Is the Concurrent Use of Sorafenib and External Radiotherapy Feasible for Advanced Hepatocellular Carcinoma? A Meta-Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Searching Process
2.2. Data Items and Collection
2.3. Risk of Bias and Assessment of the Quality
2.4. Statistics
2.5. Protocol Registration
3. Results
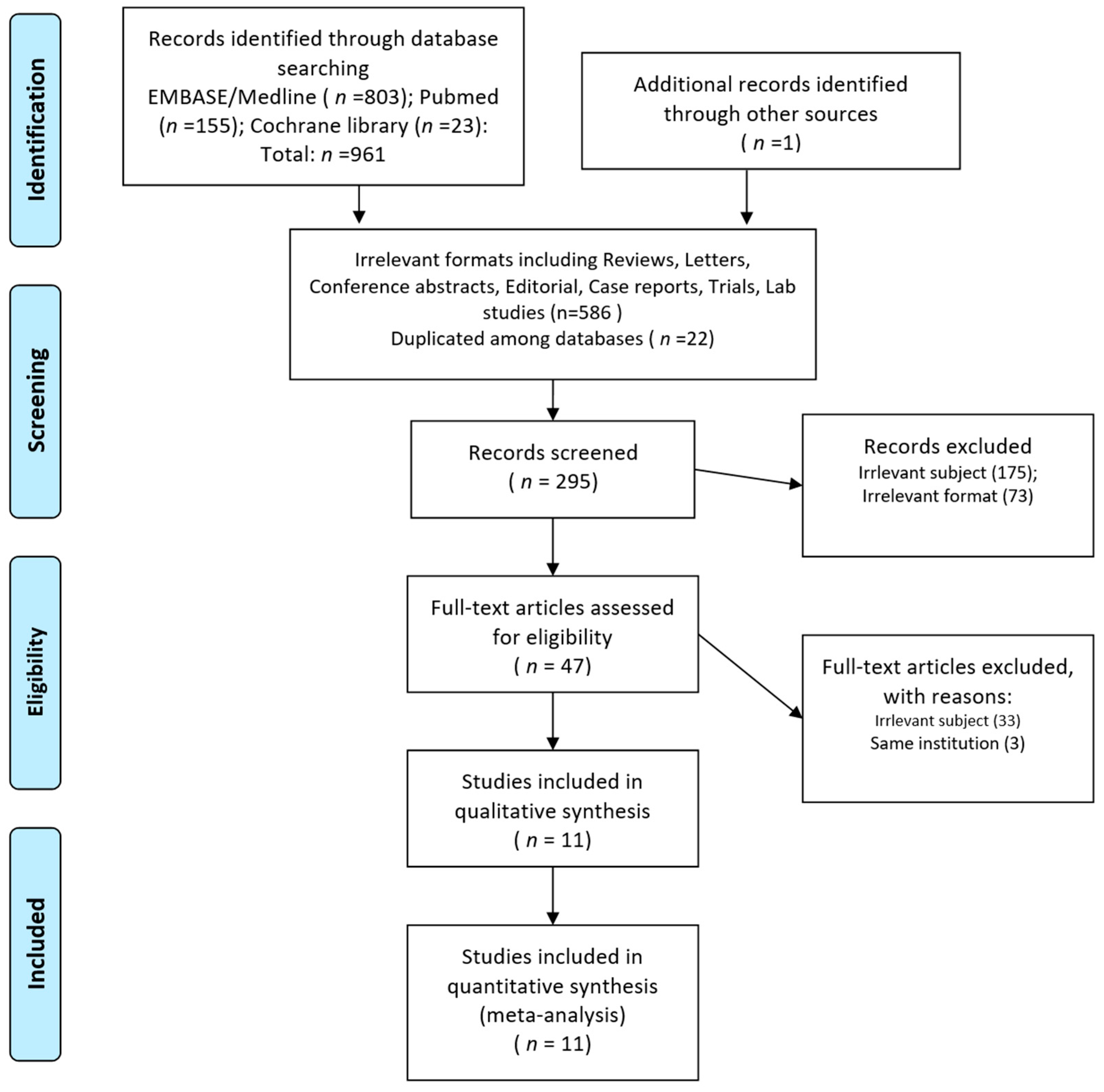
3.1. Study Selection and Characteristics
3.2. Quality Assessment and Selection of Studies
3.3. Summary of Individual Study Results
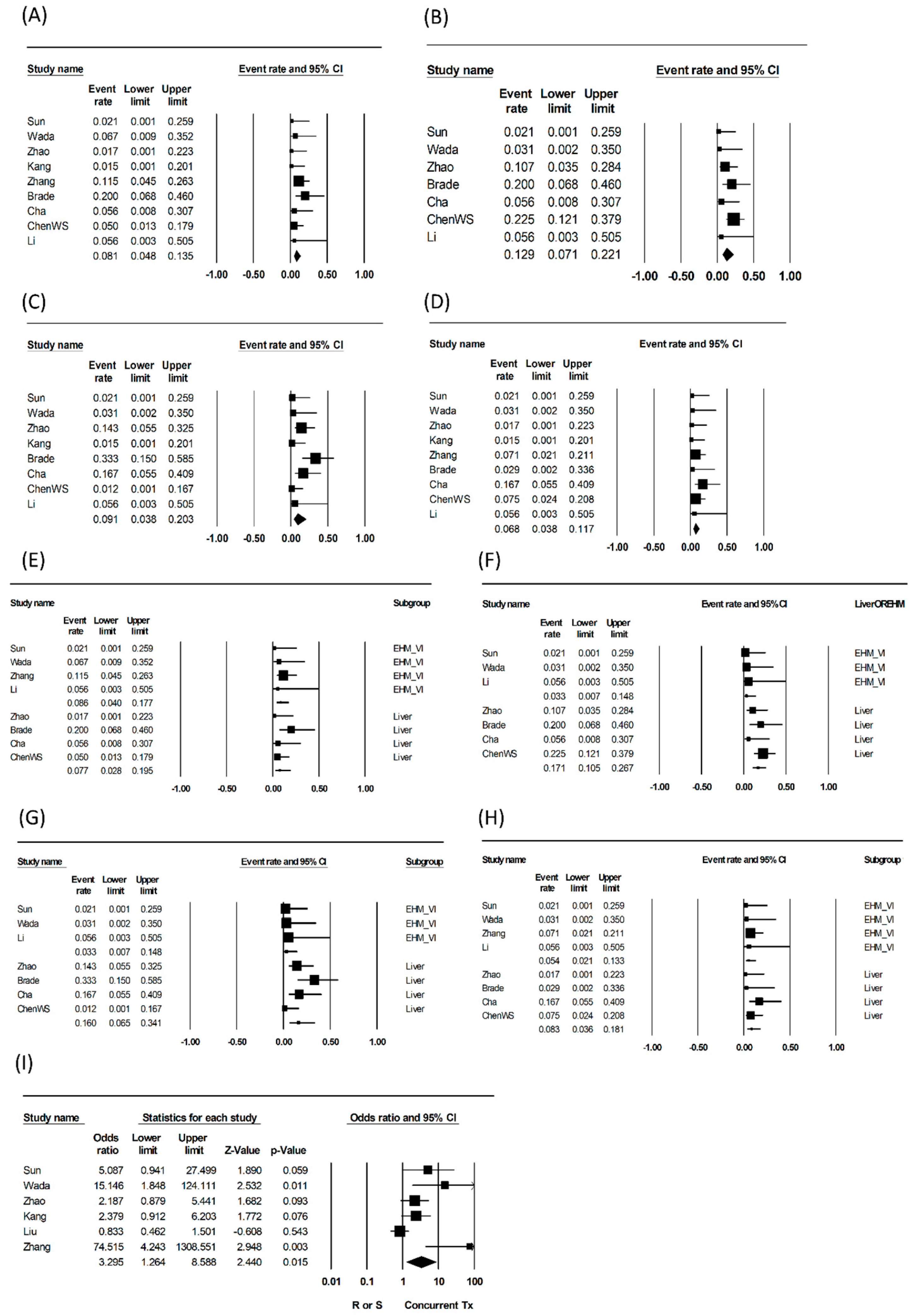
3.4. Synthesized Results and Qualitative Analyses of Endpoints
3.5. Qualitative Assessment of Grade 4 or 5 and Descriptive Toxicities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethical Consideration and Consent for Publication
References
- Cassim, S.; Raymond, V.A.; Lacoste, B.; Lapierre, P.; Bilodeau, M. Metabolite profiling identifies a signature of tumorigenicity in hepatocellular carcinoma. Oncotarget 2018, 9, 26868–26883. [Google Scholar] [CrossRef]
- Dai, J.; Zhao, J.; Du, Y.; Zhuang, L.; McNeil, E.B.; Chongsuvivatwong, V. Adherence to Hepatocellular Carcinoma Surveillance and Perceived Barriers Among High-Risk Chronic Liver Disease Patients in Yunnan, China. Cancer Manag. Res. 2020, 12, 6209–6220. [Google Scholar] [CrossRef]
- Ayuso, C.; Rimola, J.; García-Criado, A. Imaging of HCC. Abdom. Imaging 2012, 37, 215–230. [Google Scholar] [CrossRef]
- Burrel, M.; Llovet, J.M.; Ayuso, C.; Iglesias, C.; Sala, M.; Miquel, R.; Caralt, T.; Ayuso, J.R.; Solé, M.; Sanchez, M.; et al. MRI angiography is superior to helical CT for detection of HCC prior to liver transplantation: An explant correlation. Hepatology 2003, 38, 1034–1042. [Google Scholar] [CrossRef] [PubMed]
