A Review of Clinical Practice Guidelines and Treatment Recommendations for Cancer Care in the COVID-19 Pandemic
Abstract
1. Introduction
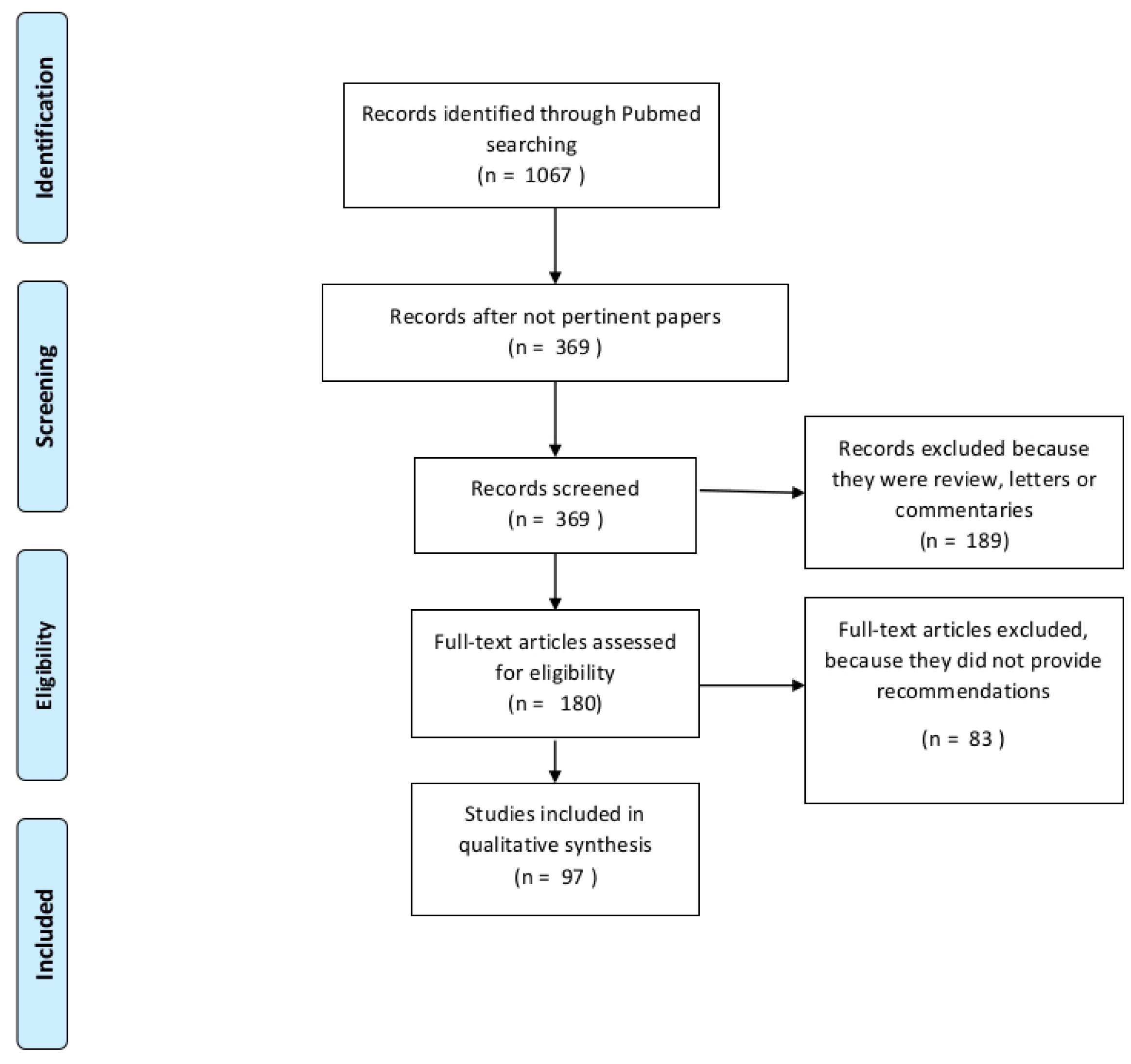
2. Results
2.1. Personal Recommendations or Single Authoritative Center Statements
2.2. Recommendations of Panels of Experts or Regional Cooperative Centers
2.3. Recommendations of Multicenter Cooperative Groups
2.4. Official Guidelines or Recommendations of Health Authorities
3. Materials and Methods
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lalani, A.-K.A.; Chi, K.N.; Heng, D.Y.; Kollmannsberger, C.K.; Sridhar, S.S.; Blais, N.; Canil, C.; Czaykowski, P.; Hotte, S.J.; Iqbal, N.; et al. Prioritizing systemic therapies for genitourinary malignancies: Canadian recommendations during the COVID-19 pandemic. Can. Urol. Assoc. J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Salari, A.; Shirkhoda, M. COVID-19 pandemic & head and neck cancer patients management: The role of virtual multidisciplinary team meetings. Oral Oncol. 2020, 105, 104693. [Google Scholar] [PubMed]
- Scotté, F.; Minvielle, E.; Mir, O.; André, F.; Barlesi, F.; Soria, J.-C. A patient reported outcome platform, a useful tool to improve monitoring and effective management of Covid-19-positive patients with cancer. Eur. J. Cancer 2020, 132, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Schrag, D.; Hershman, D.L.; Basch, E. Oncology practice during the COVID-19 pandemic. JAMA J. Am. Med. Assoc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, J.; He, J. Active and effective measures for the care of patients with cancer during the COVID-19 spread in China. JAMA Oncol. 2020. [Google Scholar] [CrossRef]
- Qadan, M.; Hong, T.S.; Tanabe, K.K.; Ryan, D.P.; Lillemoe, K.D. A multidisciplinary team approach for triage of elective cancer surgery at the massachusetts general hospital during the novel coronavirus COVID-19 outbreak. Ann. Surg. 2020. [Google Scholar] [CrossRef]
- Di Saverio, S.; Pata, F.; Gallo, G.; Carrano, F.; Scorza, A.; Sileri, P.; Smart, N.; Spinelli, A.; Pellino, G. Coronavirus pandemic and colorectal surgery: Practical advice based on the Italian experience. Color. Dis. 2020. [Google Scholar] [CrossRef]
- Cafarotti, S.; Patella, M.; Iosi, L.C.C. Lung cancer surgical management during the outbreak of COVID-19. J. Thorac. Oncol. 2020. [Google Scholar] [CrossRef]
- Kattan, J.; Kattan, C.; Assi, T. Do checkpoint inhibitors compromise the cancer patients’ immunity and increase the vulnerability to COVID-19 infection? Immunotherapy 2020, 19–22. [Google Scholar] [CrossRef]
- Zhao, Z.; Bai, H.; Duan, J.; Wang, J. Recommendations of individualized medical treatment and common adverse events management for lung cancer patients during the outbreak of COVID-19 epidemic. Thorac. Cancer 2020. [Google Scholar] [CrossRef]
- Banna, G.; Curioni-Fontecedro, A.; Friedlaender, A.; Addeo, A. How we treat patients with lung cancer during the SARS-CoV-2 pandemic: Primum non nocere. ESMO Open 2020, 5, e000765. [Google Scholar] [CrossRef]
- Braunstein, L.Z.; Gillespie, E.F.; Hong, L.; Xu, A.; Bakhoum, S.F.; Cuaron, J.; Mueller, B.; McCormick, B.; Cahlon, O.; Powell, S.; et al. Breast radiotherapy under COVID-19 pandemic resource constraints—Approaches to defer or shorten treatment from a comprehensive cancer center in the United States. Adv. Radiat Oncol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Mandato, V.D.; Aguzzoli, L. Management of ovarian cancer during the COVID-19 pandemic. Int. J. Gynaecol. Obstet. 2020, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Ansarin, M. Surgical management of head and neck tumours during the SARS-CoV (Covid-19) pandemic. Acta Otorhinolaryngol Ital. 2020, 1–3. [Google Scholar] [CrossRef]
- De Felice, F.; Polimeni, A.; Valentini, V. The impact of Coronavirus (COVID-19) on head and neck cancer patients’ care. Radiother. Oncol. 2020, 147, 84–85. [Google Scholar] [CrossRef]
- Jazieh, A.R.; Al Hadab, A.; Al Olayan, A.; Alhejazi, A.; Al Safi, F.; Al Qarni, A.; Farooqui, F.; Al Mutairi, N.; Alenazi, T.H. Managing oncology services during a major coronavirus outbreak: Lessons from the saudi arabia experience. JCO Glob. Oncol. 2020, 6, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Motlagh, A.; Yamrali, M.; Azghandi, S.; Azadeh, P.; Vaezi, M.; Ashrafi, F.; Zendehdel, K.; Mirzaei, H.; Basi, A.; Rakhsha, A.; et al. COVID19 prevention & care; a cancer specific guideline. Arch. Iran. Med. 2020, 23, 255–264. [Google Scholar] [CrossRef]
- Shankar, A.; Saini, D.; Roy, S.; Jarrahi, A.M.; Chakraborty, A.; Bharti, S.J.; Taghizadeh-Hesary, F. Cancer care delivery challenges amidst coronavirus disease -19 (covid-19) outbreak: Specific precautions for cancer patients and cancer care providers to prevent spread. Asian Pacific. J. Cancer Prev. 2020, 21, 569–573. [Google Scholar] [CrossRef]
- Wang, H.; Wang, S.; Yu, K. COVID-19 infection epidemic: The medical management strategies in Heilongjiang Province, China. Crit. Care 2020, 24, 10–13. [Google Scholar] [CrossRef]
- Pino, L.; Perez, C.; Cardona, A.; Triana, I. Cancer center recommendations to mitigate covid-19 impact in patients with cancer: Low-resource settings version. JCO Glob. Oncol. 2020, 6, 569–570. [Google Scholar] [CrossRef]
- Kutikov, A.; Weinberg, D.S.; Edelman, M.J.; Horwitz, E.M.; Uzzo, R.G.; Fisher, R.I. A war on two fronts: Cancer care in the time of COVID-19. Ann. Intern. Med. 2020, 172, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Cinar, P.; Kubal, T.; Freifeld, A.; Mishra, A.; Shulman, L.; Bachman, J.; Fonseca, R.; Uronis, H.; Klemanski, D.; Slusser, K.; et al. Safety at the time of the COVID-19 pandemic: How to keep our oncology patients and healthcare workers safe. J. Natl. Compr. Canc. Netw. 2020, 18, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lambertini, M.; Toss, A.; Passaro, A.; Criscitiello, C.; Cremolini, C.; Cardone, C.; Loupakis, F.; Viscardi, G.; Meattini, I.; Dieci, M.V.; et al. Cancer care during the spread of coronavirus disease 2019 (COVID-19) in Italy: Young oncologists’ perspective. ESMO Open 2020, 5, e000759. [Google Scholar] [CrossRef] [PubMed]
- Soran, A.; Gimbel, M.; Diego, E. Breast cancer diagnosis, treatment and follow-up during COVID-19 pandemic. Eur. J. Breast Heal. 2020, 16, 86–88. [Google Scholar] [CrossRef]
