Combination of Peri-Tumoral and Intra-Tumoral Radiomic Features on Bi-Parametric MRI Accurately Stratifies Prostate Cancer Risk: A Multi-Site Study
Abstract
1. Introduction
2. Results
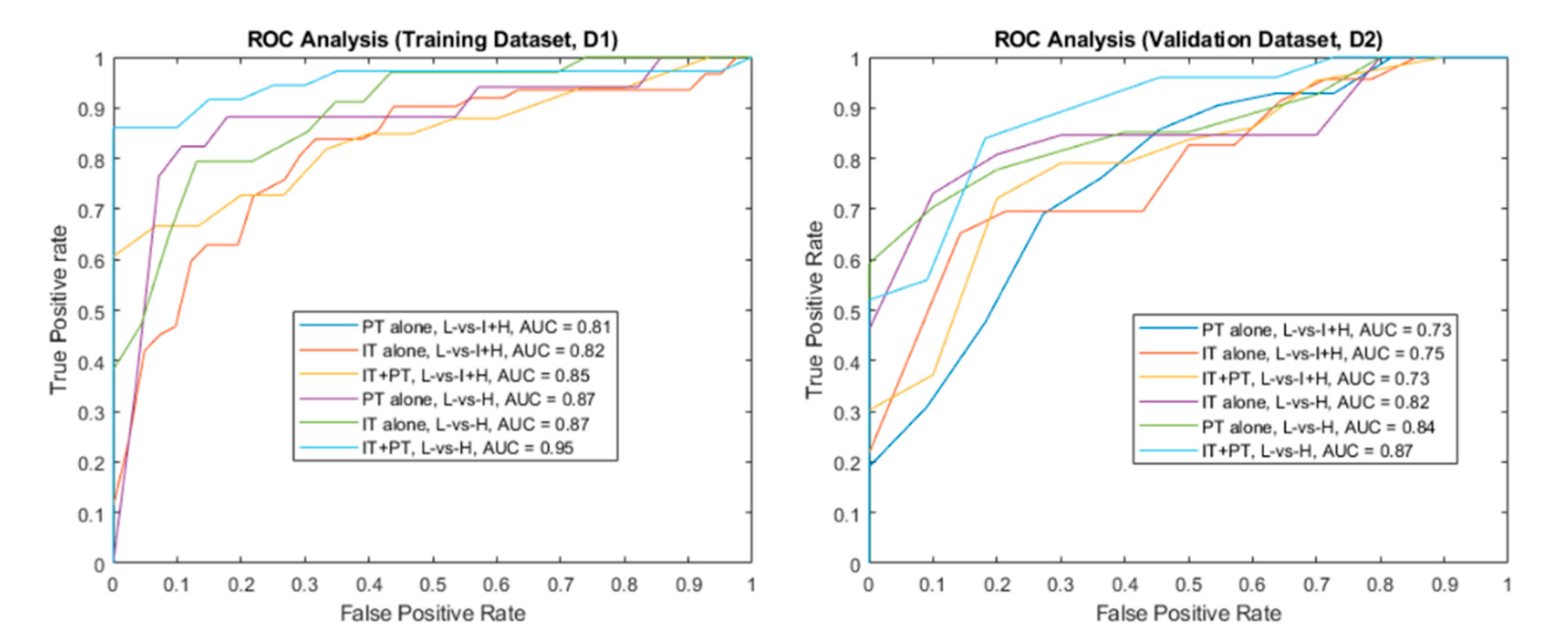
2.1. Experiment 1: Using bpmri-Derived Peri-Tumoral Radiomic Features to Stratify PCa Risk as Defined by DRCS
2.2. Experiment 2: Combining bpmri-Derived IT and PT Radiomics to Stratify PCa Risk as Defined by DRCS
2.3. Experiment 3: Comparing Radiomics-Based Risk Stratification to PI-RADS
3. Discussion
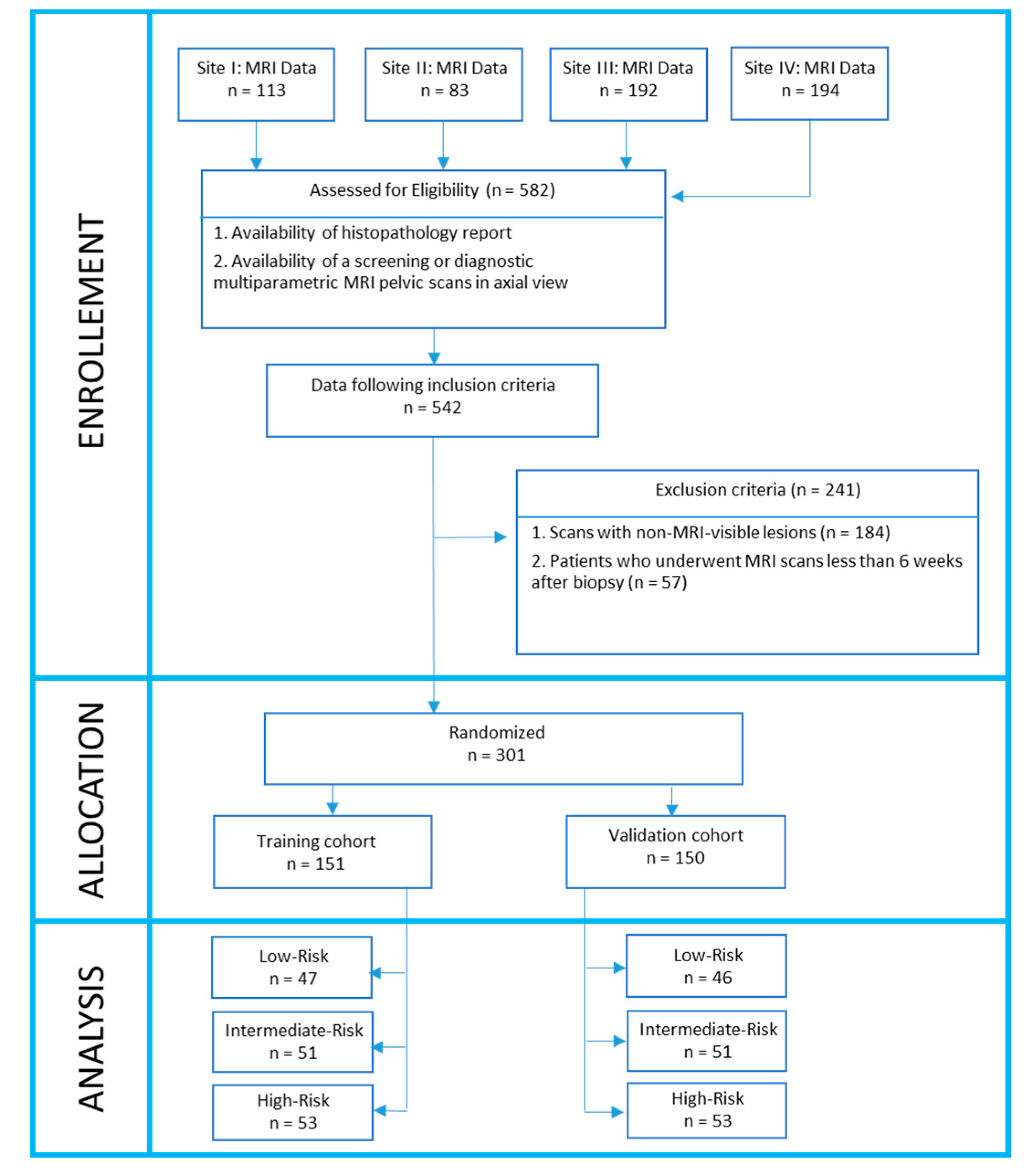
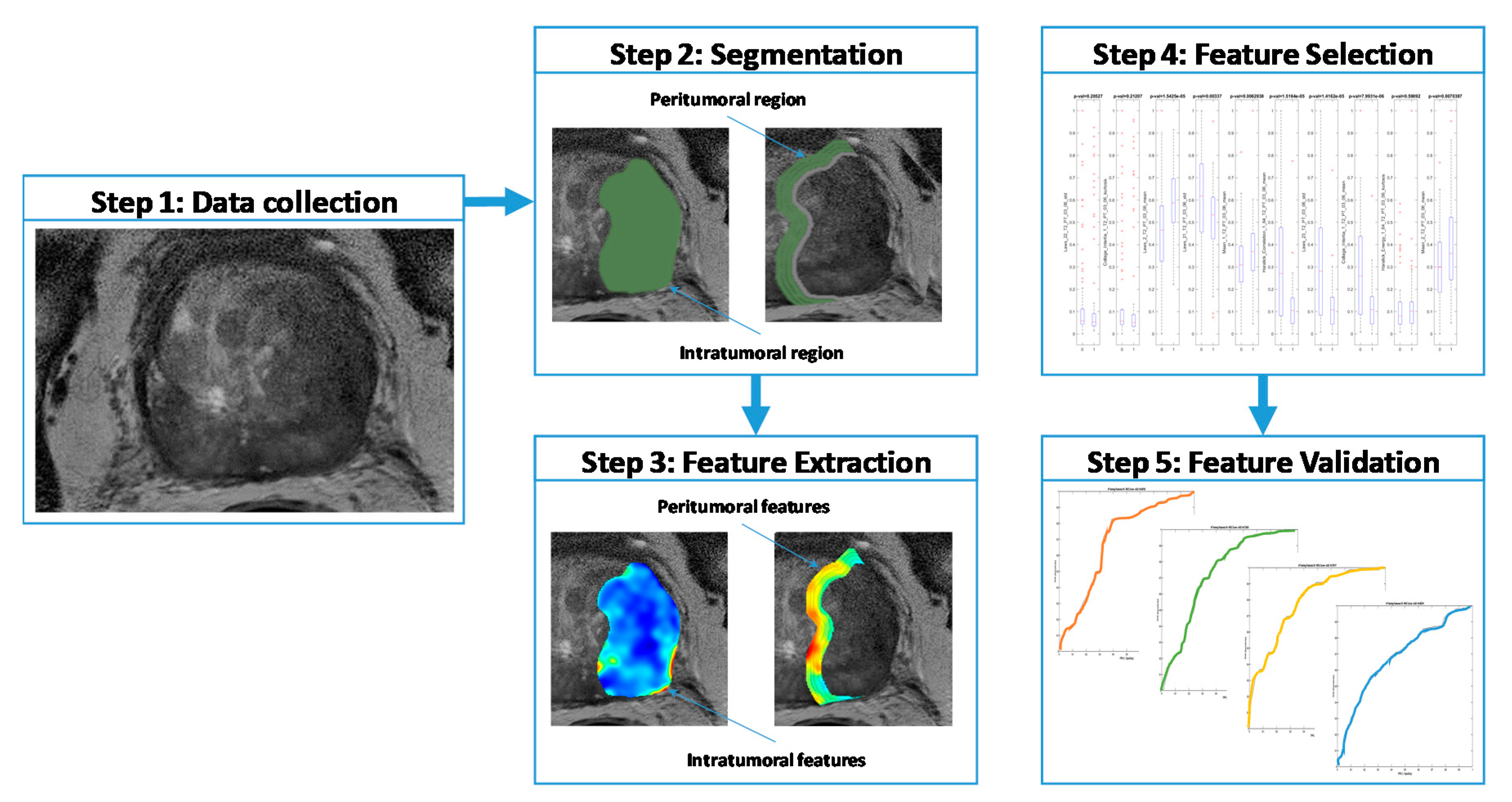
4. Materials and Methods
4.1. Dataset Description
4.2. Lesion Delineation
4.3. Pre-Processing
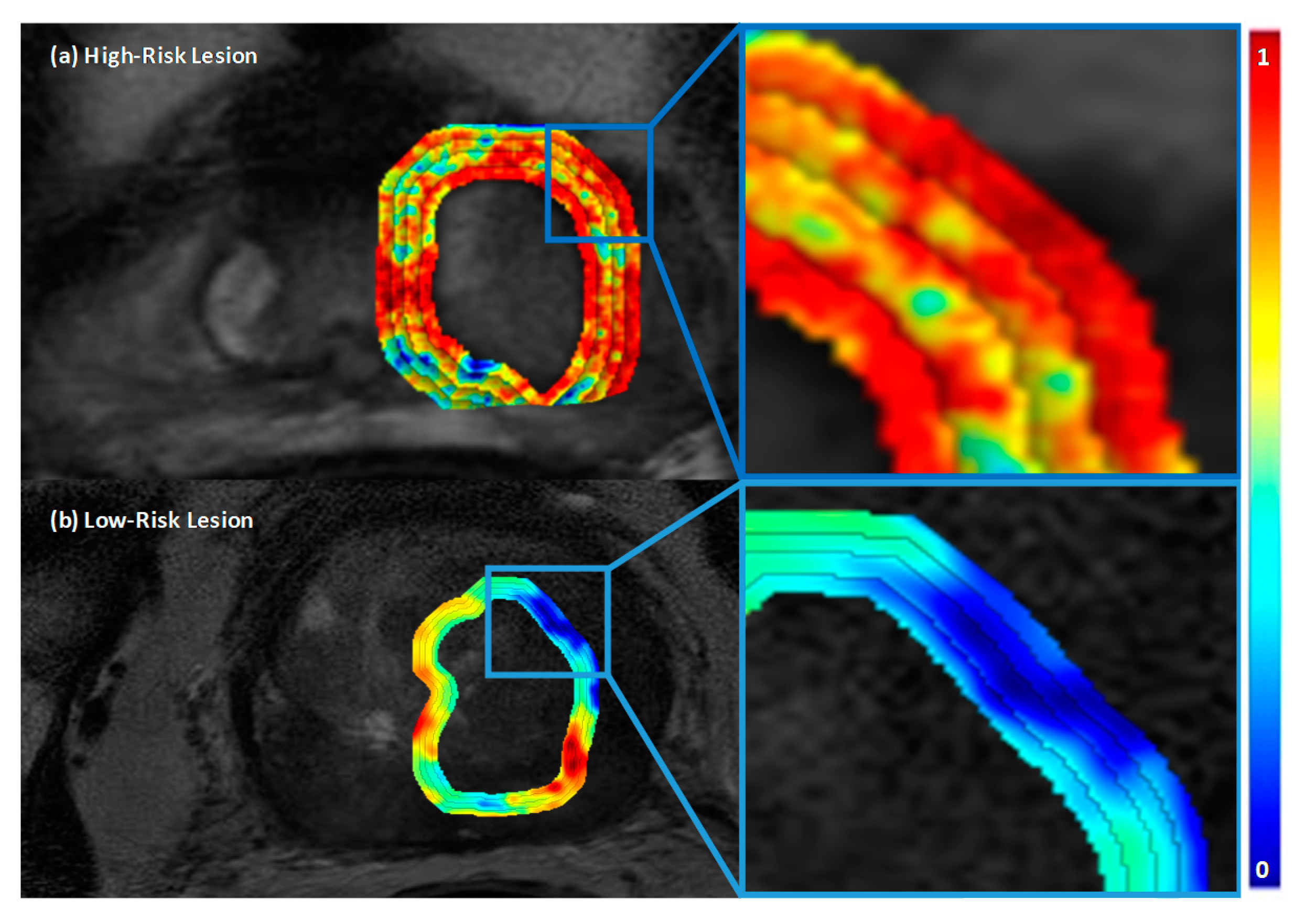
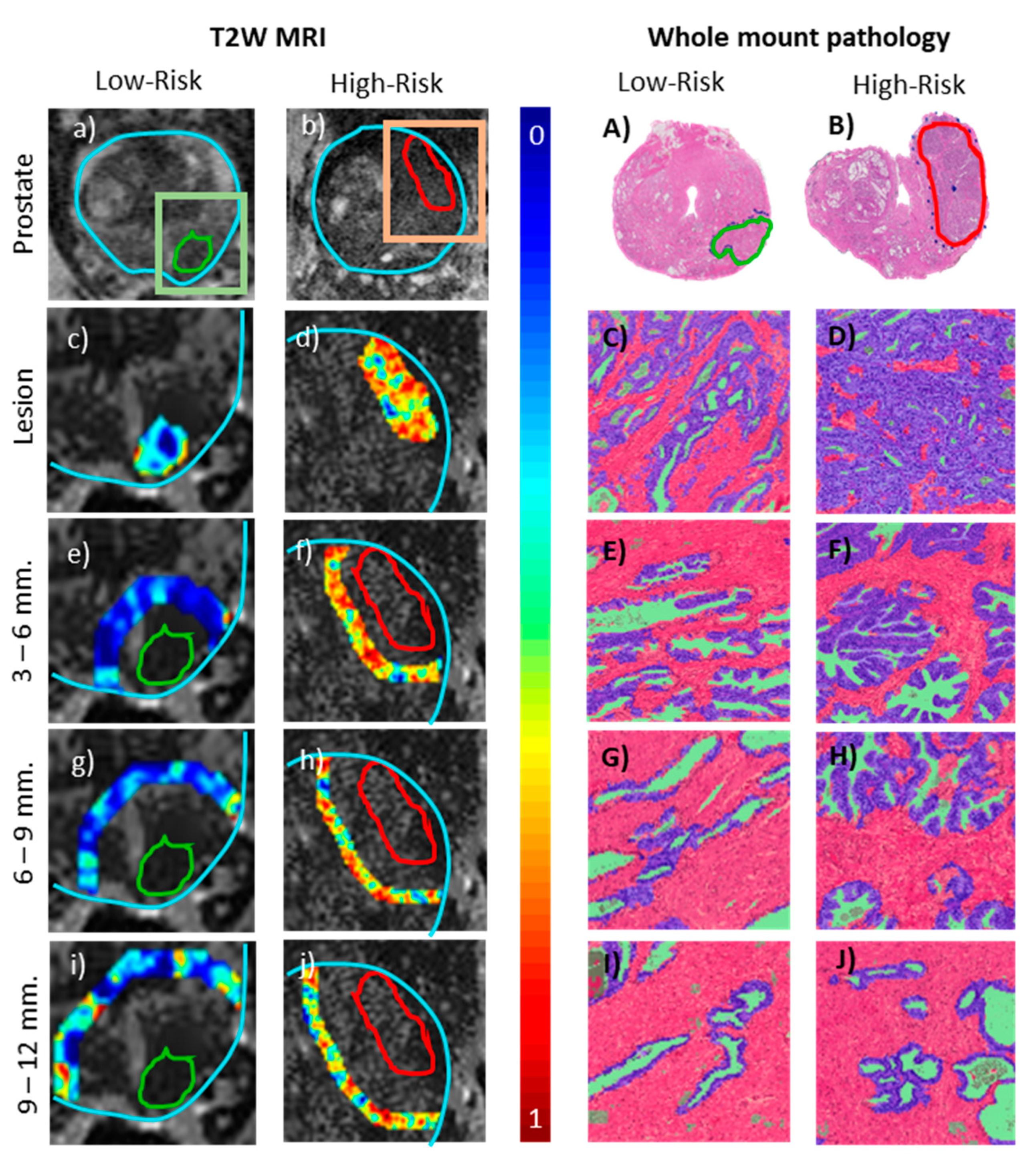
4.4. Radiomic Feature Extraction
4.5. Association with Peri-Tumoral Histopathology
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Algohary, A.; Viswanath, S.; Shiradkar, R.; Ghose, S.; Pahwa, S.; Moses, D.; Jambor, I.; Shnier, R.; Böhm, M.; Haynes, A.-M. Radiomic features on MRI enable risk categorization of prostate cancer patients on active surveillance: Preliminary findings: Radiomics Categorizes PCa Patients on AS. J. Magn. Reson. Imaging 2018, 48, 818–828. [Google Scholar] [CrossRef] [PubMed]
- Beig, N.; Khorrami, M.; Alilou, M.; Prasanna, P.; Braman, N.; Orooji, M.; Rakshit, S.; Bera, K.; Rajiah, P.; Ginsberg, J.; et al. Perinodular and intranodular radiomic features on lung CT images distinguish adenocarcinomas from granulomas. Radiology 2019, 290, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Bjurlin, M.A.; Rosenkrantz, A.B.; Lepor, H.; Taneja, S.S. Magnetic resonance imaging in prostate cancer. Transl. Androl. Urol. 2017, 6, 343–344. [Google Scholar] [CrossRef] [PubMed]
- Braman, N.; Prasanna, P.; Whitney, J.; Singh, S.; Beig, N.; Etesami, M.; Bates, D.D.B.; Gallagher, K.; Bloch, B.N.; Vulchi, M.; et al. Association of peritumoral radiomics with tumor biology and pathologic response to preoperative targeted therapy for HER2 (ERBB2) –positive breast cancer. JAMA Netw. Open 2019, 2, e192561. [Google Scholar] [CrossRef] [PubMed]