- Chalasani, N.; Horlander, J.C., Sr.; Said, A.; Hoen, H.; Kopecky, K.K.; Stockberger, S.M., Jr.; Manam, R.; Kwo, P.Y.; Lumeng, L. Screening for hepatocellular carcinoma in patients with advanced cirrhosis. Am. J. Gastroenterol. 1999, 94, 2988–2993. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Qin, S.K. Features and treatment options of Chinese hepatocellular carcinoma. Chin. Clin. Oncol. 2013, 2, 38. [Google Scholar] [PubMed]
- Lee, J.; Yoon, W.S.; Koom, W.S.; Rim, C.H. Role of local treatment including radiotherapy in Barcelona Clinic of Liver Cancer stage C patients: A nationwide cohort analysis in South Korea. Cancer Manag. Res. 2019, 11, 1373–1382. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, T.S.; Blackstock, A.W.; McGinn, C. (Eds.) The Mechanism of Action of Radiosensitization of Conventional Chemotherapeutic Agents; Seminars in radiation oncology; Elsevier: Amsterdam, The Netherlands, 2003. [Google Scholar]
- Wilson, G.D.; Bentzen, S.M.; Harari, P.M. (Eds.) Biologic Basis for Combining Drugs with Radiation; Seminars in radiation oncology; Elsevier: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.F.; De Oliveira, A.C.; Santoro, A.; Raoul, J.L.; Forner, A.; et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.A.; Park, S.; Seo, Y.S.; Yoon, W.S.; Rim, C.H.; Group KLCS. Benefits of Local Treatment Including External Radiotherapy for Hepatocellular Carcinoma with Portal Invasion. Biology 2021, 10, 326. [Google Scholar] [CrossRef] [PubMed]
- Rim, C.H.; Kim, C.Y.; Yang, D.S.; Yoon, W.S. Comparison of radiation therapy modalities for hepatocellular carcinoma with portal vein thrombosis: A meta-analysis and systematic review. Radiother. Oncol. 2018, 129, 112–122. [Google Scholar] [CrossRef] [PubMed]
