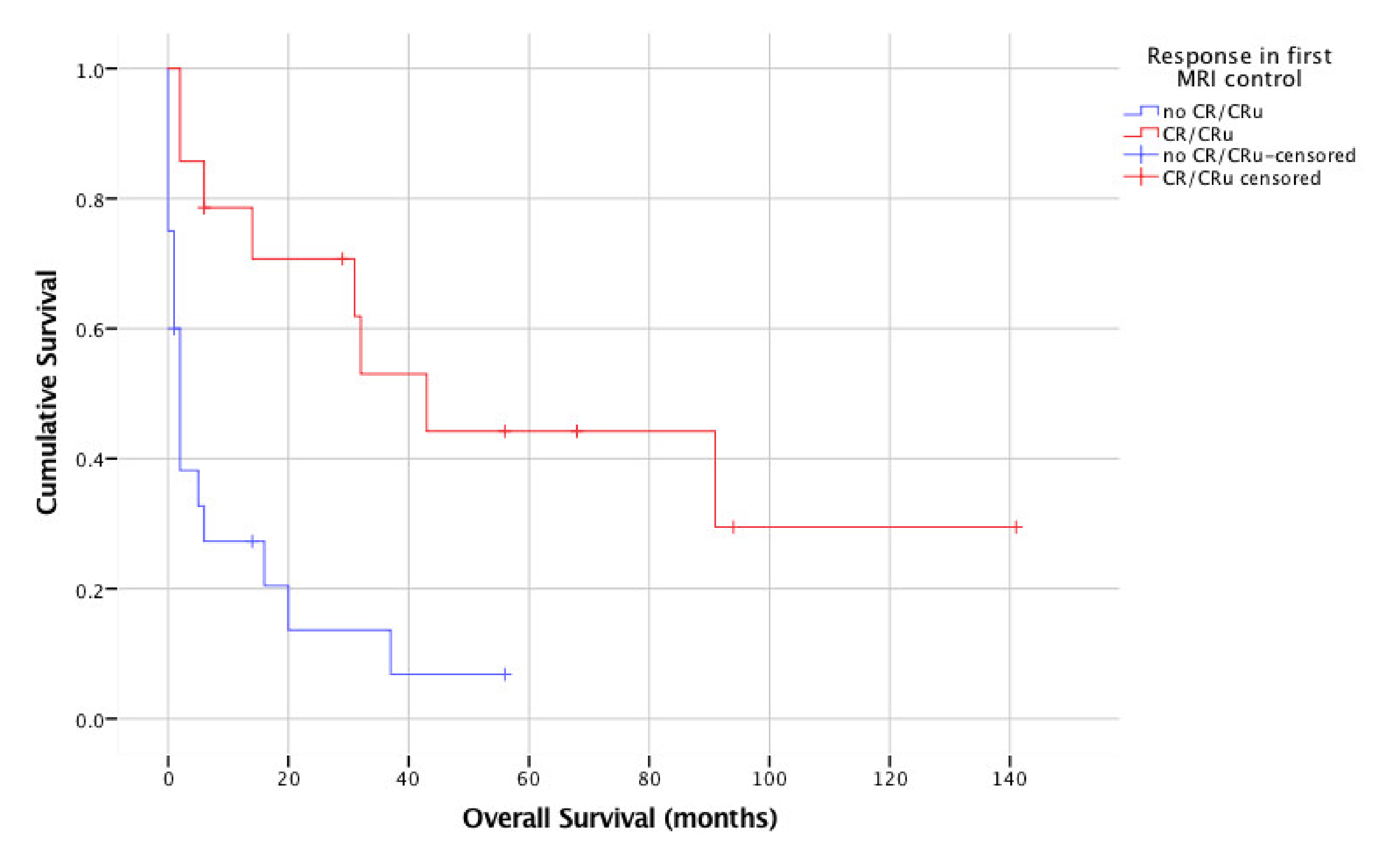
3.2. Treatment, Response and Survival
3.3. Prognostic Factors in Non-Study Patients
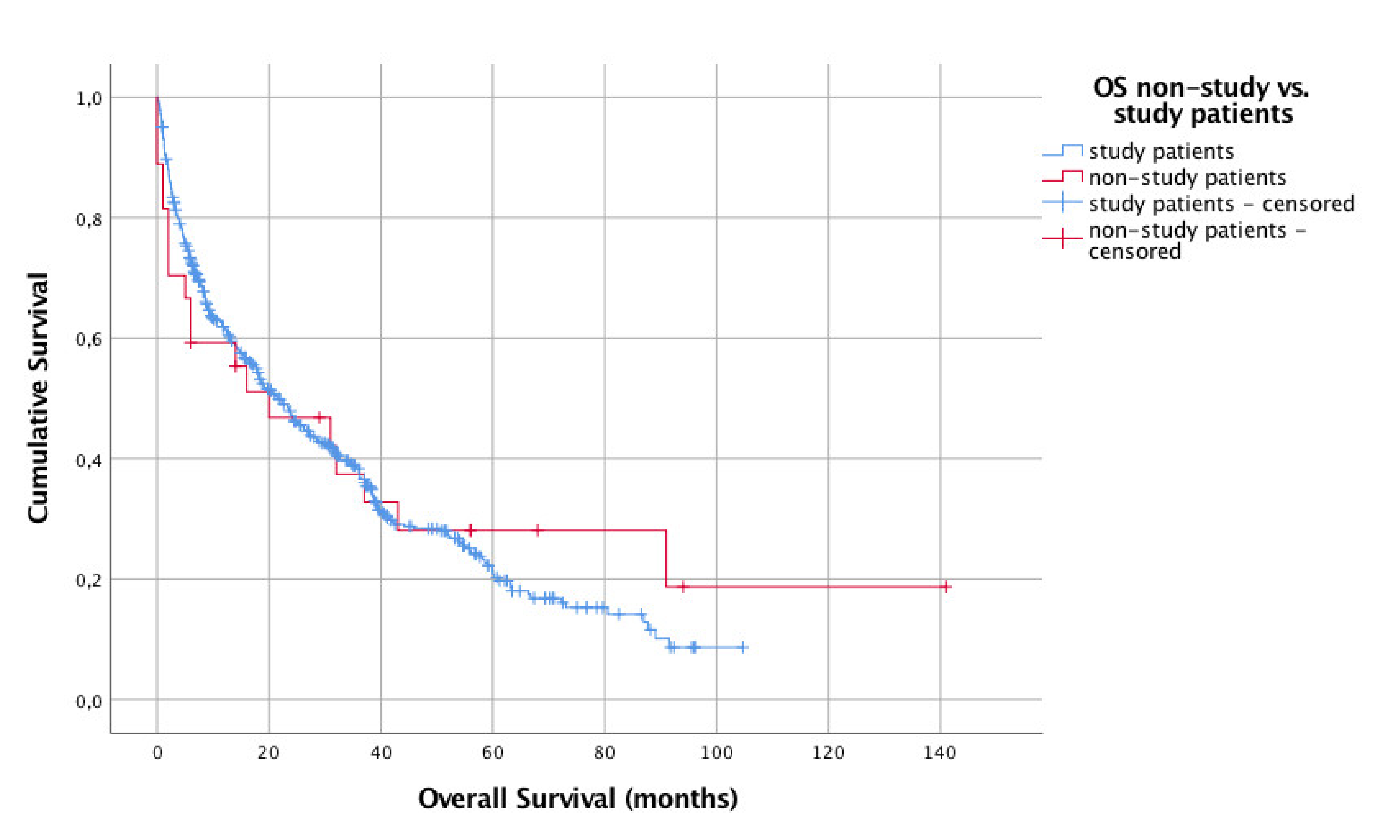
3.4. Comparison of Non-Study Patients and Study Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Cioffi, G.; Gittleman, H.; Patil, N.; Waite, K.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016. Neuro. Oncol. 2019, 21, v1–v100. [Google Scholar] [CrossRef]
- Pulczynski, E.J.; Kuittinen, O.; Erlanson, M.; Hagberg, H.; Fosså, A.; Eriksson, M.; Nordstrøm, M.; Østenstad, B.; Fluge, Ø.; Leppä, S.; et al. Successful change of treatment strategy in elderly patients with primary central nervous system lymphoma by de-escalating induction and introducing temozolomide maintenance: Results from a phase II study by the Nordic Lymphoma Group. Haematologica 2015, 100, 534–540. [Google Scholar] [CrossRef]
- Pels, H.; Schmidt-Wolf, I.G.H.; Glasmacher, A.; Schulz, H.; Engert, A.; Diehl, V.; Zellner, A.; Schackert, G.; Reichmann, H.; Kroschinsky, F.; et al. Primary central nervous system lymphoma: Results of a pilot and phase II study of systemic and intraventricular chemotherapy with deferred radiotherapy. J. Clin. Oncol. 2003, 21, 4489–4495. [Google Scholar] [CrossRef]
- Bromberg, J.E.C.; Issa, S.; Bakunina, K.; Minnema, M.C.; Seute, T.; Durian, M.; Cull, G.; Schouten, H.C.; Stevens, W.B.C.; Zijlstra, J.M.; et al. Rituximab in patients with primary CNS lymphoma (HOVON 105/ALLG NHL 24): A randomised, open-label, phase 3 intergroup study. Lancet. Oncol. 2019, 20, 216–228. [Google Scholar] [CrossRef]
- Rubenstein, J.L.; Hsi, E.D.; Johnson, J.L.; Jung, S.-H.; Nakashima, M.O.; Grant, B.; Cheson, B.D.; Kaplan, L.D. Intensive chemotherapy and immunotherapy in patients with newly diagnosed primary CNS lymphoma: CALGB 50202 (Alliance 50202). J. Clin. Oncol. 2013, 31, 3061–3068. [Google Scholar] [CrossRef] [PubMed]
- Morris, P.G.; Correa, D.D.; Yahalom, J.; Raizer, J.J.; Schiff, D.; Grant, B.; Grimm, S.; Lai, R.K.; Reiner, A.S.; Panageas, K.; et al. Rituximab, methotrexate, procarbazine, and vincristine followed by consolidation reduced-dose whole-brain radiotherapy and cytarabine in newly diagnosed primary CNS lymphoma: Final results and long-term outcome. J. Clin. Oncol. 2013, 31, 3971–3979. [Google Scholar] [CrossRef] [PubMed]