- Çakmak, G.K. Sars-CoV-2 (COVID-19) outbreak and breast cancer surgery in Turkey. Eur. J. Breast Health 2020, 16, 83–85. [Google Scholar] [CrossRef]
- Curigliano, G.; Cardoso, M.J.; Poortmans, P.; Gentilini, O.; Pravettoni, G.; Mazzocco, K.; Houssami, N.; Pagani, O.; Senkus, E.; Cardoso, F.; et al. Recommendations for triage, prioritization and treatment of breast cancer patients during the COVID-19 pandemic. Breast 2020, 52, 8–16. [Google Scholar] [CrossRef]
- Marijnen, C.; Peters, F.; Rödel, C.; Bujko, K.; Haustermans, K.; Fokas, E.; Glynne-Jones, R.; Valentini, V.; Spindler, K.-L.; Guren, M.; et al. International expert consensus statement regarding radiotherapy treatment options for rectal cancer during the COVID 19 pandemic. Radiother. Oncol. 2020. [Google Scholar] [CrossRef]
- Carneiro, A.; Wroclawski, M.L.; Nahar, B.; Soares, A.; Cardoso, A.P.; Kim, N.J.; Carvalho, F.T. Impact of the COVID-19 pandemic on the urologist’s clinical practice in Brazil: A management guideline proposal for low- and middle-income countries during the crisis period. Int. Braz. J. Urol. 2020, 46, 1–10. [Google Scholar] [CrossRef]
- Ficarra, V.; Novara, G.; Abrate, A.; Bartoletti, R.; Crestani, A.; De Nunzio, C.; Giannarini, G.; Gregori, A.; Liguori, G.; Mirone, V.; et al. Urology practice during COVID-19 pandemic. Minerva. Urol. Nefrol. 2020. [Google Scholar] [CrossRef]
- Ramirez, P.T.; Chiva, L.; Eriksson, A.G.Z.; Frumovitz, M.; Fagotti, A.; Martin, A.G.; Jhingran, A.; Pareja, R. COVID-19 global pandemic: Options for management of gynecologic cancers. Int. J. Gynecol. Cancer 2020. [Google Scholar] [CrossRef]
- Der Sarkissian, S.A.; Kim, L.; Veness, M.; Yiasemides, E.; Sebaratnam, D.F. Recommendations on dermatologic surgery during the COVID-19 pandemic. J. Am. Acad Dermatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Krengli, M.; Ferrara, E.; Mastroleo, F.; Brambilla, M.; Ricardi, U. Running a radiation oncology department at the time of coronavirus: An Italian experience. Adv. Radiat. Oncol. 2020. [Google Scholar] [CrossRef]
- Meattini, I.; Franco, P.; Belgioia, L.; Boldrini, L.; Botticella, A.; De Santis, M.C.; Marvaso, G.; Montesi, G.; Parisi, S.; Triggiani, L.; et al. Radiation therapy during the coronavirus disease 2019 (covid-19) pandemic in Italy: A view of the nation’s young oncologists. ESMO Open 2020, 5, 2019–2021. [Google Scholar] [CrossRef] [PubMed]
- Zaorsky, N.G.; Yu, J.B.; McBride, S.M.; Dess, R.T.; Jackson, W.C.; Mahal, B.A.; Chen, R.; Choudhury, A.; Henry, A.; Syndikus, I.; et al. Prostate cancer radiotherapy recommendations in response to COVID-19. Adv. Radiat. Oncol. 2020. [Google Scholar] [CrossRef]
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.; Hotte, S.J.; et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: An international collaborative group. Oncologist 2020, 2019, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Thureau, S.; Faivre, J.C.; Assaker, R.; Biver, E.; Confavreux, C.B.; Debiais, F.; Duterque-Coquillaud, M.; Giammarile, F.; Heymann, D.; Lecouvet, F.E.; et al. Adapting palliative radiation therapy for bone metastases during the Covid-19 pandemic: GEMO position paper. J. Bone Oncol. 2020. [Google Scholar] [CrossRef]
- Penel, N.; Bonvalot, S.; Minard, V.; Orbach, D.; Gouin, F.; Corradini, N.; Brahmi, M.; Marec-Berard, P.; Briand, S.; Gaspar, N.; et al. French Sarcoma Group proposals for management of sarcoma patients during COVID-19 outbreak. Bull. Cancer 2020. [Google Scholar] [CrossRef]
- Thoracic Surgery Outcomes Research Network, Inc. COVID-19 guidance for triage of operations for thoracic malignancies: A consensus statement from thoracic surgery outcomes research network. Ann. Thorac. Surg 2020. [Google Scholar] [CrossRef]
- Akladios, C.; Azais, H.; Ballester, M.; Bendifallah, S.; Bolze, P.-A.; Bourdel, N.; Bricou, A.; Canlorbe, G.; Carcopino, X.; Chauvet, P.; et al. Recommendations for the surgical management of gynecological cancers during the COVID-19 pandemic—FRANCOGYN group for the CNGOF. J. Gynecol. Obstet. Hum. Reprod. 2020, 101729. [Google Scholar] [CrossRef]
- Bartlett, D.L.; Oncology, F.T.S.O.S.; Howe, J.R.; Chang, G.; Crago, A.; Hogg, M.; Karakousis, G.; Levine, E.; Maker, A.; Mamounas, E.; et al. Management of cancer surgery cases during the COVID-19 pandemic: Considerations. Ann. Surg. Oncol. 2020, 27, 1–4. [Google Scholar] [CrossRef]
- Bitar, N.; Kattan, J.; Kourie, H.R.; Mukherji, D.; el Saghir, N. The Lebanese Society of Medical Oncology (LSMO) statement on the care of patients with cancer during the COVID-19 pandemic. Future Oncol. 2020, 16, 615–617. [Google Scholar] [CrossRef] [PubMed]
- Coles, C.; Aristei, C.; Bliss, J.; Boersma, L.; Brunt, A.; Chatterjee, S.; Hanna, G.; Jagsi, R.; Person, O.K.; Kirby, A.; et al. International guidelines on radiation therapy for breast cancer during the COVID-19 Pandemic. Clin. Oncol. 2020, 32, 279–281. [Google Scholar] [CrossRef] [PubMed]
- Fakhry, N.; Schultz, P.; Morinière, S.; Breuskin, I.; Bozec, A.; Vergez, S.; De Garbory, L.; Hartl, D.; Temam, S.; Lescanne, E.; et al. French consensus on management of head and neck cancer surgery during COVID-19 pandemic. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2020, 8–9. [Google Scholar] [CrossRef] [PubMed]
- Kimmig, R.; Verheijen, R.H.M.; Rudnicki, M. Robot assisted surgery during the COVID-19 pandemic, especially for gynecological cancer: A statement of the Society of European Robotic Gynaecological Surgery (SERGS). J. Gynecol. Oncol. 2020, 31, 1–7. [Google Scholar] [CrossRef]
- Thomson, D.J.; Palma, D.; Guckenberger, M.; Balermpas, P.; Beitler, J.J.; Blanchard, P.; Brizel, D.; Budach, W.; Caudell, J.; Corry, J.; et al. Practice recommendations for risk-adapted head and neck cancer radiation therapy during the COVID-19 pandemic: An ASTRO-ESTRO consensus statement. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 618–627. [Google Scholar] [CrossRef]
- Yahalom, J.; Dabaja, B.S.; Ricardi, U.; Ng, A.; Mikhaeel, N.G.; Vogelius, I.R.; Illidge, T.; Qi, S.; Wirth, A.; Specht, L. ILROG Emergency Guidelines for Radiation Therapy of Hematological Malignancies During the COVID-19 Pandemic. Blood 2020. [Google Scholar] [CrossRef]