- Rim, C.H.; Yoon, W.S. Leaflet manual of external beam radiation therapy for hepatocellular carcinoma: A review of the indications, evidences, and clinical trials. OncoTargets Ther. 2018, 11, 2865. [Google Scholar] [CrossRef]
- Girard, N.; Mornex, F. Sorafenib and radiotherapy association for hepatocellular carcinoma. Cancer Radiother 2011, 15, 77–80. [Google Scholar] [CrossRef]
- Yu, W.; Gu, K.; Yu, Z.; Yuan, D.; He, M.; Ma, N.; Lai, S.; Zhao, J.; Ren, Z.; Zhang, X.; et al. Sorafenib potentiates irradiation effect in hepatocellular carcinoma in vitro and in vivo. Cancer Lett. 2013, 329, 109–117. [Google Scholar] [CrossRef]
- Brade, A.M.; Ng, S.; Brierley, J.; Kim, J.; Dinniwell, R.; Ringash, J.; Wong, R.R.; Cho, C.; Knox, J.; Dawson, L.A. Phase 1 trial of sorafenib and stereotactic body radiation therapy for hepatocellular carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2016, 94, 580–587. [Google Scholar] [CrossRef]
- Chen, J.C.-H.; Liu, S.-H.; Yen, T.-Y.; Dai, K.-Y.; Hwang, J.-J.; Chen, Y.-J. Sorafenib-Induced Radiation in-Field Skin (SIRIS) Reaction: Unexpected Complication in Elder Hepatocellular Carcinoma Patients Received Sorafenib and Concurrent Radiation Therapy. Int. J. Gerontol. 2019, 13, 90–93. [Google Scholar] [CrossRef]
- Chen, S.-W.; Lin, L.-C.; Kuo, Y.-C.; Liang, J.-A.; Kuo, C.-C.; Chiou, J.-F. Phase 2 study of combined sorafenib and radiation therapy in patients with advanced hepatocellular carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 1041–1047. [Google Scholar] [CrossRef]
- Cha, J.; Seong, J.; Lee, I.J.; Kim, J.W.; Han, K.-H. Feasibility of sorafenib combined with local radiotherapy in advanced hepatocellular carcinoma. Yonsei Med. J. 2013, 54, 1178. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; He, J.; Zhang, S.; Sun, J.; Zeng, M.; Zeng, Z. Simultaneous multitarget radiotherapy using helical tomotherapy and its combination with sorafenib for pulmonary metastases from hepatocellular carcinoma. Oncotarget 2016, 7, 48586. [Google Scholar] [CrossRef] [PubMed]