- Thiel, E.; Korfel, A.; Martus, P.; Kanz, L.; Griesinger, F.; Rauch, M.; Röth, A.; Hertenstein, B.; von Toll, T.; Hundsberger, T.; et al. High-dose methotrexate with or without whole brain radiotherapy for primary CNS lymphoma (G-PCNSL-SG-1): A phase 3, randomised, non-inferiority trial. Lancet Oncol. 2010, 11, 1036–1047. [Google Scholar] [CrossRef]
- Fritsch, K.; Kasenda, B.; Schorb, E.; Hau, P.; Bloehdorn, J.; Möhle, R.; Löw, S.; Binder, M.; Atta, J.; Keller, U.; et al. High-dose methotrexate-based immuno-chemotherapy for elderly primary CNS lymphoma patients (PRIMAIN study). Leukemia 2017, 31, 846–852. [Google Scholar] [CrossRef]
- Omuro, A.; Chinot, O.; Taillandier, L.; Ghesquieres, H.; Soussain, C.; Delwail, V.; Lamy, T.; Gressin, R.; Choquet, S.; Soubeyran, P.; et al. Methotrexate and temozolomide versus methotrexate, procarbazine, vincristine, and cytarabine for primary CNS lymphoma in an elderly population: An intergroup ANOCEF-GOELAMS randomised phase 2 trial. Lancet Haematol. 2015, 2, e251–e259. [Google Scholar] [CrossRef]
- Ferreri, A.J.M.; Reni, M.; Foppoli, M.; Martelli, M.; Pangalis, G.A.; Frezzato, M.; Cabras, M.G.; Fabbri, A.; Corazzelli, G.; Ilariucci, F.; et al. High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: A randomised phase 2 trial. Lancet 2009, 374, 1512–1520. [Google Scholar] [CrossRef]
- Illerhaus, G.; Kasenda, B.; Ihorst, G.; Egerer, G.; Lamprecht, M.; Keller, U.; Wolf, H.H.; Hirt, C.; Stilgenbauer, S.; Binder, M.; et al. High-dose chemotherapy with autologous haemopoietic stem cell transplantation for newly diagnosed primary CNS lymphoma: A prospective, single-arm, phase 2 trial. Lancet Haematol. 2016, 3, e388–e397. [Google Scholar] [CrossRef]
- Ferreri, A.J.M.; Cwynarski, K.; Pulczynski, E.; Ponzoni, M.; Deckert, M.; Politi, L.S.; Torri, V.; Fox, C.P.; La Rosée, P.; Schorb, E.; et al. Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: Results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol. 2016, 3, e217–e227. [Google Scholar] [CrossRef]