- You, B.; Ravaud, A.; Canivet, A.; Ganem, G.; Giraud, P.; Guimbaud, R.; Kaluzinski, L.; Krakowski, I.; Mayeur, D.; Grellety, T.; et al. The official French guidelines to protect patients with cancer against SARS-CoV-2 infection. Lancet Oncol. 2020, 2045, 20–21. [Google Scholar] [CrossRef]
- Mohile, N.; Blakeley, O.J.; Gatson, N.T.N.; Hottinger, A.F.; Lassman, A.B.; Ney, E.D.; Olar, A.; Schiff, D.; Shih, A.H.; Strowd, R.; et al. Urgent considerations for the neuro-oncologic treatment of patients with gliomas during the COVID-19 pandemic. Neuro Oncol. 2020. [Google Scholar] [CrossRef]
- Ribal, M.J.; Cornford, P.; Briganti, A.; Knoll, T.; Gravas, S.; Babjuk, M.; Harding, C.; Breda, A.; Bex, A.; Rassweiler, J.J.; et al. EAU section offices and the EAU guidelines panels. European association of urology guidelines office rapid reaction group: An organisation-wide collaborative effort to adapt the european association of urology guidelines recommendations to the coronavirus disease 2019. Era. Eur. Urol. 2020, 78, 21–28. [Google Scholar] [CrossRef]
- Von Lilienfeld-Toal, M.; Vehreschild, J.J.; Cornely, O.; Pagano, L.; Compagno, F.; Hirsch, H.H.; Pagliuca, A. EHA Infectious Disease Scientific Working Group. Frequently asked questions regarding SARS-CoV-2 in cancer patients-recommendations for clinicians caring for patients with malignant diseases. Leukemia 2020. [Google Scholar] [CrossRef]
- Chan, A.; Ashbury, F.; Fitch, M.I.; Koczwara, B.; Chan, R.J.; MASCC Survivorship Study Group. Cancer survivorship care during COVID-19-perspectives and recommendations from the MASCC survivorship study group. Support Care Cancer 2020, 28, 3485–3488. [Google Scholar] [CrossRef] [PubMed]
- Ueda, M.; Martins, R.; Hendrie, P.C.; McDonnell, T.; Crews, J.R.; Wong, T.L.; McCreery, B.; Jagels, B.; Crane, A.; Byrd, D.R.; et al. Managing cancer care during the COVID-19 pandemic: Agility and collaboration toward a common goal. J. Natl. Compr. Canc. Netw. 2020, 18, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, L.P.; Sanabria, A.; Ridge, J.A.; Ng, W.T.; De Bree, R.; Rinaldo, A.; Takes, R.P.; Mäkitie, A.A.; Carvalho, A.L.; Bradford, C.R.; et al. COVID-19 pandemic: Effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck 2020. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.H.M.S.; Vukkadala, N.; Tsang, R.K.Y.; Sunwoo, J.B.; Holsinger, F.C.; Chan, J.Y.K.; Damrose, E.J.; Kearney, A.; Starmer, H.M. Managing head and neck cancer patients with tracheostomy or laryngectomy during the COVID-19 pandemic. Head Neck 2020, 42, 1209–1219. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, Y.; Wang, X.; Zhang, D.; Diao, D.; Chandramohan, K.; Booth, C.M. Recommendations for surgery during the novel coronavirus (COVID-19) epidemic. Indian J. Surg. 2020, 1–5. [Google Scholar] [CrossRef]
- Ardura, M.; Hartley, D.; Dandoy, C.; Lehmann, L.; Jaglowski, S.; Auletta, J.J. Transplant-Associated Learning Network Team (TALNT). Addressing the impact of the Coronavirus Disease 2019 (COVID-19) pandemic on hematopoietic cell transplantation: Learning networks as a means for sharing best practices. Biol. Blood Marrow Transpl. 2020. [Google Scholar] [CrossRef]
- Davis, A.P.; Boyer, M.; Lee, J.H.; Kao, S. COVID-19: The use of immunotherapy in metastatic lung cancer. Immunotherapy 2020. [Google Scholar] [CrossRef]
- Dietz, J.R.; Moran, M.S.; Isakoff, S.J.; Kurtzman, S.H.; Willey, S.C.; Burstein, H.J.; Bleicher, R.J.; Lyons, J.A.; Sarantou, T.; Baron, P.L.; et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. The COVID-19 pandemic breast cancer consortium. Breast Cancer Res. Treat 2020. [Google Scholar] [CrossRef]
- Finley, C.; Prashad, A.; Camuso, N.; Daly, C.; Aprikian, A.; Ball, C.G.; Bentley, J.; Charest, D.; Fata, P.; Helyer, L.; et al. Guidance for management of cancer surgery during the COVID-19 pandemic. Can. J. Surg. 2020, 63, S2–S4. [Google Scholar] [CrossRef]
- Gentileschi, S.; Caretto, A.A.; Tagliaferri, L.; Salgarello, M.; Peris, K. Skin cancer plastic surgery during the COVID-19 pandemic. Eur. J. Surg. Oncol. 2020. [Google Scholar] [CrossRef]
- Glehen, O.; Kepenekian, V.; Bouché, O.; Gladieff, L.; Honore, C.; Abba, J.; Abboud, K.; Arvieux, C.; Bakrin, N.; Delhorme, J.-B.; et al. Treatment of primary and metastatic peritoneal tumors in the Covid-19 pandemic. Proposals for prioritization from the RENAPE and BIG-RENAPE groups. J. Visc. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Maniakas, A.; Jozaghi, Y.; Zafereo, M.E.; Sturgis, E.M.; Su, S.Y.; Gillenwater, A.M.; Gidley, P.W.; Lewis, C.M.; Diaz, E.; MD Anderson Head and Neck Surgery Treatment Guidelines Consortium; et al. Head and neck surgical oncology in the time of a pandemic: Subsite-specific triage guidelines during the COVID-19 pandemic. Head Neck 2020. [Google Scholar] [CrossRef]
- Koffman, B.; Mato, A.R.; Byrd, J.C.; Danilov, A.; Hedrick, B.; Ujjani, C.; Roeker, L.; Stephens, D.M.; Davids, M.S.; Pagel, J.M.; et al. Management of CLL patients early in the COVID-19 pandemic: An international survey of CLL experts. Am. J. Hematol. 2020. [Google Scholar] [CrossRef]
- Lou, E.; Beg, S.; Bergsland, E.; Eng, C.; Khorana, A.; Kopetz, S.; Lubner, S.; Saltz, L.; Shankaran, V.; Zafar, S.Y. Modifying practices in GI oncology in the face of COVID-19: Recommendations from expert oncologists on minimizing patient risk. JCO Oncol. Pract. 2020. [Google Scholar] [CrossRef]
- Monk, B.J.; Coleman, R.L.; Moore, K.N.; Herzog, T.J.; Secord, A.A.; Matulonis, U.A.; Slomovitz, B.M.; Guntupalli, S.R.; O’Malley, D.M. COVID-19 and ovarian cancer: Exploring alternatives to intravenous (IV) therapies. Gynecol. Oncol. 2020. [Google Scholar] [CrossRef]
- O’Cathail, S.; Gilbert, D.; Sebag-Montefiore, D.; Muirhead, R. Challenges and consequences of COVID-19 in the management of anorectal cancer: Coming together through social distancing. Clin. Oncol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Patnaik, M.; Lasho, T.; Padron, E.; McCullough, K.; Al-Kali, A.; Tefferi, A.; Zeidan, A.M.; Gangat, N.; Savona, M.; Steensma, D.P.; et al. Special considerations in the management of patients with myelodysplastic syndrome/myeloproliferative neoplasm overlap syndromes during the SARS-CoV-2 pandemic. Am. J. Hematol. 2020. [Google Scholar] [CrossRef]