- Wada, Y.; Takami, Y.; Matsushima, H.; Tateishi, M.; Ryu, T.; Yoshitomi, M.; Matsumura, T.; Saitsu, H. The safety and efficacy of combination therapy of sorafenib and radiotherapy for advanced hepatocellular carcinoma: A retrospective study. Intern. Med. 2018, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, W.C.; Yoon, W.S.; Rim, C.H. Implications of Radiotherapy Utilization in South Korea from 2010 to 2019. J. Korean Med. Sci. 2021, 36, e117. [Google Scholar] [CrossRef]
- Rim, C.H.; Kim, H.J.; Seong, J. Clinical feasibility and efficacy of stereotactic body radiotherapy for hepatocellular carcinoma: A systematic review and meta-analysis of observational studies. Radiother. Oncol. 2019, 131, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Altman, D.G.; Liberati, A.; Tetzlaff, J. PRISMA statement. Epidemiology 2011, 22, 128. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Lefebvre, C.; Glanville, J.; Briscoe, S.; Littlewood, A.; Marshall, C.; Metzendorf, M.-I.; Noel-Storr, A.; Rader, T.; Shokraneh, F.; Thomas, J.; et al. Chapter 4: Searching for and selecting studies. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2; (updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 2 February 2021).
- Reeves, B.C.; Deeks, J.J.; Higgins, J.P.T.; Shea, B.; Tugwell, P.; Wells, G.A. Chapter 24: Including non-randomized studies on intervention effects. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2; (updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 2 February 2021).
- Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; University of Liverpool: Liverpool, UK, 2011. [Google Scholar]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Reeves, B.C.; Deeks, J.J.; Higgins, J.P.; Shea, B.; Tugwell, P.; Wells, G.A.; On Behalf of the Cochrane Non-Randomized Studies of Interventions Methods Group. Including non-randomized studies on intervention effects. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019; pp. 595–620. [Google Scholar]
- Cochran, W.G. The Combination of Estimates from Different Experiments. Biometrics 1954, 10, 101–129. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M.; Garner, P.; Donegan, S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin. Epidemiol. Glob. Health 2019, 7, 192–198. [Google Scholar] [CrossRef]
- Kang, J.; Zhao, X.; Nie, Q.; Zhang, L.; Zhu, Q.; Li, Q.; Wang, R. Efficacy of Stereotactic body radiation therapy with gamma-knife combined with hyperthermia and targeted drug sorafenib for the treatment of recurrent and metastatic hepatocellular carcinoma. Chin. J. Clin. Oncol. 2013, 40, 1236–1239. [Google Scholar]
- Chen, B.; Li, Y.; Wang, W.; Tan, Y.; Wang, S.; Zheng, X.; Chen, S.; Zhao, Y.; Jin, J.; Fang, H.; et al. Efficacy and Prognosis of Radiotherapy for Hepatocellular Carcinoma with Tumor Thrombosis in Main Portal Vein or/and Vena Cava. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, E215–E216. [Google Scholar] [CrossRef]
- Li, C.; Zhang, F.; Zhang, W.; Zhang, L.; Huang, Z.; Wu, P. Feasibility of 125 I brachytherapy combined with sorafenib treatment in patients with multiple lung metastases after liver transplantation for hepatocellular carcinoma. J. Cancer Res. Clin. Oncol. 2010, 136, 1633–1640. [Google Scholar] [CrossRef]
- Liu, C. Concurrent Sorafenib and Radiotherapy versus Radiotherapy Alone for Locally Advanced Hepatocellular Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, e580. [Google Scholar] [CrossRef]
- Zhang, Z.-H.; Liu, Q.-X.; Zhang, W.; Ma, J.-Q.; Wang, J.-H.; Luo, J.-J.; Liu, L.-X.; Yan, Z.-P. Combined endovascular brachytherapy, sorafenib, and transarterial chemobolization therapy for hepatocellular carcinoma patients with portal vein tumor thrombus. World J. Gastroenterol. 2017, 23, 7735. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhu, X.; Wang, H.; Dong, D.; Gao, S.; Zhu, X.; Wang, W. Safety and efficacy of transcatheter arterial chemoembolization plus radiotherapy combined with sorafenib in hepatocellular carcinoma showing macrovascular invasion. Front. Oncol. 2019, 9, 1065. [Google Scholar] [CrossRef]
- Cassim, S.; Raymond, V.A.; Dehbidi-Assadzadeh, L.; Lapierre, P.; Bilodeau, M. Metabolic reprogramming enables hepatocarcinoma cells to efficiently adapt and survive to a nutrient-restricted microenvironment. Cell Cycle 2018, 17, 903–916. [Google Scholar] [CrossRef]
- Yang, J.D.; Nakamura, I.; Roberts, L.R. The tumor microenvironment in hepatocellular carcinoma: Current status and therapeutic targets. Semin. Cancer Biol. 2011, 21, 35–43. [Google Scholar] [CrossRef]