- Ferreri, A.J.M.; Cwynarski, K.; Pulczynski, E.; Fox, C.P.; Schorb, E.; La Rosée, P.; Binder, M.; Fabbri, A.; Torri, V.; Minacapelli, E.; et al. Whole-brain radiotherapy or autologous stem-cell transplantation as consolidation strategies after high-dose methotrexate-based chemoimmunotherapy in patients with primary CNS lymphoma: Results of the second randomisation of the International Extranodal L. Lancet Haematol. 2017, 4, e510–e523. [Google Scholar] [CrossRef]
- Houillier, C.; Taillandier, L.; Dureau, S.; Lamy, T.; Laadhari, M.; Chinot, O.; Moluçon-Chabrot, C.; Soubeyran, P.; Gressin, R.; Choquet, S.; et al. Radiotherapy or autologous stem-cell transplantation for primary CNS lymphoma in patients 60 years of age and younger: Results of the intergroup ANOCEF-GOELAMS randomized phase II PRECIS study. J. Clin. Oncol. 2019, 37, 823–833. [Google Scholar] [CrossRef]
- Omuro, A.; Correa, D.D.; DeAngelis, L.M.; Moskowitz, C.H.; Matasar, M.J.; Kaley, T.J.; Gavrilovic, I.T.; Nolan, C.; Pentsova, E.; Grommes, C.C.; et al. R-MPV followed by high-dose chemotherapy with TBC and autologous stem-cell transplant for newly diagnosed primary CNS lymphoma. Blood 2015. [Google Scholar] [CrossRef]
- Cavaliere, R.; Petroni, G.; Lopes, M.B.; Schiff, D. Primary central nervous system post-transplantation lymphoproliferative disorder: An International Primary Central Nervous System Lymphoma Collaborative Group Report. Cancer 2010, 116, 863–870. [Google Scholar] [CrossRef]
- Kaulen, L.D.; Karschnia, P.; Dietrich, J.; Baehring, J.M. Autoimmune disease-related primary CNS lymphoma: Systematic review and meta-analysis. J. Neurooncol. 2020, 149, 153–159. [Google Scholar] [CrossRef]
- Seidel, S.; Korfel, A.; Kowalski, T.; Margold, M.; Ismail, F.; Schroers, R.; Baraniskin, A.; Pels, H.; Martus, P.; Schlegel, U. HDMTX-based induction therapy followed by consolidation with conventional systemic chemotherapy and intraventricular therapy ( modified Bonn protocol ) in primary CNS lymphoma: A monocentric retrospective analysis. Neurol. Res. Pract. 2019, 2, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Küker, W.; Nägele, T.; Thiel, E.; Weller, M.; Herrlinger, U. Primary central nervous system lymphomas (PCNSL): MRI response criteria revised. Neurology 2005, 65, 1129–1131. [Google Scholar] [CrossRef]
- Klein, J.P.; Moeschberger, M.L. Survival Analysis, 1st ed.; Springer: New York, NY, USA, 1997; p. 112. [Google Scholar]