- Bulten, W.; Bándi, P.; Hoven, J.; van de Loo, R.; Lotz, J.; Weiss, N.; van de Laak, J.; van Ginneken, B.; Hulsbergen-van de Kaa, C.; Litjens, G. Epithelium segmentation using deep learning in H&E-stained prostate specimens with immunohistochemistry as reference standard. Sci. Rep. 2019, 9, 864. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-C.C.; Ackerstaff, E.; Tschudi, Y.; Jimenez, B.; Foltz, W.; Fisher, C.; Lilge, L.; Cho, H.; Carlin, S.; Gillies, R.J.; et al. Delineation of tumor habitats based on dynamic contrast enhanced MRI. Sci. Rep. 2017, 7, 9746. [Google Scholar] [CrossRef]
- Chen, T.; Li, M.; Gu, Y.; Zhang, Y.; Yang, S.; Wei, C.; Wu, J.; Li, X.; Zhao, W.; Shen, J. Prostate cancer differentiation and aggressiveness: Assessment with a radiomic-based model vs. PI-RADS v2: PCa evaluation: Radiomic vs. PI-RADS. J. Magn. Reson. Imaging 2019, 49, 875–884. [Google Scholar] [CrossRef]
- Cohen, M.S.; DuBois, R.M.; Zeineh, M.M. Rapid and effective correction of RF inhomogeneity for high field magnetic resonance imaging. Hum. Brain Mapp. 2000, 10, 204–211. [Google Scholar] [CrossRef]
- D’Amico, A.V.; Whittington, R.; Malkowicz, S.B.; Schultz, D.; Blank, K.; Broderick, G.A.; Tomaszewski, J.E.; Renshaw, A.A.; Kaplan, I.; Beard, C.J.; et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 1998, 280, 969–974. [Google Scholar] [CrossRef]
- Fehr, D.; Veeraraghavan, H.; Wibmer, A.; Gondo, T.; Matsumoto, K.; Vargas, H.A.; Sala, E.; Hricak, H.; Deasy, J.O. Automatic classification of prostate cancer Gleason scores from multiparametric magnetic resonance images. Proc. Natl. Acad. Sci. USA 2015, 112, E6265–E6273. [Google Scholar] [CrossRef]
- Ginsburg, S.B.; Algohary, A.; Pahwa, S.; Gulani, V.; Ponsky, L.; Aronen, H.J.; Boström, P.J.; Böhm, M.; Haynes, A.-M.; Brenner, P.; et al. Radiomic features for prostate cancer detection on MRI differ between the transition and peripheral zones: Preliminary findings from a multi-institutional study: Radiomic Features for Prostate Cancer Detection on MRI. J. Magn. Reson. Imaging 2017, 46, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Ginsburg, S.B.; Viswanath, S.E.; Bloch, B.N.; Rofsky, N.M.; Genega, E.M.; Lenkinski, R.E.; Madabhushi, A. Novel