- Lee, Y.H.; Tai, D.; Yip, C.; Choo, S.P.; Chew, V. Combinational Immunotherapy for Hepatocellular Carcinoma: Radiotherapy, Immune Checkpoint Blockade and Beyond. Front. Immunol. 2020, 11, 568759. [Google Scholar] [CrossRef]
- Brunetti, O.; Gnoni, A.; Licchetta, A.; Longo, V.; Calabrese, A.; Argentiero, A.; Delcuratolo, S.; Solimando, A.G.; Casadei-Gardini, A.; Silvestris, N. Predictive and Prognostic Factors in HCC Patients Treated with Sorafenib. Medicina 2019, 55, 707. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B.; et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Shin, I.-S.; Rim, C.H. Updating Perspectives on Meta-Analyses in the Field of Radiation Oncology. Medicina 2021, 57, 117. [Google Scholar] [CrossRef] [PubMed]
- Shrier, I.; Boivin, J.-F.; Steele, R.J.; Platt, R.W.; Furlan, A.; Kakuma, R.; Brophy, J.; Rossignol, M. Should meta-analyses of interventions include observational studies in addition to randomized controlled trials? A critical examination of underlying principles. Am. J. Epidemiol. 2007, 166, 1203–1209. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P. When are observational studies as credible as randomised trials? Lancet 2004, 363, 1728–1731. [Google Scholar] [CrossRef]
| Author | Publication, Year | Affiliation | Recruitment, Year | Study Design | Target Disease | No. of Patients * | CPC A (%) | Sorafenib | RT Modality | Dose | Other Combination Tx. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sun [20] | Oncotarget, 2016 | Fudan Univ, China | 2011–2014 | Comparative | Lung metastases | RS 23 R 22 | 98% | 400 mg bid | Tomotherapy | 50 Gy/5F or 10 F | |
| Wada [21] | Inters Med, 2018 | Kyushu Medical Center, Japan | 2009–2015 | Comparative | Advanced HCC (MVI, EHM) | RS 15 S 47 | 100% | starting 800 mg/day | 3DCRT | M50 (30–60) | |
| Zhao [40] | Frontier Oncol, 2019 | Peking University, China | 2015–2018 | Comparative | HCC with MVI | TRS 28 TR 35 | 100% | 400 mg bid | IMRT | 5054 Gy, conventional fraction | TACE |
| Kang [35] | Chin J Clin Oncol, 2013 | Navy General Hospital, China | 2007–2009 | Comparative | Recurrent and metastatic HCC | RSh 32 Rh 39 | 64.8% | 400 mg bid | Gammaknife SBRT | 36–50 Gy, 10–13 fractions | Hyperthermia |
| Liu [38] | ASTRO abstract, 2020 | Chang Gung Memorial hospital, Taiwan | 2007–2017 | Comparative | Locally advanced HCC | RS 73 R 73, propensity matched | |||||
| Zhang [39] | World J Gastroenterol, 2017 | Fudan Univ, China | 2009–2015 | Comparative | HCC MPVTT | TRS 37 TS 31 | 86.8% | 400 mg bid | BrachyTx (I125) | mean accumulated dose 62.9 +/−2.3 Gy | TACE |
| Brade [16] | Int J Radiat Biol Phys, 2016 | Princess Margaret Hospital, Canada | 2009–2012 | Single arm | HCC not amenable for other local Tx (PVT 63%) | 15 | 100 | 200 mg OD-400 mg BID | SBRT | 30–51 Gy/6 F | |
| Cha [19] | Yonsei Med J, 2013 | Yonsei Cancer Center, Korea | 2007–2011 | Single arm | Liver HCC | 13 | 85 | 400 mg bid (92%) 200 mg bid (8%) | 3D CRT (92%) | M4 45 (30–54) in 1.8–5 Gy/F | |
| Cha-2 [19] | EHM | 5 | 400 mg bid (60%) 200 mg bid (40%) | Tomotherapy | M50.4 (30–58.42) | ||||||