- Pothuri, B.; Secord, A.A.; Armstrong, D.K.; Chan, J.; Fader, A.N.; Huh, W.; Kesterson, J.; Liu, J.F.; Moore, K.; Westin, S.N.; et al. Anti-cancer therapy and clinical trial considerations for gynecologic oncology patients during the COVID-19 pandemic crisis. Gynecol. Oncol. 2020. [Google Scholar] [CrossRef]
- Tagliaferri, L.; Di Stefani, A.; Schinzari, G.; Fionda, B.; Rossi, E.; Del Regno, L.; Gentileschi, S.; Federico, F.; Valentini, V.; Tortora, G. Skin cancer triage and management during COVID-19 pandemic. J. Eur. Acad. Dermatol. Venereol. 2020. [Google Scholar] [CrossRef]
- Tasoulis, M.K.; Roche, N.; MacNeill, F. Rationalizing breast cancer surgery during the COVID-19 pandemic. Eur. J. Surg. Oncol. 2020. [Google Scholar] [CrossRef]
- Teoh, J.Y.C.; Roupret, M.; Shariat, S.F.; Herrmann, T. Intravesical therapy for bladder cancer in the pandemic of Covid-19. World J. Urol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Troost, E.G.; Nestle, U.; Putora, P.M.; Bussink, J. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus statement. Radiother. Oncol. 2020. [Google Scholar] [CrossRef]
- Werner, M.T.; Carey, R.M.; Albergotti, W.G.; Lukens, J.N.; Brody, R.M. Impact of the COVID-19 pandemic on the management of head and neck malignancies. Otolaryngol. Head Neck Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.; Noel, C.W.; Forner, D.; Zhang, Z.; Higgins, K.M.; Enepekides, D.J.; Lee, J.M.; Witterick, I.J.; Kim, J.J.; Waldron, J.N.; et al. Considerations for head and neck oncology practices during the coronavirus disease 2019 (COVID-19) pandemic: Wuhan and Toronto experience. Head Neck 2020. [Google Scholar] [CrossRef] [PubMed]
- Bergsland, E.K.; Halperin, D.M.; Dillon, J.S.; Dasari, N.A.; Kunz, P.L.; Soares, H.P.; Pryma, D.; Bodei, L.; Hope, T.; Soulen, M.C.; et al. North American neuroendocrine tumor society guide for neuroendocrine tumor patient health care providers during COVID-19. Pancreas 2020, 49, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Terpos, E.; Engelhardt, M.; Cook, G.; Gay, F.; Mateos, M.V.; Ntanasis-Stathopoulos, I.; van de Donk, N.W.C.J.; Avet-Loiseau, H.; Hajek, R.; Vangsted, A.J.; et al. Management of patients with multiple myeloma in the era of COVID-19 pandemic: A consensus paper from the European Myeloma Network (EMN). Leukemia 2020, 22, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.K.; Lee, M.K.; Baker, J.L.; Attai, D.J.; DiNome, M.L. Taking a second look at neoadjuvant endocrine therapy for the treatment of early stage estrogen receptor positive breast cancer during the COVID-19 outbreak. Ann. Surg. 2020. [Google Scholar] [CrossRef]
- Nguyen, N.P.; Vinh-Hung, V.; Baumert, B.G.; Zamagni, A.; Arenas, M.; Motta, M.; Lara, P.C.; Myint, A.S.; Bonet, M.; Popescu, T.; et al. Older cancer patients during the COVID-19 epidemic: Practice proposal of the international geriatric radiotherapy group. Cancers 2020, 12, 1287. [Google Scholar] [CrossRef]
- Li, W.-M.; Wang, D.; Guo, J.; Yuan, G.; Yang, Z.; Gale, R.P.; You, Y.; Chen, Z.; Chen, S.; Hubei Anti-Cancer Association; et al. COVID-19 in persons with chronic myeloid leukaemia. Leukemia 2020, 34, 1799–1804. [Google Scholar] [CrossRef]
- Whisenant, J.G.; Trama, A.; Torri, V.; de Toma, A.; Viscardi, G.; Cortellini, A.; Micheilin, O.; Barlesi, F.; Dingemans, A.-M.C.; van Meerbeeck, J.; et al. TERAVOLT: Thoracic Cancers International COVID-19 Collaboration. Cancer Cell 2020, 37, 742–745. [Google Scholar] [CrossRef]
- Sharma, R.; Pinato, D.J. Management of hepatocellular cancer in the time of SARS-CoV-2. Liver Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, A.-M.C.; Soo, R.A.; Jazieh, A.R.; Rice, S.J.; Kim, Y.T.; Teo, L.L.; Warren, G.W.; Xiao, S.-Y.; Smit, E.F.; Aerts, J.G.; et al. Treatment guidance for patients with lung cancer during the coronavirus 2019 pandemic. J. Thorac. Oncol. 2020, 15, 1119–1136. [Google Scholar] [CrossRef] [PubMed]
- Viale, G.; Licata, L.; Sica, L.; Zambelli, S.; Zucchinelli, P.; Rognone, A.; Aldrighetti, D.; Di Micco, R.; Zuber, V.; Pasetti, M.; et al. Personalized risk-benefit ratio adaptation of breast cancer care at the epicenter of COVID-19 outbreak. Oncologist 2020. [Google Scholar] [CrossRef] [PubMed]
- Di Fiore, F.; Thésaurus National de Cancérologie Digestive (TNCD); Société Nationale Française de Gastroentérologie (SNFGE); Fédération Francophone de Cancérologie Digestive (FFCD); Groupe Coopérateur multidisciplinaire en Oncologie (GERCOR); Fédération Nationale des Centres de Lutte Contre le Cancer (UNICANCER); Société Française de Chirurgie Digestive (SFCD); Société Française d’Endoscopie Digestive (SFED); Société Française de Radiothérapie Oncologique (SFRO) and Société Française de Radiologie (SFR); Association Chirurgie Hepato-Biliaire et Transplantation (ACHBT); et al. COVID-19 epidemic: Proposed alternatives in the management of digestive cancers: A French intergroup clinical point of view (SNFGE, FFCD, GERCOR, UNICANCER, SFCD, SFED, SFRO, SFR). Dig. Liver Dis. 2020, 52, 597–603. [Google Scholar] [CrossRef]
- Hungria, V.; Garnica, M.; Crusoé, E.D.Q.; Filho, R.J.P.D.M.; Martinez, G.; Bittencourt, R.; de Farias, D.L.C.; Braga, W.M.; Neto, J.V.P.; Ribeiro, G.N.; et al. Managing patients with multiple myeloma during the COVID-19 pandemic: Recommendations from an expert panel—ABHH monoclonal gammopathies committe. Hematol. Transfus. Cell Ther. 2020. [Google Scholar] [CrossRef]
- Desideri, I.; Pilleron, S.; Battisti, N.M.L.; Gomes, F.; De Glas, N.; Neuendorff, N.R.; Liposits, G.; Paredero-Pérez, I.; Lok, W.C.W.; Loh, K.P.; et al. Caring for older patients with cancer during the COVID-19 pandemic: A young international society of geriatric oncology (SIOG) global perspective. J. Geriatr. Oncol. 2020. [Google Scholar] [CrossRef]
- Geskin, L.J.; Trager, M.H.; Aasi, S.Z.; Bickers, D.R.; Carvajal, R.D.; Nghiem, P.; Taback, B.; Zeitouni, N.C.; Samie, F.H. Perspectives on the recommendations for skin cancer management during the COVID-19 pandemic. J. Am. Acad. Dermatol. 2020, 83, 295–296. [Google Scholar] [CrossRef]
- Valenza, F.; Papagni, G.; Marchianò, A.; Daidone, M.G.; De’Braud, F.; Colombo, M.P.; Frignani, A.; Galmozzi, G.; Ladisa, V.; Pruneri, G.; et al. Response of a comprehensive cancer center to the COVID-19 pandemic: The experience of the fondazione IRCCS-istituto nazionale dei tumori di milano. Tumori 2020. [Google Scholar] [CrossRef]