PCA-VIP scheme for ranking MRI protocols and identifying computer-extracted MRI measurements associated with central gland and peripheral zone prostate tumors: Quantitative MRI Features of CG and PZ Tumors. J. Magn. Reson. Imaging 2015, 41, 1383–1393. [Google Scholar] [CrossRef] [PubMed]
- Greer, M.D.; Shih, J.H.; Lay, N.; Barrett, T.; Bittencourt, L.; Borofsky, S.; Kabakus, I.; Law, Y.M.; Marko, J.; Shebel, H.; et al. Interreader variability of prostate imaging reporting and data system version 2 in detecting and assessing prostate cancer lesions at prostate MRI. Am. J. Roentgenol. 2019, 212, 1197–1205. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.C.; Long, F.H.; Ding, C. Feature selection based on mutual information criteria of max-dependency, max-relevance, and min-redundancy. IEEE Trans. Pattern Anal. Mach. Intell. 2005, 27, 1226–1238. [Google Scholar] [CrossRef]
- Hattangadi, J.; Park, C.; Rembert, J.; Klifa, C.; Hwang, J.; Gibbs, J.; Hylton, N. Breast stromal enhancement on MRI Is associated with response to neoadjuvant chemotherapy. Am. J. Roentgenol. 2008, 190, 1630–1636. [Google Scholar] [CrossRef]
- Khorrami, M.; Khunger, M.; Zagouras, A.; Patil, P.; Thawani, R.; Bera, K.; Rajiah, P.; Fu, P.; Velcheti, V.; Madabhushi, A. Combination of peri- and intratumoral radiomic features on baseline CT scans predicts response to chemotherapy in lung adenocarcinoma. Radio. Artif. Intell. 2019, 1, 180012. [Google Scholar] [CrossRef]
- Laws, K.I. Rapid Texture Identification. In Image Processing for Missile Guidance; Wien, T.F., Ed.; International Society for Optics and Photonics: San Diego, CA, USA, 1980; Volume 338. [Google Scholar] [CrossRef]
- Litjens, G.J.S.; Elliott, R.; Shih, N.N.; Feldman, M.D.; Kobus, T.; Hulsbergen-van de Kaa, C.; Barentsz, J.O.; Huisman, H.J.; Madabhushi, A. Computer-extracted features can distinguish noncancerous confounding disease from prostatic adenocarcinoma at multiparametric MR imaging. Radiology 2016, 278, 135–145. [Google Scholar] [CrossRef]
- Liu, L.; Tian, Z.; Zhang, Z.; Fei, B. Computer-aided detection of prostate cancer with MRI. Acad. Radiol. 2016, 23, 1024–1046. [Google Scholar] [CrossRef]