| Chen B [36] | ASTRO abstract, 2019 | Peking University, China | 2010–2016 | Single arm | HCC with MVI | 8 | 100 | IMRT | M50 (28–66) | ||
| Chen WS [18] | Int J Radiat Biol Phys, 2014 | 3 hospitals in Taiwan | 2010–2013 | Single arm | Locally advanced HCC | 40 | 100% | starting 400 mg bid | IMRT | 50–60 Gy in 2–2.5 Gy/F | |
| Li [37] | J Cancer Res Clin Oncol, 2010 | Sun Yat-Sen Univ, Taiwan | 2006–2009 | Single arm | Lung metastases | 8 | 400 mg bid | BrachyTx (I125) | Minimial peripheral dose 120–160 Gy |
| Author | RT target | No. of Patients * | Reliable Comparability | OS | Grade ≥3 Toxicity: GI | Hepatologic | Hematologic | Dermatologic |
|---|---|---|---|---|---|---|---|---|
| Sun | EHM (lung mets) | RS 23 R 22 | No | RS: 91.1% (1 y), 78.8% (2 y) R: 66.8% (1 y), 30.4% (2 y) (p = 0.007) | RS, R: 0% | RS, R: 0% | RS, R: 0% | RS, R: 0% |
| Wada | EHM or MVI (not intrahepatic) | RS 15 S 47 | Yes | RS: M31.2mo., 93.3% (1 y), 56.9% (2 y) S: M12.1mo., 47.9% (1 y), 12.4% (2 y); (p < 0.01) | RS: 6.7% S: 2.2% (p = NS) | RS: 0% S: 6.4% (p = 0.23) | RS: 0% S: 0% | RS: 0% S: 4.3% (p = 0.24) |
| Zhao | Liver HCC | TRS 28 TR 35 | Yes | TRS: M19 mo TR: M15.2 mo (p = 0.094) | TRS: 0% TR: 0% | TRS: 10.7% TR: 11.4% (p = 1.0) | TRS: 14.3% TR: 17.1% (p = 1.0) | TRS: 0% TR: 0% |
| Kang | EHM or Liver HCC | RSh 32 Rh 39 | Yes | RSh: 62.5% (1 y) Rh: 41.2% (1 y) (p = 0.048) | RSh, Rh: 0% | Not assessable | RSh, Rh: 0% | RSh, Rh: 0% |
| Liu | Liver HCC | RS 73 R 73, propensity matched | Yes | RS: M9.6 R: M9.9 (p = 0.544) | ||||
| Zhang | PVT only | TRS 37 TS 31 | Yes | TRS: 54.3% (1 y), 14.1% (2 y) TS: 0% (1 y) (p < 0.001) | TRS: 11.5% (diarrhea) TS: 3.6% (diarrhea) (p = NS) | Grade not assessed | TRS: 7.1% (HFS) TS: 3.6% (HFS) (p = NS) | |
| Brade | Liver HCC | 15 | NA | M26.3 mo, 62.5% (1 y) | 20% (GI bleeding and SBO) | 20% (LFT elevation) | 33.3% (thrombocytopenia) | 0% |
| Cha | Liver HCC | 13 | NA | M7.8 mo, 35% (1 y) | 5.6% (DU bleed) | 5.6% (LFT elevation) | 16.7% (thrombocytopenia) | 16.7% (HFS) |
| Cha-2 | EHM | 5 | NA | M15.7 mo, 60% (1 y) | ||||
| Chen B | Liver HCC | 8 | NA | |||||
| Chen WS | Liver HCC | 40 | NA | M14 mo, 52.5% (1 y), 32% (2 y) | 5% (diarrhea) | 22.50% | 0% | 7.5% (HFS) |
| Li | EHM (lung mets) | 8 | NA | M21 mo, 100% (1 y), 50% (2 y) | 0 | 0 | 0 | 0 |
| Subject Studies | No. of Studies | Patients Underwent Concurrent Treatment | Heterogeneity p | I2 | Pooled Rate (95% CI) | Subgroup Comparison p |
|---|---|---|---|---|---|---|
| Gastrointestinal toxicity | ||||||
| All studies | 9 | 217 | 0.444 | ~0% | 8.1% (4.8–13.5) | NA |
| Non–intrahepatic | 4 | 83 | 0.649 | ~0% | 8.6% (4.0–17.7) | 0.859 |
| Intrahepatic | 4 | 102 | 0.198 | 35.8% | 7.7% (2.8–19.5) | |
| Hepatologic toxicity | ||||||
| All studies | 7 | 148 | 0.259 | 22.4% | 12.9% (7.1–22.1) | NA |
| Non-intrahepatic | 3 | 46 | 0.882 | ~0% | 3.3% (0.7–14.8) | 0.041 |
| Intrahepatic | 4 | 102 | 0.366 | 5.4% | 17.1% (10.5–26.7) | |
| Hematologic toxicity | ||||||
| All studies | 8 | 180 | 0.045 | 51.3% | 9.1% (3.8–20.3) | NA |