- Vecchione, L.; Stintzing, S.; Pentheroudakis, G.; Douillard, J.-Y.; Lordick, F. ESMO management and treatment adapted recommendations in the COVID-19 era: Colorectal cancer. ESMO Open 2020, 5 (Suppl. 3), e000826. [Google Scholar] [CrossRef]
- Spolverato, G.; Capelli, G.; Restivo, A.; Bao, Q.R.; Pucciarelli, S.; Pawlik, T.M.; Gronchi, A. The management of surgical patients during the coronavirus disease 2019 (COVID-19) pandemic. Surgery 2020, 168, 4–10. [Google Scholar] [CrossRef]
- De Azambuja, E.; Trapani, D.; Loibl, S.; Delaloge, S.; Senkus, E.; Criscitiello, C.; Poortman, P.; Gnant, M.; di Cosimo, S.; Cortes, J.; et al. ESMO management and treatment adapted recommendations in the COVID-19 era: Breast cancer. ESMO Open 2020, 5 (Suppl. 3), e000793. [Google Scholar] [CrossRef] [PubMed]
- Catanese, S.; Pentheroudakis, G.; Douillard, J.Y.; Lordick, F. ESMO management and treatment adapted recommendations in the COVID-19 era: Pancreatic cancer. ESMO Open 2020, 5 (Suppl. 3), e000804. [Google Scholar] [CrossRef] [PubMed]
- Jozaghi, Y.; Zafereo, M.E.; Perrier, N.D.; Wang, J.R.; Grubbs, E.; Gross, N.D.; Fisher, S.; Sturgis, E.M.; Goepfert, R.P.; Lai, S.Y.; et al. Endocrine surgery in the Coronavirus disease 2019 pandemic: Surgical triage guidelines. Head Neck 2020, 42, 1325–1328. [Google Scholar] [CrossRef] [PubMed]
- Jereczek-Fossa, B.A.; Palazzi, M.F.; Soatti, C.P.; Cazzaniga, L.F.; Ivaldi, G.B.; Pepa, M.; Amadori, M.; Antognoni, P.; Arcangeli, S.; CODRAL (Board of Directors of Radiation Oncology Departments in Lombardy) Network. COVID-19 outbreak and cancer radiotherapy disruption in lombardy, Northern Italy. Clin. Oncol. 2020, 32, e160–e161. [Google Scholar] [CrossRef] [PubMed]
- Van de Haar, J.; Hoes, L.R.; Coles, C.E.; Seamon, K.; Fröhling, S.; Jäger, D.; Valenza, F.; De Braud, F.; de Petris, L.; Bergh, J.; et al. Caring for patients with cancer in the COVID-19 era. Nat. Med. 2020, 26, 665–671. [Google Scholar] [CrossRef]
- Yerramilli, D.; Xu, A.J.; Gillespie, E.F.; Shepherd, A.F.; Beal, K.; Gomez, D.; Yamada, J.; Tsai, C.J.; Yang, T.J. Palliative radiotherapy for oncologic emergencies in the setting of COVID-19: Approaches to balancing risks and benefits. Adv. Radiat. Oncol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Al-Rashdan, A.; Roumeliotis, M.; Quirk, S.; Grendarova, P.; Phan, T.; Cao, J.; Logie, N.; Smith, W.; Barbera, L. Adapting radiation therapy treatments for patients with breast cancer during the COVID-19 pandemic: Hypo-fractionation and accelerated partial breast irradiation to address world health organization recommendations. Adv. Radiat. Oncol. 2020. [Google Scholar] [CrossRef]
| Author/Year | Journal | Country | Type of Study | Disease | Synthesis of Main Recommendations |
|---|---|---|---|---|---|
| Ansarin/2020 | Acta Otorhinolaryngol Ital | Italy | Personal view or multi-authors review | H&N | Recommendations about surgery and compromise between the necessary cancer treatments and the risk of infection |
| Banna/2020 | ESMO Open | Italy and Switzerland | Personal view or multi-authors review | Lung | A decisional tool to support oncologists and physicians in treatment for patients with lung cancer: primum non nocere |
| Cafarotti/2020 | J Thorac Oncol | Switzerland | Personal view or multi-authors review | Lung | An algorithm of care to balance the risk of dying from cancer or from potentially fatal infection |
| Di Saverio/2020 | Colorectal Dis | Italy | Personal view or multi-authors review | Colorectal | Management of patients needing surgery to mitigate some risks and reduce exposure to other patients |
| Falandry/2020 | J Geriatr Oncol | France | Personal view or multi-authors review | Various | Challenges with the management of older patients with cancer |
| Kattan/2020 | Immunotherapy | France and Lebanon | Personal view or multi-authors review | Various | A careful selection of the most efficacious anti-tumor weaponry with the lower risk of weaning the patients’ immune system |
| Mandato/2020 | Obstet Gynecol | Italy | Personal view or multi-authors review | Ovarian | Finding new effective strategies in cancer care is mandatory (allocate resources and real-life treatment) |
| Schrag/2020 | JAMA | US | Personal view or multi-authors review | Various | Planning for resuming cancer treatment and screening to mitigate harms; changes will transform cancer treatment |
| Scotté/2020 | Eur J Cancer | France | Personal view or multi-authors review | Various | Use of telemedicine for monitoring and optimizing referral of Covid-19-positive patients with cancer (CAPRI programme) |
| Zhao/2020 | Thorac Cancer | China | Personal view or multi-authors review | Lung | Recommendations and suggestions of individualized treatment strategies and management of common adverse events for patients with lung cancer |
| Braunstein/2020 | Adv Radiat Oncol | US | Single authoritative center view | Breast | The parsimonious application of breast radiotherapy without compromising long term oncologic outcomes |
| Davis/2020 | Immunotherapy | Australia | Single authoritative center view | Immunotherapy | Suggestions about immunotherapy use during pandemic |
| De Felice/2020 | Radiother Oncol | Italy | Single authoritative center view | H&N | To offer adequate individualized treatment recommendations based on both the epidemic situation and the patient’s own condition |
| Gentileschi/2020 | Eur J Surg Oncol | Italy | Single authoritative center view | Skin | Skin cancer management |
| Kligerman/2020 | Head Neck | US and Hong Kong | Single authoritative center view | H&N | To help minimize the risk of aerosolization and SARS-CoV-2 exposures in head and neck cancer patients with tracheostomy and TL |
| Qadan/2020 | Ann Surg | US | Single authoritative center view | Various | A multidisciplinary team approach for triage of elective cancer surgery |
| Salari/2020 | Oral Oncol | Iran | Single authoritative center view | H&N | The role of virtual multidisciplinary team meetings |
| Tagliaferri/2020 | J Eur Acad Dermatol Venereol | Italy | Single authoritative center view | Skin | Management of skin cancers during COVID-19 era |
| Tasoulis/2020 | Eur J Surg Oncol | UK | Single authoritative center view | Breast | Position of The Royal Marsden regarding breast cancer surgery |
| Wang/2020 | JAMA Oncol | China | Single authoritative center view | Various | More attention should be paid to patients with cancer as a special population |