- Madabhushi, A.; Udupa, J.K. New methods of MR image intensity standardization via generalized scale: Generalized scale-based intensity standardization. Med. Phys. 2006, 33, 3426–3434. [Google Scholar] [CrossRef]
- McLaughlin, R.L.; Newitt, D.C.; Wilmes, L.J.; Jones, E.F.; Wisner, D.J.; Kornak, J.; Proctor, E.; Joe, B.N.; Hylton, N.M. High resolution in vivo characterization of apparent diffusion coefficient at the tumor-stromal boundary of breast carcinomas: A pilot study to assess treatment response using proximity-dependent diffusion-weighted imaging: HR-DWI of Breast Tumor-Stromal Boundary. J. Magn. Reson. Imaging 2014, 39, 1308–1313. [Google Scholar] [CrossRef]
- Mehralivand, S.; Shih, J.H.; Rais-Bahrami, S.; Oto, A.; Bednarova, S.; Nix, J.W.; Thomas, J.V.; Gordetsky, J.B.; Gaur, S.; Harmon, S.A.; et al. A magnetic resonance imaging–based prediction model for prostate biopsy risk stratification. JAMA Oncol. 2018, 4, 678. [Google Scholar] [CrossRef] [PubMed]
- Nonn, L.; Ananthanarayanan, V.; Gann, P.H. Evidence for field cancerization of the prostate. Prostate 2009, 69, 1470–1479. [Google Scholar] [CrossRef] [PubMed]
- Parmar, C.; Grossmann, P.; Bussink, J.; Lambin, P.; Aerts, H.J.W.L. Machine learning methods for quantitative radiomic biomarkers. Sci. Rep. 2015, 5, 13087. [Google Scholar] [CrossRef]
- Parra, A.N.; Lu, H.; Li, Q.; Stoyanova, R.; Pollack, A.; Punnen, S.; Choi, J.; Abdalah, M.; Lopez, C.; Gage, K.; et al. Predicting clinically significant prostate cancer using DCE-MRI habitat descriptors. Oncotarget 2018, 9, 37125–37136. [Google Scholar] [CrossRef]
- Partin, A.W.; Yoo, J.; Carter, H.B.; Pearson, J.D.; Chan, D.W.; Epstein, J.I.; Walsh, P.C. The Use of Prostate Specific Antigen, Clinical Stage and Gleason Score to Predict Pathological Stage in Men with Localized Prostate Cancer. J. Urol. 1993, 150, 110–114. [Google Scholar] [CrossRef]
- Prasanna, P.; Tiwari, P.; Madabhushi, A. Co-occurrence of local anisotropic gradient orientations (CoLlAGe): A new radiomics descriptor. Sci. Rep. 2016, 6, 37241. [Google Scholar] [CrossRef] [PubMed]