| Non-intrahepatic | 3 | 46 | 0.882 | ~0% | 3.3% (0.7–14.8) | 0.078 |
| Intrahepatic | 4 | 102 | 0.08 | 55.6% | 16.0% (6.5–34.1) | |
| Dermatologic toxicity | ||||||
| All studies | 9 | 217 | 0.619 | ~0% | 6.8% (3.8–11.7) | NA |
| Non-intrahepatic | 4 | 83 | 0.839 | ~0% | 5.4% (2.1–13.3) | 0.485 |
| Intrahepatic | 4 | 102 | 0.321 | 14.3% | 8.3% (3.6–18.1) | |
| Overall survival | 6 | 455 | 0.002 | 73.5% | OR: 3.3 (1.3–8.59, p = 0.015) |
| Author | RT Target | No. of Patients * | Grade 4 or 5 Toxicities RILD | Qualitative Interpretation |
|---|---|---|---|---|
| Sun | EHM (lung mets) | RS 23 R 22 | 0% no RILD | All toxicities were G1 or 2 toxicities |
| Wada | EHM or MVI (not intrahepatic) | RS 15 S 47 | Grade 1 or 2 hematologic, dermatologic adverse events were higher in the RS group Overall grade ≥3 toxicity incidences are similar (20% vs. 19.2%, p = NS) | |
| Zhao | Liver HCC | TRS 28 TR 35 | 0% no RILD | All skin reactions and HFS were G1 or 2 toxicities, but these toxicities were of a higher grade with TRS (92.9% & 17.9% vs. 68.6% & 0%) |
| Kang | EHM or Liver HCC | RSh 32 Rh 39 | 0% RILD not assessed | No significant difference in G1 or 2 BM suppression, fatigue, nausea between arms Overall G3 complication 9.4% |
| Liu | Liver HCC | RS 73 R 73, propensity matched | No significant difference in RILD and GI bleeding | |
| Zhang | PVT only | TRS 37 TS 31 | 1 case of HTN G4 (3.2%) in TRS no lethal toxicity | Adding brachyTx. improved portal hypertension symptoms (new ascites, liver dysfunction), and OS (p < 0.001, 1 yr OS 54.3% vs. 0%) |
| Brade | Liver HCC | 15 | 1 case of liver enzyme change G4; 1 case of SBO G4 1 case of upper GI bleeding, rupture and death (6.7%) | |
| Cha | Liver or EHM | 18 | 1 case of G4 thrombocytopenia (5.6%) no RILD | |
| Chen B | Liver HCC | 8 | No lethal toxicity no RILD | |
| Chen WS | Liver HCC | 40 | 4 cases (11.1%) G4-5 hepatic toxicity RILD 15% (6 cases, 3 of which died without tumor progression) | |
| Li | EHM (lung mets) | 8 | No RILD no lethal toxicity |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rim, C.H.; Park, S.; Shin, I.-S.; Yoon, W.S. Is the Concurrent Use of Sorafenib and External Radiotherapy Feasible for Advanced Hepatocellular Carcinoma? A Meta-Analysis. Cancers 2021, 13, 2912. https://doi.org/10.3390/cancers13122912
Rim CH, Park S, Shin I-S, Yoon WS. Is the Concurrent Use of Sorafenib and External Radiotherapy Feasible for Advanced Hepatocellular Carcinoma? A Meta-Analysis. Cancers. 2021; 13(12):2912. https://doi.org/10.3390/cancers13122912
Chicago/Turabian StyleRim, Chai Hong, Sunmin Park, In-Soo Shin, and Won Sup Yoon. 2021. "Is the Concurrent Use of Sorafenib and External Radiotherapy Feasible for Advanced Hepatocellular Carcinoma? A Meta-Analysis" Cancers 13, no. 12: 2912. https://doi.org/10.3390/cancers13122912
APA StyleRim, C. H., Park, S., Shin, I.-S., & Yoon, W. S. (2021). Is the Concurrent Use of Sorafenib and External Radiotherapy Feasible for Advanced Hepatocellular Carcinoma? A Meta-Analysis. Cancers, 13(12), 2912. https://doi.org/10.3390/cancers13122912