| Thompson/2020 | Ann Surg | USA | Single authoritative center view | Breast | Revised indication of neoadjuvant endocrine therapy for the treatment of early stage estrogen receptor positive breast cancer |
| Li/2020 | Leukemia | China | Single authoritative center view | Chronic myeloid leukemia | Questionnaires of subjects with chronic myeloid leukemia during COVID-19 pandemic |
| Sharma/2020 | Liver Int | UK | Single authoritative center view | Hepatocellular Cancer (HCC) | Recommendations for the treatment of HCC during COVID-19 pandemic |
| Yerramilli/2020 | Adv Radiat Oncol | USA | Single authoritative center view | Various | Use of hypofractionated radiation therapy for patients requiring palliation for oncologic emergencies |
| Valenza/2020 | Tumori | Italy | Single authoritative center view | Various | Screening of patients accessing to a Comprehensive Cancer Center with real-time PCR of nose-throat swabs |
| Viale/2020 | Oncologist | Italy | Single authoritative center view | Breast | Personalized strategies for optimal breast cancer management |
| Cakmak/2020 | Eur J Breast Health | Turkey | Panel of experts or regional recommendations | Breast | Recommendations about timing of surgery of breast cancer according to biology and risk |
| Carneiro/2020 | Int Braz J Urol | Brazil | Panel of experts or regional recommendations | Urologic | Suggestions and recommendations for the management of urological conditions in times of COVID-19 crisis in Brazil and other low- and middle-income countries |
| Cinar/2020 | J Natl Compr Canc Netw | US | Panel of experts or regional recommendations | Various | Strategies to mitigate transmission of COVID-19 in an effort to reduce morbidity and mortality associated with the disease for patients with cancer and for the healthcare workers |
| Curigliano/2020 | Breast | International | Panel of experts or regional recommendations | Breast | Advise on how to triage, prioritize, and organize diagnostic procedures, surgical, radiation, and medical treatments in breast cancer |
| Dietz/2020 | Breast Cancer Res Treat | US | Panel of experts or regional recommendations | Breast | Recommendations for prioritization, treatment and triage of breast cancer patients during the COVID-19 pandemic |
| Ficarra/2020 | Minerva Urol Nefrol | Italy | Panel of experts or regional recommendations | Urologic | Strategies for the reorganization of urological routine practice and a set of recommendations to facilitate the process of rescheduling surgical activity |
| Finley/2020 | Can J Surg | Canada | Panel of experts or regional recommendations | Various | Recommendations about cancer surgery by Canadian surgeons |
| Head and Neck Surgery Treatment Guidelines Consortium/2020 | Head Neck | US | Panel of experts or regional recommendations | H&N | Head and Neck cancer treatment according to site and stage of disease is presented |
| Jazieh/2020 | JCO Glob Oncol | Saudi Arabia | Panel of experts or regional recommendations | Various | It is important to have a robust mechanism to prioritize patients to ensure the provision of timely care while preventing further harm by guiding staff to provide care in safety |
| Koffman/2020 | Am J Hematol | US | Panel of experts or regional recommendations | CLL | Recommendation about CLL treatment by a CLL panel of experts |
| Kowalski/2020 | Head Neck | International | Panel of experts or regional recommendations | H&N | Procedures essential to maintain safety of otolaryngologists and maxillofacial surgeons exposed to the greatest risk of infection |
| Krengli/2020 | Adv Radiat Oncol | Italy | Panel of experts or regional recommendations | Various | To adopt preventive measures and recommendations for patients, professionals, and clinical operations to minimize the risk of infection while safely treating cancer patients |
| Kutikov/2020 | Ann Intern Med | US | Panel of experts or regional recommendations | Various | Risks must be balanced carefully, public health strategies implemented thoroughly, and resources utilized wisely |
| Lalani/2020 | Can Urol Assoc J | Canada | Panel of experts or regional recommendations | Genitourinary | Recommendations to assist in prioritizing systemic therapies for patients with genitourinary cancers |
| Lambertini/2020 | ESMO Open | Italy | Panel of experts or regional recommendations | Various | Practical suggestions on how to implement cancer care during the COVID-19 outbreak |
| Liu/2020 | Indian J Surg | International | Panel of experts or regional recommendations | Various | An approach for the management of surgical patients in the context of the COVID-19 pandemic |
| Lou/2020 | JCO Oncol Pract | US | Panel of experts or regional recommendations | Gastrointestinal | GI cancer treatment with the aim of minimizing patient risk during pandemic |
| Marijnen/2020 | Radiother Oncol | International | Panel of experts or regional recommendations | Rectal | Radiotherapy treatment options for rectal cancer during the COVID-19 pandemic |
| Meattini/2020 | ESMO Open | Italy | Panel of experts or regional recommendations | Various | Recommendations in order to keep cancer care as safe as possible for both patients and healthcare providers |
| Mohile/2020 | Neuro Oncol | International | Panel of experts or regional recommendations | Glioma | To highlight opportunities to maximize the benefit and minimize the risk of glioma management during this pandemic and potentially, in the future |
| Monk/2020 | Gynecol Oncol | US | Panel of experts or regional recommendations | Ovarian | Recommendation about alternative routes of therapy for ovarian cancer |
| Motlagh/2020 | Arch Iran Med | Iran | Panel of experts or regional recommendations | Various | Two limit the exposure of cancer patients to medical environments, and modify the treatment modalities to reduce the probability of myelosuppression (delaying diagnostic and therapeutic services, shortening the treatment course, or prolonging the interval between treatment courses) |
| O’Cathail/2020 | Clin Oncol | UK | Panel of experts or regional recommendations | Anorectal | Management of anorectal cancers provided by experts of UK |