- Roma, A.A.; Magi-Galluzzi, C.; Kral, M.A.; Jin, T.T.; Klein, E.A.; Zhou, M. Peritumoral lymphatic invasion is associated with regional lymph node metastases in prostate adenocarcinoma. Mod. Pathol. 2006, 19, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Schlenker, B.; Apfelbeck, M.; Armbruster, M.; Chaloupka, M.; Stief, C.G.; Clevert, D.-A. Comparison of PI-RADS 3 lesions with histopathological findings after MRI-fusion targeted biopsy of the prostate in a real world-setting. Clin. Hemorheol. Microcirc. 2019, 71, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Shiradkar, R.; Ghose, S.; Jambor, I.; Taimen, P.; Ettala, O.; Purysko, A.S.; Madabhushi, A. radiomic features from pretreatment biparametric MRI predict prostate cancer biochemical recurrence: Preliminary findings: Prostate cancer recurrence prediction. J. Magn. Reson. Imaging 2018, 48, 1626–1636. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA A Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Turkbey, B.; Choyke, P.L. PIRADS 2.0: What Is New? Diagn. Interv. Radiol. 2015, 21, 382–384. [Google Scholar] [CrossRef]
- Vargas, H.A.; Hötker, A.M.; Goldman, D.A.; Moskowitz, C.S.; Gondo, T.; Matsumoto, K.; Ehdaie, B.; Woo, S.; Fine, S.W.; Reuter, V.E.; et al. Updated prostate imaging reporting and data system (PI-RADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: Critical evaluation using whole-mount pathology as standard of reference. Eur. Radiol. 2016, 26, 1606–1612. [Google Scholar] [CrossRef] [PubMed]
- Viswanath, S.E.; Chirra, P.V.; Yim, M.C.; Rofsky, N.M.; Purysko, A.S.; Rosen, M.A.; Bloch, B.N.; Madabhushi, A. Comparing radiomic classifiers and classifier ensembles for detection of peripheral zone prostate tumors on T2-weighted MRI: A multi-site study. BMC Med. Imaging 2019, 19, 22. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.; Suh, C.H.; Kim, S.Y.; Cho, J.Y.; Kim, S.H.; Moon, M.H. Head-to-Head comparison between biparametric and multiparametric MRI for the diagnosis of prostate cancer: A systematic review and meta-analysis. Am. J. Roentgenol. 2018, 211, W226–W241. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, B.; Sun, X.; Cao, G.; Rubin, D.L.; Napel, S.; Ikeda, D.M.; Kurian, A.W.; Li, R. Heterogeneous enhancement patterns of tumor-adjacent parenchyma at MR imaging are associated with dysregulated signaling pathways and poor survival in breast cancer. Radiology 2017, 285, 401–413. [Google Scholar] [CrossRef]