- Abrey, L.E.; Ben-Porat, L.; Panageas, K.S.; Yahalom, J.; Berkey, B.; Curran, W.; Schultz, C.; Leibel, S.; Nelson, D.; Mehta, M.; et al. Primary central nervous system lymphoma: The Memorial Sloan-Kettering Cancer Center prognostic model. J. Clin. Oncol. 2006, 24, 5711–5715. [Google Scholar] [CrossRef]
- Ferreri, A.J.M.; Blay, J.-Y.; Reni, M.; Pasini, F.; Spina, M.; Ambrosetti, A.; Calderoni, A.; Rossi, A.; Vavassori, V.; Conconi, A.; et al. Prognostic scoring system for primary CNS lymphomas: The International Extranodal Lymphoma Study Group experience. J. Clin. Oncol. 2003, 21, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Blay, J.Y.; Conroy, T.; Chevreau, C.; Thyss, A.; Quesnel, N.; Eghbali, H.; Bouabdallah, R.; Coiffier, B.; Wagner, J.P.; Le Mevel, A.; et al. High-dose methotrexate for the treatment of primary cerebral lymphomas: Analysis of survival and late neurologic toxicity in a retrospective series. J. Clin. Oncol. 1998, 16, 864–871. [Google Scholar] [CrossRef]
- Pels, H.; Juergens, A.; Schirgens, I.; Glasmacher, A.; Schulz, H.; Engert, A.; Schackert, G.; Reichmann, H.; Kroschinsky, F.; Vogt-Schaden, M.; et al. Early complete response during chemotherapy predicts favorable outcome in patients with primary CNS lymphoma. Neuro. Oncol. 2010, 12, 720–724. [Google Scholar] [CrossRef] [PubMed]
- Sarid, N.; Bokstein, F.; Blumenthal, D.T.; Weiss-Meilik, A.; Gibstein, L.; Avivi, I.; Perry, C.; Ram, R. Impact of contemporary regimens on the outcomes and toxicity of primary CNS lymphoma: A single-center retrospective analysis of 73 patients. J. Neurooncol. 2021, 151, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Zeremski, V.; Koehler, M.; Fischer, T.; Schalk, E. Characteristics and outcome of patients with primary CNS lymphoma in a “real-life” setting compared to a clinical trial. Ann. Hematol. 2016, 95, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Houillier, C.; Soussain, C.; Ghesquières, H.; Soubeyran, P.; Chinot, O.; Taillandier, L.; Lamy, T.; Choquet, S.; Ahle, G.; Damaj, G.; et al. Management and outcome of primary CNS lymphoma in the modern era. Neurology 2020, 94, e1027–e1039. [Google Scholar] [CrossRef]