| Patnaik/2020 | Am J Hematology | International | Panel of experts or regional recommendations | Myelodisplastic/myeloproliferative syndrome | Recommendation about treatment by a panel of experts |
| Pino/2020 | JCO Glob Oncol | Colombia | Panel of experts or regional recommendations | Various | Prioritization of adequate pathways for patients in low- and middle-income settings is critical |
| Pothuri/2020 | Gynecol Oncol | US | Panel of experts or regional recommendations | Gynecologic | An expert panel convened to develop initial consensus guidelines regarding anti-neoplastic therapy during the COVID-19 pandemic with respect to gynecologic cancer care and clinical trials |
| Ramirez/2020 | Int J Gynecol Cancer | International | Panel of experts or regional recommendations | Gynecologic | To share options in both the management and surveillance of patients diagnosed with gynecologic cancers during this time of global crisis |
| Sarkissian/2020 | J Am Acad Dermatol | US | Panel of experts or regional recommendations | Dermatologic | Recommendations regarding dermatological surgery during COVID-19 pandemic |
| Shankar/2020 | Asian Pac J Cancer Prev | International | Panel of experts or regional recommendations | Various | Specific precautions for cancer patients and cancer care providers to prevent spread |
| Soran/2020 | Eur J Breast Health | US | Panel of experts or regional recommendations | Breast | A consensus and a statement that may guide breast care professionals (Magee-Breast Cancer Program) |
| Teoh/2020 | World J Urol | EU | Panel of experts or regional recommendations | Bladder | Intravesical therapies recommendations |
| Ueda/2020 | J Natl Compr Canc Netw | US | Panel of experts or regional recommendations | Various | The importance of organizational structure, preparation, agility, and a shared vision to provide cancer treatment to patients in the face of uncertainty and rapid change |
| Wang/2020 | Crit Care | China | Panel of experts or regional recommendations | Various | Medical management strategies |
| Werner/2020 | Otolaryngol Head Neck Surg | US | Panel of experts or regional recommendations | H&N | Care of cancer patients with head and neck cancers by US experts |
| Wu/2020 | Otolaryngol Head Neck Surg | International | Panel of experts or regional recommendations | H&N | Point of view about head and neck cancer treatment during pandemic by Toronto and Wuhan hospitals |
| Akladios/2020 | J Gynecol Obstet Hum Reprod | France | Multicenter cooperative groups | Gynecologic | Recommendations about curative treatment of cervical, ovarian and endometrial cancers according to stage and risk groups |
| Al-Shamsi/2020 | Oncologist | International | Multicenter cooperative groups | Various | Consideration of risk and benefit for active intervention in the cancer population during an infectious disease pandemic must be individualized |
| Ardura/2020 | Biol Blood Marrow Transplant | US | Multicenter cooperative groups | Hematologic cancers (stem cell transplantation) | Recommendations about hematopoietic stem cell transplantation during COVID-19 |
| Glehen/2020 | J Visc Surg | France | Multicenter cooperative groups | Peritoneal | RENAPE and BIG-RENAPE guidelines for peritoneal cancers |
| Penel/2020 | Ann Oncol | France | Multicenter cooperative groups | Sarcoma | General recommendations for the management of sarcoma patients |
| Thureau/2020 | J Bone Oncol | International | Multicenter cooperative groups | Bone metastasis | The COVID-19 crisis requires a reorganization of the health system, particularly in radiotherapy. A single 8Gy fraction is recommended for most clinical situations |
| Thoracic Surgery Outcomes Research Network/2020 | Ann Thorac Surg | US | Multicenter cooperative groups | Thoracic | A document to offer guidance and to facilitate decisions when caring for patients with thoracic malignancies during the COVID-19 pandemic |
| Whisenant/2020 | Cancer Cell | International | Multicenter cooperative groups | Thoracic Cancers | Evaluation of the impact of COVID-19 infection in patients with non-small cell lung cancer, small cell lung cancer, mesothelioma, thymic epithelial tumors, and thoracic carcinoid/neuroendocrine tumors. Thoracic Cancers International COVID-19 collaboration |
| Dingemans/2020 | J Thorac Oncol | International | Multicenter cooperative groups | Lung | Multidisciplinary recommendations for the treatment of lung cancer during COVID-19 pandemic |
| Di Fiore/2020 | Dig Liver Dis | France | Multicenter cooperative groups | Gastrointestinal tumors | Alternatives in the management of digestive cancers during COVID-19 pandemic. Clinical point of view of the French Intergroup |
| Hungria/2020 | Hematol Transfus Cell Ther | Brazil | Multicenter cooperative groups | MM | Recommendations for the treatment of MM during COVID-19 pandemic. Recommendations from the ABHH Monoclonal Gammopathies Committee |
| Geskin/2020 | J Am Acad Dermatol | USA | Multicenter cooperative group | Skin | Recommendations for the treatment of skin cancer patients during COVID-19 pandemic |
| Spolverato/2020 | Surgery | Italy | Multicenter cooperative group | Surgical cancer patients | Management of surgical patients with cancer |
| De Azambuja/2020 | ESMO Open | EU | Multicenter cooperative group | Breast | Recommendations for the treatment of breast cancer patients during COVID-19 pandemic |
| Catanese/2020 | ESMO Open | EU | Multicenter cooperative group | Pancreas | Recommendations for the treatment of pancreatic cancer patients during COVID-19 pandemic |
| Jozaghi/2020 | Head Neck | USA | Multicenter cooperative group | Endocrine | Recommendations for the treatment of endocrine surgical cancer patients during COVID-19 pandemic |
| Jereczek-Fossa/2020 | Clin Oncol | Italy | Multicenter cooperative group | Various | Online questionnaires on how Lombardy radiotherapy departments have coped with COVID-19 pandemic |
| Van De Haar/2020 | Nat Med | EU | Multicenter cooperative group | Various | A report on how seven comprehensive cancer centers in EU have organized their healthcare systems during COVID-19 pandemic |
| Al-Rashdan/2020 | Adv Radiat Oncol | Canada | Multicenter cooperative group | Breast | Use of hypo-fractionation and accelerated partial breast irradiation for breast cancer during COVID-19 pandemic |