- Yoo, S.; Kim, J.K.; Jeong, I.G. Multiparametric magnetic resonance imaging for prostate cancer: A review and update for urologists. Korean J. Urol. 2015, 56, 487. [Google Scholar] [CrossRef]
| Low-vs.-(Intermediate + High) | Low-vs.-High | |||
|---|---|---|---|---|
| Experiment 1 (Intra-Tumoral features) | Feature Name (Parameters) | Protocol | Feature Name (Parameters) | Protocol |
| Mean (1) | ADC | Gabor (3, θ = 2.9 rad) | T2W | |
| Gabor (3, θ = 0.0 rad) | T2W | Mean (3) | T2W | |
| Mean (2) | ADC | Haralick (Sum of Average) | ADC | |
| Haralick (Sum of Average) | ADC | Mean (1) | ADC | |
| Variance (2) | ADC | Gabor (5, θ = 0.0 rad) | ADC | |
| Gabor (λ = 5, θ = 0.0 rad) | ADC | Gabor (3, θ = 0.1 rad) | ADC | |
| Gabor (λ = 4, θ = 0.0) | ADC | Gabor (3, θ = 0.7 rad) | T2W | |
| Gabor (λ = 3, θ = 0.1 rad) | ADC | Gabor (3, θ = 1.8 rad) | ADC | |
| Gabor (λ = 3, θ = 1.8 rad) | T2W | Gabor (3, θ = 2.4 rad) | ADC | |
| Gabor (λ = 3, θ = 2.4 rad) | ADC | Mean (2) | ADC | |
| Experiment 2 (Peri-Tumoral features) | Haralick (Entropy difference) (3–6 mm) | T2W | Haralick (Info measure 1) (3–6 mm) | T2W |
| Haralick (Momentum difference) (6–9 mm) | ADC | Haralick (Sum of Entropy) (3–6 mm) | ADC | |
| Gabor (lambda = 3, theta = 0 rad) (9–12 mm) | T2W | Haralick (Correlation) (3–6 mm) | ADC | |
| Haralick (Sum of Entropy) (3–6 mm) | T2W | Laws 9 (9–12 mm) | ADC | |
| Haralick (Entropy difference) (3–6 mm) | ADC | Laws (12) (3–6 mm) | T2W | |
| Haralick (Correlation) (3–6 mm) | ADC | Haralick (Info measure 2) (3–6 mm) | T2W | |
| Haralick (Entropy difference) (6–9 mm) | ADC | Haralick (Entropy) (3–6 mm) | ADC | |
| Gabor (λ = 3, θ = 0 rad) (6–9 mm) | ADC | Laws (11) (9–12 mm) | ADC | |
| Haralick (Info measure 2) (9–12 mm) | ADC | Laws (4) (9–12 mm) | ADC | |
| Haralick (Entropy difference) (6–9 mm) | T2W | Haralick (Energy) | ADC | |