- Hart, A.; Baars, J.W.; Kersten, M.J.; Brandsma, D.; van Tinteren, H.; de Jong, D.; Spiering, M.; Dewit, L.; Boogerd, W. Outcome of patients with primary central nervous system lymphoma treated outside clinical trials. Neth. J. Med. 2014, 72, 218–223. [Google Scholar]
- Korfel, A.; Martus, P.; Nowrousian, M.R.; Hossfeld, D.K.; Kirchen, H.; Brücher, J.; Stelljes, M.; Birkmann, J.; Peschel, C.; Pasold, R.; et al. Response to chemotherapy and treating institution predict survival in primary central nervous system lymphoma. Br. J. Haematol. 2005, 128, 177–183. [Google Scholar] [CrossRef]
- Seidel, S.; Schlegel, U. Have treatment protocols for primary CNS lymphoma advanced in the past 10 years. Expert Rev. Anticancer Ther. 2019, 19. [Google Scholar] [CrossRef]
| Chemotherapy | Day 0 | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 |
| Cycles 1–3 (1 cycle = 2 weeks) | x | x | |||||
| Rituximab 375–500 mg/m2 IVa | |||||||
| MTX 3000–5000 mg/m2 IV | x | ||||||
| Ifosfamide 800 mg/m2 IV | x | x | |||||
| Liposomal AraC 50 mg ITHb | x | ||||||
| x | |||||||
| Cycles 4 + 6 (1 cycle = 3 weeks) | x | ||||||
| Cytarabine 3000 mg/m2 IV | x | ||||||
| Liposomal AraC 50 mg ITHb | |||||||
| MTX 2,5 mg + prednisolone 3 mg ICVc | x | x | x | ||||
| AraC 10 mg ICVc | x | ||||||
| x | |||||||
| Cycle 5 (1 cycle = 2 weeks)d | |||||||
| MTX 3000–5000 mg/m2 IV | x | x | |||||
| Ifosfamide 800 mg/m2 IV | x | x | |||||
| Liposomal AraC 50 mg ITH b | x | x | |||||
| MTX 2,5 mg + prednisolone 3 mg ICVc | x | ||||||
| AraC 10 mg ICVc | x |
| Characteristics | All Non-Study Patients (n = 34) | Non-Study Patients with HDMTX (n = 27) | Study Patients in G-PCNSL-SG1 (n = 526) |
|---|---|---|---|
| Age, years | |||
| Median (range*) | 74.5 (65–77) | 71 (62–76) | 63 (55–69) |
| < 65 years | 9 (26.5%) | 9 (33.3%) | 291 (55.3%) |
| ≥ 65 years | 25 (73.5%) | 18 (66.7%) | 235 (44.7%) |
| Sex | |||
| Male | 13 (38.2%) | 12 (44.4%) | 299 (56.8%) |
| Female | 21 (61.8%) | 15 (55.6%) | 227 (43.2%) |
| KPS | |||
| Median (range*) | 40 (30–50) | 40 (20–50) | 70 (50–90) |
| Involvement of deep brain structures | |||
| Yes | 27 (79.4%) | 22 (81.5%) | data not available |
| No | 7 (20.6%) | 5 (18.5%) | |
| Lactate dehydrogenase | |||
| Normal | 18 (52.9%) | 12 (44.4%) | 198 (37.6%) |
| Elevated | 15 (44.1%) | 14 (51.9%) | 109 (20.7%) |