| Bartlett/2020 | Ann Surg Oncol | US | Official guidelines or health authorities’ recommendations | Various | Considerations in management of cancer surgery cases during the COVID-19 pandemic |
| Bitar/2020 | Future Oncol | Lebanon | Official guidelines or health authorities’ recommendations | Various | Recommendations for daily practice for the care of cancer patients relate to prevention of contamination, prioritization of patients, avoiding overcrowded clinics, ensuring the separation of oncology departments from other units, and management of palliative care patients |
| Coles/2020 | Clin Oncol | International | Official guidelines or health authorities’ recommendations | Breast | Recommendations where RT is minimized and targeted to those with the highest risk of relevant breast recurrence, to protect our patients and health care professionals from potential exposure to COVID-19 as well as reducing the workload for health care providers and/or infrastructure |
| Kimmig/2020 | J Gynecol Oncol | International | Official guidelines or health authorities’ recommendations | Gynecologic | Robot assisted surgery (RAS) may help to reduce hospital stay for patients that urgently need complex-oncological-surgery, thus making room for COVID-19 patients |
| Ribal/2020 | Eur Urol | EU | Official guidelines or health authorities’ recommendations | Urologic | Position of EAU and reporting of guidelines recommendations during pandemic |
| Thomson/2020 | Int J Radiat Oncol Biol Phys | International | Official guidelines or health authorities’ recommendations | H&N | This statement attempts to address the immediate impacts of the COVID-19 pandemic on HNC clinical practice. Practice recommendations for risk-adapted head and neck cancer radiotherapy |
| Troost/2020 | Radiother Oncol | US + EU | Official guidelines or health authorities’ recommendations | Lung | ASTRO and ESTRO recommendations |
| Von Lillenfeld-Toal/2020 | Leukemia | EU | Official guidelines or health authorities’ recommendations | Various | EHA Infectious Disease Scientific Working Group recommendations of cancer treatment |
| Yahalom/2020 | Blood | International | Official guidelines or health authorities’ recommendations | Hematologic | Recommendations for alternative radiation treatment schemes: maintaining clinical efficacy and safety by increasing the dose per fraction while reducing the number of daily treatments |
| You/2020 | Lancet Oncol | France | Official guidelines or health authorities’ recommendations | Various | In a situation where available care facilities are scarce, prioritization should involve the patients managed with curative-intent therapeutic strategies, and those with a life expectancy of 5 years or more, acknowledging that final decisions lie with the referring clinicians |
| Zaorsky/2020 | Adv Radiat Oncol | US and UK | Official guidelines or health authorities’ recommendations | Prostate | A RADS framework (Remote visits, and Avoidance, Deferment, and Shortening of radiotherapy) was created and applied to determine the appropriate management for men with prostate cancer during the global COVID-19 pandemic |
| Chan/2020 | Support Care Cancer | USA/Canada/Australia | Official guidelines or health authorities’ recommendations | Various | Three priority areas of survivorship care identified: triage of immediate needs of cancer survivors, tele-survivorship care, alternative models of care. A qualitative survey of Multinational Association of Supportive Care in Cancer (MASCC) Survivorship Study Group |
| Bergsland/2020 | Pancreas | USA | Official guidelines or health authorities’ recommendations | Neuroendocrine tumors (NETs)/carcinomas (NECs) | Recommendations for the treatment of NETs/NECs during COVID-19 pandemic: Official guidelines of the North American Neuroendocrine Tumor Society |
| Terpos/2020 | Leukemia | EU | Official guidelines or health authorities’ recommendations | Multiple Myeloma (MM) | Recommendations for the treatment of MM during COVID-19 pandemic: European Myeloma Network (EMN) Consensus Paper |
| Nguyen/2020 | Cancers | International | Official guidelines or health authorities’ recommendations | Various | Practice proposal for the management of older cancer patients during COVID-19 pandemic. Proposal of the International Geriatric Radiotherapy Group |
| Desideri/2020 | J Geriatr Oncol | International | Official guidelines or health authorities’ recommendations | Various | Recommendations for the treatment of older cancer patients during COVID-19 pandemic. Global perspective of the Young International Society of Geriatric Oncology (SIOG) |
| Vecchione/2020 | ESMO Open | EU | Official guidelines or health authorities’ recommendations | Colorectal | ESMO recommendations: redefinition of diagnostic and therapeutic algorithms in colorectal cancer |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaniboni, A.; Ghidini, M.; Grossi, F.; Indini, A.; Trevisan, F.; Iaculli, A.; Dottorini, L.; Moleri, G.; Russo, A.; Vavassori, I.; et al. A Review of Clinical Practice Guidelines and Treatment Recommendations for Cancer Care in the COVID-19 Pandemic. Cancers 2020, 12, 2452. https://doi.org/10.3390/cancers12092452
Zaniboni A, Ghidini M, Grossi F, Indini A, Trevisan F, Iaculli A, Dottorini L, Moleri G, Russo A, Vavassori I, et al. A Review of Clinical Practice Guidelines and Treatment Recommendations for Cancer Care in the COVID-19 Pandemic. Cancers. 2020; 12(9):2452. https://doi.org/10.3390/cancers12092452
Chicago/Turabian StyleZaniboni, Alberto, Michele Ghidini, Francesco Grossi, Alice Indini, Francesca Trevisan, Alessandro Iaculli, Lorenzo Dottorini, Giovanna Moleri, Alessandro Russo, Ivano Vavassori, and et al. 2020. "A Review of Clinical Practice Guidelines and Treatment Recommendations for Cancer Care in the COVID-19 Pandemic" Cancers 12, no. 9: 2452. https://doi.org/10.3390/cancers12092452
APA StyleZaniboni, A., Ghidini, M., Grossi, F., Indini, A., Trevisan, F., Iaculli, A., Dottorini, L., Moleri, G., Russo, A., Vavassori, I., Brevi, A., Rausa, E., Boni, L., Dondossola, D., Valeri, N., Ghidini, A., Tomasello, G., & Petrelli, F. (2020). A Review of Clinical Practice Guidelines and Treatment Recommendations for Cancer Care in the COVID-19 Pandemic. Cancers, 12(9), 2452. https://doi.org/10.3390/cancers12092452