| Experiment 3 (Intra- and Peri-Tumoral features) | Laws (15) | T2W | Gabor (6 Hz, 2.0 rad) (3–6 mm) | T2W |
| Canny | T2W | Gabor (6 Hz, 2.8 rad) (3–6 mm) | T2W | |
| Collage (Entropy) (6–9 mm) | ADC | Haralick (Momentum Sum) | ADC | |
| Laws (11) | ADC | Gabor (6 Hz, 1.8 rad) | ADC | |
| Haralick (Entropy) | ADC | Mean (9–12 mm) | T2W | |
| Collage | ADC | Gabor (2.5 Hz, 0.4 rad) | T2W | |
| Haralick (Info measure 1) (3–6 mm) | T2W | Gabor (3 Hz, 0.4 rad) | T2W | |
| Laws (17) (3–6 mm) | ADC | Gabor (3.5 Hz, 0.4 rad) | T2W | |
| Haralick (Info measure 2) | T2W | Gabor (5 Hz, 1.6 rad) | ADC | |
| Haralick (Info measure 2) | ADC | Gabor (6 Hz, 1.6 rad) | ADC | |
| D’Amico Classification | PI-RADS v2 | Total | Combined Radiomic Features (IT + PT) | ||
|---|---|---|---|---|---|
| High (3–5) | Low (1–2) | High | Low | ||
| High-Risk | 41 | 12 | 53 | 37 | 16 |
| Intermediate-Risk | 33 | 18 | 51 | 28 | 23 |
| Low-Risk | 15 | 31 | 46 | 4 | 42 |
| Total | 89 | 61 | 150 | 69 | 81 |
| Cohort | Institution 1 | Institution 2 | Institution 3 | Institution 4 |
| Number of Subjects | 32 | 73 | 45 | 81 |
| Age (mean ± SD) | 65.1 ± 6.4 | 62.6 ± 10.8 | 64.3 ± 5.6 | 68.5 ± 8.05 |
| PSA (mean ± SD) ng/mL | 6.9 ± 5.8 | 5.9 ± 4.2 | 9.8 ± 6.3 | 8.08 ± 6.1 |
| Lesion size (mean ± SD) cm3 | 1.10 ± 1.79 | 0.67 ± 0.82 | 1.02 ± 1.16 | 0.86 ± 0.66 |
| Gleason Scores (number of lesions) | 6(8), 7(8), 8(11), 9(5) | 6(23), 7(8), 8(9), 9(33) | 6(8), 7(11), 8(16), 9(10) | 6(38), 7(24), 8(13), 9(6) |
| PI-RADS (mean ± SD) | 4.19 ± 1.05 | 3.65 ± 1.06 | 3.59 ± 1.35 | 2.56 ± 1.59 |
| Scanner | ||||
| Manufacturer | Philips Achieva | Siemens Verio | Siemens Verio | Philips Achieva |
| Coil type | Body coil | Endorectal coil | Body coil | Endorectal coil |
| T2-Weighted MRI | ||||
| Field-of-view (mm2) | 220 × 220 | 140 × 140 | 200 × 200 | 260 × 260 |
| Matrix size | 444 × 332 | 384 × 384 | 320 × 320 | 256 × 256 |
| Diffusion-Weighted MRI | ||||
| Field-of-view (mm2) | 180 × 180 | 260 × 186 | 260 × 260 | 260 × 260 |
| Matrix size | 128 × 128 | 116 × 162 | 128 × 128 | 128 × 128 |
| b-values (s/mm2) | 0, 1500 | 0, 50, 1000, 1500, 2000 | 0, 50, 600, 1000, 1400 | 0, 400, 900, 1500 |