| Not done | 1 (3%) | 1 (3.7%) | 30 (5.7%) |
| No specification | 0 | 0 | 189 (35.9%) |
| CSF cytology | |||
| Positive | 2 (5.9%) | 1 (3.7%) | 44 (8.4 %) |
| Negative | 18 (52.9%) | 17 (63.0%) | 294 (55.9%) |
| Suspect | 0 | 0 | 23 (4.4%) |
| Not done/no specification | 14 (41.2%) | 9 (33.3%) | 165 (31.4%) |
| CSF protein elevation | |||
| Elevated | 14 (41.2%) | 13 (48.1%) | 154 (29.3%) |
| Normal | 6 (17.6%) | 5 (18.5%) | 150 (29.3%) |
| Not done/no specification | 14 (41.2%) | 9 (33.3%) | 222 (42.2%) |
| Model | Variable | Hazard ratio | p | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|
| 27 vs. 526 patients, univariate | Arm a | 0.93 | 0.766 | 0.586 | 1.483 |
| 27 vs. 526 patients, multivariate | Arm a Age b | 0.48 1.39 | 0.005 <0.001 | 0.29 1.24 | 0.80 1.55 |
| Karnofsky c | 0.87 | <0.001 | 0.82 | 0.92 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seidel, S.; Margold, M.; Kowalski, T.; Baraniskin, A.; Schroers, R.; Korfel, A.; Thiel, E.; Weller, M.; Martus, P.; Schlegel, U. Patients with Primary Central Nervous System Lymphoma Not Eligible for Clinical Trials: Prognostic Factors, Treatment and Outcome. Cancers 2021, 13, 2934. https://doi.org/10.3390/cancers13122934
Seidel S, Margold M, Kowalski T, Baraniskin A, Schroers R, Korfel A, Thiel E, Weller M, Martus P, Schlegel U. Patients with Primary Central Nervous System Lymphoma Not Eligible for Clinical Trials: Prognostic Factors, Treatment and Outcome. Cancers. 2021; 13(12):2934. https://doi.org/10.3390/cancers13122934
Chicago/Turabian StyleSeidel, Sabine, Michelle Margold, Thomas Kowalski, Alexander Baraniskin, Roland Schroers, Agnieszka Korfel, Eckhard Thiel, Michael Weller, Peter Martus, and Uwe Schlegel. 2021. "Patients with Primary Central Nervous System Lymphoma Not Eligible for Clinical Trials: Prognostic Factors, Treatment and Outcome" Cancers 13, no. 12: 2934. https://doi.org/10.3390/cancers13122934
APA StyleSeidel, S., Margold, M., Kowalski, T., Baraniskin, A., Schroers, R., Korfel, A., Thiel, E., Weller, M., Martus, P., & Schlegel, U. (2021). Patients with Primary Central Nervous System Lymphoma Not Eligible for Clinical Trials: Prognostic Factors, Treatment and Outcome. Cancers, 13(12), 2934. https://doi.org/10.3390/cancers13122934