| Feature Category | Feature Type | Number of Features Extracted (Total) | Relevance to Prostate Cancer |
|---|---|---|---|
| Signal Intensity | T2w images, ADC maps | 1 × 2 (2) | Cancers are usually hypo-intense on MRI |
| First Order Statistics | Mean, Median, Sobel | 9 × 2 (18) | Intensity variability |
| Gabor | Frequency, Orientation | 76 × 2 (152) | Low-level oriented edges |
| Gray-level co-occurrence | Haralick | 3 × 13 × 2 (78) | Structural heterogeneity |
| Texture Energy | Laws’ texture energy | 25 × 2 (50) | Appearance of ROI |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Algohary, A.; Shiradkar, R.; Pahwa, S.; Purysko, A.; Verma, S.; Moses, D.; Shnier, R.; Haynes, A.-M.; Delprado, W.; Thompson, J.; et al. Combination of Peri-Tumoral and Intra-Tumoral Radiomic Features on Bi-Parametric MRI Accurately Stratifies Prostate Cancer Risk: A Multi-Site Study. Cancers 2020, 12, 2200. https://doi.org/10.3390/cancers12082200
Algohary A, Shiradkar R, Pahwa S, Purysko A, Verma S, Moses D, Shnier R, Haynes A-M, Delprado W, Thompson J, et al. Combination of Peri-Tumoral and Intra-Tumoral Radiomic Features on Bi-Parametric MRI Accurately Stratifies Prostate Cancer Risk: A Multi-Site Study. Cancers. 2020; 12(8):2200. https://doi.org/10.3390/cancers12082200
Chicago/Turabian StyleAlgohary, Ahmad, Rakesh Shiradkar, Shivani Pahwa, Andrei Purysko, Sadhna Verma, Daniel Moses, Ronald Shnier, Anne-Maree Haynes, Warick Delprado, James Thompson, and et al. 2020. "Combination of Peri-Tumoral and Intra-Tumoral Radiomic Features on Bi-Parametric MRI Accurately Stratifies Prostate Cancer Risk: A Multi-Site Study" Cancers 12, no. 8: 2200. https://doi.org/10.3390/cancers12082200
APA StyleAlgohary, A., Shiradkar, R., Pahwa, S., Purysko, A., Verma, S., Moses, D., Shnier, R., Haynes, A.-M., Delprado, W., Thompson, J., Tirumani, S., Mahran, A., Rastinehad, A. R., Ponsky, L., Stricker, P. D., & Madabhushi, A. (2020). Combination of Peri-Tumoral and Intra-Tumoral Radiomic Features on Bi-Parametric MRI Accurately Stratifies Prostate Cancer Risk: A Multi-Site Study. Cancers, 12(8), 2200. https://doi.org/10.3390/cancers12082200






